Abstract
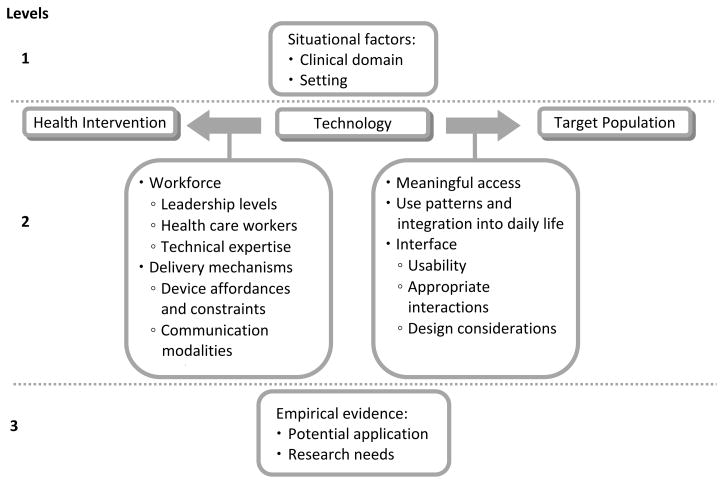
Health information technologies (HIT) have great potential to advance health care globally. In particular, HIT can provide innovative approaches and methodologies to overcome the range of access and resource barriers specific to developing countries. However, there is a paucity of models and empirical evidence informing the technology selection process in these settings. We propose a framework for selecting patient-oriented technologies in developing countries. The selection guidance process is structured by a set of filters that impose particular constraints and serve to narrow the space of possible decisions. The framework consists of three levels of factors: 1) situational factors, 2) the technology and its relationship with health interventions and with target patients, and 3) empirical evidence. We demonstrate the utility of the framework in the context of mobile phones for behavioral health interventions to reduce risk factors for cardiovascular disease. This framework can be applied to health interventions across health domains to explore how and whether available technologies can support delivery of the associated types of interventions and with the target populations.
Keywords: Medical informatics, Health behavior, Developing countries, Patient care, Cellular Phone, Cardiovascular Disease
1. Introduction
Health information technologies (HIT), which include computers, mobile devices, and other technologies used in the management of medical information, have great potential to promote health and support healthcare around the world. In recent years, the technologies for information delivery within healthcare systems have proliferated in developed countries. There is also increasing attention towards developing patient-oriented healthcare delivery, including devices that support patient self-management, health decision making, and patient education.
Most recently, there is a growing body of research exploring the potential of HIT in developing countries, although not as extensively as it has been explored in developed countries [1–3]. These research and development activities focus on HIT to support clinics and healthcare providers [4–6]. However, research on patient-oriented HIT is sparse in these settings. In environments where patients often face access barriers to healthcare, patient-oriented interventions can better connect or deliver healthcare services with patients and engage patients in their health management efforts. Our particular focus is in technologies that mediate delivery of interventions to consumers and patients, including lifestyle modification information, health monitoring, management of chronic illness, and preventive care as they have been shown to be effective when delivered to patients [7].
There are a range of immense challenges to designing and implementing technology to improve health in developing countries; these challenges include limited healthcare resources, medical expertise, access to healthcare, access to technology, and infrastructure and technical expertise to support technology [8, 9]. HIT can provide innovative approaches and methodologies to overcoming these access and resource barriers. The comparatively fragile state of affairs and dearth of resources highlight the need to reduce uncertainty and waste of resources by trial and error during the development of health interventions in these settings. There is potential to exacerbate existing health disparities, and careful implementation can help to reduce potentially negative outcomes. However, there is a paucity of research to form an empirical basis for making informed decisions and to guide the technology selection and intervention development processes in these settings.
From a health research point of view, frameworks can guide research by leveraging existing knowledge to conceptualize a particular problem and identify a suitable approach, to define specific possibilities for empirical query, and to formulate hypotheses. Specifically, a technology selection framework is a class of frameworks concerned with facilitating decisions pertaining to the development or acquisition of technology. They can guide the early stages of conceptualizing, developing, and implementing HIT research agendas. A technology selection framework integrates factors concerned with decision making, selection criteria, and configuration of component processes of technology selection [10]. Existing technology selection frameworks usually present different levels of filters, or criteria that gradually constrain the selection space. There can be high level (e.g. environment) and low level filters (e.g. the selection of a particular model of a technology).
Frameworks can thus reduce trial and error and waste of resources by poorly conceived research and implementation. We propose a technology selection framework for selecting an appropriate technology for a patient-oriented HIT intervention in developing countries. There are examples of technology selection frameworks developed in the context of developed nations, such as for telecommunication service selection [11] and selection of internet access technologies in rural communities [12]. In developed nations, much of the emphasis in technology management is placed on control of technological development and technology utilization. Developing nations often lack the resources to develop technology themselves, and emphasis is rather on selection of the most suitable technology and the best means of technology transfer to rapidly achieve economic and social development goals [13]. Developed and developing nations also diverge in their social, political, technical, and economic constraints as well as national goals [14]. A framework that considers HIT factors in developing countries is more appropriate to inform context-specific technology selection models. A technology selection framework was developed for telecommunications in developing countries [14]; however this framework addresses telecommunications in general and is not adapted for healthcare. A model of HIT selection for developing countries presents the considerations of implementing health technologies [15]. However, there isn’t a specific framework that guides the decision making process for health technology selection in developing countries.
2. Technology Selection Framework
The framework emerged as a product of our work with various consumer health interventions employing both mobile and non-mobile health technologies. Experience revealed recurring challenges and barriers related to mismatches among health interventions, technology, and target populations. Often the knowledge needed to guide such an initiative was not available. A theoretically motivated framework could yield insight into the appropriate configuration of dependent factors to maximize benefits and overcome barriers given specific intervention settings and conditions. We endeavored to identify additional challenges, barriers, and candidate solutions with a focus on the intersection of informatics, human factors, public health, communication, and sociocultural factors. The framework emerged through a process of review and synthesis. The purpose of this paper is to articulate the framework and explore its implications.
We investigated the concept of a technology selection framework, which was found to be a construct used predominantly in the business sector to examine management and financial decisions. With the aid of a health science librarian, we identified a selection of consumer health interventions in developing countries from a wide range of literature databases including Medline, PsycINFO, and Science Citation Index. A review of literature and case examples of HIT interventions revealed different challenges and lessons learned in the technology selection process. Through these methods, we have elicited and synthesized the different stages of technology selection and the barriers and considerations within each stage.
We propose a technology selection framework for selecting an appropriate technology to deliver and engage patients with health interventions, in the context of developing countries. Such a framework guides the decision making process around technology selection, and gives rise to a technology-selection method. This framework considers high-level filters, and is potentially applicable to a range of technologies, domains, target populations, and clinical settings. The conditions and setting in which the framework is applied are dynamic, but the framework criteria are static; it can help researchers anticipate and be responsive to changes on the ground and can also be used for reevaluating interventions at future points as well. The framework does not address considerations specific to particular devices (e.g. a model of glucose meters), settings, or health domains, but can contribute to the development of these more specific models. The framework presents three levels of component processes for consideration when planning to develop a technology-based patient health intervention in a low-resource setting, and highlights areas for necessary further research.
Technologies have great potential to manage, exchange, and target information for health interventions, but there are many factors involved in making them successful and considering whether they are a good fit. Different technologies are appropriate in different settings and for specific purposes. Understanding the environment to research and develop technology for patient-oriented health in developing countries draws on a range of research areas and disciplines, including public health practices, sociomedical science models, informatics methods, cognitive science and user-centered design principles. This can be a complex research and development endeavor with many variables to consider.
2.1 Level 1: Situational factors
Clinical domain
Level 1 begins with the consideration of situational factors, which include the clinical domain, and identification of appropriate and effective health interventions within that domain.
For example, HIV treatment adherence, risk reduction counseling, and decision support would all be health interventions within the clinical domain of HIV/AIDS. Interventions can potentially address common co-morbidities concurrently, particularly if they share similar risk factors. Also, the health conditions and functional status of target patients would need to be compatible with the physical and cognitive demands required of the technology. Identification of appropriate health interventions and the target population will inform the other factors in the selection process.
Setting
The setting is a crucial situational factor [16], and presents a wide range of unique obstacles for consideration in developing countries. The environmental setting must accommodate the technology; some climates that are excessively humid or excessively arid may require selection of more robust technologies. Sufficient security to protect the valuable technology units, particularly in public settings, must be in place. Additionally, infrastructure support to maintain the technology is important. This type of support may take the form of internet connectivity, mobile network signal, electricity, battery packs, or a power generator. The clinic, home, and any other settings in which the technology may be used are also important; the technologies must be suitable to all settings. These setting and environment obstacles are often more prevalent in developing countries, and innovative approaches are necessary to overcome the unique challenges in these settings.
2.2.1 Level 2: Technology and Health Intervention
In the relationship between the health intervention and the technology, there are a set of factors to consider whether the technology appropriately meets the needs of the health intervention.
Workforce
A crucial requisite for successful implementation of any intervention is adequate healthcare workforce, as they make up the frontline of delivery for health interventions. There needs to be committed and skilled personnel at all levels to ensure sufficient programmatic and technical support [16]. This would include leadership commitment, staff support, and technical expertise to make sure the technology is reliable. Workforce is often scarce, and education and experience levels can vary. Supplemental training may be necessary to enable workforce to interact with and manage the health technology, and facilitate delivery of the health intervention. Workforce may also be needed to train patients to use technologies. However, as workforce is often scarce and overburdened already with responsibilities, an intervention must be designed that doesn’t require a high learning curve or increase these burdens, but may help alleviate constraints on time and tasks.
Delivery mechanisms
Health interventions must be delivered in an appropriate and effective manner. The technology must meet the delivery needs and communication methods of the health intervention. There are different ways in which various technologies mediate different communication modalities; each medium offers diverse sets of constraints and costs [17]. For example, email communication offers asynchronous communication and reviewability through durable textual information, but does not convey visual or audible properties such as facial expressions, gestures, or intonations. While email may be suitable for casual or non-urgent communication, it is usually not suitable for information-sensitive or urgent communication. Intervention effectiveness can be optimized through careful consideration of fit between the communication requirements of the health intervention and the communication affordances and constraints of various media types.
2.2.2 Level 2: Technology and Target Population
A set of factors determine whether a technology is suitable and appropriate to the target population.
Meaningful access
Target populations should have meaningful access to the technology. Meaningful access encompasses accessibility and affordability of equipment, connectivity, skill development, ongoing technical support, and appropriate content [18]. If access to a computer is rare or costly, but access to a mobile phone line is more affordable, then the mobile phone line would be more practical for an intervention that requires frequent communication. Cost effectiveness and perceived value both influence this consideration. Technology penetration may influence providers and general public at different rates.
Use patterns
The use patterns and how the technology plays a role in daily life would also inform suitability of a technology for the intended health intervention. If a technology is a shared resource, but the health intervention risks sharing private health information, then a more personal or more secure device may be appropriate [19]. Knowing whether a mobile phone is habitually carried with a person or frequency of checking email may influence the reach and effectiveness of an email-based or mobile phone-based intervention. Leveraging this knowledge about the frequency and extent of use of different technologies can better inform selection of a technology that matches the communication frequency and needs of the health intervention. Integrating the technology and health intervention with minimal disruption of the existing use patterns and daily practices can also facilitate positive reception and adoption of health interventions.
Interface
The interface for interaction must be easy to use, culturally relevant, and be appropriate for interaction [20, 21]. Navigation pathways, menu structures, and meaningful icons would need to be adapted for local relevance and ease of use, taking into account cultural representations and understanding of concepts. For example, a study of South Africa students found that interpreting the meaning of hierarchical information structure posed difficulty, although this concept forms the basis of menu structures and navigation pathways of technologies in developed countries [20]. A variety of languages should be supported by the technology to enable greater reach among the patient population, particularly for those that use local languages. Limited literacy among target populations may require audio or visual interface for interaction [3]. The mode of interaction between the technology and the end-user is also an important consideration – mobile phones have a small screen and small buttons for interaction whereas a computer uses monitor, keyboard, and mouse as the main methods of interaction. For those interventions that may require frequent input/output, an efficient and easy-to-use interface would be essential. A simple and clear visual display can increase appeal and usability. Usability and design are important considerations to improve adoption and use rates [22].
2.3 Level 3: Empirical evidence
Careful consideration of the factors that influence the fit between the task, the technology, and the population would inform but would not cover all considerations that guide selection of the appropriate technology for the proposed purpose and setting. As mentioned earlier, empirical evidence in these research areas may be lacking. However, if empirical evidence is available, then it could further inform potential for application of the technology and additional research needs, such as cost-effectiveness, reduction of errors, changes in patient outcomes, and user satisfaction [23].
Potential for application
Although empirical evidence to inform the technology selection may be sparse, there may be related examples in other application domains, in other settings, or with different populations, from which parallels can be drawn and lessons can be extracted. It is important to uncover evidence supporting the potential of the chosen technology to fit the required needs, particularly in similar types of settings or with similar target populations. Generalizability of existing studies can inform the design and development of the chosen technology. Exploring the application of technology-mediated treatment adherence in a range of settings, within a range of health domains, and with a variety of target populations can reveal some of the common successes and obstacles that might be encountered and planned for in advance. For example, an evaluation of a PDA-based system to collect tuberculosis test results in Peru revealed user acceptance and positive attitudes towards PDAs, workforce training required to learn the devices, and improved efficiency of collection and reach of populations through use of mobile devices [24]. Sharing experiences from such a study can inform similar mobile technology-based delivery of health interventions in developing countries. Another example is a review of information systems for follow-up of HIV and TB patients in developing countries which revealed important lessons learned about cost-effectiveness, functional requirements and how information systems help to overcome the unique challenges encountered in developing countries [6]. It can be difficult to draw parallels among diverse settings and conditions; careful extraction and application of lessons and parallels should be observed.
Research Needs
The previous two levels of consideration break down the factors for consideration, . Research needs can be revealed through careful consideration of missing information links among any of these factors. Consulting empirical evidence can reveal additional relevant topics, and whether there is sufficient research or evidence on those topics. For example, identifying whether evaluation metrics exist that can be adapted for the purpose of the chosen technology can inform the need to develop appropriate evaluation metrics for use with the chosen technology.
3. Case Example: Mobile phones and lifestyle modification for cardiovascular disease
The framework proposed offers a basis to consider the different properties of technologies, individuals, and health interventions, and how these interact with each other when developing a technology-based health intervention. To illustrate an instantiation of this framework, we use the example of appraising the use of mobile phones for lifestyle modification interventions to reduce behavioral risk factors for cardiovascular disease [25].
3.1 Level 1: Situational factors
Clinical domain
Chronic diseases in general, and cardiovascular diseases (CVD) in particular, are growing health burdens in developing countries, making up 80% of the global burden of CVD-related disability and death [26]. In developing countries, CVD is affecting younger populations of working age, causing economic impact [27]. Populations are also living to older ages in which CVD is more likely to develop. Trends of urbanization are increasing around the world; urbanization is associated with CVD risk factors such as tobacco smoking, reduced physical activity, and poor dietary habits [28]. By 2020, CVD is projected to be the leading cause of death and disability around the world due to the rising incidence rates in low- and middle-income countries [26]. CVD is the health domain considered for this illustrative example of the framework because it has a high prevalence, and the interventions to reduce behavioral risk factors depend on communication methods that can be mediated by technologies.
Setting
Mobile phones are versatile and by definition, mobile. Individuals can use mobile phones for communication while at home, in work settings, and anywhere in between [29], which is an advantage for health communication methods for reducing behavioral risk factors. Two essential requirements for mobile phones are mobile signal reach and electricity infrastructure. Mobile signals can be inhibited by geographic barriers such as hills or far distances between signal towers. The source setting from which the communications to patients are initiated must not be affected by weak mobile signals. Use of the mobile phone is limited by frequent need for charging the battery, particularly in regions that have limited electricity infrastructure. Using lower powered phones or incorporating battery power saving strategies can help to mitigate this issue, but will likely be a continual difficulty.
3.2.1 Level 2: Technology and Individual
Mobile phones are gaining increasing market penetration around the world, including in developing countries. While the usage rates of computer, internet, and other technologies are steadily growing in resource poor settings, mobile phone usage is growing at the highest rate. The existing infrastructure of mobile phones offers a wide-reaching and effective means of communication for consumers in developing regions, particularly in rural locations [30]. While mobile phones are more cost-effective and user-friendly than other types of technologies, there are also drawbacks of limited data transmission, cost for device and for service to the device, language, and literacy demands. However, growing market penetration and the communication properties of mobile phones create opportunities for innovation in promoting healthy behaviors. Mobile phones can easily be lost, damaged, or stolen, but the economic impact of such incidents would likely be lower than repair and recovery costs associated with computers or other more expensive technological devices.
3.2.2 Level 2: Technology and Health Intervention
Most risk factors for CVD can be reduced by modifying health behaviors, such as better management of hypertension, reduction of tobacco smoking, healthy dietary habits, and regular physical activity. There are evidence-based approaches to health behavior change that targets lifestyle modification to reduce behavioral risk factors for CVD. These approaches employ interactive communication methods including collaborative goal setting and action planning, tailored messages that target individuals at the stage of change and self efficacy, individualized assessment and feedback, monitoring and follow-up of progress, and a social support network [31]. Ultimately, effective interventions require communication tools that facilitate: 1) dynamic patient-provider interaction, 2) communication with support groups, family members, and friends, and 3) access to tailored information and feedback.
Workforce
Supporting lifestyle modifications may require training in delivering CVD interventions, and these types of interactive communication would require time and committed persons to follow-up and monitor patients’ progress. Computer-based algorithms can also be designed to receive feedback or to deliver routine communications via SMS or audio. While such algorithms can reduce workload on workforce, a combination of health intervention and technology training would be required to supplement workforce knowledge and skills in incorporating health technologies into their workflow. Training would be targeted appropriately to different levels of workforce, and would include technology management training, technical training, training on use of the technology, and how to deliver health interventions using the technology. As mobile phones are commonly used and are relatively simple devices, training workforce to use them would not likely be very arduous [29]. However, recruiting technical expertise and training workforce to develop, operate, and maintain knowledge-based systems will be more difficult. An environment that engenders healthcare workers comfort and familiarity with mobile technologies helps to extend their use of mobile technologies to their work with patients. This in turn would encourage patient participation and engagement in using the technology in monitoring and managing their own healthcare.
Delivery mechanisms
Mobile phones support two basic communication modalities [17]: synchronous audible communication (phone call), and durable textual information (SMS or text messaging). These two basic modalities give rise to a range of health-related functions, including reminders/alerts, patient education, health monitoring, health reporting, storage of information on SIM card, and query/search for health information; these are all interactive communication methods employed by health behavior change interventions. Additional communication modalities supported by mobile phones may be available for more advanced phones, or with the purchase of data plans to support those functionalities. The current environment in which Bluetooth, camera, phone-based applications, and internet access capabilities are available makes it impossible to assume ubiquity and majority access. However, the additional consideration of these functionalities enables a much wider range of health-related actions. For example, Bluetooth capabilities allow for synchronization of multiple devices and data exchange over low bandwidth, cameras can be used to monitor and track dietary habits [32], and phone-based applications can be developed to support many different information management functions.
From a theoretical viewpoint, the communication functionalities provided by mobile phones support the interactive communication methods required by health behavior change interventions; this suggests that mobile technologies would sufficiently support the communication methods utilized to deliver lifestyle modification interventions. The next step is to explore whether there is any empirical evidence that would support practical implementation and the overall feasibility of this type of intervention.
3.3 Level 3: Empirical evidence
Potential for application
In the context of behavioral risk factors for CVD, there are examples in developed countries and with low-resource populations of developed countries displaying innovative methods of utilizing the functionalities of mobile phones to deliver smoking cessation [33], weight management [34], physical activity tracking interventions [35], and disease self-management strategies [36]. A report published by the United Nations Foundation describes 51 different projects across developing regions in Africa, Asia, and South America that utilize mobile technologies for health. While most of the initiatives described in the report are directed at healthcare workers, there are some that engage health consumers, for purposes such as remote monitoring of health conditions, education and awareness programs, and treatment support efforts. Studies in Thailand and South Africa showed that daily text message reminders improved medication adherence of TB patients. The study in South Africa provides real-time monitoring of medication adherence and provides medication reminders using a pillbox with SIM card and transmitter, and text messaging reminders. The study increased medication adherence rates from 60% to 90%, and the technology is now available worldwide [37, 38]. A study in China showed that text message reminders to patients improved attendance at appointments and cost one-third less than the previous method of phone reminders. Examination of similar case studies revealed that effective and far-reaching communication, strong partnerships, well-designed technology, long-term funding plan, setting measurable goals, and collaboration are key building blocks for successful projects [37]. Extracting valuable lessons learned from successful projects can inform project design and implementation, help plan for anticipated challenges, and improve efficiency and effectiveness of projects.
The Microsoft Research Initiative recently funded projects as part of the “Cell Phone as a Platform for Healthcare Awards” [39]. One such project is guided by a multi-faceted user-centered design approach to develop Smart Phones with an interface and functionalities that match the needs of the population (elderly), setting (rural or urban), and health intervention (diabetes self-management) [40]. As in many developed nations, China has a growing diabetes epidemic that is particularly acute among the elderly population. The particular technology selected for development enables multiple forms of input to accommodate users with very basic computer and literacy skills, supports a range of self-management and education functions needed for diabetes self care, and the data can be readily shared with providers given the existing infrastructure. Although the project is still in its early phases, the investigators are attuned to a range of variables at different levels, from individual to community. They have made judicious technology selections based on their understanding of the target population and engineered conditions that increase the likelihood of success of this health intervention.
Research Needs
Some empirical evidence exists that provide insight into several of the factors that affect technology selection. There are some studies exploring in detail the use patterns of different technologies in developing countries [41–43]. There is also emerging research in exploring the use of mobile phones with patients in developing countries, such as for HIV treatment adherence and management [44], CVD behavior change and emotional support [45], and development of social support software [46]. Technology interaction and usability studies reveal use barriers and innovative alternatives to more appropriate icons and menu and navigation structures [47]. In addition, there is growth in technology research promoting human development, termed Information and Communication Technology for Development (ICT4D), User-centered Design for Development (UCD4D), and Human Computer Interaction for Development (HCI4D) [48–51]. These contribute to the development of culturally relevant and meaningful technology interfaces and to local adaptation of existing investigation methods for use in developing countries. Similarities and parallels can be drawn between the behavior-related health management skills for CVD and for other global chronic diseases such as HIV, TB, and diabetes.
Exemplifying the framework in the consideration of mobile phones for CVD reflects the usefulness of the framework to represent the problem space and consider the filtering criteria. Given the constraints discussed, mobile phones emerged from the possible technology options as having the prerequisite properties of being productive and useful in these settings. The applied example provides further theoretical evidence supporting the potential of mobile phones to meet the communication needs and requirements of CVD behavior modification interventions in the context of developing countries.
4. Conclusion
There is a growing interest in implementing HIT in developing countries, but its potential remains largely untapped. The unique barriers and paucity of empirical evidence in these settings challenge the development and implementation of new HIT initiatives. The adaptation and development of frameworks and models specific to developing countries can begin to guide and expand research efforts in this area. In this paper we propose a framework for considering and selecting appropriate technologies to deliver and support patient-oriented health interventions in the context of developing countries. The framework considers high-level factors of the decision-making process, including situational factors, technology fit with health interventions and target populations, and empirical evidence. It differs from other technology selection frameworks in that it draws on the social and cognitive sciences in understanding technology-mediated health behaviors. The framework is applicable to a range of technologies, clinical domains, and settings.
This framework is based on review and synthesis. Further testing is needed to assess its predictive validity and determine whether it can effectively guide the technology selection process. However, in our view, a theoretically sound and grounded framework can serve to conceptualize a problem and formulate potential approaches, seed hypotheses for empirical exploration, and help anticipate and adapt to dynamic factors. The conditions on the ground and the state of technology are perpetually changing and much of the value of a framework lies in its ability to accommodate such changes. For example, Web 2.0 technologies have enjoyed considerable growth and are beginning to infiltrate the healthcare arena. Social networking sites such as Facebook have become popular in developing nations such as Indonesia and Turkey. Given the myriad of potential Web 2.0 and social technologies, the framework can inform the decisions about which of these technologies would best further health promotion efforts amidst scarce resources. However, opportunities for health interventions are not yet apparent in low resource settings. This framework can be applied to health interventions in a range of health domains to explore how and whether available technologies can be used to support delivery of the associated types of interventions and with the target populations. The framework can also contribute to the development of more precise models that address specific device, setting, or clinical domain considerations. The framework highlights research areas for further development, and helps to inform potential research trajectories in the development of health information technologies.
Figure 1.
The three levels of consideration factors for technology selection
Acknowledgments
This work is supported by a grant from the National Institute for Nursing Research (1R21NR010710) awarded to David Kaufman. We thank Andrew Kanter, Jessica Ancker, and Yalini Senathirajah for their help in reviewing and preparing the manuscript. Connie Chan is supported by NLM predoctoral fellowship T15-LM007079.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Tomasi E, Facchini LA, Maia MFS. Health information technology in primary health care in developing countries: a literature review. Bulletin of the World Health Organization. 2004;82(11):867–74. [PMC free article] [PubMed] [Google Scholar]
- 2.Edejer TTT. Disseminating health information in developing countries: the role of the internet. 2000:797–800. doi: 10.1136/bmj.321.7264.797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brewer E, Demmer M, Du B, Ho M, Kam M, Nedevschi S, et al. The Case for Technology in Developing Regions. COMPUTER. 2005:25–38. [Google Scholar]
- 4.Odero W, Rotich J, Yiannoutsos CT, Ouna T, Tierney WM. Innovative approaches to application of information technology in disease surveillance and prevention in Western Kenya. Journal of Biomedical Informatics. 2007;40(4):390–7. doi: 10.1016/j.jbi.2006.12.007. [DOI] [PubMed] [Google Scholar]
- 5.Mamlin B, Biondich PG, Wolfe BA, Fraser H, Jazayeri D, Allen C, et al. Cooking up an open source EMR for developing countries: OpenMRS-a recipe for successful collaboration. AMIA Annu Symp Proc. 2006;529:33. [PMC free article] [PubMed] [Google Scholar]
- 6.Fraser HSF, Allen C, Bailey C, Douglas G, Shin S, Blaya J. Information systems for patient follow-up and chronic management of HIV and tuberculosis: a life-saving technology in resource-poor areas. Journal of Medical Internet Research. 2007;9(4) doi: 10.2196/jmir.9.4.e29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gustafson DH, Hawkins RP, Boberg EW, McTavish F, Owens B, Wise M, et al. CHESS: 10 years of research and development in consumer health informatics for broad populations, including the underserved. International Journal of Medical Informatics. 2002;65(3):169–77. doi: 10.1016/s1386-5056(02)00048-5. [DOI] [PubMed] [Google Scholar]
- 8.Chandrasekhar CP, Ghosh J. Information and communication technologies and health in low income countries: the potential and the constraints. Bulletin of the World Health Organization. 2001;79:850–5. [PMC free article] [PubMed] [Google Scholar]
- 9.Clifford GD, Blaya JA, Hall-Clifford R, Fraser HSF. Medical information systems: A foundation for healthcare technologies in developing countries. BioMedical Engineering OnLine. 2008;7(1):18. doi: 10.1186/1475-925X-7-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shehabuddeen N, Probert D, Phaal R. From theory to practice: challenges in operationalising a technology selection framework. Technovation. 2006;26(3):324–35. [Google Scholar]
- 11.Lee D-J, Ahn J-K. Factors affecting companies’ telecommunication service selection strategy. Omega. 2007;35(5):486–93. [Google Scholar]
- 12.Malladi S, Min KJ. Decision support models for the selection of internet access technologies in rural communities. Telematics and Informatics. 2005;22(3):201–19. [Google Scholar]
- 13.Sharif MN, Sundararajan V. A quantitative model for the evaluation of technological alternatives. Technological forecasting and social change. 1983;24(1):15–29. [Google Scholar]
- 14.Ruder KA, Pretorius MW, Maharaj BT, editors. A Technology Selection Framework for the Telecommunications Industry in Developing Countries. 2008. [Google Scholar]
- 15.Drury P. eHealth: A Model of Developing Countries. eHealth International 2005. 2005 December;2(2) [Google Scholar]
- 16.Brewer E, Demmer M, Ho M, Honicky RJ, Pal J, Plauché M, et al. The Challenges of Technology Research for Developing Regions. IEEE PERVASIVE COMPUTING. 2006:15–23. [Google Scholar]
- 17.Clark HH, Brennan SE. Grounding in communication. Perspectives on socially shared cognition. 1991:127–49. [Google Scholar]
- 18.Baur C. An Analysis of Factors Underlying E-Health Disparities. Cambridge Quarterly of Healthcare Ethics. 2008;17(04):417–28. doi: 10.1017/S0963180108080547. [DOI] [PubMed] [Google Scholar]
- 19.Kaplan WA. Can the ubiquitous power of mobile phones be used to improve health outcomes in developing countries. Globalization and Health. 2006;2(9):1744–8603. doi: 10.1186/1744-8603-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Walton M, Vukovic V. Cultures, literacy, and the web: dimensions of information” scent. interactions. 2003;10(2):64–71. [Google Scholar]
- 21.Horsky J, Zhang J, Patel VL. To err is not entirely human: Complex technology and user cognition. Journal of Biomedical Informatics. 2005;38(4):264–6. doi: 10.1016/j.jbi.2005.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Cogburn DL. HCI in the so-called developing world: what’s in it for everyone. interactions. 2003;10(2):80–7. [Google Scholar]
- 23.Blaya J, Holt B, Fraser HSF, editors. Making the eHealth Connection. Bellagio, Italy: 2008. Evaluations of the Impact of eHealth Technologies in Developing Countries: A Systematic Review. [Google Scholar]
- 24.Blaya JA, Cohen T, Rodríguez P, Kim J, Fraser HSF. Personal digital assistants to collect tuberculosis bacteriology data in Peru reduce delays, errors, and workload, and are acceptable to users: cluster randomized controlled trial. International Journal of Infectious Diseases. 2008 doi: 10.1016/j.ijid.2008.09.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan CV, Kaufman DR. Mobile phones as mediators of health behavior change in cardiovascular disease in developing countries. Studies in health technology and informatics. 2009;143:453–8. [PubMed] [Google Scholar]
- 26.Gaziano TA, Reddy KS, Paccaud F, Horton S, Chaturvedi V. Cardiovascular Disease. In: Jamison DT, Brenman JG, Measham AR, Alleyne G, Claeson M, Evans DB, et al., editors. Disease Control Priorities in Developing Countries. 2. New York: Oxford University Press and The World Bank; 2006. [Google Scholar]
- 27.Gaziano TA. Reducing The Growing Burden Of Cardiovascular Disease In The Developing World. Health Affairs. 2007;26(1):13–24. doi: 10.1377/hlthaff.26.1.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Popkin BM. Global nutrition dynamics: the world is shifting rapidly toward a diet linked with noncommunicable diseases. American Journal of Clinical Nutrition. 2006;84(2):289. doi: 10.1093/ajcn/84.1.289. [DOI] [PubMed] [Google Scholar]
- 29.Vodafone. Africa: The Impact of Mobile Phones. 2005 March; [cited 2008]; Available from: www.vodafone.com/etc/medialib/attachments/cr_downloads.Par.78351.File.dat/GPP_SIM_paper_3.pdf.
- 30.Parikh TS, Lazowska ED, editors. Designing an architecture for delivering mobile information services to the rural developing world. ACM; New York, NY, USA: 2006. [Google Scholar]
- 31.Neuhauser L, Kreps GL. Rethinking Communication in the E-health Era. Journal of Health Psychology. 2003;8(1):7. doi: 10.1177/1359105303008001426. [DOI] [PubMed] [Google Scholar]
- 32.Kikunaga S, Tin T, Ishibashi G, Wang DH, Kira S. The application of a handheld personal digital assistant with camera and mobile phone card (Wellnavi) to the general population in a dietary survey. Journal of nutritional science and vitaminology. 2007;53(2):109–16. doi: 10.3177/jnsv.53.109. [DOI] [PubMed] [Google Scholar]
- 33.Rodgers A, Corbett T, Bramley D, Riddell T, Wills M, Lin RB, et al. Do u smoke after txt? Results of a randomised trial of smoking cessation using mobile phone text messaging. British Medical Journal. 2005;14(4):255. doi: 10.1136/tc.2005.011577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsai CC, Lee G, Raab F, Norman GJ, Sohn T, Griswold WG, et al. Usability and feasibility of PmEB: a mobile phone application for monitoring real time caloric balance. Mobile Networks and Applications. 2007;12(2):173–84. [Google Scholar]
- 35.Consolvo S, Everitt K, Smith I, Landay JA. Design requirements for technologies that encourage physical activity. Proceedings of the SIGCHI conference on Human Factors in computing systems; 2006. pp. 457–66. [Google Scholar]
- 36.Vidrine DJ. Impact of a cell phone intervention on mediating mechanisms of smoking cessation in individuals living with HIV/AIDS. Nicotine & Tobacco Research. 2006;8:103–8. doi: 10.1080/14622200601039451. [DOI] [PubMed] [Google Scholar]
- 37.Vital Wave Consulting. mHealth for Development: The Opportunity of Mobile Technology for Healthcare in the Developing World. Washington, DC and Berkshire, UK: UN Foundation-Vodafone Foundation Partnership; 2009. [Google Scholar]
- 38.Planting S. Simpill Solution for TB. 2007 [updated March 2, 2007; cited 2008 August 26]; Available from: http://free.financialmail.co.za/innovations/07/0302/minn.htm.
- 39.Microsoft Corporation. Cell Phone as a Platform for Healthcare Awards. 2009 [cited 2009 August 26]; Available from: http://research.microsoft.com/en-us/um/redmond/about/collaboration/awards/cellphone-healthcare_awards.aspx.
- 40.Ma Jiao (Maggie), LeRouge Cindy, Flaherty Joseph, DeLeo G. Use Smart Phones to Promote Diabetes Self!Management: Robust Elderly in Urban and Rural China. St. Louis, MO: St. Louis University; 2008. [Google Scholar]
- 41.Donner J. Research Approaches to Mobile Use in the Developing World: A Review of the Literature. The Information Society. 2008;24(3):140–59. [Google Scholar]
- 42.Sinha C, editor. Effect of Mobile Telephony on Empowering Rural Communities in Developing Countries; Conference on Digital Divide, Global Development and the Information Society; 2005 November 14–16; Tunisia. [Google Scholar]
- 43.Mishra S, Singh IP, editors. mHealth; A Developing Country Perspective; 2008 July 13-August 8; Bellagio, Italy. [Google Scholar]
- 44.Curioso WH, Kurth AE. Access, use and perceptions regarding Internet, cell phones and PDAs as a means for health promotion for people living with HIV in Peru. BMC Medical Informatics and Decision Making. 2007;7:24. doi: 10.1186/1472-6947-7-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Piette JD, Lange I, Issel M, Campos S, Bustamante C, Sapag J, et al. Use of telephone care in a cardiovascular disease management programme for type 2 diabetes patients in Santiago, Chile. Chronic Illness. 2006;2(2):87. doi: 10.1177/17423953060020020401. [DOI] [PubMed] [Google Scholar]
- 46.Kolko BE, Rose EJ, Johnson EJ. Communication as information-seeking: the case for mobile social software for developing regions. Proceedings of the 16th international conference on World Wide Web; 2007. pp. 863–72. [Google Scholar]
- 47.Marsden G. Using HCI to leverage communication technology. interactions. 2003;10(2):48–55. [Google Scholar]
- 48.Dray SM, Siegel DA, Kotzé P. Indra’s Net: HCI in the developing world. interactions. 2003;10(2):28–37. [Google Scholar]
- 49.Chetty M, Chetty RG, editors. HCI4D: HCI Challenges in the Global South; Computer Human Interaction (CHI) 2007; April 28-May 3 2007; San Jose, CA. [Google Scholar]
- 50.Puri SK, Byrne E, Nhampossa JL, Quraishi ZB, editors. Contextuality of participation in IS design: a developing country perspective. ACM; New York, NY, USA: 2004. [Google Scholar]
- 51.Byrne E, Sahay S. Participatory design for social development: A South African case study on community-based health information systems. Information Technology for Development. 2007;13(1):71–94. [Google Scholar]