Abstract
Twenty-seven Navajo adults with moderate to severe acute inflammatory diarrhea were hospitalized and randomly given ampicillin or sulfamethoxazole-trimethoprim. All patients had invasive diarrhea as defined by sheets of fecal leukocytes, seen on methylene blue wet-slide preparations, and significant clinical symptoms, including postural hypotension from dehydration or fever (temperature greater than 100 degrees F [or 37.8 degrees C]). Patients were followed daily for 5 days in the hospital. Responses of symptoms in all 13 patients who were given sulfamethoxazole-trimethoprim were comparable to or better than those 14 patients randomly assigned to receive ampicillin. Nineteen (73%) of the 27 patients had culture-proven shigellosis, 6 of whom had ampicillin-resistant Shigella isolates. All isolates were susceptible to sulfamethoxazole-trimethoprim in vitro. The eight patients with culture-proven shigellosis treated with sulfamethoxazole-trimethoprim responded as well as the eight patients with ampicillin-susceptible infections treated with ampicillin. Three of the eight patients successfully treated with sulfamethoxazole-trimethoprim had ampicillin-resistant organisms. The three patients with ampicillin-resistant organisms who were treated with ampicillin appeared to do less well; one was a clinical and bacteriological failure at 72 h and subsequently improved after sulfamethoxazole-trimethoprim therapy. As predicted by in vitro susceptibility studies and by studies in children, sulfamethoxazole-trimethoprim was highly effective in treating adult patients with shigellosis and appears to be the treatment of choice in areas where ampicillin resistance among Shigella is common.
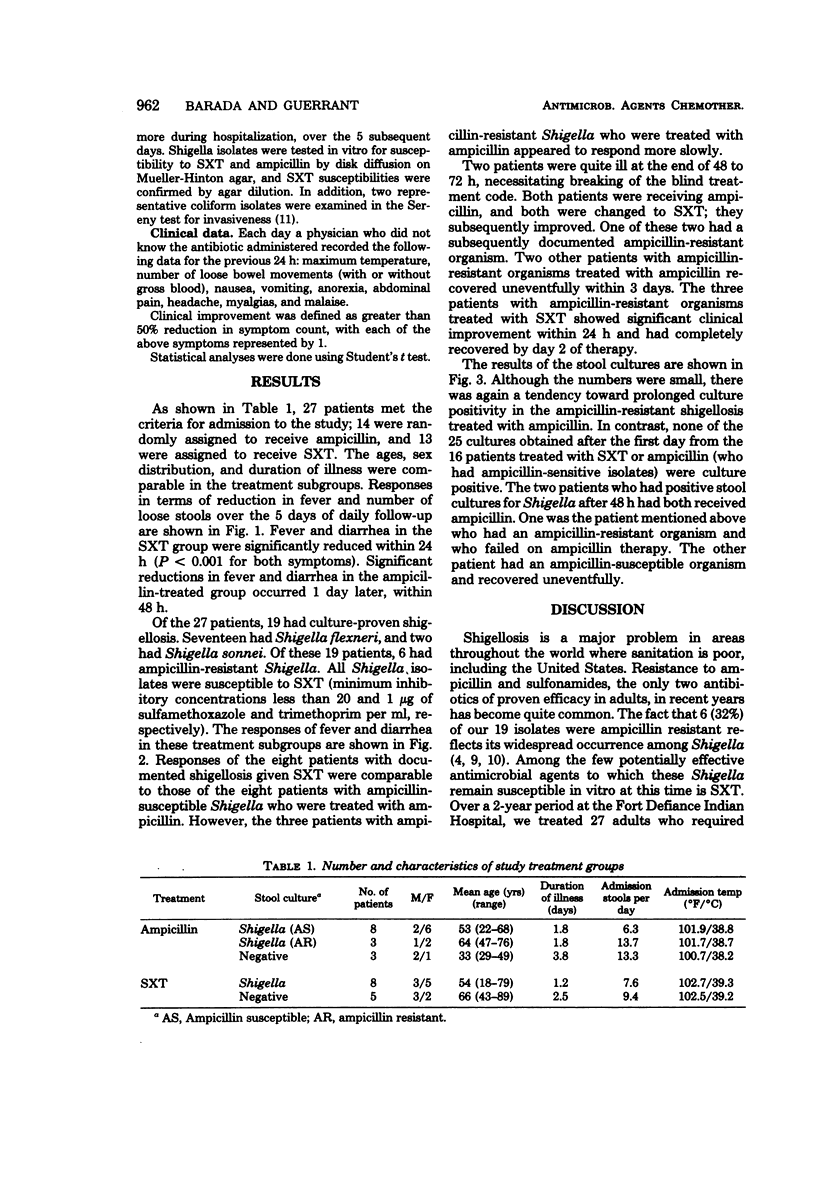
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blaser M. J., Berkowitz I. D., LaForce F. M., Cravens J., Reller L. B., Wang W. L. Campylobacter enteritis: clinical and epidemiologic features. Ann Intern Med. 1979 Aug;91(2):179–185. doi: 10.7326/0003-4819-91-2-179. [DOI] [PubMed] [Google Scholar]
- Chang M. J., Dunkle L. M., Van Reken D., Anderson D., Wong M. L., Feigin R. D. Trimethoprim-sulfamethoxazole compared to ampicillin in the treatment of shigellosis. Pediatrics. 1977 May;59(5):726–729. [PubMed] [Google Scholar]
- Haltalin K. C., Nelson J. D., Ring R., 3rd, Sladoje M., Hinton L. V. Double-blind treatment study of shigellosis comparing ampicillin, sulfadiazine, and placebo. J Pediatr. 1967 Jun;70(6):970–981. doi: 10.1016/s0022-3476(67)80275-0. [DOI] [PubMed] [Google Scholar]
- Korzeniowski O. M., Barada F. A., Rouse J. D., Guerrant R. L. Value of examination for fecal leukocytes in the early diagnosis of shigellosis. Am J Trop Med Hyg. 1979 Nov;28(6):1031–1035. doi: 10.4269/ajtmh.1979.28.1031. [DOI] [PubMed] [Google Scholar]
- Nelson J. D., Kusmiesz H., Jackson L. H. Comparison of trimethoprim-sulfamethoxazole and ampicillin theraphy for shigellosis in ambulatory. J Pediatr. 1976 Sep;89(3):491–493. doi: 10.1016/s0022-3476(76)80561-6. [DOI] [PubMed] [Google Scholar]
- Nelson J. D., Kusmiesz H., Jackson L. H., Woodman E. Trimethoprim-sulfamethoxazole therapy for shigellosis. JAMA. 1976 Mar 22;235(12):1239–1243. [PubMed] [Google Scholar]
- SERENY B. Experimental shigella keratoconjunctivitis; a preliminary report. Acta Microbiol Acad Sci Hung. 1955;2(3):293–296. [PubMed] [Google Scholar]
- Schlossberg D., McGowan J. E., Jr Letter: Shigella infection and antibiotic resistance. Ann Intern Med. 1975 Jul;83(1):120–121. doi: 10.7326/0003-4819-83-1-120_2. [DOI] [PubMed] [Google Scholar]
- Skirrow M. B. Campylobacter enteritis: a "new" disease. Br Med J. 1977 Jul 2;2(6078):9–11. doi: 10.1136/bmj.2.6078.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Then R. L., Angehrn P. Low trimethoprim susceptibility of anaerobic bacteria due to insensitive dihydrofolate reductases. Antimicrob Agents Chemother. 1979 Jan;15(1):1–6. doi: 10.1128/aac.15.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


