Abstract
Dermatologic surgery and aesthetic dermatology are rapidly emerging and expanding specialties in India. However, dermatologists practicing surgeries and aesthetics in India represent a highly selected group and are mostly confined to metros. Dermatologists in the peripheral and remote regions need to reach these specialists for the benefit of their patients and teledermatology is an invaluable tool for this purpose. Video-conference, store and forward, Satellite communication, Hybrid teledermatology, mobile teledermatology, Integration model, nurse-led teledermatology, teledermatology focusing difficult-to-manage cases, screening and triage services are the various teledermatology services developed to suit the needs of dermatology care from a distance. Types of teledermatology service, pattern of net work connectivity and purpose of dermatology service are the three cardinal parameters for management of the dermatoses from a distance. This article reviews the literature, and analyzes the possible options available for a teledermatosurgery practice.
Keywords: Dermatosurgery, teledermatology, dermatopathology, dermatology
INTRODUCTION
Consultation is seeking an expert opinion. Expert opinion obtained for medical purpose from a distance is called Telemedical consultation. The distance can be between the continents, countries, states, cities or even doctors a few meters apart. World health organization defines telemedicine as practice of health care using interactive audio, visual, and data communications. In 1995 Prednia and co-workers[1] introduced the term ‘Teledermatology’ (TD) and in 1997, Zelickson and Homan[2] first demonstrated video conference teledermatology in their nursing home setting. TD is a subset of telemedicine that incorporates telecommunications technologies (information technology) to deliver dermatology services at a distance. The common principle of TD services is to reach the unreached for dermatology care.
Telemedicine reduces travel, waiting time, treatment cost, minimizes follow-up visits and helps to deliver specialty health care services to remote geographic regions. Dermatology is a Visual specialty; Image is the gold standard for dermatological diagnosis.[3] Chronic disorders that require a long duration of treatment need frequent monitoring and several followup visits. It involves travel expenses, and also a prolonged waiting time. These the above circumstances have made dermatology an ideal specialty for telemedical applications and it is not suprising that dermatologists have been early adopters for Tele medical applications.[4]
TD delivers screening and triage services in Melanoma and pigmented skin lesions.[3] TD can be used for screening, triage and select patients for dermatosurgery practice. TD delivers treatment and follow-up care in leg ulcers and to discuss difficult -to-manage cases like the Inflammatory and neoplastic conditions[5] from worldwide experts and Education of health care professionals and patients. It is observed to achieve 81% concordance for exchanging opinions on challenging inflammatory and skin neoplasm’s.[5]
CLASSIFICATION
Different teledermatological tools available are [Figure 1]:
Figure 1.
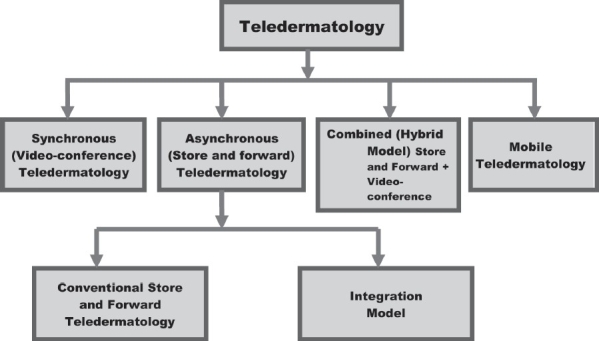
Various teledematological tools
Real time or videoconference
Video consultation uses video-conferencing equipment to connect the patient, often with their general practitioner (GP) or nurse present, with a distant consultant. The evaluation of diagnostic accuracy varies between 67-80% compared to face-to-face consultation.[6] Initial studies on economic evaluation of interactive teledermatology compared to face-to-face consultation considered video conference to be expensive. However more recent studies[7] have confirmed it to be economical. This is due to the improved technology and decrease in the hardware cost. Table 1 summarizes the various types of videoconference (VC) available for practice.
Table 1.
Type of videoconference, their components and cost-effectiveness while setting a video conference teledermatology center[16]
| Type | Components | Cost |
|---|---|---|
| Stand-alone VC | Video codec with built in camera (pan, tilt and zoom), built in micro phone and audio-video interfaces to connect line/network interface ISDN/LAN | Expensive |
| PC based VC with PC add-on card codec | PC, web camera with built in microphone with audio/video output to connect ISDN/LAN | Moderately expensive |
| PC based VC with In-Camera codec* | Built in video-camera is connected to the PC through USB port. | Less expensive |
| PC based VC Using web camera And software* | Video codec function (audio-video compression and data formatting) is done using software loaded on PC. | Cheapest |
| A web camera is connected to PC using a USB port. |
To connect to multimedia projector and achieve large display VGA/XVGA out put of the PC may be used. (Reproduced with permission Kanthraj GR and Srinivas CR. Ind J Dermatol Venerol Leprol 2007; 73:5-12.)
Satellite communication net work (Satcom) is an Indian space research organization (ISRO) initiative to reach the unreached and inaccessible remote geographic regions where connectivity cannot be established is achieved through satellite connectivity.[8] Skin camps are organized by mounting SATCOM on a bus or a van that travels to those remote geographic regions where Integrated services digital network (ISDN) connection cannot be established and establishes satellite net work connectivity with a tertiary center[9] and delivers dermatology care.
Store and forward system
The store and forward (SAF) stores patient data (digital images, clinical and demographic information) sent by GP’s in an electronic medium for future access by consultants in referral centers to deliver the quality health care in remote geographic regions. SAF involves transmission of digital images and asynchronous evaluation is practiced. Simultaneous presence of the health care professional is not required. About 80-90% of dermatological conditions may be diagnosed by SAF TD.[10] It is the most commonly used technology. There is 60–80% total agreement and 70-90% partial agreement when in person diagnosis is compared to both real time (synchronous) and SAF TD.[10] Various feasibility studies on SAF TD are summarized in Table 2 and it has been found to be cheap, easy to set up and practice.
Table 2.
Feasibility studies involving store and forward and mobile (cellular) teledermatology practice
| Author/Year | Contribution | Device | Model | Charge couple device reskolution (mege pixles) | Image resolution (pixles) | Storage (JPEG)KB | Diagnosis agreement* % |
|---|---|---|---|---|---|---|---|
| Whited et al.[11], 1999 | Store and forward of skin lesions | Digital camera | - | - | 1280×1000 | 68 | |
| High et al.[12], 2000 | Store and forward of skin lesions | Digital camera | Sony DSC – F1 | - | 640×480 | - | 89 |
| Sony Corporation Newyork | |||||||
| Tucker et al.[13], 2005 | Digital imaging of skin lesions for teleconsultation | Digital camera | Fuji-film MX-1700 | - | 640×480 | 32MB | 58 |
| Mahendran et al.[14], 2005 | Digital imaging and teleconsultation of skin malignancies | Digital camera | Coolpix 950 Nikon Corporation | - | 1200×1600 | - | 48 |
| Salmhofer et al.[15], 2005 | Digital camera in wound teleconsultation | Digital camera | Coolpix995 Nikon Corporation | 3.3 | 2048×1536 | 1500 | 87 |
| Braun et al.[20], 2005 | Cellular phone in telemedical wound care | Cellular phone | Nokia 7650 Espoo, Finland | - | 640×480 | 15-22 | 82 |
| Massone et al.[21], 2005 | Cellular Phone in teledermatology | Cellular phone | Nokia 7650 Espoo, Finland | - | 640×480 | 13-35 | 70 |
| Massone et al.[22], 2006 | Personal digital assistants in teledermatology | Personal digital assisstants | Sony Clie PEG – NZ90, Tokyo, Japan | 2 | 1200×1600 | 829-989 | 79 |
Compared to face to face consultation (Gold Standard)
Low cost electronic equipments, quick electronic transfer of high quality digital images and universal access to the health care workers enhance the practice of SAF. SAF uses digital camera with an average 640 × 480 pixels image resolution. Different diagnosis agreement rates (of 68%,[11] 89%,[12] 58%[13] and 48%[14]) have been documented in various studies. The images are rapidly transferred[6] and stored in JPEG (Joint photographers expert group; http://www.jpeg.org) format using the internet. Poor image quality and lack of referral proforma data may lead to poor agreement.[14] Telemedical wound care and follow up uses digital camera with a good agreement to face-to-face, which is regarded as the Gold standard.[15]
A referral hospital can have a fixed time on a day depending on the caseload for a teledermatology clinic to prevent unnecessary delay. General practitioner can send history with photograph well in advance. Relevant discussions are made, as both ends are prepared. Patient, general practitioners or nurse available in the given period, interacts by e-chat or web cam or voice mail for any clarifications required from the consultant. This approach has been recommended while offering periodic follow-up care.[16] SAF provides patient, referring clinician and dermatologist satisfaction.[7] Referring clinician has an additional advantage of educational benefit.[7]
Data transmission medium: The Internet, Wi-Fi and Wi-Max
Digital lines to enhance data transmission are called ‘Integrated services digital network’ (ISDN). Increase in the number of ISDN line increases the data carrying capacity or bandwidth from 128 kbps (one ISDN line) to 256 and 384 kbps (two and three ISDN lines) respectively.[6]
Wi-fi[16] and Wi-Max[16] are super speed wireless network connections that enable high-speed transmission of the data. Wi-Fi (wireless fidelity) enables wireless local area network (WLAN) connections to mobile devices, digital camera, PC computers and personal digital assistants.[16] There devices are with Wi-Fi built in, while others require adding a Wi-Fi network card. Wi-fi uses radio-waves, radio transmitters called routers with receivers (access points / hot spots). Superior to Wi-Fi is Wi-Max (worldwide interoperability for micro wave access). It is a broadband wireless access technology providing super speed Internet access at 70mbit/s. Images may be received in large number by referral hospital during a clinical trial or teleconsultation. Speed of the transfer medium is important for rapid and easy retrieval of large data. Therefore, a telemedical center should have Wi-Fi or Wi-Max installation for Quality and Speed of data transmission.[16]
Hybrid model
The combination of SAF TD in the first step, followed by VC TD in the second step is called Hybrid TD.[17,18] It saves time, clarifies doubts and avoids misinterpretation from both the ends. This process achieves best physician and patient satisfaction.
Mobile or cellular teledermatology
Portable devices like cellular phones and personal digital assistants provides inbuilt camera to capture digital images, computing, and net working features to deliver dermatology care at a distance. They provide immediate image access and direct interaction and it is possible to obtain clarification. Periodic evaluation of leg ulcers and skin images using cellular phones and Personal digital assistants are practiced. Quality and speed of image transmission is no longer an obstacle. Melanoma screening with cellular phones using mobile teledermocscopy revealed a diagnostic agreement of 90% compared to face-to-face consultation.[19]
Cellular phones[20,21] and Personal digital assistants[22,23] allow taking good quality images and sending them to the expert from remote geographic regions via a wireless network e.g., global system for mobiles (GSM) and universal mobile telecommunication system (UMTS). New generation cellular phones allow to take good quality images and transmit them directly to other cellular phones (via multimedia messages) and computers (via e-mail or blue tooth-wireless connection) the diagnosis agreement is 82% compared to face-to-face consultation.[20] A feasibility study[20] confirmed the importance of cellular phone in telemedical wound care. Transfer of skin images using cellular phones with a diagnosis agreement of 70% is documented.[21] Various feasibility studies on mobile TD are summarized in Table 2.
Personal digital assistants
Laptops, hand held computers are convenient to handle and offer combined features like camera, computing, and networking are called personal digital assistants.[22,23] They are convenient for health care professionals to capture and transfer the images. Massone et al,[22] demonstrated the importance of personal digital assistants in teledermatology with a 79% diagnosis agreement.
Diagnostic agreement is low for cutaneous malignancies when there is poor quality of images, and lack of referral proforma data.[14] Recent studies[24] have proved that digital photography gives such a high image quality, that a neoplastic lesion that cannot be diagnosed with a high quality digital image, rarely could be diagnosed with face -to -face consultation.[24] Advances in digital imaging and internet solutions have overcome technical limitations.[3] Teleconsultation applied as a screening method for malignant tumors is a useful technique that can be incorporated in dermatology for day- to- day practice.[24]
Integration model
Health care professionals in rural areas are the’ eyes’ for the expert. For the expert to guide them, deliver follow up and monitor the progress they should have a periodic audit of visual parameters and dimensions.This has been demonstrated in the treatment and follow up of leg ulcers. Various authors[25–31] have demonstrated the effectiveness of computerized measurements of leg ulcers to monitor therauptic assessment.
The systematic functional integration of electronic devices and software to capture, transfer, store, measure and deliver follow-up care is the principle of integration model and has been used effectively for leg ulcers in remote geographic regions.[32] It is illustrated in the [Figure 2]. In step 1 close up image of the ulcer with the surrounding skin is suitable for teleconsultation.[6] The images are captured, irrespective of its site either by digital or cellular phones camera [Figure 2]. In step 2 images are transferred via e-mail. In Step 3 calculations of wound margins (area and perimeter) is done by Computer Aided Design software (CAD). In Step 4 the software professional delivers the result. Periodic evaluation is performed. Bizarre shaped lesions at any site are measured accurately and stored. It is useful for forensic experts to reproduce at the time of expert evidence.
Figure 2.
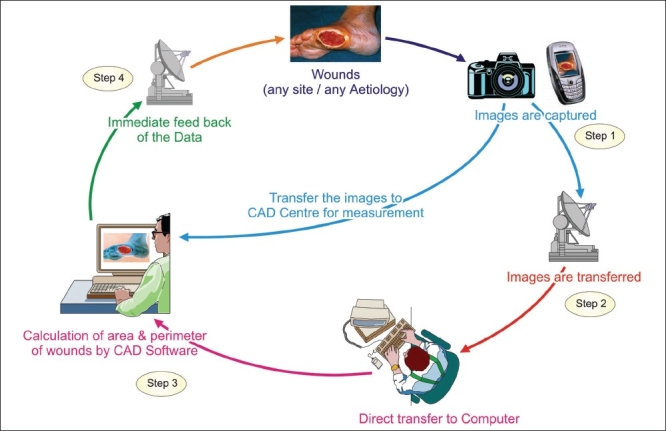
The integration model to capture, transfer, measure and follow-up of skin lesions to deliver SAF teledermatology care[32] (Reproduced with permission from American Medical Association, Kanthraj GR. Arch Dermatol 2005;141:1470-71)
Immediate access of visual parameters and measurement of lesions are achieved. Routine follow- up care in a remote area under close supervision of higher center is performed. Computerized measurements are rapid, easy, and precise and suited for SAF TD.[16,32] This approach enables diagnosis, management, and periodic assessment of leg ulcers and delivers follow-up care to achieve physician and Patient satisfaction. Repigmented vitiligo can be serially monitored after medical or surgical treatment.[26] Serial monitoring of the images and determination of their dimensions and percentage of pigmentation documents the progress of re-pigmentation.
The system automatically plots wound healing regression or vitiligo repigmentation on the computerized graph. Rapid capture, transfer and calculation with negligible human intervention minimizing inter observer and intra observer variations are achieved.[32] The programmer does the calculation and provides the results to dermatologists at telemedical center. Computer professionals process the large data without any additional burden to the experts. All health care professionals at a tertiary centre utilize the software in a centralized location maximizing SAF telemedical center’s utility and generalizability.[27]
APPLICATIONS OF TELEDERMATOLOGY
Teledermatological monitoring of leg ulcers
SAF and mobile TD play a key role in leg ulcer management. It is a chronic disorder that requires frequent and periodic monitoring. Patient needs frequent visits from a Long distance incurring huge costs. It can be more distressing in elderly as leg ulcer is known to occur more frequently requiring prolonged waiting time. HCP needs to be trained for digital photography, uploading, web application and wound care. 90% of images for consultation are excellent.[33] Good response is observed in 70% of cases with a good patient and physician satisfaction.[33] SAF and mobile TD hold a great potential for long term wound care along with the Co-operation with home care nurses.[25] Leg ulcers are monitored for slough, necrosis and granulation tissue formation.[15] In a recent study the feasibility and acceptance of teledermatology for wound management has been demonstrated.[34] Consultant personally examined, assessed, classified and recommended the medications for the ulcers in the initial visit. Follow up visits were done by the home care nurses using SAF TD.. In 90% of teleconsultations qualities of images were good with good physician and patient satisfaction.[33]
Teledermatopathology
Teledermatopathology is an important area for application of telemedicinal tools.[35–37] Teledermatopathology involves transmission of images from distant locations to consulting dermatopathologists. It is of relevance to the Indian scenario where there are only a few dermatopathologists and even general histopathologists are available only in citiis. Teledermatopathology is achieved by a) video- image (dynamic) analysis b) store and forward (static) c) and virtual slide system (VSS).[35]
VSS is a recently developed technology wherein using a robotic microscope, any field of the specimen is magnified at the discretion of the dermato-pathologist. VSS stores the images on a virtual slide server available on the web.[36] VSS is being used for the diagnosis of pigmented skin lesions, difficult- to-manage cases and inflammatory skin diseases. Though more expensive than the store and forward system, VSS represents the future in this discipline. A study[36] investigated the role of teledermatopathology by VSS in forty-six biopsy specimens from inflammatory skin diseases. Telediagnoses agreed with gold standard and conventional diagnosis with an average of 73% and 74%, respectively.[36] Complete concordance among all teleconsultants with gold standard and conventional diagnosis was found in 20% of the cases. The study concluded that the system is not fully suitable for diagnosis of inflammatory dermatoses, as the diagnosis and interpretation often depends on availability of complete clinical data and because of the intrinsic difficulties in diagnosis of such diseases. This is of particular relevance to Indian situation where most biopsies are performed for inflammatory diseases and where skin cancer is less prevalent. Recent concept of Hybrid teledermatopthology[37] incorporates the advantages of both dynamic and virtual slide system and over comes the individual shortcomings. It consists of motorized microscopes with remote control and scanner for slide digitization.
Teledermatology in Cutaneous aesthetic surgery
SAF can be used to screen and determine the suitability of the lesion for treatment by dermatosurgery. Some examples include conditions such as keloids, hemangiomas, scars, vitiligo lesions for grafting, hirsutism for laser assisted hair reduction, ageing changes of skin and images of scalp for hair transplantation etc. VC can also be used for pre-surgery counseling for aesthetic procedures. VC increases patient satisfaction as patient directly interacts with the aesthetic surgeon for any clarifications. Selected centers can have Hybrid teledermatology to screen patients for procedures and counseling for aesthetic procedure. Mobile teledermatology is used to screen and deliver follow-up care after aesthetic surgery. Integration model[32] finds its application in objective assessment after medical or surgical treatment of vitiligo and leg ulcers. Types of tedermatology service, purpose and area of application and their potential use in aesthetic surgery are summarized in Table 3.
Table 3.
Types of teledermatology service, purpose, area of application and their potential use in dermatosurgery
| Type of teledermatology service | Purpose | Dermatoses/Area of application |
|---|---|---|
| Hybrid model (Combination) | Incorporates the advantages of both synchronous and asynchronous teledermatology | Routine teledermatology service and follow-up care |
| Conventional store and forward teledermatology | Screening | To determine the suitability for a dermto-surgery |
| Video-conference teledermatology | Counseling and Education | Pre surgery counseling |
| Integration model | Follow-up care after medical or surgical treatment | Leg ulcers and vitiligo |
| Mobile or cellular teledermatology | Sreening and follow-up care after dermatosurgeries | Leg ulcers, vitiligo or any dermatosurgery procedure |
Nurse-led teledermatology service
Training of Health care professionals for TD practice at all levels in basics of dermatology including computer knowledge, art of counseling, history taking skills, filling the Performa, photography and Video clips. Administration of intralesional steroids, training for skin biopsies, removal of skin tags, cryosurgery and other simple dermatosurgical techniques are taught.[38] Interprofessional collaborative working environment to share the expertise in decision making is promoted. A nurse advice the management guided by consultants, motivates and delivers for follow-up care. They understand the physical, psychological and social effects of skin disease.[39]
Counseling
Preparing the patient for TD practice by educating the dermatoses, the technology adopted and its limitations involved in delivering dermatology care. Medical reimbursement equivalent to that of the traditional face-to-face examination in an approved rural health care setting are practiced.[18]
Imaging and law
Photographs form important medico-legal evidence and play a vital role in maintenance of the dermatology records.[40] It has its special significance as digital images are used to capture, store, measure, transfer and deliver follow up care. The image measurement is important for periodic follow-up care and medico-legal expert opinion. US Federal courts have ruled that digital images can furnish sufficient medical data to provide dermatological care.[40] Preservation of privacy and confidentiality of digital images in the era of teledermatology is important.[3,41] In difficult- to-manage Case or in doubt, a dermatologist can be sued for a wrong diagnosis. “One cannot take shelter on the pretext of a teledermatology consultation.” A principle of traditional consultation applies to TD care.[6] In case of doubt a dermatologist should call for face-to-face examination and investigates on priority. They should obtain written consent from patient to store and forward the images. Confidentiality of Images has to be maintained.[6]
FUTURE DIRECTIONS
Health access barriers, poverty, large geographic regions and deficiency of dermatologists in rural regions have increased the needs of the TD service in India. A Proper reimbursement and insurance policies need to be implemented for teledermatology consultation and surgery. Training the existing nurses for digital photography, internet applications and computing needs to be implemented. Mobile TD finds its application and active survey is carried out by HCP using cellular phones to screen the dermatoses. Teleconsultation is an effective alternative and should be considered when a service is under pressure.[42] Incorporation of telemedicine and nurse led telemedicine effectively in rural India can enhance delivery of health care. Academic bodies have to introduce telemedicine education in medical and nursing training. House surgery period in undergraduate education should be made to used train telemedicine and thereyby offer service to rural India.
CONCLUSION
TD research is progressing in an arithmetic ratio (in additions) while advancement in information technology is progressing in geometric ratio (in multiples).[16] Dermatosugoens need to explore the feasibility of technology application in the interest of the patient and conduct studies. They need to work along with their respective Government, Ministry of Health and national health services of their regions to formulate clinical, technical and administrative standards to facilitate expansion of teledermatology in practice and introduce it as a curriculum in medical education. There is need to to accelerate research and adopt innovative techniques to deliver quality health care to remote geographic regions and achieve the goal to reach the unreached.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Perednia DA, Allen A. Telemedicine technology and clinical applications. JAMA. 1995;273:483–8. [PubMed] [Google Scholar]
- 2.Zelickson BD, Homan L. Teledermatology in the nursing home. Arch Dermatol. 1997;133:171–4. [PubMed] [Google Scholar]
- 3.Di Stefani A, Zalaudek I, Argenziano G, Chimenti S, Soyer HP. Feasibility of a two-step teledermatologic approach for the management of pigmented skin lesions. Dermatol Surg. 2007;33:686–92. doi: 10.1111/j.1524-4725.2007.33144.x. [DOI] [PubMed] [Google Scholar]
- 4.Eminović N, de Keizer NF, Bindels PJ, Hasman A. Maturity of teledermatology evaluation research: A systematic literature review. Br J Dermatol. 2007;56:412–9. doi: 10.1111/j.1365-2133.2006.07627.x. [DOI] [PubMed] [Google Scholar]
- 5.Lozzi GP, Soyer HP, Massone C, Micantonio T, Kraenke B, Forgnoli MC, et al. The additive value of second opinion teleconsulting in the management of patients with challenging inflammatory, neoplastic skin diseases: A best practice model in dermatology? J Eur Acad Dermatol Venereol. 2007;21:30–4. doi: 10.1111/j.1468-3083.2006.01846.x. [DOI] [PubMed] [Google Scholar]
- 6.Eedy DJ, Wootton R. Teledermatology: A review. Br J Dermatol. 2001;144:696–707. doi: 10.1046/j.1365-2133.2001.04124.x. [DOI] [PubMed] [Google Scholar]
- 7.Whited JD. Teledermatology research review. Int J Dermatol. 2006;45:220–9. doi: 10.1111/j.1365-4632.2004.02427.x. [DOI] [PubMed] [Google Scholar]
- 8.Sathyamurthy LS, Bhaskaranarayana A. Telemedicine: Indian space agency's (ISRO) initiatives for specialty to remote and rural population. In: Sathyamurthy LS, Murthy RL, editors. Telemedicine manual guide book for practice of telemedicine. 1st ed. Bangalore: Indian space research organization, department of space. Government of India; 2005. pp. 9–13. [Google Scholar]
- 9.Feroze K. Teledermatology in India: Practical implications. Indian J Med Sci. 2008;62:208–14. [PubMed] [Google Scholar]
- 10.Heinzelmann PJ, Williams CM, Lugn NE, Kvedar JC. Clinical outcomes associated with telemedicine / telehealth. Telemedicine journal and E-Health. 2005;11:329–47. doi: 10.1089/tmj.2005.11.329. [DOI] [PubMed] [Google Scholar]
- 11.Whited JD, Hall RP, Simel DL, Foy ME, Stechuchak KM, Drugge RJ, et al. Reliability and accuracy of dermatologists clinic – based and digital image consultations. J Am Acad Dermatol. 1999;41:693–702. doi: 10.1016/s0190-9622(99)70003-4. [DOI] [PubMed] [Google Scholar]
- 12.High WA, Houston MS, Calobrisi SD, Drage LA, McEvoy MT. Assessment of the accuracy of low- cost store and forward teledermatology consultation. J Am Acad Dermatol. 2000;42:776–83. doi: 10.1067/mjd.2000.104519. [DOI] [PubMed] [Google Scholar]
- 13.Tucker WFG, Lewis FA. Digital imaging: A diagnostic screening tool? Int J Dermatol. 2005;44:479–81. doi: 10.1111/j.1365-4632.2005.01990.x. [DOI] [PubMed] [Google Scholar]
- 14.Mahendran R, Goodfield MJ, Sheehan-Dare RA. An evaluation of the role of a store -and –forward teledermatology system in skin cancer diagnosis and management. Clin Exp Dermatol. 2005;30:209–14. doi: 10.1111/j.1365-2230.2005.01735.x. [DOI] [PubMed] [Google Scholar]
- 15.Salmhofer W, Hofmann-wellenhof R, Gobler G, Rieger-Engelbogen K, Gunegger D, Binder B, et al. Wound teleconsultation in patients with chronic leg ulcers. Dermatology. 2005;210:211–7. doi: 10.1159/000083512. [DOI] [PubMed] [Google Scholar]
- 16.Kanthraj GR, Srinivas CR. Store and forward teledermatology. Indian J Dermatol Venerol Leprol. 2007;73:5–12. doi: 10.4103/0378-6323.30643. [DOI] [PubMed] [Google Scholar]
- 17.Fieleke DR, Edison K, Dyer JA. Pediatric teledermatology: A survey of current use. Pediatr Dermatol. 2008;25:158–62. doi: 10.1111/j.1525-1470.2008.00624.x. [DOI] [PubMed] [Google Scholar]
- 18.Edison KE, Dyer JA. Teledermatology in Missouri and beyond. Mol Med. 2007;104:139–43. [PubMed] [Google Scholar]
- 19.Massone C, Hofmann-Wellenhof R, Ahlgrimm-Siess V, Gabler G, Ebner C, Soyer HP. Melanoma screening with cellular phones. PLoS One. 2007;2:e483. doi: 10.1371/journal.pone.0000483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Braun RP, Vecchietti JL, Thomas L, Prins C, French LE, Gewirtzman AJ, et al. Telemedical wound care using a new generation of mobile telephones: A feasibility study. Arch Dermatol. 2005;141:254–8. doi: 10.1001/archderm.141.2.254. [DOI] [PubMed] [Google Scholar]
- 21.Massone C, Lozzi GP, Wurm E, Hofmann-Wellenhof R, Schoellnast R, Zalaudek I, et al. Cellular phones in clinical teledermatology. Arch Dermatol. 2005;141:1319–20. doi: 10.1001/archderm.141.10.1319. [DOI] [PubMed] [Google Scholar]
- 22.Massone C, Lozzi GP, Wurm E, Hofmann-Wellenhof R, Schoellnast R, Zalaudek I, et al. Personal digital assistants in teledermatology. Br J Dermatol. 2006;154:801–2. doi: 10.1111/j.1365-2133.2006.07175.x. [DOI] [PubMed] [Google Scholar]
- 23.Scheinfeld NS. Creating and utilizing multi media dermatology medical record for pocket PC personal digital assistant. Skin Med. 2005;4:33–7. doi: 10.1111/j.1540-9740.2005.03144.x. [DOI] [PubMed] [Google Scholar]
- 24.Martinez-Garcia S, Odelboz-Gonzalez J, Martin-Gonzalez T, Samaniego-Gonzalez E, Crespo-Erchiga V. Teledermatology. Review of 917 Teleconsults. Actas Dermosifiliogr. 2007;98:318–24. [PubMed] [Google Scholar]
- 25.Coleridge Smith PD, Scurr JH. Direct method of measuring venous ulcers. Br J Surg. 1989;76:689. doi: 10.1002/bjs.1800760712. [DOI] [PubMed] [Google Scholar]
- 26.Kanthraj GR, Srinivas CR, Shenoi SD, Suresh B, Ravikumar BC, Deshmukh RP. Wound measurement by Computer Aided Design (CAD): A practical approach for software utility. Int J Dermatol. 1998;37:714–5. doi: 10.1046/j.1365-4362.1998.00438.x. [DOI] [PubMed] [Google Scholar]
- 27.Kanthraj GR. Computer or simple wound measurements: When Greek meets Greek, then comes the Tug-of-war. Arch Dermatol. 1999;135:992–4. doi: 10.1001/archderm.135.8.992. [DOI] [PubMed] [Google Scholar]
- 28.Rajbhandari SM, Harris ND, Sutton M, Lockett C, Eaton S, Gadour M, et al. Digital imaging: An accurate and easy method of measuring foot ulcers. Diabetes Med. 1999;16:339–42. doi: 10.1046/j.1464-5491.1999.00053.x. [DOI] [PubMed] [Google Scholar]
- 29.Samad A, Hayes S, French L, Dodds S. Digital imaging versus conventional contact tracing for the objective measurement of venous leg ulcers. J Wound Care. 2002;11:137–40. doi: 10.12968/jowc.2002.11.4.26385. [DOI] [PubMed] [Google Scholar]
- 30.Moore K. Using wound area measurement to predict and monitor response to treatment of chronic wounds. J Wound Care. 2005;14:229–32. doi: 10.12968/jowc.2005.14.5.26771. [DOI] [PubMed] [Google Scholar]
- 31.Solomon C, Munro AR, Vanrij AM, Christie R. The use of video image analysis for the measurement of venous ulcers. Br J Dermatol. 1995;133:565–70. doi: 10.1111/j.1365-2133.1995.tb02706.x. [DOI] [PubMed] [Google Scholar]
- 32.Kanthraj GR. The integration of the internet, mobile phones, digital photography and computer aided design software to achieve telemedical wound measurement and care. Arch Dermatol. 2005;141:1470–1. doi: 10.1001/archderm.141.11.1470. [DOI] [PubMed] [Google Scholar]
- 33.Binder B, Hofmann-Wellenhof R, Salmhofer W, Okcu A, Kerl H, Soyer HP. Teledermatological monitoring of leg ulcers in cooperation with home care nurses. Arch Dermatol. 2007;143:1511–4. doi: 10.1001/archderm.143.12.1511. [DOI] [PubMed] [Google Scholar]
- 34.Hofmann-Wellenhof R, Salmhofer W, Binder B, Okeu A, Kerl H, Soyer HP. Feasibility and acceptance of telemedicine for wound care in patients with chronic leg ulcers. J Telemed Telecare. 2006;12:15–7. doi: 10.1258/135763306777978407. [DOI] [PubMed] [Google Scholar]
- 35.Massone C, Brunasso AM, Campbell TM, Soyer HP. State of the art of teledermato pathology. Am J Dermatopathol. 2008;30:446–50. doi: 10.1097/DAD.0b013e3181822057. [DOI] [PubMed] [Google Scholar]
- 36.Massone C, Peter Soyer H, Lozzi GP, Di Stefani A, Leinweber B, Gabler G, et al. Feasibility and diagnostic agreement in teledermatopathology using a virtual slide system. Hum Pathol. 2007;38:546–54. doi: 10.1016/j.humpath.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 37.Mencarelli R, Marcolongo A, Gasparetto A. Organizational model for a telepathology system. Diagn Pathol. 2008;3:57. doi: 10.1186/1746-1596-3-S1-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Armstrong AW, Dorer DJ, Lugn NE, Kvedar JC. Economic evaluation of interactive teledermatology compared with conventional care. Telemed J E Health. 2007;13:91–9. doi: 10.1089/tmj.2006.0035. [DOI] [PubMed] [Google Scholar]
- 39.Lawton S, Timmons S. The relationship between technology and changing professional roles in health care: A case-study in teledermatology. Stud Health Technol Inform. 2006;122:669–71. [PubMed] [Google Scholar]
- 40.Scheinfeld N. Photographic images, digital imaging, dermatology and the law. Arch Dermatol. 2004;140:473–6. doi: 10.1001/archderm.140.4.473. [DOI] [PubMed] [Google Scholar]
- 41.Goldberg DJ. Digital photography, confidentiality and teledermatology. Arch Dermatol. 2004;140:477–8. doi: 10.1001/archderm.140.4.477. [DOI] [PubMed] [Google Scholar]
- 42.Ferguson J. How to do a telemedical consultation. J Telemed Telecare. 2006;12:220–7. doi: 10.1258/135763306777889037. [DOI] [PubMed] [Google Scholar]


