Abstract
Flexible flatfoot is a normal foot shape that is present in most infants and many adults. The arch elevates spontaneously in most children during the first decade of life. There is no evidence that a longitudinal arch can be created in a child’s foot by any external forces or devices. Flexible flatfoot with a short Achilles tendon, in contrast to simple flexible flatfoot, is known to cause pain and disability in some adolescents and adults. Joint-preserving, deformity-correcting surgery is indicated in flexible flatfeet with short Achilles tendons when conservative measurements fail to relieve pain under the head of the plantar flexed talus or in the sinus tarsi area. Osteotomy is the fundamental and central procedure of choice. In almost all cases, Achilles tendon lengthening is required. In some cases, rigid supination deformity of the forefoot is present, requiring identification and concurrent treatment.
Keywords: Flatfoot, Adolescent, Achilles tendon contracture, Calcaneal lengthening osteotomy, Arthroereisis
Introduction
There are very few foot conditions that remain as poorly understood as the congenital flexible flatfoot, primarily because of the large volume of conflicting and poorly conducted research studies that have been carried out over many decades. This foot shape is common, often familial, rarely painful, and even more rarely disabling, yet the flexible flatfoot generates interest, investigation, and controversy. There is, in fact, no consensus among health care providers as to whether flatfoot represents a deformity or a variation of normal foot shape.
Harris and Beath [1], in their 1947 study of foot problems in 3,600 recruits in the Royal Canadian Army, stated that the flexibility of the subtalar joint and the longitudinal arch, along with the ability of both to reverse their alignments, was more important than the static shape of the foot. The flexible, or hypermobile, flatfoot accounted for most of the flatfeet that they identified in their study population. This type was determined to be the normal contour of a strong and stable foot, and not the cause of pain and disability. No one before nor since then has provided scientific evidence to refute their claim, yet the controversy continues.
Epidemiology
The true incidence of flatfoot is unknown, primarily because there is no consensual agreement on the strict clinical or radiographic criteria for defining a flatfoot. At the root of this dilemma is the lack of a universally accepted definition of a “normal,” in contrast to an “average height,” longitudinal arch. Traditionally, a flatfoot has been defined subjectively as a weight-bearing foot with an abnormally low or absent longitudinal arch. This definition is based solely upon the static anatomic comparison of the height of the arch within a population. It fails to take into consideration the etiology of the flatfoot, the functional relationships between the bones, and the presence or evidence-based expectation of future pain or disability. It also ignores normal anatomic variations in arch height among adults, between children and adults, and between racial groups. It is well recognized that there is a higher incidence of flatfeet in blacks [2–5] than Caucasians, and that these flatfeet, like those in Caucasians, rarely cause disability.
Morley [6] evaluated the heel-to-arch width ratio on the footprints of children in the first decade of life and found that nearly 100% of 2-year-olds were flatfooted, while the same pattern was seen in only 4% of 10-year-old children. Though he and other authors [7, 8] believed that many of these flatfeet actually had an arch that was obscured by a fat pad, Gould et al. [9] and others [10, 11] refuted the fat pad theory with radiographic evidence of actual flattening of the medial longitudinal arch. Staheli et al. [12] used the footprint technique to evaluate the shape of the plantar surface in 882 asymptomatic feet in normal people aged 1–80 years. He demonstrated that most infants are flatfooted, that the arch develops spontaneously during the first decade of life in most children, and that flatfeet are within the normal confidence limits for arch height in adults as well as children. Vanderwilde et al. [13] confirmed these findings with the first comprehensive study on normative radiographic measurements of the foot in children. They found that there is a large spectrum of normal values for children of different ages, that these normal values are different from adult normal values, and that these normal values change spontaneously with age into the adult norms.
Comprehensive, normative radiographic values have recently become available for the adult foot [14]. Wide variations were found in all measurements. Since all feet of the study subjects, despite anatomic variations, were painless and therefore “normal,” the conclusions were that radiographs should not direct treatment, even if the values are beyond the normal range. Radiographs can define the static relationships between bones, but they cannot provide clinical information on pain, flexibility, or function.
Despite the lack of a strict definition, it is believed that most children [6–9, 12, 13] and at least 20% of adults [1] have flatfeet, most of which are flexible. Harris and Beath [1], using their own anatomic criteria, identified flatfeet in approximately 23% of their adult study subjects. They subdivided flatfeet into three types: flexible flatfoot (FFF), flexible flatfoot with short tendo-Achilles (FFF-STA), and peroneal spastic or rigid flatfoot. They found that flexible flatfoot accounted for approximately two-thirds of all flatfeet and, in contrast to the latter two types, rarely caused disability. They emphasized that the flatness of the arch in weight-bearing was of less importance than the mobility of the joints and tendons [1, 15]. They identified contracture of the Achilles tendon in association with flexible flatfoot in 25% of the total number of subjects with FFF and noted that this type was often accompanied by pain and functional disability [1, 15]. Rigid flatfoot, characterized by restricted motion of the subtalar joint, accounted for approximately 9% of all the flatfeet that they studied. These were most commonly associated with tarsal coalitions and were occasionally symptomatic. Tarsal coalitions and other conditions that cause rigid flatfoot are not the focus of this review and will not be discussed in detail. Certain features of the rigid flatfoot will, however, be mentioned to aid with differentiation from the flexible flatfoot.
While it is possible to document the number of individuals with painful FFF (with or without short tendo-Achilles) that seek medical attention, it is not possible to accurately document the much larger number of individuals with asymptomatic FFF who do not seek medical attention and, therefore, go uncounted. It is, thus, impossible to accurately estimate the risk of pain or disability from this very common foot shape. Nevertheless, the risk has been estimated to be small, even according to proponents of most surgical procedures for painful flatfeet.
Pathogenesis
There are two main theories explaining the pathogenesis of FFF: a type of flatfoot that is present from birth and is accompanied by good joint mobility and apparently normal muscle function. Duchenne [16] and others [17–21] believed that coordinated and normal function of the muscles of the foot and ankle was responsible for the maintenance of the longitudinal arch and that sub-clinical muscle weakness was responsible for the flexible flatfoot. This theory was refuted by Basmajian et al., whose electromyographic studies of the muscles of the foot and ankle [22, 23] showed that the height of the longitudinal arch is determined by features of the bone–ligament complex, and that the muscles maintain balance, accommodate the foot to uneven terrain, protect the ligaments from unusual stresses, and propel the body forward. Proponents of this bone–ligament theory believe that the shape of the longitudinal arch under static loads is determined by the shape and interrelationship of the bones, coupled with the strength and flexibility of the ligaments [1, 15, 22, 24–28]. It is unproven whether the abnormal shape of individual bones and joints represents a primary or secondary reflection of a long-standing flatfoot, though most current authors conclude that excessive ligamentous laxity is the primary abnormality. Muscles are necessary for function and balance, but not for structural integrity. Mann and Inman [28] confirmed that muscle activity is not required to support the arch in static weight-bearing. They also found that the intrinsic muscles are the principal stabilizers of the foot during propulsion, and that greater intrinsic muscle activity is required to stabilize the transverse tarsal and subtalar joints in a flatfooted individual than in one with an average height arch.
There are no long-term prospective studies on the natural history of untreated FFF in regard to the development of pain, only the cross-sectional study of Harris and Beath [1, 15]. They found that, whereas FFF is rarely a cause for concern, FFF-STA often causes pain and disability. It is unknown whether the short tendo-Achilles in these feet is a primary pathologic feature or a secondary developmental deformity. Harris and Beath [15] believed that FFF and FFF-STA are separate entities, although the documentation of early clinical differentiation has not been reported.
Biomechanics/pathomechanics
The functions of the foot include the provision of a stable, but supple, platform that adapts to the ground during the early stance phase of gait, followed by conversion to a rigid lever during push-off [29–33]. Several authors have represented the complex interrelationships between the bones of the mid- and hindfoot as a mitered hinge [29, 30, 32–34], though that analogy is clearly too simplistic. Using that as a first approximation or basic foundation, one must add a thorough understanding of the shape, structure, relationships, and motions of the subtalar joint complex to truly understand the biomechanics of the foot.
The subtalar joint complex is comprised of three bones (possibly four, if one includes the cuboid), several important ligaments (including the spring, or calcaneo-navicular ligament), and multiple joint capsules that all function together as a unit. Almost 200 years ago, Scarpa [35] noted similarities between the subtalar joint complex and the hip joint. He compared the femoral head to the talar head, and the pelvic acetabulum to the so-called “acetabulum pedis,” a cup-like structure made up of the navicular, spring ligament, and anterior end of the calcaneus and its facets. It is not a perfect comparison, but the two anatomic areas share certain features that seem to make the comparison both valid and worthwhile. The hip, a pure ball-and-socket joint with a central rotation point, is comprised of two bones, one intra-articular ligament, and a joint capsule. The subtalar joint is not an independent ball-and-socket joint, though the combined motions of the subtalar joint and the immediately adjacent ankle joint give that impression. Its axis of motion is in an oblique plane that is neither frontal, sagittal, nor coronal. This creates motions that are best described with the unique terms “inversion” and “eversion.” The stable structure in the hip joint is the acetabulum (the socket), while the stable structure in the subtalar joint complex is the talus (the ball). Inversion is comprised of plantar flexion, supination, and internal rotation of the acetabulum pedis around the head of the talus [36]. The static position of inversion of the subtalar joint is called hindfoot varus and is found in cavovarus feet and clubfeet. Eversion is a combination of dorsiflexion, pronation, and external rotation of the acetabulum pedis around the talar head. Hindfoot valgus is the static position of the everted subtalar joint and is seen in flatfeet and skewfeet.
The tibia and talus internally rotate during the first half of the stance phase of the gait cycle while the subtalar joint complex everts. The talar head plantar flexes because of the lost support from the acetabulum pedis. The foot becomes quite supple, or unlocked, and flattens. During the latter part of the stance phase, the tibia and talus externally rotate, while the subtalar joint complex inverts, so that the acetabulum pedis once again supports the head of the talus. The talus dorsiflexes and the entire foot becomes more rigid, or locked. This diminishes stress on the muscles and ligaments during push-off.
The flexible flatfoot begins stance in an unlocked, everted position, and does not completely convert to a rigid, inverted lever during the latter portion of stance. Based on the work by Mann and Inman [28], who found that greater intrinsic muscle activity is required to stabilize the transverse tarsal and subtalar joints in a flatfooted individual than in one with an average height arch, this might be expected to lead to foot fatigue and pain. Fortunately, foot fatigue and pain seem to occur only in some flatfooted individuals [37].
The orthopedist is urged to avoid the use of the term “pronated” as a substitute for the term “flatfoot.” While it is true that pronation is a component of the hindfoot deformity in this condition, the subtalar joint is dorsiflexed and externally rotated, the midfoot is abducted, and the forefoot is supinated in relation to the hindfoot. The term “flatfoot” encompasses all of these multi-site three-dimensional deformities and is, therefore, a better choice of term.
Clinical features
Flexible flatfeet rarely cause pain or disability in infancy and childhood. Children in this age group usually present for evaluation because of their parents’ concern about the appearance of the feet or because of a family history of special shoe wearing during childhood.
The clinical assessment of a child with a flatfoot should consist of a general examination of the musculoskeletal system, in addition to the specific foot and ankle examination. The general examination is aimed at assessing torsional and angular variations of the lower extremities and the walking pattern. The patient should be examined for evidence of generalized ligamentous laxity, which can include touching the thumb to the volar forearm, hyperextension of the metacarpo-phalangeal joints of the fingers to 90°, hyperextension of the elbows and/or knees into recurvatum, and touching the palms to the ground with the knees extended. It is often rewarding to inquire about familial flatfeet and to examine the feet of other family members who are present in the examination room. Flexible flatfeet may cause rapid and uneven shoe wear in older children and adolescents, so the child’s shoes should be examined.
Assessment of the foot and ankle begins with the recognition, as first clearly stated by Mosca [38], that “the foot is not a joint.” This simplistic and seemingly apparent fact is the foundation for the appropriate assessment and management of foot deformities in children. There are at least two segmental deformities, often in opposite directions from each other, in all congenital and developmental deformities of the child’s foot [38]. For example, a flatfoot is a combination of deformities that includes valgus deformity of the hindfoot and supination deformity of the forefoot. These are rotationally opposite direction deformities that, according to Mosca [38], give the impression that the foot has been “wrung out like a towel.” In a symptomatic flatfoot, there is also a contracture of the gastrocnemius alone or the entire triceps surae (Achilles tendon).
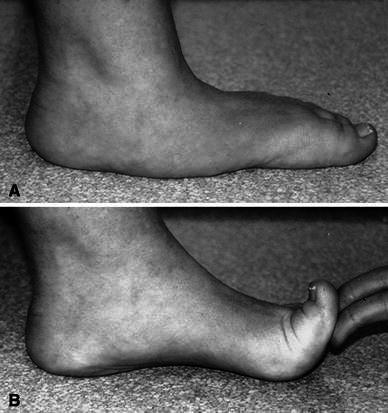
The clinical appearance of a flatfoot is more complicated than the simple depression or absence of a longitudinal arch. There is a straight or convex plantar-medial border of the foot. The lateral border is straight or concave. The midfoot sags and touches the ground in weight-bearing (Fig. 1a). The foot appears externally rotated in relation to the leg and the weight-bearing axis of the lower extremity passes medial to the mid-axis of the hindfoot. The hindfoot is in valgus alignment (Fig. 1b).
Fig. 1.

Flexible flatfeet. a Convex medial border with midfoot sag. b Valgus hindfoot (Fig. 10-3, p. 139, from ref. [127], with permission)
The flexibility of flatfoot is a more important feature than the static shape. Flexibility refers to the motion of the subtalar joint complex and requires careful assessment. The subtalar joint will invert from valgus to neutral and a longitudinal arch will be observed in a flexible flatfoot that is dangling in the air while the individual is seated. A longitudinal arch can also be created by dorsiflexing the great toe (Fig. 2). This so-called toe-raising test, initially described by Jack [27] and explained by Hicks [26], is due to the “windlass action” of the plantar fascia. A windlass is an apparatus for moving heavy weights. It consists of a horizontal cylinder which is rotated by the turn of a crank. A winch (spool and crank) is affixed to one end, and a cable is wound around the winch, pulling a weight that is attached to the opposite end. The plantar fascia simulates a cable attached to the metatarso-phalangeal joints at one end and the calcaneus at the opposite end. Dorsiflexion of the toes (the crank) winds the plantar fascia around the heads of the metatarsals (the cylinder). This winding of the plantar fascia shortens the distance between the calcaneus and metatarsals and elevates the medial longitudinal arch. The windlass effect is also demonstrated when toe-standing, by means of the same biomechanics (Fig. 3).
Fig. 2.
Jack’s toe-raising test. An arch is created in a flexible flatfoot (FFF) by the windlass action of the great toe and plantar fascia (Fig. 10-6, p. 141, from ref. [127], with permission)
Fig. 3.
a Weight-bearing left FFF. b In toe-standing, heel valgus converts to varus and the longitudinal arch can be seen (Fig. 10-5, p. 140, from ref. [127], with permission)
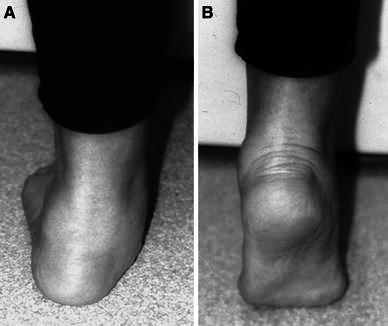
Supination deformity of the forefoot on the hindfoot is revealed when the valgus hindfoot is passively inverted to neutral (Fig. 4). It should be apparent that this separate, rotationally opposite, segmental deformity exists in a flatfoot. If not, a flatfooted individual would stand on the plantar-medial aspect of the everted/pronated hindfoot and the plantar-medial aspect of the first metatarsal, with the lateral forefoot elevated off the ground. Instead, compensatory forefoot supination places all metatarsal heads on the ground for shared weight-bearing when the hindfoot is everted.
Fig. 4.

Forefoot supination can best be appreciated when the hindfoot is inverted to neutral (Fig. 10-7, p. 142, from ref. [127], with permission)
A flexible flatfoot with short tendo-Achilles (FFF-STA) has the same subtalar joint mobility of an FFF, but is differentiated from it by a limitation of ankle dorsiflexion. Short tendo-Achilles should be considered as a proxy for contracture of either the gastrocnemius alone or the entire triceps surae (tendo-Achilles), as both prevent the talus from dorsiflexing in the ankle joint during the stance phase of gait. With an STA, the dorsiflexion force is shifted to the subtalar joint which, as a component of eversion, enables dorsiflexion of the calcaneus (acetabulum pedis) in relation to the talus. This false dorsiflexion often results in foot and ankle pain either under the head of the talus or in the sinus tarsi area.
Assessment of true ankle dorsiflexion and Achilles tendon excursion are important, yet difficult, to evaluate accurately. The subtalar joint complex must be inverted to neutral and held locked in that position in order to isolate and assess the motion of the talus in the ankle joint. The knee is flexed and the ankle is dorsiflexed while maintaining neutral alignment of the subtalar joint. Dorsiflexion is measured as the angle between the plantar-lateral border of the foot and the anterior tibial shaft. Less than 10° of dorsiflexion indicates contracture of the soleus muscle, which equates to contracture of the entire tendo-Achilles. The knee is then extended while maintaining neutral alignment of the subtalar joint and trying to maintain dorsiflexion of the ankle joint. Dorsiflexion is remeasured. If more than 10° of dorsiflexion was possible with the knee flexed, but less than 10° of dorsiflexion is possible with the knee extended, the gastrocnemius alone is contracted (Fig. 5). One should differentiate contracture of the gastrocnemius from contracture of the entire triceps surae (tendo-Achilles), because both can cause pain that justifies surgical management, but the surgical technique obviously varies between them.
Fig. 5.

The subtalar joint must be held in neutral position and the knee extended in order to accurately assess ankle dorsiflexion (Fig. 10-8, p. 142, from ref. [127], with permission)
In contrast to these two types of flexible flatfoot is the rigid flatfoot, which was defined by Harris and Beath [1, 15] as being characterized by the restriction of subtalar joint motion. The arch remains flat when the foot is dangling in the air while the individual is seated, as well as during toe-standing and the toe-raising test. This type of flatfoot can occasionally cause pain and disability.
Most flexible and rigid flatfeet do not hurt. Acquired and environmental causes of pain may occur in a foot with any foot shape, including flatfoot. Therefore, one must not automatically assume that pain is related to shape. If pain is the presenting complaint, it is critically important to inquire about its exact location and precipitating causes. Those characteristics of pain in a flatfoot can often indicate the Harris and Beath type of flatfoot that exists in the patient. Pain from FFF-STA is usually located on the plantar-medial aspect of the midfoot and occasionally in the sinus tarsi area. Pain from a rigid flatfoot may be experienced at several sites, including the medial hindfoot, the sinus tarsi area, and, occasionally, the plantar-medial midfoot. In both of these conditions, the pain is exacerbated by activities and relieved by rest. Night pain is extremely unusual. Redness, swelling, and warmth are not characteristic findings.
Radiographic evaluation
Radiographs of the flexible flatfoot are not necessary for diagnosis, but they may be indicated to help with the assessment of uncharacteristic pain, decreased flexibility, and for surgical planning. Weight-bearing anteroposterior (AP) and lateral views of the foot are generally sufficient to evaluate the flexible flatfoot. Without weight-bearing, or at least simulated weight-bearing, the radiographic relationships between the bones will not represent the true clinical deformities. The addition of the oblique and the axial, or Harris, views is necessary to evaluate the rigid and/or painful flatfoot. A calcaneo-navicular tarsal coalition is best seen on the oblique view, and a talo-calcaneal tarsal coalition can often be seen on the axial view (though a computed tomography [CT] scan is preferable for complete evaluation of that condition). An AP view of the ankle is also necessary, in most cases, to assess varus or valgus deformity at that adjacent joint. The lateral appearance of the ankle can be appreciated on the lateral image of the foot.
The lateral radiograph of a flatfoot reveals plantar flexion of the calcaneus, measured by the calcaneal pitch [39], and an even greater degree of plantar flexion of the talus, measured by the talo-horizontal angle [40] (Fig. 6). Meary [41] defined a normal longitudinal arch as having a continuous straight line formed by the lines drawn through the mid-axis of the talus and the mid-axis of the first metatarsal on a standing lateral radiograph. He defined a flatfoot as one with a plantar sag where those two lines intersect, but there is, in fact, a range of normal values that includes a few degrees of plantar sag.
Fig. 6.

Standing lateral radiograph showing three fairly reliable angular measurements: the calcaneal pitch (CP), talo-horizontal angle (T-H), and Meary’s talus–first metatarsal angle (T-1MT) (Fig. 4, p. 507, from ref. [110], with permission)
The lateral view can also be used to identify the site of the midfoot sag, i.e., the site of the angular deformity. Although the foot is not a single bone, Paley’s [42] concept of the center of rotation of angulation (CORA) can be applied to the foot in a modified version. The site of intersection of the axis of the talus and that of the first metatarsal in a flatfoot is most often located in the head of the talus or at the talo-navicular joint, which indicates that the midfoot sag is at the talo-navicular joint (Fig. 7b). But the CORA can alternatively be located at the naviculo-cuneiform joint, or within the body of one of the mid-tarsal bones. A CORA located in the body of the talus or higher indicates a skewfoot deformity (Fig. 8b)
Fig. 7.
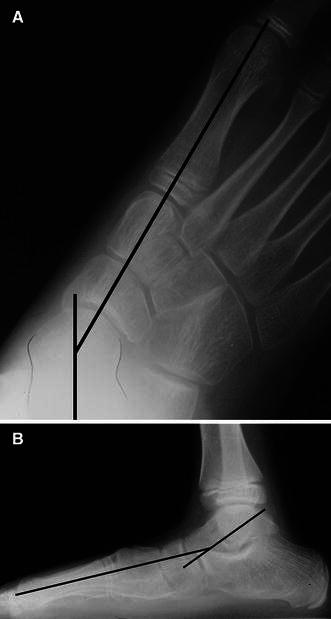
Standing radiographs of a flatfoot showing talus and first metatarsal axis lines crossing at the center of rotation of angulation (CORA) in the center of the head of the talus, indicating a single deformity at the talo-navicular joint. a Anteroposterior view. b Lateral view (Fig. 10-10, p. 144, from ref. [127], with permission)
Fig. 8.

Standing radiographs of a skewfoot showing two opposite direction angular deformities between the talus and the first metatarsal, making the CORA for those bones meaningless. a Anteroposterior view. b Lateral view (Fig. 3A, B, p. 506, from ref. [110], with permission)
It is more difficult to interpret the AP radiograph than the lateral one. The navicular is laterally positioned on the head of the talus in a flatfoot. Since the navicular does not normally ossify until the age of 3–4 years, and since its early ossification is asymmetric toward the lateral aspect of the cartilaginous anlage, assessment of the talo-navicular joint alignment must be accomplished indirectly. The AP talus–first metatarsal angle has been used as an alternative means of evaluating that relationship, but it may be unreliable as well, particularly if there is adduction at the tarso-metatarsal joints, as exists in a skewfoot (Fig. 8a). Using the CORA method, the true site or sites of deformity can be determined. In a simple flatfoot, the CORA should be in the head of the talus or at the talo-navicular joint, which indicates eversion of the subtalar joint that is manifest as abduction at the talo-navicular joint (Fig. 7a). Knowledge of the CORA on the AP and lateral radiographs has implications for surgical treatment.
Treatment
There are no controlled prospective studies documenting the avoidance of long-term pain or disability by prophylactic non-operative or operative treatment of asymptomatic FFF. Therefore, the treatment of people with asymptomatic FFF does not seem reasonable, though there are health care providers who ignore the evidence and treat these feet non-operatively and operatively.
One can currently conclude from the published data that the typical FFF has a normal, but not average, longitudinal arch height. There is no reason to treat that which is normal. Some FFF have arches that are clinically and radiographically beyond 2 standard deviations from average. These are technically abnormal, but there is no evidence that they will necessarily cause disability, so there is no rational indication for treatment. There may, in fact, be some specific advantages to having flatfeet. Giladi et al. [43] found that military recruits with flatfeet had significantly less risk of stress fractures than those with average or high arches.
Despite the absence of scientific evidence for derived benefit, the treatment of asymptomatic flexible flatfoot has been advocated for years. Although several authors [18, 44–46] believed that muscle weakness was responsible for flatfootedness, muscle strengthening exercises with the goal of developing an arch in a child’s foot are unfounded [22].
Several uncontrolled studies in the US have reported that definite permanent increases in arch height can be achieved both clinically and radiographically by the use of “corrective shoes,” over-the-counter and custom-molded arch supports, custom orthoses, and heel wedges [40, 47]. However, the effect of any intervention cannot be determined without appropriate untreated matched controls. And several scientific clinical and radiographic studies [6, 7, 9, 10, 12, 13] have shown that the height of the longitudinal arch increases spontaneously during the first decade of life.
A number of critical investigations of these treatment modalities have shown no positive treatment effect [4, 9, 48–55]. Penneau et al. [51] found no significant radiographic differences between barefeet and those same feet when four types of special shoe modifications and inserts were donned. Rose [52, 53] showed that shoe heel wedges did not change the shape of the foot. The foot maintained its original shape by shifting through the heel pad fat unless the forefoot was also supinated. He further noted that the foot remained flat despite years of using the devices. Helfet [56] stated that arch supports are actually dangerous since they lead to dependency, or what he called a life sentence. The foot remains flat and discontinuation of the device later in life increases the likelihood of symptoms. In the best prospective, randomized study on this topic so far reported, Wenger et al. [55] were unable to show a treatment effect for shoe modifications and inserts on the development of the longitudinal arch in normal children followed for 3–5 years when compared with untreated matched controls.
A potentially negative effect of extrinsic factors on the shape and development of the longitudinal arch is suggested, but not proven, by studies from developing countries. In 1958, Sim-Fook and Hodgson [4] reported that the flatfeet in their non-shoe-wearing Chinese study subjects were asymptomatic, mobile, and flexible. Somewhat surprisingly, they found a slightly higher incidence of flatfeet among the shoe-wearing population, some of which were painful and exhibited restricted mobility. Rao and Joseph [57], in 1992, similarly reported that flatfoot was more common in children in India who wore close-toed shoes than in those who did not wear shoes or who wore slippers or sandals.
Refuting the often-heard comment that at least these devices do no harm is the study by Driano et al. [58], who reported long-term negative psychologic effects on adults who had worn shoe modifications as children compared with controls who did not. Nevertheless, the practice remains commonplace among some health care providers.
Occasionally, flexible flatfoot in a young child is associated with diffuse activity-related pain, causes early fatigue, creates medial foot calluses, and leads to rapid shoe breakdown. Diffuse, non-localized, and nocturnal pain is also occasionally associated with flexible flatfoot. These leg aches, or growing pains, are believed to represent an overuse, or fatigue, syndrome [59]. This is consistent with the findings of Mann and Inman [28] that flatfooted individuals demonstrate greater intrinsic muscle activity than those with higher arches. Soft over-the-counter and firm custom-molded shoe inserts have been shown to relieve or diminish symptoms, and to increase the useful life of shoes without a simultaneous permanent increase on the height of the arch [40, 47, 48, 50, 60]. There is little information available to recommend one device over another.
The exact diagnosis must be established before prescribing orthotic devices. Their use with FFF-STA and rigid flatfeet could actually worsen the symptoms. The talus in an FFF-STA cannot dorsiflex normally because of the tendo-Achilles contracture. Therefore, an orthotic device that is designed to invert the subtalar joint by elevating the anterior end of the talus will meet resistance and increase pressure under the head of the talus, thereby, creating more pressure and pain than that which originally existed. By definition, the shape of a rigid flatfoot will not change with an orthotic device or any other non-surgical intervention. As with the FFF-STA, an orthotic will merely increase pressure and pain under the head of the talus.
It seems reasonable to try to convert a symptomatic FFF-STA to an asymptomatic FFF by heelcord-stretching exercises, which can be performed by parents on their children when they are very young and can be easily monitored by parents when the children are older. There have been no long-term studies on the effectiveness of this program, but it conforms to present knowledge, does no harm, and costs nothing. Therapists are not required. Heelcord-stretching is accomplished with the knee in extension and the subtalar joint in neutral alignment to slight inversion. It is important, though difficult, to achieve this position of the subtalar joint during stretching. Doing so avoids false dorsiflexion through the everted subtalar joint and concentrates the stretch at the ankle joint.
Surgery is rarely, if ever, indicated for flexible flatfoot. If the goal of surgery is to change the shape of the foot, a shape that does not necessarily create problems, the documented risks and complications related to surgery must be weighed against the generally benign natural history of the foot shape itself. Nevertheless, numerous surgical procedures to correct flatfoot have been proposed during the last century. They will be discussed and referenced specifically in the following paragraphs. The indications for these procedures, whether for the correction of deformity, relief of symptoms, or prophylaxis against anticipated pain and disability, are difficult to ascertain from a review of the literature. Therefore, the absolute and comparative success of these procedures is unclear because the reported series: used inconsistent surgical indications; likely included at least some patients with diagnoses other than true FFF; had patients of significantly different ages; lacked standardized evaluation criteria; and frequently had short follow-up. The procedures can be categorized as soft tissue plications, tendon lengthenings and transfers, osseous excisions, osteotomies, arthrodesis of one or more joints, and the interposition of bone or synthetic implants into the sinus tarsi. Combinations of these procedures have been reported.
Isolated soft tissue procedures [19, 61–66] have had routinely unreliable results, leading to their virtual abandonment. The failure of tendon transfer procedures underscores our understanding of the insignificant role of muscles in the maintenance of the arch. Isolated tendo-Achilles lengthening has been suggested to convert a painful FFF-STA to a painless FFF when performed before secondary adaptive or degenerative joint changes, the potential sequelae of FFF-STA, have occurred [15]. However, unsatisfactory results have led most surgeons to combine heelcord-lengthening with a concurrent procedure that changes the shape of the foot.
Bone excision operations [67–69] have been abandoned because of their obvious destructive nature. Arthrodesis of one or more of the joints in the subtalar complex has been abandoned as treatment for FFF because of the detrimental effect of eliminating the shock-absorbing function of that important joint complex. Talo-navicular [70], subtalar [71], and triple [72–74] arthrodeses shift stress to the ankle and mid-tarsal joints, leading to premature degenerative arthrosis at those sites [72–81].
Pseudoarthrodesis, or so-called arthroereisis, procedures were introduced between 1946 and 1977 as variations on a method to restrict excessive subtalar joint eversion by placing a bone block in the sinus tarsi [17, 82–84]. The bone grafts occasionally underwent resorption with recurrence of the deformity, or remained and resulted in the restriction of subtalar motion (essentially a pseudoarthrodesis) with its associated problems. Arthroereisis by means of synthetic implants was started in the late 1970s because of the reported problems and complications associated with the bony arthroereisis procedures. No less than ten types of synthetic implants and methods for insertion have been reported, most with follow-up of less than 2 years [85–97]. Reported problems and complications have led to an ongoing search for a better implant and a better method for implantation. The variety and succession of past implant materials and designs have prevented a validation study from being performed to determine the overall effectiveness of the procedure or even to validate the concept of the procedure [93].
There is no clear consensus among proponents on the indications for arthroereisis. Nevertheless, many are performed and the reported complication rate with the use of synthetic implants is 3.5–30%, with the most recent studies reporting rates of 3.5–11% [85–87, 89–97]. The complications include those associated with inappropriate implantation (not usually counted, but certainly a major issue, especially if one considers the often-reported indication of performing the operation in an asymptomatic physiologic FFF in a young child), surgeon error (malpositioning, overcorrection, undercorrection, extrusion of implant, wrong size of implant), biomaterials problems (breakage, degradation), and biologic problems (foreign body reaction, synovitis, infection, persistent and recurrent pain, implant-induced sinus tarsi impingement pain, intraosseous ganglion cyst within the talus, osteonecrosis of the talus, peroneal spasm, calcaneus fracture) [85–87, 89–97].
The Maxwell–Brancheau arthroereisis (MBA) implant, a large cylinder-shaped titanium screw [90, 91], and the Giannini flatfoot expanding implant, a Teflon/stainless steel expansion drywall anchor design [85, 86], are perhaps the most commonly used implants at the present time, based on the number of articles in the literature. According to published descriptions, both are inserted into the sinus tarsi anterior to the posterior facet along the trajectory of the tarsal canal between the posterior and middle facets. The originators of these implants [85, 86, 90, 91], as well as other authors [87, 92–95, 97], and even the product technique manuals, are evasive regarding the depth to which the implants enter the tarsal canal, though they certainly appear to enter it. Nevertheless, proponents consider them to be extra-articular, if inserted properly, because they do not technically touch articular cartilage, though they clearly encroach upon it. The arthroereisis implants mechanically block eversion, but also decrease the total subtalar joint motion [88, 97], indicating that their effect is, in fact, intra-articular. Furthermore, a magnetic resonance imaging (MRI) study of the subtalar joint in adults with these implants found that the tarsal canal is smaller in height and length than the sizes of implants generally used [95], again suggesting encroachment.
In published studies on subtalar and triple arthrodeses, stress transfer to adjacent joints with the development of degenerative arthroses was not seen for at least 10 years [72–81], which is longer than the follow-up in any of the reports on arthroereisis. Additionally, these implants, not surprisingly, lead to resorption of the adjacent cortical surfaces of the talus and calcaneus (Fig. 9), the long-term effects of which are unknown. And no one has demonstrated or reported whether the implant stays with the calcaneus or with the talus during inversion and eversion of the subtalar joint, whether it matters, and how the answer relates to the long-term success of the procedure.
Fig. 9.
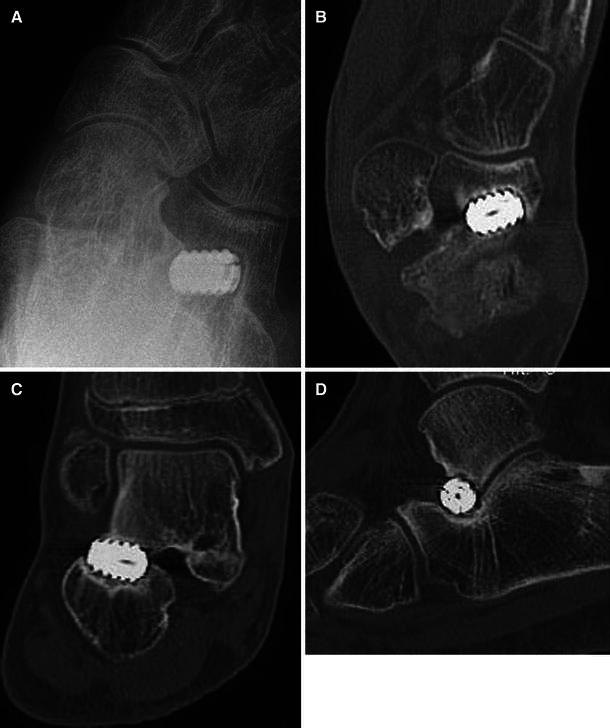
Radiographic and computed tomography (CT) scan images showing resorption of adjacent cortical surfaces of talus and calcaneus due to the presence of a Maxwell–Brancheau arthroereisis (MBA) implant (Fig. 10-11, p. 147, from ref. [127], with permission)
Both the MBA and Giannini arthroereisis implants are now offered as bioabsorbable implants made of poly-l lactic acid (PLLA), but the original metal designs seem to be used most often. The bioabsorbable implants have even shorter follow-up than the original designs. Based on MRI findings, Giannini et al. [85] reported complete resorption of the implant by 4 years after implantation in 21 adolescents. Saxena and Nguyen [95] found MRI evidence of residual bioabsorbable implant at greater than 4 years after implantation. These authors stated that there were no cystic changes noted in the bones, but acknowledged that granuloma formation from PLLA can appear in a delayed fashion. Additionally, their MRI study of the subtalar joint in adults with these implants found that the tarsal canal is smaller in height and length than the implant sizes generally used. They felt that this was a particular problem for the metal implants, and less so for the bioabsorbable ones, unless one considers that children and adolescents have an even smaller canal than the ones which they studied. Finally, they questioned the benefit of the bioabsorbable implants, since half of their patients required or were recommended to have explantation.
The bottom line seems to be that more information and, in particular, long-term studies are needed before arthroereisis can be recommended for children with painful flatfeet. Even more important is the need for the proponents of arthroereisis to clarify surgical indications based on the best scientific evidence available. Finally, it should be clearly noted that the technique of arthroereisis has not been expanded to any other joint in the body, the implications of which are significant.
Perhaps the most popular procedures used to correct FFF during the last century were the many modifications of Hoke’s limited mid-tarsal arthrodeses [18, 24, 27, 79, 98–103]. Hoke [18] felt that the greatest abnormality in painful FFF was localized to the navicular and the two medial cuneiform bones. He reported favorable short-term results with the fusion of these three bones combined with tendo-Achilles lengthening. The Hoke procedure modifications combine arthrodesis of one or more mid-tarsal joints with soft tissue plication across the talo-navicular joint. Tendo-Achilles lengthening was performed with all of the Hoke procedure modifications when 10–15° of dorsiflexion could not be demonstrated after correction of the deformity. Favorable short-term results were consistently reported with these procedures, but unsatisfactory long-term results were reported in 49–80% of cases [24, 79, 100]. The unsatisfactory feet in these series frequently showed persistence or recurrence of pain and deformity, and degenerative changes at the talo-navicular and subtalar joints in addition to the persistence or recurrence of pain and deformity. The originators of these techniques acknowledged that the procedures were not capable of correcting severe hindfoot valgus deformity. This should not have been too surprising, because these procedures do not directly correct the pathologically malaligned subtalar joint, but, instead, address the secondary forefoot supination deformity.
Osteotomy is the last category of procedures that has been used to treat flatfeet. This is a biologic approach that does not depend on soft tissues that are known to stretch out, and it avoids arthrodeses/arthroereisis and the known complications of those procedures. There are two types of osteotomies of the calcaneus that address valgus deformity of the hindfoot. Gleich [104] and, later, Koutsogiannis [105] described an oblique osteotomy of the posterior calcaneus in which the posterior fragment is displaced medially to correct the apparent heel valgus. It does not actually correct the malalignment of the subtalar joint, but merely creates a compensating deformity to improve the valgus angulation of the heel. Recalling Scarpa’s analogy to the hip [35], I believe that the posterior calcaneal displacement osteotomy is the Chiari osteotomy of the acetabulum pedis. Koutsogiannis reported successful “correction” of valgus deformity in 30 of 34 feet, but arch restoration rarely occurred. Other authors confirmed these same results in FFF [45], as well as in paralytic flatfeet [106]. The posterior calcaneus osteotomy does not correct the multiple components of subtalar joint eversion, such as external rotation and dorsiflexion of the acetabulum pedis. Rathjen and Mubarak [107] reported good correction of flatfoot deformities by combining a modification of this osteotomy (medially based closing wedge with medial displacement) with a closing wedge osteotomy of the medial cuneiform, an opening wedge osteotomy of the cuboid, and medial reefing of the talo-navicular joint.
The Dwyer [108] lateral opening wedge osteotomy of the posterior calcaneus represents another attempt to correct severe heel valgus. It is performed less frequently than the medial displacement osteotomy because it does not correct the deformity as completely. The reason for this is that the location of the osteotomy is not at the CORA [42]. The CORA is located at the subtalar joint, so an adjacent angular osteotomy must be combined with translation of the posterior fragment. Alternatively, one can use translational displacement alone, as with the Koutsogiannis procedure, to center the plantar aspect of the posterior calcaneus under the mid-axis of the tibia.
The other osteotomy for correction of valgus deformity of the hindfoot is the calcaneal lengthening osteotomy, conceptualized by Evans [109] and elaborated by Mosca [110, 111]. Evans believed that the lateral column of the flatfoot was shorter than the medial column, a situation exactly opposite to that found in a cavo-varus foot. For painful flatfeet, he equalized the lengths of the columns by inserting a corticocancellous graft into an osteotomy of the anterior calcaneus that was made 1.5 cm proximal to, and parallel with, the calcaneo-cuboid joint. That was the entire extent of his description. By lengthening the calcaneus in this way, he showed that the heel valgus, talo-navicular sag, and lateral subluxation of the navicular on the head of the talus could all be simultaneously corrected. Armstrong and Carruthers [112] recommended the technique and highlighted its advantages to be: correction of hindfoot valgus without the need for arthrodesis, preservation of some subtalar motion, versatility for pronated and abducted feet of different etiologies, and simplicity of execution. Phillips [113] reported a 7–20-year (average 13 years) follow-up of Evans’ patients. Seventeen of the 23 feet had good to very good results when assessed by strict criteria. Anderson and Fowler [114] also reported very good results with this procedure in nine feet followed for an average of 6.5 years. They reaffirmed the correction of all components of the deformity by this simple technique and advised performing the procedure between the ages of 6 and 10 years in appropriate individuals to allow remodeling of the tarsal joints, a consideration not mentioned by Evans.
In 1995, Mosca [110] reported the short-term results of calcaneal lengthening for valgus deformity of the hindfoot from various underlying etiologies in 31 feet in 20 children. He reported correction of all components of even severe eversion positioning of the subtalar joint complex, including dorsiflexion, pronation, and external rotation of the acetabulum pedis around the talar head, at the site of deformity. Function of the subtalar joint was restored, symptoms were relieved, and, at least theoretically, the ankle and mid-tarsal joints were protected from early degenerative arthrosis by avoiding arthrodesis. He stressed the need for strict indications for surgery, specifically a flexible or rigid flatfoot with Achilles or gastrocnemius contracture and intractable pain in the medial midfoot and/or sinus tarsi, despite prolonged attempts at conservative management.
As previously noted, Evans provided very little information on the technique, which made interpretation difficult and surgical success inconsistent by those who read his article. Mosca thoughtfully considered Evans’ concept and applied an understanding of foot biomechanics and the principles of foot deformity-correction surgery to develop a reliable method for achieving consistently good surgical outcomes. His published contributions [36, 110, 111, 115–117] include the location of the skin incision, the specific location and direction of the osteotomy (exiting medially between the anterior and middle facets), the management of the soft tissue constraints along the plantar-lateral border of the foot and the soft tissue redundancy along the plantar-medial border, stabilization of the calcaneo-cuboid joint to prevent subluxation, the need to recognize and concurrently manage rigid forefoot supination deformity if present, and the importance of lengthening the Achilles or gastrocnemius tendon if contracted (which is usually the case in the symptomatic FFF) (Fig. 10).
Fig. 10.
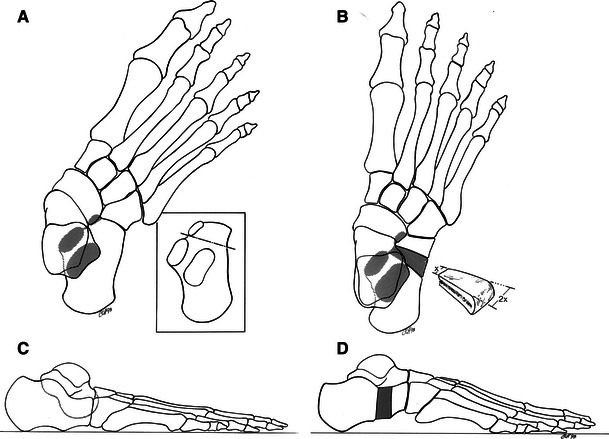
Painful FFF. a, c Anteroposterior (AP) and lateral preoperative sketches of actual radiographs. The talo-first metatarsal angle is markedly abducted on the AP view. The lateral view shows severe talo-navicular sag and a 0° calcaneal pitch. b, d AP and lateral sketches of actual radiographs following a calcaneal lengthening osteotomy and tendo-Achilles lengthening. All components of the deformity are corrected, subtalar motion is preserved, and symptoms are relieved (Fig. 2A–D, p. 502–503, from ref. [110], with permission)
Other authors have subsequently confirmed the efficacy of the calcaneal lengthening osteotomy for relieving pain and correcting deformity in painful flatfeet [118–126].
Obviously, more long-term critical follow-up studies are needed for this procedure and all other conservative and surgical methods of treatment for symptomatic FFF. The Evans/Mosca procedure is unique, however, in that it corrects all components of even the most severe valgus deformities of the hindfoot while preserving subtalar joint motion.
Overview
Flexible flatfoot is a normal foot shape that is present in a large percentage of the population. There are more flatfeet in children than in adults. The arch elevates in most children spontaneously during the first decade of life. There is no evidence that a longitudinal arch can be created in a child’s foot by any external forces or devices. Flexible flatfoot with a short Achilles tendon, in contrast to simple flexible flatfoot, is known to cause pain and disability in some adolescents and adults. Surgery is indicated in flexible flatfeet with short Achilles tendons when conservative measurements fail to relieve pain under the head of the plantar flexed talus or in the sinus tarsi area. Joint-preserving, deformity-correcting osteotomy techniques should be used along with Achilles tendon lengthening in those cases. Rigid forefoot supination is an additional deformity in many flatfeet that, if present, must be identified and treated concurrently during surgical reconstruction.
References
- 1.Harris RI, Beath T. Army foot survey. Ottawa: National Research Council of Canada; 1947. pp. 1–268. [Google Scholar]
- 2.Bonnet WL, Baker DR. Diagnosis of pes planus by X-ray. Radiology. 1946;46:36–45. doi: 10.1148/46.1.36. [DOI] [PubMed] [Google Scholar]
- 3.Mann RA. Miscellaneous afflictions of the foot. In: Mann RA, editor. Surgery of the foot. St. Louis: CV Mosby; 1986. pp. 230–238. [Google Scholar]
- 4.Sim-Fook L, Hodgson AR. A comparison of foot forms among the non-shoe and shoe-wearing Chinese population. J Bone Joint Surg Am. 1958;40:1058–1062. [PubMed] [Google Scholar]
- 5.Stewart SF. Human gait and the human foot: an ethnological study of flatfoot. I. Clin Orthop Relat Res. 1970;70:111–123. [PubMed] [Google Scholar]
- 6.Morley AJ. Knock-knee in children. Br Med J. 1957;2:976–979. doi: 10.1136/bmj.2.5051.976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blount WP. Fractures in children. Huntingdon, NY: Kreiger; 1977. p. 185. [Google Scholar]
- 8.Tachdjian MO. The child’s foot. Philadelphia: WB Saunders; 1985. pp. 556–597. [Google Scholar]
- 9.Gould N, Moreland M, Alvarez R, Trevino S, Fenwick J. Development of the child’s arch. Foot Ankle. 1989;9:241–245. doi: 10.1177/107110078900900506. [DOI] [PubMed] [Google Scholar]
- 10.Ozonoff MB. Pediatric orthopedic radiology. Philadelphia: WB Saunders; 1979. p. 300. [Google Scholar]
- 11.Templeton AW, McAlister WH, Zim ID. Standardization of terminology and evaluation of osseous relationships in congenitally abnormal feet. Am J Roentgenol Radium Ther Nucl Med. 1965;93:374–381. [PubMed] [Google Scholar]
- 12.Staheli LT, Chew DE, Corbett M. The longitudinal arch. A survey of eight hundred and eighty-two feet in normal children and adults. J Bone Joint Surg Am. 1987;69:426–428. [PubMed] [Google Scholar]
- 13.Vanderwilde R, Staheli LT, Chew DE, Malagon V. Measurements on radiographs of the foot in normal infants and children. J Bone Joint Surg Am. 1988;70:407–415. [PubMed] [Google Scholar]
- 14.Steel MW, 3rd, Johnson KA, DeWitz MA, Ilstrup DM. Radiographic measurements of the normal adult foot. Foot Ankle. 1980;1:151–158. doi: 10.1177/107110078000100304. [DOI] [PubMed] [Google Scholar]
- 15.Harris RI, Beath T. Hypermobile flat-foot with short tendo achillis. J Bone Joint Surg Am. 1948;30:116–140. [PubMed] [Google Scholar]
- 16.Duchenne GB. Physiology of motion. Philadelphia: WB Saunders; 1959. p. 337. [Google Scholar]
- 17.Haraldsson S. Pes plano-valgus staticus juvenilis and its operative treatment. Acta Orthop Scand. 1965;35:234–256. doi: 10.3109/17453676508989356. [DOI] [PubMed] [Google Scholar]
- 18.Hoke M. An operation for the correction of extremely relaxed flat feet. J Bone Joint Surg. 1931;13:773–783. [Google Scholar]
- 19.Jones BS. Flat foot. A preliminary report of an operation for severe cases. J Bone Joint Surg Br. 1975;57:279–282. [PubMed] [Google Scholar]
- 20.Jones RL. The human foot. An experimental study of its mechanics, and the role of its muscles and ligaments in the support of the arch. Am J Anat. 1941;68:1–39. [Google Scholar]
- 21.Niederecker K. Operationsverfahren zur behandlung des plattfusses. Chir Pediatr. 1932;4:182–183. [Google Scholar]
- 22.Basmajian JV, Stecko G. The role of muscles in arch support of the foot. An electromyographic study. J Bone Joint Surg Am. 1963;45:1184–1190. [PubMed] [Google Scholar]
- 23.Gray EG, Basmajian JV. Electromyography and cinematography of leg and foot (“normal” and flat) during walking. Anat Rec. 1968;161:1–15. doi: 10.1002/ar.1091610101. [DOI] [PubMed] [Google Scholar]
- 24.Butte FL. Navicular-cuneiform arthrodesis for flat-foot: an end-result study. J Bone Joint Surg. 1937;19:496–502. [Google Scholar]
- 25.Hicks JH. The mechanics of the foot. I. The joints. J Anat. 1953;87:345–357. [PMC free article] [PubMed] [Google Scholar]
- 26.Hicks JH. The mechanics of the foot. II. The plantar aponeurosis and the arch. J Anat. 1954;88:25–30. [PMC free article] [PubMed] [Google Scholar]
- 27.Jack EA. Naviculo-cuneiform fusion in the treatment of flat foot. J Bone Joint Surg Br. 1953;35:75–82. doi: 10.1302/0301-620X.35B1.75. [DOI] [PubMed] [Google Scholar]
- 28.Mann R, Inman VT. Phasic activity of intrinsic muscles of the foot. J Bone Joint Surg Am. 1969;46:469–481. [PubMed] [Google Scholar]
- 29.Close JR, Inman VT (1953) The action of the subtalar joint. California Prosthetic Devices Research Report, series 11(24)
- 30.Close JR, Inman VT, Poor PM, Todd FN. The function of the subtalar joint. Clin Orthop Relat Res. 1967;50:159–179. [PubMed] [Google Scholar]
- 31.Elftman H. The transverse tarsal joint and its control. Clin Orthop. 1960;16:41–46. [PubMed] [Google Scholar]
- 32.Inman VT. The joints of the ankle. Baltimore: Williams & Wilkins; 1976. [Google Scholar]
- 33.Mann RA. Biomechanics of the foot and ankle. In: Mann RA, editor. Surgery of the foot. St. Louis: CV Mosby; 1986. pp. 1–30. [Google Scholar]
- 34.Manter JT. Movements of the subtalar and transverse tarsal joints. Anat Rec. 1941;80:397–410. [Google Scholar]
- 35.Scarpa A (1994) A memoir on the congenital club feet of children, and of the mode of correcting that deformity. Edinburgh: Archibald Constable, 1818:8–15 (Translated by Wishart JH, Clin Orthop Relat Res 308:4–7) [PubMed]
- 36.DuMontier TA, Falicov A, Mosca V, Sangeorzan B. Calcaneal lengthening: investigation of deformity correction in a cadaver flatfoot model. Foot Ankle Int. 2005;26:166–170. doi: 10.1177/107110070502600209. [DOI] [PubMed] [Google Scholar]
- 37.Scranton PE, Goldner JL, Lutter LD, Staheli LT. Management of hypermobile flatfoot in the child. Contemp Orthop. 1981;3:645–663. [Google Scholar]
- 38.Mosca VS. The child’s foot: principles of management [editorial] J Pediatr Orthop. 1998;18:281–282. [PubMed] [Google Scholar]
- 39.Gamble FO, Yale I. Clinical foot roentgenology. Baltimore: Williams & Wilkins; 1966. p. 153. [Google Scholar]
- 40.Bleck EE, Berzins UJ. Conservative management of pes valgus with plantar flexed talus, flexible. Clin Orthop Relat Res. 1977;122:85–94. [PubMed] [Google Scholar]
- 41.Meary R. On the measurement of the angle between the talus and the first metatarsal. Symposium: Le Pied Creux Essential. Rev Chir Orthop. 1967;53:389. [Google Scholar]
- 42.Paley D. Principles of deformity correction. Berlin: Springer-Verlag; 2002. [Google Scholar]
- 43.Giladi M, Milgrom C, Stein M, Kashtan M, Margulies J, Chisin R, Steinberg R, Aharonson Z. The low arch, a protective factor in stress fractures. Orthop Rev. 1985;14(11):81–84. [Google Scholar]
- 44.Bettmann E. The treatment of flat-foot by means of exercise. J Bone Joint Surg Am. 1937;19:821–825. [Google Scholar]
- 45.Lord JP. Correction of extreme flat foot. JAMA. 1923;81:1502. [Google Scholar]
- 46.Zadek I. Transverse-wedge arthrodesis for the relief of pain in rigid flat-foot. J Bone Joint Surg. 1935;17:453–467. [Google Scholar]
- 47.Bordelon RL. Correction of hypermobile flatfoot in children by molded insert. Foot Ankle. 1980;1:143–150. doi: 10.1177/107110078000100303. [DOI] [PubMed] [Google Scholar]
- 48.Basta NW, Mital MA, Bonadio O, Johnson A, Kang SY, O’Connor J. A comparative study of the role of shoes, arch supports, and navicular cookies in the management of symptomatic mobile flat feet in children. Int Orthop. 1977;1:143–148. [Google Scholar]
- 49.Bleck EE. The shoeing of children: sham or science? Dev Med Child Neurol. 1971;13:188–195. doi: 10.1111/j.1469-8749.1971.tb03244.x. [DOI] [PubMed] [Google Scholar]
- 50.Mereday C, Dolan CM, Lusskin R. Evaluation of the University of California Biomechanics Laboratory shoe insert in “flexible” pes planus. Clin Orthop Relat Res. 1972;82:45–58. [PubMed] [Google Scholar]
- 51.Penneau K, Lutter LD, Winter RD. Pes planus: radiographic changes with foot orthoses and shoes. Foot Ankle. 1982;2:299–303. doi: 10.1177/107110078200200508. [DOI] [PubMed] [Google Scholar]
- 52.Rose GK. Correction of the pronated foot. J Bone Joint Surg Br. 1958;40:674–683. doi: 10.1302/0301-620X.40B4.674. [DOI] [PubMed] [Google Scholar]
- 53.Rose GK. Correction of the pronated foot. J Bone Joint Surg Br. 1962;44:642–647. doi: 10.1302/0301-620X.44B3.642. [DOI] [PubMed] [Google Scholar]
- 54.Staheli LT, Giffin L. Corrective shoes for children: a survey of current practice. Pediatrics. 1980;65:13–17. [PubMed] [Google Scholar]
- 55.Wenger DR, Mauldin D, Speck G, Morgan D, Lieber RL. Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. J Bone Joint Surg Am. 1989;71:800–810. [PubMed] [Google Scholar]
- 56.Helfet AJ. A new way of treating flat feet in children. Lancet. 1956;1:262–264. doi: 10.1016/s0140-6736(56)91187-4. [DOI] [PubMed] [Google Scholar]
- 57.Rao UB, Joseph B. The influence of footwear on the prevalence of flat foot. A survey of 2300 children. J Bone Joint Surg Br. 1992;74:525–527. doi: 10.1302/0301-620X.74B4.1624509. [DOI] [PubMed] [Google Scholar]
- 58.Driano AN, Staheli L, Staheli LT. Psychosocial development and corrective shoewear use in childhood. J Pediatr Orthop. 1998;18:346–349. [PubMed] [Google Scholar]
- 59.Peterson H. Growing pains. Pediatr Clin North Am. 1986;33:1365–1372. doi: 10.1016/s0031-3955(16)36147-8. [DOI] [PubMed] [Google Scholar]
- 60.Theologis TN, Gordon C, Benson MK. Heel seats and shoe wear. J Pediatr Orthop. 1994;14:760–762. doi: 10.1097/01241398-199414060-00013. [DOI] [PubMed] [Google Scholar]
- 61.Gocht H. Schenenoperation beim pes Plano-valgus. Z Orthop Chir. 1905;14:693–697. [Google Scholar]
- 62.Legg AT. The treatment of congenital flatfoot by tendon transplantation. Am J Orthop Surg. 1912;10:584. [Google Scholar]
- 63.Phelps AM. The etiology, pathology, and treatment of flat-foot. Post Grad Med. 1892;7:104. [Google Scholar]
- 64.Roberts PW. An operation for valgus feet. JAMA. 1921;77:1571. [Google Scholar]
- 65.Ryerson EW. Tendon transplantation in flat-foot. Am J Orthop Surg. 1909;7:505. [Google Scholar]
- 66.Young CS. Operative treatment of pes planus. Surg Gynecol Obstet. 1939;68:1099–1101. [Google Scholar]
- 67.Davy R. On excision of the scaphoid bone for the relief of confirmed flatfoot. Lancet. 1889;1:675. [Google Scholar]
- 68.Golding-Bird CH. Operations on the tarsus in confirmed flat-foot. Lancet. 1889;1:677. [Google Scholar]
- 69.Stokes W (1885) Astragaloid osteotomy in the treatment of flat-foot. Trans Acad Med Ireland III: 141 [DOI] [PMC free article] [PubMed]
- 70.Lowman CL. An operative method for correction of certain forms of flatfoot. JAMA. 1923;81:1500–1502. [Google Scholar]
- 71.Grice DS. An extra-articular arthrodesis of the subastragalar joint for correction of paralytic flat feet in children. J Bone Joint Surg Am. 1952;34:927–940. [PubMed] [Google Scholar]
- 72.Adelaar RS, Dannelly EA, Meunier PA, Stelling FH, Goldner JL, Colvard DF. A long term study of triple arthrodesis in children. Orthop Clin North Am. 1976;7:895–908. [PubMed] [Google Scholar]
- 73.Angus PD, Cowell HR. Triple arthrodesis. A critical long-term review. J Bone Joint Surg Br. 1986;68:260–265. doi: 10.1302/0301-620X.68B2.3958012. [DOI] [PubMed] [Google Scholar]
- 74.Saltzman CL, Fehrle MJ, Cooper RR, Spencer EC, Ponseti IV. Triple arthrodesis: twenty-five and forty-four-year average follow-up of the same patients. J Bone Joint Surg Am. 1999;81:1391–1402. [PubMed] [Google Scholar]
- 75.Drew AJ. The late results of arthrodesis of the foot. J Bone Joint Surg Br. 1951;33:496–502. doi: 10.1302/0301-620X.33B4.496. [DOI] [PubMed] [Google Scholar]
- 76.McCall RE, Lillich JS, Harris JR, Johnston FA. The Grice extraarticular subtalar arthrodesis: a clinical review. J Pediatr Orthop. 1985;5:442–445. doi: 10.1097/01241398-198507000-00011. [DOI] [PubMed] [Google Scholar]
- 77.Ross PM, Lyne ED. The Grice procedure: indications and evaluation of long-term results. Clin Orthop Relat Res. 1980;153:194–200. [PubMed] [Google Scholar]
- 78.Scott SM, Janes PC, Stevens PM. Grice subtalar arthrodesis followed to skeletal maturity. J Pediatr Orthop. 1988;8:176–183. [PubMed] [Google Scholar]
- 79.Seymour N. The late results of naviculo-cuneiform fusion. J Bone Joint Surg Br. 1967;49:558–559. [PubMed] [Google Scholar]
- 80.Smith JB, Westin GW. Subtalar extra-articular arthrodesis. J Bone Joint Surg Am. 1968;50:1027–1035. [PubMed] [Google Scholar]
- 81.Southwell RB, Sherman FC. Triple arthrodesis: a long-term study with force plate analysis. Foot Ankle. 1981;2:15–24. doi: 10.1177/107110078100200103. [DOI] [PubMed] [Google Scholar]
- 82.Chambers EFS. An operation for the correction of flexible flat feet of adolescents. West J Surg Obstet Gynecol. 1946;54:77–86. [PubMed] [Google Scholar]
- 83.LeLièvre J. Current concepts and correction in the valgus foot. Clin Orthop Relat Res. 1970;70:43–55. [PubMed] [Google Scholar]
- 84.Miller GR. The operative treatment of hypermobile flatfeet in the young child. Clin Orthop Relat Res. 1977;122:95–101. [PubMed] [Google Scholar]
- 85.Giannini BS, Ceccarelli F, Benedetti MG, Catani F, Faldini C. Surgical treatment of flexible flatfoot in children: a four-year follow-up study. J Bone Joint Surg Am. 2001;83(Suppl 2, Pt 2):73–79. doi: 10.2106/00004623-200100022-00003. [DOI] [PubMed] [Google Scholar]
- 86.Giannini S, Girolami M, Ceccarelli F. The surgical treatment of infantile flat foot. A new expanding endo-orthotic implant. Ital J Orthop Traumatol. 1985;11:315–322. [PubMed] [Google Scholar]
- 87.Gutiérrez PR, Lara MH. Giannini prosthesis for flatfoot. Foot Ankle Int. 2005;26:918–926. doi: 10.1177/107110070502601104. [DOI] [PubMed] [Google Scholar]
- 88.Husain ZS, Fallat LM. Biomechanical analysis of Maxwell–Brancheau arthroereisis implants. J Foot Ankle Surg. 2002;41:352–358. doi: 10.1016/s1067-2516(02)80080-1. [DOI] [PubMed] [Google Scholar]
- 89.Lanham RH., Jr Indications and complications of arthroereisis in hypermobile flatfoot. J Am Podiatr Med Assoc. 1979;69:178–185. doi: 10.7547/87507315-69-3-178. [DOI] [PubMed] [Google Scholar]
- 90.Maxwell JR, Carro A, Sun C. Use of the Maxwell–Brancheau arthroereisis implant for the correction of posterior tibial tendon dysfunction. Clin Podiatr Med Surg. 1999;16:479–489. [PubMed] [Google Scholar]
- 91.Maxwell JR, Knudson W, Cerniglia M. The MBA arthroereisis implant: early prospective results. In: Vickers NS, Miller SJ, Mahan KT, editors. Reconstructive surgery of the foot and leg. Tucker, GA: The Podiatry Institute; 1997. pp. 256–264. [Google Scholar]
- 92.Needleman RL. Current topic review: subtalar arthroereisis for the correction of flexible flatfoot. Foot Ankle Int. 2005;26:336–346. doi: 10.1177/107110070502600411. [DOI] [PubMed] [Google Scholar]
- 93.Nelson SC, Haycock DM, Little ER. Flexible flatfoot treatment with arthroereisis: radiographic improvement and child health survey analysis. J Foot Ankle Surg. 2004;43:144–155. doi: 10.1053/j.jfas.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 94.Oloff LM, Naylor BL, Jacobs AM. Complications of subtalar arthroereisis. J Foot Surg. 1987;26:136–140. [PubMed] [Google Scholar]
- 95.Saxena A, Nguyen A. Preliminary radiographic findings and sizing implications on patients undergoing bioabsorbable subtalar arthroereisis. J Foot Ankle Surg. 2007;46:175–180. doi: 10.1053/j.jfas.2007.01.009. [DOI] [PubMed] [Google Scholar]
- 96.Smith SD, Millar EA. Arthrorisis by means of a subtalar polyethylene peg implant for correction of hindfoot pronation in children. Clin Orthop Relat Res. 1983;181:15–23. [PubMed] [Google Scholar]
- 97.Zaret DI, Myerson MS. Arthroerisis of the subtalar joint. Foot Ankle Clin. 2003;8:605–617. doi: 10.1016/s1083-7515(03)00041-x. [DOI] [PubMed] [Google Scholar]
- 98.Caldwell GD. Surgical correction of relaxed flatfoot by the Durham flatfoot plasty. Clin Orthop. 1953;2:221–226. [PubMed] [Google Scholar]
- 99.Coleman SS, editor. Complex foot deformities in children. Philadelphia: Lea & Febiger; 1983. pp. 193–222. [Google Scholar]
- 100.Crego CH, Jr, Ford LT. An end-result of various operative procedures for correcting flat feet in children. J Bone Joint Surg Am. 1952;34:183–195. [PubMed] [Google Scholar]
- 101.Duncan JW, Lovell WW. Modified Hoke–Miller flatfoot procedure. Clin Orthop Relat Res. 1983;181:24–27. [PubMed] [Google Scholar]
- 102.Giannestras NJ. Flexible valgus flatfoot resulting from naviculocuneiform and talonavicular sag. Surgical correction in the adolescent. In: Bateman JE, editor. Foot science. Philadelphia: WB Saunders; 1976. pp. 67–105. [Google Scholar]
- 103.Miller OL. A plastic flat foot operation. J Bone Joint Surg. 1927;9:84–91. [Google Scholar]
- 104.Gleich A. Beitrag Zur Operativen Plattfussbehandlung. Arch Klin Chir. 1893;46:358–362. [Google Scholar]
- 105.Koutsogiannis E. Treatment of mobile flat foot by displacement osteotomy of the calcaneus. J Bone Joint Surg Br. 1971;53:96–100. [PubMed] [Google Scholar]
- 106.Silver CM, Simon SD, Litchman HM. Long term follow-up observations on calcaneal osteotomy. Clin Orthop Relat Res. 1974;99:181–187. doi: 10.1097/00003086-197403000-00022. [DOI] [PubMed] [Google Scholar]
- 107.Rathjen KE, Mubarak SJ. Calcaneal-cuboid-cuneiform osteotomy for the correction of valgus foot deformities in children. J Pediatr Orthop. 1998;18:775–782. [PubMed] [Google Scholar]
- 108.Dwyer FC. Osteotomy of the calcaneum for pes cavus. J Bone Joint Surg Br. 1959;41:80–86. doi: 10.1302/0301-620X.41B1.80. [DOI] [PubMed] [Google Scholar]
- 109.Evans D. Calcaneo-valgus deformity. J Bone Joint Surg Br. 1975;57:270–278. [PubMed] [Google Scholar]
- 110.Mosca VS. Calcaneal lengthening for valgus deformity of the hindfoot. Results in children who had severe, symptomatic flatfoot and skewfoot. J Bone Joint Surg Am. 1995;77:500–512. doi: 10.2106/00004623-199504000-00002. [DOI] [PubMed] [Google Scholar]
- 111.Mosca VS. Calcaneal lengthening osteotomy for valgus deformity of the hindfoot. In: Skaggs DL, Tolo VT, editors. Master techniques in orthopaedic surgery: pediatrics. Philadelphia: Lippincott Williams & Wilkins; 2008. pp. 263–276. [Google Scholar]
- 112.Armstrong G, Carruthers CC. Evans elongation of lateral column of the foot for valgus deformity. J Bone Joint Surg Br. 1975;57:530. [Google Scholar]
- 113.Phillips GE. A review of elongation of os calcis for flat feet. J Bone Joint Surg Br. 1983;65:15–18. doi: 10.1302/0301-620X.65B1.6337167. [DOI] [PubMed] [Google Scholar]
- 114.Anderson AF, Fowler SB. Anterior calcaneal osteotomy for symptomatic juvenile pes planus. Foot Ankle. 1984;4:274–283. doi: 10.1177/107110078400400509. [DOI] [PubMed] [Google Scholar]
- 115.Mosca VS. The foot. In: Morrissy RT, Weinstein SL, editors. Lovell and Winter’s pediatric orthopedics. 5. Philadelphia: Lippincott Williams & Wilkins; 2001. pp. 1151–1215. [Google Scholar]
- 116.Sangeorzan BJ, Mosca V, Hansen ST., Jr Effect of calcaneal lengthening on relationships among the hindfoot, midfoot, and forefoot. Foot Ankle. 1993;14:136–141. doi: 10.1177/107110079301400305. [DOI] [PubMed] [Google Scholar]
- 117.Warme WJ, Mosca VS, Conrad EU. Comparison of structural bone allografts and autografts in pediatric foot surgery. Orthop Trans. 1997;21(2):651–652. doi: 10.1097/BPO.0b013e31824b6c82. [DOI] [PubMed] [Google Scholar]
- 118.Arangio GA, Chopra V, Voloshin A, Salathe EP. A biomechanical analysis of the effect of lateral column lengthening calcaneal osteotomy on the flat foot. Clin Biomech. 2007;22:472–477. doi: 10.1016/j.clinbiomech.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 119.Benthien RA, Parks BG, Guyton GP, Schon LC. Lateral column calcaneal lengthening, flexor digitorum longus transfer, and opening wedge medial cuneiform osteotomy for flexible flatfoot: a biomechanical study. Foot Ankle Int. 2007;28:70–77. doi: 10.3113/FAI.2007.0013. [DOI] [PubMed] [Google Scholar]
- 120.Doğan A, Albayrak M, Akman YE, Zorer G. The results of calcaneal lengthening osteotomy for the treatment of flexible pes planovalgus and evaluation of alignment of the foot. Acta Orthop Traumatol Turc. 2006;40:356–366. [PubMed] [Google Scholar]
- 121.Dollard MD, Marcinko DE, Lazerson A, Elleby DH. The Evans calcaneal osteotomy for correction of flexible flatfoot syndrome. J Foot Surg. 1984;23:291–301. [PubMed] [Google Scholar]
- 122.Oeffinger DJ, Pectol RW, Jr, Tylkowski CM. Foot pressure and radiographic outcome measures of lateral column lengthening for pes planovalgus deformity. Gait Posture. 2000;12:189–195. doi: 10.1016/s0966-6362(00)00075-8. [DOI] [PubMed] [Google Scholar]
- 123.Park KB, Park HW, Lee KS, Joo SY, Kim HW. Changes in dynamic foot pressure after surgical treatment of valgus deformity of the hindfoot in cerebral palsy. J Bone Joint Surg Am. 2008;90:1712–1721. doi: 10.2106/JBJS.G.00792. [DOI] [PubMed] [Google Scholar]
- 124.Viegas GV. Reconstruction of the pediatric flexible planovalgus foot by using an Evans calcaneal osteotomy and augmentative medial split tibialis anterior tendon transfer. J Foot Ankle Surg. 2003;42:199–207. doi: 10.1016/s1067-2516(03)70029-5. [DOI] [PubMed] [Google Scholar]
- 125.Yoo WJ, Chung CY, Choi IH, Cho TJ, Kim DH. Calcaneal lengthening for the planovalgus foot deformity in children with cerebral palsy. J Pediatr Orthop. 2005;25:781–785. doi: 10.1097/01.bpo.0000184650.26852.37. [DOI] [PubMed] [Google Scholar]
- 126.Zeifang F, Breusch SJ, Döderlein L. Evans calcaneal lengthening procedure for spastic flexible flatfoot in 32 patients (46 feet) with a followup of 3 to 9 years. Foot Ankle Int. 2006;27:500–507. doi: 10.1177/107110070602700704. [DOI] [PubMed] [Google Scholar]
- 127.Mosca VS. Flexible flatfoot and skewfoot. In: McCarthy JJ, Drennan JC, editors. Drennan’s the child’s foot and ankle. 2. Philadelphia: Lippincott Williams & Wilkins; 2009. pp. 136–159. [Google Scholar]


