Abstract
A consensus conference on cardio-renal syndromes (CRS) was held in Venice Italy, in September 2008 under the auspices of the Acute Dialysis Quality Initiative (ADQI). The following topics were matter of discussion after a systematic literature review and the appraisal of the best available evidence: definition/classification system; epidemiology; diagnostic criteria and biomarkers; prevention/protection strategies; management and therapy. The umbrella term CRS was used to identify a disorder of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction in the other organ. Different syndromes were identified and classified into five subtypes. Acute CRS (type 1): acute worsening of heart function (AHF–ACS) leading to kidney injury and/or dysfunction. Chronic cardio-renal syndrome (type 2): chronic abnormalities in heart function (CHF-CHD) leading to kidney injury and/or dysfunction. Acute reno-cardiac syndrome (type 3): acute worsening of kidney function (AKI) leading to heart injury and/or dysfunction. Chronic reno-cardiac syndrome (type 4): chronic kidney disease leading to heart injury, disease, and/or dysfunction. Secondary CRS (type 5): systemic conditions leading to simultaneous injury and/or dysfunction of heart and kidney. Consensus statements concerning epidemiology, diagnosis, prevention, and management strategies are discussed in the paper for each of the syndromes.
Keywords: Cardio-renal syndromes, Acute heart failure, Acute kidney injury, Chronic kidney disease, Worsening renal function, Chronic heart disease, Chronic heart failure
Introduction
Cardiac and renal diseases are common and frequently coexist to significantly increase mortality, morbidity, and the complexity and cost of care.1,2 Syndromes describing the interaction between heart and kidney have been defined and classified1,3–7 but never as a result of a consensus process. Thus, there is limited appreciation of epidemiology and standardized diagnostic criteria. Moreover, prevention and treatment is fragmented, single organ centred, and not multidisciplinary in approach. As a result, timing and quality of care may suffer. A consensus conference was organized under the auspices of the Acute Dialysis Quality Initiative (ADQI) in Venice, Italy, in September 2008. It involved opinion leaders and experts in nephrology, critical care, cardiac surgery, and cardiology. In this manuscript, we present the findings of this consensus conference.
Methods
The ADQI process was applied.8 The ADQI methodology comprises a systematic search for evidence, establishment of relevant clinical and physiological outcomes, description of current practice and analysis of areas lacking evidence and setting of a specific research agenda. Before the conference, topics were selected and work groups assembled. Groups identified the key questions and conducted a systematic literature search. During the conference, work groups assembled in breakout sessions, as well as plenary sessions where their findings were presented, debated, and refined. Key questions were identified by the group and subgroups deliberated on these questions, bringing forth recommendations to the group as a whole. Deliberations followed 3 days of discussion among 32 attendees. Summary statements were then developed by the entire group as reported here.
Results
The Steering Committee assembled an expert panel, which was divided into five smaller working groups: (i) definition and classification, (ii) epidemiology, (iii) diagnostic biomarkers, (iv) prevention, and (v) treatment.
Definition and classification
Need for consensus definition
We unanimously agreed that a consensus definition was needed to highlight the coexistence of cardiac and renal disorders and to identify the time course of heart–kidney interaction and the primacy of the organ leading to the syndrome. The goal of this definition would be to facilitate epidemiological studies, identify target populations for intervention, develop diagnostic tools, prevent and manage different syndromes.
Principles of definition and classification
We chose a broad term, using the plural (cardio-renal syndromes, CRS), to indicate the presence of multiple syndromes. We chose subtypes to recognize primary organ dysfunction (cardiac vs. renal) and acute vs. chronic time frame. We considered structural and/or functional abnormalities of both organs necessary. We added an additional subtype to capture systemic conditions affecting both organs simultaneously. We chose definitions to include accepted criteria published by national and international societies.
Consensus definition and classification of cardio-renal syndromes
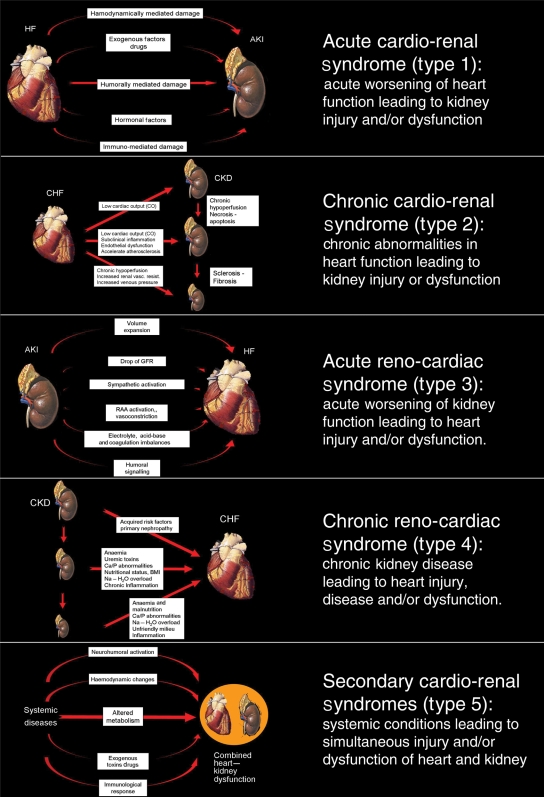
We considered definitions from the literature and used a specific publication4 as template. We defined the broad term ‘cardio-renal syndromes’ as ‘disorders of the heart and kidneys whereby acute or chronic dysfunction in one organ may induce acute or chronic dysfunction of the other’. We identified five subtypes of the syndromes (Table 1). Their pathophysiological mechanisms are described in Figure 1.
Table 1.
Cardio-renal syndromes: classification, definitions, and work group statements
| Syndromes | Acute cardio-renal (type 1) | Chronic cardio-renal (type 2) | Acute reno-cardiac (type 3) | Chronic reno-cardiac (type 4) | Secondary CRS (type 5) |
|---|---|---|---|---|---|
| Organ failure sequence | |||||
| Definition | Acute worsening of heart function (AHF–ACS) leading to kidney injury and/or dysfunction | Chronic abnormalities in heart function (CHF-CHD) leading to kidney injury or dysfunction | Acute worsening of kidney function (AKI) leading to heart injury and/or dysfunction | Chronic kidney disease (CKD) leading to heart injury, disease and/or dysfunction | Systemic conditions leading to simultaneous injury and/or dysfunction of heart and kidney |
| Primary events | Acute heart failure (AHF) or acute coronary syndrome (ACS) or cardiogenic shock | Chronic heart disease (LV remodelling and dysfunction, diastolic dysfunction, chronic abnormalities in cardiac function, cardiomyopathy) | AKI | CKD | Systemic disease (sepsis, amyloidosis, etc.) |
| Criteria for primary events | ESC, AHA/ACC | ESC, AHA/ACC | RIFLE–AKIN | KDOQI | Disease-specific criteria |
| Secondary events | AKI | CKD | AHF, ACS, arrythmias, shock | CHD (LV remodelling and dysfunction, diastolic dysfunction, abnormalities in cardiac function), AHF, ACS | AHF, ACS, AKI, CHD, CKD |
| Criteria for secondary events | RIFLE–AKIN | KDOQI | ESC, AHA/ACC | ESC, AHA/ACC | ESC, AHA/ACC, RIFLE/AKIN ESC, AHA/ACC KDOQI |
| Cardiac biomarkers | Troponin, CK-MB, BNP, NT-proBNP, MPO, IMA | BNP, NT-proBNP, C-reactive protein | BNP, NT-proBNP | BNP, NT-proBNP, C-reactive protein | C-reactive protein, procalcitonin, BNP |
| Renal biomarkers | Serum cystatine C, creatinine, NGAL. Urinary KIM-1, IL-18, NGAL, NAG | Serum creatinine, cystatin C, urea, uric acid, C-reactive protein, decreased GFR | Serum creatinine, cystatin C, NGAL. Urinary KIM-1, IL-18, NGAL, NAG | Serum creatinine, cystatin C, urea, uric acid, decreased GFR | Creatinine, NGAL, IL-18, KIM-1, NAG |
| Prevention strategies | Acutely decompensated heart failure and acute coronary syndromes are most common scenariosInciting event may be acute coronary ischaemia, poorly controlled blood pressure, and noncompliance with medication and dietary sodium intakeRandomized trials improving compliance with heart failure care management have reduced rates of hospitalization and mortality, and a reduction in the rates of acute cardio-renal syndrome (type 1) can be inferred | A common pathophysiology (neurohumoral, inflammatory, oxidative injury) could be at work to create organ dysfunctionDrugs that block the renin–angiotensin system reduce the progression of both heart failure and CKDIt is unknown whether other classes of drugs can prevent chronic cardio-renal syndrome (type 2) | Acute sodium and volume overload are part of the pathogenesisIt is unknown whether sodium and volume overload is prevented with different forms of renal replacement therapy and if this will result in lower rates of cardiac decompensation | The chronic processes of cardiac and renal fibrosis, left ventricular hypertrophy, vascular stiffness, chronic Na and volume overload, and other factors (neurohumoral, inflammatory, oxidative injury) could be at work to create organ dysfunctionA reduction in the decline of renal function and albuminuria has been associated with a reduction in cardiovascular eventsThe role of chronic uraemia, anaemia, and changes in CKD-mineral and bone disorder on the cardiovascular system is known in chronic reno-cardiac syndrome | Potential systemic factors negatively impact function of both organs acutelyIt is uncertain if reduction/elimination of the key factors (immune, inflammatory, oxidative stress, thrombosis) will prevent both cardiac and renal decline. |
| Management strategies | Specific—depends on precipitating factorsGeneral supportive—oxygenate, relieve pain & pulmonary congestion, treat arrhythmias appropriately, differentiate left from right heart failure, treat low cardiac output or congestion according to ESC guidelines(a); avoid nephrotoxins, closely monitor kidney function. | Treat CHF according to ESC guidelinesa, exclude precipitating pre-renal AKI factors (hypovolaemia and/or hypotension), adjust therapy accordingly and avoid nephrotoxins, while monitoring renal function and electrolytesExtracorporeal ultrafiltration | Follow ESC guidelines for acute CHFa specific management may depend on underlying aetiology, may need to exclude renovascular disease and consider early renal support, if diuretic resistant | Follow KDOQI guidelines for CKD management, exclude precipitating causes (cardiac tamponade). Treat heart failure according to ESC guidelinesa, consider early renal replacement support | Specific—according to etiology. General—see CRS management as advised by ESC guidelines* 2008 |
AKI, acute kidney injury; CKD, chronic kidney disease; NGAL, neutrophil gelatinase-associated lipocalin; NAG, N-acetyl-β-(d)glucosaminidase.
aAs advised by ESC guidelines 2008.
Figure 1.
Pathophysiology and definitions of the five subtypes of cardio-renal syndrome (modified by Ronco et al.105).
We chose the term CRS to indicate the bidirectional nature of the various syndromes and to recognize that this term was already established in the medical lexicon, despite lack of formal definition.
Acute cardio-renal syndrome (type 1)
Acute worsening of heart function leading to kidney injury and/or dysfunction. This is a syndrome of worsening renal function (WRF) complicating acute heart failure (AHF) and/or acute coronary syndrome (ACS). Between 27 and 40% of patients hospitalized for acute de-compensated heart failure (ADHF) appear to develop acute kidney injury (AKI)2,9 and fall into this clinical entity. These patients experience higher mortality and morbidity, and increased length of hospitalization.4
Chronic cardio-renal syndrome (type 2)
Chronic abnormalities in heart function leading to kidney injury or dysfunction. This subtype refers to a more chronic state of kidney disease complicating chronic heart disease. This syndrome is common and has been reported in 63% of patients hospitalized with congestive heart failure (CHF).10,11
Acute reno-cardiac syndrome (type 3)
Acute worsening of kidney function leading to heart injury and/or dysfunction. This subtype refers to abnormalities in cardiac function secondary to AKI. The pathophysiological mechanisms likely go beyond simple volume overload and the recent consensus definition of AKI12 may help to investigate this syndrome further.
Chronic reno-cardiac syndrome (type 4)
Chronic kidney disease (CKD) leading to heart injury, disease, and/or dysfunction. This subtype refers to disease or dysfunction of the heart occurring secondary to CKD. There is a graded and independent association between the severity of CKD and adverse cardiac outcomes. In a recent meta-analysis,13 an exponential relation between the severity of renal dysfunction and the risk for all-cause mortality was described with excess cardiovascular deaths constituting over 50% of overall mortality.
Secondary cardio-renal syndromes (type 5)
Systemic conditions leading to simultaneous injury and/or dysfunction of heart and kidney. Although this subtype does not have primary and/or secondary organ dysfunction, it refers to situations where both organs are simultaneously affected by systemic illnesses, either acute or chronic. Examples include sepsis, systemic lupus erythematosus, diabetes mellitus, amyloidosis, or other chronic inflammatory conditions.
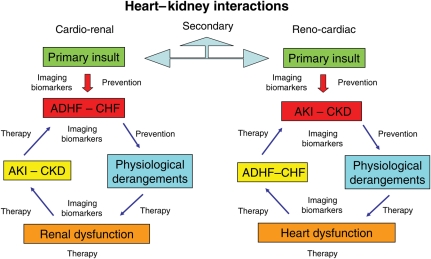
The ADQI working group recognized that many patients may populate or move between subtypes during the course of their disease. This classification is not meant to fix patients into one immovable category (Figure 2). The group discussed and considered further sub-classification, to include situations of transient or reversible dysfunction, slowly or acutely progressive vs. stable disease, however it chose a more parsimonious classification system.
Figure 2.
In cardio-renal syndromes, there are two important aspects: the first is the sequence of organ involvement and the second is the bi-directionality of signalling leading to a vicious cycle. Another important aspect is the time frame in which the derangements occur (chronic or acute). In all cases, there are moments in which prevention is possible, in others mitigation of the insult is potentially feasible, in others, therapeutic strategies must be implemented. At different times, a crucial role is played by imaging techniques and biomarkers enabling the clinician to make an early diagnosis, establish illness severity, and to potentially predict outcomes. This flowchart describes a series of conditions indicating that patients may move from one type to another of cardio-renal syndromes.
Epidemiology of cardio-renal syndromes
Cardio-renal syndromes are characterized by significant heart–kidney interactions that share similarities in pathophysiology. However, they are also likely to have important discriminating features, in terms of predisposing or precipitating events, natural history, and outcomes. A description of the epidemiology of heart–kidney interaction, stratified by the CRS subtypes, is a critical initial step towards understanding the overall burden of disease for each CRS subtype and vital in determining the presence of gaps in knowledge and helping design future trials.
Acute cardio-renal syndrome (type 1)
A large body of literature has examined AKI due to worsening heart function. Most studies are retrospective, secondary, and/or post hoc analyses from large databases2,9,14–18 or clinical trials of drug therapy.19,20 The term ‘WRF’ has been used to describe the acute and/or sub-acute changes in kidney function in patients ADHF or ACS. Its incidence estimates range between 19 and 45%. This broad range is largely attributable to variations in the definitions of WRF, the observed time-at-risk and the population under study. Most studies have found that WRF/AKI in ADHF/ACS occurs early after presentation to hospital. In both ADHF and ACS, the development of WRF/AKI has been associated with greater short- and long-term all-cause and cardiovascular mortality, prolonged duration of hospitalization,9,15,21–23 increased readmission rates,24,25 accelerated progression to CKD stages 4–5,17 and higher healthcare costs.15 In addition, there seems to be a biological gradient between severity of AKI and risk of death.24 Two studies have also shown the risk of poor outcome persists regardless of whether WRF/AKI was transient or sustained22,25 and that even small acute changes in SCr (0.3 mg/dL) can modify the risk of death.19 Venous congestion may be an important haemodynamic factor driving WRF in patient with ADHF.26 In ICU patients admitted with ADHF, WRF was associated with greater central venous pressure (CVP) on admission and after intensive medical therapy. This finding was apparent across the spectrum of systemic blood pressure, pulmonary capillary wedge pressure, cardiac index, and estimated glomerular filtration rates.26
Chronic cardio-renal syndrome (type 2)
Chronic heart disease and CKD frequently co-exist, and often the clinical scenario does not permit to distinguish which disease came first. Large database studies do not distinguish between type 2 and type 4 CRS. Nevertheless, between 45 and 63.6% of patients with CHF have evidence of CKD.11,27 In these studies, CKD was associated with higher all-cause and cardiac-specific mortality. A ‘dose–response’ or graded association between decline in kidney function and worse clinical outcome was generally noted. An example of Type 2 CRS could be congenital heart disease (CHD). In selected circumstances, long-standing CHD results in adaptive alterations in kidney perfusion and neurohormonal activation. In a study of 1102 adult patients with CHD, over 50% had evidence of kidney dysfunction, and 9% had eGFR < 60 mL/min/1.73 m2.28 This latter group had a three-fold increase in mortality. Kidney dysfunction was observed even among CHD patients with simple anatomical cardiac defects. A further challenge in describing the epidemiology of type 2 CRS is that patients may also transition between type 1 and type 2 CRS at various time points.
Acute reno-cardiac syndrome (type 3)
Defining the epidemiology of acute reno-cardiac syndrome (type 3) is challenging for several reasons: (i) considerable heterogeneity in predisposing conditions, (ii) different methods for defining AKI, (iii) variable baseline risk for the development of acute cardiac dysfunction (i.e. increased susceptibility in individuals with sub-clinical cardiovascular disease), and (iv) failure of many clinical studies of AKI to report the occurrence of acute cardiac dysfunction as outcomes. Accordingly, incidence estimates and clinical outcomes of acute cardiac dysfunction secondary to AKI are largely context and disease-specific. The group deliberated that RIFLE/AKIN criteria should be used to define AKI in the epidemiological studies.12
An example of type 3 CRS could be the development of an ACS, arrhythmia, or AHF after the onset of AKI or after acute glomerulonephritis or acute cortical necrosis. Toxaemia, fluid and sodium retention, humoral mediators, and electrolyte derangements may all contribute to acute dysfunction of the heart. Another case could be cardiac surgery-associated AKI (CSA-AKI), where AKI contributes to fluid overload and to the development of latent cardiac dysfunction. We also recognize that CSA-AKI may also represent type 1 CRS. This discrimination may have relevance as these two presentations may be characterized by important differences in epidemiology, risk factors, associated outcomes, and need for differing therapeutic interventions. The incidence of CSA-AKI has been reported between 0.3 and 29.7%.29–34 This large range in incidence is attributed to the different definitions used.35 However, the challenge in understanding the epidemiology of type 3 CRS is that its incidence and associated risk factors fail to consider the inciting event for CSA-AKI as either primarily AKI-related or heart-related.
Chronic reno-cardiac syndrome (type 4)
Several observational studies have evaluated the cardiovascular event rates and outcomes in selected CKD populations.36–48 Cardiac disease in CKD patients is common and cardiac-specific mortality rates are 10- to 20-fold higher compared with age and sex-matched non-CKD populations.36,42,49,50 In non-renal replacement therapy (RRT) dependent CKD patients, the prevalence of CVD correlates with severity of CKD. Several observational studies have found graded increases in the prevalence of CVD and heart failure (HF), along with higher risk of subsequent cardiac events associated with degree of decline in kidney function.40,45–48 This dose–response trend also translated into similar trends for the risk of cardiac-specific and all-cause mortality.36,40,43–45,48 Thus CKD likely accelerates the risk for and development of CVD.39,46,47
Secondary cardio-renal syndromes (type 5)
There are limited data on the epidemiology of secondary CRS (type 5) due to the large number of potential contributing acute and chronic systemic conditions. Accordingly, estimates of incidence, risk identification, and associated outcomes for type 5 CRS are considered largely disease and/or context-specific and may be time varying. We recognize that several chronic systemic illnesses (i.e. diabetes mellitus, hypertension, amyloidosis) could potentially fulfil the definition for CRS type 5, however, they may also at particular times in their natural history, fulfil criteria for other CRS subtypes. Importantly, in this context, there is currently an incomplete understanding of the pathophysiological mechanisms of secondary heart–kidney interactions.
A prototypical condition that may lead to CRS type 5 is sepsis. Sepsis is common and its incidence is increasing,51,52 with a mortality estimated between 20 and 60%.51–53 Approximately 11–64% of septic patients develop AKI that is associated with a higher morbidity and mortality.54–60 Abnormalities in cardiac function are also common in sepsis.61–63 Observational data have found ∼30–80% of septic patients have elevated cardiac-specific troponins,64–70 that often correlate with reduced left ventricular function.62,64,69,70 Acute kidney injury and myocardial injury/dysfunction in severe sepsis/septic shock are exceedingly common, yet there is a lack of integrative and epidemiological studies that have specifically examined for insight on its pathophysiology, incidence, risk identification, and associated outcomes.
Diagnosis and biomarkers of cardio-renal syndromes
The consensus group deliberated on the role of biomarkers in the diagnosis of the different types of the syndrome. The intention was to integrate biomarkers into the diagnosis of the various CRS, especially those that deal with AKI on top of acute cardiac disease. If biomarkers are to be clinically useful in these settings, physicians must be able to answer the following questions: (i) can biomarkers be used to (early) identify and classify CRS? (ii) Can biomarkers be used to risk-stratify patients with regard to reversibility? (iii) Can biomarkers be used as targets for treatment? (iv) Can biomarkers be used to monitor the effects of treatment?6,63–69 (v) Can imaging of the heart and kidneys be combined effectively with biomarkers across the spectrum of diagnosis and treatment of CRS?
Natriuretic peptides and heart failure
B-type natriuretic peptides (BNP and NT-proBNP) are established diagnostic tools in ADHF71 and represent independent predictors of cardiovascular events and overall mortality in critical illness,72 ACS,73 and stable HF.74 Natriuretic peptides (NPs) are elevated in patients with CRS (type 1) in which AKI occurs as a consequence of ADHF. Moreover, they have shown prognostic utility in patients with various stages of renal insufficiency,75,76 demonstrating potential applications in CRS types 2 and 4. Although many previous studies support the usefulness of BNP in the diagnosis and management of HF patients,77,78 the relationship between BNP, renal function, and the severity of HF is less clear. Patients with CKD have higher levels of BNP and NT-proBNP than age- and gender-matched subjects without reduced renal function, even in the absence of clinical CHF.79 Although these higher levels of NPs have been attributed to reduced renal clearance, there is likely some contribution from other mechanisms.80,81
Biomarkers of renal injury
Neutrophil gelatinase-associated lipocalin
Neutrophil gelatinase-associated lipocalin (NGAL) seems to be one of the earliest kidney markers of ischaemic or nephrotoxic injury in animal models and is detected in the blood and urine of humans soon after AKI.82–88 In a recent study, a single measurement of urinary NGAL was able to differentiate those with subsequent AKI, with a sensitivity and specificity of 90 and 99%, respectively. Neutrophil gelatinase-associated lipocalin could be used as an earlier marker of impending WRF during the treatment of ADHF.
Cystatin C
Cystatin C appears to be a better predictor of glomerular function than serum creatinine in patients with CKD. In AKI, urinary excretion of cystatin C has been shown to predict the requirement for RRT earlier than creatinine.89,90
Kidney injury molecule-1
Kidney injury molecule-1 (KIM-1) is a protein detectable in the urine after ischaemic or nephrotoxic insults to proximal tubular cells.91–93 Urinary KIM-1 seems to be highly specific for ischaemic AKI and not for pre-renal azotemia, CKD, or contrast induced nephropathy.94
N-acetyl-β-(d)glucosaminidase
N-acetyl-β-(d)glucosaminidase is a lysosomal brush border enzyme found in proximal tubular cells.94–96 N-acetyl-β-(d)glucosaminidase has been shown to function as a marker of kidney injury, reflecting particularly the degree of tubular damage.94 It is not only found in elevated urinary concentrations in AKI and CKD, but also in diabetic patients, patients with essential hypertension, and HF.97–99
Interleukin-18
Interleukin-18 (IL-18) is a pro-inflammatory cytokine detected in the urine after acute ischaemic proximal tubular damage.100 It displays good sensitivity and specificity for ischaemic AKI with an AUC > 90%101 with increased levels 48 h prior to increases in serum creatinine.102 Urinary NGAL and IL-18 have been studied as joint biomarkers for delayed graft function following kidney transplantation.103
Of the biomarkers presented above, NGAL (urine and plasma) and Cystatin C are most likely to be integrated into clinical practice in the near future. Clinical trials will be needed to see if earlier identification of AKI and the use of specific treatment algorithms based on these markers will improve prognosis.
Bioimpedance vector analysis
There is a general agreement that bioimpedance vector analysis (BIVA) may contribute to a better definition of the patient's hydration status. This may be used in combination with NGAL and BNP to guide fluid management strategies. In this way, patients will be kept within the narrow window of adequate hydration preventing worsening of both kidney and heart function.
Imaging
Imaging techniques have an additional role with respect to the laboratory biomarkers in CRS. They may enhance, extend, and refine our ability to quantify renal damage and function. In patients affected by suspected CRS, it is prudent to avoid the use of iodinated contrast media if not strictly necessary. The presence of coronary disease should be excluded by stress echo or stress myocardial perfusion (SPECT/PET) in types III, IV, and V CRS and in types I and II CRS when the primary cardiac disease is valvular, congenital, or myopathic. In the future, research should be directed toward experimental studies that apply molecular imaging techniques (MRI and MRS, PET, etc.) to the search for in vivo specific markers for diagnosis and severity evaluation of the different types of CRS. Also in the future, non-invasive imaging techniques should be refined to quantify renal blood flow. Such data can then be correlated with cardiac and renal biomarkers and most importantly guide ongoing therapy designed to optimize renal blood flow and ultimately preserve kidney function. As for type 1 CRS, venous congestion and high CVP seem to be associated with impaired renal function and independently related to all-cause mortality in a broad spectrum of patients with cardiovascular disease.104
Prevention of cardio-renal syndromes
The rationale for the prevention of CRS is based on the concept that once the syndrome begins it is difficult to interrupt, not completely reversible in all cases, and associated with serious adverse outcomes. We approached prevention using a proposed classification system.4,105,106
Acute cardio-renal syndrome (type 1)
The most important preventive approach in patients with de novo HF consists of the basic preventive strategies of the American Heart Association/American College of Cardiology for Stage A and B HF. These call for blood pressure control, use of drugs that block the renin–angiotensin–aldosterone system, beta-adrenergic blockers (BB), coronary artery disease risk factor modification, and compliance with dietary and drug treatments. As venous congestion seems to be an important haemodynamic factor driving WRF26 in ADHF, future studies should evaluate whether a CVP-tailored therapy might prevent WRF in those patients.
Chronic cardio-renal syndrome (type 2)
In this setting, therapies that improve the natural history of chronic HF include angiotensin converting enzyme inhibitors (ACE-I), angiotensin receptor blockers (ARB), BB, aldosterone receptor blockers, combination of nitrates and hydralazine, and cardiac re-synchronization therapy.106,107
Acute reno-cardiac syndrome (type 3)
The clinical problem in many cases is sodium and water retention. Avoidance of hypervolaemia should help prevent cardiac decompensation. In addition, uremic changes, hyperkalaemia, and mediators of inflammation can have adverse cardiac consequences.106,108 As mentioned previously, prototypical scenarios for type 3 CRS include forms of AKI (e.g. rapidly progressive glomerulonephritis) that secondarily lead to LV dysfunction. Contrast-induced AKI in most cases is asymptomatic106,109 and unlikely to cause cardiac dysfunction. However, some patients with contrast-induced AKI develop progressive renal failure, volume overload, and ADHF requiring intensive care treatment and/or transient and sometimes permanent dialysis.110
Chronic reno-cardiac syndrome (type 4)
Type 4 CRS is a common syndrome since it involves the progression of CKD, often due to diabetes mellitus and hypertension, with accelerated calcific atherosclerosis, progressive LVH, and the development of diastolic and systolic dysfunction.111 The core prevention concept beyond attention to usual risk factor modification is that the reduction in the rate of progression of CKD may lead to reduced rates of type 4 CRS.
Secondary cardio-renal syndrome (type 5)
A core concept is that treatment of the primary illness (diabetes mellitus, amyloidosis, sepsis, rhabdomyolysis, haemorrhagic shock, etc.) in general improves both heart and kidney function.
Management strategies of cardio-renal syndromes
Although there are clinical guidelines for managing both HF and CKD,10,112,113 there are no agreed guidelines for managing patients with cardio-renal and/or reno-cardiac syndromes.114
Acute cardio-renal syndrome (type 1)
Both abnormal renal function and also a deterioration early in the course of treatment of ADHF increase mortality. Thus, any treatment for HF should have a neutral effect or preferably improve renal function.112
The management of ADHF is described in the recent ESC/ESICM guidelines.112 Vasodilators115 and loop diuretics are widely recommended in cases of ADHF and in CRS type 1. However, loop diuretics predispose to electrolyte imbalances, and hypovolaemia leading to neurohumoral activation, reduced renal glomerular flow with further rises in serum urea and creatinine.116 Vasodilators (e.g. nesiritide) may also affect renal function117 and in some cases exacerbate renal injury. Vasopressin receptor 2 antagonists can improve hyponatraemia, but without any clear survival benefit.118 If congestion coincides with low blood pressure, inotropic agents should be considered.
In cardiogenic shock, treatments are designed to increase cardiac output and restore renal blood flow. Although inotropic drugs, typically dobutamine or dopamine, may tide patients over, they are often associated with increased mid-term mortality.119 Other agents include phosphodiesterase inhibitors, milrinone, and levosimendan.112 Extracorporeal ultrafiltration may be useful in ADHF associated with diuretic resistance. If systemic hypotension persists, then norepineprine may be considered, along with elective ventilation and/or intra-aortic balloon pumping. Depending upon pre-existing co-morbidity and the underlying aetiology, left ventricular assist devices as a bridge to transplantation or cardiac surgery may be appropriate.120 It should be mentioned that over-treatment with loop diuretics, ACE-I, and/or spironolactone may induce AKI.
Chronic cardio-renal syndrome (type 2)
Therapeutic approaches to patients with CHF are complex and involve the elimination and treatment of the underlying cause and/or disease leading to damage of the cardiovascular system and CHF progression. Self-care management is an important strategy in CHF, encompassing adherence to treatment, symptom recognition, and lifestyle changes (diet and nutrition, smoking cessation, exercise training).112
Angiotensin converting enzyme inhibitors,121 beta-blockers,122 ARBs,123 and aldosterone antagonists124 significantly reduce mortality and morbidity in CHF. The optimal approach is to combine ACE-I and beta-blocker, titrate dosages, to which either an ARB or aldosterone antagonist is subsequently added depending on clinical condition and patient characteristics. In patients unable to tolerate these agents, hydralazine and nitrates may be an option.112 Digoxin and diuretics improve symptoms in CHF but have no effect on mortality.119
Cardiac re-synchronization therapy is now recommended for symptomatic CHF patients (NYHA III–IV) with poor left ventricular ejection fraction (LVEF) and QRS prolongation,112 as are implantable cardiac defibrillators for both survivors of cardiac arrest and/or sustained ventricular arrhythmias and also for symptomatic CHF patients with impaired LVEF. In selected patients who do not respond to treatment, mechanical assist devices and/or cardiac transplantation may be appropriate.120
Therapy of CHF with concomitant renal impairment is still not evidence-based, as these patients are generally excluded from CHF trials.121–124 Typically, these patients are hypervolemic, and more intensive diuretic treatment is needed.113 Thiazide diuretics may be less effective, and loop diuretics are preferred.113 To improve natriuresis, loop diuretic infusions are more potent, and combinations with amiloride, aldosterone antagonists, or metolazone may be considered,124 as increasing doses of loop diuretics are associated with worse outcomes.125 In refractory cases, RRT may be required.
Angiotensin converting enzyme inhibitor and ARB initiation may cause deterioration in renal function, which is frequently transient and reversible. Patients with CKD or renal artery stenosis are at a higher risk, and careful monitoring is recommended. If renal function declines, then other secondary causes such as excessive diuresis, persistent hypotension, prescription of nephrotoxic agents or underlying renovascular disease should be excluded. Hyperkalaemia occurs with these agents and dietary restriction may be required.121,123,124
Anaemia is often present in patients with type 2 CRS, and correction of anaemia may improve symptoms without increasing survival.112 Renal dysfunction is associated with altered drug clearances, and some drugs, e.g. digoxin and allopurinol, require dose adjustment, and the risk of spontaneous haemorrhage with warfarin is increased.
Acute reno-cardiac syndrome (type 3)
As previously discussed, type 3 CRS has only recently been recognized as a clinical entity, hence there is little known about the treatment of this complication. Since a typical clinical scenario would include AKI following contrast exposure, or following cardiovascular surgery (CSA-AKI), prevention likely affords a better chance to improve outcome than treating established disease. To prevent contrast nephropathy, many potential preventive strategies have been studied, and available evidence indicates that isotonic fluids have been the most successful intervention to date, with conflicting data surrounding N-acetylcysteine.126,127 Recently, Solomon et al.,128 using a more sensitive definition of AKI, identified a possible role for the low-osmolar, non-ionic monomer iopamidol. Germane to the discussion of CRS, they identified that patients suffering AKI secondary to contrast were almost twice as likely to suffer downstream adverse events, including cardiovascular events, in the year following the contrast exposure, indicative of the serious consequences of type 3 CRS.
In terms of prevention of CSA-AKI, in a recent prospective, double-blind study of patients with left ventricular dysfunction undergoing cardiac surgery, nesiritide was associated with improved post-operative renal function compared with patients without nesiritide, thus suggesting a renoprotective property.129
Chronic reno-cardiac syndrome (type 4)
The aetiology of HF in CKD is multifactorial. Despite cardioprotective strategies such as ACE-Is and/or beta-blockers only a minority of dialysis patients are prescribed these drugs.130 Antihypertensives have been thought to increase intradialytic hypotension, but this has not been proven.131
Progressive CKD often leads to sodium retention due to reduced renal excretion,113 and similarly during haemodialysis due to dietary noncompliance, inappropriately high dialysate sodium and inability to achieve target or ‘dry’ weight.132 Besides preventing hypervolaemia and a positive sodium balance, the other key management strategies include correcting anaemia and minimizing vascular calcification.113,114
Conclusions
The aim of the ADQI consensus conference on CRS was to facilitate better understanding of their epidemiology, opportunities for early diagnosis through biomarkers, development of preventive strategies, and application of evidence-based management strategies (where available). A further aim was to allow identification of gaps in the literature and provide direction for future research including clinical trials. We have defined five syndromes that can now be the target of future studies, described series of biomarkers which may facilitate the identification and treatment of such syndromes and have outlined general strategies for prevention and management. We hope this document will serve as starting point for focused research into the care of these conditions which affect so many people worldwide.
Funding
The ADQI consensus conference was supported by the non profit organization AARVI (Associazione Amici del Rene di Vicenza) and its research branch IRRIV (International Renal Research Insitute of Vicenza). Funding to pay the Open Access publication charges for this article was provided by AARVI-IRRIV (Associazione Amici del Rene di Vicenza and International Renal Research Institute of Vicenza).
Conflict of interest: none declared.
References
- 1.Heywood JT. The cardiorenal syndrome: lessons from the ADHERE database and treatment options. Heart Fail Rev. 2004;9:195–201. doi: 10.1007/s10741-005-6129-4. [DOI] [PubMed] [Google Scholar]
- 2.Forman DE, Butler J, Wang Y, Abraham WT, O'Connor CM, Gottlieb SS, Loh E, Massie BM, Rich MW, Stevenson LW, Young JB, Krumholz HM. Incidence, predictors at admission, and impact of worsening renal function among patients hospitalized with heart failure. J Am Coll Cardiol. 2004;43:61–67. doi: 10.1016/j.jacc.2003.07.031. [DOI] [PubMed] [Google Scholar]
- 3.Isles C. Cardiorenal failure: pathophysiology, recognition and treatment. Clin Med. 2002;2:195–200. doi: 10.7861/clinmedicine.2-3-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ronco C, House AA, Haapio M. Cardiorenal syndrome: refining the definition of a complex symbiosis gone wrong. Intensive Care Med. 2008;34:957–962. doi: 10.1007/s00134-008-1017-8. [DOI] [PubMed] [Google Scholar]
- 5.Liang KV, Williams AW, Greene EL, Redfield MM. Acute decompensated heart failure and the cardiorenal syndrome. Crit Care Med. 2008;36(Suppl. 1):S75–S88. doi: 10.1097/01.CCM.0000296270.41256.5C. [DOI] [PubMed] [Google Scholar]
- 6.Bongartz LG, Cramer MJ, Doevendans PA, Joles JA, Braam B. The severe cardiorenal syndrome: 'Guyton revisited'. Eur Heart J. 2005;26:11–17. doi: 10.1093/eurheartj/ehi020. [DOI] [PubMed] [Google Scholar]
- 7.Schrier RW. Cardiorenal versus renocardiac syndrome: is there a difference? Nat Clin Pract Nephrol. 2007;3:637. doi: 10.1038/ncpneph0673. [DOI] [PubMed] [Google Scholar]
- 8.Kellum JA, Bellomo R, Ronco C. Acute Dialysis Quality Initiative (ADQI): methodology. Int J Artif Organs. 2008;31:90–93. doi: 10.1177/039139880803100202. [DOI] [PubMed] [Google Scholar]
- 9.Gottlieb SS, Abraham W, Butler J, Forman DE, Loh E, Massie BM, O'Connor C M, Rich MW, Stevenson LW, Young J, Krumholz HM. The prognostic importance of different definitions of worsening renal function in congestive heart failure. J Card Fail. 2002;8:136–141. doi: 10.1054/jcaf.2002.125289. [DOI] [PubMed] [Google Scholar]
- 10.National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39(Suppl. 2 1):S1–S266. [PubMed] [Google Scholar]
- 11.Heywood JT, Fonarow GC, Costanzo MR, Mathur VS, Wigneswaran JR, Wynne J. High prevalence of renal dysfunction and its impact on outcome in 118,465 patients hospitalized with acute decompensated heart failure: a report from the ADHERE database. J Card Fail. 2007;13:422–430. doi: 10.1016/j.cardfail.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 12.Kellum JA, Levin N, Bouman C, Lameire N. Developing a consensus classification system for acute renal failure. Curr Opin Crit Care. 2002;8:509–514. doi: 10.1097/00075198-200212000-00005. [DOI] [PubMed] [Google Scholar]
- 13.Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, McAlister F, Garg AX. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol. 2006;17:2034–2047. doi: 10.1681/ASN.2005101085. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg A, Hammerman H, Petcherski S, Zdorovyak A, Yalonetsky S, Kapeliovich M, Agmon Y, Markiewicz W, Aronson D. Inhospital and 1-year mortality of patients who develop worsening renal function following acute ST-elevation myocardial infarction. Am Heart J. 2005;150:330–337. doi: 10.1016/j.ahj.2004.09.055. [DOI] [PubMed] [Google Scholar]
- 15.Krumholz HM, Chen YT, Vaccarino V, Wang Y, Radford MJ, Bradford WD, Horwitz RI. Correlates and impact on outcomes of worsening renal function in patients > or =65 years of age with heart failure. Am J Cardiol. 2000;85:1110–1113. doi: 10.1016/s0002-9149(00)00705-0. [DOI] [PubMed] [Google Scholar]
- 16.Krumholz HM, Parent EM, Tu N, Vaccarino V, Wang Y, Radford MJ, Hennen J. Readmission after hospitalization for congestive heart failure among Medicare beneficiaries. Arch Intern Med. 1997;157:99–104. [PubMed] [Google Scholar]
- 17.Newsome BB, Warnock DG, McClellan WM, Herzog CA, Kiefe CI, Eggers PW, Allison JJ. Long-term risk of mortality and end-stage renal disease among the elderly after small increases in serum creatinine level during hospitalization for acute myocardial infarction. Arch Intern Med. 2008;168:609–616. doi: 10.1001/archinte.168.6.609. [DOI] [PubMed] [Google Scholar]
- 18.Parikh CR, Coca SG, Wang Y, Masoudi FA, Krumholz HM. Long-term prognosis of acute kidney injury after acute myocardial infarction. Arch Intern Med. 2008;168:987–995. doi: 10.1001/archinte.168.9.987. [DOI] [PubMed] [Google Scholar]
- 19.Jose P, Skali H, Anavekar N, Tomson C, Krumholz HM, Rouleau JL, Moye L, Pfeffer MA, Solomon SD. Increase in creatinine and cardiovascular risk in patients with systolic dysfunction after myocardial infarction. J Am Soc Nephrol. 2006;17:2886–2891. doi: 10.1681/ASN.2006010063. [DOI] [PubMed] [Google Scholar]
- 20.Nohria A, Hasselblad V, Stebbins A, Pauly DF, Fonarow GC, Shah M, Yancy CW, Califf RM, Stevenson LW, Hill JA. Cardiorenal interactions: insights from the ESCAPE trial. J Am Coll Cardiol. 2008;51:1268–1274. doi: 10.1016/j.jacc.2007.08.072. [DOI] [PubMed] [Google Scholar]
- 21.Cowie MR, Komajda M, Murray-Thomas T, Underwood J, Ticho B. Prevalence and impact of worsening renal function in patients hospitalized with decompensated heart failure: results of the prospective outcomes study in heart failure (POSH) Eur Heart J. 2006;27:1216–1222. doi: 10.1093/eurheartj/ehi859. [DOI] [PubMed] [Google Scholar]
- 22.Logeart D, Tabet JY, Hittinger L, Thabut G, Jourdain P, Maison P, Tartiere JM, Solal AC. Transient worsening of renal function during hospitalization for acute heart failure alters outcome. Int J Cardiol. 2008;127:228–232. doi: 10.1016/j.ijcard.2007.06.007. [DOI] [PubMed] [Google Scholar]
- 23.Metra M, Nodari S, Parrinello G, Bordonali T, Bugatti S, Danesi R, Fontanella B, Lombardi C, Milani P, Verzura G, Cotter G, Dittrich H, Massie BM, Dei Cas L. Worsening renal function in patients hospitalised for acute heart failure: clinical implications and prognostic significance. Eur J Heart Fail. 2008;10:188–195. doi: 10.1016/j.ejheart.2008.01.011. [DOI] [PubMed] [Google Scholar]
- 24.Smith GL, Vaccarino V, Kosiborod M, Lichtman JH, Cheng S, Watnick SG, Krumholz HM. Worsening renal function: what is a clinically meaningful change in creatinine during hospitalization with heart failure? J Card Fail. 2003;9:13–25. doi: 10.1054/jcaf.2003.3. [DOI] [PubMed] [Google Scholar]
- 25.Latchamsetty R, Fang J, Kline-Rogers E, Mukherjee D, Otten RF, LaBounty TM, Emery MS, Eagle KA, Froehlich JB. Prognostic value of transient and sustained increase in in-hospital creatinine on outcomes of patients admitted with acute coronary syndrome. Am J Cardiol. 2007;99:939–942. doi: 10.1016/j.amjcard.2006.10.058. [DOI] [PubMed] [Google Scholar]
- 26.Mullens W, Abrahams Z, Francis GS, Sokos G, Taylor DO, Starling RC, Young JB, Tang WH. Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol. 2009;53:589–596. doi: 10.1016/j.jacc.2008.05.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ahmed A, Rich MW, Sanders PW, Perry GJ, Bakris GL, Zile MR, Love TE, Aban IB, Shlipak MG. Chronic kidney disease associated mortality in diastolic versus systolic heart failure: a propensity matched study. Am J Cardiol. 2007;99:393–398. doi: 10.1016/j.amjcard.2006.08.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dimopoulos K, Diller GP, Koltsida E, Pijuan-Domenech A, Papadopoulou SA, Babu-Narayan SV, Salukhe TV, Piepoli MF, Poole-Wilson PA, Best N, Francis DP, Gatzoulis MA. Prevalence, predictors, and prognostic value of renal dysfunction in adults with congenital heart disease. Circulation. 2008;117:2320–2328. doi: 10.1161/CIRCULATIONAHA.107.734921. [DOI] [PubMed] [Google Scholar]
- 29.Burns KE, Chu MW, Novick RJ, Fox SA, Gallo K, Martin CM, Stitt LW, Heidenheim AP, Myers ML, Moist L. Perioperative N-acetylcysteine to prevent renal dysfunction in high-risk patients undergoing cabg surgery: a randomized controlled trial. J Am Med Assoc. 2005;294:342–350. doi: 10.1001/jama.294.3.342. [DOI] [PubMed] [Google Scholar]
- 30.Leacche M, Rawn JD, Mihaljevic T, Lin J, Karavas AN, Paul S, Byrne JG. Outcomes in patients with normal serum creatinine and with artificial renal support for acute renal failure developing after coronary artery bypass grafting. Am J Cardiol. 2004;93:353–356. doi: 10.1016/j.amjcard.2003.10.020. [DOI] [PubMed] [Google Scholar]
- 31.Chertow GM, Levy EM, Hammermeister KE, Grover F, Daley J. Independent association between acute renal failure and mortality following cardiac surgery. Am J Med. 1998;104:343–348. doi: 10.1016/s0002-9343(98)00058-8. [DOI] [PubMed] [Google Scholar]
- 32.Conlon PJ, Stafford-Smith M, White WD, Newman MF, King S, Winn MP, Landolfo K. Acute renal failure following cardiac surgery. Nephrol Dial Transplant. 1999;14:1158–1162. doi: 10.1093/ndt/14.5.1158. [DOI] [PubMed] [Google Scholar]
- 33.Bove T, Calabro MG, Landoni G, Aletti G, Marino G, Crescenzi G, Rosica C, Zangrillo A. The incidence and risk of acute renal failure after cardiac surgery. J Cardiothorac Vasc Anesth. 2004;18:442–445. doi: 10.1053/j.jvca.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 34.Mangano CM, Diamondstone LS, Ramsay JG, Aggarwal A, Herskowitz A, Mangano DT. Renal dysfunction after myocardial revascularization: risk factors, adverse outcomes, and hospital resource utilization. The Multicenter Study of Perioperative Ischemia Research Group. Ann Intern Med. 1998;128:194–203. doi: 10.7326/0003-4819-128-3-199802010-00005. [DOI] [PubMed] [Google Scholar]
- 35.Hoste EA, Cruz DN, Davenport A, Mehta RL, Piccinni P, Tetta C, Viscovo G, Ronco C. The epidemiology of cardiac surgery-associated acute kidney injury. Int J Artif Organs. 2008;31:158–165. doi: 10.1177/039139880803100209. [DOI] [PubMed] [Google Scholar]
- 36.Cheung AK, Sarnak MJ, Yan G, Berkoben M, Heyka R, Kaufman A, Lewis J, Rocco M, Toto R, Windus D, Ornt D, Levey AS. Cardiac diseases in maintenance hemodialysis patients: results of the HEMO Study. Kidney Int. 2004;65:2380–2389. doi: 10.1111/j.1523-1755.2004.00657.x. [DOI] [PubMed] [Google Scholar]
- 37.Culleton BF, Larson MG, Wilson PW, Evans JC, Parfrey PS, Levy D. Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int. 1999;56:2214–2219. doi: 10.1046/j.1523-1755.1999.00773.x. [DOI] [PubMed] [Google Scholar]
- 38.Dries DL, Exner DV, Domanski MJ, Greenberg B, Stevenson LW. The prognostic implications of renal insufficiency in asymptomatic and symptomatic patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2000;35:681–689. doi: 10.1016/s0735-1097(99)00608-7. [DOI] [PubMed] [Google Scholar]
- 39.Foley RN, Murray AM, Li S, Herzog CA, McBean AM, Eggers PW, Collins AJ. Chronic kidney disease and the risk for cardiovascular disease, renal replacement, and death in the United States Medicare population, 1998 to 1999. J Am Soc Nephrol. 2005;16:489–495. doi: 10.1681/ASN.2004030203. [DOI] [PubMed] [Google Scholar]
- 40.Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004;351:1296–1305. doi: 10.1056/NEJMoa041031. [DOI] [PubMed] [Google Scholar]
- 41.Henry RM, Kostense PJ, Bos G, Dekker JM, Nijpels G, Heine RJ, Bouter LM, Stehouwer CD. Mild renal insufficiency is associated with increased cardiovascular mortality: The Hoorn Study. Kidney Int. 2002;62:1402–1407. doi: 10.1111/j.1523-1755.2002.kid571.x. [DOI] [PubMed] [Google Scholar]
- 42.Herzog CA, Ma JZ, Collins AJ. Poor long-term survival after acute myocardial infarction among patients on long-term dialysis. N Engl J Med. 1998;339:799–805. doi: 10.1056/NEJM199809173391203. [DOI] [PubMed] [Google Scholar]
- 43.Hillege HL, Nitsch D, Pfeffer MA, Swedberg K, McMurray JJ, Yusuf S, Granger CB, Michelson EL, Ostergren J, Cornel JH, de Zeeuw D, Pocock S, van Veldhuisen DJ. Renal function as a predictor of outcome in a broad spectrum of patients with heart failure. Circulation. 2006;113:671–678. doi: 10.1161/CIRCULATIONAHA.105.580506. [DOI] [PubMed] [Google Scholar]
- 44.Mahon NG, Blackstone EH, Francis GS, Starling RC, III, Young JB, Lauer MS. The prognostic value of estimated creatinine clearance alongside functional capacity in ambulatory patients with chronic congestive heart failure. J Am Coll Cardiol. 2002;40:1106–1113. doi: 10.1016/s0735-1097(02)02125-3. [DOI] [PubMed] [Google Scholar]
- 45.McCullough PA, Jurkovitz CT, Pergola PE, McGill JB, Brown WW, Collins AJ, Chen SC, Li S, Singh A, Norris KC, Klag MJ, Bakris GL. Independent components of chronic kidney disease as a cardiovascular risk state: results from the Kidney Early Evaluation Program (KEEP) Arch Intern Med. 2007;167:1122–1129. doi: 10.1001/archinte.167.11.1122. [DOI] [PubMed] [Google Scholar]
- 46.McCullough PA, Li S, Jurkovitz CT, Stevens LA, Wang C, Collins AJ, Chen SC, Norris KC, McFarlane SI, Johnson B, Shlipak MG, Obialo CI, Brown WW, Vassalotti JA, Whaley-Connell AT. CKD and cardiovascular disease in screened high-risk volunteer and general populations: the Kidney Early Evaluation Program (KEEP) and National Health and Nutrition Examination Survey (NHANES) 1999–2004. Am J Kidney Dis. 2008;51(4 Suppl. 2):S38–S45. doi: 10.1053/j.ajkd.2007.12.017. [DOI] [PubMed] [Google Scholar]
- 47.McCullough PA, Li S, Jurkovitz CT, Stevens L, Collins AJ, Chen SC, Norris KC, McFarlane S, Johnson B, Shlipak MG, Obialo CI, Brown WW, Vassalotti J, Whaley-Connell AT, Brenner RM, Bakris GL. Chronic kidney disease, prevalence of premature cardiovascular disease, and relationship to short-term mortality. Am Heart J. 2008;156:277–283. doi: 10.1016/j.ahj.2008.02.024. [DOI] [PubMed] [Google Scholar]
- 48.Muntner P, He J, Hamm L, Loria C, Whelton PK. Renal insufficiency and subsequent death resulting from cardiovascular disease in the United States. J Am Soc Nephrol. 2002;13:745–753. doi: 10.1681/ASN.V133745. [DOI] [PubMed] [Google Scholar]
- 49.Johnson DW, Craven AM, Isbel NM. Modification of cardiovascular risk in hemodialysis patients: an evidence-based review. Hemodial Int. 2007;11:1–14. doi: 10.1111/j.1542-4758.2007.00146.x. [DOI] [PubMed] [Google Scholar]
- 50.Herzog CA. Dismal long-term survival of dialysis patients after acute myocardial infarction: can we alter the outcome? Nephrol Dial Transplant. 2002;17:7–10. doi: 10.1093/ndt/17.1.7. [DOI] [PubMed] [Google Scholar]
- 51.Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001;29:1303–1310. doi: 10.1097/00003246-200107000-00002. [DOI] [PubMed] [Google Scholar]
- 52.Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003;348:1546–1554. doi: 10.1056/NEJMoa022139. [DOI] [PubMed] [Google Scholar]
- 53.Alberti C, Brun-Buisson C, Burchardi H, Martin C, Goodman S, Artigas A, Sicignano A, Palazzo M, Moreno R, Boulme R, Lepage E, Le Gall R. Epidemiology of sepsis and infection in ICU patients from an international multicentre cohort study. Intensive Care Med. 2002;28:108–121. doi: 10.1007/s00134-001-1143-z. [DOI] [PubMed] [Google Scholar]
- 54.Bagshaw SM, Lapinsky S, Dial S, Arabi Y, Dodek P, Wood G, Ellis P, Guzman J, Marshall J, Parrillo JE, Skrobik Y, Kumar A. Acute kidney injury in septic shock: clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy. Intensive Care Med. 2009;35:871–881. doi: 10.1007/s00134-008-1367-2. [DOI] [PubMed] [Google Scholar]
- 55.Hoste EA, Lameire NH, Vanholder RC, Benoit DD, Decruyenaere JM, Colardyn FA. Acute renal failure in patients with sepsis in a surgical ICU: predictive factors, incidence, comorbidity, and outcome. J Am Soc Nephrol. 2003;14:1022–1030. doi: 10.1097/01.asn.0000059863.48590.e9. [DOI] [PubMed] [Google Scholar]
- 56.Lopes JA, Jorge S, Resina C, Santos C, Pereira A, Neves J, Antunes F, Prata MM. Acute renal failure in patients with sepsis. Crit Care. 2007;11:411. doi: 10.1186/cc5735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Oppert M, Engel C, Brunkhorst FM, Bogatsch H, Reinhart K, Frei U, Eckardt KU, Loeffler M, John S. Acute renal failure in patients with severe sepsis and septic shock—a significant independent risk factor for mortality: results from the German Prevalence Study. Nephrol Dial Transplant. 2008;23:904–909. doi: 10.1093/ndt/gfm610. [DOI] [PubMed] [Google Scholar]
- 58.Vincent JL, Sakr Y, Sprung CL, Ranieri VM, Reinhart K, Gerlach H, Moreno R, Carlet J, Le Gall JR, Payen D. Sepsis in European intensive care units: results of the SOAP study. Crit Care Med. 2006;34:344–353. doi: 10.1097/01.ccm.0000194725.48928.3a. [DOI] [PubMed] [Google Scholar]
- 59.Yegenaga I, Hoste E, Van Biesen W, Vanholder R, Benoit D, Kantarci G, Dhondt A, Colardyn F, Lameire N. Clinical characteristics of patients developing ARF due to sepsis/systemic inflammatory response syndrome: results of a prospective study. Am J Kidney Dis. 2004;43:817–824. doi: 10.1053/j.ajkd.2003.12.045. [DOI] [PubMed] [Google Scholar]
- 60.Bagshaw SM, George C, Bellomo R. Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care. 2008;12:R47. doi: 10.1186/cc6863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Charpentier J, Luyt CE, Fulla Y, Vinsonneau C, Cariou A, Grabar S, Dhainaut JF, Mira JP, Chiche JD. Brain natriuretic peptide: a marker of myocardial dysfunction and prognosis during severe sepsis. Crit Care Med. 2004;32:660–665. doi: 10.1097/01.ccm.0000114827.93410.d8. [DOI] [PubMed] [Google Scholar]
- 62.ver Elst KM, Spapen HD, Nguyen DN, Garbar C, Huyghens LP, Gorus FK. Cardiac troponins I and T are biological markers of left ventricular dysfunction in septic shock. Clin Chem. 2000;46:650–657. [PubMed] [Google Scholar]
- 63.Jardin F, Fourme T, Page B, Loubieres Y, Vieillard-Baron A, Beauchet A, Bourdarias JP. Persistent preload defect in severe sepsis despite fluid loading: a longitudinal echocardiographic study in patients with septic shock. Chest. 1999;116:1354–1359. doi: 10.1378/chest.116.5.1354. [DOI] [PubMed] [Google Scholar]
- 64.Fernandes CJ, Jr, Akamine N, Knobel E. Cardiac troponin: a new serum marker of myocardial injury in sepsis. Intensive Care Med. 1999;25:1165–1168. doi: 10.1007/s001340051030. [DOI] [PubMed] [Google Scholar]
- 65.Spies C, Haude V, Fitzner R, Schroder K, Overbeck M, Runkel N, Schaffartzik W. Serum cardiac troponin T as a prognostic marker in early sepsis. Chest. 1998;113:1055–1063. doi: 10.1378/chest.113.4.1055. [DOI] [PubMed] [Google Scholar]
- 66.Turner A, Tsamitros M, Bellomo R. Myocardial cell injury in septic shock. Crit Care Med. 1999;27:1775–1780. doi: 10.1097/00003246-199909000-00012. [DOI] [PubMed] [Google Scholar]
- 67.Arlati S, Brenna S, Prencipe L, Marocchi A, Casella GP, Lanzani M, Gandini C. Myocardial necrosis in ICU patients with acute non-cardiac disease: a prospective study. Intensive Care Med. 2000;26:31–37. doi: 10.1007/s001340050008. [DOI] [PubMed] [Google Scholar]
- 68.Ammann P, Fehr T, Minder EI, Gunter C, Bertel O. Elevation of troponin I in sepsis and septic shock. Intensive Care Med. 2001;27:965–969. doi: 10.1007/s001340100920. [DOI] [PubMed] [Google Scholar]
- 69.Mehta NJ, Khan IA, Gupta V, Jani K, Gowda RM, Smith PR. Cardiac troponin I predicts myocardial dysfunction and adverse outcome in septic shock. Int J Cardiol. 2004;95:13–17. doi: 10.1016/j.ijcard.2003.02.005. [DOI] [PubMed] [Google Scholar]
- 70.Ammann P, Maggiorini M, Bertel O, Haenseler E, Joller-Jemelka HI, Oechslin E, Minder EI, Rickli H, Fehr T. Troponin as a risk factor for mortality in critically ill patients without acute coronary syndromes. J Am Coll Cardiol. 2003;41:2004–2009. doi: 10.1016/s0735-1097(03)00421-2. [DOI] [PubMed] [Google Scholar]
- 71.Maisel A, Hollander JE, Guss D, McCullough P, Nowak R, Green G, Saltzberg M, Ellison SR, Bhalla MA, Bhalla V, Clopton P, Jesse R. Primary results of the Rapid Emergency Department Heart Failure Outpatient Trial (REDHOT). A multicenter study of B-type natriuretic peptide levels, emergency department decision making, and outcomes in patients presenting with shortness of breath. J Am Coll Cardiol. 2004;44:1328–1333. doi: 10.1016/j.jacc.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 72.Meyer B, Huelsmann M, Wexberg P, Delle Karth G, Berger R, Moertl D, Szekeres T, Pacher R, Heinz G. N-terminal pro-B-type natriuretic peptide is an independent predictor of outcome in an unselected cohort of critically ill patients. Crit Care Med. 2007;35:2268–2273. doi: 10.1097/01.CCM.0000284509.23439.5B. [DOI] [PubMed] [Google Scholar]
- 73.Morrow DA, de Lemos JA, Blazing MA, Sabatine MS, Murphy SA, Jarolim P, White HD, Fox KA, Califf RM, Braunwald E. Prognostic value of serial B-type natriuretic peptide testing during follow-up of patients with unstable coronary artery disease. J Am Med Assoc. 2005;294:2866–2871. doi: 10.1001/jama.294.22.2866. [DOI] [PubMed] [Google Scholar]
- 74.Latini R, Masson S, Anand I, Salio M, Hester A, Judd D, Barlera S, Maggioni AP, Tognoni G, Cohn JN. The comparative prognostic value of plasma neurohormones at baseline in patients with heart failure enrolled in Val-HeFT. Eur Heart J. 2004;25:292–299. doi: 10.1016/j.ehj.2003.10.030. [DOI] [PubMed] [Google Scholar]
- 75.Carr SJ, Bavanandan S, Fentum B, Ng L. Prognostic potential of brain natriuretic peptide (BNP) in predialysis chronic kidney disease patients. Clin Sci (Lond) 2005;109:75–82. doi: 10.1042/CS20040351. [DOI] [PubMed] [Google Scholar]
- 76.Austin WJ, Bhalla V, Hernandez-Arce I, Isakson SR, Beede J, Clopton P, Maisel AS, Fitzgerald RL. Correlation and prognostic utility of B-type natriuretic peptide and its amino-terminal fragment in patients with chronic kidney disease. Am J Clin Pathol. 2006;126:506–512. doi: 10.1309/M7AAXA0J1THMNCDF. [DOI] [PubMed] [Google Scholar]
- 77.Januzzi JL, Jr, Camargo CA, Anwaruddin S, Baggish AL, Chen AA, Krauser DG, Tung R, Cameron R, Nagurney JT, Chae CU, Lloyd-Jones DM, Brown DF, Foran-Melanson S, Sluss PM, Lee-Lewandrowski E, Lewandrowski KB. The N-terminal Pro-BNP investigation of dyspnea in the emergency department (PRIDE) study. Am J Cardiol. 2005;95:948–954. doi: 10.1016/j.amjcard.2004.12.032. [DOI] [PubMed] [Google Scholar]
- 78.McCullough PA, Nowak RM, McCord J, Hollander JE, Herrmann HC, Steg PG, Duc P, Westheim A, Omland T, Knudsen CW, Storrow AB, Abraham WT, Lamba S, Wu AH, Perez A, Clopton P, Krishnaswamy P, Kazanegra R, Maisel AS. B-type natriuretic peptide and clinical judgment in emergency diagnosis of heart failure: analysis from Breathing Not Properly (BNP) Multinational Study. Circulation. 2002;106:416–422. doi: 10.1161/01.cir.0000025242.79963.4c. [DOI] [PubMed] [Google Scholar]
- 79.McCullough PA, Sandberg KR. Sorting out the evidence on natriuretic peptides. Rev Cardiovasc Med. 2003;4(Suppl. 4):S13–S19. [PubMed] [Google Scholar]
- 80.Focaccio A, Volpe M, Ambrosio G, Lembo G, Pannain S, Rubattu S, Enea I, Pignalosa S, Chiariello M. Angiotensin II directly stimulates release of atrial natriuretic factor in isolated rabbit hearts. Circulation. 1993;87:192–198. doi: 10.1161/01.cir.87.1.192. [DOI] [PubMed] [Google Scholar]
- 81.Munagala VK, Burnett JC, Jr, Redfield MM. The natriuretic peptides in cardiovascular medicine. Curr Probl Cardiol. 2004;29:707–769. doi: 10.1016/j.cpcardiol.2004.07.002. [DOI] [PubMed] [Google Scholar]
- 82.Xu S, Venge P. Lipocalins as biochemical markers of disease. Biochim Biophys Acta. 2000;1482:298–307. doi: 10.1016/s0167-4838(00)00163-1. [DOI] [PubMed] [Google Scholar]
- 83.Mori K, Lee HT, Rapoport D, Drexler IR, Foster K, Yang J, Schmidt-Ott KM, Chen X, Li JY, Weiss S, Mishra J, Cheema FH, Markowitz G, Suganami T, Sawai K, Mukoyama M, Kunis C, D'Agati V, Devarajan P, Barasch J. Endocytic delivery of lipocalin–siderophore–iron complex rescues the kidney from ischemia–reperfusion injury. J Clin Invest. 2005;115:610–621. doi: 10.1172/JCI23056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Mishra J, Ma Q, Prada A, Mitsnefes M, Zahedi K, Yang J, Barasch J, Devarajan P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J Am Soc Nephrol. 2003;14:2534–2543. doi: 10.1097/01.asn.0000088027.54400.c6. [DOI] [PubMed] [Google Scholar]
- 85.Mishra J, Mori K, Ma Q, Kelly C, Barasch J, Devarajan P. Neutrophil gelatinase-associated lipocalin: a novel early urinary biomarker for cisplatin nephrotoxicity. Am J Nephrol. 2004;24:307–315. doi: 10.1159/000078452. [DOI] [PubMed] [Google Scholar]
- 86.Supavekin S, Zhang W, Kucherlapati R, Kaskel FJ, Moore LC, Devarajan P. Differential gene expression following early renal ischemia/reperfusion. Kidney Int. 2003;63:1714–1724. doi: 10.1046/j.1523-1755.2003.00928.x. [DOI] [PubMed] [Google Scholar]
- 87.Schmidt-Ott KM, Mori K, Kalandadze A, Li JY, Paragas N, Nicholas T, Devarajan P, Barasch J. Neutrophil gelatinase-associated lipocalin-mediated iron traffic in kidney epithelia. Curr Opin Nephrol Hypertens. 2006;15:442–449. doi: 10.1097/01.mnh.0000232886.81142.58. [DOI] [PubMed] [Google Scholar]
- 88.Mori K, Nakao K. Neutrophil gelatinase-associated lipocalin as the real-time indicator of active kidney damage. Kidney Int. 2007;71:967–970. doi: 10.1038/sj.ki.5002165. [DOI] [PubMed] [Google Scholar]
- 89.Herget-Rosenthal S, Marggraf G, Husing J, Goring F, Pietruck F, Janssen O, Philipp T, Kribben A. Early detection of acute renal failure by serum cystatin C. Kidney Int. 2004;66:1115–1122. doi: 10.1111/j.1523-1755.2004.00861.x. [DOI] [PubMed] [Google Scholar]
- 90.Herget-Rosenthal S, Poppen D, Husing J, Marggraf G, Pietruck F, Jakob HG, Philipp T, Kribben A. Prognostic value of tubular proteinuria and enzymuria in nonoliguric acute tubular necrosis. Clin Chem. 2004;50:552–558. doi: 10.1373/clinchem.2003.027763. [DOI] [PubMed] [Google Scholar]
- 91.Han WK, Bailly V, Abichandani R, Thadhani R, Bonventre JV. Kidney Injury Molecule-1 (KIM-1): a novel biomarker for human renal proximal tubule injury. Kidney Int. 2002;62:237–244. doi: 10.1046/j.1523-1755.2002.00433.x. [DOI] [PubMed] [Google Scholar]
- 92.Ichimura T, Hung CC, Yang SA, Stevens JL, Bonventre JV. Kidney injury molecule-1: a tissue and urinary biomarker for nephrotoxicant-induced renal injury. Am J Physiol Renal Physiol. 2004;286:F552–F563. doi: 10.1152/ajprenal.00285.2002. [DOI] [PubMed] [Google Scholar]
- 93.Vaidya VS, Ramirez V, Ichimura T, Bobadilla NA, Bonventre JV. Urinary kidney injury molecule-1: a sensitive quantitative biomarker for early detection of kidney tubular injury. Am J Physiol Renal Physiol. 2006;290:F517–F529. doi: 10.1152/ajprenal.00291.2005. [DOI] [PubMed] [Google Scholar]
- 94.Liangos O, Perianayagam MC, Vaidya VS, Han WK, Wald R, Tighiouart H, MacKinnon RW, Li L, Balakrishnan VS, Pereira BJ, Bonventre JV, Jaber BL. Urinay NAG activity and KIM-1 level are associated with adverse outcomes in acute renal failure. J Am Soc Nephrol. 2007;18:904–912. doi: 10.1681/ASN.2006030221. [DOI] [PubMed] [Google Scholar]
- 95.Bazzi C, Petrini C, Rizza V, Arrigo G, Napodano P, Paparella M, D'Amico G. Urinary N-acetyl-beta-glucosaminidase excretion is a marker of tubular cell dysfunction and a predictor of outcome in primary glomerulonephritis. Nephrol Dial Transplant. 2002;17:1890–1896. doi: 10.1093/ndt/17.11.1890. [DOI] [PubMed] [Google Scholar]
- 96.Wellwood JM, Ellis BG, Price RG, Hammond K, Thompson AE, Jones NF. Urinary N-acetyl- beta-d-glucosaminidase activities in patients with renal disease. Br Med J. 1975;3:408–411. doi: 10.1136/bmj.3.5980.408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Uslu S, Efe B, Alatas O, Kebapci N, Colak O, Demirustu C, Yoruk A. Serum cystatin C and urinary enzymes as screening markers of renal dysfunction in diabetic patients. J Nephrol. 2005;18:559–567. [PubMed] [Google Scholar]
- 98.Harmankaya O, Ozturk Y, Basturk T, Obek A. Urinary excretion of N-acetyl-beta-d-glucosaminidase in newly diagnosed essential hypertensive patients and its changes with effective antihypertensive therapy. Int Urol Nephrol. 2001;32:583–584. doi: 10.1023/a:1014443217611. [DOI] [PubMed] [Google Scholar]
- 99.Matsushima H YH, Machiguchi T, Muso E, Matusyama E, Tamura T, Sasayama S. Urinary albumin and TGF 1 levels as renal damage indices in patients with congestive heart failure. Clin Exp Nephrol. 2002;6:9. [Google Scholar]
- 100.Melnikov VY, Ecder T, Fantuzzi G, Siegmund B, Lucia MS, Dinarello CA, Schrier RW, Edelstein CL. Impaired IL-18 processing protects caspase-1-deficient mice from ischemic acute renal failure. J Clin Invest. 2001;107:1145–1152. doi: 10.1172/JCI12089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Parikh CR, Jani A, Melnikov VY, Faubel S, Edelstein CL. Urinary interleukin-18 is a marker of human acute tubular necrosis. Am J Kidney Dis. 2004;43:405–414. doi: 10.1053/j.ajkd.2003.10.040. [DOI] [PubMed] [Google Scholar]
- 102.Parikh CR, Abraham E, Ancukiewicz M, Edelstein CL. Urine IL-18 is an early diagnostic marker for acute kidney injury and predicts mortality in the intensive care unit. J Am Soc Nephrol. 2005;16:3046–3052. doi: 10.1681/ASN.2005030236. [DOI] [PubMed] [Google Scholar]
- 103.Parikh CR, Jani A, Mishra J, Ma Q, Kelly C, Barasch J, Edelstein CL, Devarajan P. Urine NGAL and IL-18 are predictive biomarkers for delayed graft function following kidney transplantation. Am J Transplant. 2006;6:1639–1645. doi: 10.1111/j.1600-6143.2006.01352.x. [DOI] [PubMed] [Google Scholar]
- 104.Damman K, van Deursen VM, Navis G, Voors AA, van Veldhuisen DJ, Hillege HL. Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. J Am Coll Cardiol. 2009;53:582–588. doi: 10.1016/j.jacc.2008.08.080. [DOI] [PubMed] [Google Scholar]
- 105.Ronco C, Haapio M, House AA, Anavekar N, Bellomo R. Cardiorenal syndrome. J Am Coll Cardiol. 2008;52:1527–1539. doi: 10.1016/j.jacc.2008.07.051. [DOI] [PubMed] [Google Scholar]
- 106.Hunt SA. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure) J Am Coll Cardiol. 2005;46:e1–e82. doi: 10.1016/j.jacc.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 107.Boerrigter GC-BL, Abraham WT, St. John Sutton MG, Heublein D, Kruger KM, Hill MR, McCullough PA, Burnett JC. Cardiac resynchronization therapy with biventricular pacing improves renal function in heart failure patients with reduced glomerular filtration rate. Circulation. 2007;116:II_405. [Google Scholar]
- 108.Kelly KJ. Distant effects of experimental renal ischemia/reperfusion injury. J Am Soc Nephrol. 2003;14:1549–1558. doi: 10.1097/01.asn.0000064946.94590.46. [DOI] [PubMed] [Google Scholar]
- 109.McCullough PA. Acute kidney injury with iodinated contrast. Crit Care Med. 2008;36(Suppl. 4):S204–S211. doi: 10.1097/CCM.0b013e318168cdc3. [DOI] [PubMed] [Google Scholar]
- 110.McCullough PA, Wolyn R, Rocher LL, Levin RN, O'Neill WW. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997;103:368–375. doi: 10.1016/s0002-9343(97)00150-2. [DOI] [PubMed] [Google Scholar]
- 111.McCullough PA. Cardiovascular disease in chronic kidney disease from a cardiologist's perspective. Curr Opin Nephrol Hypertens. 2004;13:591–600. doi: 10.1097/00041552-200411000-00003. [DOI] [PubMed] [Google Scholar]
- 112.Dickstein K, Cohen-Solal A, Filippatos G, McMurray JJ, Ponikowski P, Poole-Wilson PA, Stromberg A, van Veldhuisen DJ, Atar D, Hoes AW, Keren A, Mebazaa A, Nieminen M, Priori SG, Swedberg K, Vahanian A, Camm J, De Caterina R, Dean V, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Auricchio A, Bax J, Bohm M, Corra U, della Bella P, Elliott PM, Follath F, Gheorghiade M, Hasin Y, Hernborg A, Jaarsma T, Komajda M, Kornowski R, Piepoli M, Prendergast B, Tavazzi L, Vachiery JL, Verheugt FW, Zannad F. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM) Eur J Heart Fail. 2008;10:933–989. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 113.Taal M, Tomson C. Clinical practice guidelines. Module 1. Chronic kidney disease. http://www.renal.org/pages/pages/guidelines/current/ckd.php . Published online ahead of print 7 August 2009.
- 114.Cassidy M, Richardson D, Jones C. Clinical practice guidelines. Module 2. Complications. http://www.renal.org/pages/pages/guidelines/current/complications.php . Published online ahead of print 7 August 2009.
- 115.Hollenberg SM. Vasodilators in acute heart failure. Heart Fail Rev. 2007;12:143–147. doi: 10.1007/s10741-007-9017-2. [DOI] [PubMed] [Google Scholar]
- 116.Sackner-Bernstein JD, Skopicki HA, Aaronson KD. Risk of worsening renal function with nesiritide in patients with acutely decompensated heart failure. Circulation. 2005;111:1487–1491. doi: 10.1161/01.CIR.0000159340.93220.E4. [DOI] [PubMed] [Google Scholar]
- 117.Owan TE, Chen HH, Frantz RP, Karon BL, Miller WL, Rodeheffer RJ, Hodge DO, Burnett JC, Jr, Redfield MM. The effects of nesiritide on renal function and diuretic responsiveness in acutely decompensated heart failure patients with renal dysfunction. J Card Fail. 2008;14:267–275. doi: 10.1016/j.cardfail.2007.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ho JE, Teerlink JR. Role of tolvaptan in acute decompensated heart failure. Expert Rev Cardiovasc Ther. 2008;6:601–608. doi: 10.1586/14779072.6.5.601. [DOI] [PubMed] [Google Scholar]
- 119.Zannad F, Mebazaa A, Juilliere Y, Cohen-Solal A, Guize L, Alla F, Rouge P, Blin P, Barlet MH, Paolozzi L, Vincent C, Desnos M, Samii K. Clinical profile, contemporary management and one-year mortality in patients with severe acute heart failure syndromes: The EFICA study. Eur J Heart Fail. 2006;8:697–705. doi: 10.1016/j.ejheart.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 120.Tatsumi E, Nakatani T, Imachi K, Umezu M, Kyo SE, Sase K, Takatani S, Matsuda H. Domestic and foreign trends in the prevalence of heart failure and the necessity of next-generation artificial hearts: a survey by the Working Group on Establishment of Assessment Guidelines for Next-Generation Artificial Heart Systems. J Artif Organs. 2007;10:187–194. doi: 10.1007/s10047-007-0384-1. [DOI] [PubMed] [Google Scholar]
- 121.The SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 122.Bangalore S, Messerli FH, Kostis JB, Pepine CJ. Cardiovascular protection using beta-blockers: a critical review of the evidence. J Am Coll Cardiol. 2007;50:563–572. doi: 10.1016/j.jacc.2007.04.060. [DOI] [PubMed] [Google Scholar]
- 123.Pfeffer MA, Swedberg K, Granger CB, Held P, McMurray JJ, Michelson EL, Olofsson B, Ostergren J, Yusuf S, Pocock S. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet. 2003;362:759–766. doi: 10.1016/s0140-6736(03)14282-1. [DOI] [PubMed] [Google Scholar]
- 124.Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N Engl J Med. 1999;341:709–717. doi: 10.1056/NEJM199909023411001. [DOI] [PubMed] [Google Scholar]
- 125.Hasselblad V, Gattis Stough W, Shah MR, Lokhnygina Y, O'Connor CM, Califf RM, Adams KF., Jr Relation between dose of loop diuretics and outcomes in a heart failure population: results of the ESCAPE trial. Eur J Heart Fail. 2007;9:1064–1069. doi: 10.1016/j.ejheart.2007.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Jasuja D, Mor MK, Hartwig KC, Palevsky PM, Fine MJ, Weisbord SD. Provider knowledge of contrast-induced acute kidney injury. Am J Med Sci. 2009;338:280–286. doi: 10.1097/MAJ.0b013e3181a87e21. [DOI] [PubMed] [Google Scholar]
- 127.Palevsky PM. Defining contrast-induced nephropathy. Clin J Am Soc Nephrol. 2009;4:1151–1153. doi: 10.2215/CJN.03410509. [DOI] [PubMed] [Google Scholar]
- 128.Solomon RJ, Mehran R, Natarajan MK, Doucet S, Katholi RE, Staniloae CS, Sharma SK, Labinaz M, Gelormini JL, Barrett BJ. Contrast-induced nephropathy and long-term adverse events: cause and effect? Clin J Am Soc Nephrol. 2009;4:1162–1169. doi: 10.2215/CJN.00550109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Mentzer RM, Jr, Oz MC, Sladen RN, Graeve AH, Hebeler RF, Jr, Luber JM, Jr, et al. Effects of perioperative nesiritide in patients with left ventricular dysfunction undergoing cardiac surgery:the NAPA Trial. J Am Coll Cardiol. 2007;49:716–726. doi: 10.1016/j.jacc.2006.10.048. [DOI] [PubMed] [Google Scholar]
- 130.Gowdak LH, Arantes RL, de Paula FJ, Krieger EM, De Lima JJ. Underuse of American College of Cardiology/American Heart Association Guidelines in hemodialysis patients. Ren Fail. 2007;29:559–565. doi: 10.1080/08860220701395002. [DOI] [PubMed] [Google Scholar]
- 131.Davenport A, Cox C, Thuraisingham R. Achieving blood pressure targets during dialysis improves control but increases intradialytic hypotension. Kidney Int. 2008;73:759–764. doi: 10.1038/sj.ki.5002745. [DOI] [PubMed] [Google Scholar]
- 132.Davenport A, Cox C, Thuraisingham R. The importance of dialysate sodium concentration in determining interdialytic weight gains in chronic hemodialysis patients: the PanThames Renal Audit. Int J Artif Organs. 2008;31:411–417. doi: 10.1177/039139880803100506. [DOI] [PubMed] [Google Scholar]