Abstract
Background
Children with Autistic Disorder (AD) evidence more co-occurring maladaptive behaviours than their typically developing peers and peers with intellectual disability because of other aetiologies. The present study investigated the prevalence of Clinically Significant maladaptive behaviours during early childhood and identified at-risk subgroups of young children with AD.
Method
Parents rated their child’s maladaptive behaviours on the Child Behaviour Checklist (CBCL) in 169 children with AD aged 1.5 to 5.8 years.
Results
One-third of young children with AD had a CBCL Total Problems score in the Clinically Significant range. The highest percentage of Clinically Significant scores were in the Withdrawal, Attention, and Aggression CBCL syndrome scales. There was a high degree of co-morbidity of Clinically Significant maladaptive behaviours. Several subject characteristic risk factors for maladaptive behaviours were identified.
Conclusions
Findings highlight the need to include behavioural management strategies aimed at increasing social engagement, sustained attention and decreasing aggressive behaviour in comprehensive intervention programmes for young children with AD.
Keywords: Keywords autism, autistic disorder, behaviour problems, children, child behaviour checklist, maladaptive behaviour
Introduction
Autistic Disorder (AD), the most common and severe autism spectrum disorder (ASD), is defined by a triad of impairments in communication, social reciprocity, and repetitive/restricted interests and behaviours (American Psychiatric Association 2000). Children with AD often exhibit maladaptive behaviours, defined as co-occurring internalising (e.g. emotionally reactive, depressed/anxious affect, somatic complaints and withdrawal) and externalising (e.g. aggression, defiance and inattentive) behaviour problems that negatively impact everyday activities (Bradley et al. 2004; Eisenhower et al. 2005; Brereton et al. 2006). Maladaptive behaviours often cause more distress to caregivers than the core autistic symptoms (Hastings et al. 2005; Lecavalier et al. 2006). Maladaptive behaviours can also interfere with intervention efforts and thereby impact the long-term prognosis of children with AD(e.g. Horner et al. 1992). Maladaptive behaviours during early childhood (≤5 years-old) are of particular concern given that these are critical years for intervention (Harris & Handleman 2000; National Research Council 2001; Stone & Yoder 2001).
Previous researchers have investigated maladaptive behaviours in young children with AD (≤5 years-old) by comparing mean frequency or severity scores on behaviour measures of children with ASD and comparison groups (e.g. Gadow et al. 2004, 2005; Eisenhower et al. 2005; Weisbrot et al. 2005; Herring et al. 2006). Children aged 3 to 5 years with ASD exhibit more frequent or severe internalising behaviours, including obsessions, compulsions, anxiety, and emotional reactivity, and externalising behaviours, including inattention and tics, than children with intellectual disability (ID) give to other aetiologies and non-ASD clinic and community samples of children with average intelligence (Gadow et al. 2004, 2005; Eisenhower et al. 2005; Weisbrot et al. 2005). Several studies suggest a high prevalence of aggressive behaviour in children with ASD aged 3 to 5 years (Green et al. 2000; Horner et al. 2002), although at least one study indicates that children with ASD may not display a higher frequency of aggressive behaviour than their typically developing peers (Gadow et al. 2004).
Few studies have examined the prevalence of maladaptive behaviours that occur at a Clinically Significant level (i.e. markedly impacts daily functioning and merits clinical attention), or maladaptive behaviours that warrant a clinical diagnosis, in young children with ASD. Eisenhower et al. (2005) found that 46.2% of a sample of 14 children with ASD aged 3 to 5 years had a Child Behaviour Checklist (CBCL; Achenbach & Rescorla 2000) Total Problems score in the Borderline Clinical or Clinical range. Using the Early Childhood Inventory, fourth Edition (Gadow & Sprafkin 1997 2000), Gadow et al. (2004) found that 36.1% and 42.9% of boys and girls with ASD, respectively, aged 3 to 5 years scored above the Symptom Criterion (i.e. the minimum symptoms necessary for a DSM-IV diagnosis) for Attention-Deficit/Hyperactivity Disorder. In contrast, 5% to 19% scored about the Symptom Criterion for various anxiety disorders and less than 2% scored above the Symptom Criterion for Oppositional Defiant Disorder. Researchers have not examined the co-morbidity, or the extent to which young children with AD exhibit multiple maladaptive behaviours at a Clinically Significant level.
Conclusions from these previous studies (Green et al. 2000; Horner et al. 2002; Gadow et al. 2004, 2005; Eisenhower et al. 2005; Herring et al. 2006; Weisbrot et al. 2005) are limited by the inclusion of young children within the broader ASD continuum. In older children and adults with ASD, individuals with Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS) and Asperger’s Disorder exhibit a lower frequency or severity of maladaptive behaviours than individuals with AD (e.g. Kurita 1991; Ehlers et al. 1997; Gadow et al. 2004; Weisbrot et al. 2005). Differences in maladaptive behaviours among ASD diagnosis may also occur in early childhood. Studies involving the broader ASD population may merely reflect the average of discrepant profiles of maladaptive behaviours. Research using clearly defined samples of young children with specific ASD diagnoses is arguably warranted to fully understand the prevalence of maladaptive behaviours.
Moreover, an investigation of the subject characteristic correlates of maladaptive behaviours in young children with AD is needed to identify at-risk subgroups. In older children and adults with ASD, cognitive functioning and adaptive behaviour are important predictors of maladaptive behaviours. Individuals with ASD with low cognitive functioning and adaptive behaviour exhibit more maladaptive behaviours than high functioning individuals (de Bildt et al. 2005; Dominick et al. 2007; Shattuck et al. 2007). Expressive language is negatively correlated with maladaptive behaviours in older children with ASD as well as children within the broader developmental disability population (e.g. Durand 1993; Howlin et al. 2004; Dominick et al. 2007; Shattuck et al. 2007). Severity of autistic behaviours has also been shown to be positively associated with maladaptive behaviours in older children with ASD (Dominick et al. 2007).
Discrepant findings have been reported for the association between gender and maladaptive behaviour in older children and adults with ASD. While several studies report no gender differences in maladaptive behaviours (Howlin et al. 2004; Shattuck et al. 2007), girls with ASD have been shown to exhibit a slightly higher frequency or severity of a few maladaptive behaviours (Nyden et al. 2000; Gadow et al. 2004; Holtmann et al. 2005). Age is an important subject characteristic correlate of maladaptive behaviour in the ASD population, with findings of a decline in maladaptive behaviours from childhood to adulthood (Tonge & Einfeld 2000; Shattuck et al. 2007). A previous study suggests that age-related changes in maladaptive behaviours also occur during early childhood. Similar to their typically developing peers (e.g. Van der Valk et al. 2003; Frigerio et al. 2004), a decrease in externalising maladaptive behaviours and a trend towards an increase in internalising maladaptive behaviours was found from age 3 to 5 years in children with ASD (Eisenhower et al. 2005). Few studies have examined the association between ethnicity and maladaptive behaviour in an AD or ASD population.
The purpose of this study is to identify: (1) the prevalence of Clinically Significant maladaptive behaviours; and (2) subject characteristic risk factors for maladaptive behaviours through parentreport on the CBCL of 169 children diagnosed with AD aged 1.5 to 5.9 years. Based on previous studies of children with ASD, young children with AD were hypothesised to have a relatively high prevalence of Clinically Significant sleep problems and inattention, and a relatively low prevalence of Clinically Significant anxiety and aggressive behaviour. Cognitive functioning, adaptive behaviour, and expressive language were expected to be negatively correlated with maladaptive behaviours. Severity of autistic symptoms was predicted to be positively correlated with maladaptive behaviours. Girls with AD were expected to have more maladaptive behaviours than boys, although gender differences were predicted to be limited. Externalising maladaptive behaviours were hypothesised to decrease and internalising behaviours were expected to increase with age.
Method
Participants
Six hundred and five children aged 1.5 to 5.8 years were referred to an interdisciplinary autism clinic in the northwest region of the United States by their primary medical care provider between August 2003 and January 2007. Two hundred and thirtyfour children (38.7%) were diagnosed with AD based on criteria in the DSM-IV TR. In the International Classification of Diseases, 10th Edition (ICD-10; World Health Organization 1993) comparable criteria are listed for Childhood Autism. The present study is based on the 169 children with AD for whom complete data were obtained. For the remaining 65 children, parents either did not have time or chose not to complete the CBCL during the evaluation period; previous testing was done elsewhere, or an alternative measure of maladaptive behaviour or cognitive functioning was administered. A one-way multivariate analysis of variance (manova) was conducted to compare the subject characteristics of 169 children included in the study and the 65 children not included. The following subject characteristics were included in the manova: age (years), gender (0 = male, 1 = female), ethnicity (0 = Caucasian, 1 = non-Caucasian), non-verbal cognitive functioning (Mullen Scales of Early Learning Visual Reception age equivalency/chronological age), expressive language (Mullen Scales of Early Learning Expressive Language age equivalency/chronological age), severity of autistic behaviours [Autism Diagnostic Observation Schedule, Generic (ADOS-G) Combined score], and adaptive behaviour [Vineland Adaptive Behaviour Composite (ABC) score]. There was not a significant difference in subject characteristics between the 169 children included in the present study and the 65 children with incomplete data (Wilks’ Lambda = 0.97, F1,233 = 0.71, P = 0.64). Parents who completed the CBCL were predominately mothers. Given the de-identified nature of the dataset, a waiver of consent was obtained from the university Internal Review Board. Table 1 displays the subject characteristics of the participants.
Table 1.
Participant subject characteristics
| n = 169 | |
|---|---|
| Age in years (mean, SD) | 3.51 (0.86) |
| Sex (n) | |
| Male | 132 |
| Female | 38 |
| Ethnicity (n) | |
| Caucasian | 98 |
| African-American | 6 |
| Hispanic | 14 |
| Asian/Pacific Islander | 9 |
| Other | 13 |
| Not reported | 30 |
| MSEL Visual Reception AE (mean, SD) | 1.89 (0.78) |
| MSEL Expressive Language AE (mean, SD) | 1.39 (0.80) |
| Vineland ABC (mean, SD) | 60.44 (7.45) |
MSEL AE (Age-Equivalencies) are in months. Participants for whom parents did not report ethnicity were not included in analyses involving ethnicity.
ABC, Adaptive Behaviour Composite; MSEL, Mullen Scales of Early Learning.
Measures
Autistic Disorder
AD diagnosis was based on multidisciplinary (i.e. Occupational Therapist, Speech-Language Pathologist, Psychologist, and Developmental Paediatrician) team consensus. The ADOS-G (Lord et al. 2000) is a standardised, play-based assessment of communication, social interaction, play, and imaginary use of materials, was administered to all children. The ADOS-G has four modules based on expressive language ability (Lord et al. 2000). Scoring of the ADOS-G involves diagnostic algorithms for four domains: Communication, Social Interaction, Play/Creativity, and Restricted/Repetitive Behaviours or Interests. Cut-off scores in the domains of Communication, Social Interaction, and Combined (Communication + Social Interaction), allow a child to be placed in a(n) Autism, ASD or Non-spectrum category. The authors report good to excellent reliability of the items, domains, and classification categories and satisfactory ability to differentiate children with autism from children not on the autism spectrum (Lord et al. 2000). All participants diagnosed with AD in the present study had an ADOS-G Combined score at or above the cut-off for the Autism category.
A semi-structured diagnostic interview of the 12 DSM-IV-TR criteria for AD was completed with parents. Interviews were conducted by a Developmental Paediatrician or Psychologist, who determined whether each criterion was met or unmet based on parent responses. Children diagnosed with AD met DSM-IV-TR criteria for a diagnosis of AD based on this interview, including at least six out of the 12 criteria and onset of symptoms prior to 3 years of age.
Adaptive Behaviour
The Vineland Adaptive Behaviour Scales, Survey Interview Form (Sparrow et al. 2005) is a semistructured caregiver interview of a child’s personal and social everyday living skills. Open-ended questions are used to determine if the child ‘usually’, ‘sometimes or partially’, or ‘never’ performs various behaviours within the domains of: Communication, Daily Living Skills, Socialisation Skills and Motor Skills. These domains are combined to form the ABC score, which is a standard score (M = 100, SD = 15). The Vineland ABC score has satisfactory reliability and concurrent validity (Sparrow et al. 2005).
Developmental Functioning
The Mullen Scales of Early Learning (MSEL; Mullen 1995) is a standardised measure of cognitive, motor, and language development for infants and children up to 68 months of age. The Visual Reception scale assesses visual perceptual ability including visual discrimination and visual memory. The Expressive Language scale assesses spontaneous language, specific verbal responses to questions and concept formation. Satisfactory reliability and strong concurrent validity with the Bayley Scales of Infant Development and the Preschool Language Assessment have been reported for the MSEL (Mullen 1995). In previous studies of children with ASD (Akshoomoff 2006; Fidler et al. 2006; Carter et al. 2007), MSEL age-equivalent scores were used to assess non-verbal and language functioning because of the insensitivity of standard scores among lower functioning children. To remain consistent with this approach, the MSEL Visual Reception age-equivalency score was used to measure non-verbal cognitive ability. The MSEL Expressive Language age-equivalency was used to measure expressive language ability.
Maladaptive Behaviour
The CBCL, for ages 1.5 through 5 years, is a caregiver-completed paper and pencil measure of maladaptive behaviour. The CBCL consists of 99 items that address specific internalising and externalising problematic behaviours and one item in which caregivers can write in up to three additional problematic behaviours. Caregivers are asked to rate the frequency of each behaviour on a three-point Likert scale (0 = Not True, 1 = Somewhat or Sometimes True, 2 = Very True or Often True). Scores are summed to form seven syndrome scales (Emotionally Reactive, Anxious/Depressed, Somatic Complaints, Withdrawn, Sleep Problems, Attention Problems and Aggressive Behaviour) which were analysed in the present study. The Emotionally Reactive, Anxious/Depression, Somatic Complaints, and Withdrawn scales combine to yield the Internalising Problems composite score. The Attention Problems and Aggressive Behaviour scales combine to yield the Externalising Problems composite score. The syndrome scales, as well as 32 items inquiring about additional problematic behaviours, and the one item for which caregivers can write in other behaviour problems are combined to form the Total Problems composite score. The seven syndrome scales and three composite scores are converted to T-scores (M = 50, SD = 10). A T-score of 70 and above (at least two standard deviations above the mean for the general population) is generally considered to be Clinically Significant, and was used as the criterion for Clinical Significance in the present study. The manual for the CBCL reports adequate reliability and validity for scale scores (Achenbach & Rescorla 2000).
Procedure
Children were individually administered the MSEL and ADOS-G by licensed professionals. The ADOS-G was administered and scored by two professionals; at least one professional had reached clinical reliability standards (Lord et al. 2000). A Developmental Paediatrician or Psychologist conducted the diagnostic clinical interview of DSM-IV TR criteria for AD and conducted an interview to complete the Vineland with parents. Parents were asked to complete the CBCL. In all, the procedure took 2 to 3 h.
Results
Data Analysis Plan
Descriptive data were used to identify the percentage of young children with AD with Clinically Significant CBCL composite or syndrome scale scores and the co-morbidity of these scores. In order to identify subject characteristic risk factors for maladaptive behaviours, correlations were first conducted between the CBCL Externalising Problems and Internalising Problems composite scores and subject characteristics. To further assess the strength of these correlations, step-wise regressions were conducted using CBCL Externalising and Internalising Problems scores as the dependent variable and relevant subject characteristics as the predictor variables. Correlations were also conducted between the CBCL syndrome scale scores and subject characteristics. A follow-up one-way MANOVA was conducted to identify differences in the relevant CBCL syndrome scales among the ethnic categories.
Prevalence of Clinically Significant Maladaptive Behaviours
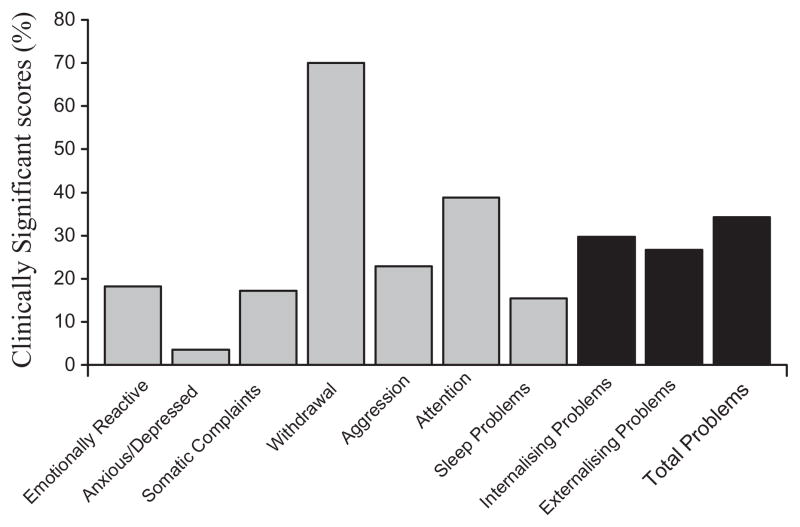
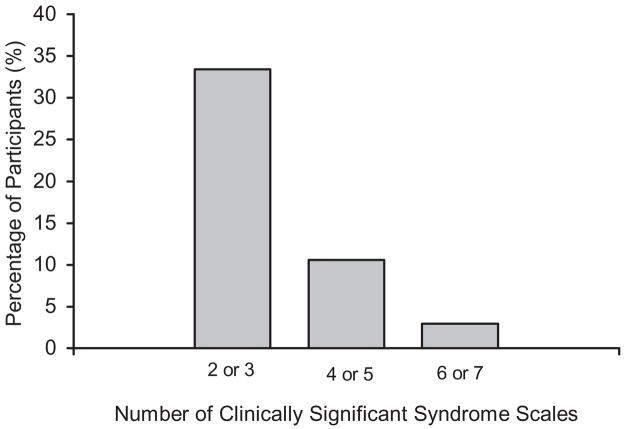
Fig. 1 displays the percentage of young children with AD rated by their parents to have Clinically Significant CBCL composite or syndrome scale score. For the CBCL composite scores, 29.6% of young children with AD had a Clinically Significant Internalising Problems and 27.2% had a Clinically Significant Externalising Problems (27.2%) composite score. One-third (34.3%) of young children with AD had a Total Problems score in the Clinically Significant range. The large majority of participants (81.7%) had at least one CBCL syndrome scale score in the Clinically Significant range. The CBCL syndrome scales with the highest percentage of Clinically Significant scores were Withdrawn (70.4%), Attention (38.5%) and Aggression (22.5%). In contrast, 18.2% of young children with AD had a Clinically Significant Emotionally Reactive score and 17.2% had a Clinically Significant Somatic Complaints syndrome score. The CBCL Anxious/Depressed (3.6%) and Sleep Problems (15.4%) syndrome scales had the lowest prevalence of Clinically Significant scores. Fig. 2 presents the co-morbidity of Clinically Significant CBCL syndrome scale scores. Overall, 46.8% of young children with AD had more than one CBCL syndrome scale in the Clinically Significant range. Specifically, 33.4% had two or three CBCL syndrome scale scores in the Clinically Significant range, 10.5% had four or five CBCL syndrome scale scores in the Clinically Significant range and 2.9% had six or seven CBCL syndrome scale scores in the Clinically Significant range.
Figure 1.
Percentage of young children with Autistic Disorder with a Clinically Significant Child Behaviour Checklist Composite or syndrome scale score.
Figure 2.
Number of Clinically Significant Child Behaviour Checklist syndrome scales exhibited by young children with Autistic Disorder.
Subject Characteristic Correlates
Correlations were conducted between the CBCL Externalising Problems and Internalising Problems composite and syndrome scale scores (T-scores) and subject characteristics [gender (0 = male, 1 = female), age (years), ethnicity (0 = Caucasian, 1 = non-Caucasian), non-verbal cognitive functioning (MSEL Visual Reception age equivalency/chronological age), expressive language (MSEL Expressive Language age equivalency/chronological age), severity of autistic behaviours (ADOS-G Combined score) and adaptive behaviour (Vineland ABC Composite score)]. Table 2 presents the results of the correlations. The CBCL Externalising Problems composite score was significantly negatively correlated with non-verbal cognitive functioning, expressive language and adaptive behaviour. There was not a significant correlation between the CBCL Externalising Problems composite score and age, gender, ethnicity or severity of autistic behaviours. The CBCL Internalising Problems composite score was significantly positively correlated with age and significantly negatively correlated with expressive language, non-verbal cognitive functioning and adaptive behaviour. There was not a significant correlation between the CBCL Internalising Problems composite score and gender, ethnicity or severity of autistic behaviours.
Table 2.
Correlations among Subject Characteristics and Child Behaviour Checklist Composite and Syndrome Scales
| Gender | Age | Ethnicity | MSEL Visual Reception | MSEL Expressive Language | Severity of Autistic | Vineland ABC | |
|---|---|---|---|---|---|---|---|
| Externalising problems | −0.11 | 0.10 | 0.14 | −0.32** | −0.21** | −0.13 | −0.16* |
| Attention problems | −0.03 | 0.11 | 0.17* | −0.31** | −0.26** | −0.06 | −0.20** |
| Aggressive behaviour | −0.11 | 0.03 | 0.05 | −0.32** | −0.19* | −0.11 | −0.19* |
| Internalising problems | −0.13 | 0.16* | 0.16 | −0.17* | −0.21* | 0.01 | −0.29** |
| Emotionally reactive | −0.19* | 0.05 | 0.13 | −0.14 | −0.20* | −0.06 | −0.15 |
| Anxious/Depressed | −0.14 | 0.12 | 0.21** | −0.20* | −0.23** | −0.01 | −0.25** |
| Somatic complaints | −0.10 | 0.25** | −0.03 | −0.05 | −0.10 | −0.10 | −0.24** |
| Withdrawal | −0.05 | 0.17* | 0.16* | −0.12 | −0.15 | −0.11 | −0.34** |
| Sleep problems | −0.24* | 0.02 | 0.22** | −0.05 | −0.07 | −0.02 | −0.09 |
P < 0.05,
P < 0.01.
ABC, Adaptive Behaviour Composite; MSEL, Mullen Scales of Early Learning.
Step-wise regressions were conducted to further assess the strength of these correlations. Using the outcome of CBCL Externalising Problems, three predictors were entered into the analysis in the following order: non-verbal cognitive functioning, expressive language and adaptive behaviour. Nonverbal cognitive functioning emerged as the strongest predictor of CBCL Externalising Problems, accounting for 10% of the variance (F1,168 = 19.32, P < 0.01). Using the outcome of CBCL Internalising Problems, four predictors were entered into the analysis in the following order: adaptive behaviour, expressive language, non-verbal cognitive functioning and age. Adaptive behaviour emerged as the strongest predictor of the CBCL Internalising Problems, accounting for 8% of the variance (F1,168 = 15.21, P < 0.01).
Gender was significantly correlated with the CBCL Sleep Problems and Emotionally Reactive syndrome scales, such that boys with AD had higher scores than girls. Age was significantly positively correlated with the CBCL Somatic Complaints and Withdrawal syndrome scales. Non-verbal cognitive functioning was significantly negatively correlated with the CBCL Attention, Aggression, and Anxious/Depressed syndrome scales. Expressive Language was significantly negatively correlated with the CBCL Attention, Aggression, Emotionally Reactive, and Anxious/Depressed syndrome scales. Severity of autistic behaviours was not significantly correlated with any of the CBCL syndrome scales. Adaptive behaviour was significantly negatively correlated with the CBCL Attention, Aggression, Emotionally Reactive, Anxious/Depressed, Somatic Complaints and Withdrawal syndrome scales.
Ethnicity was significantly correlated with the CBCL Attention, Anxious/Depressed, Withdrawal, and Sleep Problems syndrome scale such that non-Caucasian children with AD had higher scores than Caucasian children. To further investigate this finding, a one-way MANOVA was conducted to identify differences among the five ethnicity categories (Caucasian, African-American, Hispanic, Asian/Pacific Islander and Other) in the relevant CBCL syndrome scales. There was not a significant difference in the CBCL syndrome scales by ethnic category (Wilks’ Lambda = 0.96, F4,135 = 1.40, P = 0.24), likely because of the small number of participants within each category and small effect size of ethnicity.
Discussion
Children with AD exhibit more maladaptive behaviours than their typically developing peers and peers with ID because of other aetiologies (Bradley et al. 2004; Brereton et al. 2006). These maladaptive behaviours are distressing to caregivers and can interfere with intervention services (Hastings et al. 2005; Lecavalier et al. 2006). Little is known about the prevalence of maladaptive behaviours during early childhood (≤5 years), which is a critical period for intervention efforts (Harris & Handleman 2000; Stone & Yoder 2001). In this study, we examined the prevalence of parent-rated Clinically Significant maladaptive behaviours in a large and well-defined sample of young children (≤5 years-old) with AD. We also identified subject characteristic correlates of maladaptive behaviours.
One-third of young children with AD had a CBCL Total Problems score in the Clinically Significant range, indicating the presence of maladaptive behaviours at a level that markedly impacts daily functioning and thus is likely to interfere with early learning activities. More than two-thirds of young children with AD were rated as exhibiting a Clinically Significant level of withdrawal behaviour. Impairment in social relatedness is a core feature of AD, and thus it is not surprising that the majority of young children with AD were reported to have difficulty engaging with others. A similar prevalence of withdrawal behaviour has been reported for older children with ASD (Bolte et al. 1999). Clinically Significant levels of attention problems were reported for 38.5% of young children with AD, which is consistent with past reports of a high prevalence of inattention in younger children with ASD (e.g. Gadow et al. 2004, 2005); Weisbrot et al. 2004). In support of previous findings, aggressive behaviour was common among young children with AD (e.g. Green et al. 2000; Horner et al. 2002), with 22.5% of children exhibiting Clinically Significant problems with aggression. Overall, the greatest behavioural obstacles for successful early intervention services appear to be getting young children with AD to engage with providers, ensuring that they sustain attention during activities, and managing aggressive behaviour.
In the present study, there was a relatively low prevalence of Clinically Significant anxious or depressed mood. This finding is consistent with findings from a previous study (Gadow et al. 2004) suggesting that difficulties with affect regulation are not common during early childhood in ASD. There was a high rate of co-morbidity of maladaptive behaviours in the present study. One-third (33.4%) of young children with AD were rated as having two to three Clinically Significant maladaptive behaviours and 13.4% were rated as having four or more Clinically Significant maladaptive behaviours. This finding suggests that behaviour management strategies included in early intervention programmes should be designed to address numerous internalising and externalising maladaptive behaviours, as children with AD are likely to demonstrate more than one problem behaviour.
Several subject characteristic correlates of maladaptive behaviours were identified in the present study. The strongest predictor of overall externalising maladaptive behaviour was non-verbal cognitive ability and the strongest predictor of overall internalising maladaptive behaviour was adaptive behaviour. This finding is consistent with research in older children and adults with ASD (e.g. de Bildt et al. 2005; Shattuck et al. 2007), and indicates that across the lifespan, individuals with low cognitive ability and adaptive behaviour are at a greater risk for maladaptive behaviours than high functioning individuals. In the present study, non-verbal cognitive ability and adaptive behaviour accounted for 8% to 10% of the variance in internalising and externalising behaviours, respectively, suggesting that these subject characteristics have important but limited predictive value in early childhood.
Low expressive language was a risk factor for inattention as well as several internalising maladaptive behaviours in this study. This finding supports research of individuals with developmental disabilities, and indicates that maladaptive behaviours may often be inappropriate attempts to communicate needs (e.g. Durand, 1993; Day & Horner 1994). Functional communication training aimed at teaching young children with AD appropriate ways to communicate their needs may lead to declines in maladaptive behaviours. In contradiction to our hypothesis and past research of children with ASD (Dominick et al. 2007), severity of autistic behaviours was not predictive of maladaptive behaviours. Severity of autistic behaviours may be an important risk factor for maladaptive behaviours when considering an ASD population, given the large variation in the presentation of autistic behaviours. However, severity of autistic behaviours may not be a key risk factor for maladaptive behaviours when more defined population of young children with AD is considered.
Gender was largely unrelated to maladaptive behaviours in the present study, with the exception that girls with AD evidenced more sleep problems and difficulty with emotional reactivity than boys. This finding is consistent with previous findings that girls with ASD have a slightly more severe presentation than boys, although gender differences are limited (Nyden et al. 2000; Gadow et al. 2004; de Bildt et al. 2005; Holtmann et al. 2005; Herring et al. 2006; Shattuck et al. 2007). Age was positively associated with internalising maladaptive behaviours, and specifically somatic complaints and withdrawal in the present study. This finding parallels the pattern seen in typically developing children (van der Valk et al. 2003; Frigerio et al. 2004) and supports a previous report (Eisenhower et al. 2005) of an increase in internalising maladaptive behaviours and decrease in externalising maladaptive behaviours during early childhood for ASD. In the present study, non-Caucasian children with AD displayed more maladaptive behaviours than Caucasian children. Within the typically developing literature, ethnic-minority children also score higher than Caucasian children on parent-report behaviour measures (Sandberg et al. 1991; Raadal et al. 1994; Keiley et al. 2000). It is difficult to determine whether this finding reflects differences in maladaptive behaviours because of being an ethnic-minority, differences in socioeconomic status, measurement bias or differences in parent perspectives.
There are several limitations to this study. The number of correlations conducted between CBCL scores and subject characteristics increases the chance of type 1 errors (i.e. erroneously finding a significant association). However, stepwise regression analyses were conducted to account for interrelationships among subject characteristics and consistent trends emerged in the data. In order to increase confidence in findings, follow-up studies are needed. Moreover, this study used a parentrated measure of maladaptive behaviours. Observational and interview measures of maladaptive behaviours are needed in order to strengthen conclusions. The extent to which parent-factors, such as level of distress, availability of supports, or cultural and socioeconomic differences, influenced parent ratings of maladaptive behaviours could not be determined.
Participants in this study were referred to an autism clinic located in a large tertiary hospital and research university that serves a wide geographical region. Young children with AD included in this study are thought to be similar to those referred to other large specialty autism clinics. However, results from this study may not generalise to children with AD who are not referred for AD diagnosis until later ages or children with AD diagnosed outside of a specialty autism clinic. In addition, 27.8% of participants assessed in the autism clinic were excluded from this study because of incomplete data. The subject characteristics of the excluded participants did not differ from those of the participants in the study. However, there may be important differences in parent or environmental characteristics between these groups.
Research is needed to identify additional risk factors for maladaptive behaviours in young children with AD as the subject characteristics included in this study accounted for a limited portion of variance. Additional research is also needed to identify the prevalence of Clinically Significant maladaptive behaviours in other ASD groups such as young children with PDD-NOS and Asperger’s Disorder and determine the similarities or dissimilarities to that of children with AD. Furthermore, in this study maladaptive behaviours were considered as co-occurring behaviour problems. The high prevalence of many maladaptive behaviours in children with AD begs the question of whether these behaviours are better considered features of AD as opposed to separate co-morbid problems. This issue has been brought up by several other researchers (Matese et al. 1994; Tsai 1996; Perry 1998; Gillberg & Billstedt 2000; Gadow et al. 2005). Consensus has yet to be reached on the best approach for conceptualising co-morbid maladaptive behaviours in an AD population and thus this issue is in need of further research attention and discussion.
In conclusion, findings from this study highlight the need to include behavioural management strategies in any comprehensive intervention programme for young children with AD. This appears particularly true for young children with AD who have low non-verbal cognitive functioning, expressive language and adaptive skills. Ethnic-minority children and girls are also at a somewhat greater risk of maladaptive behaviours during early childhood. Behavioural management strategies will need to address a variety of maladaptive behaviours given the high rate of co-morbidity and increasingly be aimed at internalising behaviours as children with AD age from the first to second year of life to age 5 years. Most importantly, behavioural management efforts should be aimed at increasing social engagement, sustained attention and decreasing aggressive behaviour.
References
- Achenbach T, Rescorla L. Child Behavior Checklist. ASEBA; Burlington, VT: 2000. [Google Scholar]
- Akshoomoff N. Use of the Mullen Scales of Early Learning for the assessment of young children with autism spectrum disorders. Child Neuropsychology. 2006;12:269–77. doi: 10.1080/09297040500473714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. American Psychiatric Association Press; Washington, D.C: 2000. Text Revision. [Google Scholar]
- Bolte S, Dickhut H, Poustka F. Patterns of parent-rated problems indicative of autism. Psychopathology. 1999;32:93–7. doi: 10.1159/000029072. [DOI] [PubMed] [Google Scholar]
- Bradley EA, Summers JA, Wood HL, Bryson SE. Comparing rates of psychiatric and behavior disorders in adolescents and young adults with severe intellectual disability with and without autism. Journal of Autism and Developmental Disorders. 2004;34:151–61. doi: 10.1023/b:jadd.0000022606.97580.19. [DOI] [PubMed] [Google Scholar]
- Brereton AV, Tonge BJ, Einfeld SL. Psychopathology in children and adolescents with autism compared to young people with intellectual disability. Journal of Autism and Developmental Disorders. 2006;36:863–70. doi: 10.1007/s10803-006-0125-y. [DOI] [PubMed] [Google Scholar]
- Carter AS, Black DO, Tewani S, Connolly CE, Kadlec MB, Tager-Flusberg H. Sex differences in toddlers with autism spectrum disorders. Journal of Autism and Developmental Disorders. 2007;37:86–97. doi: 10.1007/s10803-006-0331-7. [DOI] [PubMed] [Google Scholar]
- Day HM, Horner RH. Multiple functions of problem behaviors: assessment and interventions. Journal of Applied Behavior Analysis. 1994;27:279–90. doi: 10.1901/jaba.1994.27-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bildt A, Sytema S, Kraijer D, Sparrow S, Minderaa R. Adaptive functioning and behavior problems in relation to level of education in children and adolescents with intellectual disability. Journal of Intellectual Disability Research. 2005;49:672–81. doi: 10.1111/j.1365-2788.2005.00711.x. [DOI] [PubMed] [Google Scholar]
- Dominick KC, Orstein Davis N, Lainhart J, Tager- FLusberg H, Folstein J. Atypical behaviors in children with autism and children with a history of language impairment. Research in Developmental Disabilities. 2007;28:145–62. doi: 10.1016/j.ridd.2006.02.003. [DOI] [PubMed] [Google Scholar]
- Durand VM. Functional communication training using assistive devices: effects on challenging behavior. Augmentative and Alternative Communication. 1993;9:168–76. [Google Scholar]
- Ehlers S, Nyden A, Gillberg C, Dahlgren-Sandberg A, Dahlgren SO, Hjelmquist E, et al. Asperger syndrome, autism, and attention disorders: a comparison study of the cognitive profile of 120 children. Journal of Child Psychology and Psychiatry. 1997;38:207–17. doi: 10.1111/j.1469-7610.1997.tb01855.x. [DOI] [PubMed] [Google Scholar]
- Eisenhower AS, Baker BL, Blacher J. Preschool children with intellectual disability; syndrome specificity, behaviour problems, and maternal well-being. Journal of Intellectual Disability Research. 2005;49:657–71. doi: 10.1111/j.1365-2788.2005.00699.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fidler DJ, Hepburn S, Rogers S. Early learning and adaptive behaviour in toddlers with Down syndrome: evidence for an emerging behavioural phenotype? Down Syndrome Research and Practice. 2006;9:37–44. doi: 10.3104/reports.297. [DOI] [PubMed] [Google Scholar]
- Frigerio A, Caltaneo C, Cataldo M, Schiatti A, Molteni M, Battaglia M. Behavioral and emotional problems among Italian children and adolescents aged 4 to 18 years as reported by parents and teachers. European Journal of Psychological Assessment. 2004;20:124–33. [Google Scholar]
- Gadow KD, Sprafkin J. Checkmate Plus. Stoney Brook; NY: 1997. Early Childhood Symptom Inventory – 4 Norms Manual. [Google Scholar]
- Gadow KD, Sprafkin J. Checkmate Plus. Stony Brook; NY: 2000. Early Childhood Symptom Inventory – 4 Screening Manual. [Google Scholar]
- Gadow KD, DeVincent CJ, Pomeroy J, Azizian A. Psychiatric symptoms in preschool children with PDD and Clinic and Comparison samples. Journal of Autism and Developmental Disorders. 2004;34:379–93. doi: 10.1023/b:jadd.0000037415.21458.93. [DOI] [PubMed] [Google Scholar]
- Gadow KD, DeVincent CJ, Pomeroy J. Comparison of DSM-IV symptoms in elementary schoolaged children with PDD versus clinic and community samples. Autism. 2005;9:392–415. doi: 10.1177/1362361305056079. [DOI] [PubMed] [Google Scholar]
- Gillberg C, Billstedt E. Autism and Asperger Syndrome: Coexistence with other clinical disorders. Acta Psychiatrica Scandinavia. 2000;102:321–30. doi: 10.1034/j.1600-0447.2000.102005321.x. [DOI] [PubMed] [Google Scholar]
- Green J, Gilcharist A, Burton D, Cox A. Social and psychiatric functioning in adolescents with Asperger’s syndrome compared with conduct disorder. Journal of Autism and Developmental Disorders. 2000;30:279–93. doi: 10.1023/a:1005523232106. [DOI] [PubMed] [Google Scholar]
- Harris S, Handleman J. Age and IQ at intake as predictors of placement for young children with autism: a four- to six-year follow-up. Journal of Autism and Developmental Disorders. 2000;30:137–42. doi: 10.1023/a:1005459606120. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Kovshoff H, Ward NJ, Espinosa F, Brown T, Remington B. Systems analysis of stress and positive perceptions in mothers and fathers of pre-school children with autism. Journal of Autism and Developmental Disorders. 2005;35:635–44. doi: 10.1007/s10803-005-0007-8. [DOI] [PubMed] [Google Scholar]
- Herring S, Gray L, Taffe J, Tonge G, Sweeney D, Einfield S. Behaviour and emotional problems in toddlers with pervasive developmental disorders and developmental delay: association with parental mental health and family functioning. Journal of Intellectual Disability Research. 2006;50:874–882. doi: 10.1111/j.1365-2788.2006.00904.x. [DOI] [PubMed] [Google Scholar]
- Holtmann M, Bolte S, Poustka F. Attention-Deficit/Hyperactivity Disorder symptoms in Pervasive Developmental Disorders: association with autistic behavior domains and coexisting psychopathology. Psychopathology. 2005;40:172–7. doi: 10.1159/000100007. [DOI] [PubMed] [Google Scholar]
- Horner RH, Diemer SM, Brazeau KC. Educational support for students with severe problem behaviors in Oregon: a descriptive analysis from the 1987–88 school year. Journal of the Association for Persons with Severe Handicaps. 1992;17:154–69. [Google Scholar]
- Horner RH, Carr EG, Strain PS, Todd AW, Reed HK. Problem behavior interventions for young children with autism: a research synthesis. Journal of Autism and Developmental Disorders. 2002;32:423–46. doi: 10.1023/a:1020593922901. [DOI] [PubMed] [Google Scholar]
- Howlin P, Goode S, Hutton J, Rutter M. Adult outcome for children with autism. Journal of Child Psychology and Psychiatry. 2004;45:212–29. doi: 10.1111/j.1469-7610.2004.00215.x. [DOI] [PubMed] [Google Scholar]
- Keiley M, Bates JE, Dodge KA, Pettit GS. A cross domain growth analysis: externalizing and internalizing behavior during 8 years of childhood. Journal of Abnormal Child Psychology. 2000;28:161–79. doi: 10.1023/a:1005122814723. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kurita H. School refusal in pervasive developmental disorders. Journal of Autism and Developmental Disorders. 1991;30:162–7. doi: 10.1007/BF02206993. [DOI] [PubMed] [Google Scholar]
- Lecavalier L, Leone S, Wiltz J. The impact of behaviour problems on caregiver stress in young people with autism spectrum disorders. Journal of Intellectual Disability Research. 2006;50:172–83. doi: 10.1111/j.1365-2788.2005.00732.x. [DOI] [PubMed] [Google Scholar]
- Lord C, Risi S, Lambrecht L, Cook EH, Leventhal BL, DiLavore PC, et al. The Autism Diagnostic Observation Schedule-Generic: a standard measure of social and communication deficits associated with the spectrum of autism. Journal of Autism and Developmental Disorders. 2000;30:205–23. [PubMed] [Google Scholar]
- Matese M, Matson JL, Sevin J. Comparison of psychiatric and autistic children using behavioral observations. Journal of Autism and Developmental Disorders. 1994;24:83–94. doi: 10.1007/BF02172214. [DOI] [PubMed] [Google Scholar]
- Mullen E. Mullen Scales of Early Learning AGS Edition. American Guidance Systems; Circle Pines, MN: 1995. [Google Scholar]
- National Research Council. Educating Children with Autism. National Academy Press, Committee on Educational Interventions for Children with Autism, Division of Behavioral and Social Sciences and Education; Washington, DC: 2001. [Google Scholar]
- Nyden A, Hjelmquist E, Gillberg C. Autism spectrum and attention deficit disorders in girls. Some neuropsychological aspects. European Child and Adolescent Psychiatry. 2000;9:180–5. doi: 10.1007/s007870070041. [DOI] [PubMed] [Google Scholar]
- Perry R. Misdiagnosed ADD/ADHD: rediagnosed PDD. Journal of the American Academy of Child and Adolescent Psychiatry. 1998;27:113–4. doi: 10.1097/00004583-199801000-00024. [DOI] [PubMed] [Google Scholar]
- Raadal M, Milgrom P, Cauce AM, Mancl L. Behavior problems in 5- to 11-year-old children from low-income families. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:1017–25. doi: 10.1097/00004583-199409000-00013. [DOI] [PubMed] [Google Scholar]
- Sandberg DE, Meyer-Bahlburg HF, Yager TJ. The Child Behavior Checklist nonclinical standardization samples: should they be utilized as norms? Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:124–34. doi: 10.1097/00004583-199101000-00019. [DOI] [PubMed] [Google Scholar]
- Shattuck PT, Seltzer MM, Greenberg JS, Orsmond GI, Bolt D, Kring S, et al. Change in autism symptoms and maladaptive behaviors in adolescents and adults with an autism spectrum disorder. Journal of Autism and Developmental Disorders. 2007;37:1735–47. doi: 10.1007/s10803-006-0307-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sparrow SS, Cicchetti DV, Balla DA. Vineland Adaptive Behavior Scales. 2. AGS Publishing; Circle Pines, MN: 2005. [Google Scholar]
- Stone WL, Yoder PJ. Predicting spoken language level in children with autism spectrum disorders. Autism. 2001;5:341–61. doi: 10.1177/1362361301005004002. [DOI] [PubMed] [Google Scholar]
- Tonge BJ, Einfeld SL. The trajectory of psychiatric disorders in young people with intellectual disabilities. Australian and New Zealand Journal of Psychiatry. 2000;34:80–4. doi: 10.1046/j.1440-1614.2000.00695.x. [DOI] [PubMed] [Google Scholar]
- Tsai LY. Brief report: Comorbid psychiatric disorders of autistic disorder. Journal of Autism and Developmental Disorders. 1996;26:159–63. doi: 10.1007/BF02172004. [DOI] [PubMed] [Google Scholar]
- Van der Valk JC, Van den Oord EJ, Verhulst FC, Boomsa DI. Genetic and environmental contributions to the stability and change in children’s internalizing and externalizing problems. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;41:1212–20. doi: 10.1097/00004583-200310000-00012. [DOI] [PubMed] [Google Scholar]
- Weisbrot DM, Gadow KD, DeVincent CJ, Pomeroy J. The presentation of anxiety in children with pervasive developmental disorders. Journal of Child and Adolescent Psychopharmacology. 2005;15:477–96. doi: 10.1089/cap.2005.15.477. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Clinical Descriptions and Guidelines. World Health Organization; Geneva: 1993. The ICD-10 Classification Of Mental and Behavioural Disorders. [Google Scholar]