Sir,
Major shoulder surgery can now be performed as day case procedures, thanks to advancements in minimally invasive techniques and regional anesthesia. However, once the regional anesthetic block has worn off, at an average of 20h, the rebound pain can be significant. Many day-case patients are at home at this time, without immediate access to stronger analgesia. Although patients are advised to preload with anti-inflammatories and analgesics prior to the regional block wearing off this does not always occur due to variability in time of regional wearing off and patient compliance.
Diclofenac hydroxyethylpyrollidine (DHEP) patches have proven to reduce pain and inflammation in the direct treatment of acute and chronic inflammatory conditions.[1–11] They release the active ingredient over a 12-24 hour period,[13] with less systemic side-effects than oral forms and better patient compliance.[14] DHEP patches have also proven beneficial for day-case laparoscopic surgery by reducing postoperative analgesic requirements and hospital stay.[15]
We assessed the analgesic effect and postoperative recovery of diclofenac patches compared to tablets in day case arthroscopic shoulder surgery. Thirty one patients underwent arthroscopic shoulder procedures over a six-month period in a specialist day surgery hospital. The patients were randomized in two groups: Group 1 (17 patients) received diclofenac tablets in addition to paracetamol and codeine and Group 2 (14 patients) had diclofenac patches in addition to paracetamol and codeine. All patients also had a single shot interscalene regional with levobupivicaine, intravenous paracetamol intraoperatively and cold compression therapy. The patches were changed twelve hourly after application and continued to be used at least 48h postsurgery. Simple randomisation was applied and ethical approval not specifically sought, although all patients were consented accordingly. The patients and investigators were not blinded.
[Table 1] lists the procedures performed. The most common was arthroscopic shoulder stabilisation procedure.
Table 1.
Types of shoulder procedures performed and number.
| Procedures | Number |
|---|---|
| Arthroscopic Shoulder Stabilisation | 17 |
| Arthroscopic SLAP Repair | 1 |
| Arthroscopic Subacromial Decompression | 3 |
| Arthroscopic AC Joint Excision | 1 |
| Arthroscopic Rotator Cuff Repair | 4 |
| Arthroscopic Capsular Release | 3 |
| Other | 2 |
All patients were contacted by telephone an average of 48h postsurgery and completed a 5 point visual analogue pain scale, where 0 was no pain and 5 maximum pain. They were also asked about any additional analgesic requirements and their comfort level. Chi-squared statistical analysis was performed using ‘Analyse-it’ software package.
The mean age of Group 1 was 32.7 years and Group 2 was 40.5 years (p>0.05). The male:female ratio in group 1 was 14:3 and in group 2 was 12:2. The mean surgical time was 75 minutes in Group 1 and 72 minutes in Group 2 (p>0.05). The mean time from end of procedure to discharge from the day surgery hospital was three hours and 43 minutes for Group 1 and three hours and 31 minutes for Group 2 (p>0.05). The mean pain score for at 48h post-op was 1.7 in Group 1 and 1.1 in Group 2 [Figure 1]. This was significant (p=0.031). One patient in each group required additional analgesia in the form of Tramadol. There were no side-effects to the diclofenac tablets or patches.
Figure 1.
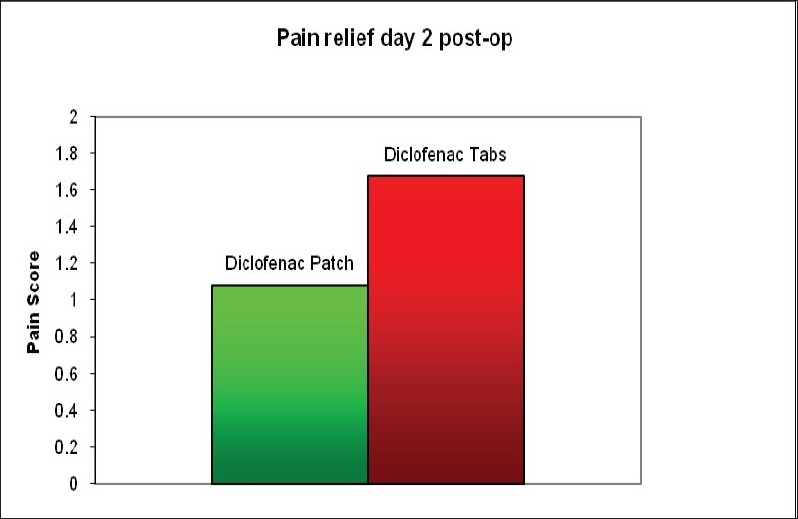
Post-operative pain score on the second postoperative day
In conclusion, diclofenac patches provides significantly better pain relief compared to tablets in the early postoperative period following arthroscopic shoulder surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Gschwend MH, Martin W, Arnold P, Verdun MO, Cambon N, Frentzel A, et al. Determination of the transdermal bioavailability of a newly developed diclofenac sodium patch in comparison with a reference preparation. Arzneimittelforschung. 2005;55:403–13. doi: 10.1055/s-0031-1296879. [DOI] [PubMed] [Google Scholar]
- 2.Predel HG, Koll R, Pabst H, Dieter R, Gallacchi G, Giannetti B, et al. Diclofenac patch for topical treatment of acute impact injuries: A randomised, double blind, placebo controlled, multicentre study. Br J Sports Med. 2004;38:318–23. doi: 10.1136/bjsm.2003.005017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bruhlmann P, Michel BA. Topical diclofenac patch in patients with knee osteoarthritis: A randomized, double-blind, controlled clinical trial. Clin Exp Rheumatol. 2003;21:193–8. [PubMed] [Google Scholar]
- 4.Galer BS, Rowbotham M, Perander J, Devers A, Friedman E. Topical diclofenac patch relieves minor sports injury pain: Results of a multicenter controlled clinical trial. J Pain Symp Manage. 2000;19:287–94. doi: 10.1016/s0885-3924(00)00125-1. [DOI] [PubMed] [Google Scholar]
- 5.Solignac M. Assessment of a topical NSAIDs in the treatment of pain and inflammation: The example of Flector Plaster, a local bioadhesive plaster containing diclofenac epolamine. Presse Med. 2004;33:3S10–3. [PubMed] [Google Scholar]
- 6.Solignac M. Proof of the pharmacodynamic activity of Flector Plaster in healthy volunteers and patients suffering from osteo-arthritis of the knee. Presse Med. 2004;33:3S5–9. [PubMed] [Google Scholar]
- 7.Affaitati G, Vecchiet F, Lerza R, De Laurentis S, Iezzi S, Festa F, et al. Effects of topical diclofenac (DHEP plaster) on skin, subcutis and muscle pain thresholds in subjects without spontaneous pain. Drugs Exp Clin Res. 2001;27:69–76. [PubMed] [Google Scholar]
- 8.Rosenthal M, Bahous I. A controlled clinical study on the new topical dosage form of DHEP plasters in patients suffering from localized inflammatory diseases. Drugs Exp Clin Res. 1993;19:99–105. [PubMed] [Google Scholar]
- 9.Gallacchi G, Marcolongo R. Pharmacokinetics of diclofenac hydroxyethylpyrrolidine (DHEP) plasters in patients with monolateral knee joint effusion. Drugs Exp Clin Res. 1993;19:95–7. [PubMed] [Google Scholar]
- 10.Jenoure P, Segesser B, Luhti U, Gremion G. A trial with diclofenac HEP plaster as topical treatment in minor sport injuries. Drugs Exp Clin Res. 1993;19:125–31. [PubMed] [Google Scholar]
- 11.Dreiser RL, Tisne-Camus M. DHEP plasters as a topical treatment of knee osteoarthritis: A double-blind placebo-controlled study. Drugs Exp Clin Res. 1993;19:117–23. [PubMed] [Google Scholar]
- 12.Galeazzi M, Marcolongo R. A placebo-controlled study of the efficacy and tolerability of a nonsteroidal anti-inflammatory drug, DHEP plaster, in inflammatory peri- and extra-articular rheumatological diseases. Drugs Exp Clin Res. 1993;19:107–15. [PubMed] [Google Scholar]
- 13.Assandri A, Canali S, Giachetti C. Local tolerability and pharmacokinetic profile of a new transdermal delivery system, diclofenac hydroxyethylpyrrolidine plaster. Drugs Exp Clin Res. 1993;19:89–95. [PubMed] [Google Scholar]
- 14.Martens M. Efficacy and tolerability of a topical NSAID patch (local action transcutaneous flurbiprofen) and oral diclofenac in the treatment of soft-tissue rheumatism. Clin Rheumatol. 1997;16:25–31. doi: 10.1007/BF02238759. [DOI] [PubMed] [Google Scholar]
- 15.Alessandri F, Lijoi D, Mistrangelo E, Nicoletti A, Crosa M, Ragni N. Topical diclofenac patch for postoperative wound pain in laparoscopic gynecologic surgery: A randomized study. J Minim Invasive Gynecol. 2006;13:195–200. doi: 10.1016/j.jmig.2006.02.001. [DOI] [PubMed] [Google Scholar]


