Abstract
Objective
Intractable anemia, such as aplastic anemia or that presumably associated with chronic herpes virus infections, sometimes require bone marrow transplant. We investigated the use of traditional Chinese medicine (TCM) for the treatment of intractable anemia.
Method
Placenta Hominis (PH), steam boiled and roasted, and Cervi Cornus Colla (deer antler glue) has been used in China for hundreds of years to treat anemia. After consent was obtained, we prescribed these two materials for a 74-year-old female with aplastic anemia and a 26-year-old male with presumably a virus-induced anemia. Concomitant conventional therapy was continued in both patients as prescribed by their respective attending physicians.
Conclusion
Conventional therapy with steroid hormones, immunosuppressive drugs, platelet and erythrocyte transfusions were not effective in these patients. In addition, both patients suffered from serious side effects. In two patients, ingestion of Placenta Hominis and Cervi Cornus Colla with TCM prescriptions increased the platelet and enhanced the hemoglobin concentration in several months of therapy accompanied by a dramatic improvement in quality of life. The addition to conventional therapy of PH and Cervi Cornus Colla, the latter of which is very easy to obtain, may be one of the potentially advantageous choices in case of otherwise intractable anemia.
Keywords: placenta, antler glue, Cervi Cornus Colla, anemia, aplastic anemia
Introduction
Patients with aplastic anemia manifest the symptoms of both anemia and thrombocytopenia. In aplastic anemia, pluripotent stem cells are dysfunctional and fail to produce a full range of blood cells. This results in varying degrees of pancytopenia with hypocellular bone marrow. The cause is often idiopathic, and the treatments include bone marrow transplantation, immunosuppressive therapy, and supportive therapy, such as blood and platelet transfusions and hematopoietic growth factors. For hundreds of years in China, Placenta Hominis (PH; ‘ze he che’ in Chinese) has been used to tonify or regulate the “blood” and also tonify the “essence”, in addition to warming “kidney”.1
The clinical disease of anemia, in traditional Chinese medicine (TCM) principles, can be understood to be a deficiency in “blood and essence”. These TCM theories are hypotheses based on accumulated experiences in diagnosis and treatment and are not yet proven by Western medicine.
We hypothesized that PH would work for anemia and applied for intractable anemia.
In this paper, one 74-year-old female with acquired aplastic anemia and one 26-yearold male with severe anemia and thrombocytopenia who were diagnosed at other hospitals and did not respond to conventional therapy. They were treated with TCM prescriptions. These included Placenta Hominis and Cervi Cornus Colla (Deer Antler Glue; ‘lu jiao jiao’ in Chinese). They responded with notable improvement in blood examination paramaters and quality of life (QOL).
Materials and methods
In China, after complete lavage by traditional methods, PH2–4 is washed thoroughly, steam-sterilized, and roasted before being sold on the market. We imported PH from Jin Mi Lan You Xian Gongsi ( ; 49–51, Bonham, Strand West, 12/F, Bld. C-D, Hong Kong). PH was ground into powder before adding it to a filtered decoction right after filtration when the temperature was still near 100 °C. The mixture was ingested after it had cooled to room temperature.
; 49–51, Bonham, Strand West, 12/F, Bld. C-D, Hong Kong). PH was ground into powder before adding it to a filtered decoction right after filtration when the temperature was still near 100 °C. The mixture was ingested after it had cooled to room temperature.
To make sure the powder was not harmful, the author (YH) took 2 g/day for three days, 3 g/day for next three days, and then continued an intake of 4 g/day for three days. Fortunately, YH had no trouble but rather felt increased vitality. Her mother also desired to take it because of her continuing cough. She took 3 g/day for five days which was when her cough stopped without any troubles.
Conventional therapy, such as immunosuppressive drugs and prednisolone, was continued in conjunction with TCM treatment, including PH and animal materials with the consent of the patients.
The prescriptions for Case 1, a 74-year-old female, are shown in Tables 1 and 2. As shown in Figures 1 and 2, the patient had been taking a photosensitizer dye for two years. Cyclosporine and prednisolone were also being taken before the TCM treatment was initiated. Granulocyte colony stimulating factor (G-CSF) was transfused about once every two weeks to prevent the white blood cell (WBC) levels from decreasing below the appropriate limit.
Table 1.
Prescription A (modified gui pi tang) for case 1
| Main functions* | Herbs (g/day) | |
|---|---|---|
| Tonify Qi | Spleen, lung | Gingseng Radix (Ren shen) 3 |
| Spleen, lung | Codonopsitis Pilosulae Radix (Dang shen) 3 | |
| Kidney, spleen | Discoreae Oppositae Radix (Shan yao) 3 | |
| Heart | Roasted Glycyrrhizae Radix (Zhi gang cao) 3 | |
| Lung, spleen | Astragau Radix (Huang qi) 5 | |
| Tonify blood | Warm and tonify Kidney | Hominis Placenta (Zi he che) 4 |
| Angelicae Radix (Dang gui) 3 | ||
| Euphoria longan (Long yan rou) 3 | ||
| Expel cold | Warm interior | Roasted Aconiti Tuber (Pao fu zi) 3 |
| Warm middle | Zingiber officinale (Gan jiang) 2 | |
| Hemostasis | Artemisia argyi (Ai ye) 2 | |
| Invigorate blood | Curcuma longa (Yu jin) 2 | |
| Notoginseng Radix (San qi) 2 | ||
| Tonify vital essence | Ganoderma lucidum (Ling zhi) | |
| Dry dampness, expel phlegm | Polia (Fu ling) 3 | |
| Rhizoma Atractylodis (Cang zhu) 4 |
Notes: Numerals indicate intake (g/day).
Theoretical main functions. In parenthesis Chinese pronunciation is described in pinyin.
Table 2.
Added herbs in sequence to Prescription A
| Main functionsa | Herbs (g/day) | |
|---|---|---|
| B | Regulate Qi, improve the transport function of the spleen |
Citrus Reticulata (Chen pi) 3 Citrus Aurantium (Zhi shi) 3 |
| C | Spread liver Qi Raise yang, clean heat, detoxify Promote the movement of Qi Tonify blood, prevent promotion to carcinogenesis |
Bupleuri Radix (Chai hu) 1 Cimicifuga Foetida (Sheng ma) 1 Magnolia officinalis (Hou po) 2 Tabebuia Avellanedae 2 |
| D | Break up blood stasis Invigorate blood, remove stasis Prevent night sweat |
Prunus Persica (Tau ren) 3 Ligustici chuanxiong Rhizoma (Chuan xiong) 2 Ostreae Testa (Mu li) 3 |
| E | Nourish and tonify essence and blood, tonify yang | Gelatinum Cervi Cornu (Lu jiao jiao)3 |
| F | Improve hyperlipidemia | Tinospora Tuberculata 6T/dayb |
Notes: Numerals indicate intake (g/day)
Theoretical main functions.
One tablet contain 0.125 g of dried herb. In parentheses Chinese pronunciation is described in pinyin.
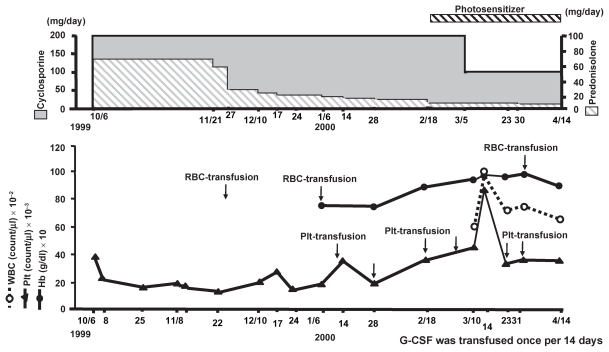
Figure 1.
Changes of Hb and Plt during hospitalization.
Abbreviations: G-CSF, granulocyte colony-stimulating factor; Hb, hemoglobin; Plt, platelet; RBC, red blood cell; WBC, white blood cells.
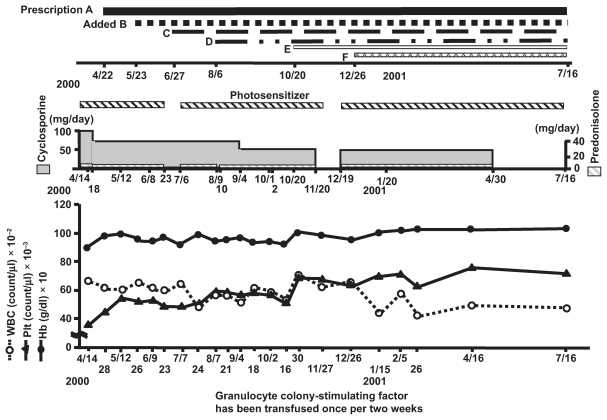
Figure 2.
Changes of Hb, Plt and WBC after starting TCM therapy.
Abbreviations: Hb, hemoglobin; Plt, platelet; TCM, traditional Chinese medicine; WBC, white blood cells.
The change in the hemoglobin (Hb) concentration and platelet (Plt) count before TCM treatment is shown in Figure 1.
For Case 2, the starting formula is provided in Table 3. This included Radix Sanguisorbae Officinalis5 (di yu) 3 g/day and Flos Sophorae Japonicae5 (huai hua) 3 g/day from March 31st to April 28th 1999 to stop bleeding. The second formula (prescription 1) is shown in Table 4. Along with this formula, PH (zi he che) 4 g/day and Notoginseng Radix6 (san qi) 2 g/day were taken as well. The details are shown in Figure 3.
Table 3.
Modified bu zhong yi qi tang (MBZYQT)a
| Main functionsb | Herbs | |
|---|---|---|
| Tonify Qi | Lung, spleen | Astragau Radix (Huang qi) |
| Spleen, lung | Gingseng Radix (Ren shen) | |
| Spleen | Atractylodes Macrocephala (bai zhu) | |
| Heart, spleen | ||
| Roasted Glycyrrhizae Radix (Zhi gang cao) | ||
| Zizyphi Fructus (da zao) | ||
| Regulate Qi, improve the transport function of the spleen | Citrus Reticulata (Chen pi) | |
| Spread liver Qi | Bupleuri Radix (chai hu) | |
| Tonify blood | Angelicae Radix (dang gui) | |
| Rehmanniae Radix | ||
| Glutinosae (shu di huang) | ||
| Paeoniae Radix (bai shao) | ||
| Tonify yin | Lung, stomach | Tuber Ophiopogonis (mai men dong) |
| Herba Dendrobii (shi hu) | ||
| Warm lung | Asiasari Radice (xi xin) | |
| Disperse cold | Magnoliae Flos (xin yi) | |
| Disperse cold | Cinnamoni Cortex (rou gui) | |
| Roasted Aconiti Tuber (pao fu zi) |
Table 4.
Prescription 1
| Main functions | Herbs (g/day) | |
|---|---|---|
| Tonify Qi | Spleen, lung | Gingseng Radix (Ren shen) 3 |
| Spleen, lung | Codonopsitis Pilosulae Radix (Dang shen) 3 | |
| Kidney, spleen | Discoreae Oppositae Radix (Shan yao) 3 | |
| Heart, spleen | Roasted Blycyrrhizae Radix (Zhi gang cao) 3 | |
| Lung, spleen | Astragau Radix (Huang qi) 5 | |
| Dry dampness, expel phlegm | Mildly Qi tonic | Polia (Fu ling) 3 |
| Rhizoma Atractylodis (Cang zhu) 4 | ||
| Expel cold | Warm interior | Roasted Aconiti Tuber (Pao fu zi) 3 |
| Warm middle | Zingiber officinale (Gan jiang) 2 | |
| Tonify blood | Angelicae Radix (Dang gui) 3 | |
| Euphoria longan (Long yan rou) 3 | ||
| Rehmanniae Radix Glutinosae (Shu di huang) 3 | ||
| Polygoni Multifloli Radix (He shou wu) 3 | ||
| Promote the movement of Qi | Magnolia Officinalis (Hou po) 3 | |
| Tonify vital essence | Ganoderma lucidum (Ling zhi) 2 | |
| Tonify digestive function | Crataegi Fructus (Shan zha) 3 | |
| Nourish and tonify essence and blood, tonify yang | Gelatinum Cervi Cornu (Lu jiao jiao) |
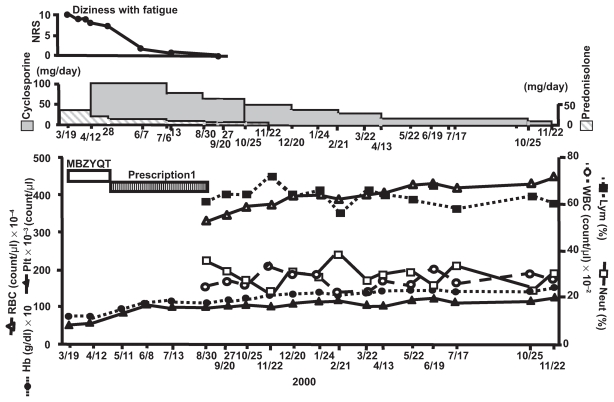
Figure 3.
Change of Hb, Plt, WBC, RBC and the percentage of lymphocyte and neutrophil.
Abbreviations: Hb, hemoglobin; MBZYQT, modified bu zhong yi qi tang; Plt, platelet; RBC, red blood cells; WBC, white blood cells.
The four diagnostic procedures of TCM which include ”Looking”, “Hearing”, “Asking” and “Feeling”, were carried out on the first visit, as shown in Table 5 (Case 1) and Table 6 (Case 2).7
Table 5.
Diagnosis based on TCM theory with “Four Procedures” (Case 1)
| Feeling (Pulse) | (A) slippery, (B) fine, (C) weak |
| Looking | (D) purple spots, (E) pale complexion (white), (F) blue and pale tongue body, (G) dark color of vena sublingualis, (H) moon face, |
| Hearing and asking | (I) appetite loss, (J) constipation, (K) pancytopenia, (L) sensitive to heat, hot palm, sweaty sole, dream much (M) feel cold below the ankle, (N) general fatigue |
| Diagnosis | Spleen Qi deficiency (B, C, D, I, J, N), blood deficiency (B, C, E, F) yin deficiency (C, K, L), yang deficiency(M), dampness and phlegm, (A, H) blood stasis (F, G) |
Notes: Letters in parentheses show the diagnosis based on “Four Procedures”: feeling, looking, hearing and asking.
Table 6.
Diagnosis based on TCM theory with “Four Procedures” (Case 2)
| Feeling (Pulse) | (A) string-like, (B) rapid (100/min) |
| Looking | (C) pale complexion, (D) pale tongue body, (E) slightly dark vena sublingualis |
| Hearing and asking | (F) generalized fatigue, (G) palpitations, shortness of breath, (H) diarrhea, (I) weak by nature, (J) intolerant to cold (K) difficulty falling asleep, dream abundantly, (L) sweaty palms and soles, (M) emphysema |
| Diagnosis | Qi deficiency (F, I), “Heart Qi Deficiency” (B, G), “Blood Deficiency” (B, C, D) yin deficiency (B, K, L), yang deficiency (J), “Blood Stasis” (E), simultaneous “Spleen” and “Lung” dysfunction (H, M) |
Notes: Letters in parentheses show the diagnosis based on “Four Procedures”: “feeling, looking, hearing and asking”.
Case reports
Case 1
The patient first presented with purpura at another general hospital in September 1999. She was examined thoroughly, and diagnosed as having acquired aplastic anemia of unknown etiology.
The changes in blood examination parameters since the time of admission to that hospital are shown in Figure 1. After several Plt transfusions, the Plt count increased to 87,000/μl, followed by a prompt decrease to 34,000/μl. The minimum Plt count was 15,000/μl. Erythrocyte (red blood cell [RBC]) transfusion seemed to provide a slight increase in the Hb level, but it gradually decreased again. When WBC count of normal leukocyte classification decreased, G-CSF was transfused about once a fortnight. The patient resumed photosensitizing dye on February 19, 2000 after an interruption of a two-year course of therapy while being hospitalized. This seemed to improve the Hb level. Therefore, RBC were not transfused, and the Hb maintainted a relatively good level compared with the Plt level observed since starting the photosensitizing dye. Though her fatigue slightly improved, her anemia did not. As shown in Figure 2, examination just prior to consultation at the Hijikata clinic in April 2000, revealed a Plt count of 36000/μl and Hb level of 8.9 g/dl. On April 22nd, 2000, she presented to the Hijikata clinic.
Her past history was notable for palpitation and hypertension evident since 47 years of age, coincident with menopause. She had been taking amlodipine with good blood pressure control. As shown in Table 5, the results determined by TCM diagnostic procedures utilizing the “Four examinations” such as “Looking”, “Feeling”, “Hearing”, and “Asking” are shown. She had a slippery, fine and weak pulse, which in TCM indicates a Qi deficiency,6 a pale complexion, which suggests “Blood” deficiency,7 and a blue, pale tongue body color and a dark coloration of the vena sublingualis, which suggests blood stasis.8 She exhibited purpura, suggesting the “Spleen” was not properly regulating the “Blood”.9 She complained of appetite loss and severe constipation as side-effects of the conventional therapy along with general fatigue, which indicates a “Spleen” Qi deficiency.12 She also complained of a cold feeling below the ankle, which indicates a yang deficiency of the “Kidney”13 while also a sensitivity to heat with hot palms and sweaty soles, which indicates a general yin deficiency.14 Furthermore, she had insomnia, considerable dream acitivity (yin deficiency).14 The slippery pulse implied excessive body dampness and the moon face suggested the presence of phlegm.
Finally, she was diagnosed as having “Spleen” Qi deficiency, “Blood” deficiency, yin deficiency, yang deficiency, dampness, phlegm and blood stasis (Table 5).
Accordingly, we administered prescription A, modified gui pi tang.15 In this prescription, it is considered that ren shen, dang shen, shan yao, huang qi, and zhi gang cao tonify the “Spleen”, ”Heart”, “Lung”, and “Kidney” Qi. Ze he che or PH, dang gui, and long yan rou tonify the blood.16 PH warms and tonifies the kidney as well. Pao fu zi, gan jiang, and ai ye expel cold. Yu jin and san qi invigorate the blood, and ling zhi tonifies the vital essence, as shown in Table 1.
In Figure 2, on April 28th, six days after starting TCM therapy, the Plt count and Hb level increased from 36,000/μl to 47,000/μl and 8.9 g/dl to 9.6 g/dl, respectively. On May 12th, 30 days after TCM had started, Plt increased to 54,000/μl and Hb to 9.8 g/dl. However, the patient complained of flatulence. We added herb mixture B to prescription A to improve the transport function of the digestive system. On June 27th, her flatulence, constipation, Plt and Hb were unchanged, so we added another herbal mixture C to distribute the liver Qi, raise yang, clean heat, detoxify and promote the movement of the Qi in the digestive system as well as tonify blood (Table 2). To a small degree the Hb concentration and Plt count increased, but the WBC decreased. The increase of Hb and Plt after administration of prescription C might imply Tabebuia Avellanedae (TA) may have some effect which improve anemia, as well. This is because this is the only herb to improve anemia among the herbs in mixture C.17 She complained of excessive perspiration at night and persistent constipation.
On July 27th, we added prescription D to treat night sweats and to resolve blood stasis. Although initially Plt increased, Hb did not respond at all. On October 16th, we added Cervi Cornus Colla (lu jiao jiao)18 to tonify the “Kidney” yang so as to nourish and tonify the “Kidney Essence” and “Blood”, because cold feeling below the ankle persisted. Soon thereafter, Plt sharply increased and Hb increased from 9.1 to 9.9 g/dl. On December 15th, as she had requested treatment of her fatty liver, a side effect of the conventional therapies, we added Tinospora Tuberculata (ayurubeda’s herb) (F) to improve lipid metabolism.19–21 Further improvement in Plt and Hb was observed. Cyclosporine was reduced to 25 mg in December 2000 which may have influenced the blood tests somewhat.
When she presented on January 16th, 2001, her moon face, night sweats, appetite loss, and fatigue had disappeared almost completely. Although not entirely good, her blood examination parameters have been stable so far.
Finally, the considerable improvement in the Plt count and Hb concentration occurred after the administration of prescription A, including PH and Cervi Cornus Colla, with a small additional improvement after the administration of Tabebuia Avellanedae and Tinospora Tuberculata.
Case 2
The patient had been suffering from tonsillitis, swollen lymph nodes, and fever since August 1999. The fever resolved with antibiotics, but general fatigue and yellowish white sputum production continued. As a result of bone marrow aspiration at a municipal hospital, he was suspected to be in a chronic state of virus-associated hemophagocytic syndrome.
He consulted Toyodo Hijikata clinic on March 18th, 2000, because no improvement had been observed in spite of steroid treatment.
He had been suffering from empyema and nasal obstruction since childhood. He reported palpitations and shortness of breath. In Table 6, the findings and the diagnosis based on TCM principles are shown. He had a string-like rapid pulse (100/min) and his tongue body color was very pale, which suggested severe anemia. The vena sublingualis was slightly dark. Blood pressure was 150/70. His complexion was pale. He complained of general fatigue, diarrhea, difficulty in falling asleep, empyema with nasal obstruction and sweaty palms and soles. He was self described as by nature, weak and intolerant to cold. The diagnoses were Qi deficiency, “Heart” Qi deficiency,8 “Blood” deficiency,7 yin deficiency,14 yang deficiency,13 blood stasis,10 and simultaneous “Spleen” and “Lung” dysfunction.22 The details are presented in Table 6.
We administered modified Bu zhong yi qi tang (MBZYQT) (tonify the middle and augment the Qi decoction).23 to tonify and regulate Qi, disperse the liver Qi, promote the movement of Qi, tonify the “Blood “and “Essence”, and expel “Cold” (Table 3).
As shown in Figure 3, from March 31st until April 28th, 2000 he took Sanguisorbae Radix (di yu) and Sophorae Flos (huai hua) to stop hemorrhoidal bleeding by a cooling of his “Blood” constitution.5 It worked dramatically. On April 12th, his prednislone dose was reduced and cyclosporine therapy initiated because the prednislone did not work. As fatigue was present accompanied by dizziness, he was asked to express his fatigue level with a numerical rating scale NRS (maximum = 10, no fatigue = 0). Fatigue and dizziness continued at the second visit on April 28th. Accordingly, a second formula including animal material such as Cervi Cornus COlla was administered (Table 4). At the same time, PH (zi he che) 4 g/day and Notoginseng Radix (san qi) 2 g/day were started and continued until all of the TCM treatment was finished (Figure 3). Thereafter, the Plt count and Hb level steadily increased, and dizziness, along with fatigue, decreased. Anemia continued to improve at each blood examination.
Previous administration of prednisolone had not improved dizziness accompanied by fatigue. After starting MBZYQT, however, it decreased a little. Blood examination continued to improve until November 22nd, 2001.
After stopping TCM treatment, the patient gradually decreased the conventional therapies. Approximately one year later he was sufficiently recovered to go to work for a company. His Plt count was 126,000/μl and Hb level, 15.1 g/dl. on December 1st, 2001 (Figure 3).
Discussion
Both cases received TCM therapy, including PH, together with animal material such as Cervi Cornus Colla (Deer Antler Glue) as well as conventional therapies for anemia. The PH tonifies the “Kidney” yang in addition to nourishing the “Blood”. The Cervi Cornus Colla (Deer Antler Glue) is a cheaper and weaker substitute for deer velvet, which is expensive, and similarly tonifies “Kidney” and fortifies the yang.13 The result was that administration of these two substances caused an improvement in the Plt count, Hb concentration, and QOL, without recrudescence thus far.
In these cases, PH and Cervi Cornus Colla would warm and tonify the “Kidney” and augment the “Blood” and “Essence” which indicates an influence of the “Marrow system” by the “Kidney-Marrow” in TCM principles. The “Marrow” produces the “Bone marrow” and fills the spinal cord and the brain in TCM theory.23
However, as shown in Figure 3, the white cell classification in Case 2 indicated a higher ratio of lymphocytes, which coincides with the suggestion of a chronic state of virus-associated hemophagocytic syndrome. Even in this case, these two substances worked for the improvement of his anemia.
Animal materials can help to treat successfully certain cases in which herbs do not work for intractable anemic diseases. Because the human placenta must be removed completely from the uterus after childbirth and is then normally discarded, there is a role for animal material in intractable anemia as it is comparatively easy to obtain.
Patients with aplastic anemia or incurable anemia who are awaiting bone marrow transplantation, usually wait for some time before an human leukocyte antigen-matched donor is found. In such a case, the intake of PH and animal material beneficial to anemia may yield some improvement in blood test parameters as well as patient symptoms, including overall QOL. We believe TCM therapy including PH and Cervi Cornus Colla will be one of the alternative choices for treating otherwise intractable anemia.
However, it is important to be be careful not to apply too much PH and Cervi Cornus Colla in patients with yin deficiency. 14 Because they warm the “Kidney”, leading to a general warming of the body organs followed by aggravation of the yin deficiency, which result in symptoms such as coughing up blood, body heat such as “Steaming Bones”, and night sweats.1
Accordingly, there must be a careful watch of the clinical course so as not to cause yin deficiencies by prescribing excessive quantities of PH and Cervi Cornus Colla.
Finally, the specific mechanisms of actions of these human and animal materials in anemia remain unclear. Therefore this is an important subject for future investigation and a greater number of clinical cases need to be accumulated.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bensky D, Clavey D, Stoger E, Gamble A. Chinese Herbal Medicine Materia Medica. 3rd Ed. Vista, CA: Eastland Press; 2004. pp. 806–807. [Google Scholar]
- 2.Zhongguo Z. Yixueke xueyuan hongguoxiehe yikedaxue yaoyongzhi-wuyanjiusuo; 46 zhiheche; zhongyaozhi. Di lu ce: renminweisheng-chufanshe; 1998. p. 179. [Google Scholar]
- 3.Song tangshenwei zhuan (1082) Shang zhigou yiwei san min jiaodian zhengleibencao. Di shi wu quan renbao huaxiachufanshe; 1993. p. 435. [Google Scholar]
- 4.Shizhen L. Bencaowangmu renbu. Di wuxier quan renbao: Renminweishengchufanshe; 1982. p. 2963. (1578) [Google Scholar]
- 5.Bensky D, Clavey D, Stoger E, Gamble A. Chinese Herbal Medicine Materia Medica. 3rd Ed. Vista, CA: Eastland Press; 2004. pp. 570–575. [Google Scholar]
- 6.Bensky D, Clavey D, Stoger E, Gamble A. Chinese Herbal Medicine Materia Medica. 3rd Ed. Vista, CA: Eastland Press; 2004. pp. 559–562. [Google Scholar]
- 7.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 143–174. [Google Scholar]
- 8.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 166–171. [Google Scholar]
- 9.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 145–146. [Google Scholar]
- 10.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 150–151. [Google Scholar]
- 11.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 244–245. [Google Scholar]
- 12.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 242–243. [Google Scholar]
- 13.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 253–254. [Google Scholar]
- 14.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 187–188. [Google Scholar]
- 15.Bensky D, Barolet R. Chinese Herbal Medicine: Formulas and Strategies. Vista, CA: Eastland Press; 1990. Restore the spleen decoction; pp. 255–257. [Google Scholar]
- 16.Bensky D, Clavey D, Stoger E, Gamble A. Chinese Herbal Medicine Materia Medica. 3rd Ed. Vista, CA: Eastland Press; 2004. pp. 750–766. [Google Scholar]
- 17.Hijikata Y, Kaneko J, Lu X, Nasu M, Yamashita S. Traditional Chinese medicine improves the course of refractory leukemic lymphoblastic lymphoma and acute lymphocytic leukemia: Two case reports. The American Journal of Chinese Medicine. 1995;23(2):195–211. doi: 10.1142/S0192415X95000250. [DOI] [PubMed] [Google Scholar]
- 18.Bensky D, Clavey D, Stoger E, Gamble A. Chinese Herbal Medicine Materia Medica. 3rd Ed. Visita, CA: Eastland Press; 2004. pp. 766–770. [Google Scholar]
- 19.Hijikata Y, et al. Effect of Tinospora tuberculata on hyperlipemia. J Kampo Med. 2001;48(1):106–112. [Google Scholar]
- 20.Yokozawa T, Wang TS, Chen CP, Hattori M. Tinospora tuberculata suppresses nitric oxide synthesis in mouse macrophages. Biol Pharm Bull. 1999;22(12):1306–1309. doi: 10.1248/bpb.22.1306. [DOI] [PubMed] [Google Scholar]
- 21.Yokozawa T, Wang TS, Chen CP, Hattori M. Inhibition of nitric oxide release by an aqueous extract of Tinospora tuberculata. Phytother Res. 2000;14(1):51–53. doi: 10.1002/(sici)1099-1573(200002)14:1<51::aid-ptr545>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 22.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 108–109. [Google Scholar]
- 23.Bensky D, Barolet R. Chinese Herbal Medicine: Formulas and Strategies. Vista, CA: Eastland Press; 1990. Restore the spleen decoction; pp. 241–243. [Google Scholar]
- 24.Maciocia G. The Foundations of Chinese Medicine. Edinburgh: Churchill Livingstone; 1989. pp. 96–97. [Google Scholar]