Summary
The implementation of routine computer-based screening for suicidal ideation and other psychosocial domains through standardized patient reported outcome instruments in two high volume urban HIV clinics is described. Factors associated with an increased risk of self-reported suicidal ideation were determined.
Background
HIV/AIDS continues to be associated with an under-recognized risk for suicidal ideation, attempted as well as completed suicide. Suicidal ideation represents an important predictor for subsequent attempted and completed suicide. We sought to implement routine screening of suicidal ideation and associated conditions using computerized patient reported outcome (PRO) assessments.
Methods
Two geographically distinct academic HIV primary care clinics enrolled patients attending scheduled visits from 12/2005 to 2/2009. Touch-screen-based, computerized PRO assessments were implemented into routine clinical care. Substance abuse (ASSIST), alcohol consumption (AUDIT-C), depression (PHQ-9) and anxiety (PHQ-A) were assessed. The PHQ-9 assesses the frequency of suicidal ideation in the preceding two weeks. A response of “nearly every day” triggered an automated page to pre-determined clinic personnel who completed more detailed self-harm assessments.
Results
Overall 1,216 (UAB= 740; UW= 476) patients completed initial PRO assessment during the study period. Patients were white (53%; n=646), predominantly males (79%; n=959) with a mean age of 44 (± 10). Among surveyed patients, 170 (14%) endorsed some level of suicidal ideation, while 33 (3%) admitted suicidal ideation nearly every day. In multivariable analysis, suicidal ideation risk was lower with advancing age (OR=0.74 per 10 years;95%CI=0.58-0.96) and was increased with current substance abuse (OR=1.88;95%CI=1.03-3.44) and more severe depression (OR=3.91 moderate;95%CI=2.12-7.22; OR=25.55 severe;95%CI=12.73-51.30).
Discussion
Suicidal ideation was associated with current substance abuse and depression. The use of novel technologies to incorporate routine self-reported screening for suicidal ideation and other health domains allow for timely detection and intervention for this life threatening condition.
Introduction
Despite advances in therapy that transformed HIV/AIDS into a treatable chronic illness, it continues to be associated with an under-recognized risk for suicidal ideation, as well as attempted and completed suicide.[1-2] The presence of suicidal ideation represents an important predictor for subsequent attempted and completed suicide.[3] Though spontaneous disclosure of suicidal ideation is relatively rare, patients often endorse these thoughts when questioned specifically, providing an opportunity for intervention.[4] Previous reports indicate up to two-thirds of individuals who committed suicide were seen by a healthcare provider the month prior to death.[5] As high rates of suicidal ideation and associated comorbidities (ex: mental health diagnoses, substance abuse, etc.) have been reported in HIV-infected adults, the development of strategies to incorporate screening and timely intervention for suicidal ideation into the routine clinical care setting could greatly benefit this high risk group.[1, 6-7]
Individuals often report a preference for computerized screening over human interview for sensitive subject matter such as sexual function, drug use, and suicidal thoughts.[4, 8-9] In a study of 3,000 patients in eight primary care clinics, computer-based, self-reported screening was found to be more accurate than clinician assessment for prediction of suicidal ideation and other mental health symptoms.[10] Thus, the implementation of self-reported, standarized, computerized assessments may represent an accurate and viable strategy to screen for suicidal ideation during routine clinic visits.
In the present study, our goals were to: (1) Implement routine self-administered computerized screening for suicidal ideation (and other psycho-social domains) linked to automated activation of a response team in two high volume, urban HIV clinics; and (2) Identify factors associated with self-reported suicidal ideation as determined by computerized screening in a contemporary sample of HIV-infected individuals.
Methods
Study Setting
This study was conducted among a convenience sample of patients at the University of Alabama at Birmingham (UAB) 1917 HIV/AIDS Clinic Cohort and the University of Washington (UW) Harborview Medical Center HIV Clinic. The UAB 1917 Clinic provides HIV primary care for over 1,700 active patients and is a 100% quality controlled observational cohort study that was recently recognized for excellence in information integrity.[11-12] The UW Harborview Medical Center HIV Clinic provides comprehensive care to 1,600 patients and is the largest single provider of HIV care in the Northwestern United States.[13-14]
UAB and UW are part of the Center for AIDS Research Network of Integrated Clinical Systems (CNICS), an NIH-funded (R24) collaborative research resource that integrates a broad range of clinical data collected through point-of-care electronic medical record systems across multiple academic medical centers engaged in the longitudinal care of individuals with HIV/AIDS.[15] The Institutional Review Board for Protection of Human Subjects at each site reviewed and approved this study. The assessment of patient reported outcomes (PRO), a series of standardized, validated psycho-social instruments described below, was integrated into routine clinical care at UAB in April 2008 and at UW in December 2005.
Computerized Self-Reported PRO Assessment Software and Implementation
An open-source, web-based software application incorporating patient reported assessments across multiple psychosocial domains was developed and implemented at both sites with support from the CNICS collaborative. PRO assessments were conducted using touch-screen desktop computers (UAB) or tablet computers (UW). Previous studies report the impact of touch-screen interfaces in decreasing the barriers to information entry.[16-17] Touch-screens provide an acceptable and efficient method of obtaining self-reported data related to quality of life and psychological distress.[17-18] By using computers rather than face-to-face interviewing, social desirability bias or the tendency of respondents to reply in a manner that will be viewed favorably by others may be decreased. Normalcy statements or phrasing of questions to decrease perception of judgment were utilized in several of the standardized instruments (i.e. some patients forget to take their medications on the weekends, how many days over the last week have you forgotten to take your medications?).
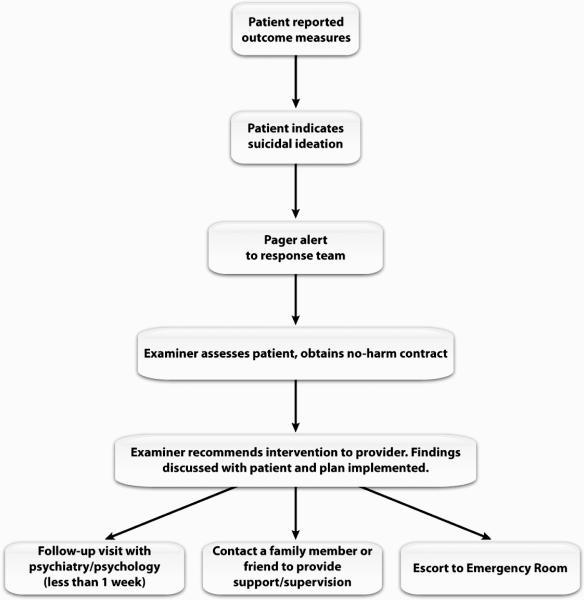
Upon arrival to their scheduled clinic visit, each patient was given a four-digit temporary code to access their PRO session (ticket number) or was logged in by a staff member. Both sites emphasized avoiding the disruption of routine clinic operations (i.e., workflow). Accordingly, PRO assessments were integrated into the clinic workflow by having hardware available where patients passively waited during regular visits (i.e., waiting and examination rooms). Patients could pause and rejoin the PRO assessment by re-entering their ticket number at different physical locations in the clinics as dictated by the clinic registration/intake/care process (Figure 1).
Figure 1.
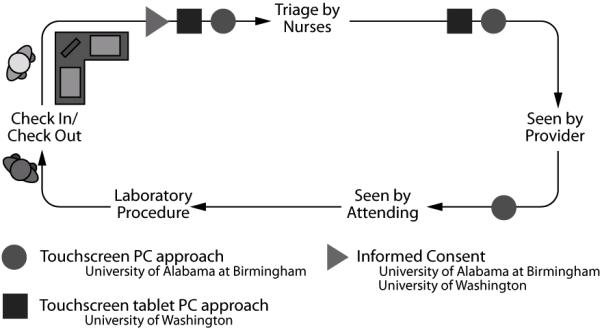
Diagram of clinic workflow and time of assessment at University of Alabama at Birmingham and University of Washington.
Providers included physicians and nurse practitioners/physician assistants. Both sites had a full-time employee to coordinate the administration of the computerized survey. At UAB, two touch-screen computers were available in the waiting area, and each patient examination room was outfitted with a touch-screen computer (n=8). At UW, a wireless network provided internet connectivity for two tablet computers used for survey administration.
Study Period/Participants
The current study, nested within the larger CNICS study, included HIV-infected adults who attended at least one routine primary care appointment and completed their first PRO before February 2009. After obtaining written informed consent, participants were provided with standardized instructions for completing the computerized assessment and basic instructions for computer use. The initial PRO completed by each patient during the study period was included. Patients who were cognitively impaired, medically unstable, or did not speak English were ineligible for study participation. Those with vision impairment or inadequate literacy or inability to complete the assessment were aided by research assistants. Patients were excluded from analysis if they did not answer the suicidal ideation question in the depression instrument (PHQ-9).
Instruments and scoring
The psycho-social domains assessed by the PROs include depression (PHQ-9), anxiety (PHQ Anxiety Module), alcohol risk (AUDIT-C), and substance abuse (ASSIST).[13] Mean time of completion of all instruments was between 10-15 minutes during pre-implementation testing. Patients were categorized per their responses to the anxiety (PHQ Anxiety Module: no anxiety, anxiety symptoms, panic syndrome) and alcohol (AUDIT-C: no risk, low risk, or at-risk for abuse) as previously validated in the literature.[19-21] Substance abuse (crack/cocaine, amphetamines, opioids, and intravenous drug use) was categorized into never, historical, or current (prior 3 months) per the responses to the ASSIST instrument.[22-23]
Suicidal ideation was measured by the patient’s response to the ninth question of the PHQ-9: “Please indicate how often over the last 2 weeks you have...thought you would be better off dead or hurting yourself in some way”. Response options included “not at all,” “several days,” “more than half of the days” and “nearly every day.” Because the dependent variable (suicidal ideation) was included in the predictor variable (PHQ-9 score), the question pertaining to suicidal ideation was removed from the PHQ-9 score calculation as previously validated in the literature (calculated PHQ-8 score).[24-26] Thus, PHQ-8 scores were calculated and used in all analyses.
Suicide response protocol
Because the PHQ-9 question on suicidality involved both active and passive ideation, we focused on only the highest risk group, those endorsing a response of “nearly every day,” for an immediate response with a full suicide assessment. At UAB, a licensed mental health professional and research assistant comprised the response team, whereas, at UW, it included a social worker supervisor and physician. The response team assessed the at-risk individual’s suicide plan, plan lethality, suicidal ideation frequency, attempt history, symptoms, current morbid thoughts, and preoccupation with death. When needed, a contract for safety was completed. After assessment, an intervention was recommended, ranging from establishing a follow-up or new appointment with a mental health provider within one week, to immediate emergency department referral for further psychiatric evaluation. The results of the patient’s suicide risk assessment and the recommended course of action were discussed with both the patient and their primary HIV healthcare provider (Figure 2).
Figure 2.
Response Protocol for Suicidal Ideation
Statistical Analyses
Outcomes
Variables were selected a priori based upon review of the literature and included socio-demographic characteristics (age, sex, race, and health insurance information), clinical/laboratory results (current CD4 cell count, HIV viral load, and antiretroviral therapy utilization), and psycho-social assessments (PHQ-9/depression, PHQ/anxiety, AUDIT-C/alcohol abuse, and ASSIST/substance abuse). Any level of self-reported suicidal ideation was modeled as the outcome variable consistent with prior research.[1] Data concerning subsequent emergency department (ED) visits were retrieved by chart review at each institution.
Analyses
Descriptive statistics were computed for all study variables to ensure assumptions of statistical tests were met. To compare means between groups, the two-sample t-test (if normality assumptions were met); for continuous and categorical outcomes, the Wilcoxon rank sum test and Chi-squared test were utilized respectively. Logistic regression analyses were performed to determine which factors were associated with the presence of suicidal ideation. As all patients that experienced suicidal ideation also had self reported depression on the PHQ, mild depression was used as the referent group for this independent variable. Due to colinearity between the depression and anxiety measures, anxiety was excluded from logistic regression modeling. All statistical analyses were performed using SAS software, version 9.1.3 (SAS Institute).
Results
A total of 1,268 PRO sessions, were completed during the study period. Of these, 52 were excluded (UAB=26; UW=26) due to not answering the suicidal ideation question and a total of 1,216 (UAB= 740; UW= 476) patients were included in analyses. The mean age was 44 (± 10) years, 53% (n=646) were white and 79% were male (n=959). The mean CD4 cell count was 454 (± 277) cells/mm3, and 15% of the study population was uninsured (n=180). Most patients were on antiretroviral therapy (80%; n=977). Among these individuals, 68% (n=606) had an undetectable (<50 copies/mL) HIV viral load at the time of assessment. Statistically significant differences (p<0.05) were seen between sites regarding self-reported rates of depression, anxiety, alcohol risk, and overall substance abuse (Table 1).
Table 1.
Patient characteristics and results of initial computerized, self-reported assessments at the UAB and UW HIV/AIDS Clinics. (N=1216)
| Overall (n=1216) Mean ± SD or n(%) |
UAB (n= 740) Mean ± SD or n(%) |
UW (n= 476) Mean ±SD or n(%) |
P-value | |
|---|---|---|---|---|
| Age | 44 (± 10) | 44 (± 10) | 43 (± 9) | 0.23 |
|
Gender
Male Female |
959 (78.9 ) 257 (21.1) |
547 (73.9) 193 (26.1) |
412 (86.6) 64 (13.4) |
<0.001 |
|
Race White Black/Other* |
646 (53 ) 570 (47 ) |
337(45.5) 403 (54.5) |
309 (64.9) 167 (35.1) |
<0.001 |
|
Insurance
Private Health Insurance Public Health Insurance Uninsured |
418 (34) 618 (51) 180 (14.8) |
300 (40.5) 294 (39.7) 146 (19.7) |
118 (24.8) 324 (68.1) 34 (7.1) |
<0.001 |
| CD4 count cell/mm 3 | 454 (± 277) | 479 (± 295) | 415 (± 241) | <0.001 |
|
On Antiretroviral Therapy
Yes No |
977 (80.4) 239 (19.7) |
598 (80.8) 142 (19.2) |
379 (79.6) 97 (20.4) |
0.61 |
|
HIV VL (copies/mL) On ART < 50 c/mL > 50 c/mL Off ART < 50 c/mL > 50 c/mL |
587 (60.1) 390 (39.9) 19 (8.0) 220 (92.1) |
331 (55.4) 267 (44.7) 13 (9.2) 129 (90.9) |
256 (67.6) 123 (32.5) 6 (6.2) 91 (93.8) |
< 0.001 0.40 |
| Depression Score (PHQ9) | 5.3 (± 6.6) | 3.1 (± 5.3) | 8.7 (± 7.1) | <0.001 |
|
Level of Depression (PHQ9)
No Depression (0-4) Mild (5-9) Moderate (10-14) Moderately Severe (15-19) Severe (≥20) Unknown |
720 (59.2) 231 (19.0) 118 (9.7) 82 (6.7) 60 (4.9) 5 (0.4) |
557 (75.3) 97 (13.1) 42 (5.7) 23 (3.1) 18 (2.4) 3 (0.4) |
163 (34.2) 134 (28.2) 76 (16.0) 59 (12.4) 42 (8.8) 2 (0.4) |
<0.001 |
|
Suicidal Ideation
Not at all Several days ½ the days Nearly every day |
1046 (86.0) 104 (8.6) 33 (2.7) 33 (2.7) |
692(93.5) 29 (3.9) 6 (0.8) 13 (1.8) |
354 (74.4) 75 (15.7) 27 (5.7) 20 (4.2) |
<0.001 |
| Depression Score (PHQ8) | 5.7 (± 7.0) | 3.3 (± 5.7) | 9.3 (± 7.3) | <0.001 |
|
Level of Depression (PHQ-8)
No Depression (0-4) Mild (5-9) Moderate (10-14) Moderately Severe (15-19) Severe (≥20) Unknown |
722 (59.4) 199 (16.4) 124 (10.2) 77 (6.3) 89 (7.3) 5 (0.4) |
558 (75.4) 86 (11.6) 46 (6.2) 23 (3.1) 25 (3.4) 2 (0.3) |
164 (34.5) 113 (23.7) 78 (11.3) 54 (11.3) 64 (13.5) 3 (0.6) |
<0.001 |
| Anxiety Score | 0.9 (± 1.8) | 0.5 (± 1.4) | 1.5 (± 2.1) | <0.001 |
|
Anxiety Symptoms (PHQ-A)
No anxiety (0) Anxiety symptoms (1-4) Panic syndrome (≥5) Unknown |
943 (77.6) 125 (10.3) 128 (10.5) 20 (1.6) |
638 (86.2) 57 (7.7) 36 (4.9) 9 (1.2) |
305 (64.1) 68 (14.3) 92 (19.3) 11 (2.3) |
<0.001 |
| Alcohol Score (Audit-C) | 1.9 (± 2.4) | 1.7 (± 2.3) | 2.3 (± 2.5) | <0.001 |
|
Alcohol Risk (Audit-C)
No Risk (0) Lower Risk (1-4) At-Risk (≥5) Unknown |
471 (38.7) 528 (43.4) 175 (14.4) 42 (3.5) |
95 (12.8) 301 (40.7) 323 (43.7) 21 (2.8) |
148 (31.1) 227 (47.7) 80 (16.8) 21 (4.4) |
<0.001 |
|
Substance Abuse (ASSIST)
Never Yes – Historical Yes – Current Unknown |
595 (48.9) 419 (34.4) 182 (14.9) 34 (2.8) |
462 (62.4) 208 (28.1) 55 (7.5) 15 (2.0) |
133 (27.9) 211(44.3) 127 (26.7) 5 (1.1 ) |
<0.001 |
|
Crack/ Cocaine Use
Never Yes – Prior Yes – Current Unknown |
658 (54.1) 116 (9.5) 422 (34.7) 20 (1.6) |
481 (65.0) 200 (27.0) 43 (5.8) 16 (2.2) |
177 (37.2) 222 (46.7) 73 (15.3) 4 (0.8) |
<0.001 |
|
Amphetamine Use
Never Yes – Historical Yes – Current Unknown |
868 (71.4) 233 (19.2) 90 (7.4) 25 (2.1) |
650 (87.8) 64 (8.7) 11 (1.5) 15 (2.0) |
218 (45.8) 169 (35.5) 79 (16.6) 10 (2.1) |
<0.001 |
|
Opioid Use
Never Yes – Historical Yes – Current Unknown |
1048 (86.2) 120 (9.9) 22 (1.8) 26 (2.1) |
687 (92.8) 28 (3.8) 7 (1.0) 18 (2.4) |
361 (75.8) 92 (19.3) 15 (3.2) 8 (1.7) |
<0.001 |
|
IV Drug Use
Never Yes – Historical Yes – Current Unknown |
1015 (83.5) 137 (11.2) 30 (2.5) 34 (2.8) |
688 (93.0) 34 (4.6) 1 (0.1) 17 (2.3) |
327 (68.7) 103 (21.6) 29 (6.1) 17 (3.6) |
<0.001 |
Overall, 170 (14%) of the total population (UAB n=48; UW n=122) self-reported some degree of suicidal ideation (Table 1). In adjusted logistic regression analysis, advancing age was found to decrease the risk of self-reported suicidal ideation (OR 0.74 per 10 year increment; 95% CI 0.58-0.96). The absence of depression on PHQ-9 assessment decreased the risk of self-reported suicidal ideation (OR 0.08 no depression; 95% CI 0.03-0.21). The risk for reporting suicidal ideation increased incrementally with the severity of depression (OR 3.91 moderate depression, 95% CI 2.12-7.22; OR 25.55 severe depression, 95% CI 12.73-51.30). Current substance abuse (OR 1.88, 95% CI 1.03-3.44) was found to increase the risk for self-reported suicidal ideation, while prior or historical substance abuse (OR 1.15, 95% CI 0.66-1.98) did not. Higher CD4 values exhibited a trend towards a decreased risk of suicidal ideation (0.98 CD4 per 50 cell/mm increase, 95% CI 0.94-1.02).
The suicide response team at each site intervened only when patients reported the highest degree of suicidal ideation, i.e., thinking “nearly every day” they would be “better off dead or hurting themselves in some way.” Among 170 patients reporting any degree of suicidality, 33 (3% overall; UAB n=13 (27%); UW, n=20 (16%)) reported suicidality of this frequency. Most were assessed by the suicide response team (UAB n=12; UW n=19), while two patients refused further assessment after screening (UAB n=1; and UW n=1). A total of 28 individuals (UAB n=10; UW n=18) were referred for a follow-up or new mental health provider visit within one week or had a pending mental health provider visit. Three (UAB n=2; UW n=1) were immediately referred to the emergency department (ED) for further psychiatric evaluation, and 28 (UAB n=10; UW n=18) were subsequently scheduled for a follow-up visit with a mental health provider for the next week. One patient (UAB) refused to go to the ED and requested to leave the clinic, commited to return if allowed to first arrange child care, but did not return as agreed. None of these patients were admitted to the hospital as a result of psychiatry assessment in the ED.
Discussion
While other studies have investigated factors associated with suicidal ideation in HIV primary care settings, this is the first study to implement and evaluate suicidal ideation screening through computerized, self-reported assessment as part of routine HIV clinical care.[1, 6-7] We have successfully implemented routine on-going touch-screen based assessment of multiple PROs in two academic, high volume clinics with minimal workflow disruption. Among our study sample, 170 (14%) patients endorsed some level of suicidal ideation while 33 (3%) admitted suicidal ideation nearly every day. The odds of reporting suicidality were increased with more severe depression and current substance abuse, while advancing age was associated with lower risk. Our experience supports the use of novel technologies and user friendly interfaces (i.e., touch-screens or tablet computers) to facilitate the collection of self-reported information in high volume clinical settings.[17] Such interventions augment the detection of suicidal ideation and other important psychosocial co-morbidities allowing for timely diagnosis and intervention for these potentially life-threatening conditions.[3, 27-28]
The relationship between depression and suicidal ideation is well established across multiple studies.[29-31] In our study, 97% of patients reporting suicidal ideation had concurrent depressive symptoms per their PHQ-9 assessment, while those with “no depression” experienced a significantly decreased risk for self-reported suicidal ideation (OR=0.08; 95% CI=0.03-0.21). In concordance with prior reports in non-HIV infected samples, the magnitude of risk for self-reported suicidal ideation increased incrementally with greater severity of self-reported depression (Table 2).
Table 2.
Unadjusted and adjusted analyses of factors associated with suicidal ideation preceding primary care visit at the University of Alabama at Birmingham and the University of Washington HIV/AIDS Clinics. (N=1216)
| Suicidal Ideation Mean ± SD or n(%) |
No Suicidal Ideation Mean ± SD or n(%) |
Unadjusted OR (95%CI) |
Adjusted OR (95%CI) |
|
|---|---|---|---|---|
| Age (per 10 years) | 41.9 (±7.9) | 43.8 (±9.9) | 0.81 (0.69-0.96) | 0.74 (0.58-0.96) |
|
Gender
Female Male |
24 (14.1) 146 (85.9) |
233 (22.3) 813 (77.7) |
1.0 1.74 (1.11-2.75) |
1.0 1.87 (0.99-3.52) |
|
Race White Black/Other* |
105 (61.8) 65 (38.2) |
541 (51.7) 505 (48.3) |
1.0 0.66 (0.48-0.93) |
1.0 1.22 (0.77-1.95) |
|
Insurance
Private Public Uninsured |
35(20.6) 119 (70.0) 16 (9.4) |
383 (36.62) 499 (47.7) 164 (15.7) |
1.0 2.61 (1.75-3.89) 1.07 (0.58-1.98) |
1.0 1.28 (0.74-2.22) 0.84 (0.38-1.85) |
|
Location
UW UAB |
122 (71.8) 48 (28.2) |
354 (33.8) 692 (66.2) |
1.0 0.20 (0.14-0.29) |
1.0 0.84 (0.51-1.39) |
| CD4 (per 50 cells/mm3) | 383 (± 238.0) | 466 (± 281.0) | 0.94 (0.91-0.97) | 0.98 (0.94-1.02) |
|
ART Therapy
No Yes |
39 (22.9) 131 (77.1) |
200 (19.1) 846 (80.9) |
1.0 0.79 (0.54-1.17) |
--- |
|
Level of Depression (PHQ-8)
No Depression (0-4) Mild (5-9) Moderate (10-14) Moderately Severe (15-19) Severe (≥20) Unknown |
5 (2.94) 21 (12.4) 39 (22.9) 50 (29.4) 52(30.6) 1 (0.6) |
717 (68.6) 178 (17.0) 85 (8.1) 32 (3.1) 8 (0.8) 4 (0.4) |
0.06 (0.02-0.16) 1.0 3.89 (2.16-7.02) 9.16 (4.85-17.31) 21.70 (11.37-41.43) 2.12 (0.23-19.86) |
0.08 (0.03-0.21) 1.0 3.91 (2.12-7.22) 9.08 (4.67-17.63) 25.55 (12.73-51.30) 2.05 (0.20-21.64) |
|
Anxiety Symptoms (PHQA)
No anxiety (0) Anxiety symptoms (1-4) Panic syndrome (≥5) Unknown |
59 (34.7) 34 (20.0) 71 (41.8) 6 (3.5) |
884 (84.5) 91 (8.7) 57 (5.5) 14 (1.3) |
1.0 5.60 (3.49-8.99) 18.66 (12.06-28.89) 6.42 (2.38-17.32) |
--- |
|
Alcohol Use (Audit-C)
No Risk (0) Lower Risk (1-4) At-Risk (≥5) Unknown |
55 (32.35) 73 (42.9) 36 (21.2) 6 (3.5) |
416 (39.8) 455 (43.5) 139 (13.3) 36 (3.4) |
1.0 1.21 (0.84-1.77) 1.96 (1.23-3.11) 1.26 (0.51-3.13) |
1.0 1.43 (0.86-2.38) 1.14 (0.61-2.14) 2.36 (0.62-9.05) |
|
Substance Abuse (ASSIST)
Never Yes - Historical Yes - Current |
42 (24.7) 69 (40.6) 59 (34.7) |
123 (12.0) 350 (34.1) 123 (12.0) |
1.0 2.60 (1.73-3.90) 6.32 (4.06-9.82) |
1.0 1.15 (0.66-1.98) 1.88 (1.03-3.44) |
Active substance abuse was also associated with self-reported suicidal ideation in our sample. Suicide plans and attempts have been associated with substance abuse disorders in various settings.[32-33] Active substance abuse may act both as a risk factor for increased risk of suicidal ideation and a sign of an underlying mental health condition.[33] In our sample, current substance abuse almost doubled the odds for self-reported suicidal ideation (OR 1.88; 95% CI=1.03-3.44) while historical substance abuse was not related to an increased risk of suicidality. An additional advantage of our approach is the ability to detect active substance abuse in real-time through computerized self-reported assessment (i.e., ASSIST) that allows for timely intervention and involvement of substance abuse professionals at the point of care.
Our findings should be interpreted with respect to the limitations of our study. Though our findings may not be generalizable to other national or international settings, inclusion of data from two geographically distinct cohorts represents a strength of this analysis. As with all observational studies, we were able to identify associations but cannot attribute causality and unmeasured confounding may have affected our findings. It is possible that functional healthcare literacy may have introduced bias by influencing study participation and the ability of some patients to complete the computerized PRO self-assessment. Although touch-screen, computer-assisted interviewing techniques were used to decrease social desirability bias and decrease computer literacy barriers to use, these factors may have still impacted data collection and introduced bias. In addition, assisting some patients with PRO completion may have potentially introduced bias and impacted study results (estimated at less than 5% of total patients). Further study is needed to determine the impact of our suicidal ideation screening and intervention protocols on long term attempted and completed suicides.
These limitations notwithstanding, our results advance the understanding of suicidal ideation in HIV primary care in several ways. First, we describe a functional model to systematically capture and coordinate a real-time, systems-based response to suicidal ideation in the outpatient HIV clinical care setting. Second, we were able to confirm factors associated with computerized self-reported suicidal ideation (i.e., severity of depression, current substance abuse). These factors are similar to those previously reported in the literature collected via patient interview or paper based questionnaires suggesting our approach represents a viable surrogate method for information capture.[34-35] Perhaps most importantly, the implementation of computerized self-assessment strategies in routine care represents a potentially transformative technology to screen for suicidal ideation as well as other patient reported outcomes which would significantly enhance detection, referral, and, ultimately, the overall cost-effectiveness of care through timely intervention.
Acknowledgements
The authors would like to thank the UAB 1917 HIV / AIDS Clinic Cohort Observational Database project, the UAB Center for AIDS Research, CFAR (grant P30-AI27767), CFAR-Network of Integrated Clinical Systems, CNICS (grant 1 R24 AI067039-1), and the Mary Fisher CARE Fund for their assistance and support of this project. Specifically, we would like to thank Suneetha Thogaripally for help with data, Dustin Rinehart for building the figures, Eric Webster for software support, and Barbara Files-Kennedy for assistance in patient reported outcomes collection. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Sources of Support: The UAB 1917 HIV / AIDS Clinic Cohort Observational Database project receives financial support from the following: UAB Center for AIDS Research (grant P30-AI27767), CFAR-Network of Integrated Clinical Systems, CNICS (grant 1 R24 AI067039-1), and the Mary Fisher CARE Fund. The content is solely the responsibility of the authors and does not necessarily represent the official views of any other agency providing support for this study. UW sources of support include the UW Center for AIDS Research (grant P30-A1-27757) and NIMH RO1 084759.
Footnotes
Potential conflicts of interest:
1. Sarah T. Lawrence: no conflicts of interest related to this manuscript.
2. James H. Willig has received research funding and/or consulted for: Bristol-Myers Squibb, Gilead, Merck and Tibotec.
3. Heidi M. Crane has received research funding and/or consulted for: no conflicts of interest related to this manuscript.
4. Jiatao Ye: no conflicts of interest related to this manuscript.
5. Inmaculada Aban: no conflicts of interest related to this manuscript.
6. William Lober: no conflicts of interest related to this manuscript
7. Christa R. Nevin: no conflicts of interest related to this manuscript.
8. D. Scott Batey: no conflicts of interest related to this manuscript.
9. Michael J. Mugavero has received research funding and/or consulted for: Tibotec Therapeutics, Bristol-Myers Squibb and Gilead.
10. Cheryl McCullumsmith has received research funding and/or consulted for: Boehringer Ingelheim Pharmaceuticals, Inc.
11. Mari Kitahata has received research funding and/or consulted for: Gilead
12. James L. Raper: no conflicts of interest related to this manuscript.
13. Micheal S. Saag has received research funding and/or consulted for: Adrea Pharmaceuticals, Avexa, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead, GlaxoSmithKline, Merck, Monogram Biosciences, Panacos, Pfizer, Progenics, Roche, Serono, Tanox, Tibotec, Trimeris, and Vertex
14. Joseph E. Schumacher has received research funding and/or consulted for: Boehringer Ingelheim Pharmaceuticals, Inc.
References
- 1.Sherr L, Lampe F, Fisher M, et al. Suicidal ideation in UK HIV clinic attenders. AIDS (London, England) 2008 Aug 20;22(13):1651–8. doi: 10.1097/QAD.0b013e32830c4804. [DOI] [PubMed] [Google Scholar]
- 2.Robertson K, Parsons TD, Van Der Horst C, Hall C. Thoughts of death and suicidal ideation in nonpsychiatric human immunodeficiency virus seropositive individuals. Death studies. 2006 Jun;30(5):455–69. doi: 10.1080/07481180600614435. [DOI] [PubMed] [Google Scholar]
- 3.Ranieri WF, Steer RA, Lavrence TI, Rissmiller DJ, Piper GE, Beck AT. Relationships of depression, hopelessness, and dysfunctional attitudes to suicide ideation in psychiatric patients. Psychological reports. 1987 Dec;61(3):967–75. doi: 10.2466/pr0.1987.61.3.967. [DOI] [PubMed] [Google Scholar]
- 4.Greist JH, Gustafson DH, Stauss FF, Rowse GL, Laughren TP, Chiles JA. A computer interview for suicide-risk prediction. The American journal of psychiatry. 1973 Dec;130(12):1327–32. doi: 10.1176/ajp.130.12.1327. [DOI] [PubMed] [Google Scholar]
- 5.Hirschfeld RM, Russell JM. Assessment and treatment of suicidal patients. The New England journal of medicine. 1997 Sep 25;337(13):910–5. doi: 10.1056/NEJM199709253371307. [DOI] [PubMed] [Google Scholar]
- 6.Hawton K, Fagg J. Suicide, and other causes of death, following attempted suicide. Br J Psychiatry. 1988 Mar;152:359–66. doi: 10.1192/bjp.152.3.359. [DOI] [PubMed] [Google Scholar]
- 7.van der Sande R, van Rooijen L, Buskens E, et al. Intensive in-patient and community intervention versus routine care after attempted suicide. A randomised controlled intervention study. Br J Psychiatry. 1997 Jul;171:35–41. doi: 10.1192/bjp.171.1.35. [DOI] [PubMed] [Google Scholar]
- 8.Kobak KA, Greist JH, Jefferson JW, Katzelnick DJ. Computer-administered clinical rating scales. A review. Psychopharmacology. 1996 Oct;127(4):291–301. doi: 10.1007/s002130050089. [DOI] [PubMed] [Google Scholar]
- 9.Lucas RW, Mullin PJ, Luna CB, McInroy DC. Psychiatrists and a computer as interrogators of patients with alcohol-related illnesses: a comparison. Br J Psychiatry. 1977 Aug;131:160–7. doi: 10.1192/bjp.131.2.160. [DOI] [PubMed] [Google Scholar]
- 10.Kroenke CD, Spitzer A. The PHQ-9: A new depression diagnostic and severity measure. Psychiatric Annals. 2002;32(9) [Google Scholar]
- 11.Ulett KB, Willig JH, Lin HY, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS patient care and STDs. 2009 Jan;23(1):41–9. doi: 10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Willig JH, Abroms S, Westfall AO, et al. Increased regimen durability in the era of once-daily fixed-dose combination antiretroviral therapy. AIDS (London, England) 2008 Oct 1;22(15):1951–60. doi: 10.1097/QAD.0b013e32830efd79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crane HM, Lober W, Webster E, et al. Routine collection of patient-reported outcomes in an HIV clinic setting: the first 100 patients. Current HIV research. 2007 Jan;5(1):109–18. doi: 10.2174/157016207779316369. [DOI] [PubMed] [Google Scholar]
- 14.Kitahata MM, Dillingham PW, Chaiyakunapruk N, et al. Electronic human immunodeficiency virus (HIV) clinical reminder system improves adherence to practice guidelines among the University of Washington HIV Study Cohort. Clin Infect Dis. 2003 Mar 15;36(6):803–11. doi: 10.1086/368085. [DOI] [PubMed] [Google Scholar]
- 15.Kitahata MM, Rodriguez B, Haubrich R, et al. Cohort profile: the Centers for AIDS Research Network of Integrated Clinical Systems. Int J Epidemiol. 2008 Oct;37(5):948–55. doi: 10.1093/ije/dym231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Carbonell CSE. Finger Instead of Mouse: Touch Screens as a Means of Enhancing Universal Access Universal Access Theoretical Perspectives, Practice, and Experience. Vol. 2615. Springer-Verlag; Berlin Heidelberg: 2003. pp. 387–97. N. [Google Scholar]
- 17.Fann JR, Berry DL, Wolpin S, et al. Depression screening using the Patient Health Questionnaire-9 administered on a touch screen computer. Psychooncology. 2009 Jan;18(1):14–22. doi: 10.1002/pon.1368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Allenby A, Matthews J, Beresford J, McLachlan SA. The application of computer touch-screen technology in screening for psychosocial distress in an ambulatory oncology setting. European journal of cancer care. 2002 Dec;11(4):245–53. doi: 10.1046/j.1365-2354.2002.00310.x. [DOI] [PubMed] [Google Scholar]
- 19.Bush K, Kivlahan DR, McDonell MB, Fihn SD, Bradley KA, Ambulatory Care Quality Improvement Project (ACQUIP) The AUDIT alcohol consumption questions (AUDIT-C): an effective brief screening test for problem drinking. Arch Intern Med. 1998 Sep 14;158(16):1789–95. doi: 10.1001/archinte.158.16.1789. Alcohol Use Disorders Identification Test. [DOI] [PubMed] [Google Scholar]
- 20.Bradley KA, Bush KR, Epler AJ, et al. Two brief alcohol-screening tests From the Alcohol Use Disorders Identification Test (AUDIT): validation in a female Veterans Affairs patient population. Arch Intern Med. 2003 Apr 14;163(7):821–9. doi: 10.1001/archinte.163.7.821. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: the PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol. 2000 Sep;183(3):759–69. doi: 10.1067/mob.2000.106580. [DOI] [PubMed] [Google Scholar]
- 22.Newcombe DA, Humeniuk RE, Ali R. Validation of the World Health Organization Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): report of results from the Australian site. Drug Alcohol Rev. 2005 May;24(3):217–26. doi: 10.1080/09595230500170266. [DOI] [PubMed] [Google Scholar]
- 23.WHO ASSIST Working Group The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002 Sep;97(9):1183–94. doi: 10.1046/j.1360-0443.2002.00185.x. [DOI] [PubMed] [Google Scholar]
- 24.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001 Sep;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. J Affect Disord. 2009 Apr;114(13):163–73. doi: 10.1016/j.jad.2008.06.026. [DOI] [PubMed] [Google Scholar]
- 26.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999 Nov 10;282(18):1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 27.Kemball RS, Gasgarth R, Johnson B, Patil M, Houry D. Unrecognized suicidal ideation in ED patients: are we missing an opportunity? The American journal of emergency medicine. 2008 Jul;26(6):701–5. doi: 10.1016/j.ajem.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rihmer Z. Strategies of suicide prevention: focus on health care. Journal of affective disorders. 1996 Jul 8;39(2):83–91. doi: 10.1016/0165-0327(96)00007-9. [DOI] [PubMed] [Google Scholar]
- 29.Gonda X, Fountoulakis KN, Kaprinis G, Rihmer Z. Prediction and prevention of suicide in patients with unipolar depression and anxiety. Annals of general psychiatry. 2007;6:23. doi: 10.1186/1744-859X-6-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Henriksson MM, Aro HM, Marttunen MJ, et al. Mental disorders and comorbidity in suicide. The American journal of psychiatry. 1993 Jun;150(6):935–40. doi: 10.1176/ajp.150.6.935. [DOI] [PubMed] [Google Scholar]
- 31.Rihmer Z. Suicide risk in mood disorders. Current opinion in psychiatry. 2007 Jan;20(1):17–22. doi: 10.1097/YCO.0b013e3280106868. [DOI] [PubMed] [Google Scholar]
- 32.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008 Feb;192(2):98–105. doi: 10.1192/bjp.bp.107.040113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Regier DA, Farmer ME, Rae DS, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990 Nov 21;264(19):2511–8. [PubMed] [Google Scholar]
- 34.Gliatto MF, Rai AK. Evaluation and treatment of patients with suicidal ideation. Am Fam Physician. 1999 Mar 15;59(6):1500–6. [PubMed] [Google Scholar]
- 35.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999 Jul;56(7):617–26. doi: 10.1001/archpsyc.56.7.617. [DOI] [PubMed] [Google Scholar]