Abstract
RNA splicing is an increasingly recognized regulator of immunity. Here, we demonstrate that after Mycobacterium tuberculosis infection (mRNA) il12rb1 is spliced by dendritic cells (DCs) to form an alternative (mRNA) il12rb1Δtm that encodes the protein IL-12Rβ1ΔTM. Compared with IL-12Rβ1, IL-12Rβ1ΔTM contains an altered C-terminal sequence and lacks a transmembrane domain. Expression of IL-12Rβ1ΔTM occurs in CD11c+ cells in the lungs during M. tuberculosis infection. Selective reconstitution of il12rb1−/− DCs with (mRNA) il12rb1 and/or (mRNA) il12rb1Δtm demonstrates that IL-12Rβ1ΔTM augments IL-12Rβ1-dependent DC migration and activation of M. tuberculosis-specific T cells. It cannot mediate these activities independently of IL12Rβ1. We hypothesize that M. tuberculosis-exposed DCs express IL-12Rβ1ΔTM to enhance IL-12Rβ1-dependent migration and promote M. tuberculosis–specific T cell activation. IL-12Rβ1ΔTM thus represents a novel positive-regulator of IL12Rβ1-dependent DC function and of the immune response to M. tuberculosis.
The control of M. tuberculosis infection occurs through an acquired antigen-specific CD4+ T cell response and the IL12B gene is essential to this response (Cooper et al., 2007; Cooper, 2009). Although IL-12 plays an expected role in modulating Th1 responses to M. tuberculosis, we have also shown that IL-12(p40)2 is required for DCs to migrate in response to chemokines after exposure to mycobacterial and other pathogenic stimuli (Khader et al., 2006; Robinson et al., 2008). That this migration may be important in initiating T cell responses is suggested by the observation that depletion of CD11c+ cells before infection delays T cell activation and influences the outcome of infection (Tian et al., 2005).
IL-12 family members mediate their biological activities through specific, high-affinity dimeric receptors. All these receptors share IL-12Rβ1, a 100-kD glycosylated protein that spans the plasma membrane and serves as a low-affinity receptor for the IL-12p40 subunit of IL-12 family members (Chua et al., 1994, 1995); coexpression with IL-12Rβ2 or IL-23R results in high-affinity binding of IL-12 and IL-23, respectively, and confers biological responsiveness to these cytokines (Presky et al., 1996; van Rietschoten et al., 2000; Parham et al., 2002). Polymorphisms in IL12B or IL12RB1 are associated with psoriasis (Capon et al., 2007), atopic dermatitis, and other allergic phenotypes (Takahashi et al., 2005) and, importantly, nonfunctional IL12RB1 alleles predispose to mycobacterial susceptibility (Altare et al., 1998; de Jong et al., 1998; Filipe-Santos et al., 2006; Fortin et al., 2007). Thus, understanding how IL-12Rβ1 expression and IL-12Rβ1–dependent signaling is regulated has important implications for tuberculosis and may impact other diseases.
Given that CD11c+ cells contribute to the control of M. tuberculosis infection (Tian et al., 2005) and that IL-12(p40)2 is required for their migration in response to pathogenic stimuli (Khader et al., 2006; McCormick et al., 2008; Robinson et al., 2008), we sought to determine if IL-12Rβ1 is required for DC migration after exposure to this organism. In the course of these investigations we not only confirmed this hypothesis but also discovered that DCs express both IL-12Rβ1 and a novel IL-12Rβ1 splice variant (IL-12Rβ1ΔTM) in response to M. tuberculosis. This splice variant can be seen at the mRNA level in CD11c+ cells from the lungs of M. tuberculosis–infected mice and as a protein in the membrane of DCs. Importantly, we have determined that IL-12Rβ1ΔTM functions to enhance IL-12Rβ1–dependent DC migration and promote CD4+ T cell activation. This finding not only impacts our understanding of DC migration and IL-12Rβ1–dependent mycobacterial immunity it also reveals a previously unknown positive regulator of IL-12Rβ1–dependent events.
RESULTS
IL-12Rβ1 is required for M. tuberculosis–induced DC migration and function
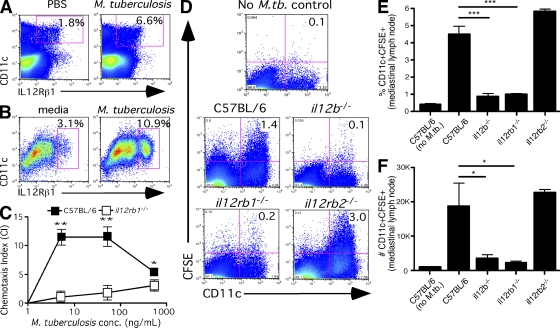
As il12b is required for DC migration in response to M. tuberculosis (Khader et al., 2006), it was necessary to determine whether il12rb1, which encodes the receptor for IL-12β (Presky et al., 1998; Wang et al., 1999; Oppmann et al., 2000), is expressed by DCs in response to M. tuberculosis and if it is required for subsequent DC migration and T cell priming. To do this, we delivered M. tuberculosis via the intratracheal route and found that the frequency of CD11c+ cells expressing IL-12Rβ1 in the lungs increases 3 h after delivery (Fig. 1 A); BM-derived DCs (BMDCs) also respond to M. tuberculosis by increasing the expression of IL-12Rβ1 on CD11c+ cells (Fig. 1 B). To test if il12rb1 was required for DC migration after mycobacterial stimulation, we generated an immature population of il12rb1−/− BMDCs and tested its ability to migrate toward the homeostatic chemokine CCL19 using a previously established method (Khader et al., 2006). il12rb1−/− DCs are morphologically and phenotypically similar to C57BL/6 DCs (unpublished data); however, in an in vitro transwell assay, il12rb1−/− DCs had a significantly lower migratory response toward CCL19 after exposure to varying concentrations of M. tuberculosis compared with C57BL/6 controls (Fig. 1 C). To determine if this was also true in vivo, we administered a mixture of M. tuberculosis and CFSE to il12b−/−, il12rb1−/−, il12rb2−/−, and C57BL/6 mice via the trachea and the number of CFSE+ CD11c+ cells in the draining mediastinal LN (MLN) was determined 18 h later. Although nonmanipulated mice of all genotypes had similar amounts of CD11c+ cells in their lung and MLN (not depicted), we consistently observed a lower frequency (Fig. 1, D and E) and fewer numbers (Fig. 1 F) of CD11c+CFSE+ cells in the MLN of il12b−/− and il12rb1−/− mice after administration via the trachea of M. tuberculosis and CFSE. This was not true of il12rb2−/− mice, further supporting a role for IL-12(p40)2, and not IL-12p70, in DC migration (Khader et al., 2006). These results demonstrate that il12rb1 is required for M. tuberculosis–induced CD11c+ cell migration from the lung to the draining MLN.
Figure 1.
IL-12Rβ1 is required for M. tuberculosis–induced DC migration. (A) M. tuberculosis was instilled into the trachea of C57BL/6 mice, and 3 h later the frequency of CD11c+IL-12Rβ1+ cells in the lungs was determined. Dot plots are representative of four mice per condition; this experiment was performed twice with two separate BM preparations. (B) C57BL/6 BMDCs were exposed to M. tuberculosis or media alone, and 3 h later the frequency of CD11c+IL-12Rβ1+ cells was determined. Dot plots represent the same BMDC preparation stimulated with either condition and are representative of three separate experiments. (C) BMDCs generated from C57BL/6 or il12rb1−/− mice were assayed for their ability to migrate to CCL19 in a transwell assay after a 3-h exposure to M. tuberculosis (CI, number moved in response to CCL19/number moved to media alone). Data points in C represent mean and SD of triplicate values and are representative of three separate experiments; for the difference between CI induced in C57BL/6 relative to il12rb1−/− DCs, *, P < 0.05; **, P < 0.005, as determined by Student’s t test. (D–F) M. tuberculosis/CFSE was instilled via the trachea into C57BL/6, il12b−/−, il12rb1−/−, or il12rb2−/− mice. 18 h later, the frequency (D and E) and total number of CD11c+CFSE+ cells in the draining MLN were counted. The data points in E and F represent the mean and SD of combined data from four mice per group (F) and are representative of two separate experiments; for the difference between percentage and/or number of CD11c+CFSE+ cells found in C57BL/6 mice relative to il12b−/− or il12rb1−/− mice, *, P < 0.05; ***, P < 0.0005, as determined by Student’s t test.
A reduced frequency of il12rb1-sufficient CD11c+ cells in the lung delays the activation of M. tuberculosis–specific T cells
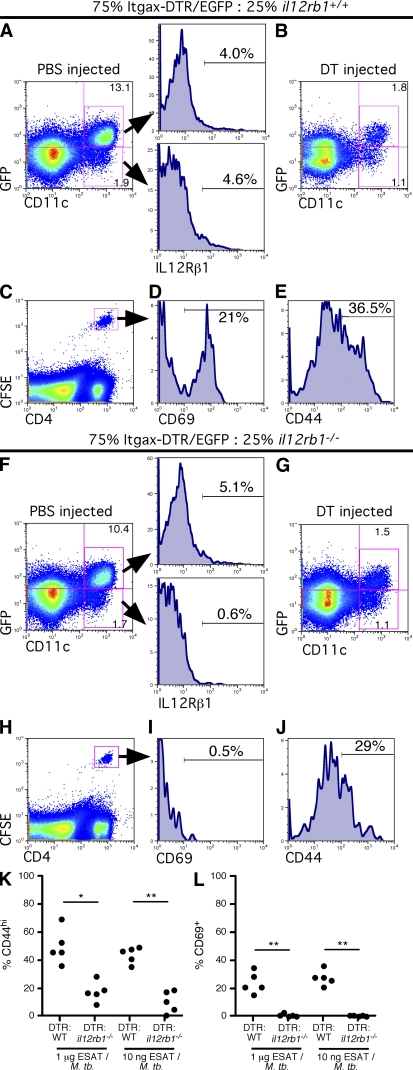
CD4+ T cell responses to M. tuberculosis antigens are initiated in the MLN (Gallegos et al., 2008; Reiley et al., 2008; Winslow et al., 2008; Wolf et al., 2008). Therefore, we speculated that a delay in CD11c+ cell migration would delay the activation of M. tuberculosis–specific CD4+ T cells. To test this idea, we used diphtheria toxin (DT) to specifically deplete il12rb1+/+ CD11c+ cells from BM chimeras that contained DT receptor–positive (DTR+) C57BL/6 CD11c+ cells and DTR-negative il12rb1−/− CD11c+ cells and measured M. tuberculosis–specific T cell activation to intratracheal administration of M. tuberculosis and antigen. The chimeras were generated by reconstituting lethally irradiated C57BL/6 mice with 25% il12rb1−/− and 75% Itgax-DTR/eGFP BM (DTR:il12rb1−/− mice) or, as a control, 25% C57BL/6 and 75% Itgax-DTR/EGFP BM (DTR:WT mice). The Itgax-DTR/eGFP mice are transgenic for a simian DTR fused to an enhanced GFP (eGFP) that is under control of the Itgax (or CD11c) promoter. Upon DT administration, CD11c+ cells containing this transgene are transiently depleted in most tissues (Jung et al., 2002).
In control DTR:WT mice injected with saline, the majority of CD11c+ cells are GFP+, demonstrating reconstitution of the lung with DTR-expressing cells (Fig. 2 A). Both GFP+ and the subset of GFP− CD11c+ cells are il12rb1+/+ and express basal levels of IL-12Rβ1 on their surface (Fig. 2 A). Upon injection of DT, the frequency of GFP+ CD11c+ cells drops ∼12-fold (Fig. 2 B), resulting in an increased ratio of GFP− to GFP+ CD11c+ cells. Treating the DTR:il12rb1−/− mice with DT resulted in a similar drop in GFP+ CD11c+ cells (Fig. 2, F and G), and therefore a greatly reduced frequency of il12rb1+/+ CD11c+ relative to il12rb1−/− CD11c+ cells in the lungs of these mice.
Figure 2.
The presence of il12rb1−/− DCs in the lung associates with impaired activation of M. tuberculosis-specific T cells in the draining MLN. Chimeras comprising 75% Itgax-DTR/EGFP:25% il12rb1+/+ or 75% Itgax-DTR/EGFP:25% il12rb1−/− were injected with either PBS (A and F) or DT (B–E and G–J). 12 h later, the frequency of CD11c+ GFP+ and CD11c+ GFP− cells remaining in the lungs after PBS injection (A and F) or DT injection (B and G) was determined. Gating based on CD11c+ GFP+ or CD11c+ GFP− cells demonstrated the level of IL-12Rβ1 surface expression (A and F). DT-injected mice subsequently received 1.5 × 106 CFSE-labeled ESAT6-specific CD4+ T cells i.v. and 1 µg ESAT61-20/50 ng irradiated M. tuberculosis via the trachea. 12 h later, the frequency of CFSE+CD4+ cells in the draining MLN (C and H) and expression levels of the activation markers CD69 (D and I) and CD44 (E and J) determined by flow cytometry. The data points in K and L represent the CD44 (K) and CD69 (L) data from 5 mice per group that received either 1 µg or 10 ng ESAT1-20 peptide with irradiated M. tuberculosis and are representative of two separate experiments with 3–4 mice per group; for the difference in %CD44hi and %CD69+ ESAT-specific CD4+ cells between the indicated groups, *, P < 0.05; **, P < 0.005, as determined by Student’s t test.
To compare the relative T cell–activating ability of lungs harboring a high frequency of il12rb1+/+ CD11c+ cells to those with a low frequency, we measured the response of antigen-specific cells in the MLN. To do this, we intravenously transferred 1.5 × 106 CFSE-labeled ESAT-specific CD4+ T cells into DT-injected DTR:WT or DTR:il12rb1−/− mice immediately before instillation via the trachea of ESAT61-20 peptide and 1 µg of irradiated M. tuberculosis. 18 h later, the frequency of ESAT-specific T cells (Fig. 2, C and H) expressing markers of activation CD69 (Fig. 2, D and I) and CD44 (Fig. 2, E and J) in the draining MLN was determined. The frequency of ESAT6-specific T cells that expressed a high level of CD44 (Fig. 2 K) and CD69 (Fig. 2 L) in response to two different doses of antigen within the 18 h of the experiment was significantly lower in the mice with a reduced frequency of il12rb1+/+ CD11c+ cells. Thus, an increase in the ratio of il12rb1−/− to il12rb1+/+ DCs in the lungs is associated with impaired activation of antigen-specific T cells in the draining MLN. These data demonstrate that il12rb1 expression in CD11c+ cells within the lung is required for M. tuberculosis–induced DC migration and induction of T cell activation in vivo.
IL-12(p40)2 initiates nuclear accumulation of NF-κB in DCs
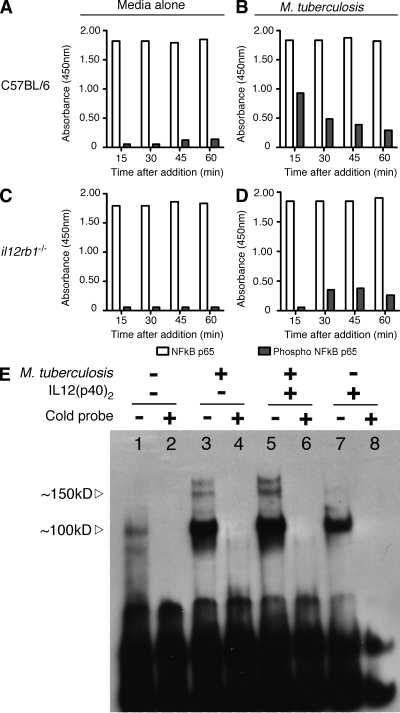
We wished to better understand the mechanism by which IL-12Rβ1–dependent signaling modulates DC chemotaxis after exposure to M. tuberculosis. Lower levels of CCR7 (the receptor for CCL19) do not account for this result, as surface expression of CCR7 is similar between activated WT and il12rb1−/− BMDCs (unpublished data). To determine if any intracellular signaling pathways that influence DC migration were altered in il12rb1−/− DCs, we measured the phosphorylation levels of NF-κB, SAPK/JNK, p38α MAP kinase, and STAT3 in these cells after stimulation with M. tuberculosis. We observed that stimulation of C57BL/6 DCs increases phospho-NF-κB levels above those of unstimulated controls (Fig. 3, A and B). However, we consistently observed that levels of phospo-NF-κB were lower in il12rb1−/− DCs compared with WT DCs at several time points, despite equivalent levels of total NF-κB (Fig. 3, C and D). No differences in phospho-SAPK/JNK, p38α MAP kinase, and STAT3 were observed between WT and il12rb1−/− DCs (unpublished data). These data suggest that NF-κB–dependent processes are compromised in il12rb1−/− DCs
Figure 3.
NF-κB signaling is impaired in il12rb1−/− DCs and can be promoted by IL-12(p40)2. (A-D) BMDCs generated from C57BL/6 and il12rb1−/− mice were exposed to M. tuberculosis (B and D) or media alone (A and C) for the indicated times. After this period, cells were harvested under nondenaturing conditions and levels of total NF-κB p65 (open bars) and phospho-NF-κB p65 (closed bars) were determined by ELISA. Shown are the light absorbance values (A450) from one experiment that is representative of two experiments with separate BMDC preparations. (E) BMDCs were generated from il12b−/− mice and exposed to media alone, M. tuberculosis, IL-12(p40)2, or both M. tuberculosis and IL-12(p40)2. 1 h later, nuclear extracts of the treated cells were isolated and EMSA of NF-κB consensus sequence-binding proteins was performed. Shown is a blot of NF-κB consensus sequence-binding proteins from DCs stimulated with media alone (lanes 1 and 2), M. tuberculosis (lanes 3 and 4), both M. tuberculosis and IL-12(p40)2 (lanes 5 and 6) or IL-12(p40)2 alone (lanes 7 and 8). The absence (−) or presence (+) of a cold NF-κB consensus probe was used to determine the specificity of each band.
Because NF-κB phosphorylation was defective in il12rb1−/− DCs, we reasoned that NF-κB binding should be enhanced when DCs are stimulated via IL-12Rβ1. To test this hypothesis, we exposed il12b−/− BMDC to M. tuberculosis and/or IL-12(p40)2 for 1 h, and, using electromobility shift assay (EMSA), compared the amount of NF-κB consensus sequence-binding proteins in nuclear extracts of the treated cells. il12b−/− BMDCs were used for this experiment to eliminate potential background NF-κB activation from endogenous IL-12(p40)2. Fig. 3 E demonstrates that the addition of M. tuberculosis to DC cultures increases the nuclear accumulation of NF-κB over that seen in untreated BMDCs (Fig. 3 E, compare lanes 1 and 3). IL-12(p40)2 was also sufficient to increase the nuclear accumulation of NF-κB over that seen in untreated BMDCs (Fig. 3 E, compare lanes 1 and 7). The addition of both M. tuberculosis and IL-12(p40)2 synergistically augmented NF-κB activation above that of each stimulus alone (Fig. 3 E, compare lanes 3 and 7 to lane 5). Thus, our data demonstrate that IL-12(p40)2 is able to stimulate NF-κB nuclear migration in DCs. Consequently, the failure of il12rb1−/− DCs to migrate (Figs. 1 and 2) associates with impaired NF-κB–dependent gene activation.
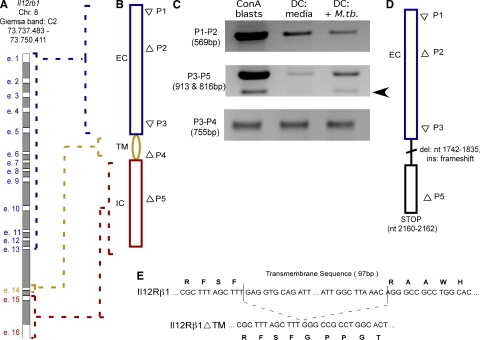
BMDCs express (mRNA) il12rb1 and an (mRNA) il12rb1 alternative splice variant after exposure to M. tuberculosis
The expression of (mRNA) il12rb1 by DCs has not been universally accepted because of an inability to reproducibly detect this transcript (Grohmann et al., 1998). However, given the influence of il12rb1 on DC migration (Figs. 1 and 2), we reexamined (mRNA) il12rb1 expression in these cells. The mouse il12rb1 gene is located on autosomal chromosome 8 and comprises 16 exons (Fig. 4 A; NCBI protein database accession no. 16161). Upon transcription and intron removal, exons 1–13 are translated into the extracellular portion of the IL-12Rβ1 protein, whereas exon 14 and exons 15–16 are translated into the transmembrane and intracellular portions, respectively (Fig. 4 B). To determine the transcription activity of this gene in DCs, we amplified cDNA from BMDC cultures with a variety of primers spanning different lengths of (cDNA) il12rb1 (Fig. 4 B). Amplification with primers (P) recognizing the extracellular-encoding region (P1–P2) resulted in an amplicon (Fig. 4 C; cDNA from concanavalin-A–activated splenocytes is used as a positive control). Amplification of a more 3′ region with primers P3–P5 also resulted in a PCR product in both unstimulated and stimulated DCs; however, under these amplification conditions a second smaller band was also observable, but only in DCs that had been stimulated with M. tuberculosis (Fig. 4 C, arrow). This second band does not appear upon amplification with primers that span the transmembrane-encoding region (P3-P4). Sequencing both the larger and smaller band amplified by primers P3–P5 revealed that the larger product represents (mRNA) il12rb1 and that the smaller product is identical, except for a 97-bp deletion (Fig. 4 D). This deletion has two effects: (1) deletion of the transmembrane sequence encoded by exon 14 and (2) a translational frame shift that results in an early stop codon. This translational frame shift also results in the loss of the Box1/2 signaling domains that are found in the IL-12Rβ1 protein (van de Vosse et al., 2003). Both the nucleotide and deduced amino acid sequence of this smaller band (Fig. 4 E) match that of a previously reported alternative splice variant of the mouse IL-12Rβ1 transcript (Chua et al., 1995). Thus, DCs respond to M. tuberculosis by expressing two species of (mRNA) il12rb1: a transmembrane-containing transcript (hereafter referred to as “(mRNA) il12rb1”) and an alternatively spliced variant of (mRNA) il12rb1 (hereafter referred to as “(mRNA) il12rb1Δtm”).
Figure 4.
DCs express an IL-12Rβ1 alternative splice variant after exposure to M. tuberculosis. (A) The genomic position and organization of the murine il12rb1 locus. Exons 1–16 are denoted e.1-e.16. (B) Upon transcription and intron removal, e.1-13 become the extracellular-encoding (EC) portion of the IL-12Rβ1 transcript, e.14 the transmembrane-encoding (TM) portion, and e15-16 the intracellular-encoding (IC) portion. Shown to the right of the transcript are the relative positions of primers 1–5 (P1-P5; Δ indicates a forward primer and ▽ indicates a reverse primer) used for amplification of IL-12Rβ1 cDNA from the indicated cell populations (C). (D-E) Sequencing of the smaller amplicon of P3-P5 (indicated by arrow) reveals an IL-12Rβ1 alternative splice variant that contains both a 97-bp deletion and (E) a frameshift insertion that eventually produces a premature stop codon. This experiment has been repeated three times with three separate BMDC preparations.
Kinetics of BMDC (mRNA) il12rb1Δtm expression after exposure to M. tuberculosis
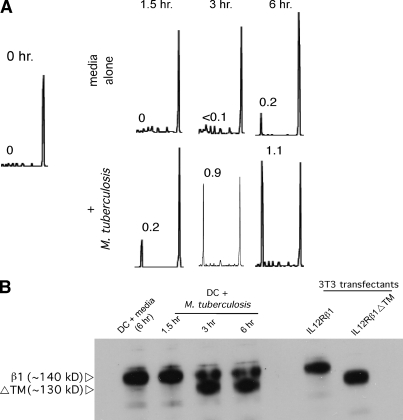
As (mRNA) il12rb1Δtm was induced in BMDCs by M. tuberculosis, we wished to quantify its expression; however, it proved difficult to design a Taqman real-time PCR probe that recognized (cDNA) il12rb1Δtm and not (cDNA) il12rb1. Thus, to better quantify the kinetics of (mRNA) il12rb1Δtm expression relative to (mRNA) il12rb1 in M. tuberculosis–stimulated DCs, we developed a PCR-based assay hereafter referred to as “IL-12Rβ1 spectratype analysis.” IL-12Rβ1 spectratype analysis is akin to TCR-CDR3 spectratype analysis (Pannetier et al., 1993) and is described in Fig. S1. When IL-12Rβ1 spectratype analysis was applied to BMDCs, we observed a dose-dependent increase in the ratio of (mRNA) il12rb1Δtm to (mRNA) il12rb1 after a 3-h exposure to M. tuberculosis (Fig. 5 A). In contrast (mRNA) il12rb1 remains the dominant transcript in unstimulated DCs for up to 6 h (Fig. 5 A). Western blot analysis demonstrated that IL-12Rβ1 is the dominant protein product in unstimulated cells, whereas IL-12Rβ1ΔTM increases in abundance after M. tuberculosis stimulation (Fig. 5 B). That IL-12Rβ1ΔTM could locate in the membrane was indicated by Western blot analysis of cellular fractions (Fig. S1 H). Thus, analysis of mRNA and Western blot analysis confirm that DCs increase the expression of il12rb1Δtm and production of IL-12Rβ1ΔTM after exposure to M. tuberculosis.
Figure 5.
IL-12Rβ1 Spectratype analysis of M. tuberculosis-activated DCs. (A) C57BL/6 BMDCs were stimulated over a period of 6 h with media alone or M. tuberculosis. Shown are representative IL-12Rβ1 spectratype data from these DCs before culture (0 h) and after 1.5, 3, or 6 h of culture. The numbers adjacent to peaks of an individual IL-12Rβ1 spectra indicate the relative ratio of that peak’s area (the smaller peak representing IL-12Rβ1ΔTM) to the area of the larger peak that represents IL-12Rβ1. Spectra are representative of four BMDC cultures per condition; this experiment was performed twice. (B) Denaturing Western blot analysis of the same cells to confirm changing protein levels of IL-12Rβ1 and IL-12Rβ1ΔTM; NIH/3T3 cells transfected with the indicated plasmid constructs served as positive controls; blots were probed with polyclonal anti-IL-12Rβ1.
To assess the specificity of (mRNA) il12rb1 splicing in response to M. tuberculosis, we stimulated DCs with a variety of other microbial and cytokine stimuli. Specifically, DCs were stimulated with Mycobacterium avium and Yersinia pestis at an identical MOI, as well as with M. avium cell wall extract, Escherichia coli LPS, TNF, IL-12, and IL-12(p40)2; production of IL-12Rβ1ΔTM was subsequently assessed by IL-12Rβ1 Spectratype analysis. Both M. avium and Y. pestis were capable of activating DCs as measured by IL-12p40 production (Fig. S2 A). As shown in Fig. S2 B, over a 6-h incubation M. avium was capable of eliciting IL-12Rβ1ΔTM production with kinetics that were similar to that elicited by M. tuberculosis. This was also observed with M. avium cell wall extract (Fig. S2 C). Stimulation with Y. pestis and purified LPS (Fig. S2, D and E) failed to generate IL-12Rβ1ΔTM over the same 6-h period. Production of IL-12Rβ1ΔTM protein was also not observed after stimulation of DCs with varying Y. pestis MOI (Fig. S2 I). Negative results were also obtained with TNF, IL-12, and IL-12(p40)2–stimulated DCs (Fig. S2, F–H). Thus, DCs increase the expression of il12rb1Δtm in response to M. tuberculosis and the related organism M. avium, but not upon stimulation with Gram-negative Y. pestis, purified LPS, and cytokines TNF, IL-12, and IL-12(p40)2.
Human DCs respond to stimuli by splicing IL-12Rβ1
After activation, human DCs increase surface expression of IL-12Rβ1 (Nagayama et al., 2000). Two isoforms of the human IL-12Rβ1 transcript are reported in publicly available databases: full-length IL-12RB1 (isoform 1; Swiss-Prot ID P42701-1) and a shorter isoform, missing the transmembrane domain and with an altered C-terminal amino-acid sequence that is the product of alternative splicing (isoform 2; Swiss-Prot P42701-3; sequences available at http://www.uniprot.org/uniprot/P42701; Fig. S3, A and B). To determine if human DCs splice the IL-12Rβ1 transcript after stimulation in a manner that is analogous to mouse DCs, we exposed monocyte-derived DCs to a variety of stimuli, some of which are known inducers of DC IL-12Rβ1 expression (Nagayama et al., 2000). We then assessed the relative levels of transcripts for IL-12Rβ1 isoforms 1 and 2 using specific primers; cDNA from CD3+ PBMCs was used as a positive control. All samples expressed IL-12Rβ1 when assayed with primers that recognized both isoforms 1 and 2 (Fig. S3 C, top). However, amplification with primers specific to either isoform 1 (Fig. S3 C, middle) or isoform 2 (Fig. S3 C, bottom) revealed that these two transcripts were differentially expressed depending on the stimulus. Specifically, the production of isoform 2 was strongly associated with exposure to LPS, IL-1β, IL-2, and CCL3. Stimulation of human DCs with M. tuberculosis also elicited expression of IL-12Rβ1 isoform 2 over a 6-h time course (Fig. S3 D). We conclude from these experiments that human DCs, like mouse DCs, respond to specific stimuli by splicing the IL-12Rβ1 transcript.
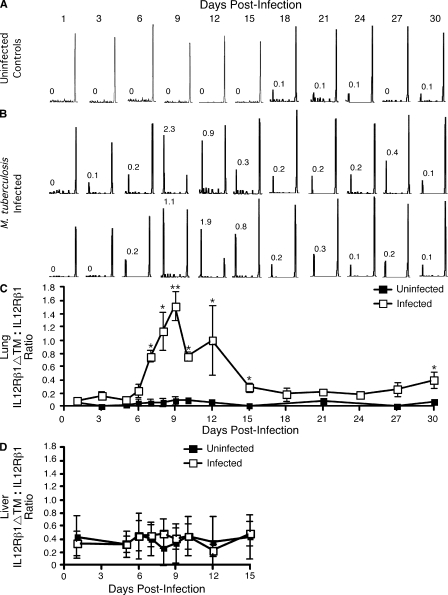
(mRNAs) il12rb1 and il12rb1Δtm are expressed by CD11c+ cells in the M. tuberculosis–infected lung
We next asked whether (mRNA) il12rb1Δtm is expressed in response to M. tuberculosis infection in vivo. To assess this, a time course of (mRNA) il12rb1Δtm abundance relative to (mRNA) il12rb1 in mice aerogenically infected with M. tuberculosis was performed. In uninfected controls, the expression of (mRNA) il12rb1Δtm was minimal over the entire 30-d period, with (mRNA) il12rb1 being the dominant transcript observed (Fig. 6 A). In M. tuberculosis–infected animals, however, a shift in the ratio of (mRNA) il12rb1Δtm to (mRNA) il12rb1 in the lung is observed at 9 d after infection (Fig. 6 B), with (mRNA) il12rb1Δtm reaching 2.3-fold higher in abundance than (mRNA) il12rb1 in some cases. After 9–12 d, the ratio of (mRNA) il12rb1Δtm to (mRNA) il12rb1 in the lung diminished, but still remained higher than that of uninfected controls up to day 30. This result was observed in several independent experiments (Fig. 6 C). In the liver, an organ distal to the initial site of infection, we observed elevated baseline levels of (mRNA) il12rb1Δtm expression compared with the lung (Fig. 6 D); however, these levels remained unchanged through the early course of M. tuberculosis infection (Fig. 6 D). In summary, (mRNA) il12rb1Δtm is expressed subsequent to M. tuberculosis infection in vivo—the relative ratio to (mRNA) il12rb1 being dependent on time after infection.
Figure 6.
IL-12Rβ1ΔTM is expressed in the M. tuberculosis-infected lung. C57BL/6 mice were aerogenically infected with 100 CFU M. tuberculosis. At the indicated times after infection the lungs of both (A) uninfected and (B) infected mice were harvested for IL-12Rβ1 spectratype analysis. Shown are representative spectra from (A) one individual uninfected mouse at each indicated time point or (B) two individual M. tuberculosis-infected mice from each time point. The numbers adjacent to peaks of an individual IL-12Rβ1 spectra indicate the relative ratio of that peak’s area (the smaller peak representing IL-12Rβ1ΔTM) to the area of the larger peak that represents IL-12Rβ1. (C) The ratio of IL-12Rβ1ΔTM to IL-12Rβ1 expressed in the lung of uninfected and M. tuberculosis-infected animals. (D) The ratio of IL-12Rβ1ΔTM to IL-12Rβ1 expressed in the liver of uninfected and M. tuberculosis-infected animals. Data points in C and D represent the mean and SD of the IL-12Rβ1ΔTM to IL-12Rβ1 ratios expressed in 4–8 individual mice per time point and are combined from two separate experiments; for the difference between infected lungs relative to uninfected lungs, *, P < 0.05; **, P < 0.005, as determined by Student’s t test.
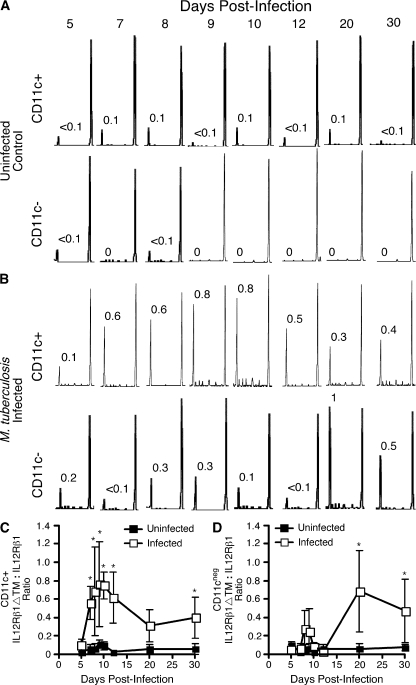
The expression of IL-12Rβ1ΔTM by DCs in vitro (Fig. 5) and by the M. tuberculosis–infected lung in vivo (Fig. 6) prompted us to determine whether CD11c+ cells from M. tuberculosis–infected lungs are the source of this transcript. To do this, CD11c+ cells from the lungs of M. tuberculosis–infected mice were isolated by magnetic beads at various time points after infection and expression of (mRNA) il12rb1Δtm was determined as described in Fig. 6. CD11c+ cells from M. tuberculosis–infected mice consistently expressed a higher ratio of (mRNA) il12rb1Δtm to (mRNA) il12rb1 compared with those isolated from uninfected controls, the highest being observed at 7–12 d after infection (compare top panels of Fig. 7, A and B). Notably, the CD11c− cells from M. tuberculosis–infected mice also expressed a higher ratio of (mRNA) il12rb1Δtm to (mRNA) il12rb1 compared with uninfected controls, the highest being observed at 20 and 30 d after infection (compare bottom panels of Fig. 7, A and B). This result was observed in several independent experiments (Fig. 7 C-D). These data demonstrate that after low-dose aerogenic M. tuberculosis infection, lung CD11c+ cells exhibit increased expression of (mRNA) il12rb1Δtm and that CD11cneg cells can also express this transcript as infection progresses.
Figure 7.
Lung CD11c+ and CD11c− populations increase IL-12Rβ1ΔTM expression after M. tuberculosis infection. C57BL/6 mice were aerogenically infected with 100 CFU M. tuberculosis. At the indicated times after infection lung CD11c+ and CD11c− populations were magnetically separated from both (A) uninfected and (B) infected mice. Subsequently generated cDNA was used for IL-12Rβ1 spectratype analysis. Shown are representative spectra expressed by CD11c+ and CD11c− cells from (A) an individual uninfected mouse at each time point or (B) an individual M. tuberculosis—infected mouse at each time point. The numbers adjacent to peaks of an individual IL-12Rβ1 spectrum indicate the relative ratio of that peak’s area (the smaller peak representing IL-12Rβ1ΔTM) to the area of the larger peak that represents IL-12Rβ1. Spectra are representative of four mice per time point. (C) The ratio of IL-12Rβ1ΔTM to IL-12Rβ1 expressed by lung CD11c+ cells from uninfected and M. tuberculosis—infected animals. (D) The ratio of IL-12Rβ1ΔTM to IL-12Rβ1 expressed by lung CD11c- cells from uninfected and M. tuberculosis-infected animals. Data points in (C and D) represent the mean and SD of the IL-12Rβ1ΔTM to IL-12Rβ1 ratios expressed in four individual mice per time point; for the difference between the indicated populations from infected lungs relative to uninfected lungs, *, P < 0.05, as determined by Student’s t test.
Similar to M. tuberculosis, M. avium and Y. pestis are lung-tropic intracellular pathogens. Because exposure to M. avium, but not Y. pestis, increased DC expression of (mRNA) il12rb1Δtm, we next determined if (mRNA) il12rb1Δtm was also expressed in the M. avium– or Y. pestis–infected lung. For this, mice were aerogenically infected with M. avium (Fig. S4 A) or intranasally with Y. pestis KIMD27 (Fig. S4 C) and a time course of (mRNA) il12rb1Δtm abundance relative to (mRNA) il12rb1 was performed. As with M. tuberculosis, we observed a shift in the ratio of (mRNA) il12rb1Δtm to (mRNA) il12rb1 in the lung at 8 d after infection with M. avium (Fig. S4 B). Despite similar numbers of CFU at 4 d after infection, only one out of five Y. pestis–infected animals showed expression of (mRNA) il12rb1Δtm (Fig. S4 D, top). Negative results were also obtained upon infection with the more immunostimulatory strain Y. pestis KIMD27/pLpxL (Robinson et al., 2008; Fig. S4 D, bottom). Thus, although M. tuberculosis (Fig. 6) and M. avium induce expression of (mRNA) il12rb1Δtm in the lungs, Y. pestis does not.
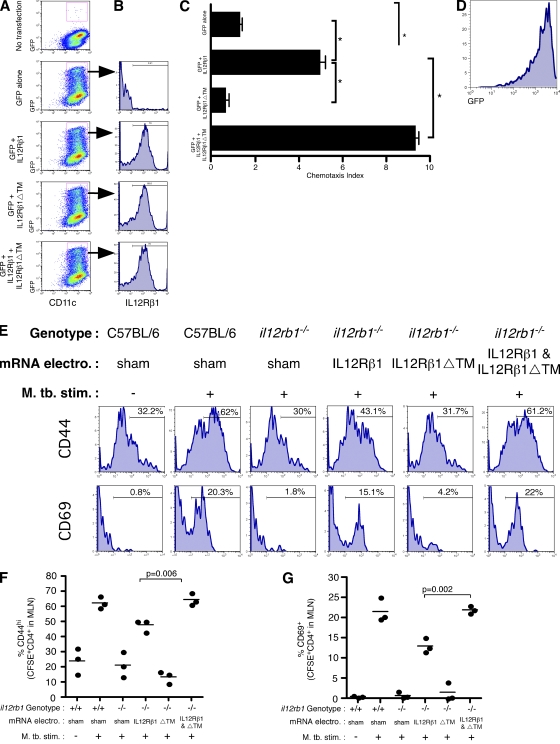
IL-12Rβ1ΔTM enhances IL-12Rβ1–dependent migration
DCs exhibit IL-12(p40)2– and il12rb1–dependent migration in response to M. tuberculosis after only a 3-h exposure to this organism (Fig. 1 C; Khader et al., 2006; Robinson et al., 2008). Given that (mRNA) il12rb1Δtm is generated and translated within this timeframe (Fig. 5), we investigated whether IL-12Rβ1ΔTM contributed to M. tuberculosis–induced, IL-12(p40)2–dependent DC migration. To do this, we selectively restored mRNAs that encode IL-12Rβ1, IL-12Rβ1ΔTM, or both IL-12Rβ1 and IL-12Rβ1ΔTM to il12rb1−/− DCs, which contain a genomic neo insertion that disrupts exons 1–3 of the il12rb1 locus (Wu et al., 1997) and thus lack both these proteins (Fig. 4). We co-transfected GFP encoding mRNA with the specific mRNAs via electroporation and found that an antibody specific for the common extracellular portion of the IL-12Rβ1 and IL-12Rβ1ΔTM only labeled GFP+ CD11c+ cells if mRNAs for either IL-12Rβ1 or IL-12Rβ1ΔTM were delivered to the il12rb1−/− DCs (Fig. 8, A and B). After stimulation with M. tuberculosis, il12rb1−/− DCs transfected with GFP and IL-12Rβ1 were capable of migrating toward CCL19 whereas those transfected with GFP alone were not (Fig. 8 C). il12rb1−/− DCs transfected with GFP and IL-12Rβ1ΔTM had migratory levels equivalent to those transfected with GFP alone. However, cotransfection with GFP, IL-12Rβ1 and IL-12Rβ1ΔTM resulted in a greater chemotaxis index than when DCs were transfected with GFP and IL-12Rβ1. The majority of migrated cells were GFP+, suggesting that migration required transfection of the migrating cell and was not an indirect effect (Fig. 8 D). These data demonstrate that IL-12Rβ1ΔTM can enhance IL-12Rβ1–dependent DC migration.
Figure 8.
IL-12Rβ1ΔTM enhances IL-12Rβ1-dependent migration. (A–D) il12rb1−/− CD11c+ BMDCs were transfected with mRNAs encoding either GFP, GFP and IL-12Rβ1, GFP and IL-12Rβ1ΔTM, or GFP and IL-12Rβ1 and IL-12Rβ1ΔTM. 24 h later, (A) cells were analyzed by flow cytometry for GFP expression among CD11c+ cells and (B) expression of transfected IL-12Rβ1 was examined by gating on GFP+CD11c+ cells. (C) The migratory ability of DCs transfected with the indicated mRNAs was assessed as performed in Fig. 1 C. Data points represent the mean and SD of the combined data from three separate experiments with different BM preparations per experiment. For the difference between CI induced in the indicated groups, *, P < 0.05, as determined by Student‘s t test. (D) Flow cytometric analysis of those cells that had migrated and transfected with GFP and IL-12Rβ1 and IL-12Rβ1ΔTM demonstrates that the migratory DCs from this group were mostly GFP+. (E) We compared the ability of il12rb1−/− DCs transfected with indicated mRNAs to activate M. tuberculosis-specific T cells in vivo; sham-transfected C57BL/6 DCs were used as a positive control. After transfection the indicated DCs populations were cultured with M. tuberculosis and ESAT1-20 peptide; after this they were instilled via the trachea into C57BL/6 mice containing transferred CFSE-labeled ESAT-specific CD4+ cells. Shown are histograms of CD44 and CD69 expression on CFSE+CD4+ 12 h later in the draining MLN. Each histogram is representative of four mice per condition. (F and G) The combined (F) CD44 and (G) CD69 data gated on CFSE+CD4+ in the draining MLN are shown; these data are representative of two independent experiments with three to four mice per group.
Finally, given that IL-12Rβ1ΔTM enhanced IL-12Rβ1-dependent DC migration in vitro, we determined whether its expression in DCs accelerated the activation of M. tuberculosis-specific T cells in vivo. il12rb1−/− BMDCs were selectively restored with mRNAs for IL-12Rβ1, IL-12Rβ1ΔTM, or both IL-12Rβ1 and IL-12Rβ1ΔTM as described in Fig. 8. After their electroporation and overnight culture, DCs were cultured with irradiated M. tuberculosis and ESAT1-20 peptide for 3 h. After this period, DCs were washed and instilled via the trachea into the lungs of C57BL/6 mice that had previously received 5 × 106 CFSE-labeled ESAT-TCR CD4+ cells. 12 h after DC instillation, the surface expression of CD44 and CD69 by CFSE+CD4+ cells in the draining MLN was assessed by flow cytometry. As anticipated, mice that received sham electroporated il12rb1−/− DCs had fewer activated M. tuberculosis–specific T cells in the draining MLN relative to those that received sham electroporated C57BL/6 DCs (Fig. 8 E). Restoration of IL-12Rβ1 alone to il12rb1−/− DCs elevated the frequency of CD44hi and CD62Llo M. tuberculosis–specific T cells; however, restoring IL-12Rβ1ΔTM alone to il12rb1−/− DCs did not elevate the frequency of activated M. tuberculosis-specific T cells. Importantly, only when both IL-12Rβ1 and IL-12Rβ1ΔTM were restored to il12rb1−/− DCs did the frequency of activated M. tuberculosis-specific T cells return to the level seen in mice that received C57BL/6 DCs. This result was observed across several independent experiments (Fig. 8, F and G). These data demonstrate that IL-12Rβ1ΔTM can enhance IL-12Rβ1–dependent DC migration from the lung and activation of M. tuberculosis–specific T cells in the lung draining MLN.
DISCUSSION
DCs are pivotal for initiating immunity to M. tuberculosis and other diseases of the pulmonary tract (Tian et al., 2005; Lambrecht, 2008), and they have been shown to transport M. tuberculosis from the lungs to the MLN (Wolf et al., 2007). IL-12 family members are secreted by DCs after Mtb stimulation (Jang et al., 2008) and are required for their ability to generate an efficient T cell response (Zhang et al., 2003; Khader et al., 2006). Here, we demonstrate that after their encounter with M. tuberculosis, DCs express IL-12Rβ1 and an IL-12Rβ1 splice variant that we have termed “IL-12Rβ1ΔTM.” In contrast to IL-12Rβ1, IL-12Rβ1ΔTM contains an altered C-terminal sequence and lacks a transmembrane domain; nevertheless, IL-12Rβ1ΔTM is still membrane associated. Selective reconstitution of il12rb1−/− DCs with IL-12Rβ1 and/or IL-12Rβ1ΔTM demonstrates that IL-12Rβ1ΔTM augments IL-12Rβ1-dependent DC migration; however, it cannot substitute for IL-12Rβ1. Importantly, after M. tuberculosis infection of the lung, CD11c+ cells in this organ express IL-12Rβ1ΔTM. Further, reconstitution of il12rb1−/− DCs with IL-12Rβ1 and IL-12Rβ1ΔTM accelerates in vivo CD4+ T cell activation compared with il12rb1−/− DCs reconstituted with IL-12Rβ1 alone. Thus, we propose that in response to M. tuberculosis DCs express IL-12Rβ1ΔTM, a novel positive regulator of IL-12Rβ1–dependent signaling, and that this enhances IL-12Rβ1–dependent migration and M. tuberculosis–specific CD4+ T cell activation.
Alternative splicing is emerging as an important regulator of immunity (Lynch, 2004). It is estimated that >75% of human genes undergo alternative splicing, many of which are exclusively expressed by the immune system (Johnson et al., 2003). The list of proteins regulated by splicing includes those involved in intracellular signaling cascades (i.e., Fyn and Syk), membrane adhesion (i.e., CD31, CD44, and CD54), and cell activation (i.e., CD45 and CD152; Lynch, 2004). Alternatively spliced cytokine receptors can regulate inflammatory events by functioning as either agonists or antagonists of cytokine signaling (Levine, 2004). The list of alternatively spliced cytokine receptors include members of the class I cytokine receptor superfamily (IL-4R, IL-5R, IL-6R, IL-7R, IL-9R, EpoR, GCSFR, GMCSFR, gp130, and LIFR), class II cytokine receptor superfamily (IFNAR1 and IFNAR2), IL-1/TLR family (IL-1RII and IL-1RAcP), TGF receptor family (TRI and activin receptor-like kinase 7), and TNFR superfamily (TNFRSF6/Fas/CD95, TNFRSF9/4-1BB/CD137, and IL-17R; Levine, 2004).
To this list of spliced and functioning cytokine receptors we can now add IL-12Rβ1ΔTM. The mouse IL-12Rβ1 and IL-12Rβ1ΔTM cDNAs were originally cloned based on their nucleotide homology to human IL-12Rβ1 (Chua et al., 1995). When transfected into COS cells, both cDNAs produced proteins that bind [125I]IL-12 with similar low affinities, suggesting that IL-12Rβ1 and IL-12Rβ1ΔTM were both expressed on the cell surface (Chua et al., 1995). However, no function had or has been ascribed to IL-12Rβ1ΔTM since that time. Here, we have demonstrated that although mouse IL-12Rβ1ΔTM cannot substitute for IL-12Rβ1, it can function in DCs to enhance IL-12(p40)2– and IL-12Rβ1–dependent migration. That this may be relevant to our understanding of human DC biology is suggested by our observation that human PBMC-derived DCs also respond to stimulation by splicing (mRNA) IL12RB1 to generate a protein with similar characteristics as the mouse variant. Curiously, for humans, the stimuli that elicit (mRNA) IL12RB1 splicing are broader in origin than for mice. Whether human IL-12Rβ1ΔTM performs the same function in human DCs should certainly be investigated. It should be mentioned that IL-12Rβ1ΔTM expression is likely not restricted to DCs and may augment functions other than migration. The expression of (mRNA) il12rb1 and (mRNA) il12rb1Δtm in the CD11cneg fraction of M. tuberculosis–infected lungs suggests that the proteins encoded by these sequences may play a role during the chronic stage of infection. Whether IL-12Rβ1ΔTM functions to enhance IL-12Rβ1–dependent processes in T and NK cells is a focus of future investigations.
Further questions raised by the data include which signaling pathways are required in order for (mRNA) IL-12Rβ1 to be spliced? Our data demonstrate that for mouse DCs, both M. tuberculosis and M. avium elicit (mRNA) IL-12Rβ1 splicing, whereas Y. pestis stimulation does not; this despite the fact that Y. pestis does induce DC migration (Robinson et al., 2008). This suggests that although induction of (mRNA) il12rb1 is sufficient for DC migration, the augmented migration resulting from induction of (mRNA) il12rb1Δtm is a unique aspect of mycobacterial activation of DCs. We have begun to address the molecular mechanism by which IL-12Rβ1ΔTM augments DC migration and show that IL-12Rβ1–deficient DCs have a reduced M. tuberculosis–dependent NF-κB activation and that IL-12(p40)2 can induce NF-κB activation alone and augment M. tuberculosis–dependent NF-κB activation. Because it lacks any known intracellular signaling capacity, IL-12Rβ1ΔTM may enhance IL-12Rβ1–mediated NF-κB activation by increasing the affinity of IL-12(p40)2 for IL-12Rβ1 or by forming some other structure that favors IL-12(p40)2–dependent signaling. In particular, as IL-12p40 binds only to dimer/oligomers of IL-12Rβ1 (Chua et al., 1995), it is possible that the IL-12Rβ1ΔTM stabilizes oligomerization of IL-12Rβ1. Although it is possible that the splice variant may be secreted into the supernatant, we have not been able to detect it in this fraction, even after 10-fold concentration, which leads us to postulate that the splice variant acts at the membrane. Future investigations in our laboratory will test this idea, as well as determine how IL-12Rβ1ΔTM remains membrane-associated despite the absence of a TM-domain.
A large body of data demonstrates the essential function that the IL12RB1 gene serves in humans to positively regulate immunity to mycobacterial pathogens. The association between IL12RB1 deficiency and mycobacterial susceptibility undoubtedly reflects the importance of the IL12RB1 gene to a wide variety of cell types. The expression of IL-12Rβ1 mRNA is increased during active pulmonary tuberculosis in humans (Taha et al., 1999); expression of human IL-12Rβ1ΔTM during pulmonary tuberculosis has never been assessed. Although this study has focused on the importance of il12rb1 to DC function after their exposure to M. tuberculosis, our data present a novel pathway whereby a deficiency in IL-12Rβ1ΔTM results in an impaired DC function and reduced T cell activation. The generation of a mouse specifically lacking IL-12Rβ1ΔTM but not IL-12Rβ1 is underway, and this will further our understanding of this important pathway.
MATERIALS AND METHODS
Mice.
All mice were bred at the Trudeau Institute and were treated according to National Institutes of Health and Trudeau Institute Animal Care and Use Committee guidelines. All animal protocols were approved by the Trudeau Institute Animal Care and Use Committee. C57BL/6, B6.129S1-Il12btm1jm/J (i.e., il12b−/− mice; Magram et al., 1996), B6.129S1-Il12rb2tm1jm/J (i.e., il12rb2−/− mice; Wu et al., 2000), and B6.FVB-Tg(Itgax-DTR/EGFP)57Lan/J (i.e., CD11c-DTR; Jung et al., 2002) mice were originally purchased from The Jackson Laboratory. C57BL/6 mice deficient of the B6.129S1-Il12rb2tm1jm/J (il12rb1−/− mice) have been previously described (Wu et al., 1997), as have ESAT61-20-specific TCR-transgenic mice (Reiley et al., 2008).
Cell preparations.
M. tuberculosis infections were performed and the lung tissue and lymph nodes were processed as described previously (Khader et al., 2007). Single-cell suspensions were prepared from either digested lung tissue or lymph nodes by direct dispersal through a 70-µm nylon tissue strainer (BD). The resultant suspension was treated with Geys solution (155 mM NH4Cl, 10 mM KHCO3) to remove any residual red blood cells, washed twice with complete media, counted, and stained for subsequent flow cytometric analysis.
BMDCs.
BMDCs were generated from BM of 4–5-wk-old C57BL/6 mice harvested via perfusion of the femur and tibia medullary cavities with ice cold DMEM. Marrow suspensions were pelleted and incubated in Geys solution to lyse red blood cells, and the marrow was then resuspended at 4 × 105 cells/ml in complete supplemented DMEM (cDMEM). 5 ml of BM homogenate was plated in a Petri dish (Corning, Inc.) along with 5 ml of 40 ng/ml recombinant murine GM-CSF (Peprotech) in cDMEM solution for a final concentration of 20 ng/ml GM-CSF. Cultures were maintained at 37°C at 10% CO2 for 3 d, at which time an additional 10 ml of 20 ng/ml GM-CSF in cDMEM was added. At 6 d, nonadherent cells were collected and the presence of CD11c+ cells confirmed by flow cytometric analysis. For indicated experiments CD11c+ cells were positively selected by magnetic purification. In these cases 106 CD11c+ cells were placed in a 2 ml culture with or without indicated concentrations of M. tuberculosis, Y. pestis, M. avium, TNF, IL-12, or IL-12(p40)2 in cDMEM for varying amounts of time at 37°C and 10% CO2. After this period, cells were collected and either lysed for RNA and/or protein as indicated or used for chemotaxis measurements.
Flow cytometry.
All antibodies used for flow cytometric analysis were purchased from BD or eBioscience. Experimental cells were washed with FACS buffer (2% FCS in PBS), FC receptors were blocked using anti-CD16/CD32 (BD; clone 2.4G2) for 15 min and cells were stained with antibodies that recognize CD11c (clone HL3), I-Ab (clone AF6-120.1), and IL-12Rβ1 (CD212, clone 114). For all surface markers, positive staining was established using appropriate isotype controls. Data were acquired using a FACSCalibur (BD) and analyzed with FlowJo software (Tree Star, Inc.).
In vitro chemotaxis measurement.
BMDCs were activated with indicated concentrations of irradiated M. tuberculosis and their ability to respond to the chemokine CCL19 (25 ng/ml; R&D Systems) was determined using the previously described in vitro transwell chemotaxis assay (Khader et al., 2006).
In vivo tracking of lung CD11c+ DCs.
C57BL/6, il12b−/−, il12rb1−/−, and il12rb2−/− mice received a suspension of 5 µg of irradiated M. tuberculosis in a 5-mM CFSE (Invitrogen) solution delivered via the trachea. 18 h after instillation, the draining MLNs were harvested, and single-cell suspensions were prepared. Flow cytometry was used to determine the frequency and total number of CFSE-labeled CD11c+ cells that had accumulated within the MLN.
BM chimeras.
To generate mice in which only CD11c+ cells were deficient of il12rb1, we generated mixed BM chimeras comprising of irradiated C57BL/6 hosts reconstituted with 75% CD11c-DTR/25% il12rb1−/− BM. Intraperitoneal injection of DT (resuspended in sterile PBS) should theoretically remove CD11c+ cells expressing the DTR leaving in this case only il12rb1−/− CD11c+ cells. In brief, 6–10 wk old C57BL/6 hosts were lethally irradiated with 950 Rads (i.e., a split dose of 475 Rads each, 4 h apart). The irradiated hosts then received 107 whole BM donor cells comprising either 75% CD11c-DTR/25% il12rb1−/− BM or 75% CD11c-DTR/25% C57BL/6 BM as a control. BM was prepared as described in the BMDCs section. Mice were allowed at least 6 wk to reconstitute. Before ESAT1-20/M. tuberculosis instillation, all mice received an i.p. injection of 4 ng DT/g of body mass to ablate DTR-transgenic CD11c+ cells.
Cell culture.
For the generation of Concanavalin A blasts, C57BL/6 spleens were dispersed through a 70-µm nylon cell strainer (BD) and the cellular homogenate was pelleted (270 g, 6 min at 4°C) and resuspended in 2 ml of Geys solution to remove red blood cells. Splenocytes were washed and resuspended at 20 × 106 cells/ml in cDMEM, and 1 ml of splenocytes was plated in 6-well dishes (Corning, Inc.) along with 1 ml of 10 µg/ml Concanavalin A in cDMEM solution (Sigma-Aldrich) for a final concentration of 5 µg/ml Concanavalin A. Cultures were maintained at 37°C at 10% CO2 for 3 d before cells were harvested for RNA and/or protein as indicated.
RNA purification and cDNA synthesis.
Total RNA was isolated from indicated tissues and/or cell populations using the RNeasy method (QIAGEN) and was treated with DNase (Ambion). cDNA was subsequently synthesized using SuperScript II reverse transcription PCR kit (Invitrogen) with random hexamer primers.
PCR.
To amplify the IL-12Rβ1 transcript, we used primer pairs that selectively amplify the extracellular, transmembrane, or intracellular encoding portions. The relative positions of these primers (labeled P1-P6) are illustrated in Fig. 3 B. P1–4 sequences are taken directly from a previous study of IL-12Rβ1 expression in DCs (Grohmann et al., 1998). The 5′-3′ sequences of these and the other primers used in our study are as follows: P1, 5′-TATGAGTGCTCCTGGCAGTAT-3′; P2, 5′-GGCATGCTCCAATCACTCCAG-3′; P3, 5′-AATGTGCTCGCCAAAACTCG-3′; P4, 5′-GCCAATGTATCCGAGACTGC-3′. Primer P5 was designed for this study; its sequence is as follows: 5′-CTGCCTCTGCCTCTGAGTCT-3′. IL-12Rβ1 transcripts were amplified by PCR in a 25-µl reaction comprising the following: 2.5 µl of a 10× PCR buffer (200 mM Tris, pH 8.4, 500 mM KCl), 0.5 µl of 10 mM dNTPs, 1 µl 50 mM MgCl2, 0.1 µl of 5 U/µl Taq polymerase (Invitrogen), 1 µl of 5 µM forward primer (P1 or P3), 1 µl of 5 µM reverse primer (P2, P4 or P5), 17.9 µl of DNase-free H2O, and 1 µl of cDNA (a minimum of 200 pg cDNA). After denaturation at 94°C for 3 min, the reaction was cycled forty times under the following conditions: 94°C for 45 s, 60°C for 30 s, and 72°C for 90 s. The products of this reaction were analyzed on a 2% agarose gel or kept for IL-12Rβ1 spectratype analysis as described in the following section.
IL-12Rβ1 spectratype analysis.
IL-12Rβ1 spectratype analysis of IL-12Rβ1 and IL-12Rβ1ΔTM mRNAs, and the quantification of the resultant data, was a modification of the now commonly used TCR-CD3 Spectratype analysis (Pannetier et al., 1993). IL-12Rβ1 and IL-12Rβ1ΔTM cDNA transcripts were first amplified by PCR in the 25-µl reaction detailed above with the forward primer 5′-CAGCCGAGTAATGTACAAGG-3′ and reverse primer 5′-CTGCCTCTGCCTCTGAGTCT-3′. The forward primer corresponds to nt 1653–1672 of the mouse IL-12Rβ1 transcript and precedes the transmembrane-encoding sequence (nt 1739–1834). The reverse primer is downstream of the transmembrane-encoding sequence, corresponding to nucleotides 2067–2086 of the mouse IL-12Rβ1 transcript. To fluorescently label the IL-12Rβ1 and IL-12Rβ1ΔTM amplicons we performed a second, runoff PCR reaction as follows: 2.5 µl of the initial amplification reaction was added to 22.5 µl of a second PCR comprising 2.5 µl of 10× PCR buffer, 0.5 uL of 10 mM dNTPs, 1 uL 50 mM MgCl2, 0.1 uL of 5 U/uL Taq polymerase (Invitrogen), 2 uL of a 5 uM FAM-labeled reverse primer (FAM-5′-AGTGCTGCCACAGGGTGTA-3′), and 16.4 µl of DNase-free H2O (final volume: 25 µl). After denaturation at 94°C for 5 min, the reaction was cycled four times under the following conditions: 95°C for 2 min, 55°C for 2 min, 72°C for 20 min. 2 µl of the completed runoff PCR reaction was then added to 2.0 µl of ROX-500 size standard (Applied Biosystems) and 36 µl of HiDi Formamide (Applied Biosystems). After denaturation, the products were detected and their size and relative amount determined using an Applied Biosystems 3100 sequencer analyzed with GeneScan software (Applied Biosystems). For calculating the ratio of IL-12Rβ1ΔTM to IL-12Rβ1 (i.e., IL-12Rβ1ΔTM:IL-12Rβ1) we simply divided the area under the IL-12Rβ1ΔTM peak by the area under the reference IL-12Rβ1 peak.
Plasmids and transfections.
Plasmids expressing IL-12Rβ1 and IL-12Rβ1ΔTM cDNAs in vector pEF-BOS (Mizushima and Nagata, 1990) under the EF1α promoter have been described (Chua et al., 1995; pEF-BOS.IL-12Rβ1 and pEF-BOS.IL-12Rβ1ΔTM). pAcGFP1-N1 (Takara Bio Inc.) was used to express eGFP under the CMV promoter to identify transfected cells. For transfection into NIH/3T3 cells (American Type Culture Collection) we used the Polyfect system (QIAGEN) after the manufacturers instructions.
Western blot analysis.
SDS-PAGE analysis of reduced protein samples and subsequent transfer to PVDF membrane was performed using standard protocols. Membranes were subsequently probed overnight with 400 ng/ml goat polyclonal anti-IL-12Rβ1 (R&D Systems) in a solution of Tris-buffered saline containing 2.5% powdered milk, washed with Tris-buffered saline, secondarily probed with HRP-conjugated anti-goat IgG and detected using ECL Western blotting substrate (Thermo Fisher Scientific) for chemiluminescence. For a positive control, recombinant mouse IL-12Rβ1 (R&D Systems) was run simultaneously with each gel.
Determination of total NF-κB and phospho-NF-κB levels.
C57BL/6 and il12rb1−/− BMDCs were exposed to M. tuberculosis or media alone for indicated times. After each time point, cells were collected and washed with ice-cold PBS. Cells were subsequently lysed by addition of ice-cold lysis buffer (20 mM Tris, pH 7.5, 150 mM NaCl, 1 mM EDTA, 1 mM EGTA, 1% Triton X-100, 2.5 mM Na4P2O7, 1 mM β-glycerophosphate, 1 mM Na3VO4, and 1 µg/ml leupeptin plus 1 mM PMSF) and sonication on ice. Total lysates were centrifuged at 14,000 RPM for 10 min at 4°C; the supernatants were aliquoted and stored at −80°C until determination of total NF-κB and phospho-NF-κB levels by ELISA (PathScan Inflammation Multi-Target Sandwich ELISA; Cell Signaling Technology).
NF-κB EMSA.
Nuclear extracts from indicated cell populations were subjected to polyacrilamide electrophoresis and EMSA analysis of subsequently generated blots with a NF-κB EMSA kit (Panomics) with biotinylated NF-κB probe 5′-AGTTGAGGGGACTTTCCCAGGC-3′, as per the manufacturer’s instructions.
In vitro mRNA transcription.
To generate in vitro–transcribed (IVT) mRNA of IL-12Rβ1, IL-12Rβ1ΔTM and eGFP it was first necessary to subclone their respective cDNAs into a second plasmid, downstream of a T7 phage polymerase. The IL-12Rβ1 and IL-12Rβ1ΔTM cDNAs were first amplified out of their pEF-BOS backbones using primers that flanked their start and stop codons; specifically 5′-TGTTTCTGAGCGTGGACAAG-3′ and 5′-CCGCAGTCTTATGGGTCCT-3′. eGFP was amplified out of pAcGFP1-N1 using primers 5′-TAGCGCTACCGGACTCAGAT-3′ (cognate to the sequence just 5′ of the eGFP start codon) and 5′-GGGAGGTGTGGGAGGTTTT-3′. IL-12Rβ1, IL-12Rβ1ΔTM, and eGFP amplicons were subsequently TA-cloned into pCR2.1 downstream of the T7 phage polymerase promoter to generate the plasmids pCR2.1.IL-12Rβ1, pCR2.1.IL-12Rβ1ΔTM, and pCR2.1.eGFP, respectively. These constructs were subsequently used in the mMessage mMachine kit (Ambion) to generate 5′ capped IVT mRNA as per the manufacturer’s instruction. mRNA quality was checked by gel electrophoresis, and the concentration was determined by spectrophotometric analysis at OD260. mRNA aliquots were stored at −80°C until used for transfections.
Electroporation of DCs.
Electroporation of individual mRNAs into il12rb1−/− DCs was done as performed by Ponsaerts et al. (2002), with minor modifications. In brief, before electroporation, DCs were washed twice with electroporation buffer (Ambion) and resuspended to a final concentration of 5 × 107 cells/ml in electroporation buffer. Subsequently, 0.2 ml of the cell suspension was mixed with 20 µg of IVT mRNA and electroporated in a 0.4-cm cuvette at 300 V and 150 μF using a Gene Pulser Xcell Electroporation System (Bio-Rad Laboratories). After electroporation, fresh complete medium was added to the cell suspension and cells further incubated at 37°C in a humidified atmosphere supplemented with 5% CO2. For all electroporation experiments, the co-transfection of eGFP-mRNA was used to both confirm transfection efficiency and to identify those cells that have been successfully transfected.
In vivo migration of electroporated DCs.
After mRNA electroporation and overnight culture, 106 DCs were cultured with 10 µg/ml irradiated M. tuberculosis and 1 µM ESAT1-20 peptide for 3 h. After this time the DCs were washed, resuspended in PBS, and instilled via the trachea into the lungs of C57BL/6 mice. 18 h before instillation, each mouse had intravenously received 5 × 106 CFSE-labeled ESAT-TCR CD4+ cells. The surface expression of CD44 and CD69 on CFSE+CD4+ cells in the draining MLNs was assessed 12 h later by flow cytometry.
IL-12RB1 isoform expression by human DCs.
Monocyte-derived DCs were generated by incubating magnetically purified CD14+ monocytes from apheresis samples for 7 d with 20 ng/ml GMCSF (Peprotech) and 50 ng/ml IL-4 (R&D Systems). DCs were then incubated for 24h with 1 µg/ml LPS or for 3 d with either of the following: 10 ng/ml IL-1β, 200 ng/ml IL-10, 10 ng/ml IL-6, 20 U/ml IL-2, 50 ng/ml CCL3, 50 ng/ml PlGF, or just RPMI media (control). Alternatively, DCs were stimulated with M. tuberculosis over a 6-h period. Subsequently generated cDNA from these populations was then amplified with primer pairs that either amplified both IL-12RB1 isoforms 1 and 2 (Common: forward, 5′-ACACTCTGGGTGGAATCCTG-3′; reverse, 5′-GCCAACTTGGACACCTTGAT-3′), only isoform 1 (Isoform 1 Specific: forward, 5′-ACACTCTGGGTGGAATCCTG-3; reverse, 5′-CACCCTCTCTGAGCCTCAAC-3′) or only isoform 2 (Isoform 2 Specific: forward, 5′-ACACTCTGGGTGGAATCCTG-3′; reverse, 5′-CACTTTGGGAGGCCAAG-3′). The conditions used to amplify with these primers were the same as those used for the primary PCR of IL-12Rβ1 spectratype analysis detailed above. cDNA from CD3+ PBMCs was used as a positive control for IL-12RB1 expression. Amplicons were analyzed by 2% agarose gel electrophoresis.
Statistical analysis.
Differences between the means of experimental groups were analyzed with the two-tailed Student’s t test as the data were considered parametric. Differences with a P value of 0.05 or less were considered significant. Prism software was used for all analyses.
Online supplemental material.
Fig. S1 demonstrates the concept and validation of IL-12Rβ1 spectratype analysis. Fig. S2 shows that the expression of IL-12Rβ1ΔTM mRNA by mouse DCs is limited to mycobacterial stimulation. Fig. S3 demonstrates that two isoforms of IL-12Rβ1 are expressed by human DCs after exposure to M. tuberculosis and other specific stimuli. Fig. S4 shows that lung expression of IL-12Rβ1ΔTM mRNA also occurs during pulmonary infection with M. avium, but not Y. pestis. Online supplemental material is available at http://www.jem.org/cgi/content/full/jem.20091085/DC1.
Supplementary Material
Acknowledgments
We thank D. Duso for excellent technical assistance with all mouse procedures. We would also like to thank P. Eble, R. Bartiss, H. Trumble, and C. Eaton for maintenance and screening of mouse colonies.
This work was supported by the Trudeau Institute and the National Institutes of Health (AI067723 to A.M. Cooper; AI49823 to D.L. Woodland [trainee: R.T. Robinson] and AI084397 to R.T. Robinson).
The authors have no conflicting financial interests.
Footnotes
Abbreviations used:
- BMDC
- BM-derived DC
- DT
- diphtheria toxin
- DTR
- DT receptor
- eGFP
- enhanced GFP
- EMSA
- electromobility shift assay
- MLN
- mediastinal LN
References
- Altare F., Durandy A., Lammas D., Emile J.F., Lamhamedi S., Le Deist F., Drysdale P., Jouanguy E., Döffinger R., Bernaudin F., et al. 1998. Impairment of mycobacterial immunity in human interleukin-12 receptor deficiency. Science. 280:1432–1435. 10.1126/science.280.5368.1432 [DOI] [PubMed] [Google Scholar]
- Capon F., Di Meglio P., Szaub J., Prescott N.J., Dunster C., Baumber L., Timms K., Gutin A., Abkevic V., Burden A.D., et al. 2007. Sequence variants in the genes for the interleukin-23 receptor (IL23R) and its ligand (IL12B) confer protection against psoriasis. Hum. Genet. 122:201–206. 10.1007/s00439-007-0397-0 [DOI] [PubMed] [Google Scholar]
- Chua A.O., Chizzonite R., Desai B.B., Truitt T.P., Nunes P., Minetti L.J., Warrier R.R., Presky D.H., Levine J.F., Gately M.K., et al. 1994. Expression cloning of a human IL-12 receptor component. A new member of the cytokine receptor superfamily with strong homology to gp130. J. Immunol. 153:128–136. [PubMed] [Google Scholar]
- Chua A.O., Wilkinson V.L., Presky D.H., Gubler U.. 1995. Cloning and characterization of a mouse IL-12 receptor-beta component. J. Immunol. 155:4286–4294. [PubMed] [Google Scholar]
- Cooper A.M. 2009. Cell-mediated immune responses in tuberculosis. Annu. Rev. Immunol. 27:393–422. 10.1146/annurev.immunol.021908.132703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooper A.M., Solache A., Khader S.A.. 2007. Interleukin-12 and tuberculosis: an old story revisited. Curr. Opin. Immunol. 19:441–447. 10.1016/j.coi.2007.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong R., Altare F., Haagen I.A., Elferink D.G., Boer T., van Breda Vriesman P.J., Kabel P.J., Draaisma J.M., van Dissel J.T., Kroon F.P., et al. 1998. Severe mycobacterial and Salmonella infections in interleukin-12 receptor-deficient patients. Science. 280:1435–1438. 10.1126/science.280.5368.1435 [DOI] [PubMed] [Google Scholar]
- Filipe-Santos O., Bustamante J., Chapgier A., Vogt G., de Beaucoudrey L., Feinberg J., Jouanguy E., Boisson-Dupuis S., Fieschi C., Picard C., Casanova J.L.. 2006. Inborn errors of IL-12/23- and IFN-gamma-mediated immunity: molecular, cellular, and clinical features. Semin. Immunol. 18:347–361. 10.1016/j.smim.2006.07.010 [DOI] [PubMed] [Google Scholar]
- Fortin A., Abel L., Casanova J.L., Gros P.. 2007. Host genetics of mycobacterial diseases in mice and men: forward genetic studies of BCG-osis and tuberculosis. Annu. Rev. Genomics Hum. Genet. 8:163–192. 10.1146/annurev.genom.8.080706.092315 [DOI] [PubMed] [Google Scholar]
- Gallegos A.M., Pamer E.G., Glickman M.S.. 2008. Delayed protection by ESAT-6–specific effector CD4+ T cells after airborne M. tuberculosis infection. J. Exp. Med. 205:2359–2368. 10.1084/jem.20080353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grohmann U., Belladonna M.L., Bianchi R., Orabona C., Ayroldi E., Fioretti M.C., Puccetti P.. 1998. IL-12 acts directly on DC to promote nuclear localization of NF-kappaB and primes DC for IL-12 production. Immunity. 9:315–323. 10.1016/S1074-7613(00)80614-7 [DOI] [PubMed] [Google Scholar]
- Jang S., Uzelac A., Salgame P.. 2008. Distinct chemokine and cytokine gene expression pattern of murine dendritic cells and macrophages in response to Mycobacterium tuberculosis infection. J. Leukoc. Biol. 84:1264–1270. 10.1189/jlb.1107742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson J.M., Castle J., Garrett-Engele P., Kan Z., Loerch P.M., Armour C.D., Santos R., Schadt E.E., Stoughton R., Shoemaker D.D.. 2003. Genome-wide survey of human alternative pre-mRNA splicing with exon junction microarrays. Science. 302:2141–2144. 10.1126/science.1090100 [DOI] [PubMed] [Google Scholar]
- Jung S., Unutmaz D., Wong P., Sano G., De los Santos K., Sparwasser T., Wu S., Vuthoori S., Ko K., Zavala F., et al. 2002. In vivo depletion of CD11c(+) dendritic cells abrogates priming of CD8(+) T cells by exogenous cell-associated antigens. Immunity. 17:211–220. 10.1016/S1074-7613(02)00365-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khader S.A., Partida-Sanchez S., Bell G., Jelley-Gibbs D.M., Swain S., Pearl J.E., Ghilardi N., Desauvage F.J., Lund F.E., Cooper A.M.. 2006. Interleukin 12p40 is required for dendritic cell migration and T cell priming after Mycobacterium tuberculosis infection. J. Exp. Med. 203:1805–1815. 10.1084/jem.20052545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khader S.A., Bell G.K., Pearl J.E., Fountain J.J., Rangel-Moreno J., Cilley G.E., Shen F., Eaton S.M., Gaffen S.L., Swain S.L., et al. 2007. IL-23 and IL-17 in the establishment of protective pulmonary CD4+ T cell responses after vaccination and during Mycobacterium tuberculosis challenge. Nat. Immunol. 8:369–377. 10.1038/ni1449 [DOI] [PubMed] [Google Scholar]
- Lambrecht B.N. 2008. Lung dendritic cells: targets for therapy in allergic disease. Curr. Mol. Med. 8:393–400. 10.2174/156652408785160916 [DOI] [PubMed] [Google Scholar]
- Levine S.J. 2004. Mechanisms of soluble cytokine receptor generation. J. Immunol. 173:5343–5348. [DOI] [PubMed] [Google Scholar]
- Lynch K.W. 2004. Consequences of regulated pre-mRNA splicing in the immune system. Nat. Rev. Immunol. 4:931–940. 10.1038/nri1497 [DOI] [PubMed] [Google Scholar]
- Magram J., Connaughton S.E., Warrier R.R., Carvajal D.M., Wu C.Y., Ferrante J., Stewart C., Sarmiento U., Faherty D.A., Gately M.K.. 1996. IL-12-deficient mice are defective in IFN gamma production and type 1 cytokine responses. Immunity. 4:471–481. 10.1016/S1074-7613(00)80413-6 [DOI] [PubMed] [Google Scholar]
- McCormick S., Santosuosso M., Small C.-L., Shaler C.R., Zhang X., Jeyanathan M., Mu J., Takenaka S., Ngai P., Gauldie J., et al. 2008. Mucosally delivered dendritic cells activate T cells independently of IL-12 and endogenous APCs. J. Immunol. 181:2356–2367. [DOI] [PubMed] [Google Scholar]
- Mizushima S., Nagata S.. 1990. pEF-BOS, a powerful mammalian expression vector. Nucleic Acids Res. 18:5322. 10.1093/nar/18.17.5322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagayama H., Sato K., Kawasaki H., Enomoto M., Morimoto C., Tadokoro K., Juji T., Asano S., Takahashi T.A.. 2000. IL-12 responsiveness and expression of IL-12 receptor in human peripheral blood monocyte-derived dendritic cells. J. Immunol. 165:59–66. [DOI] [PubMed] [Google Scholar]
- Oppmann B., Lesley R., Blom B., Timans J.C., Xu Y., Hunte B., Vega F., Yu N., Wang J., Singh K., et al. 2000. Novel p19 protein engages IL-12p40 to form a cytokine, IL-23, with biological activities similar as well as distinct from IL-12. Immunity. 13:715–725. 10.1016/S1074-7613(00)00070-4 [DOI] [PubMed] [Google Scholar]
- Pannetier C., Cochet M., Darche S., Casrouge A., Zöller M., Kourilsky P.. 1993. The sizes of the CDR3 hypervariable regions of the murine T-cell receptor beta chains vary as a function of the recombined germ-line segments. Proc. Natl. Acad. Sci. USA. 90:4319–4323. 10.1073/pnas.90.9.4319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parham C., Chirica M., Timans J., Vaisberg E., Travis M., Cheung J., Pflanz S., Zhang R., Singh K.P., Vega F., To W., Wagner J., O’Farrell A.M., Mcclanahan T., Zurawski S., Hannum C., Gorman D., Rennick D.M., Kastelein R.A., De Waal Malefyt R., Moore K.W.. 2002. A receptor for the heterodimeric cytokine IL-23 is composed of IL-12Rbeta1 and a novel cytokine receptor subunit, IL-23R. J. Immunol. 168:5699–5708. [DOI] [PubMed] [Google Scholar]
- Ponsaerts P., Van Tendeloo V.F., Cools N., Van Driessche A., Lardon F., Nijs G., Lenjou M., Mertens G., Van Broeckhoven C., Van Bockstaele D.R., Berneman Z.N.. 2002. mRNA-electroporated mature dendritic cells retain transgene expression, phenotypical properties and stimulatory capacity after cryopreservation. Leukemia. 16:1324–1330. 10.1038/sj.leu.2402511 [DOI] [PubMed] [Google Scholar]
- Presky D.H., Yang H., Minetti L.J., Chua A.O., Nabavi N., Wu C.Y., Gately M.K., Gubler U.. 1996. A functional interleukin 12 receptor complex is composed of two beta-type cytokine receptor subunits. Proc. Natl. Acad. Sci. USA. 93:14002–14007. 10.1073/pnas.93.24.14002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Presky D.H., Minetti L.J., Gillessen S., Wilkinson V.L., Wu C.Y., Gubler U., Chizzonite R., Gately M.K.. 1998. Analysis of the multiple interactions between IL-12 and the high affinity IL-12 receptor complex. J. Immunol. 160:2174–2179. [PubMed] [Google Scholar]
- Reiley W.W., Calayag M.D., Wittmer S.T., Huntington J.L., Pearl J.E., Fountain J.J., Martino C.A., Roberts A.D., Cooper A.M., Winslow G.M., Woodland D.L.. 2008. ESAT-6-specific CD4 T cell responses to aerosol Mycobacterium tuberculosis infection are initiated in the mediastinal lymph nodes. Proc. Natl. Acad. Sci. USA. 105:10961–10966. 10.1073/pnas.0801496105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson R.T., Khader S.A., Locksley R.M., Lien E., Smiley S.T., Cooper A.M.. 2008. Yersinia pestis evades TLR4-dependent induction of IL-12(p40)2 by dendritic cells and subsequent cell migration. J. Immunol. 181:5560–5567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taha R.A., Minshall E.M., Olivenstein R., Ihaku D., Wallaert B., Tsicopoulos A., Tonnel A.B., Damia R., Menzies D., Hamid Q.A.. 1999. Increased expression of IL-12 receptor mRNA in active pulmonary tuberculosis and sarcoidosis. Am. J. Respir. Crit. Care Med. 160:1119–1123. [DOI] [PubMed] [Google Scholar]
- Takahashi N., Akahoshi M., Matsuda A., Ebe K., Inomata N., Obara K., Hirota T., Nakashima K., Shimizu M., Tamari M., et al. 2005. Association of the IL12RB1 promoter polymorphisms with increased risk of atopic dermatitis and other allergic phenotypes. Hum. Mol. Genet. 14:3149–3159. 10.1093/hmg/ddi347 [DOI] [PubMed] [Google Scholar]
- Tian T., Woodworth J., Sköld M., Behar S.M.. 2005. In vivo depletion of CD11c+ cells delays the CD4+ T cell response to Mycobacterium tuberculosis and exacerbates the outcome of infection. J. Immunol. 175:3268–3272. [DOI] [PubMed] [Google Scholar]
- van de Vosse E., Lichtenauer-Kaligis E.G., van Dissel J.T., Ottenhoff T.H.. 2003. Genetic variations in the interleukin-12/interleukin-23 receptor (beta1) chain, and implications for IL-12 and IL-23 receptor structure and function. Immunogenetics. 54:817–829. [DOI] [PubMed] [Google Scholar]
- van Rietschoten J.G., Smits H.H., Westland R., Verweij C.L., den Hartog M.T., Wierenga E.A.. 2000. Genomic organization of the human interleukin-12 receptor beta2-chain gene. Immunogenetics. 51:30–36. 10.1007/s002510050005 [DOI] [PubMed] [Google Scholar]
- Wang X., Wilkinson V.L., Podlaski F.J., Wu C., Stern A.S., Presky D.H., Magram J.. 1999. Characterization of mouse interleukin-12 p40 homodimer binding to the interleukin-12 receptor subunits. Eur. J. Immunol. 29:2007–2013. [DOI] [PubMed] [Google Scholar]
- Winslow G.M., Cooper A., Reiley W., Chatterjee M., Woodland D.L.. 2008. Early T-cell responses in tuberculosis immunity. Immunol. Rev. 225:284–299. 10.1111/j.1600-065X.2008.00693.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf A.J., Linas B., Trevejo-Nuñez G.J., Kincaid E., Tamura T., Takatsu K., Ernst J.D.. 2007. Mycobacterium tuberculosis infects dendritic cells with high frequency and impairs their function in vivo. J. Immunol. 179:2509–2519. [DOI] [PubMed] [Google Scholar]
- Wolf A.J., Desvignes L., Linas B., Banaiee N., Tamura T., Takatsu K., Ernst J.D.. 2008. Initiation of the adaptive immune response to Mycobacterium tuberculosis depends on antigen production in the local lymph node, not the lungs. J. Exp. Med. 205:105–115. 10.1084/jem.20071367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu C., Ferrante J., Gately M.K., Magram J.. 1997. Characterization of IL-12 receptor beta1 chain (IL-12Rbeta1)-deficient mice: IL-12Rbeta1 is an essential component of the functional mouse IL-12 receptor. J. Immunol. 159:1658–1665. [PubMed] [Google Scholar]
- Wu C., Wang X., Gadina M., O’Shea J.J., Presky D.H., Magram J.. 2000. IL-12 receptor beta 2 (IL-12R beta 2)-deficient mice are defective in IL-12-mediated signaling despite the presence of high affinity IL-12 binding sites. J. Immunol. 165:6221–6228. [DOI] [PubMed] [Google Scholar]
- Zhang G.X., Yu S., Gran B., Li J., Siglienti I., Chen X., Calida D., Ventura E., Kamoun M., Rostami A.. 2003. Role of IL-12 receptor beta 1 in regulation of T cell response by APC in experimental autoimmune encephalomyelitis. J. Immunol. 171:4485–4492. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.