Abstract
Background In response to a research recommendation made by a UK healthcare policy agency (National Institute for Health and Clinical Excellence (NICE)), this study compared the effectiveness of computer‐based cognitive behavioural therapy (CBT) with other self‐help treatment options for mild to moderate depression and anxiety.
Method Comparative, clinical feasibility study of three self‐help CBT tools with six‐month follow‐up. Out of an initial sample of 180 adults referred by their general practitioners, 100 met the inclusion criteria and after consenting to take part were allocated one of three self‐help CBT tools: the Beating the Blues® (BtB) computer programme;1 workbooks on overcoming depression and anxiety; and the Livinglifetothefull free access internet website.2
Results Only 50 of the 100 consented participants completed the allocated intervention protocols, however, drop‐out rates were not significantly different between the groups of participants allocated each of the three self‐help CBT tools. Adults aged over 24 years (χ2 = 14.5; df = 2; P = 0.001) and with symptom duration greater than four years (χ2 = 3.96; df = 1; P = 0.047) were significantly more likely to complete any of the three interventions. There was a highly significant reduction in mean Clinical Outcomes in Routine Evaluation–Outcome Measure (CORE–OM) score at week eight compared to entry in all three groups (t (49) = 9.150; P ≤0.001). Adjusting for entry scores, there was no significant difference between the three groups in CORE–OM score improvement at week eight. There was no significant association between CORE–OM score improvement at week eight and number of general practitioner (GP) consultations at six months. There was no significant association between whether participants completed the programme and number of GP consultations at six months.
Conclusions The results demonstrated that within a two‐month follow‐up period, three different tools delivering self‐help CBT all produced significant clinical benefit for adults with mild to moderate depression and anxiety. The study had limited statistical power, but none of the modalities for delivering supported self‐help CBT appeared superior to another. There was no evidence to suggest that any of these interventions would be likely to reduce subsequent service uptake. Nevertheless, this pilot study has shown sufficient benefit from each of the self‐administered CBT tools to justify larger trials of their use.
Keywords: anxiety, Bexley, CBT, depression, MIND
Introduction
Depression and anxiety are common mental health disorders. It has been reported that one in six people will be diagnosed as having depression or chronic anxiety disorder at some time during their lives.3
Symptoms of anxiety and depression range from mild to severe. NICE and the National Collaborating Centre for Mental Health have recommended a stepped care approach to the treatment and management of depression and anxiety.4 The model includes five steps of progressively higher intensity matching the severity of presenting problems. The responsibility for care within the first three steps lies with primary care teams and the use of guided self‐help and computerised CBT at step 2 is recommended.
Currently in the UK individual CBT is frequently either not available in primary care or waiting times are lengthy. As a consequence, GPs refer patients to secondary mental healthcare services or prescribe medication alone (not the recommended first line treatment). Therefore, there is a need for additional provision at primary care level as an alternative to secondary care, for people with mild to moderate depression and/or anxiety.5
Several different methods have been described for the delivery of self‐help therapies including workbooks, computer packages and internet‐based websites accessed from home. A recent meta‐analysis of studies looking at self‐help interventions for the treatment of depression suggests that a range of delivery methods can be used successfully, particularly when there is some kind of guidance or support from a professional or paraprofessional.6
This study did not aim to study the effectiveness of CBT for mild to moderate depression and anxiety provided on a self‐help basis as this has previously been demonstrated. Proudfoot et al found that computer delivered CBT was a widely applicable treatment for anxiety and/or depression in general practice and Cavanagh et al found that the BtB computerised CBT programme is an acceptable treatment for depression and/or anxiety in routine care.1,7,8
In addition, a recent meta‐analysis found that internet‐based CBT for symptoms of depression and anxiety is effective, although there were mixed results regarding the effect of size in the studies included. It was found that the more effective treatments included some kind of therapist support.9
The National Institute for Health and Clinical Excellence Technology Appraisal 51 (February 2006) recommended that BtB should be used for people with mild and moderate depression and recommended that further research is needed to identify the effectiveness of computerised CBT in comparison with other treatment options.1,10
There is current debate about whether anxiety and depression can truly be considered to be separate conditions.11 Therefore in this study people referred with either condition were both offered the same intervention.
The aim of this study was to compare the efficacy and feasibility of three methods for the provision of self‐help CBT for mild to moderate depression in order to inform service management decisions required to achieve compliance with national guidelines for the delivery of mental health services.
Method
Participants and design
The study was based in the London Borough of Bexley which has an area of 6056 hectares and an overall population of 218 307.12 The Mental Health Needs Index (MINI2K) score for Bexley is 0.79, indicating low average mental health needs for the population, and this is associated with a high rate of referrals to secondary mental health services that are considered by these services to be inappropriate (48%).13 At the 2001 census, 87.93% of Bexley residents reported themselves as White British, 3.47% as White other, 1.3% as mixed, 3.38% as Asian, 2.87% as Black, 0.71% as Chinese and 0.34% as being from other ethnic groups.
Participants were referred from general practices within the borough. GPs used the following referral criteria:
suffering from mild to moderate depression, mixed anxiety and depression or anxiety disorder
not receiving any form of psychological treatment or counselling
aged 18 plus years.
Patients were not suitable if they had:
active suicidal ideas
a current or lifetime diagnosis of psychosis, personality disorder or organic mental disorder
alcohol and/or drug dependence
had taken medication for anxiety and/or depression continuously for six months or more immediately prior to entry.
Following their agreement to participate, people were assigned one of three self‐help CBT tools on a simple consecutive numbers basis, i.e. first patient assigned to the CBT group (group one), second to group two etc.
Procedure
Research ethics approval was given by Lewisham Research Ethics Committee.
The Bexley branch of the charity MIND used three different locations in the Bexley Borough to provide the service. Participants who did not have access to the internet at home were issued with a library card specifically for the Livinglifetothefull internet programme by Bexley Borough Council.2 Staff at the libraries were informed about the course and were on hand to help with any operational or technical difficulties if necessary.
The service was widely publicised to local GPs by email, service development meetings, posters and leaflets.
Participants were sent a letter inviting them to join the programme along with a patient information leaflet giving details about it. If the participants had not responded to the letter after a week then the research coordinator attempted to contact the person once by phone. If the participant was happy to take part in the programme, the research coordinator invited them to a meeting during which they completed the CORE–OM questionnaire. If they scored more than two on items relating to thoughts of harm to self or others, or one or more on items relating to intention to harm self/taking dangerous risks with health or being physically violent to others, their suitability for the study was discussed with the senior manager of the organisation and the participant's GP. Patients suffering from severe depression and/or anxiety, or that did not meet the inclusion criteria were excluded at this stage. Patients were allocated to treatment groups on a consecutive basis (i.e. to group 1 then to group 2, group 3 etc.) after having given their consent to be involved (they and the research coordinator were unable to influence which group they were allocated to but neither the participant nor the coordinator was blinded).
Written informed consent was then gained from each participant included in the study at the start of their first appointment. The procedures for use of each of the three tools then varied, although the degree of support was roughly equivalent for each tool.
The self‐help CBT tools
All tools were delivered with the support of a single research coordinator who has a BSc in psychology, but has no clinical training or previous clinical experience. However, she did receive some initial training with Chris Williams and his team at Glasgow University for the delivery of the Overcoming Depression and Low Mood and Overcoming Anxiety workbooks and the Livinglifetothefull website.2,14,15 She also received some training from Ultrasis for the delivery of the BtB programme.1 The research coordinator did not provide any clinical advice but discussed any concerns with her manager (the director of the voluntary service) and/or a local clinical psychologist (CC).
The participant's GP retained clinical responsibility for the patient throughout the study.
Beating the Blues computer programme1
Beating the Blues is a computerised self‐help CBT programme which consists of eight 50‐minute weekly sessions.1 After some supervision during the initial session, contact with the research coordinator was minimal. Participants accessed the programme either at Mind in Bexley or at the Bexleyheath Centre or Erith Centre (statutory mental health centres). Participants were left to complete each session independently, but were advised where to find the research coordinator if they had any problems. When each session was finished, the research coordinator ensured they had all the necessary printouts from the session. At the end of the week eight session, participants completed an assessment questionnaire and then discussed their progress on the programme with the research coordinator.
Livinglifetothefull internet website2
Livinglifetothefull is a free access, self‐help CBT internet website which consists of 13 45–60 minute modules – the first module is compulsory and the other modules are picked to suit the needs of the individual.2 Participants attended an introductory appointment with the research coordinator where they were helped to sign up to the programme and shown how to use it. They then accessed it either from a home computer or a computer at their local library and were given two support phone calls at weeks two and four. They also had a final appointment at week eight to discuss and assess their progress on the programme.
Overcoming Depression and Low Mood and Overcoming Anxiety workbooks14,15
The Overcoming Depression and Low Mood and Overcoming Anxiety workbooks are based on a structured self‐help CBT approach.14,15 Participants were required to attend an initial session where the research coordinator introduced them to the tool and asked them to complete tasks for review the following week. The second appointment involved discussing any completed tasks with the coordinator in order to decide which further workbooks they would take away to complete during the course of the programme. Participants were then given a supportive phone call at week four. They also had a final appointment at week eight to discuss and assess their progress on the programme.
Outcome measures
Participants completed the CORE–OM before they started the programme and again after the final week eight session.16 The CORE–OM is a validated scale that is widely used in local mental health services and consists of 34 questions which are designed to measure levels of psychological distress. Participants' initial and final treatment scores were compared in order to assess progress.
Six months after completion of the programme, participants were sent a patient evaluation questionnaire which was designed specifically for this study. This consisted of six statements relating to the usefulness of the programme to the participant, e.g. ‘I feel better as a result of the treatment’ and ‘I would recommend the service to friends and family, or others who have similar problems to mine’. The participant rated each statement on a Likert scale from one (strongly agree) to five (strongly disagree).
At six months after completion of the programme GPs were required to complete a brief follow‐up questionnaire indicating whether the participant had consulted them in relation to their mental health since completion of the programme, and if so how many times. They were also asked to indicate if the participant had required any further treatment such as medication or referral to secondary mental health services.
Data analysis
The statistical package SPSS 14.0 for windows (2005, SPSS Inc.) was used to analyse the data. Because of the high dropout rate, initial analyses examined whether completers differed from non‐completers on demographic variables, type and length of presenting problem and medication use. Length of episode and of GP support were dichotomised due to skewed data and analysed with chi squared tests, as were age band, gender, diagnosis and whether on medication.
Although the sample was relatively small, CORE–OM scores did not appear to deviate appreciably from the norm, and therefore CORE–OM means for completers and non‐completers were compared using a t‐test, and initial scores in the three groups were compared using a one‐way analysis of variance (ANOVA). A repeated measures ANOVA, with a within group factor of time (pre‐ to post‐treatment) and a between group factor of intervention, was used to ascertain whether either of these factors predicted CORE–OM scores. Pearson correlations, or for limited range data Spearman's rho or point‐biserial correlation, between demographic and other initial variables and amount of change were carried out to explore possible associations. The six‐month data on GP visits and referral to other services were highly skewed and were analysed with non‐parametric statistics.
Results
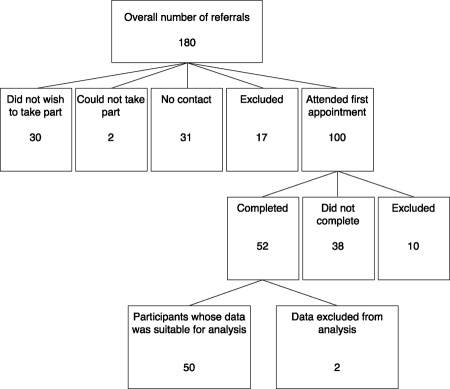
A total of 180 adults were referred by their GP to the service over a 10‐month period. Of these 128 (71%) were female and 52 (29%) were male. A total of 100 participants (30 male, 70 female) attended an initial appointment (see Figure 1 for study pathway of referrals).
Figure 1.
Study pathway of referrals
Age bands of the referred population ranged from 18 to 24 to over 75 years. The modal age band was 25 to 44 years. General practitioners referred 83 (46%) for depression, 26 (14.5%) for anxiety and 71 (39.5%) for mixed anxiety and depression. Participants reported problem duration ranging from under one year to more than 10 years (modal band one to four years). Data on ethnicity was available for 100 referrals (all of those who attended a first appointment).
Breakdown of referrals by ethnicity
86 (86%) White British
5 (5%) White other
3 (3%) mixed
3 (3%) Asian or Asian British
2 (2%) Black or Black British
1 (1%) other ethnic group
The ethnic breakdown of participants was roughly in line with that of the Bexley Borough (Bexley = 87.93% White British), although the sample size was too small to make any statistical comparisons.
Seventeen participants were excluded from the study prior to the first appointment and treatment allocation for the following reasons:
Primary diagnosis not mild–moderate depression/anxiety (n = 8)
They had been taking medication for their problem for more than six months (n = 6)
They were receiving other forms of therapy (n = 2)
They were under 18 years of age (n = 1).
Ten participants were excluded at the first appointment, after treatment allocation, for the following reasons:
their problem was considered to be too severe to comply with the inclusion criteria of mild–moderate symptoms (n = 8)
they had been taking medication for more than six months (n = 2).
Data for two participants were excluded from the analysis after they had completed the programme. This was because they were subsequently found to have been taking anti‐depression medication for more than six months (n = 1) and they had been receiving another psychological therapy at the same time (n = 1).
Completers and non‐completers of the programmes
Of the 100 participants who consented to take part in the study, 38 did not complete the programme and 12 were excluded from the analysis because they did not meet the referral criteria, leaving data for 50 service users (BtB = 16 completers; workbooks = 15 completers; internet = 19 completers). Drop‐out rates were comparable for each of the three self‐help CBT interventions (BtB = 12 non‐completers; workbooks = 11 non‐completers; internet = 15 non‐completers). Of the 50 completers, 22 were on medication and 28 were not.
There were no differences between the completers and the non‐completers (at P = 0.05) in education level, computer literacy, overall length of support from GP, length of support from GP for the current episode, diagnosis, medication used (or not) or gender. Thus there was no evidence that any of these factors influenced whether the service user completed the programme or not.
However, there was a highly significant difference in age band between the completers and non‐completers (χ2=14.5; df = 2; P = 0.001). The 18 to 24 age group was significantly less likely to complete (2 of 15 participants = 13% completed) than the 25 to 44 group (26 of 42 participants = 62% completed) or the over 45 group (22 of 31 participants = 71% completed).
Also, there was a significant difference between the completers and non‐completers in overall problem duration (χ2=3.96; df = 1; P = 0.047). Those who had a problem duration of over four years were significantly more likely to complete (70%, or 25 of 36 participants completed) than those with a problem duration of less than 4 years (48%, or 25 of 52 participants completed).
An independent t‐test showed no significant difference in CORE–OM scores at entry between the whole sample of completers and non‐completers: completers M = 2.08, standard deviation (SD) = 0.69; non‐completers M = 2.16, SD = 0.66 (t (86) = –0.56; P = 0.57). This suggests that the mental health of the completers was no more or less severe at entry than the non‐completers.
Outcome at eight weeks for the whole sample of people completing a programme
A paired t‐test indicated that there was a highly significant reduction in CORE–OM scores for the completers at week eight compared to that at entry (t (49) = 9.150; P ≤0.001). At entry M = 2.07 (SD = 0.68; 95%, confidence interval (CI) = 1.88–2.27), and at week eight M = 0.98 (SD= 0.64; 95%, CI = 0.78–1.15).
At week eight, 46 out of the 50 participants who completed (92%) showed a decrease in CORE–OM score, indicating an improvement in their mental health, with 29 (58%) moving from a clinical score on the CORE–OM to a non‐clinical score (i.e. dropping below the established mean clinical cut‐off scores for all non‐risk items on the CORE–OM of 1.36 for men and 1.50 for women).
Analysis of before and after CORE scores for the 26 cases with pure anxiety on their own demonstrated statistically significantly improvement although effect size was not as great (their mean CORE score of 1.71 was less than that of other participants at baseline).
CORE–OM scores for three participants indicated a worsening of symptoms over the eight‐week study period. Case 1 used the internet‐based tool and had scores of 1.392 at week one and 1.928 at the end. The participant explained that there had been an anniversary of a family bereavement a week before the final score was assessed and he felt that this may have affected the outcome. Cases 2 and 3 used the internet‐based and workbook tools respectively. They showed clinically insignificant change with case 2's score increasing from 1.964 at week one to 2.00 at week eight, and case 3's score increasing from 2.75 at week one to 2.964 at week eight.
Exploration of potential predictors of change
An investigation was made into whether any measured participant characteristics were associated with CORE–OM change between week one and week eight. No significant associations were found for any of the characteristics tested (age; education level; computer literacy; overall problem duration; length of episode; overall length of time of seeing GP; length of time seeing GP this episode; medication used or not; whether the client reported that the intervention suited him or her; gender and diagnosis).
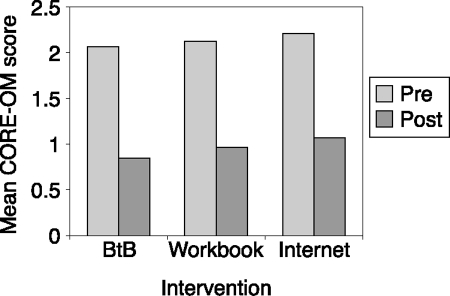
Comparison between the three tools
An ANCOVA indicated that while controlling for initial scores, there was no significant difference in the CORE–OM scores at week eight between the three self‐help CBT tools (BtB, workbooks and internet) (F (2,46) = 0.655; P = 0.524).
The overall mean difference in CORE score for each of the three self‐help interventions were as follows: BtB = 1.13 (SD 0.69; 95%, CI 0.75–1.49); workbook = 1.02 (SD 0.78; 95%, CI 0.59–1.45); internet = 1.14 (SD 1.04; 95%, CI 0.63–1.63). Paired t‐tests indicated that these differences were significant for each of the interventions. Together these analyses indicate that there was marked improvement for all three interventions and no difference in outcome between the three different interventions (see Figure 2).
Figure 2.
Mean pre‐ and post‐CORE–OM scores
Six‐month data analyses
During the six‐month follow‐up period, of the 88 participants who began the programme and were not excluded, 40 (45.5%) made no visits to the GP in connection with their mental health, 22 (25%) made one visit and the remaining 26 (29.5%) made between three and seven visits.
Spearman's rho correlation did not indicate any significant relationship between CORE–OM improvement and number of visits to the GP at six months (P ≥0.05). There was also no relationship between whether the participant completed the programme and number of visits to the GP at six months (P ≥0.05). A chi squared test did not indicate any significant differences between the three interventions regarding number of visits to the GP during the six month period post‐programme (P ≥0.05).
McNemer tests showed no significant changes as to whether medication was being prescribed at the start of the programme and at six months in either the completer or the non‐completer group (P ≥0.05). A chi squared test showed that there were also no significant differences between the three interventions as to whether medication was prescribed during the six‐month period following the programme.
Chi squared tests did not show any significant differences between the three self‐help CBT tools (BtB, workbook and internet) in the number of participants referred to counselling and secondary mental health services at six months (P ≥0.05). There were also no significant differences between the completers and the non‐completers in the number of participants referred to counselling and secondary mental health services (P ≥0.05).
Mann–Whitney tests did not show any significant differences at six months between the three different self‐help CBT tools in any of the Likert items on the patient satisfaction questionnaire (P ≥0.05).
Twenty‐eight participants completed and returned the service evaluation questionnaire. Responses to questions about accessibility and clarity of information about the service were strongly positive (86% and 84% respectively). Seventy‐three percent reported that they would recommend it to others and 46% and 42% respectively said that they would consider it a useful alternative form of treatment to counselling and medication.
Discussion
Our study has shown that within a two‐month period of follow up, three different tools delivering self‐help CBT all produced a significant improvement in mental health for adults with mild to moderate depression and anxiety. The results did not show any significant difference between the three therapies in outcome at week eight and at six‐month follow‐up there was no significant association between CORE–OM improvement and number of subsequent visits to the GP, or between completion versus dropout and number of subsequent GP visits.
Of the various participant characteristics examined, only age (i.e. a lower completion rate in younger participants) and overall problem duration (i.e. longer duration being related to higher completion rates) were found to affect completion of the programme.
The size of effect demonstrated in this study for those who completed the eight‐week self‐help CBT programme compares favourably with other studies concerning the effectiveness of self‐help CBT interventions. For example, Cavanagh et al reported an effect size of 1.00 for research completers in a naturalistic non‐randomised trial of the self‐help CBT package BtB.1,8 Also, Carlbring et al reported an effect size of 1.10 at post‐treatment in a randomised trial of internet based CBT supplemented with telephone calls.17
In common with our study, Gallatly et al demonstrated that self‐help CBT can be equally effective when provided in a number of different ways as long as there is some form of guidance/support from a professional/paraprofessional.6
However, the lack of statistical difference in effect size between the three groups may have been due to the small number of participants who completed the programme for each of the self‐help interventions (BtB = 16; workbooks = 15; internet = 19). To obtain a statistically significant difference between the three self‐help CBT interventions, given this observed effect size, would have required 45 participants per intervention. Change of staff and lack of research funds prevented the continuation of the study long enough to achieve these numbers. These are typical difficulties that have to be dealt with when research is undertaken in a district service setting.
The clinical improvement demonstrated here could have been due to spontaneous remission of symptoms over the eight‐week period, however, other studies have indicated that the short‐term spontaneous remission rates for mild–moderate depression are low. For example, Hegel et al reported that remission rates over a one‐month period ranged from 9% to 13%.18
It seemed initially surprising that at six‐month follow‐up there was no significant association between CORE–OM improvement and number of subsequent visits to the GP, or between completion versus dropout and number of subsequent GP visits. One might expect the substantial improvements reported by people in the programmes would translate to reduced need to visit their GP. Similarly one might expect programme dropout to be followed by increased GP visits. However, 45.5% of patients who were referred to the programme were also prescribed medication for their problem and therefore may have had follow‐up appointments to review their medication during this six‐month period, irrespective of improvement. In addition, 75% of those referred to the programme reported problem duration of more than one year, and it would therefore seem likely that these people would be having planned regular reviews with their GP.
In addition, the self‐help CBT programme may have been seen by GPs and/or patients as a parallel service and they may therefore have been reluctant to end the professional relationship during and after the self‐help CBT input. Therefore, the number of visits to the GP for mental health problems in the six‐month period following completion of the programme may not give an accurate indication of the success of the programme.
The lack of change in whether medication was prescribed during the six months after completion compared with at the start of the programme, in either the completers or the non‐completers, may perhaps be a result of either difficulty stopping medication or, in those who did not complete, maintaining medication in lieu of other treatment.
Only a small proportion of participants (13.6%, 12 of 88) was referred for counselling or to secondary mental health services during the six months after completion and there were no significant differences between the three self‐help CBT tools in the number of referrals. This may have been another analysis that lacked statistical power.
The poorer completion rate amongst the 18 to 24 age group may be related to a reluctance to engage with mental health services and concerns about stigma attached to mental illness. It has been suggested that teenagers in particular are more likely to access support and information via the internet.19 This younger age group may benefit more from a self‐help CBT internet programme which they can access independently and anonymously, since even limited service support of the type offered in this trial may be counterproductive for this particular group.
National guidelines currently recommend self‐help CBT as an early intervention, however, our study found that participants with an overall problem duration of more than four years were more likely to complete than those with a problem duration of under four years.20 This could be because those who have been experiencing problems for a longer period may be more determined to try alternative methods to overcome them. The analysis at week eight did not show any relationship between problem duration and amount of change during the programme. Thus there is no suggestion that any future service provision should exclude those with longer problem durations.
The initial and week eight data were gathered by the person who provided the minimal support for each intervention and therefore it is possible that participants wished when seen at week eight to give a favourable impression of how much the programme had helped them. With their study data being separate from their relationship with their GP, participants may have felt different demand characteristics in these different settings. In future studies it may be advisable to gather data from a relative or GP in addition to that from participants themselves. On the other hand, the research coordinator only had minimal contact with participants and was not delivering the interventions, but merely facilitating access to them; it therefore seems unlikely that participants would have felt a very strong social obligation to yield positive results.
Participants were not excluded from the study if they had been taking medication for six months or less, leaving open the possibility that some of the positive outcomes were a result of taking medication rather than the self‐help CBT intervention. However, counter to this, the analysis did not show any significant relationship between whether people were on medication (or not) and completion, or between medication status and improvement in CORE–OM scores, suggesting that participants had similar outcomes whether or not they were taking medication for their problem prior to starting the programme. In retrospect, it would have been better to record the timing of people starting their medication in order to be able to more completely test or rule out any potential medication‐related improvements, but it is interesting that this did not appear to affect the findings. Perhaps, if most people were not recent medication starters, these findings area reflection of relatively stable and unchanging problem status either on or off medication, which then appears to have been significantly ameliorated by the self‐help CBT interventions.
The study included people whose primary problem had been identified by their GP as pure anxiety. As discussed earlier, it is very likely that they were also experiencing some low mood since anxiety and depression are recognised as overlapping conditions.11 However, the three tools vary in the degree to which they address anxiety symptoms, with BtB not specifically targeting these.1 This study could therefore be said to have disadvantaged BtB.1 In order to check for the importance of this in interpretation of the results of this study, the statistical tests were rerun after exclusion of the 26 pure anxiety cases; this made no appreciable difference to the findings. Given that the purpose of the study was to inform commissioning in a real life setting, where GPs are being relied on to identify mental health conditions, the advantage of self‐help tools which can address a broad spectrum of symptoms is a very real one.
The study could be criticised for the lack of a control group but it was not designed to test the efficacy of the individual interventions, rather compare them. The study was initially conceived after NICE published the recommendation that local health services should provide computerised CBT. It was reasoned that what was required was not evidence that computerised CBT worked, but whether the different tools available were of equal or differing effectiveness.
For future research, it would be useful for the CORE–OM to be completed at six months in order to evaluate longer term outcomes of the interventions. A cost‐effectiveness analysis of this service is planned for the future and would make a useful contribution to health service commissioning decisions.
Conclusions
The present study adds to the body of research which has found supported self‐help CBT to be effective for the treatment of mild–moderate depression and anxiety. It has demonstrated the feasibility of delivering self‐help CBT using a new and innovative service model. It provides useful evidence on the take‐up and dropout rates for this approach as well as providing an indication of relative effect sizes for each intervention delivered under these new service conditions. Although it was not possible to say whether any of the three modes of delivery was superior to another, large effect sizes were shown for all three within a modest sample of participants.
The reported reduction in CORE–OM scores for completers of the programme was relatively high, suggesting that a future service based on these research findings could arguably give GPs an acceptable alternative for their patients.
ACKNOWLEDGEMENTS
This research was funded by a research grant from Bexley NHS Care Trust and access to a free licence to use the Beating the Blues® programme was granted by Ultrasis.1
We would like to thank all participants for their involvement in the project. We would particularly like to thank Bruce Campbell and Georgios Lyratzopoulos for their advice and assistance with editing this paper.
Contributor Information
Sarah Pittaway, Research and Guided Self Help CBT Co‐ordinator, Mind in Bexley, London, UK.
Caroline Cupitt, Consultant Clinical Psychologist, Oxleas NHS Foundation Trust, London, UK.
David Palmer, Director, Mind in Bexley, London, UK.
Nike Arowobusoye, Public Health Trainee, Bexley Care Trust, London, UK.
Ross Milne, Previous Director, Mind in Bexley, London, UK.
Sue Holttum, Senior Lecturer, Department of Applied Psychology, Canterbury Christchurch University, UK.
Hannah Patrick, Consultant in Public Health at Bexley Care Trust, London, UK.
REFERENCES
- 1.Ultrasis. Beating the Blues. www.ultrasis.com [Google Scholar]
- 2.Bexley Borough Council. Livinglifetothefull. www.livininglifetothefull.com [Google Scholar]
- 3.Mental Health Policy Group The Depression Report: a new deal for depression and anxiety disorders. London: Centre for Economic Performance, 2006 [Google Scholar]
- 4.National Institute for Health and Clinical Excellence Depression: management of depression in primary and secondary care – NICE guidance, National Clinical Practice Guideline Number 23, December 2004. London: NICE [Google Scholar]
- 5.Department of Health Improving Access to Psychological Therapies (IAPT) Programme London: Department of Health, 2007 [Google Scholar]
- 6.Gellatly J, Bower P, Hennessy S, Richards D, Gilbody S, Lovell K. What makes self‐help interventions effective in the management of depressive symptoms? Meta‐analysis and meta‐regression. Psychological Medicine 2007;37:1217–28 [DOI] [PubMed] [Google Scholar]
- 7.Proudfoot J, Ryden C, Everitt B, et al. Clinical efficacy of computerised cognitive‐behavioural therapy for anxiety and depression in primary care: randomised controlled trial. British Journal of Psychiatry 2004;184:46–54 [DOI] [PubMed] [Google Scholar]
- 8.Cavanagh K, Shapiro DA, Van Den Berg S, Swain S, Barkham M, Proudfoot J. The acceptability of computer‐aided cognitive behavioural therapy: a pragmatic study. Cognitive Behavioural Therapy 18 March 2009:1–12(Epublication ahead of print) [DOI] [PubMed] [Google Scholar]
- 9.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet‐based cognitive behaviour therapy for symptoms of depression and anxiety: a meta‐analysis. Psychological Medicine 2007;37:319–28 [DOI] [PubMed] [Google Scholar]
- 10.NICE. Technology Appraisal 51. Feb, 2006. [Google Scholar]
- 11.Tyrer P. The case for cothymia: mixed anxiety and depression as a single diagnosis. British Journal of Psychiatry 2001;179:191–3 [DOI] [PubMed] [Google Scholar]
- 12.London Borough of Bexley. Population on Census Day: key statistics. www.bexley.gov.uk/about/census/detailedkeystats.html#ks06 (accessed 6 May 2008) [Google Scholar]
- 13.Oxleas NHS Foundation Trust Depression in Presentations to the Bexley South Community Assessment and Treatment Team. Bexley Adult Mental Health Services, 2007 [Google Scholar]
- 14.Williams C. Overcoming Depression and Low Mood: a five areas approach. London: Hodder Arnold, 2006 [Google Scholar]
- 15.Williams C. Overcoming Anxiety: a five areas approach. London: Hodder Arnold, 2003 [Google Scholar]
- 16.CORE System Group CORE System (Information Management) Handbook. Leeds: CORE System Group, 1998 [Google Scholar]
- 17.Carlbring P, Bohman S, Brunt S, Buhrman M. Remote treatment of panic disorder: a randomized trial of internet‐based cognitive behaviour therapy supplemented with telephone calls. American Journal of Psychiatry 2006;163:2119–25 [DOI] [PubMed] [Google Scholar]
- 18.Hegel MT, Oxman TE, Hull JG, Swain K, Swick H. Watchful waiting for minor depression in primary care: remission rates and predictors of improvement. General Hospital Psychiatry 2006;28:205–12 [DOI] [PubMed] [Google Scholar]
- 19.University of Alberta. Teens Getting Help for Suicidal Behaviour from an Online Community. (2008). www.physorg.com/news119198259.html (accessed 27 March 2008) [Google Scholar]
- 20.National Collaborating Centre for Mental Health Depression: management of depression in primary and secondary care. National Clinical Practice Guideline Number 23. The British Psychological Society and Gaskell: London, 2004 [Google Scholar]
CONFLICTS OF INTEREST
None.