Abstract
Liposuction is a cosmetic procedure to remove fat. Liposuction may be performed either under general anaesthesia or under local anaesthesia. The procedure has been reported to be associated with significant morbidity and risk of mortality under general anaesthesia. Since the first description by Jeffrey Klein, dermatologic surgeons have made significant contributions in this field, and tumescent liposuction using microcannuale under local anaesthesia, is regarded as safe and effective. The author has performed over 200 liposuctions in the last four years in India and this article describes the procedure of microcannular tumescent liposuction in the light of her experience.
Keywords: Liposuction, tumescent anaesthesia, micro cannulae, local anaesthesia
INTRODUCTION
Liposuction is the surgical removal of subcutaneous fat by means of aspiration cannulae introduced through small skin incisions, assisted by suction. Synonyms used in literature include liposuction surgery, suction-assisted lipectomy, suction lipoplasty, fat suction, blunt suction lipectomy, and liposculpture.[1,2]
Liposuction is one of the most commonly performed cosmetic procedure today.[1] Dermatologists now perform about one third of these procedures in the United States and have pioneered many of the advances in liposuction, especially in the fields of ambulatory surgery and local anaesthesia.
In India, in the past decade since economic liberalization, the scenario has changed dramatically with respect to cosmetic procedures. Globalization, improved affluence, access to information via internet and television, and a high degree of awareness about health and beauty have all led to an increasing demand for aesthetic procedures. An increasing number of dermatologists are now performing aesthetic procedures. This article discusses the microcannular tumescent liposuction, which has emerged as the gold standard method in liposuction, in the background of our experience with about 200 patients over the last four years.
Structure of fat
Subcutaneous fat is arranged in the form of lobules separated from each other by septae.[3–6] The fibrous septae consist of blood vessels, nerves, and lymphatics. Each lobule consists of fat cells, which consist mostly of triglycerides and fill up the cell almost entirely, pushing the nucleus to one side. It has been shown that during initial weight gain in any person, there is an increase in the size of the fat cell. With continued weight gain, there is, in addition, an increase in the fat cell number as mesenchymal stem cells get converted to fat cells. Diet and exercise have been shown to decrease the fat cell size, but not the fat cell number, which is referred to as “resistant fat”.
Liposuction is a method of reducing the fat cell number and thereby, the resistant fat. Liposuction removes the resistant fat by two mechanisms:
Removal of fat cells during suction [Figure 1]
Damaging the fat cells by the to-and-fro motion of the cannula. These remaining damaged fat cells get absorbed slowly over 6–12 weeks and hence, the final result after liposuction is seen after 6–12 weeks, a fact which needs to be emphasised during counselling.
Figure 1.
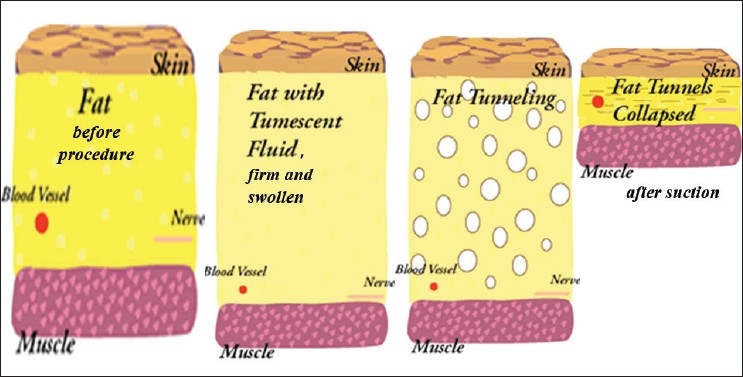
Principle of liposuction; fat before and after tumescence, and after aspiration
HISTORY OF LIPOSUCTION
Liposuction was initially developed in the late seventies in Italy and France.[7,8] At that time, liposuction was performed under general anaesthesia without any introduction of fluid, hence, called “dry liposuction”. Later, a small amount of fluid was introduced into the fat (the “wet technique”). These methods were associated with much blood loss, and patients frequently required blood transfusions. In 1985, Dr. Jeffrey A. Klein, a dermatologist in California, revolutionised liposuction surgery when he developed the tumescent technique, which permits liposuction totally by local anaesthesia and with minimal surgical blood loss.[8] Further modifications such as power liposuction and ultrasonic liposuction have been introduced with variable results. Despite these advances, the tumescent technique remains the worldwide standard of care for liposuction.[1,2]
METHODS OF LIPOSUCTION
Microcannular tumescent liposuction
The word “tumescent” means swollen and firm.[8,9] This technique involves subcutaneous infiltration of large volumes of crystalloid fluid called Klein’s solution, which contains low concentrations of lignocaine and epinephrine, followed by suction-assisted aspiration of fat by using small aspiration cannulae called microcannuale [Figure 1]. The term tumescent liposuction specifically excludes the use of any additional anaesthesia, either intravenous or gaseous, and by definition, is a method for performing liposuction surgery with the patient totally under local anaesthesia.[1,2]
The procedure of microcannular tumescent liposuction consists of two steps:
-
Induction of anaesthesia by tumescent anaesthesia:
Making 4–8 small incisions called adits (1–3 mm in size)
Introduction of a large amount (1–4 L) of Klein’s solution into the fat. Klein’s solution contains lignocaine, epinephrine, and large amounts of saline. The saline balloons the fat tissue, epinephrine causes vasoconstriction, thus, decreasing bleeding, and lignocaine induces local anaesthesia. This procedure usually lasts 45–60 minutes.
Allowing the fluid to percolate uniformly through all layers, a process called detumescence, lasts 30 minutes.
-
Aspiration of fat by microcannular liposuction:
Sucking the fat out through microcannuale which are 1.5–3 mm in diameter. This is a slow process lasting 1–1½ hours.
Leaving the incision wounds of cannulae open to drain out fluid. A small amount of fluid is left back in the tissue and is allowed to drain slowly over two days. This residual fluid provides analgesia in the immediate postoperative period.
Applying compression bandages and sending the patient home without any hospital admission.
The procedure has the advantages of safety, lack of need for hospital admission, and rapid postoperative recovery time. However, the procedure is also slow, taking 3–4 hours to perform and also, the amount of fat that can be extracted is usually limited to about 4–5 litres.
Conventional liposuction using large cannulae under general anaesthesia, largely practised by plastic surgeons, is performed as follows:
General anaesthesia is used.
Introduction of a small amount of fluid into the fat.
Making large incisions (1–1.5 cm) to introduce cannulae.
Sucking out large amounts of fat, often 8–10 litres (called megaliposuctions), quickly in 1–2 h, through large cannulae (6 mm-1 cm in diameter).
Suturing the incision wounds of cannulae.
The whole procedure lasts 2–3 hours. Thus, this method is quick, can remove large amounts of fat, and saves time for the surgeon. However, it has the following disadvantages:
As the method is under general anaesthesia, the patient has to be hospitalized, which adds significantly to the cost and the possibility of hospital-acquired infections.
General anaesthesia always has its risks.
The use of large cannulae causes greater damage to tissue and hence, increases the bleeding. This technique is associated with significant blood loss,[10,11] often needing blood transfusions.
There is a risk of side effects such as fat embolism, which can be potentially fatal.
Large cannulae need large incisions which have to be sutured and which heal with significant scars.
Recovery time is slow, as after any procedure under general anaesthesia.
Table 1 shows the comparison between the two methods.
Table 1.
Comparison of techniques
| Conventional method | Tumescent method | |
|---|---|---|
| Pain control | General anaesthesia | Local anaesthesia |
| Risks | Higher complication rate | Lower complication rate |
| Bleeding | Significant blood loss often requiring transfusion | Minimal blood loss |
| Postoperative period | Requires strong, parenteral pain-killers | Pain relief up to 24 h, needing only minimal, oral pain killers |
| Hospital admission | Needed | Outpatient procedure |
| Return to work | Days to weeks | 1–3 days |
| Cannula size | Larger cannulae | Smaller cannulae |
| Sutures | Required | Not required |
| Speed | Quick | Slow |
| Amount of fat | Large, 8–10 litres | Smaller, 3–5 litres |
| Cost | Expensive because of hospital stay | Less expensive |
Other methods of liposuction
Power-assisted liposuction[12] with a reciprocating cannula is a new technology for liposuction and has some advantages. In powered liposuction, the reciprocating motion of the cannulae mimics the to-and-fro action of the surgeon’s cannula movement, decreasing the work of the procedure and is therefore, less tiring for the physician. In addition, it allows the surgeon to remove fat more completely in “tight” areas where forceful cannula movements are difficult because of physical space constraints (e.g., per umbilical and waist areas). While powered liposuction can help to remove fat quickly, it can do so only if large cannulae are used. Usually power-assisted liposuction also needs concomitant IM or IV narcotics and sedatives, as well as sometimes using nitrous oxide. These features therefore, negate the above mentioned advantages of tumescent liposuction (safety because it is done under local anaesthesia, and finesse because of the use of microcannuale).
Ultrasound-assisted liposuction
Ultrasound-assisted liposuction (UAL) was introduced to damage the fat cells and thereby, facilitate the removal of fat.[13] However, the method had significant side effects such as burns of the skin. The damaged fat also lead to small cysts containing fluid called seromas. Ultrasound-assisted liposuction is associated with significant bruising and prolonged postoperative swelling. Most importantly, the ultrasound machines are expensive, increasing the cost of the procedure.
INDICATIONS FOR LIPOSUCTION
Liposuction can be used in the following situations:[1,2]
Fat that is resistant to diet or exercise, located in any area of the body such as the abdomen, thighs, hips, neck, face, and under the chin.
Liposuction can be used for breast reduction. In men, gynaecomastia is an important indication for liposuction.
Liposuction has been found to be useful for noncosmetic indications also, such as hyperhidrosis of axillae[14] and lipomas.[15]
Table 2 shows our experience in Indian patients. It is interesting to note that there were more male patients for this procedure than women. Gynaecomastia is the most common indication in men, whereas the abdomen is the most common area in women. Gynaecomastia causes much social embarrassment in India, particularly at the time of weddings, when the bridegroom has to sit for religious ceremonies without wearing a shirt. Eighteen women also sought the procedure for their thighs, which reflects the increasing tendency of young women to wear tight jeans. As many as 18 patients came back for a second session, one patient for a third session, and one patient for a fourth session.
Table 2.
Indications in 200 Indian patients (author's experience)
| Indications | Men (n=113) | Women (n=87) | Total |
|---|---|---|---|
| Abdomen | 45 | 37 | 82 |
| Thighs | - | 23 | 23 |
| Chin | 1 | 3 | 4 |
| Arms | - | 4 | 4 |
| Buttocks | - | 7 | 7 |
| Flanks / Love handles | 8 | 5 | 13 |
| Breast | 59 | 6 | 65 |
| Axilla | - | 2 | 2 |
PRINCIPLE OF TUMESCENT ANAESTHESIA
The most important aspect of tumescent liposuction is that a local anaesthetic is used over a wide area to provide anaesthesia and analgesia, using a sufficient quantity of lignocaine far in excess of the conventional dosage. Conventional teaching has widely regarded, without adequate pharmacological proof, that the safe upper limit for lignocaine administration is 6 mg/kg body weight. In a radical departure from this conventionally accepted fact, Klein showed that in tumescent anaesthesia, much higher doses, even up to 45–55 mg/kg weight can safely be administered.[16–20] This is because in tumescent anaesthesia, the rate of absorption of lignocaine is slow, leading to smaller peak values and hence, lesser toxicity. The reasons for the slow absorption of lignocaine are:
Subcutaneous fat has a low volume of blood flow.
Lignocaine is lipophillic and is easily sequestered in fat.
Diluted epinephrine in saline solution ensures vasoconstriction, thus, minimizing systemic absorption and bleeding.
The large volume of tumescent solution itself compresses blood vessels by hydrostatic pressure.
The very low dilution of lignocaine in Klein’s solution does not achieve the gradient required for systemic absorption.
Most of the solution is removed during aspiration, minimizing the duration for absorption.
This slow absorption from subcutaneous fat has been likened to a slow release capsule, with the fat itself acting as the capsule!!
PROCEDURE OF TUMESCENT LIPOSUCTION
Patient selection
Proper patient selection is highly important—the ideal candidates are patients with localized deposits of fat, who are not grossly obese, without significant medical problems, and have realistic expectations.[1,2,5,17,21] Many patients seek consultation in the mistaken assumption that liposuction is a treatment for weight reduction. It should be clarified to them that liposuction is only for improvement of shape and any weight loss (which will be about 4–5 kg) is only incidental. There is no definite age or weight limit for patients to undergo liposuction.
The maximum amount of fat that can be removed safely by tumescent liposuction is probably about 4–5 litres.[10] Generally, it is advisable to avoid the so-called megaliposuctions as they are associated with complications.[1,2] The risk of side effects increases with removal of larger amounts of fat. Different areas such as the abdomen and the thigh or buttock are not generally combined in one session.[18] However, it is possible to treat both buttocks or both thighs in one session. If patient desires more than one area or needs more than 4–5 litres of fat removal, the procedure may be repeated any time after two weeks.
A thorough medical history with particular reference to history of bleeding diathesis, emboli, thrombophlebitis, infectious diseases, poor wound healing, and diabetes mellitus should be always taken. Patients with a medical history of these conditions need to be examined and cleared by a physician before undergoing liposuction. Liposuction is contraindicated in patients with severe cardiovascular disease, severe coagulation disorders including thrombophilia, and during pregnancy. The patient’s history should also include noting prior abdominal surgeries such as caesarean sections which produce scarring. A detailed drug history is essential. As lignocaine is metabolized by the liver, drugs that compete with it for metabolism by the cytochrome P450 enzyme system or displace lignocaine from plasma proteins can increase lignocaine blood levels and cause lignocaine toxicity.
The physician must perform a detailed physical examination to determine that the areas of planned for surgery are amenable to liposuction. In particular, any evidence of keloids, scars, or hernia should be looked into.
Counseling
Counseling should include:[21]
Discussion on different management options, including the role of diet and exercise.
Detailed explanation about the surgical procedure, including possible postoperative complications.
Specific instructions that full results would be seen after 6–12 weeks.
Instruction that although the fat removed by liposuction does not normally come back, there may be recurrence of the problem if the patient puts on excessive weight. The importance of continued exercise and diet regulation should be stressed.
Any allergies or medical condition that the patient may have should be recorded.
As in any cosmetic procedure, the patient should not expect to achieve perfection.
Patients should be told not to expect to lose any dramatic amount of weight loss with liposuction. Weight lost is equal only to the amount of fat removed, about 3–5 kg.
Patients should also understand that liposuction does not improve cellulite or the striae. Patients can also be assured that there is no likelihood of loose skin hanging in the operative area due to the elasticity of skin. Abdominoplasty is usually not necessary for abdominal contouring but is only necessary if a large amount of excess skin or muscle laxity is present.[22,23] The recent introduction of skin tightening machines has also helped in the management of any mild laxity.
Preoperative instructions
These are routine and include:[21]
Routine blood investigations such as blood counts, bleeding and clotting time, prothrombin time, blood sugar, liver function tests, HbS Ag, HIV-ELISA, and ECG.
Advice to stop smoking and oral NSAIDs as smoking increases intraoperative bleeding.
Preoperative tranquillizers such as diazepam or lorazepam on the night before surgery to relieve any anxiety.
Injection Vitamin K to minimize postoperative bruising.
On arrival on the day of the surgery, patients are administered preoperative antibiotics such as cephalexin, and a tranquillizer such as oral lorazepam 1 mg. Oral Clonidine 0.1 mg is also administered to prevent epinephrine-induced tachycardia and as an adjuvant anxiolytic drug. The area for liposuction is topographically marked with marker ink to delineate the bulges and asymmetry [Figure 2]. Preoperative photography is vital.
Figure 2.

Topographic marking
Monitoring
Baseline vital signs including blood pressure and heart rate, are to be recorded preoperatively and monitored intraoperatively. Pulse oximeter monitoring is essential. Medical personnel trained in resuscitation, preferably an anaesthetist, should be available on the premises.
Tumescent anaesthesia
This is a very important and vital step. Proper tumescence will ensure painless and smooth aspiration.
Adits are small holes made for insertion of infiltration cannulae. These are done with 1.5–2 mm dermal punches in different locations of the area under infiltration anaesthesia with 1 mL of 2% lignocaine. The number of adits needed depends on the area involved. About 6–8 adits are normally needed for the abdomen.
Tumescent fluid is prepared as follows: The usual tumescent solution concentration used is 0.05–0.1% lignocaine and the concentration of epinephrine is at 1:1,000,000–1.5:1,000,000. As the lignocaine solution is acidic, 10 meq of sodium bicarbonate solution is added to one litre of tumescent solution to raise its pH and to prevent stinging. The acceptable maximum dose of lignocaine is 55 mg/kg for most patients, although we have used dosages up to 57 mg/kg in our patients. If higher concentrations are needed, small amounts of fluid can be reintroduced after partial aspiration to avoid excessive dosing. The recommended concentration of epinephrine in tumescent solutions is 0.25–1.5 mg/L. The total dosage of epinephrine should not exceed 50 µg/kg.
Infiltration of tumescent fluid: The delivery system for tumescent solution consists of infusion bags, infiltration pressure cuffs, an infiltration pump to hasten delivery of the fluid, and infiltration cannulae 0.5–1 mm in size. About 2–3 litres of fluid are infiltrated gradually in different directions, first into deeper layers of fat and then, into the superficial layers. The end point is a firm feel of the skin which makes the skin swollen, and difficult to grasp [Figure 3]. It is important to be slow and to avoid jerky, sudden movements to avoid pain. Normally it takes about 1 to 2 h for proper anaesthesia.
Detumescence: It is important to wait for about 30 min after tumescence for the infiltration fluid to percolate properly and its full pharmacological effects to take effect. This is indicated by a slight decrease in firmness and the ability to grasp the skin.
Figure 3.

Infiltration of tumescent fluid
ASPIRATION
The most important aspect of proper aspiration is the slow, repeated, to-and-fro movement of the cannulae.[24,25] The cannulae are of different sizes, varying in diameter from 1 to 2.5 mm. Cannulae larger than 4.5 mm in diameter are not used as they cause more tissue damage and are associated with the risk of embolism and bleeding. A smaller cannula (1 mm) is first used to create tunnels in the fat. Cannulae of gradually increasing diameter are then employed to aspirate fat. Deeper layers of fat are aspirated first and then the superficial layers. The direction of the handles is always parallel to the skin and is never vertical [Figure 4]. The nonoperating hand is used as a guide to push the fat in the direction of aspiration and also, to feel the tip of the cannula to prevent damage to the overlying skin or underlying structures. It is also important to avoid skin trauma at the adit to ensure proper healing of the adits. Care should be exercised to ensure uniform aspiration in all areas and to avoid excessive aspiration from a given area to avoid dimpling and asymmetry. Different areas are aspirated and then compared for symmetry and regularity. One great advantage of tumescent anaesthesia is that because the patient is conscious, (s) he will feel the pain and warn the surgeon if the cannula is moved deep into the muscle or into the surrounding unanaesthetized area. Also, the patient is in a position to sit or stand so that the surgeon can compare the two sides for symmetry. The process of aspiration normally takes between 90 minutes to two hours and about 3–5 litres of fat are aspirated. Blood loss is minimal and does not exceed 30–50 mL if the tumescence is proper [Figure 5]. It is important to keep the patient engaged by having a television or music in the theatre during the entire procedure.
Figure 4.

Aspiration of fat
Figure 5.

Fat aspirated; note the small amount of blood
Average amounts aspirated from different areas in our patients are shown in Table 3. The maximum amount of fat aspirated in our experience is 4.2 litres.
Table 3.
Average fluid aspiration in different areas in Indian patients
| Sl No | Male | Female | Average (mL) |
|---|---|---|---|
| 1. Abdomen | 45 | - | 3832 |
| 37 | 3611 | ||
| 2. Breast | 59 | - | 2189 |
| 06 | 4200 | ||
| 3. Thighs | 23 | 4157 | |
| 4. Arms | 04 | 2975 | |
| 5. Flanks | 08 | - | 3038 |
| 05 | 2350 | ||
| 6. Buttocks | 07 | 2965 | |
| 7. Chin | 01 | 03 | 450 |
| 237 | |||
| 8. Axilla | 02 | 1100 |
Postoperative dressing and follow-up
Postoperative dressing is a very important step in tumescent liposuction. An important feature of the tumescent procedure is that some amount of the fluid is still left behind at the end of the procedure, which ensures anaesthesia in the immediate postoperative period, minimizing the need for potent oral analgesics. This fluid drains out in 3–5 days to facilitate which the adits are not sutured and are allowed to heal by secondary intention. Tight pressure bandages are essential to ensure proper drainage of the tumescent fluid [Figure 6]. Two layers of pressure dressing (called bimodal compression) are put in place to ensure tight compression in the first two days.[26,27] Dressings are removed on the first postoperative day and the adits are opened again, if necessary, to ensure proper drainage. Improper drainage increases the possibility of panniculitis, secondary infection, and irregularity. Postoperative analgesics and antibiotics are continued. The pressure in the dressing is decreased after three days and continued for a minimum of two weeks. The patient is advised to come for follow-up for daily dressing for three days. It is important to note that while the patient can return to normal sedentary work in 1–2 days, exercise and undue exertion should be avoided for at least ten days
Figure 6.

Postoperative pressure dressing
RESULTS
Figures 7–9 show the results in the regions of the abdomen and the chest in three patients. It should be noted that there is some improvement seen immediately after surgery. However, more improvement is seen over the next three days as residual fluid drains out and also, with continued absorption of damaged fat over 4–6 weeks. Hence, final results are seen at the end of six weeks.
Figure 7.

Liposuctions results, case 1
Figure 9.

Liposuctions results, case 1
Figure 8.

Results of case 2
COMPLICATIONS
Tumescent anaesthesia is a remarkably safe procedure if all the essential steps are adhered to.[17,28–30] In the author’s experience of nearly 200 cases, side effects have been rare.
Postoperative pain: This is minimal in the first two days because of the persistent anaesthetic fluid in the tissue. Mild oral analgesics such as paracetamol are all that are required. Mild tenderness at the site of adits may be felt over 3–5 days. An antibiotic cream (such as fucidic acid or mupirocin) may be prescribed for application at the sites of the adits.
Postoperative oedema over dependent parts (such as legs and genitals) may occur and is due to the inflammation caused by the aspiration movements. It is minimized by using small cannulae and proper postoperative dressings.
Postoperative syncope is common and is vasovagal in origin due to the sudden release of pressure while removing the tight bandages. It is easily avoided by releasing the bandage in the supine position and asking the patient to get up gradually. Mild tenderness is also expected over the adit sites.
Postoperative ecchymoses may occur which usually disappears spontaneously over a week. This is common in hypertensive patients and hence, proper blood pressure control is essential.
Diffuse tenderness and induration can occur if the drainage is improper.
Panniculitis and fat necrosis are rare, but they may occur in diabetics. Hence, it is important to ensure proper diabetic control.
Postoperative infection is rare if proper aseptic precautions are followed.
Seroma formation: Seromas are cystic swellings which occur due to aggressive superficial fat aspiration. They are more common in ultrasound-assisted aspiration but were seen in only two patients encountered by the author.
Irregularity and asymmetry can occur if the amounts of fat aspirated are different in different areas and if pressure garments are not worn properly. This is common over the chest and upper abdomen. It is also common in men treated for gynaecomastia and in patients in whom large cannulae have been used to remove fat quickly.
Pigmentation is common in Indian patients over the adit scars, although none of our patients experienced any keloids.
SAFETY OF TUMESCENT LIPOSUCTION
Several serious complications have been reported with conventional liposuction done under general anaesthesia. These include pulmonary embolism, excessive blood loss, hemorrhagic necrosis of fat, and even, death.[28,29] These complications have been reported mostly in patients in whom liposuction is combined with other procedures such as abdominoplasty, or more than one area have been treated, and in megaliposuctions.
However, these complications are extremely rare in tumescent liposuction and the safety of tumescent liposuction has been well documented in literature. In our experience of 200 cases, no patient had any serious side effect and all patients recovered without any untoward incident. Extensive reviews have been carried out to establish the safety of the procedure and different parameters such as the amount of fat aspirated, type of anaesthesia, facility for surgery, and speciality of operating surgeon have all been studied in large reviews. It is important to note that while mortality has been reported with conventional liposuction, not a single death has been recorded after tumescent liposuction.[1,2,17,30–32] These studies are discussed in detail below.
In a survey of 9478 liposuction cases[31] performed by dermatologic surgeons, the risk of systemic complication was found to be as low as 0.07%. Five patients had “excessive” intra- or postoperative blood loss, and two patients had infection. There were no reported cases of disseminated intravascular coagulation, fat emboli, perforated viscus, thrombophlebitis, or death. The risk of local complications was also small. Of these, the most common were postoperative contour irregularities (2.1%), hematoma (0.47%), and persistent postoperative oedema (46%). A later (1995), more extensive survey of data on 15,336 patients undergoing tumescent liposuction also did not find any serious complications.[32]
In 1999, a study by Coleman determined whether the specialty of the physician had an effect on the incidence of malpractice claims. The study showed that < 1% of the defendants were dermatologic surgeons, even though dermatologic surgeons performed about 33% of liposuctions in the US. In 2002, in a national survey of over 66,000 liposuction cases performed using the tumescent anesthesia technique, no deaths were reported and the rate of serious adverse events was 0.68 per 1000 cases.[33] A review of the State of Florida adverse event data revealed that there were no tumescent anesthesia-related liposuction deaths.[34] In contrast, there were two deaths related to liposuction under general anaesthesia. Safety of office-based liposuction as opposed to hospital-based liposuction too has been well documented. It was found that hospital-based liposuction had three times the rate of malpractice settlements when compared with office-based liposuction surgery.[35–37]
Thus, these data have conclusively established the safety of this procedure, particularly when performed by dermatologic surgeons and as an office-based surgery. Hence, tumescent liposuction is now regarded as the gold standard method for liposuction.
SUMMARY
Tumescent liposuction is a safe and effective procedure when performed in trained hands in a proper setting. Experience and training of surgeon, proper selection of cases, and proper technique in anaesthesia and aspiration are all important to get optimal results. It is important to keep in mind that, as in any cosmetic procedure including liposuction, a final safe and satisfactory result is far more important than quick results.
MULTIPLE CHOICE QUESTIONS
-
Liposuction is performed to remove fat for:
aesthetic purpose
weight reduction
to treat diabetes
all the above
-
In tumescent technique, Klein's fluid contains the following:
pethidine
lignocaine and saline
lignocaine, epinephrine, and saline
lignocaine, epinephrine, saline, steroid
-
The safe upper limit for removing fat in tumescent liposuction is:
1 litre
5 litres
10 litres
any amount
-
The most important feature of tumescent liposuction as opposed to conventional liposuction is:
fluid is introduced into fat
is performed under local anaesthesia
bimodal compression is used
all the above
-
The safe upper limit for dosage in tumescent liposuction is:
6 mg/kg
12 mg/kg
45-55 mg/kg
None of the above
-
Detumescence is necessary to:
allow percolation of fluid through out all layers of fat
allow the patient to relax
allow the surgeon to relax
facilitate metabolism of lignocaine and thus, prevent its toxicity
ANSWERS
1:a, 2:c, 3:b, 4:d, 5:c, 6:a
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Coleman WP, 3rd, Glogau RG, Klein JA, Moy RL, Narins RS, Chuang TY, et al. Guidelines of care for liposuction. J Am Acad Dermatol. 2001;45:438–47. doi: 10.1067/mjd.2001.117045. [DOI] [PubMed] [Google Scholar]
- 2.Lawrence N, Coleman WP. Liposuction. 2002;47:105–8. doi: 10.1067/mjd.2002.122189. [DOI] [PubMed] [Google Scholar]
- 3.Johnson D, Cormack GC, Abrahams PH, Dixon AK. Computed topographic observations on subcutaneous fat: Implications for liposuction. Plast Reconstr Surg. 1996;97:387–96. doi: 10.1097/00006534-199602000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Skouge JW. The biochemistry and development of adipose tissue and pathophysiology of obesity as it relates to liposuction surgery. Dermatol Clin. 1990;8:385–93. [PubMed] [Google Scholar]
- 5.Lawrence N, Coleman WP., 3rd Liposuction. Adv Dermatol. 1996;11:19–49. [PubMed] [Google Scholar]
- 6.Klein JA. Subcutaneous fat: Anatomy and histology. In: Klein JA, editor. Tumescent technique. St Louis: Mosby; 2000. pp. 213–21. [Google Scholar]
- 7.Coleman WP., 3rd The history of liposuction and fat transplantation in America. Dermatol Clin. 1999;17:723–7. doi: 10.1016/s0733-8635(05)70121-2. [DOI] [PubMed] [Google Scholar]
- 8.Klein JA. The tumescent technique for liposuction surgery. AM J Cosmetic Surg. 1987;4:1124–32. [Google Scholar]
- 9.Klein JA. Tumescent technique for local anesthesia improves safety in large-volume liposuction. Plast Reconstr Surg. 1993;92:1085–98. [PubMed] [Google Scholar]
- 10.Courtiss EH, Choucair RJ, Donelan MB. Large-volume suction lipectomy: An analysis of 108 patients. Plast Reconstr Surg. 1992;89:1068–79. [PubMed] [Google Scholar]
- 11.Mandel MA. Blood and fluid replacement in major liposuction procedures. Aesthet Plast Surg. 1990;14:187–91. doi: 10.1007/BF01578347. [DOI] [PubMed] [Google Scholar]
- 12.Coleman WP. Powered liposuction. Dermatol Surg. 2000;26:315–8. doi: 10.1046/j.1524-4725.2000.99240.x. [DOI] [PubMed] [Google Scholar]
- 13.Narins R, Coleman WP, 3rd, Brody H, Goldman M, Hanke CW, Lillis PJ, et al. Statement on ultrasonic liposuction: Task force on ultrasonic liposuction of the American society for dermatologic surgery. Dermatol Surg. 1998;24:1035. [PubMed] [Google Scholar]
- 14.Lillis PJ, Coleman WP. Liposuction for treatment of axillary hyperhidrosis. Dermatol Clin. 1990;8:479–82. [PubMed] [Google Scholar]
- 15.Pinski KS, Roenigk HH. Liposuction of lipomas. Dermatol Clin. 1990;8:483–92. [PubMed] [Google Scholar]
- 16.Klein JA. Anesthetic formulation of tumescent solutions. Dermatol Clin. 1999;17:751–9. doi: 10.1016/s0733-8635(05)70124-8. [DOI] [PubMed] [Google Scholar]
- 17.Klein J. Two standards of care for tumescent liposuction. Dermatol Surg. 1997;23:1194–5. doi: 10.1111/j.1524-4725.1997.tb00473.x. [DOI] [PubMed] [Google Scholar]
- 18.Klein JA. Clinical pharmacology. In: Klein JA, editor. Tumescent technique. St Louis: Mosby; 2000. pp. 121–209. [Google Scholar]
- 19.Lillis PJ. Liposuction surgery under local anesthesia: Limited blood loss and minimal lidocaine absorption. J Dermatol Surg Oncol. 1988;14:1145–8. doi: 10.1111/j.1524-4725.1988.tb03472.x. [DOI] [PubMed] [Google Scholar]
- 20.Ostad A, Kageyama N, Moy RL. Tumescent anesthesia with a lidocaine dose of 55 mg/kg is safe for liposuction. Dermatol Surg. 1996;22:921–7. doi: 10.1111/j.1524-4725.1996.tb00634.x. [DOI] [PubMed] [Google Scholar]
- 21.Flynn TC, Narins RS. Preoperative evaluation of the liposuction patient. Dermatol Clin. 1999;17:729–34. doi: 10.1016/s0733-8635(05)70122-4. [DOI] [PubMed] [Google Scholar]
- 22.Bank DE, Perez MI. Skin retraction after liposuction in patients over the age of 40. Dermatol Surg. 1999;25:673–6. doi: 10.1046/j.1524-4725.1999.99105.x. [DOI] [PubMed] [Google Scholar]
- 23.Matarasso A, Matarasso SL. When does your liposuction patient require an abdominoplasty? Dermatol Surg. 1997;23:1151–60. doi: 10.1111/j.1524-4725.1997.tb00465.x. [DOI] [PubMed] [Google Scholar]
- 24.Klein JA. Microcannulas. In: Klein JA, editor. Tumescent technique. St Louis: Mosby; 2000. pp. 235–48. [Google Scholar]
- 25.Bernstein G. Instrumentation for liposuction. Dermatol Clin. 1999;17:735–49. doi: 10.1016/s0733-8635(05)70123-6. [DOI] [PubMed] [Google Scholar]
- 26.Klein JA. Post-liposuction care: Open drainage and bimodal compression. In: Klein JA, editor. Tumescent technique. St Louis: Mosby; 2000. pp. 281–93. [Google Scholar]
- 27.Klein JA. Post-tumescent liposuction care: Open drainage and bimodal compression. Dermatol Clin. 1999;17:881–90. doi: 10.1016/s0733-8635(05)70135-2. [DOI] [PubMed] [Google Scholar]
- 28.Rao RB, Ely SF, Hoffman RS. Deaths related to liposuction. N Engl J Med. 1999;340:1471–5. doi: 10.1056/NEJM199905133401904. [DOI] [PubMed] [Google Scholar]
- 29.Yoho RA, Romaine J, O’Neil D. Review of liposuction, Abdminoplasty, and facelift Mortality and Moribidity risk literature. J Dermatol Surg. 2005;31:733–743. doi: 10.1097/00042728-200507000-00001. [DOI] [PubMed] [Google Scholar]
- 30.Venkataram J, Venkataram M. Microcannular tumescent liposuction. Indian J Dermatol Venerol Leprol. 2007;73:377–83. doi: 10.4103/0378-6323.37053. [DOI] [PubMed] [Google Scholar]
- 31.Bernstein G, Hanke CW. Safety of liposuction: A review of 9,478 cases performed by dermatologists. J Dermatol Surg Oncol. 1988;14:1112–4. doi: 10.1111/j.1524-4725.1988.tb03467.x. [DOI] [PubMed] [Google Scholar]
- 32.Hanke CW, Bernstein G, Bullock S. Safety of tumescent liposuction in 15,336 patients: National survey results. Dermatol Surg. 1995;21:459–62. doi: 10.1111/j.1524-4725.1995.tb00213.x. [DOI] [PubMed] [Google Scholar]
- 33.Housman TS, Lawrence N, Mellen BG, George MN, Filippo JS, Cerveny KA, et al. The safety of liposuction: Results of a national survey. Dermatol Surg. 2002;28:971–8. doi: 10.1046/j.1524-4725.2002.02081.x. [DOI] [PubMed] [Google Scholar]
- 34.Coldiron B. Office surgical incidents: 19 months of Florida data. Dermatol Surg. 2002;28:710–3. doi: 10.1046/j.1524-4725.2002.02016.x. [DOI] [PubMed] [Google Scholar]
- 35.Coleman WP, 3rd, Hanke CW, Lillis P, Bernstein G, Narins R. Does the location of the surgery or the specialty of the physician affect malpractice claims in liposuction? Dermatol Surg. 1999;25:343–7. doi: 10.1046/j.1524-4725.1999.09015.x. [DOI] [PubMed] [Google Scholar]
- 36.Coldiron B, Schreve E, Balkrishnan R. Patient injuries from surgical procedures performed in medical offices: Three years of Florida data. Dermatol Surg. 2004;30:1435–43. doi: 10.1111/j.1524-4725.2004.30500.x. [DOI] [PubMed] [Google Scholar]
- 37.Hancox JG, Venkat AP, Hill A, Graham GF, Williford PM, Coldiron B, et al. Why are there differences in the perceived safety of office-based surgery? Dermatol Surg. 2004;30:1377–9. doi: 10.1111/j.1524-4725.2004.30432.x. [DOI] [PubMed] [Google Scholar]


