Abstract
Objective An educational outreach initiative with general practitioners (GPs) within Walsall, led by pharmacists and aimed at delivering evidence‐based guidance on stepped care management of clinical depression.
Methods Standardised educational material was produced with key messages and contributions by experts on prescribing principles and management of clinical depression based on NICE guidance. The primary care pharmacists together with a psychiatrist or other professional delivered the training through initial face‐to‐face meetings with GP practices and carrying out follow‐up visits.
Evaluation Analysis of prescribing data (PACT) on antidepressants, which included prescribing of defined daily doses (DDD) and net ingredient cost (NIC) of commonly prescribed antidepressants for the whole of Walsall teaching Primary Care Trust (tPCT) and comparison with prescribing data for the West Midlands and for England during the period June 2000 to June 2006.
Results The use of Fluoxetine increased slightly and the prescribing of Dosulepin continued to fall. The prescribing of Escitalopram, which had steadily increased prior to the launch of campaign, showed decline, resulting in savings of over £50K in the year 2005 to 2006. This was in comparison to a relative increase in the prescribing for Escitalopram for the same time period in the West Midlands and nationally. Prescribing of Dosulepin continued to fall. The total cost of prescribing for the four antidepressants fell and theses changes were sustained over the following year.
Conclusions The educational outreach campaign successfully influenced prescribing behaviour in terms of adhering to NICE guidance and cost‐effective prescribing, and also facilitated improved communication among clinicians at the primary–secondary care interface.
Keywords: depression management, education, pharmacists, prescribing, primary care
Introduction
Clinical depression is one of the most common and disabling psychiatric disorders experienced by individuals across the globe. It constitutes a significant public health concern and burden as a result of its high prevalence, long duration and likelihood of recurrence. By 2020 unipolar depression is projected to be ranked as the second highest cause of disability in both sexes throughout the world.1
In the UK, depression affects up to 10% of individuals and is the third most common reason for consultation in general practice. Whilst depressive disorders are common, they may go unrecognised. Some evidence suggests that about 50% of patients with depressive disorders attending general practices in the UK fail to get recognised or diagnosed.2,3 Similarly about 80% of patients with depression consult with non‐specific physical symptoms.4,5
Even when depression is appropriately recognised, the dosage and duration of antidepressant therapy is sometimes inadequate.6 Lack of adherence to anti‐depressant medication can arise due to insufficient communication between patient and physician, and limited or inadequate information or education relating to the treatments being provided to patients.7 Therefore, effective interventions are needed to improve the quality of care and prescribing for patients with depression.
Educational outreach visiting to clinicians (also known as academic detailing) has been established as an effective approach to modifying clinician behaviour, especially prescribing.8
The World Health Organization (WHO) has recognised the inclusion of pharmacists as active members of the healthcare team as one approach to improving psychotropic medication use.9 A UK educational outreach programme by the name of IMPACT (which was chosen for its literal meaning ‘an effect or influence when strong’ rather than as an acronym) was established in 1995 by Keele University's Department of Medicines Management.
The IMPACT programme utilises trained pharmacists to deliver locally agreed disease management guidelines. Walsall tPCT, in partnership with the Department of Medicines Management at Keele University, has conducted educational outreach campaigns using IMPACT since 1995. Examples include the management of cardiovascular disease, osteoporosis/fracture risk reduction, diabetes, hypertension and chronic obstructive pulmonary disease.
The principles of educational outreach, first established by Soumerai and Avorn, are now widely accepted and form the basis of the IMPACT educational programme.10 The key principles have been summarised in Box 1.
Box 1 Key principles of educational outreach
Conducting meetings with clinicians in their own setting
Focusing programmes on opinion leaders
Defining clear educational and behavioural objectives
Establishing credibility through a respected organisational identity, referencing authoritative and unbiased sources of information, and presenting both sides of controversial issues
Stimulating active clinician participation
Using concise educational materials
Highlighting and repeating essential messages
Providing positive reinforcement of improved practices in follow‐up visits
Soumerai and Avorn (1990)10
The NHS, like other healthcare systems, has increased its attempts to achieve the most cost‐effective use of its limited resources. It is thus increasingly important to ensure that drugs are prescribed in accordance with the clinical evidence base and as highlighted in nationally agreed guidelines. However, research has clearly shown that active intervention is needed if evidence is to be transferred into practice.
This paper presents the findings from the educational outreach campaign on the management of depression delivered to GPs in Walsall tPCT. The objectives were to: i) improve the recognition and management of depression; ii) promote prescribing of first line antidepressants based on current evidence; iii) minimise the cost to the NHS of anti‐depressant prescribing and iv) encourage a consistent approach across the health economy. Here we report on the effects of the campaign on prescribing.
Method
The educational outreach process engages clinicians in face‐to‐face discussion about a specific therapeutic topic and uses specially produced information materials to support the delivery of key messages. Walsall tPCT utilises a two‐stage approach with baseline and follow‐up visits to GP practices by trained primary care pharmacists. In the depression campaign baseline knowledge and motivations for GPs' current prescribing habits were discussed at the first visit. Standardised, high‐quality materials (information folder, posters, patient leaflets and laminated handouts) were produced with the input of Keele University's Medicines Evaluation Unit and a steering group of clinicians.
A thorough review of the evidence base was performed to ensure that the messages reflected current evidence and national guidance. Prescribing messages about depression were agreed with local primary and secondary care clinicians to ensure a consistent approach across the health economy.
At the follow‐up visits to practices these were used to highlight and repeat essential messages. Pre‐analysed prescribing data was also provided by Keele University for use in the discussion with clinicians.
Each IMPACT campaign includes a training day for the pharmacists on both therapeutic and communication skills. For the depression campaign this training day included discussion and agreement between the pharmacists and a multidisciplinary team (a psychiatrist, a GP, two mental health nurses, with pharmacists and clinicians from the Department of Medicines Management) on the content and key objectives of the campaign.
The IMPACT campaign on managing depression in primary care was launched in Walsall in July 2005 and focused on the following key issues:
Screening and assessment of depression
Treatment of mild, moderate and severe depression in the light of NICE guidelines11
Recurrent depression
Antidepressants, including general principles of prescribing, drug choice, place in therapy of newer drugs, CSM advice and adverse effects
St John's Wort
Dissemination of NICE guidelines.11
The specific prescribing related objectives identified were:
first line drug therapy to be Fluoxetine or Citalopram as per NICE guidelines
Citalopram to be preferred to Escitalopram to minimise NHS costs
encourage review of existing patients on Venlafaxine and Dosulepin to enhance patient safety.
In addition to the IMPACT pharmacist the practice visits included a local consultant psychiatrist and a primary care mental health worker where possible. This approach facilitated consistency and a better understanding of primary–secondary issues. Actions were agreed with clinicians during each meeting and the practice‐based pharmacist team provided support to implement actions. The IMPACT pharmacists maintained an electronic record of practice visits highlighting which clinicians were seen, meeting objectives, general comments on each meeting and lists of agreed actions.
The campaign was evaluated by analysis of prescribing data (PACT) on antidepressants. The analysis focused on i) prescribing of DDDs and ii) NIC of Citalopram, Escitalopram, Dosulepin and Fluoxetine for the whole of Walsall tPCT over time and compared with prescribing for the West Midlands and for England.
Results
In total 62 practice visits were carried out (covering 98% of Walsall practices) between July 2005 and January 2006. Only one practice did not agree to meeting with the IMPACT pharmacist – the information was passed onto the clinicians via the practice‐based pharmacist in this case. The average meeting time was approximately one hour. The range of actions agreed by the clinicians are summarised below.
Patient support
Use of patient leaflets such as the Good Sleep Guide and Good Relaxation Guide.
Request for copies of the Hospital Anxiety and Depression Scale (HADS)12 translated into Urdu.
Review of patients with established cardiovascular disease or hypertension on Venlafaxine.
Review of patients on Dosulepin.
Review of patients on Paroxetine at doses greater than 20 mg daily.
Review of patients on antidepressants long term, with a view to possible withdrawal.
Review of patients over 65 years of age on selective serotonin reuptake inhibitors (SSRIs) plus a diuretic.
Assess patients for risk of a gastrointestinal bleed when considering SSRIs.
Further advice requested on antidepressant choice in women of childbearing potential, or who are pregnant or breastfeeding.
Provision of list of medicines that may interact with St John's Wort.
Service development
Prescribing changes
Fluoxetine and Citalopram to be first line drug choice.
Citalopram to be preferred to Escitalopram.
Lofepramine to be preferred choice of tricyclic antidepressant.
Effects on prescribing in the Walsall tPCT
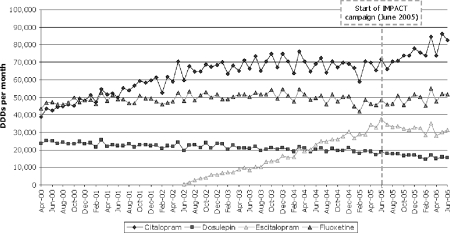
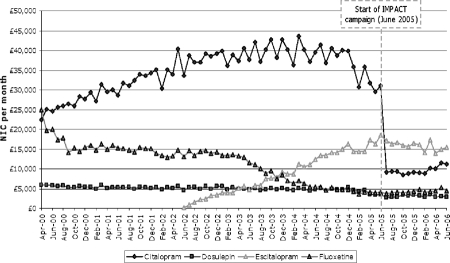
Prescribing of Citalopram, Escitalopram, Fluoxetine and Dosulepin in Walsall tPCT over the period April 2000 to June 2006 (five years before, and one year after, the IMPACT campaign) is shown in Figures 1 and 2. This data is derived from analysis of prescriptions dispensed in primary care, i.e. general practice prescribing. In the UK, the vast majority of prescriptions are issued by general practice and therefore the data analysed is largely representative of anti‐depressant prescribing within the health economy.
Figure 1.
Defined daily doses (DDDs) per month of selected antidepressants in NHS Walsall April 2000 to June 2006
Figure 2.
Spend net ingredient cost (NIC) per month on selected antidepressants in NHS Walsall April 2000 to June 2006
Prescribing of Escitalopram, which had previously been increasing, initially levelled out and then showed a small decrease. In contrast, prescribing of Citalopram had been fairly stable but increased after the campaign. The use of Fluoxetine remained stable and the prescribing of Dosulepin continued to fall. The total cost of prescribing for the four antidepressants fell. These changes were sustained one year later.
We present the comparison of tariff prices for all the available doses of Citalopram and Escitalopram as they stood during May 2005 in Table 1.
Table 1.
Differences in tariff prices between Citalopram and Escitalopram (May 2005)
| Citalopram 28 tablets | Escitalopram 28 tablets | ||
|---|---|---|---|
| 10 mg | £86.64 | 5 mg | £107.04 |
| 20 mg | £153.36 | 10 mg | £178.92 |
| 40 mg | £255.36 | 20 mg | £302.40 |
Source: Walsall teaching PCT (2005)
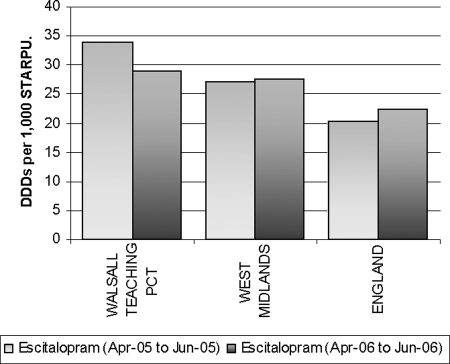
Comparison with regional and national prescribing trends
In order to understand the extent to which the local changes in prescribing might be attributable to the IMPACT campaign, the data were compared with those for the West Midlands and England (Figure 3). The data analysis confirms that the prescribing of Escitalopram within Walsall tPCT from 2005 to 2006 decreased, whereas in both the West Midlands and England prescribing of Escitalopram continued to increase during the same period.
Figure 3.
Change in prescribing of Escitalopram in prescribing quarter ending June 2005 to quarter ending June 2006
Prescribing data was analysed using items/STARPU (Specific Therapeutic Age Related Prescribing Unit). STARPU represents a prescribing volume denominator which allows comparison between different practices and organisations. The use of STARPU is an accepted and validated measure used by the UK Prescribing Support Unit which is responsible for the analysis of dispensed medications.
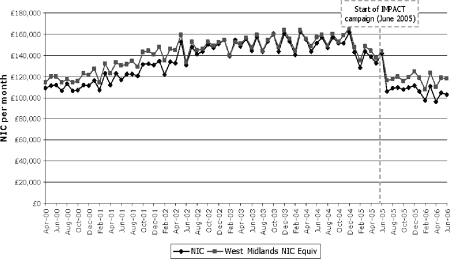
Overall antidepressant prescribing
Up to June 2005 the prescribing costs for antidepressants in Walsall were in line with those for the West Midlands as a whole. Total monthly costs of antidepressant prescribing have decreased in both the West Midlands and Walsall since late 2005. However, the data suggests that the reduction in prescribing costs has been greater in Walsall than in the West Midlands as a whole since June 2005 (Figure 4).
Figure 4.
Spend net ingredient cost (NIC) per month on all antidepressants in NHS Walsall April 2000 to June 2006
Potential cost savings
For the period June 2005 to June 2006 a saving of £55841 resulted from the reduction in the volume of prescribing of Escitalopram. Increased prescribing of Citalopram during this period incurred additional costs of £7280. Therefore, the campaign realised a saving in prescribing costs of £48 561. We did not conduct a formal health economic evaluation but the direct cost of the IMPACT campaign (campaign materials, training and sessional payments to the IMPACT pharmacists for practice visits) was approximately £12 000.
If the costs of GP and consultant time were included the estimated cost for 62 hours would be approximately £8500, calculated as actual cost on the basis of their average salaries.
Discussion
To our knowledge this is the first UK study to test the effects of educational outreach on prescribing for depression in primary care. The use of educational outreach visits has previously been identified as an intervention that may improve the practice of health care professionals, in particular in prescribing.8,9 Although educational outreach has been the subject of some study, it is not an area for which an extensive and detailed evidence base exists. The results of the Walsall IMPACT campaign on the management of depression has demonstrated that changes in prescribing can be achieved.
The objectives in relation to prescribing were that:
first line drug therapy should be Fluoxetine or Citalopram
Citalopram should be prescribed in preference to Escitalopram and
existing prescribing of Venlafaxine and Dosulepin for individual patients should be reviewed.
In Walsall the prescribing of Citalopram increased substantially and Fluoxetine slightly, while that of Dosulepin continued to decrease, and Escitalopram showed a decrease after the launch of campaign. Comparison of local prescribing with regional and national data showed that while Escitalopram prescribing decreased in Walsall it increased across the region and nationally. This finding indicates that the IMPACT campaign did affect prescribing and is the reason for the different trend in Walsall.
Prescribing of Escitalopram was greater than the West Midlands average before the launch of the IMPACT campaign. Possible reasons for this may include preferred use of Escitalopram by secondary care clinicians and effective marketing by the manufacturers of Escitalopram to primary care.
Levels of Fluoxetine prescribing had been falling since 2004 and this decline was reversed in Walsall. Since Dosulepin prescribing levels were already falling, it is more difficult to attribute any change in this to the IMPACT campaign.
Significant financial savings were made as a result of the prescribing of Citalopram in preference to the S‐enantiomer form, Escitalopram. The Drugs and Therapeutics Bulletin concluded that there is no compelling evidence to support the claim that Escitalopram is more effective, or has a faster onset of action, than Citalopram.14 The use of generic (patent expired) medicines rather than branded equivalents has an essential role in the effective use of prescribing budgets and achieving value for money for the NHS.
The results of the IMPACT campaign suggest that clinicians have accepted the case for generic Citalopram to be preferred to Escitalopram. The availability and use of generic Citalopram is the most likely explanation of the substantial reductions in total spending on Citalopram after June 2005. Total prescribing costs for antidepressants fell by a larger amount than the West Midlands average.
One possible explanation for this could be that the prescribing of cost‐effective antidepressants has been greater in Walsall than across the West Midlands as a whole. Such prescribing releases resources that can then be reallocated. Even taking into account the costs of GP and consultant time during practice visits the IMPACT campaign was cost effective.
Effectiveness of educational outreach
There is evidence to underpin the use of pharmacists to promote evidence‐based practice in mental health. A systematic review on the role of pharmacists in mental health care was undertaken by Finley, Crimson and Rush.15 The objective of this review was to specifically evaluate the impact of pharmacist delivered community based services to optimise the use of medications for mental illness. The review concluded that pharmacists can bring about improvements in the safe and efficacious use of psychotropic medications.
The NHS Centre for Reviews and Dissemination undertook a review of the available research evidence on the effectiveness of educational and organisational strategies aimed at influencing healthcare professionals' ability to improve the recognition and management of depression in primary care.16 Intervention strategies included developing practice guidelines, nurse case management and integrated care. The review identified over 30 studies, examining educational and organisational interventions relating to recognition and management of depression. The majority of interventions evaluated related to implementation of practice guidelines. However, there are fewer studies that generally look into effectiveness of pharmacist‐led prescribing information through educational outreach.
A key randomised control trial (RCT) with statistically significant outcomes cited in both reviews was carried out by van Eijk et al in South West Netherlands.17 In this study, a group of pharmacists (n = 37) delivered prescribing information and support (academic detailing) to GPs (n = 190) regarding the use of highly anticholinergic antidepressants for the elderly (over 60 years of age). The RCT had three arms: individual visits, group visits and a control group. The study evaluated the outcome of educational intervention by studying a large database covering prescriptions to people covered by national health insurance in the catchment area. The study showed positive outcomes, i.e. 26% reduction in initiating highly anticholinergic antidepressant medication for the individual intervention arm, and 45% reduction in the group intervention arm.
Studies by Crotty et al (2004) and de Burgh et al (1995), both carried out in Australia, showed that educational visits to GPs by pharmacists were acceptable and well received.18,19 Crotty et al carried out a cluster randomised control study involving pharmacists' educational visits to general medical practitioners providing services to residential care facilities. This study did not find a significant difference in the use of psychotropic medication between intervention and control facilities. The only significant finding was the significant increase in the use of ‘as required’ antipsychotic medication in the intervention group. The de Burgh et al study (1995) related to educational visits to GPs conducted by three physicians and one pharmacist; it reported a significant reduction in prescribing of benzodiazepines in both the intervention and control groups. However, the difference between both the study arms was not statistically significant.
A randomised controlled trial carried out in the USA by Avorn and Soumerai found that educational visits by pharmacist, were associated with a significant decline in the prescribing of potentially inappropriate psychotropic medications in the intervention groups.20
Watson and Sharp(2001) evaluated GP opinion of educational outreach visits by trained pharmacists.21 In their study 88% of GPs said that they benefited from the visit and 94% and 79% respectively thought that they were an acceptable and effective method of providing prescribing information. Almost three‐quarters of GPs thought that educational outreach visits were a suitable role for pharmacists and the same proportion said they would accept future visits in order to discuss prescribing issues. These findings are reflected in Walsall tPCT, where the IMPACT project is well established and positive feedback has been received from clinicians.
The pharmacist educational outreach visits were originally scheduled to last a maximum of ten minutes since this was thought to be the amount of time that most GPs would be willing to give. The median duration of the first and second cycle visits in the Watson and Sharp study (2001) was 20 minutes and 15 minutes.21 This suggests that GPs were willing to provide additional time for meetings if the issues identified for action required it. This is confirmed by most of the Walsall IMPACT visits where the average meeting time was approximately one hour.
Local feedback from both GPs and the consultant indicated that they perceived both tangible and intangible benefits from the educational outreach visits on depression. The tangible benefits included dialogue on evidence‐based practice and the intangible included development of improved relationships between primary and secondary care, which were likely to benefit delivery of services and patient care in the future.
Strengths and limitations of the study
The study design was an open before‐and‐after comparison. Such a design was appropriate because the IMPACT programme had been operating in Walsall for a decade and almost all practices were participating. This high level of participation was a strength of the study. However, the GPs' familiarity with and acceptance of educational outreach in Walsall might limit the wider generalisability of the findings. A primary care trust introducing an educational outreach campaign for the first time might not achieve such high acceptance rates and thus the effect might be smaller.
Comparisons with regional and national data provided benchmarking that enabled any differences to be identified. The changes were sustained one year after the campaign but the longer‐term effects are not known. We were able to attribute direct costs for IMPACT and set these against the changes in prescribing costs. However, we were not able to include indirect opportunity costs of GP time and consultant time, nor did we calculate the intangible benefits identified by the clinicians.
Other possible reasons for changes in prescribing habit may include implementation of the NICE guidance by the GPs on management of depression. It is also possible that some prescribers may have considered change to Citalopram for existing or new patients in view of the impending availability of generic Citalopram. During the campaign, there was no other local initiative or incentive to change antidepressant prescribing behaviour.
Conclusion
The results of the IMPACT campaign on the management of depression clearly demonstrate that educational outreach visits by primary care pharmacists in partnership with clinicians can positively influence prescribing behaviour. The results show that educational outreach visits encourage cost‐effective prescribing. Therefore NHS organisations should consider the use of educational outreach visits as part of their medicines management strategies.
ACKNOWLEDGEMENTS
The authors would like to thank: Alison Blenkinsopp, Professor of the Practice of Pharmacy, Keele University for her valuable advice and guidance on the manuscript. Mark Thomas, Data Analyst, Department of Medicines Management, Keele University for help in analysing data and preparing graphs.
NHS Walsall IMPACT Pharmacist Team members – Ms Baljeet Randhawa, Mr John Knowles, Mr Hemant Patel and NHS Walsall Primary Care Mental Health Team members for their support for the campaign.
Contributor Information
Bharat Patel, Head of Medicines Management, Walsall teaching Primary Care Trust, Jubilee House, Bloxwich Lane, Walsall, UK.
Safiullah Afghan, Consultant Psychiatrist, Dorothy Pattison Hospital, Dudley and Walsall Mental Health Partnership NHS Trust, UK.
REFERENCES
- 1.Murray CJL, Lopez AD. The Global Burden of Disease Harvard School of Public Health on behalf of the World Bank, 1996 [Google Scholar]
- 2.Marks J, Goldberg DP, Hillier VF. Determinants of the ability of general practitioners to detect psychiatric illness. Psychological Medicine 1979;9:337–53 [DOI] [PubMed] [Google Scholar]
- 3.Dowrick C, Buchan I. Twelve month outcome of depression in general practice: does detection or disclosure make a difference? BMJ 1995;311:274–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singleton N, Bumpstead R, O'Brien M, et al. Office of National Statistics: psychiatric morbidity among adults living in private households, 2000 London: HMSO, 2001 [DOI] [PubMed] [Google Scholar]
- 5.Kirmayer LJ, Robbins M, Dworkind M, et al. Somatization and recognition of depression and anxiety in primary care. American Journal of Psychiatry 1993;150:734–41 [DOI] [PubMed] [Google Scholar]
- 6.Simon G, Von Korff M. Recognition and management of depression in primary care. Archives of Family Medicine 1995;4:99–105 [DOI] [PubMed] [Google Scholar]
- 7.Piest RG, Vize C, Roberts A, et al. Lay people's attitudes to treatment of depression: results of opinion poll for Defeat Depression Campaign just before its launch. BMJ 1996;313:858–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Brien MA, Oxman AD, Davis RB, et al. Educational Outreach Visits: effects on professional practice and health care outcomes. doi: 10.1002/14651858.CD000409. The Cochrane Database of Systematic Reviews 1997, Issue 4, Art. No: CD000409. DOI 10.2002/14651858.CD000409. [DOI] [PubMed] [Google Scholar]
- 9.WHO Improving access and use of psychotropic medicines Geneva: World Health Organization, 2004 [Google Scholar]
- 10.Soumerai S, Avorn J. Principles of educational outreach (‘academic detailing’) to improve clinical decision making. Journal of the American Medical Association 1990;263:549–56 [PubMed] [Google Scholar]
- 11.National Institute of Health and Clinical Excellence (NICE) Depression: management of depression in primary and secondary care. (2007). www.nice.org.uk/nicemedia/pdf/CG23quickrefguideamended.pdf [Google Scholar]
- 12.Zigmond AS, Snaith PR. The Hospital Anxiety and Depression Scale (HADS). Acta Psychiatrica et Neurologica Scandinavica 1983;67:361–70 [DOI] [PubMed] [Google Scholar]
- 13.Kroenke K, Spitzer RL. The PHQ‐9: a new depression and diagnostic severity measure. Psychiatric Annals 2002;32:509–21 [Google Scholar]
- 14.Anon New drugs from old. Drugs and Therapeutics Bulletin 2006;44:73–7 [DOI] [PubMed] [Google Scholar]
- 15.Finley PR, Crimson ML, Rush AJ. Evaluating the impact of pharmacists in mental health: a systematic review. Pharmacotherapy 2003;23:1634–44 [DOI] [PubMed] [Google Scholar]
- 16.Effective Health Care: improving the recognition and management of depression in primary care NHS Centre for Reviews and Dissemination, University of York; Vol. 7, Number 5, 2002 [Google Scholar]
- 17.Van Eijk ME, Avorn J, Porsius AJ, et al. Reducing prescribing of highly anticholinergic antidepressants for elderly people: randomised trial of group versus individual academic detailing. BMJ 2001; 322:654–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crotty M, Whitehead C, Rowett C, et al. An outreach intervention to implement evidence based practice in residential care: a randomised control trial. BMC Health Services Research 2004;4:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.de Burgh S, Mant A, Mattick RP, et al. A controlled trial of educational visiting to improve benzodiazepine prescribing in general practice. Australian Journal of Public Health 1995;19:142–8 [DOI] [PubMed] [Google Scholar]
- 20.Avorn J, Soumerai SB, Everitt DE, et al. A randomised control trial of a programme to reduce the use of psychoactive drugs in nursing homes. New England Journal of Medicine 1992;327:168–73 [DOI] [PubMed] [Google Scholar]
- 21.Watson M, Sharp J. General practitioners' opinions of educational outreach from community pharmacists as a method of providing prescribing information. The Pharmaceutical Journal 2001;266:20–2 [Google Scholar]
CONFLICTS OF INTEREST
None.