Abstract
BACKGROUND
Physicians can play a significant role in helping to decrease the hepatitis B virus (HBV) burden among Asian Americans. Few studies have described knowledge and practice patterns in the medical community among different provider types regarding HBV and liver cancer.
OBJECTIVE
Our study explores the HBV beliefs, attitudes and practice patterns of medical providers serving Asian American communities.
DESIGN
We conducted three focus groups with primary care providers, liver specialists, and other providers predominantly serving Asian American community. We asked about practices and barriers to appropriate medical care and outreach.
PARTICIPANTS
We moderated three focus groups with 23 participants, 18 of whom completed and returned demographic surveys. Twelve were of Asian ethnicity and 13 spoke English as a second language. Only eight screened at least half of their patients, most (72%) using the hepatitis B surface antigen test.
APPROACH
We used grounded theory methods to analyze focus group transcripts.
RESULTS
Participants frequently discussed cultural and financial barriers to hepatitis care. They admitted reluctance to screen for HBV because patients might be unwilling or unable to afford treatment. Cultural differences were discussed most by primary care providers; best methods of outreach were discussed most by liver specialists; and alternative medicine was discussed most by acupuncturists and other providers.
CONCLUSIONS
More resources are needed to lower financial barriers complicating HBV care and encourage providing guideline-recommended screenings. Other providers can help promote HBV screening and increase community and cultural awareness.
KEY WORDS: provider attitudes, Hepatitis B, Asian Americans, qualitative research, focus groups
BACKGROUND
Hepatitis B virus (HBV) is a human carcinogen responsible for liver carcinoma.1 HBV is transmitted through percutaneous contact with infectious blood or body fluids, such as sex with infected partners, needle sharing, or birth to infected mothers.2 Of the estimated 1.2 to 2 million people in the US diagnosed with chronic HBV, over half are Asian Americans.3 The prevalence of chronic HBV among foreign-born Asian Americans is approximately 10%2, compared to 0.5% in the overall US population and 0.2% in whites. A fourth of individuals with untreated HBV die from liver cancer or cirrhosis.4 Since Asian Americans have the highest rates of chronic hepatitis B among all racial and ethnic groups in the US, they are also at disproportionately high risk of liver cancer, which is the third leading cause of cancer death among Asian Americans in the US, compared to 16th among whites.2,5,6
Previous research in the US has shown that lack of patient knowledge about HBV is associated with lack of screening.7–10 In turn, lack of screening and delays in diagnosis increase morbidity and mortality. Physicians play a significant role in decreasing the HBV burden among Asian Americans by improving the identification and care of persons with chronic HBV,11 promoting patient knowledge about HBV and liver cancer, and advising patients to get screened or follow treatment recommendations.12–16 Effective patient–physician communication can improve patients’ use of health care services and compliance with health care directives.17–19 Problems with communication may negatively affect patients’ perceptions of illness, screening, and treatment.20,21
Little is known about HBV knowledge and practices among different provider types. One study that targeted providers serving Asian American communities was a retrospective cohort study of health care providers’ knowledge and practices regarding HBV in Chinese-speaking patients. The authors found that many providers underestimated HBV risk.22 Surveys can provide quantitative accounts of practice patterns, but more in-depth exploration is needed to uncover factors that may impact practice. We conducted an in-depth qualitative study to better understand and elucidate the beliefs, attitudes and practice patterns of medical providers serving Asian American communities.
METHODS
After receiving approval from the institutional review board at The University of Texas M. D. Anderson Cancer Center, we performed a qualitative study involving focus groups with primary care providers (internal medicine, family and general practice), specialists (hepatologists and gastroenterologists), and other providers (pediatricians, obstetrician/gynecologists, other surgeons, and acupuncturists) who serve Houston’s Chinese, Korean, and Vietnamese communities, and manage health issues related to HBV. We included liver specialists, acupuncturists, and physicians of gastroenterology, hepatology internal medicine, family practice and obstetrics and gynecology because they play a similar role in HBV-related diagnosis, treatment and care for Asian Americans. In order to conduct the focus group in English, we excluded non-English-speaking participants.
We gathered a purposive sample of physicians serving the Asian American community, stratified into three specialty groupings (primary care physicians, liver specialists, and other providers). We compiled names and contact information for 41 primary care providers, 39 liver specialists, and 64 other medical providers from community resources such as the Asian yellow pages, advertisements in Asian newspaper classifieds, Houston Asian physician organizations, and word-of-mouth. We sent all 144 potential participants a mailed invitation, and then followed-up by e-mail, fax, or phone describing our study and asking individuals to participate. All groups were comprised of Asian and non-Asian physicians stratified by medical specialty. Homogeneous groups encourage willingness among those with similar experiences to share and are recommended in investigating complex or sensitive motivations and issues.23 Each participant was asked to complete a demographic and clinical practice questionnaire. Focus groups were conducted at local restaurants, and participants received meal reimbursements up to $75.
Each focus group included five to nine participants, an optimal number to ensure an intimate, trusting environment and still retain significance, variety, and representativeness of the ideas shared.23,24 The moderator (J.H.) followed an interview training manual created for use in qualitative research in hepatitis among Korean American,25,26 which she adapted for medical providers. The guide was developed for focus groups of Asian Americans, then adapted for health care providers by our study’s principal investigator. The moderator followed a script of questions (see Table 1) but allowed probes and participant interest redirect the conversation. Focus group sessions were conducted in English, audiotaped and transcribed. Transcripts were validated against the recordings to ensure accuracy.
Table 1.
Core Focus Group Questions
| Themes | Questions | Probes |
|---|---|---|
| Barriers to appropriate medical care | What are the major medical problems of Asian Americans? | What are patients’ knowledge / attitudes about HBV? |
| In your patient population, what is the prevalence of HBV among Asian Americans? | Why are Asian Americans at high risk? | |
| What are the barriers to medical care? | Blood attitudes? Language? Transportation? Money? | |
| Outreach | What are the best ways to reach out and educate the Asian American community? | Is there low interest among Asian Americans? Why? What should we do to improve interest? |
| What future interventions would be helpful to the Asian American community? | Physician network? Screening? Education? What role can the community MD play? | |
| Clinical knowledge and practice | Describe what you and your patients do to treat HBV | Interferon, Adefovir, Lamivudine, Entacavir? How do most patients get their medicines? |
| What are effective alternative and unconventional primary treatments you have prescribed for HBV patients? | What unconventional methods have worked? What have some of your patients done to treat HBV themselves? |
We used grounded theory methods to code the transcripts,27,28 an approach that allows building a theory that fits data and encourages new insights by coding quotations for emerging themes and building consensus between coders about the relationships between themes. Two investigators coded each transcript independently, and then met to compare codes and resolve discrepancies through discussion. We conjoined similar codes, eliminated duplicates, categorized codes into major themes, and identified relationships and a framework interconnecting and explaining those themes. Transcripts were imported into NVivo® software (Melbourne, Australia) which was used to record our consensus themes, tally code frequencies, and code relationships. We used a constant comparison method, by which we tested and applied our coding categories to each new transcript.
RESULTS
We sought to explore the attitudes, behaviors and social realities that inform how providers deliver HBV care to Asian American communities. The basic social problem facing providers was how to provide care, given cultural and financial barriers. Providers suggested solving the problem by trying to bridge cultural differences with translators, community-based outreach, and CAM awareness and by streamlining screening and care to cut expenses. We identified eleven core themes that occurred most often when providers were asked about clinical knowledge, barriers to care and recommendations for outreach. (See Table 2 for theme definitions.) Several common emerging themes occurred in all three focus groups, but some differences were also observed among provider groups.
Table 2.
Definitions of Emerging Themes, in Alphabetical Order
| Themes | Questions |
|---|---|
| Community buy-in | Suggesting venues, community involvement, and other recommendations for promoting awareness |
| Complementary and alternative medicine (CAM) | Describing uses of and knowledge and attitudes about complementary and alternative medicine |
| Cultural differences | Sharing an awareness of cultural habits, values and statistics related to HBV |
| Finance barriers | Describing problems affording HBV care and insurance |
| Language barriers | Describing language differences and translation problems |
| Linking to liver cancer | Understanding the risks and causes of liver cancer |
| Prevention | Sharing strategies for and attitudes about prevention |
| Provider knowledge | Sharing knowledge about HBV prevalence, referrals, and the provider’s role in awareness and education |
Overall, providers felt that financial barriers to patients affected how they practiced. Some demonstrated gaps in provider knowledge that might weaken the role they play in patient education. As well, language barriers, cultural differences, complementary and alternative medicine (CAM), and community buy-in were important in outreach to patients.
Demographic and Practice Characteristics
Twenty-three medical providers participated in the three focus groups, 18 of whom (all six primary care providers, seven of nine liver specialists, and five of eight other providers) completed an optional demographic survey. Participant characteristics of these 18 medical providers are summarized in Table 3. Three quarters of those who completed the survey were male, ages 40–65 (78%), more than two thirds were Asian and spoke English as a second language and the majority had graduated from medical training programs outside the US. Four liver specialists reported screening 75% or more of their patients for HBV; three primary care providers, 50% to 75%; and four other providers, 25%. Most of the providers used the hepatitis B surface antigen test (HBsAg), either alone or in combination with other tests, to screen patients for HBV and served patient populations who were up to 50% Asian. Two out of three reported that only a quarter of their patients had health insurance, and a similar proportion stated that they used translators as needed during office visits with Asian American patients. Houston’s Asian American population is 49.7% male and 74.9% adult (ages 18 and over). The median household income is approximately $66,414 and about 10% fell below the poverty line.29
Table 3.
Demographics of Study Participants
| No. (%) of Participants | ||||
|---|---|---|---|---|
| Primary care providers (n = 6) | Liver specialists (n = 7) | Other medical providers (n = 5) | Total (n = 18) | |
| Age, years | ||||
| <30 | 0 | 0 | 2 (40) | 2 (11) |
| 30-39 | 0 | 1 (14) | 1 (20) | 2 (11) |
| 40-49 | 2 (33) | 3 (43) | 0 | 5 (28) |
| 50-65 | 3 (50) | 2 (29) | 1 (20) | 6 (33) |
| >65 | 1 (17) | 1 (14) | 1 (20) | 3 (17) |
| Gender | ||||
| Male | 5 (83) | 6 (86) | 3 (60) | 14 (78) |
| Specialty | ||||
| Gastroenterology/Hepatology | 0 | 7 (100) | 0 | 7 (38) |
| Internal medicine | 3 (50) | 0 | 0 | 3 (17) |
| Family practice | 3 (50) | 0 | 0 | 3 (17) |
| Obstetrics/Gynecology | 0 | 0 | 1 (20) | 1 (6) |
| Acupuncturist | 0 | 0 | 2 (40) | 2 (11) |
| Other | 0 | 0 | 2 (40) | 2 (11) |
| Completed US Residency? | ||||
| Yes | 6 (100) | 6 (86) | 3 (60) | 15 (83) |
| Graduate of US medical school? | ||||
| Yes | 1 (17) | 3 (43) | 3 (60) | 7 (39) |
| Ethnicity | ||||
| Chinese | 3 (50) | 0 | 3 (60) | 6 (33) |
| Korean | 1 (17) | 0 | 2 (40) | 3 (17) |
| Vietnamese | 2 (33) | 1 (14) | 0 | 3 (17) |
| Latino | 0 | 1 (14) | 0 | 1 (6) |
| Caucasian | 0 | 3 (43) | 0 | 3 (17) |
| Other | 0 | 2 (29) | 2 (11) | |
| Native tongue | ||||
| Chinese | 3 (50) | 0 | 0 | 3 (17) |
| Korean | 1 (17) | 0 | 2 (40) | 3 (17) |
| Vietnamese | 2 (33) | 1 (14) | 0 | 3 (17) |
| English | 0 | 3 (43) | 2 (40) | 5 (28) |
| Other | 0 | 3 (43) | 1 (20) | 4 (22) |
| % of patients who are Asian American | ||||
| 25% | 2 (33) | 4 (57) | 4 (80) | 10 (56) |
| 25-50% | 1 (17) | 1 (14) | 0 | 2 (11) |
| 50-75% | 2 (33) | 0 | 1 (20) | 3 (17) |
| >75% | 1 (17) | 1 (14) | 0 | 2 (11) |
| No answer | 0 | 1 (14) | (0) | 1 (6) |
| % of patients with insurance | ||||
| 0% | 0 | 1 (14) | 0 | 1 (6) |
| 25% | 5 (83) | 4 (57) | 3 (60) | 12 (67) |
| 25-50% | 1 (17) | 1 (14) | 0 | 2 (11) |
| 50-75% | 0 | 0 | 2 (40) | 2 (11) |
| >75% | 0 | 1 (14) | 0 | 1 (6) |
| Use translator as needed during visits with Asian American patients | 4 (67) | 6 (86) | 2 (40) | 12 (67) |
| HBV screening testsa | ||||
| HBsAg | 6 (100) | 6 (86) | 1 (20) | 13 (72) |
| anti-HBe | 4 (67) | 2 (29) | 2 (40) | 8 (44) |
| anti-HBc | 4 (67) | 3 (43) | 1 (20) | 8 (44) |
| % of patients screened for HBV | ||||
| 25% | 1 (17) | 0 | 4 (80) | 5 (28) |
| 25-50% | 2 (33) | 1 (14) | 0 | 3 (17) |
| 50-75% | 3 (50) | 1 (14) | 0 | 4 (22) |
| >75% | 0 | 4 (57) | 0 | 4 (22) |
| No answer | 0 | 1 (14) | 0 | 1 (6) |
a HBsAg, hepatitis B surface antigen; anti-HBe, antibody to hepatitis B early antigen; anti-HBc, antibody to hepatitis B core antigen
Our findings below reflect responses from all 23 focus group participants, including 5 who did not complete demographic surveys.
Financial Barriers
When asked to describe HBV treatment, providers responded that financial impediments deterred treatment and screening, and they acknowledged that patients lacked linkage to care—e.g., limiting health options for HBV-positive patients—which discouraged patients and providers from screening. Participants admitted being somewhat reluctant to diagnose HBV because of anticipated problems with the affordability of care. Knowing that patients might not seek care discouraged providers from screening. Several responses compared the expensiveness of Western medicine to the accessibility and inexpensiveness of complementary and alternative medicine (CAM).
“[T]hey’re coming to us to have screening. But the problem is after screening, if they’re positive for [HBsAg], they do not have the money or support for process for diagnosis or treatment.”
“[CAM is] ready for them to use and cheap.”
The cost of care influenced decisions regarding whom to immunize and screen and how to do it. Providers made attempts to streamline screening to make the process faster and more affordable, although cutting corners could ultimately miss patients who were positive for antibody to hepatitis B core antigen, but negative for HBsAg. Some used other cost-minimizing screening strategies.
“[I]f you do the three tests, it doesn’t make…sense…I’m very pragmatic. I check the HBsAg, I check the hepatitis C antibody. If you are negative, you don’t have to worry. You don’t have hepatitis B and you don’t have the hepatitis C.”
“[I]f you order the panel—that is cheaper than if you have to order labs separately. If you use HBsAg [alone], that costs more than the panel with A, B, and C.”
Provider Knowledge
Discussions revealed both accuracies and limitations of provider knowledge. Most physicians accurately described the biological mechanisms of HBV transmission—i.e., through exchange of bodily fluids, vertical transmission from mother to child, and needle sharing. The other providers group was aware of culturally-specific transmission—i.e., in nail salons, particular drug use, etc.
“[T]hey [are] spreading inadvertently—people going to nail salons, get their nails filed all the time. My wife used to go and her fingers were always bleeding.”
Some providers had incorrect information about HBV transmission in the Asian population, attributing its spread to cultural dietary practices and poor hygiene.
“Because Korean custom is we eat together like when you drink wine and we made soup, if bowl soup, we eat together. We don’t separate.”
Participants felt confident about the efficacy of treatments for HBV, but many believed that the Asian American community did not share their confidence.
“[A]fter the treatment stops, [they fear] that the [disease] will return. ... They don’t trust the [treatment].”
Language Barriers and Cultural Differences
Across groups, language and cultural differences were mentioned as barriers to the role providers played in education and outreach. Even though most participants used language translators in their clinical practice (67%), and for many an Asian language was their native tongue (51%), language differences still prevented optimal HBV screening and optimal education about important aspects of HBV care. Failure to translate medical directives and jargon discouraged follow-up, and providers feared this would widen information gaps and increase prevalence of HBV.
“You can tell even [when you’re explaining it] in Vietnamese…; they still don’t understand that point. I can stand there…hours talking about hepatitis. They [come] out of the room and they tell my secretary ‘What did [the doctor] talk about?’”
“We try to get them to understand the basis of their disease and half the time it works very well and half the time it doesn’t. I can tell you people have left my clinic and never come back.”
Language and cultural barriers discouraged non-Asian physicians from providing HBV outreach to the Asian American community and prioritized the role of the Asian physician essential as educator and advocate.
“[T]here’s a certain resistance to seeing non-Asian physicians, especially for people born in Asian countries, and as a physician, I don’t know what we can do about that. We’ve actually…hire[d] an Asian physician, thinking they would be a better reach into a community that may not very open to coming to a non-Asian center.”
Complementary and Alternative Medicine (CAM)
Providers had mixed attitudes about the virtues of CAM, which includes medications and practices not generally taught in Western biomedical education. Physicians were hesitant about CAM, in particular, ingested substances. Providers worried that CAM might interfere with Western medicine.
“Some of the [CAM] people take is extremely poor, not very well made…Every year we see a couple of people with [liver or kidney] failure…because they taking some herb that someone told them it’s good for them.”
“Most of our protocols have involved research of [the] liver…most of them will prohibit botanicals and alternative complementary medicine.”
Despite admitted reservations, participants understood the importance of CAM in providing medical care to the Asian American community. Other providers shared CAM treatments they had either prescribed or considered prescribing to their patients, including acupuncture, vitamins, energy medicine, and herbs. They also discussed using CAM as a complementary treatment to be used alongside Western medicine. Liver specialists saw CAM as an opportunity to demonstrate mutual respect for different medical traditions. In turn, they thought negative attitudes about CAM might be misconstrued by patients as cultural insensitivity.
“[I]n the same way I don’t disrespect them, I’m asking them not to disrespect the things I’ve been trained so that we continue in parallel.”
“You can read the protocols and most of them will prohibit botanicals and alternative complementary medicine. You know, and that may be a mistake because road blocks saying I reject where you’re coming from, therefore you’re rejecting them from their very entry, how can you expect to bridge a line with them?”
Participants shared what they perceived were their patients’ attitudes about CAM. Primary care physicians acknowledged its popularity with their Asian American patients, who perceived CAM as a safe alternative to Western medicine. Patients were known to use CAM, but kept this information from their physicians.
“I think like most of the Asian population who believe in herbal medicine, and they believe herbal medicine is a non-chemical kind of treatment, therefore there will be no side effects, they don’t know that those that take herbal medicine can get liver pain but they don’t know”.
“[M]ost people will not admit to me that they’re using something else.”
Community Buy-in
Participants recommended particular outreach methods—e.g., community buy-in (or targeting community through culturally-specific organizations and venues such as Buddhist temples and Asian-language newspapers). Providers stressed the importance of developing culturally sensitive messages for culturally specific media outlets. Many suggested modeling Asian American outreach campaigns on best practices employed for other ethnic groups and cities and for other public health initiatives. Community centers, churches and temples, community organizations, and Asian-language newspapers, TV stations, and radio stations were the most often recommended outreach venues.
“I think that if we want to reach these patients, we should try to identify positions that are close to the community.”
Group Comparisons
Primary care providers The theme most often discussed by primary care providers was cultural differences that complicated care and outreach. In particular, participants feared that Asian American communities underestimated the disease and its prevalence. “I feel that even in Chinese American population, the appreciation is…they know hepatitis B is no good, but they really, not quite realize how serious that is.”
Liver specialists The theme most often discussed by liver specialists was outreach methods. Participants were interested in lowering barriers, offering incentives, and exploiting pre-existing fixtures of the community to increase community buy-in regarding screening, treatment, and prevention. “If we want to reach these patients, we should try to identify positions that are close to the community.”
Other medical providers The theme most often discussed by other medical providers was CAM. Overall, the group clarified how and why they used CAM—namely, (1) for very specific physical effects (“I can say main function of acupuncture is [to] dilate blood vessel…circulation of oxygen…to cells. So one of [its uses] is [for] blood clots.”), (2) as a complement to Western medicine for treating side effects (“If someone said, ‘I was nauseated and acupuncture made me feel better,’ I’m not going to argue with them. I’m going to say, ‘Great! If it makes you feel better, that’s fine.’”), and (3) for alleviating fatigue (“For hepatitis and AIDS, like that, for some immune system low patients, I give them some energy medicine or something like that.”). Screening concerns were among the three most frequently discussed issues among primary care providers and liver specialists, but not among other providers.
CONCLUSIONS
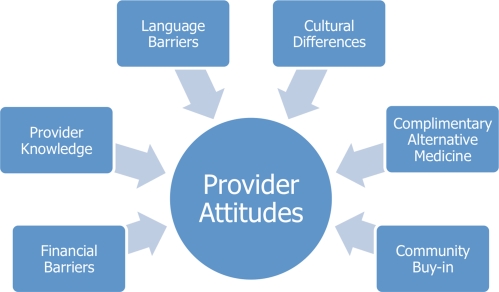
Our study revealed factors that influenced HBV screening and treatment practices: financial barriers, provider knowledge, language barriers, cultural differences, CAM, and community buy-in (Figure 1).
Figure 1.
Conceptual model of factors affecting provider practices regarding HBV screening and treatment.
Financial concerns not only hinder patients from seeking and sustaining care, but also drive physician behavior. Patients’ lack of resources influenced physicians’ approaches to HBV screening and management. Whether patients can afford care often influenced the types of serologic tests that physicians ordered, despite guidelines which recommend that all persons born in regions with high or intermediate endemicity be screened for HBV.30–35 Furthermore, providers felt conflicted about diagnosing patients who could not afford follow-up treatment. Other studies have found variance in how practitioners handle HBV prevention and treatment.36–39 Our study revealed financial domains of influence. If this finding were to be replicated in a larger, nationally representative sample of providers, it could help policymakers and insurance providers find better ways to encourage guideline-recommended services to high-risk groups.
We also found that provider knowledge may be an obstacle to appropriate care. While primary care providers and other medical professionals accurately explained the general etiology of HBV, some did not accurately explain disease transmission among Asian Americans. Other studies have reported gaps in physician knowledge about the natural history, risk factors, and test results for hepatitis.22,40 Our study identified disease transmission as a new area in which there is an information gap. Patients’ understanding of transmission and disease treatment has been found to deviate from clinical knowledge and recommendations.22,41–44 Continuing medical education (CME) for providers in HBV transmission might serve to bridge the gaps.
Our findings suggest that providers perceived cultural differences between themselves and patients as affecting patient education, outreach and patients' healthcare decisions. We found that, even in instances where providers and patients shared racial or ethnic concordance, it was difficult to translate complicated medical terms and directives. Other studies have found that providers misunderstand Asian community conceptions of illness, prevention, and pain.45 Race and ethnic concordance between provider and patient have been associated with providers' willingness to screen for HBV, patients’ perceptions of physician bedside manner, and patients' willingness to comply with health-care directives.46–48 However, there are other means by which physicians can demonstrate respect or trust without requiring race or ethnic concordance, including increasing familiarity with patients and understanding their cultural values and beliefs.49,50
Finally, CAM presented itself as a topic that physicians leveraged to demonstrate cultural sensitivity. Physicians’ and patients’ attitudes about CAM reflected cultural differences that affected care. Physicians saw potential for CAM as complementary to Western medicine, but they feared that patients’ use of CAM—and patients’ suspicions that Western medicine providers distrust CAM—might increase HBV morbidity by discouraging and delaying Western medical treatments. Increasing awareness on the part of physicians about the acceptable uses of CAM might serve as a means to help bridge cultural differences between patients and providers.
Our findings show that, while providers might not have approved of their patients relying solely on CAM, they have a growing understanding of CAM as a complement to Western treatment and as a means to bridge cultural differences. These findings are in agreement with studies suggesting that, though Western medicine practitioners may be unfamiliar with the specifics of CAM, they are increasingly accepting of it.51–55 Our findings are also in agreement with studies showing that CAM and traditional medicine providers are interested in collaborating on outreach and research.56,57 Acupuncturists and other medical provider groups should be encouraged to work in concert with liver specialists and primary care physicians to encourage screening. Furthermore, since prevention was mentioned less frequently by liver specialists and primary care physicians, these providers should be enlisted to encourage prevention.
Variations in major themes by clinician group type reflected each group's natural concerns. The other medical provider groups felt compelled to explain their practice of CAM. Liver specialists felt it important to find more effective ways to increase HBV awareness, and primary care physicians—who may see patients most often—frequently discussed how cultural differences affected provider-patient communication and relationships.
Physician demographics may have affected response outcomes. Most of our participants were male, and while most completed US residencies, fewer than half of the primary care physicians and liver specialists graduated from US medical schools. The other medical providers were younger than the liver specialists and primary care physicians. Studies suggest that how long a provider has been in practice and whether a provider is male or female can influence quality of care, provider–patient communication, and provider attitudes about CAM.58–60 Where providers obtained their medical training may also play a role.61,62 However, qualitative studies are local and include small sample sizes; therefore we cannot generalize this conclusion.
Our findings also give a glimpse into participants’ levels of cultural competency, or providers’ sensitivity to cultural health beliefs, commitment to hiring a diverse staff and providing language assistance services and document translation, and awareness of patients as individuals capable of making their own healthcare decisions rather than as stereotypes.5,63 By these standards, our participants demonstrated cultural competency, insofar as they suggested solutions to language barriers, respected CAM as an integral part of Asian American culture and a means by which patients’ attempted to be proactive about their healthcare, and recommended recruiting more physicians and advocates from within the Asian American community.
We were surprised that women’s health and health practices did not emerge as a code category, particularly since women are often both a vector of transmission and an influential figure in the Asian American community. Adding homogeneous focus groups of pediatricians and OB/GYNs might have lent more data in this regard, given that these two groups provide perinatal and post-partum neonatal care—two important entry points in HBV care. Finally, liver cancer and HBV did not thrive as a code category, possibly because physicians were of the opinion that eradicating HBV to prevent liver cancer might not be directly applicable over a heterogeneous cohort of Asian American patients.
Our study was qualitative and not designed to produce generalizable findings. Nevertheless the insights uncovered here may have some applicability to other populations and settings. Having conducted more focus groups might have yielded more discussion of emerging themes. Typically, conducting at least two groups per variable of interest is recommended to ensure theme saturation.23 Our focus groups represented a variety of perspectives. the constant comparison method used to analyze all three transcripts ensured internal validity.24 Although this study addressed clinicians’ perspectives, we recognize that patient perspectives are also important in obtaining a more complete understanding of HBV outreach and barriers to care.
Our results suggest implications for outreach strategies for all providers. Liver specialists and primary care providers could play more of a key role in promoting prevention; acupuncturists and others beyond liver specialists and primary care providers could play more of a key role in promoting screening and treatment. Other practitioners do not provide usual HBV care, but they do provide services such as prenatal, postnatal, and CAM care for Asian American patients — all important medical points of contact.
Future studies should explore the prevalence and effects of these themes in the medical community at large. Providers mentioned nail salons, Asian grocers, and other fixtures of the Asian American business community. Future research might survey or interview small business owners about their knowledge, beliefs and attitudes regarding HBV and prevention. More collaboration between Eastern and Western medicine practitioners are needed, as are more initiatives and resources to help make screening and treatment available to underinsured and underserved patients. Future studies should also investigate factors affecting care provided by nurses, physician assistants and ancillary providers who play an important and unique role in HBV care. We believe that CME for providers of care to high risk groups about liver cancer, CAM, and HBV transmission, could also help increase HBV awareness among providers and patients alike. More resources are needed to lower financial barriers to care and encourage guideline-recommended screening. Other providers can help promote HBV screening and increase community and cultural awareness.
Acknowledgements
The authors acknowledge Jing Peng for coordinating the focus groups and data entry; Mahfam Mohseni, Cheryl Rogers and Roz Bryant for assisting in coding transcripts; and Stephanie Deming for providing editorial assistance. Drs. Roundtree and Suarez-Almazor are investigators at the Houston Centers for Education and Research on Therapeutics, which receives core support from the Agency for Healthcare Research and Quality (5 U18 HS016093). The research reported in this manuscript was supported by a grant from Gilead, Inc.
Conflict of Interest None disclosed.
References
- 1.U.S. Department of Health and Human Services. Public Health Service. National Toxicology Program. Report on Carcinogens, Eleventh Edition. 2005.
- 2.Centers for Disease Control and Prevention. Asian American Populations. Available at: http://www.cdc.gov/omhd/populations/AsianAm/AsianAm.htm. Accessed on November 13, 2009.
- 3.Chao SD, Chang ET, So SK. Eliminating the threat of chronic hepatitis B in the Asian and Pacific Islander community: a call to action. Asian Pac J Cancer Prev. 2009;10(3):507–512. [PubMed] [Google Scholar]
- 4.Hwang J, Hassan MM. Survival and hepatitis status among Asian Americans with hepatocellular carcinoma treated without liver transplantation. BMC Cancer. 2009;9:46. doi: 10.1186/1471-2407-9-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.U.S. Department of Health and Human Services. Office of Minority Health. Chronic Hepatitis B in Asian Americans, Native Hawaiians and other Pacific Ilanders. Available at: http://www.omhrc.gov/templates/content.aspx?ID=7240. Accessed on November 13, 2009.
- 6.Sorrell MF, Belongia EA, Costa J, et al. National institutes of health consensus development conference statement: management of hepatitis B. Ann Intern Med. 2009;150(2):104–110. doi: 10.7326/0003-4819-150-2-200901200-00100. [DOI] [PubMed] [Google Scholar]
- 7.Taylor VM, Jackson JC, Pineda M, Pham P, Fischer M, Yasui Y. Hepatitis B knowledge among Vietnamese immigrants: implications for prevention of hepatocellular carcinoma. J Cancer Educ. 2000;15(1):51–55. doi: 10.1080/08858190009528654. [DOI] [PubMed] [Google Scholar]
- 8.Taylor VM, Jackson JC, Chan N, et al. Hepatitis B knowledge and practices among Cambodian American women in Seattle, Washington. J Community Health. 2002;27(3):151–163. doi: 10.1023/A:1015229405765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thompson MJ, Taylor VM, Jackson JC, et al. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. J Cancer Educ. 2002;17(4):222–226. doi: 10.1080/08858190209528842. [DOI] [PubMed] [Google Scholar]
- 10.Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat. 2004;11(2):97–107. doi: 10.1046/j.1365-2893.2003.00487.x. [DOI] [PubMed] [Google Scholar]
- 11.Tsai N. Management of chronic hepatitis B in Asian Americans and pacific islanders. Gastroenterol Hepatol. 2005;1(3):188–194. [Google Scholar]
- 12.Friedman DS, Hahn SR, Gelb L, et al. Doctor-patient communication, health-related beliefs, and adherence in glaucoma results from the Glaucoma Adherence and Persistency Study. Ophthalmology. 2008;115(8):1320–1327. doi: 10.1016/j.ophtha.2007.11.023. [DOI] [PubMed] [Google Scholar]
- 13.Bourbeau J, Bartlett SJ. Patient adherence in COPD. Thorax. 2008;63(9):831–838. doi: 10.1136/thx.2007.086041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jayasinghe J. Non-adherence in the hypertensive patient: can nursing play a role in assessing and improving compliance? Can J Cardiovasc Nurs. 2009;19(1):7–12. [PubMed] [Google Scholar]
- 15.Spink KS, Reeder B, Chad K, Wilson K, Nickel D. Examining physician counselling to promote the adoption of physical activity. Can J Public Health. 2008;99(1):26–30. doi: 10.1007/BF03403736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lee YY, Lin JL. The effects of trust in physician on self-efficacy, adherence and diabetes outcomes. Soc Sci Med. 2009;68(6):1060–1068. doi: 10.1016/j.socscimed.2008.12.033. [DOI] [PubMed] [Google Scholar]
- 17.Ong LM, Haes JC, Hoos AM, Lammes FB. Doctor-patient communication: a review of the literature. Soc Sci Med. 1995;40(7):903–918. doi: 10.1016/0277-9536(94)00155-M. [DOI] [PubMed] [Google Scholar]
- 18.Kerse N, Buetow S, Mainous AG, 3rd, et al. Physician-patient relationship and medication compliance: a primary care investigation. Ann Fam Med. 2004;2(5):455–461. doi: 10.1370/afm.139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kaplan SH, Greenfield S, Ware JE., Jr Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med Care. 1989;27(3 Suppl):S110–127. doi: 10.1097/00005650-198903001-00010. [DOI] [PubMed] [Google Scholar]
- 20.Wee CC, McCarthy EP, Phillips RS, Wee CC, McCarthy EP, Phillips RS. Factors associated with colon cancer screening: the role of patient factors and physician counseling. Prev Med. 2005;41(1):23–29. doi: 10.1016/j.ypmed.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 21.Simpson M, Buckman R, Stewart M, et al. Doctor-patient communication: the Toronto consensus statement. BMJ. 1991;303(6814):1385–1387. doi: 10.1136/bmj.303.6814.1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lai CJ, Nguyen TT, Hwang J, et al. Provider knowledge and practice regarding hepatitis B screening in Chinese-speaking patients. J Cancer Educ. 2007;22(1):37–41. doi: 10.1007/BF03174373. [DOI] [PubMed] [Google Scholar]
- 23.Morgan DM, ed. Successful Focus Groups: Advancing the state of the art. Vol 156. Newbury Park, CA: SAGE Publications: 1993.
- 24.Krueger R. Focus Groups: a practical guide for applied research. Thousand Oaks: Sage Publications; 1994. [Google Scholar]
- 25.Burke NJ, Jackson JC, Thai HC, et al. Honoring tradition, accepting new ways: development of a hepatitis B control intervention for Vietnamese immigrants. Ethn Health. 2004;9(2):153–169. doi: 10.1080/1355785042000222860. [DOI] [PubMed] [Google Scholar]
- 26.Choe JH, Chan N, Do HH, Woodall E, Lim E, Taylor VM. Hepatitis B and liver cancer beliefs among Korean immigrants in Western Washington. Cancer. 2005;104(12 Suppl):2955–2958. doi: 10.1002/cncr.21518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Strauss AC, Corbin J, editors. Grounded theory in practice. Thousand Oaks: Sage Publications; 1997. [Google Scholar]
- 28.Corbin J, Strauss AC. Basics of qualitative research: techniques and procedures for developing grounded theory. Thousand Oaks: Sage Publications; 1998. [Google Scholar]
- 29.U.S. Census Bureau. American FactFinder. 2006-2008 American Community Survey 3-Year Estimates. Available at: http://factfinder.census.gov. Accessed on November 9, 2009.
- 30.Lok A, McMahon B. AASLD practice guidelines: chronic hepatitis B. Hepatology. 2007;45(2):507–539. doi: 10.1002/hep.21513. [DOI] [PubMed] [Google Scholar]
- 31.Mast EE, Weinbaum CM, Fiore AE, et al. A comprehensive immunization strategy to eliminate transmission of hepatitis B virus infection in the United States: recommendations of the Advisory Committee on Immunization Practices (ACIP) Part II: immunization of adults. MMWR Recomm Rep. 2006;55(RR-16):1–33. [PubMed] [Google Scholar]
- 32.Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology. 2001;34(6):1225–1241. doi: 10.1053/jhep.2001.29401. [DOI] [PubMed] [Google Scholar]
- 33.Hampton T. Officials recommend expanded testing for chronic hepatitis B virus infection. JAMA. 2008;300(18):2108. doi: 10.1001/jama.2008.573. [DOI] [PubMed] [Google Scholar]
- 34.Lin SY, Chang ET, So SK. Why we should routinely screen Asian American adults for hepatitis B: a cross-sectional study of Asians in California. Hepatology. 2007;46(4):1034–1040. doi: 10.1002/hep.21784. [DOI] [PubMed] [Google Scholar]
- 35.Weinbaum CM, Williams I, Mast EE, et al. Recommendations for identification and public health management of persons with chronic hepatitis B virus infection. MMWR Recomm Rep. 2008;57(RR-8):1–20. [PubMed] [Google Scholar]
- 36.Gaglio PJ, Sterling R, Daniels E, et al. Hepatitis B virus and HIV coinfection: results of a survey on treatment practices and recommendations for therapy.[see comment] Clin Infect Dis. 2007;45(5):618–623. doi: 10.1086/520751. [DOI] [PubMed] [Google Scholar]
- 37.Freed GL, Bordley WC, Clark SJ, Konrad TR. Universal hepatitis B immunization of infants: reactions of pediatricians and family physicians over time. Pediatrics. 1994;93(5):747–751. [PubMed] [Google Scholar]
- 38.Freed GL, Bordley WC, Clark SJ, Konrad TR. Reactions of pediatricians to a new Centers for Disease Control recommendation for universal immunization of infants with hepatitis B vaccine.[see comment] Pediatrics. 1993;91(4):699–702. [PubMed] [Google Scholar]
- 39.Winnock M, Neau D, Castera L, et al. Hepatitis B vaccination in HIV-infected patients: a survey of physicians and patients participating in the Aquitaine cohort.[see comment] Gastroenterol Clin Biol. 2006;30(2):189–195. doi: 10.1016/s0399-8320(06)73153-0. [DOI] [PubMed] [Google Scholar]
- 40.Zickmund SL, Brown KE, Bielefeldt K, Zickmund SL, Brown KE, Bielefeldt K. A systematic review of provider knowledge of hepatitis C: is it enough for a complex disease? Dig Dis Sci. 2007;52(10):2550–2556. doi: 10.1007/s10620-007-9753-0. [DOI] [PubMed] [Google Scholar]
- 41.Hwang JP, Huang CH, Yi JK. Knowledge about hepatitis B and predictors of hepatitis B vaccination among Vietnamese American college students. J Am Coll Health. 2008;56(4):377–382. doi: 10.3200/JACH.56.44.377-382. [DOI] [PubMed] [Google Scholar]
- 42.Ma GX, Shive SE, Fang CY, et al. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. J Health Care Poor Underserved. 2007;18(1):62–73. doi: 10.1353/hpu.2007.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ma GX, Shive SE, Toubbeh JI, Tan Y, Wu D. Knowledge, attitudes, and behaviors of Chinese hepatitis B screening and vaccination. Am J Health Behav. 2008;32(2):178–187. doi: 10.5555/ajhb.2008.32.2.178. [DOI] [PubMed] [Google Scholar]
- 44.Nguyen TT, Taylor V, Chen MS, Jr, Bastani R, Maxwell AE, McPhee SJ. Hepatitis B awareness, knowledge, and screening among Asian Americans. J Cancer Educ. 2007;22(4):266–272. doi: 10.1007/BF03174128. [DOI] [PubMed] [Google Scholar]
- 45.Barrett B, Shadick K, Schilling R, et al. Hmong/medicine interactions: improving cross-cultural health care. Fam Med. 1998;30(3):179–184. [PubMed] [Google Scholar]
- 46.Ramsay DB, Friedman M, Borum ML, Ramsay DB, Friedman M, Borum ML. Does the race or gender of hepatitis C infected patients influence physicians' assessment of hepatitis A and hepatitis B serologic status? South Med J. 2007;100(7):683–685. doi: 10.1097/SMJ.0b013e318063ecc5. [DOI] [PubMed] [Google Scholar]
- 47.Flaskerud JH, Liu PY. Effects of an Asian client-therapist language, ethnicity and gender match on utilization and outcome of therapy. Community Ment Health J. 1991;27(1):31–42. doi: 10.1007/BF00752713. [DOI] [PubMed] [Google Scholar]
- 48.LaVeist TA, Nuru-Jeter A, Jones KE. The association of doctor-patient race concordance with health services utilization.[see comment] J Public Health Policy. 2003;24(3–4):312–323. doi: 10.2307/3343378. [DOI] [PubMed] [Google Scholar]
- 49.Beach MC, Roter DL, Wang NY, Duggan PS, Cooper LA. Are physicians' attitudes of respect accurately perceived by patients and associated with more positive communication behaviors? Patient Educ Couns. 2006;62(3):347–354. doi: 10.1016/j.pec.2006.06.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Meghani SH, Brooks JM, Gipson-Jones T, Waite R, Whitfield-Harris L, Deatrick JA. Patient-provider race-concordance: does it matter in improving minority patients' health outcomes? Ethn Health. 2009;14(1):107–130. doi: 10.1080/13557850802227031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wahner-Roedler DL, Vincent A, Elkin PL, Loehrer LL, Cha SS, Bauer BA. Physicians' attitudes toward complementary and alternative medicine and their knowledge of specific therapies: a survey at an academic medical center. Evid Based Complement Alternat Med. 2006;3(4):495–501. doi: 10.1093/ecam/nel036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Furlow ML, Patel DA, Sen A, Liu JR. Physician and patient attitudes towards complementary and alternative medicine in obstetrics and gynecology. BMC Complement Altern Med. 2008;8:35. doi: 10.1186/1472-6882-8-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Lee RT, Hlubocky FJ, Hu J-J, Stafford RS, Daugherty CK. An international pilot study of oncology physicians' opinions and practices on Complementary and Alternative Medicine (CAM) Integrative Cancer Therapies. 2008;7(2):70–75. doi: 10.1177/1534735408319059. [DOI] [PubMed] [Google Scholar]
- 54.Kurtz ME, Nolan RB, Rittinger WJ. Primary care physicians' attitudes and practices regarding complementary and alternative medicine. J Am Osteopath Assoc. 2003;103(12):597–602. [PubMed] [Google Scholar]
- 55.Bourgeault IL. Physicians' attitudes toward patients' use of alternative cancer therapies. CMAJ Can Med Assoc J. 1996;155(12):1679–1685. [PMC free article] [PubMed] [Google Scholar]
- 56.Chang ET, Lin SY, Sue E, Bergin M, Su J, So SKS. Building partnerships with traditional chinese medicine practitioners to increase hepatitis B awareness and prevention. J Altern Complement Med. 2007;13(10):1125–1127. doi: 10.1089/acm.2007.0655. [DOI] [PubMed] [Google Scholar]
- 57.Ben-Arye E, Scharf M, Frenkel M. How should complementary practitioners and physicians communicate? A cross-sectional study from Israel. J Am Board Fam Med: JABFM. 2007;20(6):565–571. doi: 10.3122/jabfm.2007.06.070119. [DOI] [PubMed] [Google Scholar]
- 58.Greenfield SM, Brown R, Dawlatly SL, Reynolds JA, Roberts S, Dawlatly RJ. Gender differences among medical students in attitudes to learning about complementary and alternative medicine. Complement Ther Med. 2006;14(3):207–212. doi: 10.1016/j.ctim.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 59.Choudhry NK, Fletcher RH, Soumerai SB. Systematic review: the relationship between clinical experience and quality of health care. Ann Intern Med. 2005;142(4):260–273. doi: 10.7326/0003-4819-142-4-200502150-00008. [DOI] [PubMed] [Google Scholar]
- 60.Roter DL, Hall JA. Physician gender and patient-centered communication: a critical review of empirical research. Annu Rev Public Health. 2004;25:497–519. doi: 10.1146/annurev.publhealth.25.101802.123134. [DOI] [PubMed] [Google Scholar]
- 61.Todres M, Stephenson A, Jones R. Medical education research remains the poor relation. BMJ. 2007;335(7615):333–335. doi: 10.1136/bmj.39253.544688.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Asch DA, Epstein A, Nicholson S. Evaluating medical training programs by the quality of care delivered by their alumni. JAMA. 2007;298(9):1049–1051. doi: 10.1001/jama.298.9.1049. [DOI] [PubMed] [Google Scholar]
- 63.Saha S, Beach MC, Cooper LA. Patient centeredness, cultural competence and healthcare quality. J Natl Med Assoc. 2008;100(11):1275–1285. doi: 10.1016/s0027-9684(15)31505-4. [DOI] [PMC free article] [PubMed] [Google Scholar]