There is a growing literature that evaluates the links between the food environment and dietary intake and health outcomes.1–3 Findings are highly contingent on constructed measures of the food environment, which vary substantially across studies. Furthermore, different measures assume different underlying relationships between the food environment and individual outcomes.
The development of measures to date has focused on two dimensions: the geographic definition of the food environment, and the variety of food outlet types available in the neighbourhood. Some studies have used administrative geographical units, such as the county or census tract in which the individual resides, to define an individual’s food environment. Other studies have defined the food environment to be an area of a specific radius distance (either ‘as the crow flies’ or street network) around an individual’s residence. Regarding the variety of food outlet types, some studies have investigated the predictive value of the presence or absence of a specific outlet type. Others have considered the count or the combination of outlet types or the number of an outlet type per capita. One study in this literature has considered the association between the Retail Food Environment Index (RFEI) and obesity. 4 The RFEI was constructed by the California Center for Public Health Advocacy and is the ratio of the count of fast-food outlets and convenience stores to supermarkets and produce vendors.5 One limitation of the RFEI is directly related to its definition. Depending on the size of the geographical unit of analysis, a large number of small communities may not have a supermarket or produce vendor, which would result in an undefined RFEI. In fact, this is the case for 3719 out of 7049 (52.7%) census tracts in California.
This study proposes an alternative measure to the RFEI, called the ‘Physical Food Environment Indicator’ (PFEI), and tests its association with adult body mass index (BMI) and obesity in California. The predictive value of PFEI has been analysed at two levels: county and census tract. The PFEI is defined as:
where F, C, S, L and P are the number of fast-food restaurants, convenience stores, small food stores, supermarkets and produce vendors, respectively. Including all outlet types in the denominator reduced the fraction of all tracts in California with an undefined food index measure to 15%. Small food stores are included in the denominator as they are a potential contributor to discretionary calorie consumption and obesity risk. A recent study comparing food environments in South and West Los Angeles found that South Los Angeles (where discretionary calorie consumption and obesity prevalence is significantly greater) had a higher density of convenience and small food stores and a lower density of fast-food restaurants.6
Individual-level data were taken from the California Health Interview Survey (CHIS). The CHIS is a computer-assisted telephone interview survey that covers topics such as health status, health behaviours and healthcare access. Each wave of the survey, conducted every 2 years since 2001, is representative of the state’s non-institutionalized population in that year. The analytic data in the present study are based on the 2005 wave and include 43,020 adults aged 18 years or more. The CHIS provides information on respondents’ county and census tract, which were used to map respondents to their county- and census-tract-specific PFEI and area sociodemographic characteristics. BMI (kg/m2) was calculated from self-reported weight and height. Those with a BMI of 30 or more were classified as obese.
Measures of the food environment are constructed from InfoUSA.a Using the North American Industry Classification System, fast-food outlets were defined as franchised limited-service restaurants where patrons generally order and pay before eating. Food items that are typically sold in these establishments include hotdogs, burgers, pizza, fried chicken, subs and tacos. Supermarkets and other grocery stores with annual sales more than $1 million were classified as supermarkets, and the remainder were classified as small food stores. Produce vendors included fruit and vegetable markets. Implementing the above definitions, the PFEI was calculated for all counties and 5940 census tracts in California.b
As the dependent variables were BMI (continuous) and obesity status (binary), both linear regression and logistic regression were employed, which used robust standard errors to adjust for clustering. Two specifications were used for each model: one with county-level PFEI and the other with census-tract-level PFEI as key independent variables. The regressions also controlled for individual characteristics (gender, age, race, marital status, employment status, education level, household income level, smoking, alcohol consumption and physical activity) and area-specific characteristics (population, median household income, percentage of White residents and percentage of Black residents in census tracts). Based on the regression results, the adjusted county-level obesity rates accounting for sociodemographic differences across counties were estimated. To convey the magnitude of the effects found, the associated changes in BMI and prevalence of obesity were simulated by varying the value of PFEI while keeping all other factors constant.
Given that individuals are nested in tracts and counties, multilevel analysis was used to estimate the relative contributions of contextual and compositional factors. Building on the regression models described above, two two-level models were conducted, with one having individuals clustered within counties and the other having individuals clustered within tracts. The first specification of the multilevel models only included a random intercept in order to estimate the total variation in BMI and obesity across counties or census tracts. The second specification, where individual characteristics are added, enabled interpretation of how much of the total variation in BMI and obesity can be explained by individual factors. The third specification included all the area-level characteristics except the PFEI, and the last specification included individual characteristics, area-level characteristics and the PFEI. All statistical estimations were conducted in Stata 11.0 (Stata Corp, College Station, TX, USA).
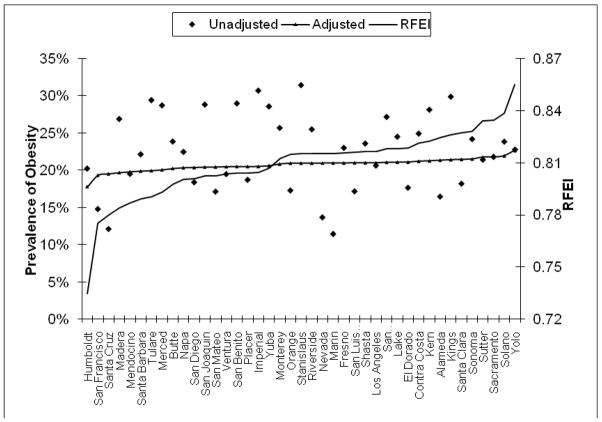
By definition, the PFEI is bounded between 0 and 1. In California, the PFEI was found to vary from 0.735 in Humboldt County to 0.855 in Yolo County. Figure 1 illustrates the PFEI and the unadjusted and adjusted prevalence of obesity across counties in California. Much of the variation in unadjusted obesity rates can be accounted for by population heterogeneity. For example, Santa Cruz (obesity rate 12.1%) has 1.2% Black population and 10.8% living in poverty compared with 9.5% and 15.4%, respectively, in San Bernardino (obesity rate 27.2%). After controlling for population heterogeneity, the adjusted prevalence of obesity continued to be positively associated with the PFEI.
Figure 1. Physical Food Environment Indicator (PFEI): unadjusted and adjusteda county-level prevalence of obesity in California.b.
RFEI, Retail Food Environment Index.
aThe adjusted rates account for all sociodemographic differences represented by the independent variables included in the regression except for the PFEI.
bThere are 58 counties in California and this figure only includes 41 counties. The other 17 counties are small and have been excluded. Generated county-level statistics of small counties are not reliable due to the sampling design of the California Health Interview Survey.
How strong is the association between the food environment and individual BMI and obesity in California? After adjusting for the covariates, tract-level PFEI was found to be predictive of a greater risk for high BMI (P<0.001) and obesity (P<0.01). The relationship between county-level PFEI and BMI (P=0.07) and obesity (P=0.05) was weaker. In the simulation to examine the magnitude of these effects, the value of the county- and tract-level PFEIs was varied and the associated changes in BMI and obesity were estimated. As shown in Table 1, the physical food environment, as measured by the PFEI, has a minimal impact on individual BMI and obesity. When the county-level PFEI increased from the 25th percentile level (0.799) to the median level (0.812) and to the 75th percentile level (0.821), the predicted obesity prevalence among women changed from 19.99% to 20.02% and 20.05%, respectively. Similar findings were obtained for the tract-level simulation and no significant differences by gender were found.
Table 1.
Simulated effects of Physical Food Environment Index (PFEI) on body mass index (BMI) and obesity by gender
| County-level PFEI |
Difference between 25th and 75th percentile | ||||
|---|---|---|---|---|---|
| 25th percentile (0.799) | Median (0.812) | 75th percentile (0.821) | |||
| Men | Mean BMI | 27.05 | 27.13 | 27.19 | 0.14 |
| Prevalence of obesity | 21.24% | 21.31% | 21.36% | 0.12% | |
| Women | Mean BMI | 25.96 | 26.04 | 26.10 | 0.14 |
| Prevalence of obesity | 19.99% | 20.02% | 20.05% | 0.06% | |
|
Tract-level PFEI |
|||||
|---|---|---|---|---|---|
| 25th percentile (0.555) | Median (0.762) | 75th percentile (0.875) | |||
| Men | Mean BMI | 27.02 | 27.11 | 27.15 | 0.13 |
| Prevalence of obesity | 21.01% | 21.49% | 21.76% | 0.75% | |
| Women | Mean BMI | 25.95 | 26.02 | 26.06 | 0.11 |
| Prevalence of obesity | 19.81% | 20.28% | 20.54% | 0.73% | |
Results for the multilevel analysis were consistent across the levels of analysis (county or tract) and outcomes of interest (BMI or obesity). This study found that 6.7% of the total variation in obesity occurs at the tract level. This fraction reduced to 3.1% with the addition of individual characteristics, to 2.1% with the addition of tract-level sociodemographic characteristics and to 1.9% with the addition of the PFEI. Overall, the variation in obesity across communities was small and more than half of it could be explained by individual characteristics. The contextual effect of the physical food environment was minimal relative to the compositional effects.
There are some potential explanations for the observed small effect of the physical food environment on BMI and obesity. First, there was little variation in food environment across tracts and counties in California, as indicated by the small changes from the 25th percentile to the 75th percentile of the PFEI. Second, on an absolute scale, there may be a threshold effect such that the PFEI is no longer predictive of health outcomes above a certain level. Third, the food environment may indeed have a limited impact on individual BMI and obesity, as suggested by this analysis. Fourth, validity of the PFEI as a measure of food environments is weak. To get deeper into this argument, sensitivity analysis was conducted using modified definitions of the RFEI. However, the results turned out to be consistently similar. Finally, the food environment could simply be a function of neighbourhood sociodemographics such that when the latter and individual characteristics are taken into account, the former no longer plays a significant role in explaining individual health outcomes.
This analysis has important limitations. The findings, although suggestive, should be interpreted carefully as the analysis is cross-sectional, and height and weight data were self-reported.7 An analysis which investigates how changes in body mass related to changes in the food environment over time may provide different insights. Factors that may influence the results but cannot be studied explicitly include the stability of the neighbourhood food environment, the length of residency, and seasonal variation that may affect food item availability and consumption patterns.
Ethical approval
This study relied on secondary data from California Health Interview Survey. All analyses were conducted at UCLA Center for Health Policy Research’s restricted data facility. Only non-identifiable aggregate results were released by the Center and used for the paper. No institutional review board approval was sought for this reason.
Acknowledgments
Funding
National Institute of Environmental Health Sciences, Grant P50ES012383.
Footnotes
InfoUSA collects information on approximately 14 million private and public US companies located by address geocoding. The data used in this paper were updated in January 2008.
The remaining 1109 census tracts do not have any fast-food restaurants, convenience stores, small food stores, supermarkets or produce vendors; therefore, the PFEI is undefined for these census tracts.
Competing interests
None declared.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.McKinnon RA, Reedy J, Morrissette MA, Lytle LA, Yoroch AL. Measures of the food environment: a compilation of the literature, 1990–2007. Am J Prev Med. 2009;36:S124–33. doi: 10.1016/j.amepre.2009.01.012. [DOI] [PubMed] [Google Scholar]
- 2.Glanz K. Measuring food environments: a historical perspective. Am J Prev Med. 2009;36:S93–8. doi: 10.1016/j.amepre.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 3.Davis B, Carpenter C. Proximity of fast-food restaurants to schools and adolescent obesity. Am J Public Health. 2009;99:505–10. doi: 10.2105/AJPH.2008.137638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.California Center for Public Health Advocacy, PolicyLink, UCLA Center for Health Policy Research. . Designed for disease: the link between local food environments and obesity and diabetes. 2008 Available at: http://www.healthpolicy.ucla.edu/pubs/Publication.aspx?pubID=250.
- 5.The California Center for Public Health Advocacy. [last accessed 15/06/2009];Searching for healthy food: the food landscape in California cities and counties. Background and methodology. Available at: http://www.publichealthadvocacy.org/searchingforhealthyfood.html.
- 6.Sturm R, Cohen D. Zoning for health? The year-old ban on new fast-food restaurants in south LA. Health Affairs. 2009;28:w1088–97. doi: 10.1377/hlthaff.28.6.w1088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jeffery RW. Bias in reported body weight as a function of education, occupation, health and weight concern. Addict Behav. 1996;21:217–22. doi: 10.1016/0306-4603(95)00050-x. [DOI] [PubMed] [Google Scholar]