Abstract
Epidemiological data indicate that obesity is a risk factor for asthma, but the mechanistic basis for this relationship is not established. Here we review data from human subjects and animal models investigating the relationship between obesity and airway hyperresponsiveness, a characteristic feature of asthma. We discuss obesity as a state of chronic systemic inflammation resulting from interactions between adipocytes and adipose tissue macrophages that are recruited to obese adipose tissue. Finally, we focus on the possibility that aspects of this inflammation, particularly obesity-related changes in TNF-α, leptin, and adiponectin, may contribute to airway hyperresponsiveness in obesity. Determining how obesity promotes asthma may uncover novel therapeutic strategies that are effective in the obese asthmatic subject.
Keywords: mice, leptin, adiponectin, tumor necrosis factor-α, adipokines
obesity is an important risk factor for asthma. Numerous (>50) cross-sectional studies performed in adults and children throughout the world have examined the impact of obesity on asthma. Virtually all demonstrate an increased prevalence of asthma in the obese and overweight (5, 19, 44, 77). Importantly, 16 of 17 prospective studies involving more than 200,000 adults and children indicate that obesity antedates asthma (5, 19, 44, 77). Obesity also worsens asthma control (56, 64, 67). The observation that either surgical or diet-induced weight loss improves asthma outcomes (51, 85) provides additional support for a relationship between obesity and asthma.
The mechanistic basis for the relationship between obesity and asthma has not been established. Below we describe the relationship between obesity and airway hyperresponsiveness (AHR), a characteristic feature of asthma, and discuss the data suggesting a role for the chronic systemic inflammation that characterizes obesity in modifying airway responsiveness in the obese.
OBESITY AND AIRWAY RESPONSIVENESS IN HUMAN SUBJECTS
Table 1 summarizes studies that have examined the impact of obesity on airway responsiveness in adults or in children. The results of these studies are mixed. Some studies have shown that obesity is a risk factor for AHR. In the only prospective longitudinal cohort study in adults, Litonjua et al. (45) reported that high initial body mass index (BMI) was associated with an increased risk of developing AHR. Similarly, weight gain was linearly related to the risk of developing AHR. Three other large cross-sectional studies in adults, one from Europe, another from China, and a third from the USA, also noted a greater prevalence of AHR or symptomatic AHR in obese vs. normal weight adults (9, 12, 84). In contrast, others have reported no increase in airway responsiveness with increasing BMI (6, 71). Similarly, inconsistent results have been obtained in children (Table 1).
Table 1.
Studies describing the impact of obesity on airway responsiveness in adults and children
| Authors (Year) (Ref. No.) | Subjects | Provocative Agent | Nature of Study | Outcome(s) |
|---|---|---|---|---|
| Studies in adults | ||||
| Celedon et al. (2001) (9) | 7,109 male and female Chinese adults | Methacholine | Cross-sectional analysis of families with at least one asthmatic member | U-shaped relationship between BMI and symptomatic AHR in both men and women |
| Schachter et al. (2001) (71) | 1,971 Australian male and female adults | Histamine | Cross-sectional analysis of randomly selected population | No effect of BMI on AHR |
| Litonjua et al. (2002) (45) | 300 US male adults | Methacholine | Prospective study of older men who developed AHR over a 3- to 4-yr period | U-shaped relationship between initial BMI and risk of developing AHR; positive linear relationship between weight gain and development of AHR |
| Chinn et al. (2002) (12) | 11,277 European male and female adults | Methacholine | Cross-sectional analysis of randomly selected population | AHR increased with BMI in men; similar trend in women, but did not reach statistical significance |
| Sood et al. (2006) (84) | 1,725 US male and female adults | Methacholine | Cross-sectional analysis of subjects referred to a pulmonary function laboratory for testing | BMI increases AHR in nonasthmatic but not in asthmatic subjects |
| Bustos et al. (2006) (6) | 1,232 Chilean male and female adults | Methacholine | Cross-sectional analysis of randomly selected population | BMI was negatively associated with AHR |
| Nicolacakis et al. (2008) (59) | 210 US male and female adults | Methacholine | Comparison of obese and nonobese asthmatic and nonasthmatic subjects | No effect of obese on AHR in either asthmatic or nonasthmatic subjects |
| Salome et al. (2008) (68) | 49 Australian male and female adults | Methacholine | Comparison of obese and nonobese nonasthmatic subjects with normal airway responsiveness | No effect of obesity on AHR as measured by FEV1 or respiratory system resistance, whereas methacholine-induced changes in respiratory system reactance were greater in obese subjects |
| Studies in children | ||||
| Tantisera et al. (2003) (88) | 1,039 US male and female children aged 5-12 yr | Methacholine | Cross-sectional analysis of asthmatic subjects in the Childhood Asthma Management Program | No effect of BMI on AHR after adjustment for baseline lung function |
| Schachter et al. (2003) (70) | 5,993 Australian children aged 7-12 yr | Histamine | Cross-sectional analysis of randomly selected population | No effect of BMI on AHR in either boys or girls |
| Huang et al. (1999) (30) | 1,459 Taiwanese male and female adolescents | Methacholine | Cross-sectional analysis of randomly selected population | AHR increased with BMI in girls but not boys |
| Hancox et al. (2005) (24) | 1,037 male and female New Zealand children | Methacholine | Prospective study of children of a birth cohort followed through 26 yr of age | No effect of BMI on AHR in girls or boys |
| Jang et al. (2006) (33) | 677 Korean male and female children | Methacholine | Cross-sectional survey | Increased AHR in obese vs. nonobese boys but not girls |
| Kaplan and Montana (1993) (38) | 17 US children | Exercise | Comparison of obese and nonobese nonasthmatic subjects | Greater exercise-induced bronchospasm in obese vs. nonobese subjects |
| Gokbel and Atas (1999) (21) | 50 Korean adolescent boys | Exercise | Comparison of obese and nonobese nonasthmatic subjects | Greater exercise-induced bronchospasm in obese vs. nonobese subjects |
| del Rio-Navarro et al. (2000) (15) | 58 Spanish children | Exercise | Comparison of obese and nonobese asthmatic and nonasthmatic subjects | Greater exercise-induced brochospasm in obese vs. nonobese asthmatic subjects and in obese vs. nonobese nonasthmatic subjects |
BMI, body mass index; AHR, airway hyperresponsiveness; FEV1, forced expiratory volume in 1 s.
Several methodological issues deserve mention here. Some studies have reported a U-shaped relationship between BMI and AHR (9, 45), with underweight as well as obesity leading to increased AHR. Failure to account for such a relationship, for example, in simple comparisons of obese vs. nonobese subjects, could negate any potential impact of BMI on AHR. At least one study also noted a differing effect of obesity on AHR in female vs. male subjects (30). Grouping subjects of both sexes together could thus obscure or attenuate any sex-specific effects of obesity. Importantly, there are numerous studies describing a role for sex in the relationship between obesity and asthma (19, 77). The method by which subjects are accrued may also impact the results. For example, choosing to examine nonasthmatic subjects specifically (59, 68) would lessen the likelihood of detecting an effect of obesity on AHR, since these subjects may have been ascertained based on their lack of AHR. Finally, and perhaps most importantly, BMI was the measure of obesity in most of the studies in Table 1. BMI is often used as a surrogate for adiposity, simply because it is available, but is not an ideal measurement. For example, in children, forced vital capacity and forced expiratory volume in 1 s (FEV1) increase with body weight (42). However, the effect is likely the result of lean body weight, since, after adjustment for height and weight, these measures of pulmonary function actually decrease with increasing percent total body fat predicted from skinfold thickness. In the obese, reductions in lung volumes do not correlate with BMI, but do correlate with fat mass, particularly truncal fat mass, as measured by dual-energy X-ray absorptiometry (10, 43). Thus using direct measures of adiposity and the distribution of adiposity, rather than BMI, might help to resolve the inconsistencies in the relationship between obesity and AHR.
The nature of the stimulus used to assess airway responsiveness may also be important. Most studies have used methacholine as the bronchoconstricting agonist (Table 1). While only three small studies have reported the impact of obesity with exercise as the bronchoconstricting agent (Table 1), all three have noted greater effects in obese vs. nonobese subjects (15, 21, 38). The pattern of bronchospasm, occurring soon after the exercise challenge, was consistent with that found in asthmatic subjects. The mechanistic bases for the bronchoconstriction induced by methacholine and that induced by exercise are not the same. Methacholine causes constriction of airway smooth muscle, whereas exercise, via changes in airway osmolarity, causes activation of mast cells and the subsequent release from these cells of several bronchoconstricting agents. Thus the relatively consistent differences between obese and nonobese subjects in exercise-induced bronchospasm could reflect greater effects of exercise on airway drying, or greater sensitivity of mast cells in obese subjects. Such changes would not be expected to impact methacholine-induced bronchoconstriction. Notably, increased numbers of mast cells were reported in the lungs of obese vs. lean mice than had been sensitized and challenged with ovalbumin (OVA) (55).
The outcome indicator used to assess airway narrowing is also important to consider. Salome et al. (68) reported no difference in methacholine-induced changes in FEV1 or respiratory system resistance in obese vs. nonobese normal subjects. In contrast, the obese subjects had greater increases in respiratory system reactance, consistent with greater airway closure and consequent hyperinflation. Indeed, a follow-up study by the same authors confirmed greater methacholine-induced airway closure in obese vs. lean subjects (11). Small airway closure, presumably in the dependent regions of the lung, has also been reported in obese subjects, even in the absence of any exogenously administered bronchoconstrictor (23, 25). The consequences of localized airway closure include dilation of the airways in the rest of the lung (since these areas now receive a greater portion of the tidal volume, leading to greater stretch of airway smooth muscle) (97). Simple measurements, such as FEV1, are unlikely to capture the complexity of these heterogeneous airway changes. Instead, studies utilizing detailed measurements of lung and airway mechanics may be necessary to fully understand the relationship between obesity and AHR.
None of the studies that have examined interactions between BMI and asthma has taken diet into account. There is evidence that dietary antioxidants and omega-3 fatty acids can affect lung function (95), and obese individuals tend to consume not just more calories, but also a less healthy diet (89). It is possible that the observed heterogeneity in the effects of obesity on AHR observed across studies (Table 1) may reflect regional differences in dietary constituents.
There is only one report of the effect of weight loss on AHR in obese individuals (1). Although there was a trend toward an improvement in AHR after 6 mo on a weight reduction program, the effect was not significant, despite an average weight loss of 17.4% of pretreatment body weight and significant improvements in flow rates and symptoms. The study was small (50 patients) and may not have been sufficiently powered to observe an effect on AHR. The authors also did not phenotype the subjects with respect to their level of atopy or airway inflammation, and it is conceivable that there are patients with particular asthma phenotypes for whom weight loss does improve AHR. Indeed, within their population, the authors noted several individuals with fairly marked reductions in airway responsiveness after weight loss.
It is important to note that AHR is very common in the general population. There are numerous environmental, genetic, and epigenetic influences on AHR, and these may obscure any additional effect of obesity without the use of large sample sizes. In contrast, such effects are nullified in studies of genetically identical mice that are often born to the same mothers and are housed together. In this context, increased airway responsiveness has been consistently noted in obese mice (see below).
OBESE MICE EXHIBIT INNATE AHR
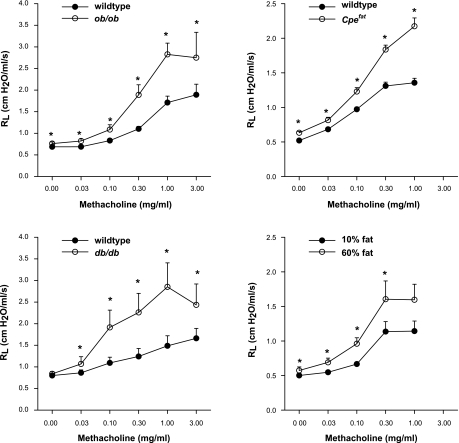
AHR to intravenous methacholine is observed in obese ob/ob and db/db that are genetically deficient in either the satiety hormone, leptin, or the leptin receptor, and in Cpefat mice that are obese because of a genetic deficiency in carboxypeptidase E, an enzyme involved in processing neuropeptides involved in eating behaviors, and in obesity induced by feeding mice a high-fat diet from the time of weaning (34, 35, 48, 66, 78, 82) (Fig. 1). The results indicate that AHR is a common feature of murine obesity. This hyperresponsiveness is independent of the bronchoconstricting agonist, since increased responses to serotonin are also observed (48). The hyperresponsiveness also seems to be a function of differences in the airways rather than the lung tissues, since, regardless of the modality of the obesity, AHR is observed when changes in airway resistance are used as the outcome indicator, but not with outcomes that reflect changes in the lung tissues (34, 35, 66, 82). While this may appear to differ from the situation in obese humans described by Salome et al. (68) (see above), it is important to note that measurements in mice were made with the chest wall open and an applied positive end-expiratory pressure of 3 cmH2O. Such interventions limit the airway closure that likely explains the greater methacholine-induced increases in measures of the lung tissue observed in obese humans (68).
Fig. 1.
Compilation of changes in pulmonary resistance (Rl) induced by intravenous methacholine in 4 types of obese mice and their lean controls. Values are means ± SE. *P < 0.05 vs. wild-type or low-fat-diet-fed control mice. Data from ob/ob and db/db mice and mice on high-fat diets are from previous publications from this laboratory [Shore et al. (78), Lu et al. (48), and Johnston et al. (34)] and are reproduced here with permission from the American Physiological Society.
In mice, both the magnitude and duration of obesity may interact to affect AHR. Ob/ob and db/db mice gain weight very quickly after weaning and are massively obese by 8 wk of age (body weight averages 175 and 150% more, respectively, than lean controls). These mice exhibit AHR even at this early age, and the magnitude of their AHR is greatest (Fig. 1). Cpefat mice gain weight more slowly, but ultimately also become substantially obese: body weight averages 23, 61, and 84% more than wild-type controls at 7, 10, and 14 wk of age, respectively. The 7-wk-old mice are not hyperresponsive, whereas the older mice are (unpublished observations). Obesity is fairly mild in mice with diet-induced obesity, and body weight is comparable (∼45% more than diet controls) at 23 and 35 wk of age (34). However, AHR is observed only in the older mice, suggesting that, with milder obesity, longer durations are required to elicit effects. Studies that incorporate not only the magnitude, but also the duration, of obesity may ultimately be required to sort out the impact of obesity on AHR in human subjects.
The mechanistic basis for the AHR observed in obese mice has not yet been established. The possibility that mechanical factors related to reductions in absolute lung volumes are involved has been previously discussed in detail (35, 76, 78). There is no overt cellular inflammation in the lungs of unchallenged obese mice (35, 48), although it is possible that normal resident immune cells are in an activated state. There is, however, increased pulmonary oxidative stress (unpublished observations), similar to the situation in the airways of obese asthmatic subjects (41). Oxidative stress contributes to many other aspects of the obese phenotype (29, 72), and oxidative stress has also been linked to asthma (40). If oxidative stress is important in the AHR observed in obese mice, it is unlikely to originate from the hyperglycemia that is a comorbidity of obesity in these models, since treating db/db mice for 2 wk with the anti-hyperglycemic agent, metformin, does not attenuate airway responsiveness in these mice (82). Below we consider data supporting the hypothesis that adipokines originating from inflamed adipose tissue may play a role in obesity-related AHR.
ADIPOKINES AND AHR
Microarray profiling of genes differentially expressed in the adipose tissue of obese vs. lean mice or humans indicates a marked obesity-related increase in expression of inflammatory genes (94, 99), including cytokines, such as TNF-α and IL-6, chemokines, such as IL-8 and monocyte chemoattractant protein-1, complement proteins, and other acute phase moieties. Together with hormones normally produced by adipocytes, including leptin and adiponectin, these adipose-derived proteins are collectively termed adipokines. The current paradigm is that these adipokines spill over into the blood. Indeed, there is substantial evidence of elevated levels of numerous proinflammatory molecules in the blood of obese vs. lean individuals that occur in proportion to the BMI and that decline with weight loss (4, 28, 32, 72, 87, 92, 93). Additional serum factors that are elevated in obesity may derive from effects of these adipokines on the vasculature (2). Circulating leukocytes are also increased (107), and it is increasingly appreciated that obesity is a state of low-grade systemic inflammation, with inflammatory activation at sites distant to the adipose tissue. Obesity-related elevations in many adipokines have been shown to correlate with the presence of obesity-related diseases, including Type 2 diabetes and atherosclerosis (18, 72), suggesting that this inflammation is functionally important. As described below, obesity-related changes in adipokines could also exacerbate airway responsiveness, precipitating asthma.
Adipose tissue macrophages (ATM) either alone or via interactions with adipocytes, appear to be the source of many of the inflammatory molecules produced by obese adipose tissue. While a few ATM exist in lean individuals, they are of the alternatively activated, M2 phenotype (49, 108) and produce few proinflammatory mediators. However, in obesity, the adipose tissue becomes infiltrated with macrophages, which can constitute upwards of 50% of the cells isolated from this tissue (94). These ATM are recruited from blood monocyte derived precursors and have an increased capacity to produce proinflammatory cytokines (49, 58, 86). Importantly, myeloid-specific knockout studies have established the importance of these ATM for some obesity-related conditions, including insulin resistance (3).
Because of the importance of ATM for the etiology of obesity-related conditions, some consideration of the factors contributing to their recruitment and activation is warranted. Necrosis of adipocytes is observed in obesity, and histological data indicate that ATM surround these necrotic cells (86). The adipose tissue of obese mice is hypoxic relative to lean mice (27, 65, 105), likely because expansion of adipose tissue mass precedes angiogenesis, leading to increasing distance between adipocytes and capillaries. One of the roles of macrophages is to phagocytose dead cells, and areas of macrophage infiltration correspond to areas of hypoxia, suggesting that hypoxia may initiate adipocyte cell death (65). Indeed, adipose tissue hypoxia appears to contribute to adipose inflammatory gene expression in obesity (27, 105), as well as to obesity-related reductions in adiponectin (27). These changes appear to be at least partly the result of increased expression of the hypoxia-dependent transcription factor, hypoxia-inducible factor-1α (104). In asthmatic subjects, systemic hypoxemia resulting from heterogeneous airway narrowing could exacerbate local adipocyte hypoxia, increasing cell death, and amplifying the attendant adipose-derived systemic inflammation. There is also increasing evidence that Toll-like receptor 4 (TLR4) activation may contribute to activation of ATM. Both adipocytes and macrophages express TLR4, and saturated fatty acids, especially C14:0, C16:0, and C18:0, stimulate TLR4 in these cells, leading to IL-6 and TNF-α expression (74). Also, high-fat diet feeding results in increased blood concentrations of endotoxin, a TLR4 ligand, likely as a result of its increased transport across the intestines, resulting from diet-induced changes in the intestinal microbiota (8).
Adipokines released into the serum from inflamed adipose tissue may circulate to the lungs and contribute to AHR [see recent reviews (75–77)]. For example, obesity increases the serum concentrations of TNF-α (28). Exogenous administration of TNF-α has been shown to induce AHR (90), while anti-TNF-α antibodies have been shown to inhibit allergen-induced AHR in mice (39). AHR induced by the air pollutant, ozone, is also attenuated in TNF receptor-deficient mice (79).
Other adipose-derived inflammatory moieties may also contribute to AHR. VEGF is also elevated in the serum of obese individuals (83), and VEGF expression in the airways of asthmatic subjects correlates inversely with airway caliber (26). Serum levels of plasminogen activator inhibitor-1 (PAI-1), an important inhibitor of both fibrinolysis and plasmin activation, are increased in the obese and decrease with weight loss (57). PAI-1 is a reasonable asthma candidate gene (50). PAI-1 is required for the AHR induced by LPS in mice (69), perhaps via effects on extracellular matrix turnover and remodeling, since PAI-1 is also required for the increased collagen and fibrin deposition that occurs in the airways after chronic allergen challenge in mice (50).
Below we focus on the possible roles of obesity-related increases in leptin and decreases in adiponectin in AHR.
Leptin
Leptin is an adipose-derived satiety hormone that is markedly elevated in obesity (34, 35). Leptin is also proinflammatory (18). Adipocyte production of leptin can be induced by infectious and inflammatory stimuli, including TNF-α and IL-1β (22). We have reported that allergen challenge to the airways of sensitized mice also increases serum leptin (80). Leptin stimulates proinflammatory cytokine production from monocytes and macrophages (20, 46, 52) and promotes formation of reactive oxygen species in neutrophils (7). Exogenous administration of leptin also augments cytokine and chemokine production in the lungs of mice after acute ozone exposure (78).
To address the relationship between leptin and AHR, we implanted microosmotic pumps, delivering a constant infusion of leptin or saline into lean, OVA-sensitized mice and challenged the mice with aerosolized OVA or PBS for several days (80). Compared with saline, delivery of leptin resulted in an approximate twofold increase in serum leptin. In mice challenged with aerosolized PBS, no effect of leptin was observed on airway responsiveness to methacholine, indicating that leptin alone does not cause AHR. However, leptin did augment the AHR induced by OVA aerosol challenge, even though it did not affect OVA-induced airway eosinophilia or T helper type 2 (Th2) cytokine expression (80). Taken together, the results suggest that leptin is capable of increasing airway responsiveness, but only in concert with other inflammatory agents. The data also indicate that leptin does not promote expression of Th2 cytokines, consistent with data from other investigators (47). Leptin receptors are expressed on CD4+ T lymphocytes, and leptin does promote survival, induce proliferation, and increase cytokine production from these cells, but the effect is on Th1, not Th2, cytokines (47, 63). Consistent with these data, a greater percentage of IFN-γ secreting CD4+ T cells is observed in blood of obese vs. lean children and correlates with serum leptin (61). In contrast, leptin appears to inhibit proliferation of regulatory T cells (14) and could promote asthma in that manner.
It is possible that the observed effects of leptin on airway responsiveness (80) are mediated via the innate immune system. Exogenous administration of leptin to lean mice before acute O3 exposure increases some aspects of their subsequent inflammatory responses (78), a response that is known to involve activation of TLRs (96). In contrast, reduction in endogenous leptin by fasting in lean mice does not affect O3-induced generation of acute phase cytokines and chemokines (36), suggesting that leptin-related increases in O3-induced inflammation require leptin concentrations above those normally observed in lean mice. Such increases are observed in obesity. However, even though leptin has the potential to augment airway responsiveness (80), it unlikely that leptin accounts for AHR observed in obese mice, since this AHR is observed both in ob/ob and db/db mice with leptin or leptin-receptor deficiency (48, 66, 78, 82), and in Cpefat mice and mice with diet-induced obesity that have marked increases in serum leptin (34, 35).
Adiponectin
In contrast to other adipokines, plasma adiponectin and adipose tissue adiponectin expression decline in obesity and rise again following weight loss (62, 73, 102). Obesity-related changes in adiponectin are likely to be functionally important, since exogenous administration of adiponectin protects obese mice against obesity-related diseases, including Type 2 diabetes and atherosclerosis (101). Adiponectin was originally identified as an energy-regulating hormone (13, 102), but also has effects on hematopoietic cells. Intriguingly, adiponectin has both pro- and anti-inflammatory effects, depending on the nature of the inciting stimulus (17). For example, adiponectin reduces TNF-α-induced NF-κB activation in endothelial cells (60) and decreases LPS-induced TNF-α production in macrophages (106). Adiponectin has also been shown to increase expression of certain anti-inflammatory moieties, including IL-10 and the endogenous IL-1 receptor antagonist (98). In contrast, adiponectin causes a dose-dependent increase in IL-6 release from synovial fibroblasts and macrophages (16, 91). Adiponectin receptors are expressed on airway epithelial cells, and adiponectin induces IL-8 release in these cells (54). Hence, the precise role of adiponectin may depend on the nature of the stimulus and the target cells affected.
To examine a possible role for adiponectin in the relationship between obesity and asthma, we implanted mini-Alzet pumps subcutaneously in lean OVA-sensitized mice. The pumps provided a continuous infusion of full-length murine recombinant adiponectin that resulted in an ∼50% increase in adiponectin vs. mice implanted with pumps delivering buffer. When the mice were subsequently challenged with aerosolized OVA, there were increases in airway responsiveness, in BAL eosinophils, and in BAL and lung Th2 cytokines in the buffer-treated mice, but these changes were either markedly attenuated or completely absent in mice treated with adiponectin (81). Recent data from others support our findings: OVA sensitization and challenge result in greater eosinophilia in adiponectin deficient vs. wild-type mice (53).
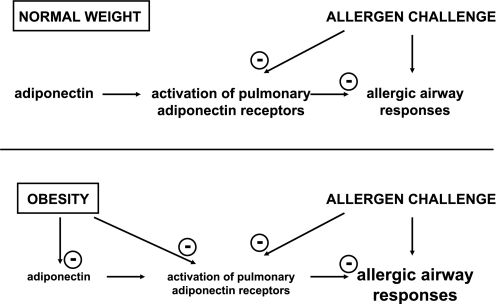
We have also reported declines in the mRNA expression of the three currently identified adiponectin binding proteins, adiponectin receptor 1 (adipoR1), adipoR2, and T-cadherin (31, 100), in lungs of OVA-challenged mice (81), indicating that the allergic airway may also be adiponectin resistant. Decreased expression of adipoR1 and adipoR2 and declines in adiponectin-induced AMP kinase activation are also observed in skeletal muscle and adipose tissue of obese mice (37, 103), indicating that adiponectin resistance also characterizes the obese state. Thus, especially when obesity-related declines in serum adiponectin are considered, the obese asthmatic subject is likely to have substantial defects in this important immunomodulatory pathway that promote allergic airway responses, including AHR (Fig. 2). Nevertheless, adiponectin therapy for asthma seems an unlikely therapeutic option. The concentration of adiponectin in the blood is very high, even in the obese, and adiponectin is a large and complex molecule with multiple oligomers. However, it is conceivable that agonists for the receptors that mediate the beneficial effects of adiponectin described above could be developed. It is also important to note that thiazolidinediones, currently used as therapeutics in Type 2 diabetes, act in part by increasing circulating adiponectin levels (62) and may ultimately prove useful in the treatment in the obese asthmatic subject.
Fig. 2.
Schematic representation of changes in the role of adiponectin in allergic airway responses in the obese state. In the airways of lean individuals, adiponectin acts on adiponectin receptors to inhibit allergic airway responses. The effects of adiponectin are somewhat inhibited by allergen-induced reductions in the expression of adiponectin receptors. In obesity, there are reductions in the levels of circulating adiponectin, as well as further reductions in adiponectin receptors, limiting the beneficial effects of adiponectin and thus amplifying allergic airway responses.
CONCLUSIONS
Obesity is an important risk factor for asthma, but the mechanistic basis for this relationship remains to be established. The adipose tissue of obese individuals is infiltrated with activated macrophages that interact with adipocytes to promote a state of systemic inflammation. Changes in many adipose-derived inflammatory moieties, including TNF-α, leptin, and adiponectin, have the capacity to promote AHR and may thus contribute to asthma in the obese.
GRANTS
This work was supported by National Institute of Environmental Health Sciences Grants ES-013307 and ES-000002 and National Heart, Lung, and Blood Institute Grant HL-084044.
DISCLOSURES
No conflicts of interest are declared by the author.
REFERENCES
- 1. Aaron SD, Fergusson D, Dent R, Chen Y, Vandemheen KL, Dales RE. Effect of weight reduction on respiratory function and airway reactivity in obese women. Chest 125: 2046–2052, 2004 [DOI] [PubMed] [Google Scholar]
- 2. Adya R, Tan BK, Punn A, Chen J, Randeva HS. Visfatin induces human endothelial VEGF and MMP-2/9 production via MAPK and PI3K/Akt signaling pathways: novel insights into visfatin angiogenesis. Cardiovasc Res 78: 356–365, 2008 [DOI] [PubMed] [Google Scholar]
- 3. Arkan MC, Hevener AL, Greten FR, Maeda S, Li ZW, Long JM, Wynshaw-Boris A, Poli G, Olefsky J, Karin M. IKK-beta links inflammation to obesity-induced insulin resistance. Nat Med 11: 191–198, 2005 [DOI] [PubMed] [Google Scholar]
- 4. Bastard JP, Maachi M, Lagathu C, Kim MJ, Caron M, Vidal H, Capeau J, Feve B. Recent advances in the relationship between obesity, inflammation, and insulin resistance. Eur Cytokine Netw 17: 4–12, 2006 [PubMed] [Google Scholar]
- 5. Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med 175: 661–666, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bustos P, Amigo H, Oyarzun M, Rona RJ. Is there a causal relation between obesity and asthma? Evidence from Chile. Int J Obes Relat Metab Disord 29: 804–809, 2005 [DOI] [PubMed] [Google Scholar]
- 7. Caldefie-Chezet F, Poulin A, Tridon A, Sion B, Vasson MP. Leptin: a potential regulator of polymorphonuclear neutrophil bactericidal action? J Leukoc Biol 69: 414–418, 2001 [PubMed] [Google Scholar]
- 8. Cani PD, Bibiloni R, Knauf C, Waget A, Neyrinck AM, Delzenne NM, Burcelin R. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57: 1470–1481, 2008 [DOI] [PubMed] [Google Scholar]
- 9. Celedon JC, Palmer LJ, Litonjua AA, Weiss ST, Wang B, Fang Z, Xu X. Body mass index and asthma in adults in families of subjects with asthma in Anqing, China. Am J Respir Crit Care Med 164: 1835–1840, 2001 [DOI] [PubMed] [Google Scholar]
- 10. Chambers EC, Heshka S, Huffaker LY, Xiong Y, Wang J, Eden E, Gallagher D, Pi-Sunyer FX. Truncal adiposity and lung function in older black women. Lung 186: 13–17, 2008 [DOI] [PubMed] [Google Scholar]
- 11. Chapman DG, Berend N, King GG, Salome CM. Increased airway closure is a determinant of airway hyperresponsiveness. Eur Respir J 32: 1563–1569, 2008 [DOI] [PubMed] [Google Scholar]
- 12. Chinn S, Jarvis D, Burney P. Relation of bronchial responsiveness to body mass index in the ECRHS. European Community Respiratory Health Survey. Thorax 57: 1028–1033, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Combs TP, Berg AH, Obici S, Scherer PE, Rossetti L. Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J Clin Invest 108: 1875–1881, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. De Rosa V, Procaccini C, Cali G, Pirozzi G, Fontana S, Zappacosta S, La Cava A, Matarese G. A key role of leptin in the control of regulatory T cell proliferation. Immunity 26: 241–255, 2007 [DOI] [PubMed] [Google Scholar]
- 15. del Rio-Navarro B, Cisneros-Rivero M, Berber-Eslava A, Espinola-Reyna G, Sienra-Monge J. Exercise induced bronchospasm in asthmatic and non-asthmatic obese children. Allergol Immunopathol (Madr) 28: 5–11, 2000 [PubMed] [Google Scholar]
- 16. Ehling A, Schaffler A, Herfarth H, Tarner IH, Anders S, Distler O, Paul G, Distler J, Gay S, Scholmerich J, Neumann E, Muller-Ladner U. The potential of adiponectin in driving arthritis. J Immunol 176: 4468–4478, 2006 [DOI] [PubMed] [Google Scholar]
- 17. Fantuzzi G. Adiponectin and inflammation: consensus and controversy. J Allergy Clin Immunol 121: 326–330, 2008 [DOI] [PubMed] [Google Scholar]
- 18. Fantuzzi G. Adipose tissue, adipokines, inflammation. J Allergy Clin Immunol 115: 911–919, 2005 [DOI] [PubMed] [Google Scholar]
- 19. Ford ES. The epidemiology of obesity and asthma. J Allergy Clin Immunol 115: 897–910, 2005 [DOI] [PubMed] [Google Scholar]
- 20. Gainsford T, Willson TA, Metcalf D, Handman E, McFarlane C, Ng A, Nicola NA, Alexander WS, Hilton DJ. Leptin can induce proliferation, differentiation, and functional activation of hemopoietic cells. Proc Natl Acad Sci USA 93: 14564–14568, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gokbel H, Atas S. Exercise-induced bronchospasm in nonasthmatic obese and nonobese boys. J Sports Med Phys Fitness 39: 361–364, 1999 [PubMed] [Google Scholar]
- 22. Grunfeld C, Zhao C, Fuller J, Pollack A, Moser A, Friedman J, Feingold KR. Endotoxin and cytokines induce expression of leptin, the ob gene product, in hamsters. J Clin Invest 97: 2152–2157, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hakala K, Mustajoki P, Aittomaki J, Sovijarvi AR. Effect of weight loss and body position on pulmonary function and gas exchange abnormalities in morbid obesity. Int J Obes Relat Metab Disord 19: 343–346, 1995 [PubMed] [Google Scholar]
- 24. Hancox RJ, Milne BJ, Poulton R, Taylor DR, Greene JM, McLachlan CR, Cowan JO, Flannery EM, Herbison GP, Sears MR. Sex differences in the relation between body mass index and asthma and atopy in a birth cohort. Am J Respir Crit Care Med 171: 440–445, 2005 [DOI] [PubMed] [Google Scholar]
- 25. Hedenstierna G, Santesson J, Norlander O. Airway closure and distribution of inspired gas in the extremely obese, breathing spontaneously and during anaesthesia with intermittent positive pressure ventilation. Acta Anaesthesiol Scand 20: 334–342, 1976 [DOI] [PubMed] [Google Scholar]
- 26. Hoshino M, Nakamura Y, Hamid QA. Gene expression of vascular endothelial growth factor and its receptors and angiogenesis in bronchial asthma. J Allergy Clin Immunol 107: 1034–1038, 2001 [DOI] [PubMed] [Google Scholar]
- 27. Hosogai N, Fukuhara A, Oshima K, Miyata Y, Tanaka S, Segawa K, Furukawa S, Tochino Y, Komuro R, Matsuda M, Shimomura I. Adipose tissue hypoxia in obesity and its impact on adipocytokine dysregulation. Diabetes 56: 901–911, 2007 [DOI] [PubMed] [Google Scholar]
- 28. Hotamisligil GS, Shargill NS, Spiegelman BM. Adipose expression of tumor necrosis factor-alpha: direct role in obesity-linked insulin resistance. Science 259: 87–91, 1993 [DOI] [PubMed] [Google Scholar]
- 29. Houstis N, Rosen ED, Lander ES. Reactive oxygen species have a causal role in multiple forms of insulin resistance. Nature 440: 944–948, 2006 [DOI] [PubMed] [Google Scholar]
- 30. Huang SL, Shiao G, Chou P. Association between body mass index and allergy in teenage girls in Taiwan. Clin Exp Allergy 29: 323–329, 1999 [DOI] [PubMed] [Google Scholar]
- 31. Hug C, Wang J, Ahmad NS, Bogan JS, Tsao TS, Lodish HF. T-cadherin is a receptor for hexameric and high-molecular-weight forms of Acrp30/adiponectin. Proc Natl Acad Sci USA 101: 10308–10313, 2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Jackson MB, Ahima RS. Neuroendocrine and metabolic effects of adipocyte-derived hormones. Clin Sci (Lond) 110: 143–152, 2006 [DOI] [PubMed] [Google Scholar]
- 33. Jang AS, Lee JH, Park SW, Shin MY, Kim DJ, Park CS. Severe airway hyperresponsiveness in school-aged boys with a high body mass index. Korean J Intern Med 21: 10–14, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Johnston RA, Theman TA, Lu FL, Terry RD, Williams ES, Shore SA. Diet-induced obesity causes innate airway hyperresponsiveness to methacholine and enhances ozone-induced pulmonary inflammation. J Appl Physiol 104: 1727–1735, 2008 [DOI] [PubMed] [Google Scholar]
- 35. Johnston RA, Theman TA, Shore SA. Augmented responses to ozone in obese carboxypeptidase E-deficient mice. Am J Physiol Regul Integr Comp Physiol 290: R126–R133, 2006 [DOI] [PubMed] [Google Scholar]
- 36. Johnston RA, Theman TA, Terry RD, Williams ES, Shore SA. Pulmonary responses to acute ozone exposure in fasted mice: effect of leptin administration. J Appl Physiol 102: 149–156, 2007 [DOI] [PubMed] [Google Scholar]
- 37. Kadowaki T, Yamauchi T, Kubota N. The physiological and pathophysiological role of adiponectin and adiponectin receptors in the peripheral tissues and CNS. FEBS Lett 582: 74–80, 2008 [DOI] [PubMed] [Google Scholar]
- 38. Kaplan TA, Montana E. Exercise-induced bronchospasm in nonasthmatic obese children. Clin Pediatr (Phila) 32: 220–225, 1993 [DOI] [PubMed] [Google Scholar]
- 39. Kim J, McKinley L, Natarajan S, Bolgos GL, Siddiqui J, Copeland S, Remick DG. Anti-tumor necrosis factor-alpha antibody treatment reduces pulmonary inflammation and methacholine hyper-responsiveness in a murine asthma model induced by house dust. Clin Exp Allergy 36: 122–132, 2006 [DOI] [PubMed] [Google Scholar]
- 40. Kirkham P, Rahman I. Oxidative stress in asthma and COPD: antioxidants as a therapeutic strategy. Pharmacol Ther 111: 476–494, 2006 [DOI] [PubMed] [Google Scholar]
- 41. Komakula S, Khatri S, Mermis J, Savill S, Haque S, Rojas M, Brown L, Teague GW, Holguin F. Body mass index is associated with reduced exhaled nitric oxide and higher exhaled 8-isoprostanes in asthmatics. Respir Res 8: 32, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Lazarus R, Colditz G, Berkey CS, Speizer FE. Effects of body fat on ventilatory function in children and adolescents: cross-sectional findings from a random population sample of school children. Pediatr Pulmonol 24: 187–194, 1997 [DOI] [PubMed] [Google Scholar]
- 43. Li AM, Chan D, Wong E, Yin J, Nelson EA, Fok TF. The effects of obesity on pulmonary function. Arch Dis Child 88: 361–363, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Litonjua AA, Gold DR. Asthma and obesity: common early-life influences in the inception of disease. J Allergy Clin Immunol 121: 1075–1084, 2008 [DOI] [PubMed] [Google Scholar]
- 45. Litonjua AA, Sparrow D, Celedon JC, DeMolles D, Weiss ST. Association of body mass index with the development of methacholine airway hyperresponsiveness in men: the Normative Aging Study. Thorax 57: 581–585, 2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Loffreda S, Yang SQ, Lin HZ, Karp CL, Brengman ML, Wang DJ, Klein AS, Bulkley GB, Bao C, Noble PW, Lane MD, Diehl AM. Leptin regulates proinflammatory immune responses. FASEB J 12: 57–65, 1998 [PubMed] [Google Scholar]
- 47. Lord GM, Matarese G, Howard JK, Baker RJ, Bloom SR, Lechler RI. Leptin modulates the T-cell immune response and reverses starvation-induced immunosuppression. Nature 394: 897–901, 1998 [DOI] [PubMed] [Google Scholar]
- 48. Lu FL, Johnston RA, Flynt L, Theman TA, Terry RD, Schwartzman IN, Lee A, Shore SA. Increased pulmonary responses to acute ozone exposure in obese db/db mice. Am J Physiol Lung Cell Mol Physiol 290: L856–L865, 2006 [DOI] [PubMed] [Google Scholar]
- 49. Lumeng CN, Bodzin JL, Saltiel AR. Obesity induces a phenotypic switch in adipose tissue macrophage polarization. J Clin Invest 117: 175–184, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Ma Z, Paek D, Oh CK. Plasminogen activator inhibitor-1 and asthma: role in the pathogenesis and molecular regulation. Clin Exp Allergy 39: 1136–1144, 2009 [DOI] [PubMed] [Google Scholar]
- 51. Maniscalco M, Zedda A, Faraone S, Cerbone MR, Cristiano S, Giardiello C, Sofia M. Weight loss and asthma control in severely obese asthmatic females. Respir Med 102: 102–108, 2008 [DOI] [PubMed] [Google Scholar]
- 52. Martin-Romero C, Santos-Alvarez J, Goberna R, Sanchez-Margalet V. Human leptin enhances activation and proliferation of human circulating T lymphocytes. Cell Immunol 199: 15–24, 2000 [DOI] [PubMed] [Google Scholar]
- 53. Medoff BD, Okamoto Y, Leyton P, Weng M, Sandall BP, Raher MJ, Kihara S, Bloch KD, Libby P, Luster AD. Adiponectin-deficiency increases allergic airway inflammation and pulmonary vascular remodeling. Am J Respir Cell Mol Biol 41: 397–406, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Miller M, Cho JY, Pham A, Ramsdell J, Broide DH. Adiponectin and functional adiponectin receptor 1 are expressed by airway epithelial cells in chronic obstructive pulmonary disease. J Immunol 182: 684–691, 2009 [DOI] [PubMed] [Google Scholar]
- 55. Mito N, Kitada C, Hosoda T, Sato K. Effect of diet-induced obesity on ovalbumin-specific immune response in a murine asthma model. Metabolism 51: 1241–1246, 2002 [DOI] [PubMed] [Google Scholar]
- 56. Mosen DM, Schatz M, Magid DJ, Camargo CA., Jr The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol 122: 507–511, 2008 [DOI] [PubMed] [Google Scholar]
- 57. Nawrocki AR, Scherer PE. The delicate balance between fat and muscle: adipokines in metabolic disease and musculoskeletal inflammation. Curr Opin Pharmacol 4: 281–289, 2004 [DOI] [PubMed] [Google Scholar]
- 58. Nguyen MT, Favelyukis S, Nguyen AK, Reichart D, Scott PA, Jenn A, Liu-Bryan R, Glass CK, Neels JG, Olefsky JM. A subpopulation of macrophages infiltrates hypertrophic adipose tissue and is activated by free fatty acids via Toll-like receptors 2 and 4 and JNK-dependent pathways. J Biol Chem 282: 35279–35292, 2007 [DOI] [PubMed] [Google Scholar]
- 59. Nicolacakis K, Skowronski ME, Coreno AJ, West E, Nader NZ, Smith RL, McFadden ER., Jr Observations on the physiological interactions between obesity and asthma. J Appl Physiol 105: 1533–1541, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Ouchi N, Kihara S, Arita Y, Okamoto Y, Maeda K, Kuriyama H, Hotta K, Nishida M, Takahashi M, Muraguchi M, Ohmoto Y, Nakamura T, Yamashita S, Funahashi T, Matsuzawa Y. Adiponectin, an adipocyte-derived plasma protein, inhibits endothelial NF-kappaB signaling through a cAMP-dependent pathway. Circulation 102: 1296–1301, 2000 [DOI] [PubMed] [Google Scholar]
- 61. Pacifico L, Di Renzo L, Anania C, Osborn JF, Ippoliti F, Schiavo E, Chiesa C. Increased T-helper interferon-gamma-secreting cells in obese children. Eur J Endocrinol 154: 691–697, 2006 [DOI] [PubMed] [Google Scholar]
- 62. Pajvani UB, Hawkins M, Combs TP, Rajala MW, Doebber T, Berger JP, Wagner JA, Wu M, Knopps A, Xiang AH, Utzschneider KM, Kahn SE, Olefsky JM, Buchanan TA, Scherer PE. Complex distribution, not absolute amount of adiponectin, correlates with thiazolidinedione-mediated improvement in insulin sensitivity. J Biol Chem 279: 12152–12162, 2004 [DOI] [PubMed] [Google Scholar]
- 63. Papathanassoglou E, El-Haschimi K, Li XC, Matarese G, Strom T, Mantzoros C. Leptin receptor expression and signaling in lymphocytes: kinetics during lymphocyte activation, role in lymphocyte survival, and response to high fat diet in mice. J Immunol 176: 7745–7752, 2006 [DOI] [PubMed] [Google Scholar]
- 64. Peters-Golden M, Swern A, Bird SS, Hustad CM, Grant E, Edelman JM. Influence of body mass index on the response to asthma controller agents. Eur Respir J 27: 495–503, 2006 [DOI] [PubMed] [Google Scholar]
- 65. Rausch ME, Weisberg S, Vardhana P, Tortoriello DV. Obesity in C57BL/6J mice is characterized by adipose tissue hypoxia and cytotoxic T-cell infiltration. Int J Obes (Lond) 32: 451–463, 2008 [DOI] [PubMed] [Google Scholar]
- 66. Rivera-Sanchez YM, Johnston RA, Schwartzman IN, Valone J, Silverman ES, Fredberg JJ, Shore SA. Differential effects of ozone on airway and tissue mechanics in obese mice. J Appl Physiol 96: 2200–2206, 2004 [DOI] [PubMed] [Google Scholar]
- 67. Saint-Pierre P, Bourdin A, Chanez P, Daures JP, Godard P. Are overweight asthmatics more difficult to control? Allergy 61: 79–84, 2006 [DOI] [PubMed] [Google Scholar]
- 68. Salome CM, Munoz PA, Berend N, Thorpe CW, Schachter LM, King GG. Effect of obesity on breathlessness and airway responsiveness to methacholine in non-asthmatic subjects. Int J Obes (Lond) 32: 502–509, 2008 [DOI] [PubMed] [Google Scholar]
- 69. Savov JD, Brass DM, Berman KG, McElvania E, Schwartz DA. Fibrinolysis in LPS-induced chronic airway disease. Am J Physiol Lung Cell Mol Physiol 285: L940–L948, 2003 [DOI] [PubMed] [Google Scholar]
- 70. Schachter LM, Peat JK, Salome CM. Asthma and atopy in overweight children. Thorax 58: 1031–1035, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Schachter LM, Salome CM, Peat JK, Woolcock AJ. Obesity is a risk for asthma and wheeze but not airway hyperresponsiveness. Thorax 56: 4–8, 2001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Scherer PE. Adipose tissue: from lipid storage compartment to endocrine organ. Diabetes 55: 1537–1545, 2006 [DOI] [PubMed] [Google Scholar]
- 73. Serra A, Granada ML, Romero R, Bayes B, Canton A, Bonet J, Rull M, Alastrue A, Formiguera X. The effect of bariatric surgery on adipocytokines, renal parameters and other cardiovascular risk factors in severe and very severe obesity: 1-year follow-up. Clin Nutr 25: 400–408, 2006 [DOI] [PubMed] [Google Scholar]
- 74. Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS. TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 116: 3015–3025, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Shore SA. Obesity and asthma: implications for treatment. Curr Opin Pulm Med 13: 56–62, 2007 [DOI] [PubMed] [Google Scholar]
- 76. Shore SA. Obesity and asthma: lessons from animal models. J Appl Physiol 102: 516–528, 2007 [DOI] [PubMed] [Google Scholar]
- 77. Shore SA, Johnston RA. Obesity and asthma. Pharmacol Ther 110: 83–102, 2006 [DOI] [PubMed] [Google Scholar]
- 78. Shore SA, Rivera-Sanchez YM, Schwartzman IN, Johnston RA. Responses to ozone are increased in obese mice. J Appl Physiol 95: 938–945, 2003 [DOI] [PubMed] [Google Scholar]
- 79. Shore SA, Schwartzman IN, Le Blanc B, Murthy GG, Doerschuk CM. Tumor necrosis factor receptor 2 contributes to ozone-induced airway hyperresponsiveness in mice. Am J Respir Crit Care Med 164: 602–607, 2001 [DOI] [PubMed] [Google Scholar]
- 80. Shore SA, Schwartzman IN, Mellema MS, Flynt L, Imrich A, Johnston RA. Effect of leptin on allergic airway responses in mice. J Allergy Clin Immunol 115: 103–109, 2005 [DOI] [PubMed] [Google Scholar]
- 81. Shore SA, Terry RD, Flynt L, Xu A, Hug C. Adiponectin attenuates allergen-induced airway inflammation and hyperresponsiveness in mice. J Allergy Clin Immunol 118: 389–395, 2006 [DOI] [PubMed] [Google Scholar]
- 82. Shore SA, Williams ES, Zhu M. No effect of metformin on the innate airway hyperresponsiveness and increased responses to ozone observed in obese mice. J Appl Physiol 105: 1127–1133, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Silha JV, Krsek M, Sucharda P, Murphy LJ. Angiogenic factors are elevated in overweight and obese individuals. Int J Obes (Lond) 29: 1308–1314, 2005 [DOI] [PubMed] [Google Scholar]
- 84. Sood A, Verhulst SJ, Varma A, Eagleton LE, Henkle JQ, Hopkins-Price P. Association of excess weight and degree of airway responsiveness in asthmatics and non-asthmatics. J Asthma 43: 447–452, 2006 [DOI] [PubMed] [Google Scholar]
- 85. Stenius-Aarniala B, Poussa T, Kvarnstrom J, Gronlund EL, Ylikahri M, Mustajoki P. Immediate and long term effects of weight reduction in obese people with asthma: randomised controlled study. BMJ 320: 827–832, 2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Strissel KJ, Stancheva Z, Miyoshi H, Perfield JW, 2nd, DeFuria J, Jick Z, Greenberg AS, Obin MS. Adipocyte death, adipose tissue remodeling, and obesity complications. Diabetes 56: 2910–2918, 2007 [DOI] [PubMed] [Google Scholar]
- 87. Takahashi K, Mizuarai S, Araki H, Mashiko S, Ishihara A, Kanatani A, Itadani H, Kotani H. Adiposity elevates plasma MCP-1 levels leading to the increased CD11b-positive monocytes in mice. J Biol Chem 278: 46654–46660, 2003 [DOI] [PubMed] [Google Scholar]
- 88. Tantisira KG, Litonjua AA, Weiss ST, Fuhlbrigge AL. Association of body mass with pulmonary function in the Childhood Asthma Management Program (CAMP). Thorax 58: 1036–1041, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Tantisira KG, Weiss ST. Complex interactions in complex traits: obesity and asthma. Thorax 56, Suppl 2: 64–73, 2001 [PMC free article] [PubMed] [Google Scholar]
- 90. Thomas PS, Yates DH, Barnes PJ. Tumor necrosis factor-alpha increases airway responsiveness and sputum neutrophilia in normal human subjects. Am J Respir Crit Care Med 152: 76–80, 1995 [DOI] [PubMed] [Google Scholar]
- 91. Tsatsanis C, Zacharioudaki V, Androulidaki A, Dermitzaki E, Charalampopoulos I, Minas V, Gravanis A, Margioris AN. Adiponectin induces TNF-alpha and IL-6 in macrophages and promotes tolerance to itself and other pro-inflammatory stimuli. Biochem Biophys Res Commun 335: 1254–1263, 2005 [DOI] [PubMed] [Google Scholar]
- 92. Vasudevan AR, Wu H, Xydakis AM, Jones PH, Smith EO, Sweeney JF, Corry DB, Ballantyne CM. Eotaxin and obesity. J Clin Endocrinol Metab 91: 256–261, 2006 [DOI] [PubMed] [Google Scholar]
- 93. Vincent HK, Taylor AG. Biomarkers and potential mechanisms of obesity-induced oxidant stress in humans. Int J Obes (Lond) 30: 400–418, 2006 [DOI] [PubMed] [Google Scholar]
- 94. Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW., Jr Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 112: 1796–1808, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Weiss ST. Obesity: insight into the origins of asthma. Nat Immunol 6: 537–539, 2005 [DOI] [PubMed] [Google Scholar]
- 96. Williams AS, Leung SY, Nath P, Khorasani NM, Bhavsar P, Issa R, Mitchell JA, Adcock IM, Chung KF. Role of TLR2, TLR4, and MyD88 in murine ozone-induced airway hyperresponsiveness and neutrophilia. J Appl Physiol 103: 1189–1195, 2007 [DOI] [PubMed] [Google Scholar]
- 97. Winkler T, Venegas JG. Complex airway behavior and paradoxical responses to bronchoprovocation. J Appl Physiol 103: 655–663, 2007 [DOI] [PubMed] [Google Scholar]
- 98. Wulster-Radcliffe MC, Ajuwon KM, Wang J, Christian JA, Spurlock ME. Adiponectin differentially regulates cytokines in porcine macrophages. Biochem Biophys Res Commun 316: 924–929, 2004 [DOI] [PubMed] [Google Scholar]
- 99. Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112: 1821–1830, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Yamauchi T, Kamon J, Ito Y, Tsuchida A, Yokomizo T, Kita S, Sugiyama T, Miyagishi M, Hara K, Tsunoda M, Murakami K, Ohteki T, Uchida S, Takekawa S, Waki H, Tsuno NH, Shibata Y, Terauchi Y, Froguel P, Tobe K, Koyasu S, Taira K, Kitamura T, Shimizu T, Nagai R, Kadowaki T. Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 423: 762–769, 2003 [DOI] [PubMed] [Google Scholar]
- 101. Yamauchi T, Kamon J, Waki H, Imai Y, Shimozawa N, Hioki K, Uchida S, Ito Y, Takakuwa K, Matsui J, Takata M, Eto K, Terauchi Y, Komeda K, Tsunoda M, Murakami K, Ohnishi Y, Naitoh T, Yamamura K, Ueyama Y, Froguel P, Kimura S, Nagai R, Kadowaki T. Globular adiponectin protected ob/ob mice from diabetes and ApoE-deficient mice from atherosclerosis. J Biol Chem 278: 2461–2468, 2003 [DOI] [PubMed] [Google Scholar]
- 102. Yamauchi T, Kamon J, Waki H, Terauchi Y, Kubota N, Hara K, Mori Y, Ide T, Murakami K, Tsuboyama-Kasaoka N, Ezaki O, Akanuma Y, Gavrilova O, Vinson C, Reitman ML, Kagechika H, Shudo K, Yoda M, Nakano Y, Tobe K, Nagai R, Kimura S, Tomita M, Froguel P, Kadowaki T. The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7: 941–946, 2001 [DOI] [PubMed] [Google Scholar]
- 103. Yamauchi T, Nio Y, Maki T, Kobayashi M, Takazawa T, Iwabu M, Okada-Iwabu M, Kawamoto S, Kubota N, Kubota T, Ito Y, Kamon J, Tsuchida A, Kumagai K, Kozono H, Hada Y, Ogata H, Tokuyama K, Tsunoda M, Ide T, Murakami K, Awazawa M, Takamoto I, Froguel P, Hara K, Tobe K, Nagai R, Ueki K, Kadowaki T. Targeted disruption of AdipoR1 and AdipoR2 causes abrogation of adiponectin binding and metabolic actions. Nat Med 13: 332–339, 2007 [DOI] [PubMed] [Google Scholar]
- 104. Ye J. Emerging role of adipose tissue hypoxia in obesity and insulin resistance. Int J Obes (Lond) 33: 54–66, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Ye J, Gao Z, Yin J, He Q. Hypoxia is a potential risk factor for chronic inflammation and adiponectin reduction in adipose tissue of ob/ob and dietary obese mice. Am J Physiol Endocrinol Metab 293: E1118–E1128, 2007 [DOI] [PubMed] [Google Scholar]
- 106. Yokota T, Oritani K, Takahashi I, Ishikawa J, Matsuyama A, Ouchi N, Kihara S, Funahashi T, Tenner AJ, Tomiyama Y, Matsuzawa Y. Adiponectin, a new member of the family of soluble defense collagens, negatively regulates the growth of myelomonocytic progenitors and the functions of macrophages. Blood 96: 1723–1732, 2000 [PubMed] [Google Scholar]
- 107. Zaldivar F, McMurray RG, Nemet D, Galassetti P, Mills PJ, Cooper DM. Body fat and circulating leukocytes in children. Int J Obes (Lond) 30: 906–911, 2006 [DOI] [PubMed] [Google Scholar]
- 108. Zeyda M, Farmer D, Todoric J, Aszmann O, Speiser M, Gyori G, Zlabinger GJ, Stulnig TM. Human adipose tissue macrophages are of an anti-inflammatory phenotype but capable of excessive pro-inflammatory mediator production. Int J Obes (Lond) 31: 1420–1428, 2007. [DOI] [PubMed] [Google Scholar]