Abstract
Background:
Soft tissue augmentation with autologous fat graft has been increasingly used by plastic surgeons despite unpredictable results. Several techniques have been described to prevent the main setback of this technique, fat graft resorption. However, there is no ideal technique described for this purpose.
Materials and Methods:
Twenty patients with subcutaneous tissue loss, atrophy or hypoplasia were treated with lipofilling. A subcutaneous pouch is dissected at the deformed area and later it is filled with autologous fat graft.
Results:
Graft maintenance during the postoperative period was satisfactory. Overcorrection was not performed except for the first three cases. Patient, surgeon and layman satisfaction was surveyed. Satisfaction was rated between 0 and 10. The mean score was 7.67 ± 1.22.
Conclusion:
The authors describe a technique for soft tissue augmentation which effectively corrects contour deformities, provides a low resorption rate and a relatively non-visible scar without causing irregularities.
Keywords: Autologous fat graft, dissected pouch, lipofilling, soft tissue augmentation
INTRODUCTION
Despite unpredictable results, clinical use of autologous fat transfer for soft tissue augmentation has increased among plastic surgeons. The rising interest in this procedure has paralleled the development and popularity of liposuction for body contouring This popularity may be due to the opportunity of having an already present material at hand to augment or restore areas of the face with volume loss or contour irregularities. Additionally currently available filler materials such as hyaluronic acid, bovine collagen, polymethyl methacrylate, calcium hydroxyapatite suffer from distinct disadvantages.
While satisfactory results can be achieved in the early postoperative period, long-term results may be disappointing for both the patient and the surgeon. The most common difficulty is the estimation of the resorption rate. Several techniques have been suggested for maximum fat survival including atraumatic fat harvesting technique, centrifugation, graft washing and addition of growth factor. However, there is no ideal technique described for this purpose.
The authors of this paper describe an alternative technique for soft tissue augmentation: Placement of autologous fat graft in a dissected pouch. A smooth and regular surface could be obtained with this soft tissue augmentation technique. The intervention also results in a relatively invisible scar.
MATERIALS AND METHODS
From August 2005 to July 2007, 20 patients (15 females and 5 males, age range 23-56 years) with subcutaneous tissue loss, atrophy or hypoplasia were treated with the described technique in our clinics. Patient characteristics, augmented area, incision localizations, filled volume (ml) are summarized in Table 1. The patients were informed about the technique and alternative options including their benefits, limitations, and complications.
Table 1.
Demographic profile and operative data of study patients
| Age/ Sex | Augmented area | Incision | Volume ml |
|---|---|---|---|
| 32/F | Bilateral, trochanter | Gluteal crisis | 2×85 |
| 34/F | Multiple depression areas on the left thigh | Multiple incision | 2-3 per incision |
| 35/F | Left zygomatic depression | Hairline | 3 |
| 26/M | Bilateral cheek | Preauricular | 2×11 |
| 42/F | Bilateral cheek | Preauricular | 2×7 |
| 56/F | Bilateral cheek | Preauricular | 2×7 |
| 23/F | Bilateral malar augmentation | Preauricular | 2×7 |
| 33/F | Bilateral medial thigh | Medial knee crisis | 2×95 |
| 46/F | Left cheek (postradiotherapy) | Nasolabial | 26 |
| 24/M | Right malar depression | Nasolabial | 8 |
| 27/F | Bilateral facial atrophy | Preauricular | 2×45 |
| 22/F | Right anterior thigh | Old scar | 8 |
| 24/F | Left hemifacial atrophy | Nasolabial | 11 |
| 30/F | Left hemifacial atrophy | Preauricular | 14 |
| 53/M | Post-maxillectomy depression | Nasolabial | 33 |
| 26/M | Glabellar depression scar | Old scar | 4 |
| 27/M | Right supraorbital depression scar | Old scar | 5 |
| 27/F | Bilateral malar augmentation | Nasolabial | 2×5 |
| 32/F | Bilateral malar augmentation | Nasolabial | 2×7 |
| 30/F | Right lateral thigh | Old scar | 50 |
Surgical technique
Areas to be augmented were marked. Using deep sedation, the recipient area and lower abdomen or medial thigh were prepared with povidone iodine and draped. The tumescent solution containing 0.08% lidocaine and 1:500,000 of epinephrine was infiltrated into the donor and recipient sites. Approximately 0.5-1 cm skin incisions were made in the appropriate place. For example, preauricular incision was preferred for hemifacial augmentation and nasolabial fold incision for malar augmentation. Subcutaneous dissections were performed with blunt scissors and extended 1-2 cm further to the marked area. The dissection plane was between dermis and local fat tissue. After dissection was completed, gentle compression was applied while the fat graft was being harvested.
Fat graft was harvested using a 5-mm blunt, three-holed suction cannula, attached to a 50-ml syringe. Preferred donor sites were the lower abdomen in 13 patients, and lower extremity in seven patients. After insertion of the cannula, under mild negative pressure, fat graft was aspirated with the aid of repeated back and forth motions of cannula. Approximately 10-20 ml fat graft per syringe was harvested. By aspiration of saline, the fat graft within the syringe was washed off from blood, oil and tumescent solution. Harvested fat was injected into the dissected plane via incision and then incision was sutured with fine polypropylene. Overcorrection was not performed with the exception of the first three cases. Irregularities were arranged with a gentle massage. The grafted sites were immobilized for a week with a compression dressing. Antibiotic and anti-inflammatory medications were used in the postoperative period.
RESULTS
A total of 20 patients (facial augmentation in 15 patients, lower extremity intervention in five patients) underwent soft tissue augmentation with the described technique. Procedure-related complications were not observed in donor and recipient areas. In one patient, debulking was performed with liposuction at the tenth postoperative month due to persistence of overcorrection on left cheek. A new injection procedure was applied in one patient due to resorption. The mean postoperative follow-up was 1.7 years. The degree of improvement was scored by patients, surgeons and laymen. The satisfaction questionnaires were answered at the sixth postoperative month. Postoperative satisfaction was rated between 0 and 10, with 0 the worst and 10 the best grade. The overall satisfaction score was 7.67 ± 1.22 [Table 2]. Some results are shown in Figures 1–3.
Table 2.
Satisfaction questionnaire
| Patient | Surgeon | Layman | Overall |
|---|---|---|---|
| 7.75 ± 1.02 | 7.56 ± 1.5 | 7.6 ± 1.14 | 7.67 ± 1.22 |
Figure 1.

A 24-year-old woman with moderate left-sided hemifacial atrophy. Preoperative views (a,c,e), postoperative views (b, d, f). Nasolabial incision is unnoticeable
Figure 3.
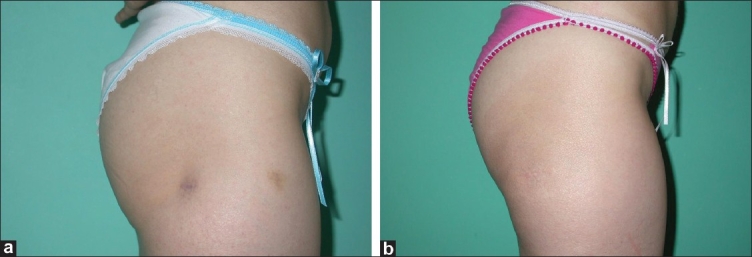
Right lateral thigh was dissected through old liposuction scar and then augmented with 50 cc fat graft
Figure 2.

A 32-year-old woman who underwent bilateral malar augmentation. Preoperative views (a,c,e), postoperative views (b, d, f); 7 cc autologous fat graft per side was filled via nasolabial incision
DISCUSSION
Over the past two decades, treatment of soft tissue losses (congenital, acquired or senile) with lipofilling has shown encouraging clinical results in terms of texture, softness and quality of skin pattern. Autologous fat tissue has been considered as an ideal filler for soft tissue augmentation because it is biocompatible, versatile, stable, long-lasting, natural-appearing, readily available, abundant, inexpensive, and can be harvested easily and repeatedly, with minimal trauma to the donor sites.[1] Therefore autologous fat tissue transfers have been devised to reestablish volume and contour that have been lost due to various causes. Despite extensive clinical use and optimism, there remains an uncertainty among practitioners regarding viability of the transferred fat.
There are various autologous fat transfer techniques from the points of donor site, harvesting method, type of anesthesia and the injection technique for soft tissue augmentation. En bloc fat graft harvesting is the least traumatic technique to the graft and has been shown to reduce tissue loss and improve fat graft survival.[2] In a rabbit model investigating the effect of different techniques on fat graft survival, Marques et al., found that surgical excision increased survival rates. However, surgically excised fat tissue transfer results with both donor and recipient area scars. Even if the donor area is preferred at a non-visible localization or the graft is harvested using a previous scar, en bloc fat cannot be introduced from a small incision. Therefore, syringe aspiration of fat appears to be the most popular method for fat harvesting.[3,4]
High fat graft resorption rates have been attributed to traumatic handling of the graft during the harvest and the injection stages. A number of authors recommend the use of half of the normal suction pressure to avoid mechanical injury to adipocytes during aspiration.[5] The shaft of the needle may produce higher shear and wake vortices, resulting in decreased cell viability.[5] The use of a 5-mm diameter blunt suction cannula prevented traumatization of harvested fat tissue. With the wide-diameter cannula, macro particle fat graft could be obtained almost similar in size with en bloc graft.
The most important uncertainties of the use of aspirated fat graft injection are about the quantity of the graft and the required degree of overcorrection. Overcorrection is a vague concept and there is no agreement on the amount or even the need of it. Different resorption rates are described in the literature. According to our previous experience and the literature data, we made overcorrection in the initial three operations, like the other lipofilling techniques. Even after the end of the first postoperative year, we observed persistence of overcorrection. Moreover, we had to debulk the overcorrected fat in the patient. We have not performed overcorrection since this experience. We had to make an additional injection only in one patient after four months.
Some other uncertainties for autologous fat transfer are the appropriate fat graft injection level and whether to perform the injection multilaminar or not.[4] To improve survival of fat grafts after transplantation, several injection techniques, such as 3-4 mm pearl transfer, roll injection, multitunnel fan-shape injection and multilane radial injection have been suggested.[1,6–8]
The most common complication of autologous fat transfer is related to the placement of inappropriate amount of fat. Irregular resorption remains a problem when using autologous, nonvascularized free fat grafts for correction of soft-tissue defects. Growth factors, beta blockers, insulin, growth media, and hyperbaric oxygen have been used for the prevention of irregular resorption. Yet some authors recommend minimal handling and no preparatory treatment of the intended graft tissue.[5,9,10] The other common problem is the presence of irregularities during the injection. We did not observe any undesirable outcome except in the first three patients in whom overcorrection was performed. Remarkable irregularities were not observed in the recipient areas.
Fat injection through cannula with positive high pressure could be potentially destructive to the adipocytes' cellular membranes and ultimately reduce graft survival.[11] Excess volume injection leads to a positive pressure space for the fat graft. This may be another reason for reduced fat graft survival. Our fat graft technique eliminates trauma to the fat during the injection step of the procedure and also eliminates the pressure of the surrounding tissue. Unlike many fat injection techniques, this method enhances the potential for preservation of the adipocytes' cellular membranes and microcirculation, possibly resulting in an increased probability for successful survival of the fat graft.
In conclusion, our fat injection technique combines fat injection and en bloc technique, provides a low resorption rate, a relatively non-visible scar, which is an important problem for en bloc fat transfer and eliminates irregularities. Autologous fat transplantation with the described technique can effectively correct contour deformities that require moderate augmentation. We have had great success in our series utilizing dissected pouch filling.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Coleman SR. Structural fat grafts: The ideal filler? Clin Plast Surg. 2001;28:111–9. [PubMed] [Google Scholar]
- 2.Kononas TC, Bucky LP, Hurley C, May JW., Jr The fate of suctioned and surgically removed fat after reimplantation for soft-tissue augmentation: A volumetric and histologic study in the rabbit. Plast Reconstr Surg. 1993;91:763–8. doi: 10.1097/00006534-199304001-00001. [DOI] [PubMed] [Google Scholar]
- 3.Marques A, Brenda E, Saldiva PH, Amarante MT, Ferreira MC. Autologous fat grafts: A quantitative and morphometric study in rabbits. Scand J Plast Reconstr Surg Hand Surg. 1994;28:241–7. doi: 10.3109/02844319409022006. [DOI] [PubMed] [Google Scholar]
- 4.Kaufman MR, Miller TA, Huang C, Roostaien J, Wasson KL, Ashley RK, et al. Autologous fat transfer for facial recontouring: Is there science behind the art? Plast Reconstr Surg. 2007;119:2287–96. doi: 10.1097/01.prs.0000260712.44089.e7. [DOI] [PubMed] [Google Scholar]
- 5.Smith P, Adams WP, Jr, Lipschitz AH, Chau B, Sorokin E, Rohrich RJ, et al. Autologous human fat grafting: Effect of harvesting and preparation techniques on adipocyte graft survival. Plast Reconstr Surg. 2006;117:1836–44. doi: 10.1097/01.prs.0000218825.77014.78. [DOI] [PubMed] [Google Scholar]
- 6.Xie Y, Li Q, Zheng D, Lei H, Pu LL. Correction of hemifacial atrophy with autologous fat transplantation. Ann Plast Surg. 2007;59:645–53. doi: 10.1097/SAP.0b013e318038fcb7. [DOI] [PubMed] [Google Scholar]
- 7.Ellenbogen R. Free autogenous pearl fat grafts in the face – a preliminary report of a rediscovered technique. Ann Plast Surg. 1986;16:179–94. doi: 10.1097/00000637-198603000-00001. [DOI] [PubMed] [Google Scholar]
- 8.Guerrerosantos J. Long-term outcome of autologous fat transplantation in aesthetic facial recontouring: Sixteen years of experience with 1936 cases. Clin Plast Surg. 2000;27:515–43. [PubMed] [Google Scholar]
- 9.Ayhan M, Senen D, Adanali G, Görgü M, Erdoğan B, Albayrak B. Use of beta blockers for increasing survival of free fat grafts. Aesthetic Plast Surg. 2001;25:338–42. doi: 10.1007/s002660010145. [DOI] [PubMed] [Google Scholar]
- 10.Shoshani O, Shupak A, Ullmann Y, Ramon Y, Gilhar A, Kehat I, et al. The effect of hyperbaric oxygenation on the viability of human fat injected into nude mice. Plast Reconstr Surg. 2000;106:1390–6. doi: 10.1097/00006534-200011000-00028. [DOI] [PubMed] [Google Scholar]
- 11.Guyuron B, Majzoub RK. Facial augmentation with core fat graft: A preliminary report. Plast Reconstr Surg. 2007;120:295–302. doi: 10.1097/01.prs.0000264399.40701.71. [DOI] [PubMed] [Google Scholar]


