Abstract
AIM: To investigate the association of gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS) in Iranian patients and examine the prevalence of functional symptoms of the gastrointestinal tract in patients presenting with either IBS, GERD or both.
METHODS: Six thousand four hundred and seventy six patients presented to the Gastro-intestinal (GI) clinic with symptoms of functional dysfunction of GI tract, 1419 patients (62.0% women, 38.0% men; mean age: 37.4 ± 11.5 years) met Rome II or Rome III criteria (depending on the year of diagnosis) for IBS. 2658 patients were diagnosed with GERD based on clinical presentation and endoscopic findings. We assessed other functional symptoms (epigastric pain, nausea, vomiting, belching, constipation and diarrhea) in patients suffering from GERD, IBS or both.
RESULTS: Among IBS subjects, 63.6% (69.0% women, 31.0% men; mean age: 36.4 ± 10.3 years) also had GERD, whereas 34.7% of the non-IBS patients had GERD [odds ratio (OR) = 3.2, 95% confidence interval (CI): 2.9-3.7, P < 0.0001]. Among patients with GERD, 33.9% of subjects met Rome criteria compared to 13.5% of non-GERD patients (OR = 3.6, 95% CI: 3.1-4.3, P < 0.0001). Prevalence of all functional symptoms was higher in overlapping GERD and IBS subjects, when compared with their prevalence in the IBS subjects without GERD or GERD only subjects (P < 0.05).
CONCLUSION: This finding shows that in overlapping GERD and IBS, other functional abnormalities of the GI tract are also highly prevalent, suggesting a common underlying dysfunction.
Keywords: Gastro-esophageal reflux disease, Irritable bowel syndrome, Helicobacter pylori, Gastro-intestinal dysfunction, Endoscopy
INTRODUCTION
Irritable bowel syndrome (IBS), affecting approximately 10%-15% of the population is defined by Rome criteria as “abdominal pain or discomfort associated with altered bowel habits and disordered defecation”[1-5]; gastroesophageal reflux disease (GERD) is characterized by the symptoms of heart burn and regurgitation caused by reflux of stomach content and is experienced once daily by 7% and once monthly by 44%[6,7] of patients. Originally, GERD and IBS were considered to be distinct issues, but common clinical features between IBS and GERD[8,9] suggest that an overlap between these conditions might exist. Recently, a considerable overlap between GERD and IBS in both population based and clinical based studies have been reported[10-13]. In addition, some evidence suggested that GERD, like IBS, should be considered as a gastrointestinal motility disorder, which suggests that similar pathophysiological characteristics might contribute to GERD and IBS[9,14].
In the current study, we used a large clinic-based data-base to estimate the prevalence of overlap between GERD and IBS. We also examined the prevalence of a number of clinical symptoms of Gastro-intestinal (GI) functional motility disorders like belching, nausea and vomiting, constipation and diarrhea in patients presenting with GERD, IBS or both. We predicted that if GERD and IBS are different presentations of the same pathologic process in function and motility of GI tract, the more severe the disorder, the more prevalent the functional symptoms should be; therefore we expected a higher prevalence of dysfunctional symptoms in patients with overlapping GERD and IBS.
MATERIALS AND METHODS
All patients referred to a subspecialty practice medical group from March 1997 to March 2007 were enrolled. Five hundred and four patients were excluded because of not having follow up sessions, defined as having only one visit or lacking final diagnosis in the records, or having peptic ulcer found on endoscopy, and the remaining 6476 patients (mean age = 37.9 ± 13.4 years) were registered. Patients filled in a questionnaire about presence and severity of functional symptoms at every visit. All of the final diagnoses available in the records had been made by gastroenterologists who were participating in the gastroenterology department related to Tehran Medical University as academic staff.
GERD was defined as having clinical presentations such as heart burn, regurgitation and dysphagia. 91% of patients with clinically assumed GERD had undergone standard upper gastrointestinal endoscopy (UGIE). Patients who showed endoscopic evidence of GERD, like esophagitis, were not tested further. Those who did not show evidence of GERD were confirmed by pH monitoring. Patients with peptic ulcer found on endoscopy were excluded from the study. Subjects were diagnosed with IBS by fulfilling Rome II or Rome III criteria.
The records were then reviewed for the following items: (1) demographic data (including patient’s record number, age and sex); (2) symptoms of GERD, IBS and other symptoms related to the dysfunction of upper and lower GI tract such as: epigastric pain, nausea, vomiting and belching, constipation and diarrhea; (3) non-gastrointestinal complaints which included back pain and headache; (4) being a Helicobacter pylori (H. pylori) carrier or not. A number of patients diagnosed with GERD or IBS were evaluated for H. pylori during the clinical evaluation for the diagnosis and were found to have H. pylori infection by means of either C-urea breath test, urease test in obtained biopsies during UGIE or serum checking; (5) whether GERD in clinically suspicious patients is confirmed by UGIE or not; and (6) final diagnosis of GERD and IBS. Patients were classified according to their final diagnosis, as suffering from: (1) IBS (IBS group); (2) GERD (GERD group); and (3) both GERD and IBS (GERD + IBS group).
Statistical analysis
Extracted data was analyzed using SPSS version 14.0 (SPSS Inc., Chicago, IL, USA). χ2 test was used to compare qualitative variables, whereas t-test was used to compare discontinuous quantitative variables. A P value less than 0.05 was considered to indicate a statistically significant difference.
RESULTS
Six thousand four hundred and seventy six patients including 3185 (49.2%) men and 3291 (50.8%) women were enrolled in the study. No statistically significant difference was found in mean age of men and women. One thousand four hundred and nineteen (21.9%) of patients were diagnosed with IBS, using Rome II or Rome III criteria for IBS. The IBS group was made up of 539 (38.0%) male and 880 (62.0%) female, with a mean age of 37.4 ± 11.5 years. There were no differences in mean age between men and women. Two thousand six hundred and fifty eight (41%) were diagnosed with GERD, 95.8% were experiencing heart burn, 3.0% presented with regurgitation and 1.2% presented with dysphagia (Figure 1). The diagnosis of GERD had been confirmed in 69.2% of GERD patients with UGIE and in 21.8% with pH monitoring. There was a slight difference in sex distribution of GERD, men making up 44.7% and women making up 55.3% of the patients; the mean age of GERD subjects was 37.9 ± 13.4 years without any considerable difference for men and women.
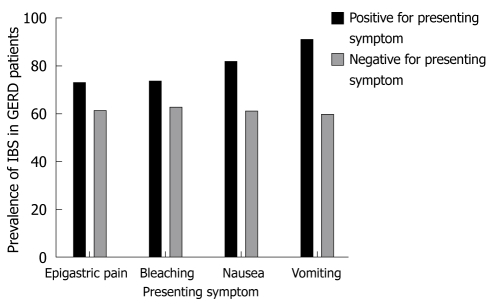
Figure 1.
Prevalence of irritable bowel syndrome (IBS) in patients with gastroesophageal reflux disease (GERD) based on their presenting symptoms. The probability of having simultaneous GERD and IBS was significantly higher in patients presenting with either of these functional symptoms; however, nausea and vomiting were more strongly related to the overlap of two diseases.
Among 1419 patients diagnosed with IBS, 902 (63.6%) also had GERD whereas 34.7% of non-IBS patients had GERD [odds ratio (OR) = 3.2, 95% confidence interval (CI) = 2.9-3.7, P < 0.0001]. On the other hand 33.9% of GERD subjects met Rome criteria for IBS compared to 13.5% of non-GERD sufferers (OR = 3.6, 95% CI: 3.1-4.3, P < 0.0001). 34.4% of the endoscopically diagnosed GERD patients had overlapping IBS; reciprocally 62.4% of the IBS patients had GERD diagnosed by endoscopy or pH monitoring.
69.0% of patients with both GERD and IBS were women and 31.0% were men; while women make up 50.0% of GERD only patients (P < 0.0001 vs GERD + IBS group) and 61.1% of IBS only patients (P < 0.0001 vs GERD + IBS group). The mean age of patients with GERD and IBS was 36.4 ± 10.3, statistically similar to IBS patients without GERD and GERD subjects without IBS (P > 0.5).
Table 1 presents the prevalence of other gastrointestinal functional symptoms in the three mentioned groups. Remarkably, these symptoms were significantly more frequent in patients with both GERD and IBS compared to non-GERD non-IBS patients. Statistical analysis showed the following significant differences: epigastric pain (22.9% vs 9.6%, P < 0.0001), nausea (15.9% vs 4.8%, P < 0.0001), vomiting (16.0% vs 5.3%, P < 0.0001), constipation (12.2% vs 4.2%, P < 0.0001), diarrhea (18.7% vs 7.3%, P < 0.0001), headache (6.8% vs 2.4%, P < 0.0001), back pain (6.0% vs 3.7%, P = 0.03).
Table 1.
Comparison of frequency of functional symptoms in patients with IBS, GERD and GERD + IBS
| Frequency | GERD only patients (n = 1522) | IBS only patients (n = 738) | GERD + IBS (n = 433) |
P value |
||
| IBS vs GERD | GERD + IBS vs IBS | GERD + IBS vs GERD | ||||
| Nausea | 10.8% | 6.2% | 15.9% | 0.02 | < 0.0001 | < 0.0001 |
| Vomiting | 11.6% | 3.3% | 18.8% | < 0.0001 | < 0.0001 | < 0.0001 |
| Epigastric pain | 18.9% | 14.9% | 22.9% | 0.037 | < 0.0001 | < 0.0001 |
| Belching | 4.1% | 6.4% | 10.2% | 0.03 | 0.015 | < 0.0001 |
| Headache | 2.8% | 4.4% | 6.8% | 0.058 | 0.07 | < 0.0001 |
| Back pain | 3.6% | 3.3% | 6.0% | 0.74 | 0.025 | 0.004 |
Pair-wise comparison of frequency of nausea, vomiting, epigastric pain, belching, headache and low back pain in patients with IBS alone, GERD alone and GERD + IBS showed that the frequency of all of these functional symptoms was significantly higher in patients in GERD + IBS group. IBS: Irritable bowel syndrome; GERD: Gastroesophageal reflux disease.
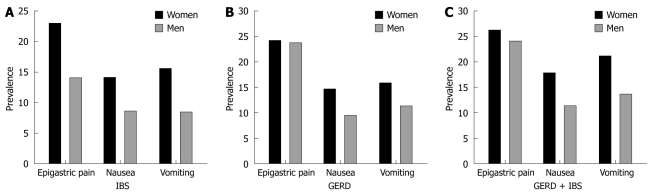
In comparison with men, women in the IBS group were more likely to experience epigastric pain (23.0% vs 14.1%, P < 0.0001), nausea (14.2% vs 8.7%, P = 0.003) and vomiting (15.6% vs 8.5%, P < 0.0001). 14.7% and 16.0% of women with GERD suffered nausea and vomiting, respectively, whereas 9.6% and 11.4% of male GERD patients had nausea and vomiting (P < 0.0001, P = 0.001, respectively). Women complaining of both GERD and IBS had a trend toward experiencing nausea and vomiting more than men; 17.8% of women and 11.4% of men complained of nausea (P = 0.015) and 21.2% of women and 13.6% of men suffered from vomiting (P = 0.007, Figure 2).
Figure 2.
Sex distribution of functional symptoms in patients with IBS (A), GERD (B), GERD + IBS (C). In all of the groups the prevalence of nausea and vomiting was significantly higher in women than in men. Considering that nausea and vomiting were the most frequent symptoms in overlapping diseases, it is explainable by a high prevalence of overlap in women.
We determined the differential prevalence of IBS in patients with GERD based on presenting and accompanying functional symptoms (Figure 1). 72.9% of patients with GERD who presented with epigastric pain also had IBS compared to 61.2% of GERD patients without epigastric pain (P < 0.0001). 73.6% of GERD patients reporting belching were also diagnosed to have IBS whereas 62.6% of GERD subjects without belching were suggested to have IBS (P = 0.015). IBS was present in 81.7% of GERD patients with a complaint of nausea while 61.0% of patients with GERD, not accompanied by nausea also suffered from IBS simultaneously (P < 0.0001). 90.9% of patients with GERD and vomiting were considered to have IBS compared to 59.4% of GERD subjects without vomiting who were assumed to have IBS (P < 0.0001). These findings suggest a considerable overlap between functional dyspepsia, GERD and IBS. Among the total upper GI symptoms assessed, 40.5% of the IBS group, 39.2% of the GERD group and 47.8% of both GERD + IBS group reported one or more functional symptoms; two or more symptoms were present in 10.9% of IBS group, 10.3% of GERD group and 15.9% of GERD + IBS; 2.7% of IBS patients, 1.7% of GERD patients and 3.9% of GERD + IBS patients complained of three or more symptoms while 0.2% of the IBS group, 0.1% of the GERD group and 0.3% of GERD + IBS group were known to have four symptoms. There was no significant difference when the association between number of overlapping symptoms and GERD and IBS was evaluated.
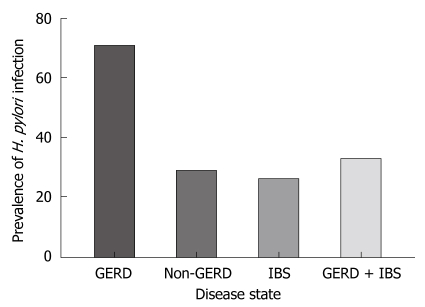
About 373 of IBS patients, 1323 of the GERD group and 287 of GERD + IBS group were evaluated for H. pylori infection. 70.9% of GERD patients were found to have H. pylori infection significantly more than non-GERD patients (29.1%, P < 0.0001). IBS group patients and GERD + IBS patients were not significantly affected by H. pylori infection in proportion to non-IBS and non-GERD + IBS patients (P > 0.5). This finding is interesting because it shows that in GERD + IBS patients whose symptoms might have a common functional abnormality, the prevalence of Helicobacter infection is significantly lower than GERD only patients (Figure 3).
Figure 3.
Frequency of Helicobacter pylori (H. pylori) infection in patients with IBS, GERD, GERD + IBS. The frequency of H. pylori infection was significantly higher in patients with GERD alone compared to patients with GERD + IBS.
DISCUSSION
IBS and its comorbidities have recently been the focus of extensive research. In spite of the fact that other surveys have indicated the increased prevalence of GERD in IBS and vice versa[8-13] to our knowledge, no similar survey to this study has evaluated the overlap between GERD, IBS and upper gastrointestinal symptoms suggestive of functional dyspepsia in such a large sample consisting of 6476 patients.
21.9% and 41.0% of patients enrolled in the present study had been diagnosed as having IBS and GERD, respectively. The high prevalence of IBS in this survey can be explained by the fact that the place of study had been a referral gastroenterology centre.
63.6% of IBS patients had GERD, and 33.9% of GERD patients also had IBS. Kennedy et al[15] reported 46.5% of GERD patients to have IBS and 47% of IBS patients to suffer from GERD. Hungin et al[2] stated that IBS sufferers were twice as likely to suffer from GERD (22% vs 10%). Guillemot et al[16] in a large clinical based data base reported prevalence equal to 27% for IBS in patients with GERD while Fass et al[17] using a database consisting of about 6000 patients reported a very high prevalence of IBS in GERD patients (60%). Nastaskin et al[18] in a systematic review, reported the prevalence to be about 49%. Lee et al[12] reported a 24% overlap in a Korean population with a sample size of 1400, and a cohort study reported the relative risk of developing IBS in GERD patients to be 3.5[13].
Although clinical judgment of GERD has a sensitivity of 78% and specificity of 60%[6,19], in order to strengthen the method of study we also assessed the overlap of IBS with GERD patients whose diagnosis was confirmed by upper gastrointestinal endoscopy. The considerable overlap still existed and 62.4% of IBS patients also had endoscopically confirmed GERD and 34.4% of endoscopically confirmed GERD patients also had IBS.
By evaluating the frequency of these conditions in relation to the demographic aspects of the affected individuals, we found out that women are more likely to experience GERD and IBS at the same time compared to men, despite the similar sex distribution in GERD only patients. Other studies have demonstrated a higher prevalence of IBS in women[2,20,21], but this study shows a higher proportion of women in GERD + IBS group compared to the prevalence of women in IBS only patients; probably because the same factors which contribute to IBS are more frequent in women than men. One of these factors is sex hormones which was assumed to play a role in IBS, based on the exacerbation of IBS symptoms with the onset of menses[22]. Another possibility might be a lower pain perception threshold in women compared to men; although visceral hyperalgesia is a leading hypothesis for IBS[23-27] there is no available data on the differences in pain perception between men and women.
Functional dyspepsia is consistent with gastrointestinal symptoms such as nausea, vomiting, bloating, and postprandial fullness in the absence of organic disease[5,20,28,29]. It is stated in a review article that 23%-87% of patients with IBS had also functional dyspepsia and 13%-87% of dyspeptic patients complained of IBS[30]. In the current study we examined epigastric pain, nausea, vomiting and belching which were shown to have a higher prevalence in patients presenting with both GERD and IBS in comparison to IBS only patients. This finding suggests a more advanced pathology in patients with both GERD and IBS. Other studies have estimated the prevalence of epigastric pain to be 20%-45%, nausea to be 24%-73% and vomiting to be 7%-27% of IBS patients[31-35]. No similar finding in patients suffering from both GERD and IBS has been reported. 47.8% of patients with both GERD and IBS and 40.5% of IBS patients were associated with one or more functional symptoms. Stanghellini et al[35] observed a high frequency (66%) of functional dyspepsia in IBS patients.
In the present study, we found nausea and vomiting to be the only symptoms differing between men and women. This higher prevalence in women with IBS, GERD and those with both GERD and IBS simultaneously might suggest that the higher occurrence of nausea and vomiting might be interrelated to sex hormones or some biological and psychological differences in men and women. On the other hand the mean age of IBS, GERD and GERD + IBS patients associated with either nausea or vomiting was lower than patients with other symptoms assessed in our survey.
Assessing the role of H. pylori infection in GERD and IBS patients could be a target of future research, as in the present study the prevalence of H. pylori infection in GERD patients was found to be greater than in non-GERD patients; however, we did not find any significant difference in the prevalence of H. pylori infection in patients with IBS or both IBS and GERD.
IBS is also associated with extra intestinal symptoms like frequency and urgency, sexual dysfunction, pains in muscles and joints, dyspareunia, lower back pain, and headaches[36,37]. Whether this increase in frequency of extra intestinal symptoms reflects a systemic underlying disease with different manifestations in different organs or shows psychosomatic disorder is not clear. Here we investigated the frequency of two extra-intestinal symptoms, headache and low back pain in patients with IBS, GERD and GERD + IBS. Results showed that the frequency of these symptoms was significantly higher in patients with both GERD and IBS compared to patients with GERD or IBS alone. This finding might suggest that these diseases may have similar underlying pathophysiology, but they differ in severity. Thus, patients with a severe disorder are more likely to suffer from both IBS and GERD and also extra-intestinal symptoms. There are different hypotheses about the relationship between GERD and IBS. Some suggest that although there might be similar pathophysiology, these are two different diseases and therefore require two different treatments[32,33]. Other groups postulate that visceral hyperalgesia in the GI tract in both GERD and IBS is the main reason for the observed overlap[38]. When patients are hypersensitive or hyperalgesic in the GI tract, there is a higher chance of reporting symptoms of both GERD and IBS, or other functional symptoms as reported by the current study. However, in our population of study, most of the patients presented endoscopic evidence of GERD, therefore hypersensitivity does not explain their GERD symptoms. Others suggest that the ineffective esophageal motility which contributes to GERD is part of a general disorder of smooth muscle movement in the GI tract which contributes to IBS as well[39,40]. There is another hypothesis that suggests GERD might be a systemic disease and IBS like symptoms might be a systemic presentation of GERD[16]. However, in our study there were many patients whose major complaint was IBS and GERD was found during the clinical evaluation.
In conclusion, we suggest that a considerable overlap between GERD and IBS exists with a remarkable predominance in women; we also point to the association of upper gastrointestinal symptoms with IBS in patients suffering from both GERD and IBS, particularly nausea and vomiting, with a significant trend toward affecting women. Because this is a clinic based study, the limitations of this study include the possibility of over-reporting of symptoms by patients and referral bias. Another limitation is that atypical GERD usually includes wheezing, chronic cough, hoarseness or sleep deprivation, however it might present as abdominal discomfort and alterations in bowel movement which may have led to overestimation of IBS prevalence in GERD patients. There is evidence in the literature that prevalence of GERD and IBS in the Iranian population is similar to those reported from western countries[41]. Further studies to clarify the reason for the increased prevalence of these complaints in women are warranted.
COMMENTS
Background
Gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS) are two very common disorders affecting the gastrointestinal tract. About 10% of the population experience daily discomfort from reflux of gastric contents into the esophagus. More than 10% of the population experience abdominal pain and disturbed bowel movements because of IBS.
Research frontiers
Until recently, the dominant view in clinical practice was that GERD and IBS are two different diseases with no link. This view has been challenged by a body of increasing evidence showing that prevalence of IBS like symptoms is very high in patients with GERD and vice versa. This finding inspired research and hypotheses regarding the link between these two diseases. Whether general hyperalgesia in the gastrointestinal tract or a general dysfunction in smooth muscle is responsible for this overlap is not clear.
Innovations and breakthroughs
In the current study, the authors used a large data base from a specialty clinic to investigate the prevalence of overlap between GERD and IBS. They also studied the prevalence of other functional symptoms not related to GERD and IBS in patients in addition to some symptoms outside of the gastrointestinal tract such as headache. They also investigated the correlation between Helicobacter pylori (H. pylori) infection and severity of symptoms. They found out that in addition to significant overlap between GERD and IBS, prevalence of other functional symptoms is much higher in patients with both conditions. H. pylori did not play a significant role in this regard. This finding suggests that GERD and IBS should be considered as parts of the same spectrum of diseases.
Applications
Changes in the way that clinicians and scientists think about GERD and IBS could provide opportunities to change the way we treat these conditions. The response rate of treatment for both of these conditions is not very satisfactory at the moment, hinting that our understanding of the main underlying dysfunction might not be complete. This finding might provide further insight about the correct approach in treatment of these diseases.
Terminology
GERD is characterized by the symptoms of heart burn and regurgitation caused by reflux of stomach contents. IBS is defined as abdominal pain or discomfort associated with altered bowel habits and disordered defecation.
Peer review
In this manuscript, the authors suggest a considerable overlap between GERD and IBS. The study was uniquely performed and very interesting.
Footnotes
Supported by Digestive disease research center, Tehran University of Medical Sciences
Peer reviewers: Dr. Albert J Bredenoord, MD, Department of Gastroenterology, St Antonius Hospital, PO Box 2500, 3430 EM, Nieuwegein, The Netherlands; Tomohiko Shimatani, Assistant Professor, Department of General Medicine, Hiroshima University Hospital, 1-2-3 Kasumi, Minami-ku, Hiroshima 7348551, Japan
S- Editor Wang YR L- Editor O’Neill M E- Editor Zheng XM
References
- 1.Brandt LJ, Bjorkman D, Fennerty MB, Locke GR, Olden K, Peterson W, Quigley E, Schoenfeld P, Schuster M, Talley N. Systematic review on the management of irritable bowel syndrome in North America. Am J Gastroenterol. 2002;97:S7–S26. doi: 10.1016/s0002-9270(02)05657-5. [DOI] [PubMed] [Google Scholar]
- 2.Hungin AP, Chang L, Locke GR, Dennis EH, Barghout V. Irritable bowel syndrome in the United States: prevalence, symptom patterns and impact. Aliment Pharmacol Ther. 2005;21:1365–1375. doi: 10.1111/j.1365-2036.2005.02463.x. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 4.Thompson WG, Heaton KW, Smyth GT, Smyth C. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78–82. doi: 10.1136/gut.46.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frissora CL, Koch KL. Symptom overlap and comorbidity of irritable bowel syndrome with other conditions. Curr Gastroenterol Rep. 2005;7:264–271. doi: 10.1007/s11894-005-0018-9. [DOI] [PubMed] [Google Scholar]
- 6.Nebel OT, Fornes MF, Castell DO. Symptomatic gastroesophageal reflux: incidence and precipitating factors. Am J Dig Dis. 1976;21:953–956. doi: 10.1007/BF01071906. [DOI] [PubMed] [Google Scholar]
- 7.Klauser AG, Schindlbeck NE, Müller-Lissner SA. Symptoms in gastro-oesophageal reflux disease. Lancet. 1990;335:205–208. doi: 10.1016/0140-6736(90)90287-f. [DOI] [PubMed] [Google Scholar]
- 8.Neumann H, Monkemuller K, Kandulski A, Malfertheiner P. Dyspepsia and IBS symptoms in patients with NERD, ERD and Barrett's esophagus. Dig Dis. 2008;26:243–247. doi: 10.1159/000121354. [DOI] [PubMed] [Google Scholar]
- 9.Gasiorowska A, Poh CH, Fass R. Gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS)--is it one disease or an overlap of two disorders? Dig Dis Sci. 2009;54:1829–1834. doi: 10.1007/s10620-008-0594-2. [DOI] [PubMed] [Google Scholar]
- 10.Pimentel M, Rossi F, Chow EJ, Ofman J, Fullerton S, Hassard P, Lin HC. Increased prevalence of irritable bowel syndrome in patients with gastroesophageal reflux. J Clin Gastroenterol. 2002;34:221–224. doi: 10.1097/00004836-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Smart HL, Nicholson DA, Atkinson M. Gastro-oesophageal reflux in the irritable bowel syndrome. Gut. 1986;27:1127–1131. doi: 10.1136/gut.27.10.1127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee SY, Lee KJ, Kim SJ, Cho SW. Prevalence and risk factors for overlaps between gastroesophageal reflux disease, dyspepsia, and irritable bowel syndrome: a population-based study. Digestion. 2009;79:196–201. doi: 10.1159/000211715. [DOI] [PubMed] [Google Scholar]
- 13.Ruigómez A, Wallander MA, Johansson S, Rodríguez LA. Irritable bowel syndrome and gastroesophageal reflux disease in primary care: is there a link? Dig Dis Sci. 2009;54:1079–1086. doi: 10.1007/s10620-008-0462-0. [DOI] [PubMed] [Google Scholar]
- 14.Talley NJ. A unifying hypothesis for the functional gastrointestinal disorders: really multiple diseases or one irritable gut? Rev Gastroenterol Disord. 2006;6:72–78. [PubMed] [Google Scholar]
- 15.Kennedy TM, Jones RH, Hungin AP, O'flanagan H, Kelly P. Irritable bowel syndrome, gastro-oesophageal reflux, and bronchial hyper-responsiveness in the general population. Gut. 1998;43:770–774. doi: 10.1136/gut.43.6.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guillemot F, Ducrotté P, Bueno L. Prevalence of functional gastrointestinal disorders in a population of subjects consulting for gastroesophageal reflux disease in general practice. Gastroenterol Clin Biol. 2005;29:243–246. doi: 10.1016/s0399-8320(05)80756-0. [DOI] [PubMed] [Google Scholar]
- 17.Fass R, Stanghellini V, Monnikes H. Baseline analysis of symptom spectrum in GERD clinical trial patients: result from ReQuest database. Gastroenterology. 2006;130:A629. [Google Scholar]
- 18.Nastaskin I, Mehdikhani E, Conklin J, Park S, Pimentel M. Studying the overlap between IBS and GERD: a systematic review of the literature. Dig Dis Sci. 2006;51:2113–2120. doi: 10.1007/s10620-006-9306-y. [DOI] [PubMed] [Google Scholar]
- 19.Howard PJ, Maher L, Pryde A, Heading RC. Symptomatic gastro-oesophageal reflux, abnormal oesophageal acid exposure, and mucosal acid sensitivity are three separate, though related, aspects of gastro-oesophageal reflux disease. Gut. 1991;32:128–132. doi: 10.1136/gut.32.2.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Everhart JE, Renault PF. Irritable bowel syndrome in office-based practice in the United States. Gastroenterology. 1991;100:998–1005. doi: 10.1016/0016-5085(91)90275-p. [DOI] [PubMed] [Google Scholar]
- 21.Sandler RS. Epidemiology of irritable bowel syndrome in the United States. Gastroenterology. 1990;99:409–415. doi: 10.1016/0016-5085(90)91023-y. [DOI] [PubMed] [Google Scholar]
- 22.Frissora CL, Koch KL. The role of gender and biological sex in irritable bowel syndrome. Curr Gastroenterol Rep. 2005;7:257–263. doi: 10.1007/s11894-005-0017-x. [DOI] [PubMed] [Google Scholar]
- 23.Mertz H, Fullerton S, Naliboff B, Mayer EA. Symptoms and visceral perception in severe functional and organic dyspepsia. Gut. 1998;42:814–822. doi: 10.1136/gut.42.6.814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Camilleri M, Coulie B, Tack JF. Visceral hypersensitivity: facts, speculations, and challenges. Gut. 2001;48:125–131. doi: 10.1136/gut.48.1.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mertz H, Naliboff B, Munakata J, Niazi N, Mayer EA. Altered rectal perception is a biological marker of patients with irritable bowel syndrome. Gastroenterology. 1995;109:40–52. doi: 10.1016/0016-5085(95)90267-8. [DOI] [PubMed] [Google Scholar]
- 26.Mayer EA, Gebhart GF. Basic and clinical aspects of visceral hyperalgesia. Gastroenterology. 1994;107:271–293. doi: 10.1016/0016-5085(94)90086-8. [DOI] [PubMed] [Google Scholar]
- 27.Bouin M, Lupien F, Riberdy M, Boivin M, Plourde V, Poitras P. Intolerance to visceral distension in functional dyspepsia or irritable bowel syndrome: an organ specific defect or a pan intestinal dysregulation? Neurogastroenterol Motil. 2004;16:311–314. doi: 10.1111/j.1365-2982.2004.00511.x. [DOI] [PubMed] [Google Scholar]
- 28.Cremonini F, Talley NJ. Review article: the overlap between functional dyspepsia and irritable bowel syndrome -- a tale of one or two disorders? Aliment Pharmacol Ther. 2004;20 Suppl 7:40–49. doi: 10.1111/j.1365-2036.2004.02184.x. [DOI] [PubMed] [Google Scholar]
- 29.Corsetti M, Caenepeel P, Fischler B, Janssens J, Tack J. Impact of coexisting irritable bowel syndrome on symptoms and pathophysiological mechanisms in functional dyspepsia. Am J Gastroenterol. 2004;99:1152–1159. doi: 10.1111/j.1572-0241.2004.30040.x. [DOI] [PubMed] [Google Scholar]
- 30.Whitehead WE, Palsson O, Jones KR. Systematic review of the comorbidity of irritable bowel syndrome with other disorders: what are the causes and implications? Gastroenterology. 2002;122:1140–1156. doi: 10.1053/gast.2002.32392. [DOI] [PubMed] [Google Scholar]
- 31.Whorwell PJ, McCallum M, Creed FH, Roberts CT. Non-colonic features of irritable bowel syndrome. Gut. 1986;27:37–40. doi: 10.1136/gut.27.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Talley NJ, Phillips SF, Melton J 3rd, Wiltgen C, Zinsmeister AR. A patient questionnaire to identify bowel disease. Ann Intern Med. 1989;111:671–674. doi: 10.7326/0003-4819-111-8-671. [DOI] [PubMed] [Google Scholar]
- 33.Talley NJ. Spectrum of chronic dyspepsia in the presence of the irritable bowel syndrome. Scand J Gastroenterol Suppl. 1991;182:7–10. doi: 10.3109/00365529109109530. [DOI] [PubMed] [Google Scholar]
- 34.Crean GP, Holden RJ, Knill-Jones RP, Beattie AD, James WB, Marjoribanks FM, Spiegelhalter DJ. A database on dyspepsia. Gut. 1994;35:191–202. doi: 10.1136/gut.35.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stanghellini V, Tosetti C, Barbara G, De Giorgio R, Cogliandro L, Cogliandro R, Corinaldesi R. Dyspeptic symptoms and gastric emptying in the irritable bowel syndrome. Am J Gastroenterol. 2002;97:2738–2743. doi: 10.1111/j.1572-0241.2002.07062.x. [DOI] [PubMed] [Google Scholar]
- 36.Lembo AJ, Zaman M, Krueger RF, Tomenson BM, Creed FH. Psychiatric disorder, irritable bowel syndrome, and extra-intestinal symptoms in a population-based sample of twins. Am J Gastroenterol. 2009;104:686–694. doi: 10.1038/ajg.2009.23. [DOI] [PubMed] [Google Scholar]
- 37.Levy RL, Olden KW, Naliboff BD, Bradley LA, Francisconi C, Drossman DA, Creed F. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology. 2006;130:1447–1458. doi: 10.1053/j.gastro.2005.11.057. [DOI] [PubMed] [Google Scholar]
- 38.Jones R, Lydeard S. Irritable bowel syndrome in the general population. BMJ. 1992;304:87–90. doi: 10.1136/bmj.304.6819.87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Costantini M, Sturniolo GC, Zaninotto G, D'Incà R, Polo R, Naccarato R, Ancona E. Altered esophageal pain threshold in irritable bowel syndrome. Dig Dis Sci. 1993;38:206–212. doi: 10.1007/BF01307536. [DOI] [PubMed] [Google Scholar]
- 40.Rubenstein JH, Nojkov B, Korsnes S, Adlis SA, Shaw MJ, Weinman B, Inadomi JM, Saad R, Chey WD. Oesophageal hypersensitivity is associated with features of psychiatric disorders and the irritable bowel syndrome. Aliment Pharmacol Ther. 2007;26:443–452. doi: 10.1111/j.1365-2036.2007.03393.x. [DOI] [PubMed] [Google Scholar]
- 41.Massarrat S, Saberi-Firoozi M, Soleimani A, Himmelmann GW, Hitzges M, Keshavarz H. Peptic ulcer disease, irritable bowel syndrome and constipation in two populations in Iran. Eur J Gastroenterol Hepatol. 1995;7:427–433. [PubMed] [Google Scholar]