Abstract
Adults with mild intellectual disability (ID) experience stressful social interactions and often utilize maladaptive coping strategies to manage these interactions. We investigated the specific types of Active and Avoidant coping strategies reported by 114 adults with mild ID to deal with stressful social interactions. Open-ended responses to a sentence stem task were coded into five dimensions of Active and Avoidant coping. Adults with mild ID used Problem-Focused coping most frequently and this strategy was negatively correlated with psychological distress. Emotion-Focused coping was used infrequently but was also negatively related to psychological distress. Coping accounted for a significant portion of variance in psychological distress after controlling for perceptions of stressful social interactions. Findings have important implications for informing the development of interventions to enhance the ability of adults with mild ID to cope with stressful social interactions.
Coping Strategies of Adults with Mild Intellectual Disability for Stressful Social Interactions
The experience of stress negatively impacts the psychological wellbeing of adults with intellectual disability (ID). Perceptions of stress are predictive of current and future symptoms of psychopathology among adults with mild ID (Hartley & MacLean, 2005; Hastings, Hatton, Taylor, & Maddison, 2004; Lunsky & Benson, 2001). Adults with mild ID report experiencing more frequent and severe stress from negative social interactions than from other categories of stressful events, making this category of stressors particularly detrimental for their psychological wellbeing (Bramston, Fogarty, & Cummins, 1999; Fogarty, Bramston, & Cummins, 1997). Moreover, adults with ID have more difficulty adaptively coping with stressful social interactions than other categories of stressful events (Benson & Fuchs, 1999; Hartley & MacLean, 2005; Wayment, & Zetlin, 1989). While it may be unfeasible to prevent the occurrence of all stressful social interactions, it is possible to help adults with mild ID more successfully cope with these interactions. The first step toward developing interventions to improve coping efforts is to understand the adaptive and maladaptive coping strategies generated by adults with mild ID when faced with stressful social interactions.
Coping is defined as the cognitive and behavioral efforts employed to manage the demands (external and/or internal) of a stressful situation and/or the emotions surrounding the situation (Lazarus & Folkman, 1984). The few studies that have assessed coping in people with ID indicate that adults with mild ID can identify and describe their coping efforts (Benson & Fuchs, 1999; Hartley & MacLean, 2005; Wayment, & Zetlin, 1989), and that their coping strategies can be coded into categories used with the general population (Hartley & MacLean, 2005, Wayment, & Zetlin, 1989). Only one study has examined the relation between coping and psychological health among adults with mild ID. As in the general population (for a review see Compas et al., 2001), Active coping (i.e., efforts to gain control over a stressful situation or over one’s emotions) was negatively related to psychological distress and there was a trend suggesting that Avoidant coping (i.e., efforts to avoid or disengage from a stressful situation or one’s emotions) is a maladaptive coping strategy that is positively related to symptoms of depression and anxiety (Hartley & MacLean, 2005).
People with ID have been reported to utilize more Avoidant coping strategies and fewer Active coping strategies to deal with stressful social interactions than other categories of stressful events (Benson & Fuchs, 1999; Hartley & MacLean, 2005; Wayment, & Zetlin, 1989). Wayment and Zetlin (1989) found that adolescents with learning handicaps reported more coping efforts aimed at suppressing, denying, and avoiding stressful events and thoughts about the event than non-handicapped peers particularly for stressful events in which others mistreated them or were upset at them. Hartley and MacLean (2005) assessed the self-reported coping efforts of 88 adults with mild ID through an open-ended sentence stem task. They also found that adults with mild ID reported a higher rate of Avoidant coping and lower rate of Active coping to deal with stressful social interactions than they reported for other types of stressful events. An investigation of the specific dimensions of Active and Avoidant coping used by adults with mild ID when faced with stressful social interactions and further insight into the relation between these coping strategies and psychological distress is now needed.
Active and Avoidant Coping
Various dimensions of Active and Avoidant coping have been proposed within the coping literature for the general population (Compas et al., 2001). For Active coping, Problem-Focused coping, which involves attempts to alter the stressful situation itself, is distinguished from Emotion-Focused coping, which involves efforts to alter negative affect surrounding the stressful situation (Ayers, Sandler, West, & Roosa, 1996; Connor-Smith, Compas, Wadsworth, Thomsen, & Saltzman, 2000; Walker, Smith, Garber, & Van Slyke, 1997). Support Seeking coping, a third type of Active coping, is defined as the involvement of other people as resources to seeking solutions to a stressful situation or to listen to and provide understanding for emotions surrounding the stressor (Ayers et al., 1996; Walker et al., 1997). Two dimensions of Avoidant coping are commonly identified in the general population. Behavioral Avoidance coping (i.e., staying away from the stressful situation) involves attempts to physically avoid stressful situations, while Cognitive Avoidance coping (i.e., wishing the stressful situation did not happen or repressing thoughts about it) involves attempts to ignore or avoid thinking of the stressor (e.g., Ayers et al., 1996; Walker et al., 1997).
Coping follows a predictable developmental course within the general population (Compas, Forsythe, & Wagner, 1988; Compas et al., 2001), and this may provide insight into the coping strategies of adults with mild ID. Within Active coping, Problem-Focused and Emotion-Focused coping strategies are generated more often during earlier stages of development than Support Seeking coping, which requires purposeful efforts to utilize others to identify solutions to stressful events or alter negative affect (e.g., Ayers et al., 1996; Landolt, Vollrath, & Ribi, 2002; Spirito, Stark & Knapp, 1992). In light of this developmental progression, adults with mild ID may similarly generate more Problem-Focused and Emotion-Focused coping strategies then Support Seeking coping strategies to deal with stressful social interactions.
Problem-Focused coping develops earlier than Emotion-Focused coping, which requires complex language and metacognitive capabilities to alter negative affect (e.g. Band, & Weisz, 1988; Compas, Banez, Malcarne, & Worsham, 1991; Compas et al., 1988). Metacognitive skills such as flexible, abstract thinking and focused attention are difficult for adults with mild ID (e.g., Baroff & Olley, 1999; Sturmey, 2004). Therefore, it is likely that adults with mild ID also generate more Problem-Focused coping strategies than Emotion-Focused coping strategies. Some understanding of the link between cognitions and emotions may be needed before intentional efforts can be exerted to alter negative affect through restructuring cognitions. However, Dagnan, Chadwick and Proudlove (2000) found that only 10% to 25% of adults with mild ID performed better than chance on a task requiring them to match cognitions, emotions, and situations. Similarly, Oathamshaw and Haddock (2006) found that less than 20% of a sample of adults with ID and psychosis correctly identified a cognition that matched a situation and emotion. This limited understanding of the link between emotions and cognitions may limit the use of Emotion-Focused coping in an ID population.
Cognitive Avoidance coping also requires complex metacognitive abilities to identify and then ignore or wish away distressing thoughts. Behavioral Avoidance coping strategies therefore develop earlier and are used more often at younger stages of development than Cognitive Avoidance coping in the general population (e.g., Landolt et al., 2002; Spirito et al., 1992). Given limited development of complex metacognitive skills, it is likely that adults with mild ID also generate more Behavioral Avoidant coping than Cognitive Avoidance coping when faced with stressful social interactions.
The aim of this study is to provide insight into the types of Active and Avoidant coping strategies used by adults with mild ID to deal with stressful social interactions and their relation to psychological distress. Adopting a developmental framework, the following hypotheses were made: 1) overall Active coping will be negatively related and overall Avoidant coping will be positively related to psychological distress; 2) Support Seeking coping will be used less often than other Active coping strategies; 3) Problem-Focused coping will be used more often than Emotion-Focused coping; and 4) adults with mild ID will report a greater use of Behavioral Avoidance than Cognitive Avoidance coping strategies.
Method
Participants
One hundred and twenty-seven adults with mild ID (IQ 55–70 and concomitant impairments in adaptive behavior), and adequate oral communication skills (i.e., orally communicate without the aid of another person) were recruited from disability service providers in the Rocky Mountain region of the United States to participate in the study. Participants and their legal guardians were provided with information on the nature and requirements of the study prior to consenting to be in the study. Participants with a diagnosis of autism were excluded given that deficits in social functioning are a defining aspect of this disorder and thus the experience of stressful social situations, including coping with these situations, may differ in this group. Eleven of the 127 participants were excluded because they were unable to pass the pretest outlined in the procedure section. Two participants evidenced response bias during actual testing (i.e., reported the same response option for all items) and were also excluded.
Of the remaining 114 participants, 60 participants were male and 54 were female. The age range of participants was 19 to 65 years (M = 40.33, SD = 12.52) and the mean Composite IQ was 61.82 (SD = 5.52). Ninety-five participants were Caucasian, 8 were Hispanic, 3 were African-American, 2 were Asian/Pacific Islander, and 6 were Native American. On the Adaptive Behavior Assessment System- 2nd edition (ABAS-II; Harrison & Oakland, 2006), participants had a mean General Adaptive Composite score of 63.76 (SD = 6.54). Previous studies of stress and coping among adults with ID included subjects with mixed etiology of ID (Bramston et al., 1999; Fogarty et al., 1997; Hartley & MacLean, 2005; Lunsky, 2003). In-line with this approach, participants had various etiologies for their ID with the largest proportion being of unknown etiology. Sixty-nine participants lived in group homes, 10 lived with family/host family, and 34 lived alone or shared an apartment with 1 roommate or partner. Forty-three participants (37.8%) currently had a psychiatric disorder diagnosis from their disability service provider in addition to ID (17 mood disorder, 10 anxiety disorder, 8 personality disorder, 2 psychotic disorder, 5 adjustment disorder, and 1 sexual disorder). Similar prevalence rates of psychiatric disorder have been reported for the broader ID population (Borthwick-Duffy, 1994; White, Chant, Edwards, Townsend, & Waghorn, 2005).
Measures
Subject Characteristics
Participant age, sex, living status, and ethnicity were obtained from each participant’s disability service provider. The IQ Composite score of the Kaufman Brief Intelligence Test, 2nd edition (K-BIT-2, Kaufman & Kaufman, 2004) was used to assess IQ. This is an individually administered, brief test of intelligence that assesses verbal and nonverbal abilities of people aged 6 to 90 years. The K-BIT-2 IQ Composite score has satisfactory internal consistency (.86 to .96), test-retest reliability (.88 to .92), and is highly correlated (.89) with the Wechsler Adult Intelligence Scale- 3rd Edition (Wechsler, 1997) Full Scale IQ (Kaufman & Kaufman, 2004). Staff from each participant’s disability service provider who had contact with the participant on at least a weekly basis served as informants for the ABAS-II. This scale assesses three general areas of adaptive behavior (conceptual, social, and practical), which combine to form the General Adaptive Composite (GAC) score. The GAC has high internal consistency (.97 to .99) and test-retest reliability (.86 to .99), and satisfactory concurrent validity (Harrison & Oakland, 2006).
Psychological Distress
The Birleson Depressive Short Form Self-Rating Scale (BDS-S; Birleson, 1981) is a measure of depressive symptoms originally created for typically developing children. The BDS-S has 18 items and 3 response categories (“Never,” “Sometimes,” and “Most of the Time”). When used by adults with mild ID, the scale was positively correlated with somatic complaints (r = .54) and informant ratings of depressive symptoms (r = .26) (Benson & Ivins, 1992; Lunsky & Benson, 2001). In the present study the BDS-S had a mean of 13.68 and standard deviation of 7.97. The Glasgow Anxiety Scale for People with Intellectual Disabilities (GAS-ID; Minham & Espie, 2003) is a 27-item self-rating scale. The GAS-ID has adequate internal consistency (α = .96), criterion validity with the Beck Anxiety Inventory (Beck, Epstein, Brown, & Steer, 1988), and 4-week test-retest reliability (r = .95) among adults with ID (Minham & Espie, 2003). In the present study the GAS-ID had a mean of 14.79 and standard deviation of 8.87. Given a moderate correlation between the GAS-ID and BDS-S (r = .53, p < .01), a composite measure of psychological distress was created by summing the z-scores of the BDS-S and GAS-ID. Table 1 displays the descriptive information for psychological distress and other core measures.
Table 1.
Descriptive Information for Measures of Coping, Psychological Distress, and Stressful Social Interactions
| Range |
Mean (SD) |
Median |
Inter-quarter range |
|
|---|---|---|---|---|
| Coping | ||||
| Coping (%) | 13 – 100 | 83.0 (16.5) | 86 | 75 – 100 |
| Active (%) | 0 – 100 | 56.5 (32.2) | 57 | 33 – 84 |
| Problem-Focused (%) | 0 – 100 | 34.2 (26.1) | 33 | 11 – 50 |
| Emotion-Focused (%) | 0 – 66 | 13.4 (17.0) | 0 | 0 – 25 |
| Support Seeking (%) | 0 – 75 | 17.5 (19.5) | 15 | 0 – 29 |
| Avoidant (%) | 0 – 100 | 29.6 (25.9) | 25 | 0 – 50 |
| Behavioral (%) | 0 – 100 | 19.3 (22.7) | 17 | 0 – 33 |
| Cognitive (%) | 0 – 83 | 15.4 (19.6) | 0 | 0 – 33 |
| Coping Dimensions Used (n) | 1 – 5 | 2.88 (0.86) | 3 | 2 – 3 |
| Psychological Distress | ||||
| Composite (z-score) | −2.72 – 5.07 | −.03 (−.175) | −.11 | −1.60 – 1.31 |
| Stressful Social Interactions | ||||
| Frequency (score) | 3 – 41 | 15.80 (7.83) | 15.00 | 9.75 – 20.00 |
| Stress Impact (score) | 0 – 3 | 2.07 (0.56) | 2.17 | 1.75 – 2.50 |
| Frequency × Stress Impact (score) | 0 – 280.03 | 81.04 (61.31) | 68.31 | 32.86 – 113.30 |
Stressful Social Interactions
A composite score of stressful social interactions using the Lifestress Inventory (Bramston & Bostock, 1994) and Inventory of Negative Social Interactions (INSI; Lakey, Tardiff, & Drew, 1994) was used in this study. The Lifestress Inventory is a self-report measure of daily events or life situations developed for adults with ID. The Lifestress Inventory has adequate 2 week test-retest reliability, internal consistency, and concurrent and criterion validity among people with mild ID (Bramston & Bostock, 1994; Fogarty et al., 1997; Lunsky & Bramston, 2006). The 13 item Negative Interpersonal Relations dimension assesses negative actions of others or social situations and was used in the present study. The INSI is a 40-item self-report inventory of negative social situations. Among adults with mild ID, the INSI has been shown to have satisfactory reliability and criterion validity (Lunsky & Benson, 2001; Lunsky & Bramston, 2006).
The same response format was used for the Lifestress Inventory and INSI. In the frequency rating, participants indicated if they have encountered the stressful situation described within the past 2 weeks. In the stress impact rating, participants used a 4-point Likert-type scale containing verbal descriptors (“No,” “A Little,” “Medium,” and “A Lot”) and numbers (1–4) to indicate the severity of stress incurred. Based on Fogarty et al. (1997), severity ratings were re-scored for all analyses such that a stress impact rating in which events ‘not experienced’ or ‘experienced but not stressful’ are scored 0, events perceived to have ‘A Little’ stress are scored 1, events perceived to have ‘Medium’ stress are scored 2, and events with ‘A Lot’ of stress are scored 3. A total Frequency score was created by summing the number of stressful social interactions across measures. A total Stress Impact score was created by summing severity ratings across all stressful social interactions and then dividing by the total Frequency score.
Coping Strategies
Open-ended responses to the sentence stem “When I have this problem, I” were used to assess coping strategies for each stressful social interaction endorsed on the Lifestress Inventory and INSI. This procedure has been shown to successfully elicit coping responses among adults with mild ID (Hartley & MacLean, 2005; Lunsky, 2003; Wayment & Zetlin, 1989). A sentence stem task has the advantage of avoiding the endorsement of socially desirable responses and other response biases associated with yes-no, either-or and Likert scale questionnaires (Hartley & MacLean, 2006; Finlay & Lyons, 2002).
Responses to the sentence stem were coded into the Active coping dimensions of Problem-Focused, Emotion-Focused, and Support-Seeking, and the Avoidant coping dimensions of Behavioral Avoidance and Cognitive Avoidance based on criteria by Ayers and colleagues (Ayers, Sandler, Bernzweig, Harrison, Wampler, & Lustig, 1989; Program for Prevention Research, 1999). Table 2 provides a definition and examples for these coping dimensions. It is important to note that people with ID are often dependent on staff or family in their day programs, jobs, and homes, and thus their coping efforts commonly involved staff or family. If the person with ID sought the involvement of staff or family for the direct purpose of altering the stressor (e.g., getting staff to enforce a rule or change practices/policies), the effort was coded as Problem-Focused coping. In contrast, if the person with ID involved staff or family for the purpose of soliciting advice or solutions to later fix the problem or emotional understanding, the effort was coded as Support Seeking coping.
Table 2.
Definitions of Coping Dimensions, Examples, and Cohen's Kappa Interrater Reliability
| Coping Dimension | Definition | Examples | Cohen's Kappa |
|---|---|---|---|
| Active | .87 | ||
| Problem-Focused | Cognitive and behavioral efforts to manage the stressful situation itself. |
1. "Talked to [roommate] and worked it out." 2. "I told [staff] that he wasn't doing dishes so they make him do dishes." |
.85 |
| Emotion-Focused | Efforts to manage the emotional response to a stressor by focusing directly on it in an active and constructive fashion. |
1."Think about my best friend who likes me. Is my friend." 2."Tell myself that I'm living by myself soon so don't have to see her |
.78 |
| Support-Seeking | Use of other people as a resource to identify solutions for the stressor or provide understanding of feelings. |
1."Talked to [staff] about it and they told me to tell my boss." 2. "Told my doctor about it and they made me feel better." |
.87 |
| Avoidant | .83 | ||
| Behavioral | Efforts to avoid the problem by staying away from it or leaving it. |
1."Yelled back and then go to my room so don't see her." 2. "I was so mad at my boss so I left work and didn't go back." |
.83 |
| Cognitive | Cognitive efforts to repress or not think about the problem or wish it away. |
1. "Try to forgot about it. Pretend they don't exist" 2. "Dream about being pretty." |
.76 |
Note. Criteria are modified from Ayers, Sandler, Bernzweig, Harrison, Wampler, and Lustig (1989) and Program for Prevention Research (1999). If coping effort involved managing the stressful situation itself through using staff or family (e.g., staff enforced rule or changed practice/policy), it was coded as Problem-Focused coping. If coping effort involved soliciting advice or solutions from staff or family that latter resulted in altering the stressful sitaution, it was coded as Support Seeking coping.
Two undergraduate students, naïve to the study hypotheses, were trained according to the Handbook for the Content Analysis of Children’s Coping Responses (Ayers et al., 1989; Program for Prevention Research, 1999) to independently code responses. In accordance with Ayers et al. (1989), responses that involved verbal or physical actions to implicitly or explicitly hurt or threaten others or vent feelings with no intention of altering these feelings were coded as Non-Coping efforts. Participants often reported using multiple coping strategies to deal with a single stressful event (e.g., two Problem-Focused coping strategies or an Emotion-Focused coping and Support Seeking coping strategy). When this occurred, all coping strategies were coded.
To account for differences in total number of stressful social interactions endorsed, the ratio of Coping and Non-Coping efforts in comparison to the total number of responses to the sentence stem task was calculated. Similarly, to determine the relative use of the various Active and Avoidant coping dimensions, the ratio of coping efforts in each coping dimension in comparison to the total number of coping strategies reported was used in all analyses. Table 2 also displays Cohen’s Kappa interrater reliability for the coping dimensions. Satisfactory interrater reliability was achieved for the Active and Avoidant coping dimensions.
Procedure
Participants were reminded that their responses would be confidential and that they had the right to withdraw from the study at any time. Interviews were conducted at participants’ disability service provider headquarters or home. A 2 step pretest was used to determine whether each participant could reliably use a 4-point Likert-type scale and understood the meaning of stress. In step 1, participants were required to correctly arrange a set of clear containers with varying amounts of colored water by quantity of water from least to greatest. Participants were then required to match containers to descriptors (“No” “A Little” “Medium” and “A Lot”) and a numerical scale (1 to 4). Finally, participants were required to correctly indicate where their favorite and least favorite food item fell using the containers, descriptors, or numbers. In step 2, participants were given a definition of stress (consistent with Lazarus & Folkman, 1984) and were required to provide an example of a stressful situation and define stress in their own words. This pretest was developed in a previous study (Hartley & MacLean, 2005) and shown to result in minimal response bias during actual testing.
Participants who were successful on both steps of the pretest were read the Lifestress Inventory and INSI. Clear containers filed with varying amounts of colored water were paired with the Likert-type scale descriptors and numbers to provide a visual representation of response options. For every positive response indicating the presence of a stressful social interaction, participants were asked to complete the sentence stem “When I have this problem, I.” If participants appeared confused or did not describe how they coped with the interaction, a modified statement from the Handbook for the Content Analysis of Children’s Coping Responses (Program for Prevention Research, 1999), “People do different things to solve their problems or to make themselves feel better. What do you do when you have this problem,” was read. The clarifying question “Tell me more about it” was used to seek further information when needed. The BDS-S and GAS-ID were read aloud to participants. In all, the procedure took 60–90 minutes per participant.
Results
An alpha level of ≤.01 was established as the criterion for significance in all analyses. Correlations were first conducted to identify subject characteristics (gender [0 = male, 1 = female], age [years], ethnicity [0 = Caucasian, 1 = non-Caucasian], IQ [standard score], and adaptive behavior [GAC standard score]) related to psychological Distress. There were no significant correlations between the subject characteristics and psychological distress. A one-way analysis of variance (ANOVA) indicated a trend for psychological distress to differ by living status (alone or with 1 roommate/partner, group home, or family/host family), F (2, 112) = 3.23, p = .04. Adults with mild ID living alone or with a roommate/partner (M = -.61, SD = 1.68) had somewhat less psychological distress than adults with mild ID living with family/host family (M = .73, SD = 1.05) or in a group home (M = .14, SD = 1.80).
Coping versus Non-Coping Efforts
The percentage of total responses coded as Coping, as opposed to Non-Coping, by each participant ranged from 13% to 100% (M = 83.0%, SD =16.5%). Correlations were conducted to identify subject characteristics related to the relative use of Coping efforts. There were no significant correlations between the subject characteristics and relative use of Coping efforts. A one-way ANOVA indicated that relative use of coping efforts did not significantly differ by living status (group home, alone or with 1 roommate/partner, and family/host family). A Pearson correlation indicated a significant negative correlation between relative use of Coping efforts and psychological distress (r = -.28, p <.01).
Relative Use of Active and Avoidant Coping
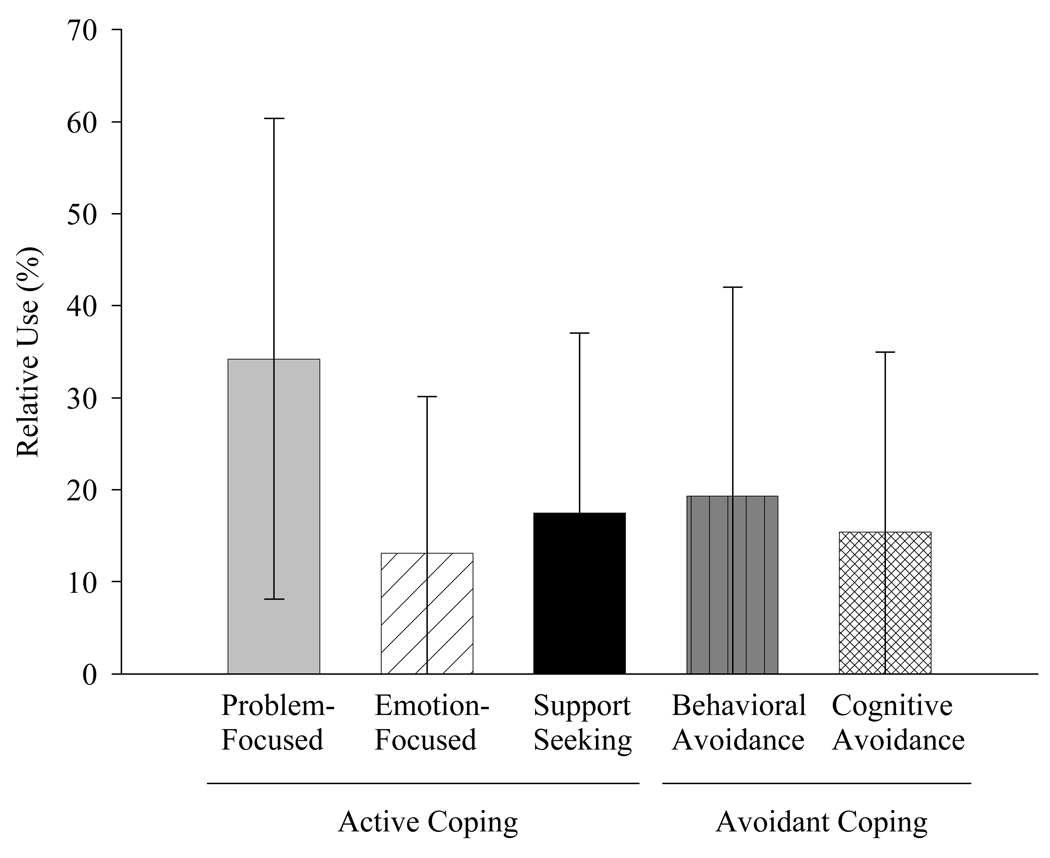
The remaining analyses pertain to the responses coded as Coping efforts. Of the 5 Active and Avoidant coping dimensions, on average participants reported using 2 to 3 dimensions of coping (M = 2.88, SD = 0.86). Specifically, 4.4% of participants used 1 coping dimension, 29.2% of participants used 2 coping dimensions, 42.5% of participants used 3 coping dimensions, 22.1% of participants used 4 coping dimensions, and 1.8% of participants used all 5 coping dimensions. A Wilcoxon related-samples comparison indicated a significant difference in the relative use of Active (M = 56.5%, SD = 32.2%) and Avoidant coping (M = 29.6%, SD =25.9%), z = −4.28, p <.01. Figure 1 presents the mean relative use and standard deviation for the Active and Avoidant coping dimensions. A Friedman nonparametric test indicated a significant difference among the relative use of five coping dimensions χ2 (4, 111) = 43.56, p <.001. Bonferroni-corrected Wilcoxon related-samples comparisons indicated that relative use of Problem-Focused coping (M = 34.2%4, SD = 26.1%) was significantly higher than Emotion-focused coping (M = 13.4%, SD =17.0; z = −6.18, p <.01) and Support Seeking coping (M =17.5%, SD = 19.5%; z = −4.41, p <.01). The relative use of Problem-Focused coping was significantly higher than Behavioral Avoidance coping (M = 19.3%, SD = 22.7%; z = −4.02, p <.01 and Cognitive Avoidance coping (M = 15.4%, SD = 19.6%; z = −4.75, p < .01. There were not significant differences in the relative use of Emotion-Focused coping and Support Seeking coping (z = −1.61, p = .12), Behavioral Avoidance (z = −1.63, p =.20), or Cognitive Avoidance coping (z = −0.33, p = .74). There was not a significant difference in the relative use of Support Seeking coping and Behavioral Avoidance (z = −0.19, p = .85) or Cognitive Avoidance coping (z = −1.15, p = .25). There was not a significant difference in the relative use of Behavioral Avoidance and Cognitive Avoidance coping, z = −1.29, p = .20.
Figure 1.
Percentage of Coping Efforts coded into the various Active and Avoidant Coping Dimensions
Correlations were conducted to identify subject characteristics related to the relative use of Active and Avoidant coping strategies. Age, the only subject characteristic significantly correlated with the relative use of coping strategies, was significantly positively correlated with Behavioral Avoidance coping (r = .24, p = .01). A repeated measures multivariate analysis of variance (MANOVA) indicated that the relative use of the coping dimensions did not significantly differ by living status (group home, family/host family, and alone with 1 roommate/partner), Wilks’ Lambda = 0.88, F (2, 112) = 1.41, p = .18.
Coping and Psychological Distress
The skewness and kurtosis of the coping, psychological distress, and stressful social interaction scores were examined. Values did not exceed an absolute value of 1.0, indicating reasonably normal distributions. The obtained data were also consistent with expected normal probability plots. Frequency histograms, however, showed a positive skew for Emotion-Focused and Cognitive Avoidance coping. Therefore, square root transformations were computed for these variables. Similar results were obtained for regression analyses using the non-transformed and transformed scores and those only the non-transformed scores are reported.
Pearson correlations were conducted between psychological distress and overall Active and Avoidant coping. There was a significant negative correlation between Active coping and psychological distress (r = -.26, p < .01). There was a trend toward a positive correlation between Avoidant coping and psychological distress (r = .21, p = .03). Pearson correlations were also conducted between the various dimensions of Active and Avoidant coping and psychological distress. There was a significant negative correlation between Problem-Focused coping and psychological distress (r = -.26, p <.01) and between Emotion-Focused coping and psychological distress (r = -.35, p <.01). There was not a significant correlation between Support Seeking coping (r = -.14, p = .14) and psychological distress. Similarly, there was not a significant correlation between Behavioral Avoidance coping (r = .11, p = .27) and psychological distress. There was a trend toward a positive correlation between Cognitive Avoidance coping and psychological distress (r = .20, p =.04).
To further examine the relationship between coping and psychological distress, a hierarchical regression analysis was conducted in which perceptions of Stressful Social Interactions (total Frequency × total Stress Impact) was entered in the first step, followed by the five coping dimensions in the second step. Results are summarized in Table 3. Using both perceptions of stressful social interactions and the five coping dimensions in the equation, 31% of the variance in psychological distress was accounted for. After controlling for the effects of perceptions of stressful social interactions and the other coping strategies, Emotion-Focused coping was significantly negatively predictive of psychological distress, β = −0.24, t (112) = 2.53, p = .01.
Table 3.
Hierarchical Regression Analyses of the Effect of Coping on Psychological Distress
| df |
β |
R2 |
ΔR2 |
F |
|
|---|---|---|---|---|---|
| Step 1- Stressful Social Interactions | 1 | .52 | .22 | 0.27** | 40.78** |
| Step 2- Coping | 5 | .26 | 0.04* | 9.22** |
p <.05,
p ≤.01
Discussion
Adults with mild ID are vulnerable to experiencing stress from negative social interactions and to using ineffective coping strategies to deal with this category of stressors (e.g., Bramston et al., 1999; Fogarty et al., 1997; Hartley & MacLean, 2005). Insight into the specific types of coping strategies used by adults with mild ID when faced with stressful social interactions and the relation between these strategies and psychological distress is the first step toward developing interventions to improve coping efforts and subsequently the psychological wellbeing of adults with mild ID. In this study we identified the use of various Active and Avoidant coping dimensions for managing stressful social interactions and their association with psychological distress.
When faced with stressful social interactions, Problem-Focused coping strategies were reported to be used more frequently by adults with mild ID than Emotion-Focused coping strategies. This finding is consistent with the developmental emergence of coping in the general population (Band, & Weisz, 1988; Compas et al., 1991; Compas et al., 1988). Cognitive efforts to alter negative emotions require complex metacognitive skills and are likely to be difficult for adults with mild ID. As predicted, adults with mild ID reported more Problem-Focused coping than Support Seeking coping. In contradiction to our hypothesis, there was not a significant difference in the relative use of Support Seeking and Emotion-Focused coping. Adults with mild ID receiving disability services often have large networks of supportive staff in their residential placement (e.g., group homes and supervised apartments), job (e.g., job coach), and disability service providers (e.g., case manager and psychologist). Many adults with mild ID also have supportive family members and friends with whom they regularly interact. The increased use of Support Seeking coping among adults with mild ID as compared to their developmentally comparable peers in the general population may reflect the typical involvement of supportive others in their everyday life.
As in the general population and a previous study of adults with mild ID (Hartley & MacLean, 2005), Active coping was negatively correlated with psychological distress (i.e., symptoms of depression and anxiety). Efforts to increase the use of Active coping by adults with mild ID in the face of stressful social interactions may help decrease psychological distress. These efforts may be best aimed at capitalizing on the natural generation of Problem-Focused coping in this population through teaching and encouraging appropriate efforts to alter stressful social situations. An initial step to such training may be social problem-solving instruction aimed at teaching processes for identifying effective solutions to interpersonal conflict. Social problem-solving programs have been developed and promising results have been found among adults with mild ID (e.g., Foss, Auty, & Irvin, 1989; Loumidis & Hill, 1997). The long-term impact of these interventions on managing stressful social interactions needs to be investigated.
Stressful social interactions are to a degree inevitable and often can not be altered through Problem-Focused coping. Efforts to increase Emotion-Focused coping strategies are thus important to reduce the ill-effects of stressful social interactions. In this study, adults with mild ID generated a low rate of Emotion-Focused coping strategies. However, in contrast to our prediction, when employed Emotion-Focused coping was an adaptive coping strategy and the only coping strategy negatively predictive of psychological distress after controlling for the experience of stressful social interactions and the other coping strategies. Interventions aimed at increasing Emotion-Focused coping have been developed for typically developing children (e.g., Pincus, & Friedman, 2004; Vernon, 1983; 1989). For instance, (Vernon 1983, 1989) designed an “emotional education” program to help children identify and change negative feelings through role plays, discussion questions, and worksheets and activities. Recent research suggests that similar “emotional education” interventions aimed at increasing Emotion-Focused coping strategies among adults with mild ID may be effective. As previously mentioned, a large percentage of people with ID can not readily identify connections between emotions and cognitions (Dagnan et al., 2000; Oathamshaw & Haddock, 2006). However, a growing body of research suggests that with training, adults with mild ID can be taught to regulate emotions through altering thoughts (e.g., Stenfert-Kroese, Dagnan, & Loumidis, 1997; Taylor, Novacco, Gillmer, Robertson, & Thorne, 2004). Research is needed to evaluate the feasibility of teaching adults with mild ID strategies for altering maladaptive cognitions as a way to regulate perceptions of stress surrounding negative interactions with others.
In line with coping literature in the general population, Emotion-Focused coping in the current study was defined as cognitive efforts to alter negative affect to be more positive (e.g., Ayers et al., 1996; Compas et al., 2001). This conceptualization fails to capture behavioral Emotion-Focused coping strategies aimed at modifying negative affect such as deep breathing relaxation or writing down feelings (Compas et al., 2001). Behavioral Emotion-Focused coping does not require complex metacognitive skills and thus may be a more viable strategy for adults with mild ID to alter negative affect and deserves further study.
Support Seeking coping was not significantly related to psychological distress in the present study. It may be that supportive others were not fully assisting adults with mild ID in identifying solutions to stressful social interactions and modifying negative affect surrounding these interactions. For instance, caregivers, friends, and family may have been describing appropriate strategies for rectifying social conflict but not actually guiding adults with mild ID in implementing these strategies. Alternatively, adults with mild ID may be seeking advice and emotional support from categories of others (i.e., other people with ID as opposed to support staff or family) unable to provide appropriate assistance. Support Seeking coping may also be maladaptive in that it fosters reliance on other people, which ultimately does not help the adult with ID develop independent problem-solving skills. Further research is needed to examine these and other possibilities. Identifying the circumstances for which Support Seeking coping is an adaptive strategy is important given that this may be a feasible way for many adults with mild ID to identify solutions to complicated stressful social interactions.
In this study, Avoidant coping was only weakly related to increased psychological distress. A similar finding was reported in a previous study (Hartley & MacLean, 2005) and suggests that Avoidant coping is not necessarily a maladaptive strategy among adults with mild ID. Adults with mild ID often have little control over their environments. They may not have the ability to modify many stressful social interactions (e.g., working with staff persons or deciding who they live with). For these negative interactions, efforts to avoid or ignore stressful social interactions may be related to better psychological outcomes than futile attempts to modify a situation that is outside of their control. Further research is needed to identify the stressful social interactions for which Avoidant coping is adaptive. However, the trend toward a positive association between Avoidant coping and psychological distress suggests that Avoidant coping should largely be discouraged and replaced with Active coping. Adults with mild ID appear to utilize relatively equal rates of Behavioral Avoidance and Cognitive Avoidance strategies when faced with stressful social interactions. Therefore, interventions should be aimed at teaching adults with mild ID how to replace both their cognitive attempts to ignore or wish away thoughts about a negative social interaction and behavioral efforts to avoid the situation with Active coping strategies.
There are several limitations to this study. Adults with mild ID receiving disability services and who had access to supportive networks of staff participated in this study. Conclusions regarding the use of coping strategies are limited to this population. However, this is the population for which we have the most opportunity to design coping interventions. The present study is also limited in that we investigated the association between coping and symptoms of depression and anxiety at one time point. This methodology does not allow for an understanding of the causal time-order relation between coping and psychological distress. Research with the typically developing population suggests that the relation between coping and psychological distress is complex and involves a bidirectional causal pathway in which maladaptive coping both leads to and is the result of psychological distress (e.g. Compas et al., 2001; Connor-Smith & Compas, 2004). Further research is needed to investigate the complex causal pathways between coping and psychological distress in an ID population.
We investigated coping strategies found to have high validity and reliability in a developmentally comparable population. Independent coders were able to reliably code the open-ended coping responses of adults with mild ID into these categories. However, this does not mean that the coping dimensions used in the present study provide the best fit to the coping efforts of adults with mild ID. Factor analysis conducted with larger samples is needed to identify the dimensions of coping that best discriminate among coping efforts by adults with mild ID. Moreover, findings from this study can only speak to coping strategies for stressful social interactions. Adults with mild ID may cope differently with other categories of stressors, and Active and Avoidant coping strategies may be related to different outcomes for these other categories of stressors.
The present study is also limited in that coping was assessed through the self-report of adults with mild ID. Self-report measures rely on retrospective reporting and are vulnerable to recall errors (Folkman & Moskowitz, 2004). In the general population, many have advocated for the need to only assess the most bothersome event that occurred that day to shorten the recall period (Folkman & Moskowitz, 2004; Stone et al., 1998). Momentary coping assessments have also been employed through the use of ecological momentary assessment techniques (Stone et al., 1998). These “real time” strategies may be a more appropriate measurement strategy for people with ID, who often have memory difficulties (e.g., Henry & MacLean, 2002; Numminen, Service, & Ruoppila, 2002). Observational studies would also help ensure that the coping strategies reported by adults with mild ID are the coping strategies actually utilized in stressful social situations.
In summary, results from this study have implications for designing coping interventions for adults with mild ID. Research efforts are now needed to examine various methods for teaching adaptive coping strategies in this population. Future research should also examine stress and coping in people with ID who have specific psychiatric disorders. In the general population, depressed persons experience high rates of stressful social interactions and employ maladaptive coping strategies to deal with these events. These processes are thought to maintain depressed affect overtime (e.g., Davila, Hammen, Burge, Paley, & Daley, 1995; Hammen, 1991; Sigmon et al., 2007). Research is needed to determine whether stress and coping also perpetuates depressed affect in adults with mild ID.
References
- Ayers TS, Sandler IN, Bernzweig JA, Harrison RJ, Wampler TW, Lustig LL. Handbook for the content analysis of Children’s coping responses. Tempe: Program for Prevention Research, Arizona State University; 1989. [Google Scholar]
- Ayers TS, Sandler IN, West SG, Roosa MW. A dispositional and situational assessment of Children’s Coping: Testing alternative models of coping. Journal of Personality. 1996;64:923–959. doi: 10.1111/j.1467-6494.1996.tb00949.x. [DOI] [PubMed] [Google Scholar]
- Band EB, Weisz JR. How to feel better when it feels bad: Children’s perspectives on coping with everyday stress. Developmental Psychology. 1988;24:247–253. [Google Scholar]
- Baroff GS, Olley JG. Mental retardation: Nature, case and management. 3rd Edition. Philadelphia, PA: Brunner/Mazel; 1999. [Google Scholar]
- Benson BA, Fuchs C. Anger-arousing situations and coping responses of aggressive adults with intellectual disabilities. Journal of Intellectual and Developmental Disability. 1999;24:207–215. [Google Scholar]
- Benson BA, Ivins J. Anger, depression, and self-concept in adults with mental retardation. Journal of Intellectual Disability Research. 1992;36:169–175. doi: 10.1111/j.1365-2788.1992.tb00492.x. [DOI] [PubMed] [Google Scholar]
- Birleson P. The validity of depressive disorder in childhood and the development of a self-rating scale: A research report. Journal of Child Psychology and Psychiatry and Allied Disciplines. 1981;22:73–88. doi: 10.1111/j.1469-7610.1981.tb00533.x. [DOI] [PubMed] [Google Scholar]
- Borthwick-Duffy SA. Epidemiology and prevalence of psychopathology in people with mental retardation. Journal of Consulting and Clinical Psychology. 1994;62:17–27. doi: 10.1037//0022-006x.62.1.17. [DOI] [PubMed] [Google Scholar]
- Bramston P, Bostock J. Measuring stress in people with intellectual disabilities: The development of a new scale. Australia and New Zealand Journal of Developmental Disabilities. 1994;19:149–157. [Google Scholar]
- Bramston P, Fogarty GJ, Cummins RA. The nature of stressors reported by people with an intellectual disability. Journal of Applied Research in Intellectual Disabilities. 1999;12:1–10. [Google Scholar]
- Compas BE, Banez GA, Malcarne V, Worsham N. Perceived control and coping with stress: A developmental perspective. Journal of Social Issues. 1991;47:23–34. [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Progress, problems, and potential in theory and research. Psychological Bulletin. 2001;127:87–127. [PubMed] [Google Scholar]
- Compas BE, Forsythe C, Wagner BM. Consistency and variability in causal attributions and coping with stress. Cognitive Therapy and Research. 1988;12:305–320. [Google Scholar]
- Connor-Smith JK, Compas BE. Coping as a moderator of relations between reactivity to interpersonal stress, health status, and internalizing problems. Cognitive Therapy and Research. 2004;28:347–368. [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68:976–992. [PubMed] [Google Scholar]
- Dagnan D, Chadwick P, Proudlove J. Toward an assessment of suitability of people with mental retardation for cognitive therapy. Cognitive Therapy and Research. 2000;24:627–636. [Google Scholar]
- Davila J, Hammen C, Burge D, Paley B, Daley SE. Poor interpersonal problem solving as a mechanism of stress generation in depression among adolescent women. Journal of Abnormal Psychology. 1995;104:592–600. doi: 10.1037//0021-843x.104.4.592. [DOI] [PubMed] [Google Scholar]
- Dumont M, Provost MA. Resilience in adolescents: Protective role of social support, coping strategies, and self-esteem. Journal of Youth and Adolescence. 1999;28:343–364. [Google Scholar]
- Finlay WM, Lyons E. Acquiescence in interviews with people who have mental retardation. Mental Retardation. 2002;40:14–29. doi: 10.1352/0047-6765(2002)040<0014:AIIWPW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Fogarty GJ, Bramston P, Cummins RA. Validation of the Lifestress Inventory for people with a mild intellectual disability. Research in Developmental Disabilities. 1997;18:435–456. doi: 10.1016/s0891-4222(97)00021-8. [DOI] [PubMed] [Google Scholar]
- Foss G, Auty WP, Irvin LK. A comparative evaluation of modeling, problem-solving, and behavioral rehearsal for teaching employment-related interpersonal skills to secondary students with mental retardation. Evaluation and Training in Mental Retardation. 1989;24:17–27. [Google Scholar]
- Folkman S, Moskowitz JT. Coping: Pitfalls and promise. Annual Review of Psychology. 2004;55:745–774. doi: 10.1146/annurev.psych.55.090902.141456. [DOI] [PubMed] [Google Scholar]
- Garner PW. The relations of emotional role taking, affective/moral attributions and emotional display rule knowledge to low-income school-age children’s social competence. Journal of Applied Developmental Psychology. 1996;17:19–36. [Google Scholar]
- Hammen C. Generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Harrison P, Oakland R. Adaptive Behavior Assessment System-Second Edition (ABAS-II.) San Antonio, TX: Harcourt Assessment, Inc; 2006. [Google Scholar]
- Hartley SL, MacLean WE., Jr A review of the reliability and validity of Likert-type scales for people with intellectual disability. Journal of Intellectual Disability Research. 2006;50:813–827. doi: 10.1111/j.1365-2788.2006.00844.x. [DOI] [PubMed] [Google Scholar]
- Hartley SL, MacLean WE., Jr Perceptions of stress and coping strategies among adults with mild mental retardation: Insight into psychological adjustment. American Journal on Mental Retardation. 2005;110:285–290. doi: 10.1352/0895-8017(2005)110[285:POSACS]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Hastings RP, Hatton C, Taylor JL, Maddison C. Life events and psychiatric symptoms in adults with intellectual disabilities. Journal of Intellectual Disability Research. 2004;48:42–47. doi: 10.1111/j.1365-2788.2004.00584.x. [DOI] [PubMed] [Google Scholar]
- Henry LA, MacLean M. Working memory performance in children with and without intellectual disabilities. American Journal on Mental Retardation. 2002;107:421–432. doi: 10.1352/0895-8017(2002)107<0421:WMPICW>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Kaufman AS, Kaufman NL. KBIT-2: Kaufman Brief Intelligence Test. 2nd ed. Minnesota: AGS Publishing; 2004. [Google Scholar]
- Lakey B, Tardiff TA, Drew JB. Negative social interactions: Assessment and relations to social support, cognitions, and psychological distress. Journal of Social and Clinical Psychology. 1994;13:42–62. [Google Scholar]
- Landolt MA, Vollrath M, Ribi K. Predictors of coping strategy selections in paediatric patients. Acta Paediatrica. 2002;91:954–960. doi: 10.1080/080352502760272650. [DOI] [PubMed] [Google Scholar]
- Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer; 1984. [Google Scholar]
- Loumidis K, Hill A. Social problem-solving groups for adults with learning disabilities. In: Stenfert-Kroese B, Dagnan D, Loumidis K, editors. Cognitive-behaviour therapy for people with learning disabilities. New York: Brunner-Routledge; 1997. pp. 86–109. [Google Scholar]
- Lunsky Y. Depressive symptoms in intellectual disability: Does gender play a role? Journal of intellectual Disability Research. 2003;47:417–428. doi: 10.1046/j.1365-2788.2003.00516.x. [DOI] [PubMed] [Google Scholar]
- Lunsky Y, Benson BA. Association between perceived social support and strain, and positive and negative outcomes for adults with mild intellectual disability. Journal of Intellectual Disability Research. 2001;45:106–114. doi: 10.1046/j.1365-2788.2001.00334.x. [DOI] [PubMed] [Google Scholar]
- Lunsky Y, Bramston P. A preliminary study of perceived stress in adults with intellectual disabilities according to self-report and informant rating. Journal of Intellectual and Developmental Disability. 2006;31:20–27. doi: 10.1080/13668250500488660. [DOI] [PubMed] [Google Scholar]
- Minham J, Espie CA. Glasgow Anxiety Scale for people with intellectual disability (GAS-ID): Development and psychometric properties of a new measure for use with people with mild intellectual disability. Journal of Intellectual Disabilities Research. 2003;47:22–30. doi: 10.1046/j.1365-2788.2003.00457.x. [DOI] [PubMed] [Google Scholar]
- Numminen H, Service E, Ruoppila I. Working memory, intelligence, and knowledge base in adult persons with intellectual disability. Research in Developmental Disabilities. 2002;23:105–118. doi: 10.1016/s0891-4222(02)00089-6. [DOI] [PubMed] [Google Scholar]
- Oathamshaw SC, Haddock G. Do people with intellectual disabilities and psychosis have the cognitive skills required to undertake cognitive behavioural therapy? Journal of Applied Research in Intellectual Disabilities. 2006;19:35–46. [Google Scholar]
- Pincus DB, Friedman AG. Children’s coping with everyday stress: Transporting treatment intervention to the school setting. Clinical Child and Family Psychology Research. 2004;7:223–240. doi: 10.1007/s10567-004-6087-8. [DOI] [PubMed] [Google Scholar]
- Program for Prevention Research. Manual for the Children’s Coping Strategies Checklist and the How I Coped Under Pressure Scale. 1999 (Available from Arizona State University, P.O. Box 876005, Tempe, AZ 85287–6005. [Google Scholar]
- Sigmon ST, Pells TJ, Schartel JG, Hermann BA, Edenfield TM, LaMattina SM, et al. Stress reactivity and coping in seasonal and nonseasonal depression. Behavior Research and Therapy. 2007;45:965–975. doi: 10.1016/j.brat.2006.07.016. [DOI] [PubMed] [Google Scholar]
- Spirito A, Stark LJ, Knaapp LG. The assessment of coping in chronically ill children: Implications for clinical practice. In: La Greca AM, Siegel J, Wallander JL, Walker CE, editors. Stress and coping in child health. New York: Guilford; 1992. pp. 314–322. [Google Scholar]
- Spirito A, Stark L, Williams C. Development of a brief coping checklist for use with pediatric populations. Journal of Pediatric Psychology. 1988;13:555–574. doi: 10.1093/jpepsy/13.4.555. [DOI] [PubMed] [Google Scholar]
- Stenfert-Kroese B, Dagnan D, Loumidis K. Cognitive-behaviour therapy for people with learning disabilities. New York: Brunner-Routledge; 1997. [Google Scholar]
- Stone AA, Schwartz JE, Neale JM, Shiffman S, Marco CA, Hickcox M, et al. A comparison of coping assessed by ecological momentary assessment and retrospective recall. Journal of Personality and Social Psychology. 1998;74:1670–1680. doi: 10.1037//0022-3514.74.6.1670. [DOI] [PubMed] [Google Scholar]
- Sturmey P. Cognitive therapy with people with intellectual disabilities: A selective review and critique. Clinical Psychology and Psychotherapy. 2004;11:222–232. [Google Scholar]
- Taylor JL, Novaco RW, Gillmer BT, Robertson A, Throne I. Individual cognitive-behavioural anger treatment for people with mild-borderline intellectual disabilities and histories of aggression: A controlled trial. The British Journal of Clinical Psychology. 2004;44:367–382. doi: 10.1348/014466505X29990. [DOI] [PubMed] [Google Scholar]
- Vernon A. Rational-emotive education. In: Ellis A, Bernard M, editors. Rational-Emotive approaches to the problems of childhood. New York: Plenum; 1983. pp. 35–57. [Google Scholar]
- Vernon A. Thinking, feeling, behaving: An emotional education curriculum for children: Grades 1–6. Champaign, Illinois: Research Press; 1989. [Google Scholar]
- Walker LS, Smith CA, Garber J, Van Slyke DA. Development and validation of the pain response inventory for children. Psychological Assessment. 1997;9:392–405. [Google Scholar]
- Wayment HA, Zetlin AG. Coping responses of adolescents with and without mild learning handicaps. Mental Retardation. 1989;27:311–316. [PubMed] [Google Scholar]
- Wechsler D. WAIS-III: Wechsler Adult Intelligence Scale. Administration and Scoring Manual. 3rd Edition. San Antonio, TX: Psychological Corportation/Harcourt Brace; 1997. [Google Scholar]
- White P, Chant D, Edwards N, Townsend C, Waghorn G. The prevalence of intellectual disability and comorbid mental illness in an Australian community sample. The Australian and New Zealand Journal of Psychiatry. 2005;39:395–400. doi: 10.1080/j.1440-1614.2005.01587.x. [DOI] [PubMed] [Google Scholar]
- Zeider M, Endler NS. Handbook of coping: Theory, research, applications. New York: John Wiley & Sons, Inc; 1996. [Google Scholar]