Abstract
Objectives
Determine if serial measurement of N-terminal pro B-type natriuretic peptide (NT-proBNP) in community dwelling elderly would provide additional prognostic information to traditional risk factors.
Background
Accurate cardiovascular risk stratification is challenging in the elderly.
Methods
NT-proBNP was measured at baseline and 2-3 years later in 2,975 community-dwelling older adults free of heart failure in the longitudinal Cardiovascular Health Study. This investigation examined the risk of new-onset heart failure (HF) and death from cardiovascular (CV) causes associated with baseline NT-proBNP and changes in NT-proBNP levels, adjusting for potential confounders.
Results
NT-proBNP levels in the highest quintile (>267.7 pg/mL) were independently associated with greater risks of HF (hazard ratio [HR] =3.05 (95%CI [confidence interval] 2.46-3.78) and CV death (HR=3.02, 95%CI 2.36-3.86) compared to the lowest quintile (<47.5 pg/mL). The inflection point for elevated risk occurred at NT-proBNP=190 pg/mL. Among participants with initially low NT-proBNP (<190 pg/mL), those who developed a >25% increase on follow-up to >190 pg/mL (21%) were at greater adjusted risk of HF (HR=2.13, 95%CI=1.68-2.71) and CV death (HR=1.91, 95%CI=1.43-2.53) compared to those with sustained low levels. Among participants with initially high NT-proBNP, those who developed >25% increase (40%) were at higher risk of HF (HR=2.06 95%CI 1.56 −2.72) and cardiovascular death (HR=1.88, 95%CI 1.37-2.57), whereas those who developed >25% decrease to ≤190pg/mL (15%) were at lower risk of HF (HR=0.58, 95%CI 0.36-0.93) and CV death (HR=0.57, 95%CI 0.32 −1.01) compared to those with unchanged high values.
Conclusion
NT-proBNP levels independently predict heart failure and cardiovascular death in older adults. NT-proBNP levels frequently change over time and these fluctuations reflect dynamic changes in cardiovascular risk.
Keywords: biomarkers, risk stratification, heart failure, elderly
Introduction
Heart failure is associated with high mortality risk and hospitalization in older adults, accounting for more than 875,000 annual admissions (1). Despite declines in the rates of cardiovascular deaths in the general population, more than 80% of cardiovascular deaths occur in the elderly (2). Traditional cardiovascular risk factors, while adept at predicting cardiovascular events in middle-aged populations, are less predictive in the elderly (3). Subclinical cardiovascular disease is common in the elderly and associated with an increased risk of cardiovascular events including heart failure (4). Furthermore, the development of new subclinical disease on repeated measures is associated with increased risk compared to subjects who remain without identifiable disease (4).
Blood-based biomarkers provide an attractive adjunctive methodology for identifying older individuals at higher risk for adverse cardiovascular events. Natriuretic peptide levels (BNP and NT-proBNP) are associated with long-term cardiovascular outcomes in the general community (5-9). However, it is controversial whether a natriuretic peptide level provides additional prognostic information beyond traditional risk-factors in this population (7,10). The CHS cohort of elderly participants with long-term follow-up, detailed risk factor assessment and electrocardiographic and echocardiographic data allows the opportunity to test if measurement of NT-proBNP provides independent and additive information. Nevertheless, a single measurement of NT-proBNP can't reflect change in subclinical disease and therefore may not optimally stratify long-term cardiovascular outcomes (4).
We hypothesized that NT-proBNP, in an ambulatory elderly population free of heart failure, would be independently associated with new onset heart failure and cardiovascular death after adjusting for prevalent comorbidities and cardiovascular risk factors. Furthermore, we anticipated that serial measurements of NT-proBNP, as a possible surrogate for change in subclinical disease status, identify a dynamic change in long-term risk for incident heart failure and cardiovascular mortality. Specifically, we hypothesized that individuals displaying increases in NT-proBNP over time have elevated risks, independent of baseline NT-proBNP levels and cardiovascular risk factors.
Methods
Study Population
CHS is a multicenter prospective observational cohort study of cardiovascular disease in the elderly. A detailed description of the study methods has been published previously (11). For the present analysis, participants with prior heart failure at study entry were excluded. Heart failure was identified by self-report and confirmed by medical record review and/or physician interview as described previously (12).
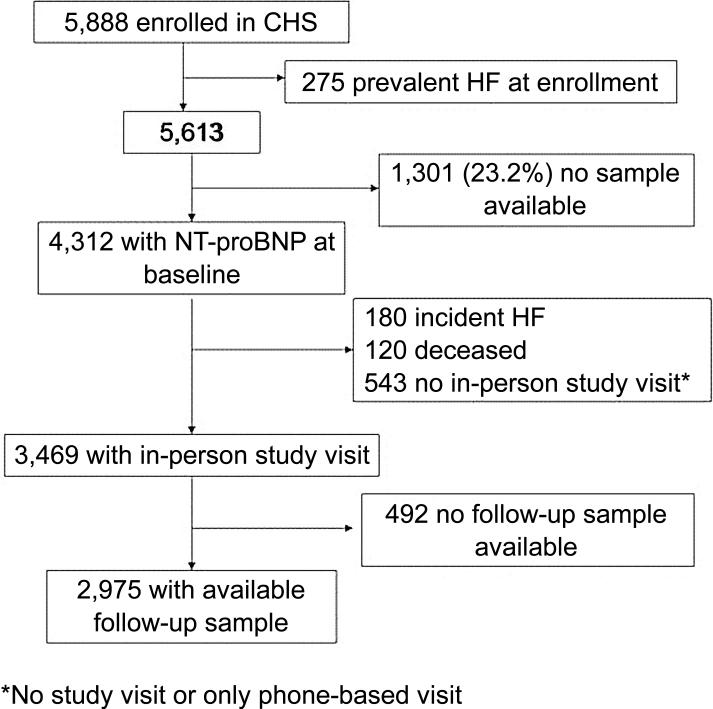
Of the 5,888 CHS participants, prevalent heart failure was present in 275 (4.7%), and sufficient serum for NT-proBNP measurement was available in 4,312 (76.8%) (Figure 1). Comparing those with and without sufficient sera volumes, there were no significant differences in demographics and most clinical measures. Modest but statistically significant differences were observed between those with and without NT-proBNP measurements in the frequency of diabetes (17.7 % vs. 8.6%), hypertension (59.4% vs. 54.9%), and current smoking (11% vs. 15%).
Figure 1. Flow diagram of cardiovascular health study participants.
Cardiovascular health study participants (CHS) with blood samples available for amino terminal pro-B-type natriuretic peptide (NT-proBNP) at baseline and follow-up visits. HF, heart failure.
The CHS was approved by the institutional review boards of the University of Washington and the participating centers. The current analysis was approved by the institutional review board of the University of Maryland, Baltimore.
Assay methods
NT-proBNP was measured in serum collected at baseline in the main CHS cohort (1989-90) and the supplemental cohort (1992-93). A second measure of NT-proBNP was performed on sera collected 3 years later for the main cohort (1992-1993) and 2 years later for the supplemental cohort (1994-1995). NT-proBNP was measured on the Elecsys 2010 system (Roche Diagnostics, Indianapolis, IN). The coefficient of variation for the NT-proBNP assay was 2-5% during the testing period, and the analytical measurement range for NT-proBNP was 5-35,000 pg/mL. All samples were stored at −70° to −80° C and were thawed prior to testing (maximum of 3 freeze-thaw cycles). Measurements of NT-proBNP using this assay do not change after 5 freeze-thaw cycles (13).
Primary Outcomes
Outcomes were incident heart failure and cardiovascular mortality. Incident heart failure events were ascertained by participant interview at semi-annual study visits, and through examination of Medicare claims data. Potential heart failure events and determination of cause of death were determined by an expert adjudication panel (14). Cardiovascular death was defined as death related to atherosclerotic heart disease (fatal myocardial infarction and definite and possible fatal coronary heart disease), death following cerebrovascular disease (fatal stroke) or death from other atherosclerotic and cardiovascular diseases as described in detail previously (14).
Other covariates
Clinical characteristics were obtained from the initial CHS study visit for each cohort (for the analysis of baseline NT-proBNP and outcomes) or at the study visit of the follow-up NT-proBNP (for the analysis of change in NT-proBNP and outcomes). The methodology for assessing cardiovascular risk factors has been described previously (12).
Coronary heart disease was defined as a history of angina, myocardial infarction, coronary angioplasty, or coronary artery bypass surgery. An ECG was performed annually; left ventricular mass was estimated from the ECG, and major ECG abnormalities including atrial fibrillation were defined according to previously described methods (15,16). Echocardiography was performed on the main cohort in 1989-90 and in both cohorts in 1995-96. Measures of interest for this analysis included left atrial diameter and qualitative LVEF (normal, borderline, or abnormal) (17).
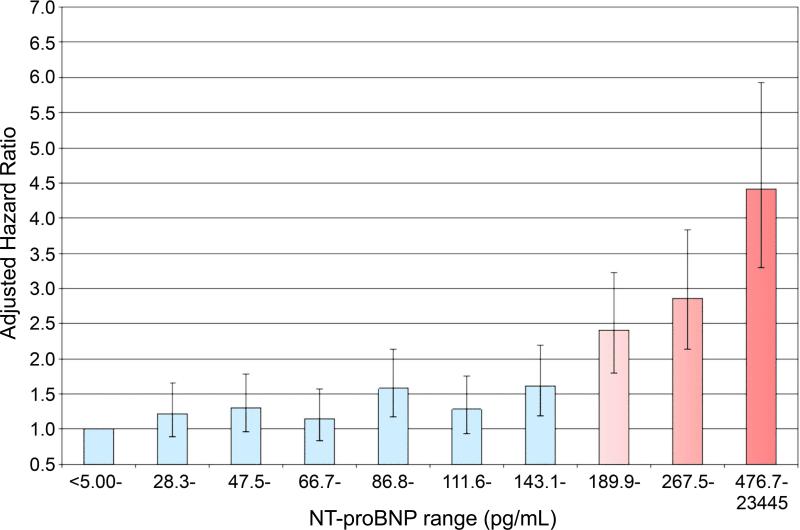
Statistical methods
Characteristics by quintile of baseline NT-proBNP were compared by Chi-square tests or one-way ANOVA as appropriate. Cumulative incidence of heart failure and cardiovascular death were estimated using the Kaplan-Meier method and compared with log-rank tests, and multivariate analyses were performed using Cox proportional hazards models. Three sets of adjustment covariates were chosen a priori among factors with an established role in predicting cardiovascular events and known or likely to influence natriuretic peptide levels : 1) “traditional” cardiovascular risk factors as defined by the Framingham risk score; (18) 2) “clinically available risk factors” – an expanded set of factors readily ascertained in a general outpatient clinical care setting (see table 2); 3) Measures of cardiac structure (LV mass by ECG, LVEF and left atrial diameter by echocardiogram). NT-proBNP was modeled as both a linear variable (after logarithmic transformation) and as quintiles. The optimal threshold of NT-proBNP for increased heart failure risk was determined by ROC analyses and by plotting the adjusted risk of heart failure for each decile of NT-proBNP; this threshold was identified at 190 pg/mL, the cut-point separating the 7th from 8th decile (figure 2). The corresponding sensitivity and specificity for incident heart failure were derived by ROC analyses.
Table 2.
Association of NT-proBNP and incident heart failure and cardiovascular mortality
| Unadjusted | Risk-Factor Adjusted* | Adjusted for clinically available factors† | |
|---|---|---|---|
| Incident heart failure | N=4,312 | N=4,292 | N=4,129 |
| 1 In-unit increment | 1.78 (1.68, 1.88) | 1.61 (1.52, 1.71) | 1.52 (1.43, 1.62) |
| Quintiles (pg/mL) | |||
| Q1 (<5.0-47.5) | Referent | Referent | Referent |
| Q2 (47.5-86.8) | 1.12 (0.91, 1.39) | 1.13 (0.91, 1.40) | 1.10 (0.89, 1.37) |
| Q3 (86.9-143.1) | 1.38 (1.13, 1.70) | 1.34 (1.08, 1.65) | 1.30 (1.05, 1.61) |
| Q4 (143.2-267.5) | 2.01 (1.65, 2.45) | 1.83 (1.48, 2.24) | 1.81 (1.46, 2.23) |
| Q5 (267.7-23445) | 4.53 (3.77, 5.46) | 3.41 (2.80, 4.18) | 3.05 (2.46, 3.78) |
| Cardiovascular mortality | |||
| 1 ln-unit increment | 1.87 (1.77, 1.98) | 1.71 (1.61, 1.82) | 1.46 (1.36, 1.57) |
| Quintiles | |||
| Q1 | Referent | Referent | Referent |
| Q2 | 1.11 (0.85, 1.44) | 1.03 (0.77, 1.39) | 1.05 (0.80, 1.36) |
| Q3 | 1.63 (1.28, 2.08) | 1.52 (1.16, 2.00) | 1.40 (1.09, 1.80) |
| Q4 | 2.39 (1.90, 3.01) | 2.16 (1.65, 2.81) | 1.91 (1.50, 2.44) |
| Q5 | 5.44 (4.38, 6.76) | 3.77 (2.91, 4.87) | 3.02 (2.36, 3.86) |
Cell values represent hazard ratios and 95% confidence intervals.
Adjusted for age, gender, race, smoking, total and HDL cholesterol, systolic blood pressure, and hypertension.
Additionally adjusted for diabetes body mass index, coronary heart disease, renal function, any major ECG abnormality, use of ACE inhibitors/angiotensin receptor blockers, beta-blockers, and diuretics; models predicting cardiovascular mortality additionally adjusted for prior stroke.
Figure 2. Hazard ratios for new onset heart failure by decile of NT-proBNP.
Demographic adjusted hazard ratios for developing new onset heart failure by decile of baseline amino terminal pro-B-type natriuretic peptide (NT-proBNP) level.
The association of change in NT-proBNP with subsequent heart failure and cardiovascular death was examined in two ways. First, change in NT-proBNP was considered as a categorical predictor. Among those with an initial NT-proBNP of <190 pg/mL, risk of heart failure and cardiovascular death were examined associated with a 1) decrease in NT-proBNP of at least 25% and 2) an increase of at least 25% to a level ≥ 190 pg/mL, compared to those with neither change. The cut-point of 190 pg/mL was derived from the deciles analysis described above, and the 25% threshold for change was based on the reported intra-individual variability in NT-proBNP in stable heart failure patients (19). Likewise, among those with a baseline NT-proBNP≥190 pg/mL, heart failure and cardiovascular death risk were examined associated with 1) a decline of at least 25% to a level <190 pg/mL, and 2) an increase of >25%, compared to those with neither change. Second, continuous changes in NT-proBNP levels were examined using residual change scores, by regressing the follow-up NT-proBNP measures on the baseline measures after logarithmic transformation, thereby correcting change in NT-proBNP for correlation between baseline and follow-up levels;(20) this change score was then entered as the predictor variable in Cox survival models. For both categorical and continuous forms of change in NT-proBNP, Cox regression models were adjusted for the elapsed time between NT-proBNP measurements, the covariates described above, and interval change in cardiovascular medications and diagnosis of coronary disease. For all Cox models, graphical and formal methods were used to test the assumption of proportional hazards.
Effect modification by coronary heart disease was examined by testing multiplicative interaction terms (6). To examine model discrimination, the C-statistic was computed for survival regression models with and without baseline NT-proBNP and interval change (21). The improvement in risk classification by addition of the change in NT-proBNP to risk-factor adjusted models with only baseline NT-proBNP was examined using the “net reclassification improvement”, which represents the net percentage of subjects correctly re-classified to risk categories (22). We categorized individuals according to model-based risk of 10-year heart failure or cardiovascular death of <10%, 10%-20%, or >20%. Statistical analysis was performed with Stata version 10 (Statacorp, College Station, TX); time-dependent C statistics were generated using R version 2.7.0.
Results
Subject Characteristics
The median NT-proBNP was 111.7 pg/mL. Participants were divided into quintiles based on initial NT-proBNP levels (table 1). Higher levels were associated with older age, female gender, Caucasian race, known coronary heart disease, a lower estimated glomerular filtration rate, a greater prevalence of major ECG abnormalities, increased left ventricular mass and decreased left ventricular ejection fraction. However, even in the highest quintile of NT-proBNP (>267.5 pg/mL) more than 80% had a normal LVEF.
Table 1.
Baseline characteristics of study population, by NT-proBNP quintile
| All | Q1 | Q2 | Q3 | Q4 | Q5 | Test for Trend | |
|---|---|---|---|---|---|---|---|
| Range (pg/mL) | <5-47.5 | 47.5-86.8 | 86.9-143.1 | 143.2-267.5 | 267.7-23445 | ||
| Age (yrs) | 72.7 (5.5) | 70.5 (4.1) | 71.1 (4.5) | 72.2 (5.0) | 73.7 (5.6) | 76.1 (6.3) | <0.001 |
| Male | 40.6% | 48.1% | 38.4% | 38.5% | 34.7% | 43.2% | 0.01 |
| African-American | 15.9% | 21.7% | 17.4% | 13.6% | 14.5% | 12.4% | <0.001 |
| CHD | 17.6% | 10.0% | 12.1% | 15.2% | 19.4% | 31.5% | <0.001 |
| Diabetes | 17.7% | 20.2% | 16.8% | 18.2% | 15.2% | 18.1% | 0.20 |
| Hypertension | 59.4% | 50.1% | 54.4% | 54.7% | 65.2% | 72.8% | <0.001 |
| Smoker | 11.1% | 12.4% | 12.5% | 9.5% | 10.8% | 10.4% | 0.02 |
| eGFR (mL/min/1.73m2) | 78.8 (22.7) | 83.7 (22.9) | 81.7 (21.6) | 79.5 (21.7) | 77.4 (23.0) | 70.1 (24.7) | <0.001 |
| BMI (kg/m2) | 26.7 (4.7) | 27.6 (4.6) | 27.1 (4.8) | 26.7 (4.7) | 26.5 (4.7) | 25.8 (4.6) | <0.001 |
| LDL-C | 3.38 (0.91) | 3.46 (0.86) | 3.48 (0.93) | 3.38 (0.90) | 3.31 (0.91) | 3.27 (0.95) | <0.001 |
| TChol | 5.49 (1.01) | 5.59 (0.96) | 5.61 (1.01) | 5.51 (1.00) | 5.42 (0.99) | 5.33 (1.07) | <0.001 |
| HDL-C | 1.41 (0.41) | 1.37 (0.39) | 1.42 (0.40) | 1.43 (0.41) | 1.44 (0.43) | 1.38 (0.41) | 0.4 |
| Medications: | |||||||
| ACEI | 6.6% | 6.2% | 6.9% | 6.0% | 6.0% | 7.8% | 0.40 |
| BB | 13.2% | 6.5% | 9.7% | 11.1% | 16.1% | 22.7% | <0.001 |
| Diuretics | 24.9% | 20.7% | 23.3% | 23.3% | 27.1% | 30.4% | <0.001 |
| Aspirin | 33.8% | 31.8% | 33.9% | 33.4% | 34.2% | 35.7% | 0.10 |
| Major ECG Abn | 28.7% | 18.4% | 18.9% | 22.7% | 30.2% | 53.7% | <0.001 |
| Systolic Function | |||||||
| Borderline | 5.2% | 4.4% | 2.7% | 4.5% | 5.0% | 9.3% | <0.001 |
| Abnormal | 2.7% | 0.2% | 0.7% | 0.8% | 2.0% | 9.7% | |
| LV mass (gm) by echo (N=2792) | |||||||
| Women | 140.2 (49.0) | 133.5 (35.4) | 130.7 (32.4) | 131.6 (35.4) | 135.0 (43.6) | 145.5 (49.2) | <0.001 |
| Men | 179.8 (54.1) | 165.9 (44.1) | 158.2 (41.3) | 170.1 (46.5) | 187.0 (56.2) | 201.8 (65.5) | <0.001 |
| Left Atrial diameter (cms) | 3.78 (0.6) | 3.79 (0.61) | 3.77 (0.59) | 3.83 (0.61) | 3.88 (0.65) | 4.14 (0.78) | <0.001 |
ACEI, Angiotenson converting enzyme inhibitor; ASA, aspirin; BB, beta blocker; BMI, body mass index; CHD, coronary heart disease; DBP, diastolic blood pressure; ECG, electrocardiogram; eGR, estimated glomerular filtration rate; LDL-C, low density lipoprotein cholesterol; LV, left ventricular; NT-proBNP, N-terminal pro B-type natriuretic peptide; SBP, systolic blood pressure; Tchol, total cholesterol
Outcomes based on the initial NT-proBNP level
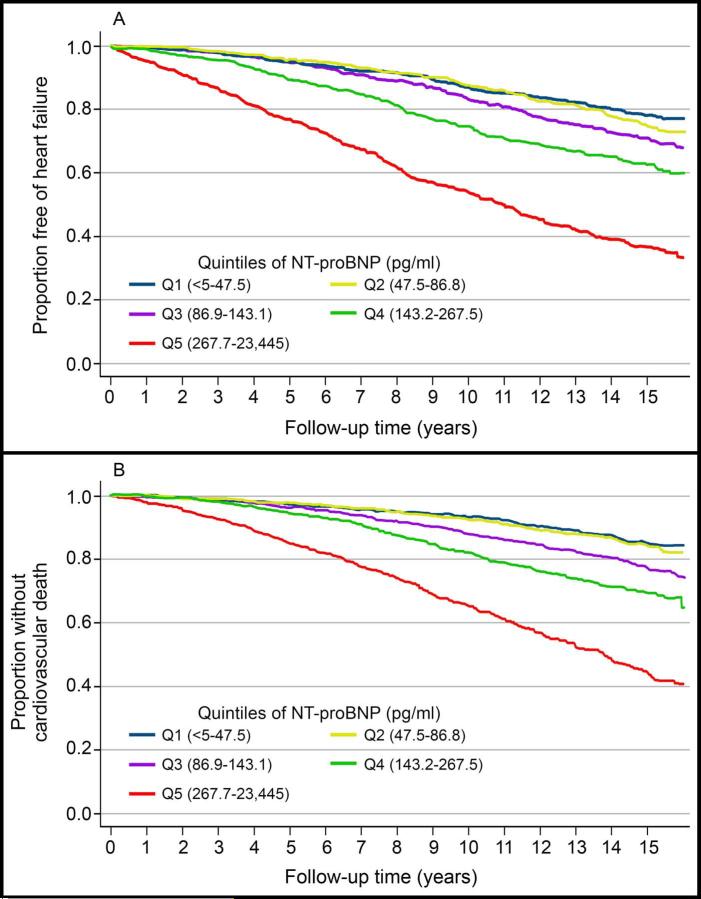
Over a median follow-up time of 11.9 years, the rates of incident heart failure and cardiovascular death were 2.6 (95% CI 2.5-2.8) and 2.1 (95%CI 1.9-2.2) per 100 person years, respectively. Time to incident heart failure and cardiovascular death by NT-proBNP quintile is shown in figure 3a and figure 3b respectively. Differentiation of risk appeared within the first year and continued throughout follow-up for both endpoints. As shown in table 2, the unadjusted risk of incident heart failure was approximately 4.5-fold higher and the risk of cardiovascular death 5.4-fold higher for subjects in the highest quintile versus the lowest quintile of NT-proBNP. After adjustment for routinely available clinical factors, the risk remained increased approximately 3-fold for both endpoints between the first and fifth quintile. With further adjustment for left ventricular mass, left atrial diameter and LVEF, hazard ratios comparing the highest to lowest quintile of NT-proBNP were 2.62 (95%CI 2.02, 3.30) for incident heart failure and 2.53 (95%CI 1.92, 3.33) for cardiovascular death. No significant or clinically important differences were observed for the effect of NT-proBNP on incident heart failure (p=0.1) or cardiovascular death (p=0.7) between those with and without prevalent coronary disease.
Figure 3. Kaplan Meier plots based on quintile of NT-proBNP.
Unadjusted Kaplan Meier plots for (A) time to new onset heart failure diagnosis and (B) time to cardiovascular death based on the quintile of the baseline visit amino terminal pro-B-type natriuretic peptide (NT-proBNP) level.
An inflection for increased risk of incident heart failure based on the adjusted hazard ratios by NT-proBNP decile was identified between the 7th and 8th deciles (figure 2). Therefore, the NT-proBNP value at the 70th percentile (190 pg/mL), was used as a cut-point to separate subjects into lower and higher risk groups. A similar inflection was seen for cardiovascular death. The associated sensitivity, specificity, positive and negative predictive value for incident heart failure during follow-up for this cut-point were 47.6%, 75.6%, 38.4% and 81.9% respectively.
Prognosis based on change in NT-proBNP level over time
Follow-up NT-proBNP samples were available in 2,975 subjects representing 85.8% of the study population that was alive, returned for an in-person follow-up visit and was without a diagnosis of heart failure in the interim (figure 1). Subjects with available sample were younger, more often male, and less often diabetic (15.6% versus 20.7%), had slightly better renal function and a lower rate of incident heart failure and cardiovascular death (supplemental table 1).
Substantial individual differences in changes of NT-proBNP were observed during follow-up. Of subjects with baseline NT-proBNP levels < 190 pg/mL, 468 (21%) had a change of > 25% and to a level ≥ 190pg/mL and 357 (16%) of subjects had a >25% decrease on the second sample measurement. For subjects with initial levels ≥ 190 pg/mL at baseline, 112 (15%) had a > 25% decrease to < 190 pg/mL and 293 (40%) had a > 25% increase on the second sample measurement. Characteristics of participants with respect to change in NT-proBNP levels are shown in table 3.
Table 3.
Characteristics of participants at follow-up NT-proBNP measure, by interval change in NT-proBNP
| Baseline <190 pg/mL (N=2,243) | ||||
|---|---|---|---|---|
| >25% Decrease | No significant increase | Increase >25% and >190 pg/mL | Test For Trend | |
| N=357 (16%) | N=1,418 (63%) | N=468 (21%) | ||
| Age (years) | 73.1 (4.0) | 73.6 (4.3) | 75.7 (5.0) | <0.001 |
| Male | 141 (39.5%) | 552 (38.9%) | 184 (39.2%) | 0.98 |
| African-American | 70 (19.6%) | 263 (18.6%) | 42 (9.0%) | <.001 |
| Diabetes | 74 (20.7%) | 237 (16.7%) | 56 (12.0%) | <.001 |
| Coronary heart disease | 41 (11.5%) | 198 (14.0%) | 124 (26.5%) | <.001 |
| Hypertension | 158 (44.4%) | 767 (54.2%) | 288 (61.5%) | <.001 |
| Major ECG abnormality | 55 (21.0%) | 241 (22.8%) | 152 (42.7%) | <.001 |
| BMI (kg/m2) | 27.7 (4.6) | 27.1 (4.5) | 26.3 (4.7) | <.001 |
| eGFR (cc/min/1.73m2) | 71.0 (15.9) | 70.1 (15.3) | 65.7 (16.0) | <.001 |
| Baseline NT-proBNP | 89.1 [59.6, 127.6] | 60.8 [33.1, 93.9] | 116.1 [75.9, 148.6] | <.001 |
| ACEI/ARB | 43 (12.0%) | 113 (8.0%) | 52 (11.1%) | 0.9 |
| Beta blocker | 23 (6.4%) | 133 (9.4%) | 85 (18.2%) | <.001 |
| Baseline ≥190 pg/mL (N=732) | ||||
|---|---|---|---|---|
| Decrease >25% and <190 pg/mL | No significant decrease | >25% Increase | Test for trend | |
| N=112 (15%) | N=327 (45%) | N=293 (40%) | ||
| Age (years) | 75.1 (5.0) | 76.6 (5.6) | 78.4 (6.1) | <.001 |
| Male | 32 (28.6%) | 101 (30.9%) | 122 (41.6%) | .003 |
| African-American | 23 (20.5%) | 36 (11.0%) | 27 (9.2%) | .005 |
| Diabetes | 18 (16.1%) | 32 (9.8%) | 46 (15.7%) | 0.51 |
| Coronary heart disease | 24 (21.4%) | 86 (26.3%) | 107 (36.5%) | <.001 |
| Hypertension | 78 (69.6%) | 215 (65.8%) | 193 (66.1%) | 0.6 |
| Major ECG abnormality | 25 (28.1%) | 98 (40.0%) | 100 (53.5%) | <.001 |
| BMI (kg/m2) | 27.7 (5.6) | 25.8 (4.6%) | 25.9 (4.6) | .007 |
| eGFR (cc/min/1.73m2) | 66.3 (15.0) | 63.0 (16.7) | 58.7 (17.0) | <.001 |
| Baseline NT-proBNP | 251.7 [216.6, 302.4] | 366.5 [247.7, 595.3] | 300.6 [237.5, 474.5] | .007 |
| ACEI/ARB | 15 (13.4%) | 38 (11.6%) | 31 (10.6%) | 0.4 |
| Beta blocker | 18 (16.1%) | 51 (15.6%) | 65 (22.2%) | .06 |
ARB, angiotensin receptor blocker; other abbreviations as in Table 1
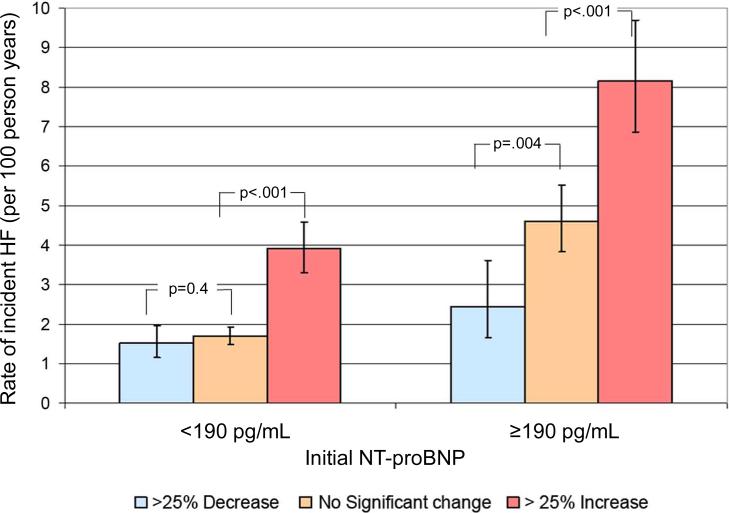
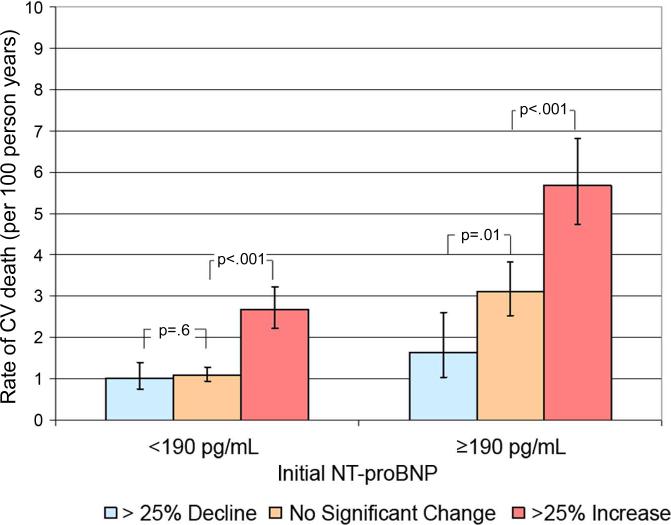
Incident rates for new onset heart failure and cardiovascular death based on change from baseline levels are shown in figure 4a and 4b. Subjects with initially low levels of NT-proBNP whose level increased at follow-up had higher rates of incident heart failure and cardiovascular death compared to subjects whose NT-proBNP level remained low and unchanged (p values<0.001), In contrast, subjects with initially low levels of NT-proBNP whose level decreased > 25% had no significant difference in outcomes compared to subjects whose NT-proBNP level remained low (figure 4 and table 4a). Subjects with initial NT-proBNP levels ≥ 190 pg/mL and who displayed a > 25% increase had a higher incidence of heart failure and cardiovascular death during follow-up compared to subjects with initially high levels that remained high but unchanged. In contrast, subjects with initial levels of NT-proBNP ≥ 190 pg/mL whose level decreased > 25% had a significantly lower incidence of both outcomes compared to subjects whose NT-proBNP level remained high and unchanged (figure 4 and table 4b). Furthermore, a “signal” for increased risk of incident heart failure with a > 25% rise in NT-proBNP level could be seen in subjects with baseline values as low as the second quintile (median baseline concentration 59.2 pg/mL, median increase 70.5. pg/mL, unadjusted HR=2.70, 95%CI 1.52-4.83). Tests of effect modification by prevalent coronary heart disease revealed no significant interactions (p>0.1). Utilizing residual change scores, baseline-corrected changes in NT-proBNP remained significantly predictive for incident heart failure and cardiovascular death after adjusting for covariates (supplemental table 2).
Figure 4. Incident rates for cardiovascular outcomes based on change of NT-proBNP level.
Incident rates for (A) new onset heart failure (HF) and (B) cardiovascular (CV) death based on change or absence of change between baseline and follow-up amino terminal pro-B-type natriuretic peptide (NT-proBNP) levels. Change in NT-proBNP level is defined among those with a baseline NT-proBNP <190 pg/mL as either a decrease in NT-proBNP of at least 25% or an increase of at least 25% to a level ≥ 190 pg/mL. Change in NT-proBNP level is defined among those with a baseline NT-proBNP ≥190 pg/mL as either a decline of at least 25% to a level <190 pg/mL or an increase of >25%.
Table 4a.
Association of clinically significant increase* in NT-proBNP and outcomes among those free of heart failure and with baseline NT-proBNP<190 pg/mL.
| Interval Change in NT-proBNP | Unadjusted | Traditional Risk Factors* | Clinically Available risk factors† | |
|---|---|---|---|---|
| Incident HF (439 events) | ||||
| >25% Decrease | 0.89 (0.67, 1.19) | 1.00 (0.74, 1.35) | 0.83 (0.60, 1.13) | |
| No Changea | Reference | Reference | Reference | |
| >25% Increase to ≥190 pg/mL | 2.41 (1.96, 2.96) | 2.10 (1.69, 2.62) | 2.13 (1.68, 2.71) | |
| CV death (315 events) | ||||
| >25% Decrease | 0.92 (0.65, 1.30) | 0.99 (0.69, 1.40) | 0.86 (0.59, 1.24) | |
| No Change | Reference | Reference | Reference | |
| >25% Increase to ≥190 pg/mL | 2.55 (2.01, 3.23) | 2.06 (1.60, 2.66) | 1.91 (1.43, 2.53) |
Table 4b.
Association of clinically significant changes in NT-proBNP and outcomes among those free of heart failure and with baseline NT-proBNP≥190 pg/mL.
| Unadjusted (N=733) | Traditional Risk Factors* | Clinically available risk factors† | ||
|---|---|---|---|---|
| Incident HF (271 events) | ||||
| >25% Decrease to <190 pg/mL | 0.53 (0.34, 0.81) | 0.51 (0.32, 0.79) | 0.58 (0.36, 0.93) | |
| <25% Change | Reference | Reference | Reference | |
| >25% Increase | 1.83 (1.42, 2.36) | 1.68 (1.30, 2.17) | 2.06 (1.56, 2.72) | |
| CV death (224 Events) | ||||
| >25% Decrease to <190 pg/mL | 0.51 (0.31, 0.85) | 0.49 (0.29, 0.84) | 0.57 (0.32, 1.01) | |
| <25% Change | Reference | Reference | Reference | |
| >25% Increase | 1.94 (1.47, 2.55) | 1.77 (1.33, 2.35) | 1.88 (1.37, 2.57) |
CV, cardiovascular; HF, heart failure; NT-proBNP, N-terminal pro B-type natriuretic peptide
Cell values represent hazard ratios and 95% confidence intervals.
Age, gender, race, smoking, hypertension, systolic BP, total and HDL cholesterol.
Additionally adjusted for baseline NT-proBNP, renal function, body mass index, diabetes, coronary heart disease (none, prevalent at baseline, or incident during interval between NT-proBNP measures), and for use of ACE inhibitor/angiotensin receptor blocker and beta blockers [both prevalent and interval use]). Models predicting cardiovascular mortality additionally adjusted for prior stroke.
Improvement in Prognostic Accuracy and Reclassification
The area under the ROC curves were calculated adjusting for demographic and cardiovascular risk factors (table 5). Demographic and cardiovascular risk factors were highly predictive of incident heart failure and cardiovascular death. Addition of baseline and follow-up NT-proBNP increased predictive accuracy significantly (p values<0.05) for both outcomes (heart failure area under the curve = 0.80, cardiovascular death area under the curve = 0.81). Model discrimination as measured by net reclassification improvement was also improved 4.5%-7.9% by the addition of change in NT-proBNP (supplemental table 3), compared to traditional risk-factor adjusted models containing baseline NT-proBNP only.
Table 5.
Area under the Receiver-Operating Curve (AUC) of consecutively more complex models predicting heart failure and cardiovascular death
| Model | AUC | |
|---|---|---|
| Incident heart failure | Cardiovascular death | |
| Demographic | 0.66 | 0.71 |
| + Co-morbidity * | 0.75† | 0.77† |
| + Baseline NT-proBNP | 0.78† | 0.79 |
| + Follow-up NT-proBNP | 0.80† | 0.81† |
NT-proBNP, N-terminal pro B-type natriuretic peptide
Similar variables to second model in table 2
p<0.05 comparing AUC to more simple nested model in previous row
Discussion
Independent of age, traditional cardiovascular risk factors, ECG and echocardiographic abnormalities, an elevated NT-proBNP level is a long-term predictor of new onset heart failure and cardiovascular death in community-dwelling individuals aged 65 and older. Furthermore, NT-proBNP levels frequently are dynamic over time, conferring a change in risk for subsequent cardiac events concordant with the direction of change of the biomarker. NT-proBNP measurement may be particularly well suited to an elderly population with highly prevalent cardiovascular risk factors.
Assessment of risk for cardiovascular events can be particularly challenging in the elderly with less accuracy associated with composite risk scores of traditional cardiovascular risk factors, including the Framingham risk score, and absent or attenuated risk prediction with the use of established biomarkers such as lipid levels and C-reactive protein compared to the general population (3,6,23,24). In contrast, a natriuretic peptide level may reflect the contributions of multiple cardiac pathologies including ischemia, fibrosis and hypertrophy in addition to hemodynamic stress, such that these biomarkers reflect the overall burden of clinical and subclinical cardiovascular disease (25).
Two prior studies have shown single measurements of NT-proBNP to independently predict outcomes in the elderly (6,9). In the first study, NT-proBNP was a significant prognostic factor of cardiovascular events only in subjects with known coronary heart disease (6). In contrast, NT-proBNP predicted cardiovascular-related mortality among older Swedish men of similar age, including those without coronary heart disease, when combined with markers of inflammation, renal function and myocardial necrosis (9). The present results expand on these prior reports by demonstrating the ability of NT-proBNP to predict both incident heart failure and cardiovascular death in a geographically and racially diverse cohort of men and women regardless of co-morbidity and independent of age, as well as echocardiographic and ECG measures of subclinical heart disease.
We also identify for the first time in a community-dwelling general population that NT-proBNP levels are dynamic and that fluctuation reflects a change in risk for subsequent cardiovascular events independent of baseline level and co-morbidity. The concept that fluctuations in natriuretic peptide levels outside acute hospitalizations reflect a change in the level of risk has been studied previously in two symptomatic patient populations including those with acute coronary syndrome presentations and those with chronic stable heart failure (26,27). Progression of levels over time may reflect the trajectory of progression of subclinical cardiovascular disease. Even at levels within the normal range, an increased NT-proBNP level corresponds with increased risk. We also observed decreases in levels are common and in participants with initial levels ≥ 190 pg/mL this reflects a significant decrease in risk of incident heart failure or cardiovascular death. This may reflect differences in cardiac pathology leading to the initial elevation.
The present findings indicate the dynamic nature of cardiovascular risk in the elderly and raise the possibility that specific interventions could delay progression to symptomatic heart failure or cardiovascular death. Prior studies targeting hypertension and sedentary lifestyle have shown success in reducing cardiovascular mortality in the elderly (28,29). Strategies particularly targeting patients identified as higher risk with initially high levels or those that progressively rise may warrant testing. Early identification of risk in the subclinical phase of cardiovascular disease may be particularly critical in the elderly as progression to symptomatic heart failure with associated elevated NT-proBNP levels may be more resistant to therapy and strategies designed to lower NT-proBNP compared to younger individuals (30). Our analyses suggest that – in older adults free of HF – a strategy of serial NT-proBNP testing would correctly risk-stratify an additional 4.5%-8% of individuals compared to a single NT-proBNP measurement alone.
Study limitations
Samples were available in approximately three-fourths of the cohort at baseline, with one quarter of these having no available sera for follow-up measures. Subjects with a blood sample at follow-up compared to those without a sample were younger and had a lower prevalence of clinical risk-factors. The differential absence of NT-proBNP measures may have introduced bias into the estimates of associations with heart failure and cardiovascular death. The duration of follow-up is a strength of this study, but cardiovascular therapy has changed over time and it is possible that more ubiquitous use of medications such as statins could have blunted the predictive value of the NT-proBNP level. Since lipid levels were not independently predictive of outcome in this population this effect is likely modest (24,31). These limitations are largely offset by the representative nature of the CHS cohort and the high levels of incident heart failure. The length of follow-up and high event rate allowed for a robust multivariate analysis and the ability to analyze the significance of change in NT-proBNP levels over longer periods of time than done previously in populations with symptomatic cardiovascular disease (26,27). Lastly, we measured NT-proBNP in samples nearly 20 years in age. Given the relative recent introduction of this assay we can't determine with certainty, through repeated measures, the stability of the samples. However, stability has been confirmed by repeated measures as far apart as two years making sample stability less likely to be an important explanation for between sample differences in NT-proBNP measurements (32). Our choice of a >25% change in NT-proBNP over time was initial based on short-term intra-individual variability in NT-proBNP in stable heart failure patients. One small study of stable HF patients confirms one-year intra-individual variability is also approximately 25% in HF patients with initially low NT-proBNP levels (33).
Conclusions
NT-proBNP level is a long-term predictor of new-onset heart failure and cardiovascular death in community dwelling elderly. Furthermore, NT-proBNP levels frequently change substantially over 2-3 years. This change in level reflects a significant change in patient risk independent of cardiovascular risk factors, ejection fraction, or medication use. Ultimately, NT-proBNP levels may guide further diagnostic testing or potential preventive measures to reduce the risk of developing heart failure or dying of cardiovascular disease.
Supplementary Material
Acknowledgments
The research reported in this article was supported by contract numbers N01-HC-85079 through N01-HC-85086, N01-HC-35129, N01 HC-15103, N01 HC-55222, N01-HC-75150, N01-HC-45133, grant number U01 HL080295 from the National Heart, Lung, and Blood Institute, with additional contribution from the National Institute of Neurological Disorders and Stroke. Additional support was provided through R01 AG-15928, R01 AG-20098, and AG-027058 from the National Institute on Aging, R01 HL-075366 from the National Heart, Lung and Blood Institute, and the University of Pittsburgh Claude. D. Pepper Older Americans Independence Center P30-AG-024827. A full list of principal CHS investigators and institutions can be found at http://www.chs-nhlbi.org/pi.htm. Additional funding was provided by Roche Diagnostics
Abbreviations and Acronyms
- BNP
B-type natriuretic peptide
- CHS
Cardiovascular Health Study
- CI
Confidence interval
- ECG
Electrocardiogram
- LV
Left ventricle
- LVEF
Left ventricular ejection fraction
- NT-proBNP
N-terminal pro B-type natriuretic peptide
- ROC
Receiver operator characteristic
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures:
Dr. deFilippi receives research grant support (>10k) and honorarium/consulting fees (>10k) from Siemens, Roche Diagnostics, BG medicine, and Critical Diagnostics.
Dr. Christenson reports that funding from Roche Diagnostics was supplied for NT-proBMP testing. Siemens Healthcare Diagnostics and Response Biomedical have supported research efforts and market NT-proBNP assays.
Dr. Seliger reports having received a research grant from Roche, Inc.
Drs. Gottdiener and Kop: No disclosures.
References
- 1.Schocken DD, Arrieta MI, Leaverton PE, Ross EA. Prevalence and mortality rate of congestive heart failure in the United States. J Am Coll Cardiol. 1992;20:301–6. doi: 10.1016/0735-1097(92)90094-4. [DOI] [PubMed] [Google Scholar]
- 2.Rosamond W, Flegal K, Friday G, et al. Heart disease and stroke statistics--2007 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2007;115:e69–171. doi: 10.1161/CIRCULATIONAHA.106.179918. [DOI] [PubMed] [Google Scholar]
- 3.D'Agostino RB, Sr., Grundy S, Sullivan LM, Wilson P. Validation of the Framingham coronary heart disease prediction scores: results of a multiple ethnic groups investigation. Jama. 2001;286:180–7. doi: 10.1001/jama.286.2.180. [DOI] [PubMed] [Google Scholar]
- 4.Kuller LH, Arnold AM, Psaty BM, et al. 10-year follow-up of subclinical cardiovascular disease and risk of coronary heart disease in the Cardiovascular Health Study. Arch Intern Med. 2006;166:71–8. doi: 10.1001/archinte.166.1.71. [DOI] [PubMed] [Google Scholar]
- 5.McKie PM, Rodeheffer RJ, Cataliotti A, et al. Amino-terminal pro-B-type natriuretic peptide and B-type natriuretic peptide: biomarkers for mortality in a large community-based cohort free of heart failure. Hypertension. 2006;47:874–80. doi: 10.1161/01.HYP.0000216794.24161.8c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kistorp C, Raymond I, Pedersen F, Gustafsson F, Faber J, Hildebrandt P. N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. Jama. 2005;293:1609–16. doi: 10.1001/jama.293.13.1609. [DOI] [PubMed] [Google Scholar]
- 7.Olsen MH, Hansen TW, Christensen MK, et al. N-terminal pro-brain natriuretic peptide, but not high sensitivity C-reactive protein, improves cardiovascular risk prediction in the general population. Eur Heart J. 2007;28:1374–81. doi: 10.1093/eurheartj/ehl448. [DOI] [PubMed] [Google Scholar]
- 8.Wang TJ, Larson MG, Levy D, et al. Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med. 2004;350:655–63. doi: 10.1056/NEJMoa031994. [DOI] [PubMed] [Google Scholar]
- 9.Zethelius B, Berglund L, Sundstrom J, et al. Use of multiple biomarkers to improve the prediction of death from cardiovascular causes. N Engl J Med. 2008;358:2107–16. doi: 10.1056/NEJMoa0707064. [DOI] [PubMed] [Google Scholar]
- 10.Wang TJ, Gona P, Larson MG, et al. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006;355:2631–9. doi: 10.1056/NEJMoa055373. [DOI] [PubMed] [Google Scholar]
- 11.Fried LP, Borhani NO, Enright P, et al. The Cardiovascular Health Study: design and rationale. Ann Epidemiol. 1991;1:263–76. doi: 10.1016/1047-2797(91)90005-w. [DOI] [PubMed] [Google Scholar]
- 12.Psaty BM, Kuller LH, Bild D, et al. Methods of assessing prevalent cardiovascular disease in the Cardiovascular Health Study. Ann Epidemiol. 1995;5:270–7. doi: 10.1016/1047-2797(94)00092-8. [DOI] [PubMed] [Google Scholar]
- 13.Ordonez-Llanos J, Collinson PO, Christenson RH. Amino-terminal pro-B-type natriuretic peptide: analytic considerations. Am J Cardiol. 2008;101:9–15. doi: 10.1016/j.amjcard.2007.11.013. [DOI] [PubMed] [Google Scholar]
- 14.Ives DG, Fitzpatrick AL, Bild DE, et al. Surveillance and ascertainment of cardiovascular events. The Cardiovascular Health Study. Ann Epidemiol. 1995;5:278–85. doi: 10.1016/1047-2797(94)00093-9. [DOI] [PubMed] [Google Scholar]
- 15.Rautaharju PM, Manolio TA, Siscovick D, et al. Utility of new electrocardiographic models for left ventricular mass in older adults. The Cardiovascular Health Study Collaborative Research Group. Hypertension. 1996;28:8–15. doi: 10.1161/01.hyp.28.1.8. [DOI] [PubMed] [Google Scholar]
- 16.Furberg CD, Manolio TA, Psaty BM, et al. Major electrocardiographic abnormalities in persons aged 65 years and older (the Cardiovascular Health Study). Cardiovascular Health Study Collaborative Research Group. Am J Cardiol. 1992;69:1329–35. doi: 10.1016/0002-9149(92)91231-r. [DOI] [PubMed] [Google Scholar]
- 17.Gottdiener JS, Arnold AM, Aurigemma GP, et al. Predictors of congestive heart failure in the elderly: the Cardiovascular Health Study. J Am Coll Cardiol. 2000;35:1628–37. doi: 10.1016/s0735-1097(00)00582-9. [DOI] [PubMed] [Google Scholar]
- 18.Third report of the expert panal on detection, evalaution, and treatment of high blood cholesterol in adults (Adult Treatment Panel III); Risk Assessment Tool for Estimating Your 10-year Risk of Having a Heart Attack. 2009.
- 19.Schou M, Gustafsson F, Nielsen PH, Madsen LH, Kjaer A, Hildebrandt PR. Unexplained week-to-week variation in BNP and NT-proBNP is low in chronic heart failure patients during steady state. Eur J Heart Fail. 2007;9:68–74. doi: 10.1016/j.ejheart.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 20.Krantz DS, Kop WJ, Gabbay FH, et al. Circadian variation of ambulatory myocardial ischemia. Triggering by daily activities and evidence for an endogenous circadian component. Circulation. 1996;93:1364–71. doi: 10.1161/01.cir.93.7.1364. [DOI] [PubMed] [Google Scholar]
- 21.Heagerty PJ, Lumley T, Pepe MS. Time-dependent ROC curves for censored survival data and a diagnostic marker. Biometrics. 2000;56:337–44. doi: 10.1111/j.0006-341x.2000.00337.x. [DOI] [PubMed] [Google Scholar]
- 22.Pencina MJ, D'Agostino RB, Sr., D'Agostino RB, Jr., Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. doi: 10.1002/sim.2929. discussion 207-12. [DOI] [PubMed] [Google Scholar]
- 23.Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;347:1557–65. doi: 10.1056/NEJMoa021993. [DOI] [PubMed] [Google Scholar]
- 24.Shlipak MG, Fried LF, Cushman M, et al. Cardiovascular mortality risk in chronic kidney disease: comparison of traditional and novel risk factors. Jama. 2005;293:1737–45. doi: 10.1001/jama.293.14.1737. [DOI] [PubMed] [Google Scholar]
- 25.Konstam MA. Natriuretic peptides and cardiovascular events: more than a stretch. Jama. 2007;297:212–4. doi: 10.1001/jama.297.2.212. [DOI] [PubMed] [Google Scholar]
- 26.Morrow DA, de Lemos JA, Blazing MA, et al. Prognostic value of serial B-type natriuretic peptide testing during follow-up of patients with unstable coronary artery disease. Jama. 2005;294:2866–71. doi: 10.1001/jama.294.22.2866. [DOI] [PubMed] [Google Scholar]
- 27.Anand IS, Fisher LD, Chiang YT, et al. Changes in brain natriuretic peptide and norepinephrine over time and mortality and morbidity in the Valsartan Heart Failure Trial (Val-HeFT). Circulation. 2003;107:1278–83. doi: 10.1161/01.cir.0000054164.99881.00. [DOI] [PubMed] [Google Scholar]
- 28.Gregg EW, Cauley JA, Stone K, et al. Relationship of changes in physical activity and mortality among older women. Jama. 2003;289:2379–86. doi: 10.1001/jama.289.18.2379. [DOI] [PubMed] [Google Scholar]
- 29.Schocken DD, Benjamin EJ, Fonarow GC, et al. Prevention of heart failure: a scientific statement from the American Heart Association Councils on Epidemiology and Prevention, Clinical Cardiology, Cardiovascular Nursing, and High Blood Pressure Research; Quality of Care and Outcomes Research Interdisciplinary Working Group; and Functional Genomics and Translational Biology Interdisciplinary Working Group. Circulation. 2008;117:2544–65. doi: 10.1161/CIRCULATIONAHA.107.188965. [DOI] [PubMed] [Google Scholar]
- 30.Pfisterer M, Buser P, Rickli H, et al. BNP-guided vs symptom-guided heart failure therapy: the Trial of Intensified vs Standard Medical Therapy in Elderly Patients With Congestive Heart Failure (TIME-CHF) randomized trial. Jama. 2009;301:383–92. doi: 10.1001/jama.2009.2. [DOI] [PubMed] [Google Scholar]
- 31.Fried LP, Kronmal RA, Newman AB, et al. Risk factors for 5-year mortality in older adults: the Cardiovascular Health Study. Jama. 1998;279:585–92. doi: 10.1001/jama.279.8.585. [DOI] [PubMed] [Google Scholar]
- 32.Cauliez B, Guignery J, Marinier S, Mariau I, Lavoinne A. Two-year stability of NT-proBNP in frozen samples using the Roche Elecsys system. Ann Clin Biochem. 2008;45:318–9. doi: 10.1258/acb.2007.007187. [DOI] [PubMed] [Google Scholar]
- 33.Schou M, Gustafsson F, Kjaer A, Hildebrandt PR. Long-term clinical variation of NT-proBNP in stable chronic heart failure patients. Eur Heart J. 2007;28:177–182. doi: 10.1093/eurheartj/ehl449. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.