Abstract
BACKGROUND
Chest radiographs are often used to diagnose community-acquired pneumonia (CAP), to monitor response to treatment and to ensure complete resolution of pneumonia. However, radiological exams may not reflect the actual clinical condition of the patient.
OBJECTIVE
To compare the radiographic resolution of mild to moderately severe CAP to resolution of clinical symptoms as assessed by the physician or rated by the patient.
DESIGN
Prospective cohort study.
PARTICIPANTS
One hundred nineteen patients admitted because of mild to moderately severe CAP with new pulmonary opacities.
MAIN MEASURES
Radiographic resolution and clinical cure of CAP were determined at day 10 and 28. Radiographic resolution was defined as the absence of infection-related abnormalities; clinical cure was rated by the physician and defined by improvement of signs and symptoms. In addition, the CAP score, a patient-based symptom score, was calculated.
KEY RESULTS
Radiographic resolution, clinical cure and normalization of the CAP score were observed in 30.8%, 93% and 32% of patients at day 10, and in 68.4%, 88.9% and 41.7% at day 28, respectively. More severe CAP (PSI score >90) was independently associated with delayed radiographic resolution at day 28 (OR 4.7, 95% CI 1.3–16.9). All 12 patients with deterioration of radiographic findings during follow-up had clinical evidence of treatment failure.
CONCLUSIONS
In mild to moderately severe CAP, resolution of radiographic abnormalities and resolution of symptoms scored by the patient lag behind clinical cure assessed by physicians. Monitoring a favorable disease process by routine follow-up chest radiographs seems to have no additional value above following a patient's clinical course.
KEY WORDS: community-acquired pneumonia, chest radiography, clinical cure, patients’ perspective, radiology
INTRODUCTION
Chest radiography is an important diagnostic tool in patients suspected of having lower respiratory tract infection to confirm or exclude a diagnosis of pneumonia.
In addition, chest radiographs are often used to monitor poor response to treatment and to ensure complete resolution of pneumonia. In general, radiographs are not recommended for routine follow-up in patients that are clinically improving, although these clinical guideline recommendations are only based on “grade D” recommendations, i.e., expert opinion.1–4 This lack of evidence may lead to unnecessary use of chest radiographs in patients hospitalized because of CAP, a practice that has important health care cost implications given that CAP is one of the leading causes of hospitalization in the western world.5–7 Moreover, the relationship between radiological cure and clinical cure according to the patient’s perspective (self-reported symptoms) has never been studied.
Therefore, we compared radiographic resolution of CAP to clinical cure as assessed by the physician or rated by the patient using a validated symptom score, the CAP score.8 We also assessed clinical parameters and etiology associated with delayed radiographic resolution.
METHODS
Study Population
Details of the study cohort have been reported before.9 In short, adults admitted because of mild to moderately severe CAP [defined as a Pneumonia Severity Index (PSI) score of ≤110] and with radiological evidence of a new opacity were eligible for inclusion.10 All patients were initially treated with intravenous amoxicillin monotherapy.1 On admission, a physical exam, routine laboratory test and a chest radiograph were obtained. Furthermore, we scored pneumonia-related symptoms at enrollment using the CAP score, a short patient-based questionnaire. This validated questionnaire contains eight items for adults admitted to the hospital with CAP based on respiratory symptoms and on well-being.8 The survey provides a CAP respiratory, a CAP well-being and a total CAP score. Low values indicate more severe symptoms. On admission, patients were also asked to retrospectively evaluate their symptoms and general health status 1 month before the onset of pneumonia (pre-pneumonia score). Patients were followed for a maximum of 28 days. At each follow-up visit (day 10 and day 28), we repeated the chest radiography, physical examination, laboratory analyses and CAP score.
Interpretation of Radiographs
The radiologists on call, who had been provided with information on the patient’s clinical condition, evaluated the chest radiographs. Chest radiographs were reviewed according standard radiographic criteria for the presence of opacities, pleural fluid, pulmonary edema, other findings related to infection like atelectasis and pre-existent abnormalities.11, 12 Complete radiographic resolution was defined as the absence of any chest radiographic abnormality potentially related to infection.
Analytical Approach
To compare time to radiographic resolution of CAP with time to clinical cure according to the physician and patient, proportions of radiographic resolution, clinical cure and normalization of the CAP score were compared at each follow-up visit. Clinical cure was defined as (continued) resolution or improvement of symptoms and clinical signs related to pneumonia, without the need for additional or alternative antibiotic therapy by the opinion of the treating physician.13 Normalization of the CAP score was defined as a CAP score equal to or greater than the initial pre-pneumonia score, and this was regarded as a proof of clinical cure according to the patient’s perspective.14 Multivariable regression analysis was performed to assess parameters associated with delayed radiographic resolution on day 10 and 28. In all analyses, two-tailed significance levels of p < 0.05 were used. Statistical analysis was performed with the statistical software package SPSS 15.0. for Windows (SPSS Inc., Chicago, IL).
RESULTS
Study Population
A total of 119 patients with mild to moderately severe CAP (mean PSI score 65.5 ± 22.1; mean age 56.6 ± 17.8 years) were enrolled. About two third of patients (n = 79, 66.4%) had at least one co-morbid illness. In 43 patients (36.1%), a bacterial etiology was established, with Streptococcus pneumoniae as the most frequently identified pathogen, in 33 (27.7%) patients. Data on radiology were obtained in 107 (89.9%) patients at day 10 and in 95 (79.8%) patients at day 28. Eighteen patients (15.1%) showed complete radiological cure after 10 days, and these observations were carried forward.
Radiographic Resolution, Clinical Cure and the CAP Score
Table 1 shows the rates of resolution of radiographic abnormalities associated with CAP. Subgroup analysis indicated that radiographic resolution was slightly slower in patients with S. pneumoniae infection as compared to other etiologies, 24.1% vs. 31.9% at day 10 and 56.0% vs. 69.4% at day 28, respectively.
Table 1.
Patterns of Resolution of Radiological Abnormalities Associated with CAP
| Day | No. | Cumulative dropouta no. (%) | Chest radiograph findings | ||||
|---|---|---|---|---|---|---|---|
| No. (%) | |||||||
| Normal | Opacities | Pleural fluid | Pulmonary edema | Atelectasis/ other findings related to infection | |||
| 0 | 119 | 0 (0%) | 0 (0%) | 119 (100%) | 11 (9.2%) | 5 (4.2%) | 6 (5.0%) |
| 10 | 107 | 12 (10.1%) | 33 (30.8%) | 65 (60.7%) | 17 (15.9%) | 0 (0%) | 15 (14.0%) |
| 28 | 95 | 24 (20.2%) | 65 (68.4%) | 23 (24.2%) | 4 (4.2%) | 0 (0%) | 9 (9.5%) |
aCumulative dropout reflects the number of patients in whom no follow-up radiography was performed
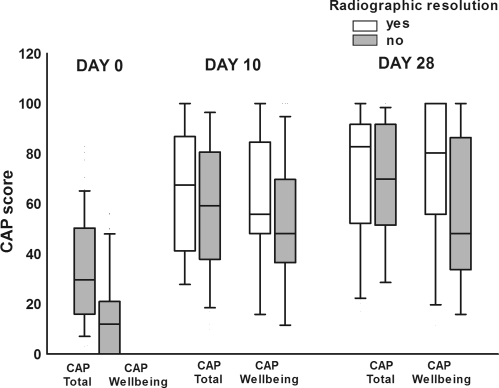
After 10 days of follow-up, clinical cure (physician based) was observed in 106/114 patients (93.0%), normalization of the CAP score in 33/103 patients (32.0%) and radiographic resolution in 33/105 patients (30.8%). At day 28, continued clinical cure was observed in 96/108 patients (88.9%), whereas 43/103 (41.7%) had normalization of the CAP score and 65/95 (68.4%) had complete radiographic resolution. Patients with radiographic resolution at day 10 and day 28 had significantly higher CAP well-being scores at day 10 (62.5 vs. 50.1; p = 0.02) and day 28 (71.6 vs. 59.9; p = 0.02) as compared to patients without radiographic resolution of CAP (Fig. 1).
Figure 1.
Clinical symptoms rated by patients (CAP score) according to radiographic resolution of CAP.
Delayed Radiographic Resolution and Clinical Cure
At day 10, 62 patients (57.9%) had an incomplete radiological response and at day 28 days 30 patients (31.6%); 12/107 (11.2%) patients had deterioration of radiological findings during follow-up. All patients with radiological deterioration had one or more clinical or laboratory signs suggesting clinical failure: fever (n = 11), abnormal auscultatory findings (n = 5), high respiration rate (n = 1), increased inflammatory markers (n = 5) or delayed normalization of the CAP score (n = 10). None of the patients developed deterioration of chest radiography during the second part of follow-up (day 10–day 28).
Multivariable analysis demonstrated that dyspnea on admission was independently associated with delayed radiographic resolution at day 10 (OR 7.4, 95% CI 2.1–26.0; p = 0.002), whereas COPD was associated with a faster radiological recovery (OR 0.3, 95% CI 0.1–0.8; p = 0.01). At day 28, only a PSI score >90 was identified as an independent predictor of delayed radiographic resolution (OR 4.7, 95% CI 1.3–16.9; p = 0.02).
DISCUSSION
We found that about a third of patients (30%) with mild to moderately severe CAP had radiographic resolution after 10 days and 70% after 1 month. This is comparable to previous studies that reported radiological cure rates of 35.1% to 87% 3 to 4 weeks after diagnosis of CAP.15–18 We used a more strict definition of radiological cure that might underestimate radiological cure rate, because patients with some improvement on chest radiography were classified as having no radiological cure. This stricter definition makes good clinical sense since confirmation of complete radiological clearance is important to exclude a non-infectious underlying cause of pneumonia or radiographic abnormalities, such as obstructing tumors.
We also showed that radiological cure and resolution of symptoms as rated by patients lags behind clinical cure as assessed by physicians. Apparently, when patients are considered cured by their physician, they do not feel they are back to baseline.
Patients with pneumococcal pneumonia had a slower resolution of infectious-related findings on the chest radiograph as compared to patients with a viral or unknown etiology of pneumonia. This is line with several previous studies demonstrating a slower resolution in pneumococcal and legionella pneumonia as compared to other etiologies.5, 19 The reason for delayed radiological cure in a S. pneumoniae infections may be explained by the development of complications that are related to pneumococcal pneumonia, like pleural effusion or empyema.20 The severity of CAP was also an independent predictor of delayed radiographic resolution, similar to our previous studies in severe CAP where rates of radiographic resolution were lower than in current study of mild to moderately severe CAP (1 week: 25% vs 50%, 1 month: 30% vs 70%).5
All 12 patients who experienced deterioration of the chest radiograph during follow-up had clinical signs of deterioration. Since only 30% of patients had radiological cure at 10 days, incomplete resolution of pulmonary infiltrates in the absence of clinical deterioration should not be a reason for treatment changes.
In conclusion, complete radiological clearance rate in patients with mild to moderately severe pneumonia is 30% after 10 days and 70% after 1 month. Severity of pneumonia on admission was associated with delayed radiological clearance. Radiographic resolution and resolution of symptoms as scored by the patient lag behind clinical cure as assessed by physicians. All patients with deterioration of radiographic findings during follow-up had clinical evidence of treatment failure. Therefore, monitoring a favorable disease process by means of routine short-term follow-up chest radiography in patients with mild to moderately severe CAP leads to unnecessary resource use and has no additional value above clinical decisions based on patient’s clinical symptoms. Based on the present study, follow-up chest radiographs to exclude underlying diseases should not be performed within 4 weeks after initial diagnosis. Further studies to more clearly define an optimal time frame for follow-up chest radiographs, or if such follow-up is ever indicated, are needed.
Acknowledgment
We thank all the patients and investigators who participated in this trial. This study was presented at the 48th Interscience Conference on Antimicrobial Agents and Chemotherapy and the Infectious Disease Society 46th annual meeting, Washington, DC, 2008 (no. 2002).
Transparency declarations The study was approved by the medical ethics committees of all participating hospitals.
Conflicts of interest None disclosed.
Financial support Health care insurance board, Amstelveen, The Netherlands (grant OG99-038).
Footnotes
This research was supported by a health care insurance board grant, Amstelveen, The Netherlands (grant OG99-038).
References
- 1.Schouten JA, Prins JM, Bonten MJ, et al. Revised SWAB guidelines for antimicrobial therapy of community-acquired pneumonia. Neth J Med. 2005;63:323–35. [PubMed] [Google Scholar]
- 2.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2):S27–72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mandell LA, Marrie TJ, Grossman RF, Chow AW, Hyland RH. Canadian guidelines for the initial management of community-acquired pneumonia: an evidence-based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. The Canadian community-acquired pneumonia working group. Clin Infect Dis. 2000;31:383–421. doi: 10.1086/313959. [DOI] [PubMed] [Google Scholar]
- 4.Woodhead M, Blasi F, Ewig S, et al. Guidelines for the management of adult lower respiratory tract infections. Eur Respir J. 2005;26:1138–80. doi: 10.1183/09031936.05.00055705. [DOI] [PubMed] [Google Scholar]
- 5.Bruns AH, Oosterheert JJ, Prokop M, Lammers JW, Hak E, Hoepelman AI. Patterns of resolution of chest radiograph abnormalities in adults hospitalized with severe community-acquired pneumonia. Clin Infect Dis. 2007;45:983–91. doi: 10.1086/521893. [DOI] [PubMed] [Google Scholar]
- 6.Granet KM, Wallach SL, Horvath K, Jaeger J. Chest radiographs in patients with community-acquired pneumonia. N J Med. 1996;93:37–41. [PubMed] [Google Scholar]
- 7.Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA. 2005;294:2712–9. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- 8.Moussaoui R, Opmeer BC, Bossuyt PM, Speelman P, Borgie CA, Prins JM. Development and validation of a short questionnaire in community acquired pneumonia. Thorax. 2004;59:591–5. doi: 10.1136/thx.2003.015107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moussaoui R, Borgie CA, van den BP, et al. Effectiveness of discontinuing antibiotic treatment after 3 days versus 8 days in mild to moderate-severe community acquired pneumonia: randomised, double blind study. BMJ. 2006;332:1355. doi: 10.1136/bmj.332.7554.1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fine MJ, Auble TE, Yealy DM, et al. A prediction rule to identify low-risk patients with community-acquired pneumonia. N Engl J Med. 1997;336:243–50. doi: 10.1056/NEJM199701233360402. [DOI] [PubMed] [Google Scholar]
- 11.Fraser R, Pare J, Pare P, et al. Diagnosis of Diseases of the Chest. Philadelphia: W.B. Saunders Company; 1998; 4, 461;494–511;545–573;663–667.
- 12.Virkki R, Juven T, Mertsola J, Ruuskanen O. Radiographic follow-up of pneumonia in children. Pediatr Pulmonol. 2005;40:223–7. doi: 10.1002/ppul.20258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chow AW, Hall CB, Klein JO, Kammer RB, Meyer RD, Remington JS. Evaluation of new anti-infective drugs for the treatment of respiratory tract infections. Infectious Diseases Society of America and the Food and Drug Administration. Clin Infect Dis. 1992;15(Suppl 1):S62–88. doi: 10.1093/clind/15.Supplement_1.S62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moussaoui R, Opmeer BC, Borgie CA, et al. Long-term symptom recovery and health-related quality of life in patients with mild-to-moderate-severe community-acquired pneumonia. Chest. 2006;130:1165–72. doi: 10.1378/chest.130.4.1165. [DOI] [PubMed] [Google Scholar]
- 15.Mittl RL, Jr, Schwab RJ, Duchin JS, Goin JE, Albeida SM, Miller WT. Radiographic resolution of community-acquired pneumonia. Am J Respir Crit Care Med. 1994;149:630–5. doi: 10.1164/ajrccm.149.3.8118630. [DOI] [PubMed] [Google Scholar]
- 16.Solh AA, Aquilina AT, Gunen H, Ramadan F. Radiographic resolution of community-acquired bacterial pneumonia in the elderly. J Am Geriatr Soc. 2004;52:224–9. doi: 10.1111/j.1532-5415.2004.52059.x. [DOI] [PubMed] [Google Scholar]
- 17.Eisernberg GM, Flippin HF, Isael HL, Strandness de Jr, Weiss W. Delayed resolution of pneumonias. Med Clin North Am 1956;40:1291–303. [DOI] [PubMed]
- 18.Metre T. Pneumococcal pneumonia treated with antibiotics; the prognostic significance of certain clinical findings. N Engl J Med. 1954;251:1048–52. doi: 10.1056/NEJM195412232512604. [DOI] [PubMed] [Google Scholar]
- 19.Macfarlane JT, Miller AC, Roderick Smith WH, Morris AH, Rose DH. Comparative radiographic features of community acquired Legionnaires' disease, pneumococcal pneumonia, mycoplasma pneumonia, and psittacosis. Thorax. 1984;39:28–33. doi: 10.1136/thx.39.1.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alfageme I, Munoz F, Pena N, Umbria S. Empyema of the thorax in adults. Etiology, microbiologic findings, and management. Chest. 1993;103:839–43. doi: 10.1378/chest.103.3.839. [DOI] [PubMed] [Google Scholar]