Abstract
Introduction
Pigmented villonodular synovitis (PVNS) is a benign idiopathic proliferative disorder that results in villous or nodular formation in the joints, tendons sheaths, and bursae. As PVNS is a rare pathology in children, diagnosis is often delayed. In this study, we analyze the therapeutic methods used and results obtained in the treatment of this pathology.
Materials and methods
All patients with PVNS of the knee seen between January 1988 and June 2006 were evaluated. We assessed the form of presentation, time to diagnosis, previous diagnosis, type of treatment, relapse, and the need for subsequent treatment.
Results
Nine patients with age range 2–15 years and a mean follow-up of 8.5 years were evaluated. Four patients had the diffuse form and four had the localized or nodular form; all of them were intra-articular. In only three cases were preoperative radiographic findings observed. The mean delay in diagnosis was 18 months. Open resection was performed in five patients and arthroscopic resection in four. Joint function was satisfactory in 78% of the patients at the last follow-up and there were no postoperative recurrences.
Conclusions
Magnetic resonance imaging (MRI) is a useful diagnostic tool and the way to detect relapse, and allows accurate determination of the tumor extent. Surgery is the treatment of choice. Worse results are directly related to delay in diagnosis.
Keywords: Pigmented villonodular synovitis, Knee, Children
Introduction
Pigmented villonodular synovitis (PVNS) is a rare pathology, first described by Jaffe [1] in 1941 and characterized by diffuse synovial cell proliferation with the formation of villi or round or ovoid lobulated nodules that vary in size. PVNS typically occurs in young adults between 20 and 45 years of age with no gender preference. The lesion may be diffuse or localized [2]. Patients present with pain, inflammation, and hydrarthrosis [3, 4]. The symptom duration is variable [4].
As PVNS is a rare pathology in children, diagnosis is often delayed. Furthermore, the mode of presentation is often insidious and unspecific, and the initial radiographic findings are subtle. PVNS may be difficult to distinguish from other pathologies, such as rheumatoid arthritis, hemophilic arthropathy, tuberculosis, and other inflammatory and synovial neoplastic processes.
The aim of this study was to analyze the therapeutic methods used and results obtained in the treatment of nine patients with PVNS of the knee diagnosed and treated at the Department of Pediatric Orthopedics and Traumatology of the Garrahan Hospital in Buenos Aires, Argentina.
Materials and methods
All patients with a diagnosis of PVNS seen between January 1988 and July 2006 at the Department of Pediatric Orthopedics and Traumatology of the Garrahan Hospital were retrospectively evaluated. The inclusion criteria were the following: patients younger than 16 years of age with a histological diagnosis of PVNS of the knee and a minimum follow-up period of 2 years. Patients who had undergone previous surgery of the affected knee and/or had incomplete clinical and radiographic follow-up were excluded from the series. Patient data were obtained from the clinical charts. For the data collection, a statistical model was used, in which the selected variables were included: age, gender, lesion location, form of presentation (localized or diffuse), clinical presentation, time of delay of diagnosis, previous diagnosis, type of treatment (conservative, open synovectomy, or arthroscopy), relapse, and need for subsequent treatment (Fig. 1). Relapse was defined as recurrence of the symptoms (pain, swelling, functional impairment, and decreased range of motion) and correlation with the magnetic resonance imaging (MRI) requiring additional treatment for the exploration of the affected joint or extra-articular region.
Fig. 1.

A 6-year-old patient with a long duration of symptoms before diagnosis. a, b Frontal and lateral X-rays show narrowing of the intra-articular space in the right knee
The patients underwent preoperative MRI to determine the extent of the lesion. Surgical planning aimed at total resection was tailored to each patient. An open or arthroscopic biopsy was performed first in all patients to confirm the diagnosis (Figs. 2 and 3) before the definite procedure. In the patients that underwent open resection, a conventional medial parapatellar approach was used, while in patients that underwent arthroscopic resection, four portals were used: parapatellar (anterolateral and anteromedial) and suprapatellar (internal and external), with a 30° angle to visualize the anterior compartment and the lateral and medial recesses. After closing the skin, an elastic bandage was applied and weight-bearing was allowed. Immediately postoperatively, early knee flexion and isometric exercises of the quadriceps and hamstring muscles were indicated. The data found are shown in absolute numbers and percentages.
Fig. 2.
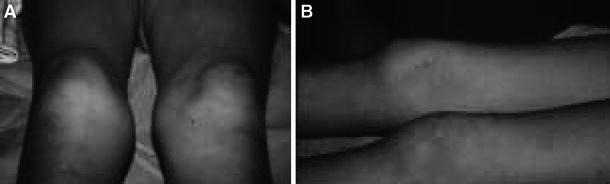
Clinical aspect. a, b Swelling of the right knee
Fig. 3.
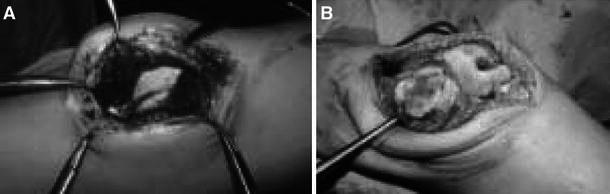
Intraoperative image. a Intra-articular view of the villi. b Marked destruction of joint cartilage
Results
Between January 1988 and July 2006, we treated 14 patients with a diagnosis of PVNS. Three patients were excluded from the series because of a different location of the PVNS (two in the hip and one in the ankle). Two patient with PVNS of the knee were excluded as well; one of them had undergone surgery at another center and was referred for treatment of sequelae and the other was lost to follow-up. Nine patients were included in the study: four males and five females. The mean age at the first consultation was 9.8 years (range, 2–15 years). All patients had a minimum follow-up of 2 years, with a mean follow-up of 8.5 years (range, 1–12 years) after diagnosis. The lesions were localized in four patients and diffuse in the remaining five. The time between symptom onset (pain, swelling, functional impairment, and decreased range of motion) and diagnosis was between 3 and 48 months (mean, 18 months). The diagnosis was delayed because of failure to refer the patients to a pediatric orthopedic surgeon. In 44% of the cases, the lesion was misdiagnosed as mono-articular juvenile rheumatoid arthritis and the delay in diagnosis was the longest in these patients (mean, 33.5 months). Only 33% of the children had positive findings on the initial X-rays (see Fig. 1; Table 1).
Table 1.
Diagnosis and presurgical evaluation of the patients
| Case | Age | Gender | Form | Follow-up (months) | Clinical findings | Delay in diagnosis (months) | Previous diagnosis |
|---|---|---|---|---|---|---|---|
| 1 | 12 | F | D | 90 | Gonalgia | 24 | RA |
| 2 | 14 | F | LI retropatellar region (Hoffa’s fat) | 78 | Gonalgia | 24 | RA |
| 3 | 15 | F | D | 108 | Gonalgia | 8 | No |
| 4 | 10 | M | LI posterior to the cruciate ligaments | 58 | Swelling | 2 | No |
| 5 | 10 | F | D | 50 | Gonalgia | 3 | No |
| 6 | 2 | F | D | 106 | Claudication, swelling | 38 | RA |
| 7 | 11 | M | D | 46 | Swelling | 4 | No |
| 8 | 7 | M | LI retropatellar region (Hoffa’s fat) | 143 | Pain, swelling | 48 | RA |
| 9 | 10 | M | LI posterior to the cruciate ligaments | 60 | Pain, swelling, functional impairment | 10 | No |
D diffuse, LI localized intra-articular, RA rheumatoid arthritis
The diagnosis was confirmed first by incisional (4 of 9), excisional (2 of 9), or arthroscopic (3 of 9) biopsy in all patients to the definitive surgery. We did not perform arthrocentesis because, in all of the cases, it was performed previously by rheumatologists at the first medical visit. Resection of the lesion was performed by open synovectomy in five cases and by arthroscopy in four (localized forms). No recurrences were seen after resection of the lesion. Seven patients recovered full range of motion or the range of motion was reduced by less than 15° after surgery. In two of four patients who had the longest delay in diagnosis (cases 1 and 8), joint movement was considerably limited and they had occasional mild to moderate pain. Patient 1 needed mobilization under anesthesia in two opportunities (Fig. 4). We did not use continuous passive motion machines at that time. The worst functional results were directly related to delay in diagnosis.
Fig. 4.
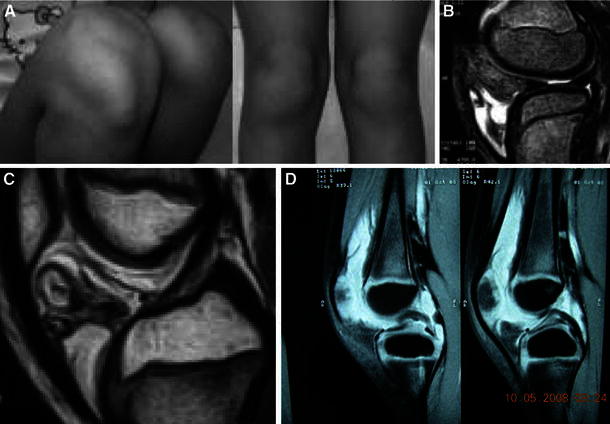
A 9-year-old patient with a 4-month history of pain and functional impairment of the right knee. a, b Anterolateral swelling of the right knee. c, d Magnetic resonance imaging (MRI): T1- and T2-weighted sequences showing a mass in the retropatellar region (Hoffa’s fat) with gradient-echo (hemosiderin deposits)
Discussion
The estimated yearly incidence of PVNS is 1.8 per one million inhabitants [5]. Even though no data exist in children, the estimated incidence is significantly lower in the pediatric age group. The etiology of the pathology is uncertain. Some authors have suggested that PVNS may be caused by an inflammatory process or a disorder of the lipid metabolism [6]. However, most consider that chronic inflammation is the underlying process [3, 7, 8]. Other authors have suggested that PVNS may be a neoplastic process, as, in rare cases, it may produce metastasis and evidence exists that some lesions are of the monoclonal type [9–13].
One characteristic of PVNS is its capacity to invade the subchondral bone, producing cysts and erosions, which is why treatment should be started as early as possible in order to avoid secondary degenerative lesions. MRI is a valuable complementary diagnostic method, as the initial X-rays are negative in a high percentage of cases. In this series, only 33% (3 of 9) of the patients had minimal radiographic signs and 77% did not have identifiable changes on the first consultation. MRI showed a mass of soft tissue with a hypo-intense signal in T1- and T2-weighted images [14, 15]. This study allows differentiation between the diffuse and localized form and the evaluation of the extent of bone and soft-tissue involvement. It is also useful in the diagnosis of cases with intra-articular location that may be mistaken for meniscal lesions or loose bodies [16, 17]. It has recently been reported that gradient-echo sequences may be especially helpful to determine the extent of the lesion in children [3]. The signal in T1- and T2-weighted images are sensitive to hemosiderin deposits behind the infrapatellar fat, which is very useful for differentiating PVNS to other pathologies.
Even though several therapeutic options have been described, the treatment of choice is surgery. Localized PVNS rarely have local recurrence after marginal arthroscopic removal [1, 12, 18, 19]. The best treatment for the diffuse forms has not been clearly defined yet, but subtotal synovectomy, either open or arthroscopic, is the most widely accepted therapy [10]. No studies comparing the results of both techniques have been published. The advantage of arthroscopy is that it is less invasive, resulting in faster functional recovery [20]. Now, with this method, we can also explore the anterior and posterior compartment in the articulation. This group described that arthroscopic treatment has some inferiority over open resection, because, at that moment, we only performed open surgery in this pathology. The disadvantages, however, are the risk of recurrence and the possibility of portal contamination.
Regardless of the technique used, the principle in diffuse forms always remains the same: subtle removal of the synovial tumor. Due to the high rate of recurrence reported in this type of PVNS, some authors have suggested radiotherapy as adjuvant treatment [21, 22]. However, the use of radiotherapy in children is controversial because of potential damage to the epiphyseal growth plate and post-radiation sarcomas [23]. As the pathology is rare in skeletally immature patients, few studies have been published including only this age group. The majority of studies have reported isolated cases with PVNS of the elbow [24], of the ankle [11, 25], of the sacrum [6], or of multifocal presentation [26, 27]. Although the knee is the most common site of presentation, few studies on PVNS of the knee in prepubertal patients have been published [5, 8, 23]. This lack of knowledge leads to delayed diagnosis in many cases, as the lesion is not suspected or is misdiagnosed as a process of similar presentation, such as rheumatoid arthritis, hemophilia, tuberculous arthritis, angiomas, synovial neoplasias, and other inflammatory processes. In our four patients in whom initially another diagnosis was suspected, this diagnostic delay led to a late treatment (mean, 33.5 months). These four cases had the lowest score in the clinical evaluation, and two of them mentioned occasional mild to moderate discomfort and limited range of motion.
This study had some limitations: the small sample size and the heterogeneity of disease presentation does not allow statistical analysis of the different therapeutic methods. On the other hand, relapse was clinically defined as recurrence of symptoms, but MRI or arthroscopy was performed to detect subclinical relapse that may have been interpreted as joint degeneration.
We do not use adjuvant therapy such as external low-dose radiotherapy or intra-articular injection of Y90 or other radioisotopes like in adults.
In conclusion, PVNS is an infrequent pathology in children. Because of its rarity, the diagnosis of PVNS in children may be made late. MRI is useful in the diagnosis of the pathology and to determine the extent of the lesion and also to confirm relapse.
Surgery is the treatment of choice, with a low recurrence rate if the lesion is accurately removed. Arthroscopy is useful in cases with the easily accessible intra-articular form. In our series, worse functional outcome was directly related to delay in the diagnosis [2].
References
- 1.Kim SJ, Shin SJ, Choi NH, Choo ET. Arthroscopic treatment for localized pigmented villonodular synovitis of the knee. Clin Orthop Relat Res. 2000;379:224–230. doi: 10.1097/00003086-200010000-00026. [DOI] [PubMed] [Google Scholar]
- 2.Walls JP, Nogi J. Multifocal pigmented villonodular synovitis in a child. J Pediatr Orthop. 1985;5(2):229–231. doi: 10.1097/01241398-198505020-00022. [DOI] [PubMed] [Google Scholar]
- 3.Eckhardt BP, Hernandez RJ. Pigmented villonodular synovitis: MR imaging in pediatric patients. Pediatr Radiol. 2004;34(12):943–947. doi: 10.1007/s00247-004-1261-1. [DOI] [PubMed] [Google Scholar]
- 4.Saulsbury FT. Pigmented villonodular synovitis of the knee in a 9-year-old child. South Med J. 2004;97(1):80–82. doi: 10.1097/01.SMJ.0000104842.97001.88. [DOI] [PubMed] [Google Scholar]
- 5.Rao AS, Vigorita VJ. Pigmented villonodular synovitis (giant-cell tumor of the tendon sheath and synovial membrane). A review of eighty-one cases. J Bone Joint Surg Am. 1984;66:76–94. [PubMed] [Google Scholar]
- 6.Kang GH, Chi JG, Choi IH. Pigmented villonodular synovitis in the sacral joint with extensive bone destruction in a child. Pediatr Pathol. 1992;12(5):725–730. doi: 10.3109/15513819209024226. [DOI] [PubMed] [Google Scholar]
- 7.Granowitz SP, D’Antonio J, Mankin HL. The pathogenesis and long-term end results of pigmented villonodular synovitis. Clin Orthop Relat Res. 1976;114:335–351. [PubMed] [Google Scholar]
- 8.Sakkers RJ, de Jong D, van der Heul RO. X-chromosome inactivation in patients who have pigmented villonodular synovitis. J Bone Joint Surg Am. 1991;73:1532–1536. [PubMed] [Google Scholar]
- 9.Choong PF, Willén H, Nilbert M, Mertens F, Mandahl N, Carlén B, Rydholm A. Pigmented villonodular synovitis. Monoclonality and metastasis—a case for neoplastic origin? Acta Orthop Scand. 1995;66:64–68. doi: 10.3109/17453679508994643. [DOI] [PubMed] [Google Scholar]
- 10.De Ponti A, Sansone V, Malcherè M. Result of arthroscopic treatment of pigmented villonodular synovitis of the knee. Arthroscopy. 2003;19(6):602–607. doi: 10.1016/S0749-8063(03)00127-0. [DOI] [PubMed] [Google Scholar]
- 11.Huracek J, Troeger H, Menghiardi B, Jundt G, Nürnberger H, Herrmann R, Landmann C. Malignant course of pigmented villonodular synovitis of the flexor tendon sheath of the small finger—case report and review of the literature. Handchir Mikrochir Plast Chir. 2000;32:283–290. doi: 10.1055/s-2000-10930. [DOI] [PubMed] [Google Scholar]
- 12.Parikh SN, Chen AL, Ergas E. Localized pigmented villonodular synovitis: arthroscopic diagnosis and management of an “invisible” lesion. Arthroscopy. 2002;18:E31. doi: 10.1053/jars.2002.31832. [DOI] [PubMed] [Google Scholar]
- 13.Ray RA, Morton CC, Lipinski KK, Corson JM, Fletcher JA. Cytogenetic evidence of clonality in a case of pigmented villonodular synovitis. Cancer. 1991;67:121–125. doi: 10.1002/1097-0142(19910101)67:1<121::AID-CNCR2820670122>3.0.CO;2-P. [DOI] [PubMed] [Google Scholar]
- 14.Mandelbaum BR, Grant TT, Hartzman S, Reicher MA, Flannigan B, Bassett LW, Mirra J, Finerman GA. The use of MRI to assist in diagnosis of pigmented villonodular synovitis of the knee joint. Clin Orthop Relat Res. 1988;231:135–139. [PubMed] [Google Scholar]
- 15.Stoller DW, Genant HK (1988) MRI of pigment vellonodular sinivitis. In: Proceedings of the American Roentgen Ray Society, San Francisco, California, May 1988
- 16.Makino A, Múscolo DL, Costa Paz M, Ayerza M. Sinovitis vellonodular pigmentada localizada de rodilla: diagnóstico con resonancia magnética y su tratamiento artroscópico. Rev Asoc Argent Ortop Traumatol. 1997;62(2):257–263. [Google Scholar]
- 17.Muscolo DL, Makino A, Costa-Paz M, Ayerza MA. Localized pigmented villonodular synovitis of the posterior compartment of the knee: diagnosis with magnetic resonance imaging. Arthroscopy. 1995;11(4):482–485. doi: 10.1016/0749-8063(95)90205-8. [DOI] [PubMed] [Google Scholar]
- 18.Beguin J, Locker B, Vielpeau C, Souquieres G. Pigmented villonodular synovitis of the knee: results from 13 cases. Arthroscopy. 1989;5:62–64. doi: 10.1016/0749-8063(89)90094-7. [DOI] [PubMed] [Google Scholar]
- 19.Moskovich R, Parisien JS. Localized pigmented villonodular synovitis of the knee. Arthroscopic treatment. Clin Orthop Relat Res. 1991;271:218–224. [PubMed] [Google Scholar]
- 20.Chin KR, Barr SJ, Winalski C, Zurakowski D, Brick GW. Treatment of advanced primary and recurrent diffuse pigmented villonodular synovitis of the knee. J Bone Joint Surg Am. 2002;84:2192–2202. doi: 10.2106/00004623-200212000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Blanco CE, Leon HO, Guthrie TB. Combined partial arthroscopic synovectomy and radiation therapy for diffuse pigmented villonodular synovitis of the knee. Arthroscopy. 2001;17:527–531. doi: 10.1053/jars.2001.24068. [DOI] [PubMed] [Google Scholar]
- 22.Kotwal PP, Gupta V, Malhotra R. Giant-cell tumour of the tendon sheath. Is radiotherapy indicated to prevent recurrence after surgery? J Bone Joint Surg Br. 2000;82:571–573. doi: 10.1302/0301-620X.82B4.10328. [DOI] [PubMed] [Google Scholar]
- 23.Bruns J, Schubert T, Eggers-Stroeder G. Pigmented villonodular synovitis in children. A case report. Arch Orthop Trauma Surg. 1993;112:148–151. doi: 10.1007/BF00449993. [DOI] [PubMed] [Google Scholar]
- 24.Aydingöz U, Leblebicioglu G, Gedikoglu G, Atay OA. Pigmented villonodular synovitis of the elbow in a 6-year-old girl. J Shoulder Elbow Surg. 2002;11(3):274–277. doi: 10.1067/mse.2002.122256. [DOI] [PubMed] [Google Scholar]
- 25.Jaffe HL, Lichtenstein L, Sutro CJ. Pigmented villonodular synovitis, bursitis and tenosynovitis. Arch Pathol. 1941;31:731–765. [Google Scholar]
- 26.Kay RM, Eckardt JJ, Mirra JM. Multifocal pigmented villonodular synovitis in a child. A case report. Clin Orthop Relat Res. 1996;322:194–197. [PubMed] [Google Scholar]
- 27.Van Emelen K, Moens P, Wouters K, Fabry G. Villonodular synovitis of the knee in a 5-year-old child. Apropos of a case. Rev Chir Orthop Reparatrice Appar Mot. 1999;85(6):621–626. [PubMed] [Google Scholar]
- 28.Tyler WK, Vidal AF, Williams RJ, Healey JH. Pigmented villonodular synovitis. J Am Acad Orthop Surg. 2006;14:376–385. doi: 10.5435/00124635-200606000-00007. [DOI] [PubMed] [Google Scholar]


