Abstract
Objective
Assess use of and reactions to an interactive, tailored CD-ROM to enhance oncologist–patient communication.
Methods
Participating oncologists (n = 48) agreed to have patient interactions audio recorded, be randomly assigned to receive/not receive a CD-ROM, have CD-ROM usage monitored (intervention group) and complete a follow-up survey.
Results
Twenty-one of 24 in the intervention group reported using the CD-ROM. Median usage minutes were 63.8. At follow-up, oncologists rated the CD-ROM from 1 (“none” or “not at all helpful”) to 5 (“a great deal” or “very helpful”). Mean responses were: 3.1 and 3.0 for 2 items assessing perceived impact on communications, 3.8–4.0 for 6 items assessing perceived helpfulness, 3.0 and 3.10 for 2 items assessing impact on affecting oncologists’ communication with patients and assistance with challenging conversations, respectively, and 3.6 for whether using the CD-ROM was worth their time. Self-report of how much oncologists had used the covered skills before and after intervention showed a perceived increase (2.8 before and 3.2 after).
Conclusions
Findings suggest the tailored interactive CD-ROM has promise for use and acceptance among oncologists.
Practice implications
If ultimately found effective in changing oncologist’s communication with patients, the CD-ROM’s widespread dissemination should be explored.
Keywords: Tailored intervention, Physician, patient communication, Oncologist
1. Introduction
Communication between patients and their oncologists is integral to high-quality cancer care. Effective communication is positively associated with patient satisfaction and treatment adherence [1,2]. Numerous studies have also shown that patient–oncologist communication could be better, particularly in how oncologists respond to patient emotion [3–8]. Patients whose emotional needs are unmet experience more anxiety and diminished quality of life [1,2,9,10]. However, few oncologists receive formal training in effective communication.
In response to this need, several training programs have been developed to improve oncologists’ communication. These programs generally involve days of intensive in-person training format including didactic instruction, interpersonal interaction, expert examples in live or videotaped format, and practice sessions, often with simulated patients. They have been found to improve communication [11–13] among those who attend, but the required time, travel, and expense associated with these programs limit access for many oncologists.
Through the SCOPE Trial (Studying Communication in Oncologist Patient Encounters), we developed an interactive, computer-based CD-ROM that focuses on addressing patient emotion and discussing prognosis. Rather than requiring attendance at a lecture or meeting, the CD-ROM can be mailed or hand delivered and used when convenient for the recipient. Therefore, if found effective, the SCOPE CD-ROM could be widely disseminated.
Two types of evaluation are important for assessing whether the SCOPE intervention warrants dissemination. The outcome evaluation (e.g., the educational impact of the intervention) will be assessed by whether use of the CD-ROM facilitates changes in oncologists’ skills and behaviors related to their communication with patients. Because the intervention cannot have any impact if oncologists do not use it and a positive impact is not likely if they do not like or find it helpful, it is also important to measure the process evaluation outcomes of usage and reactions—the extent to which oncologists in the study used the CD-ROM, liked it, and found it helpful.
It is common for studies of tailored health behavior change interventions to report both process and outcome evaluations and to include intervention exposure as a process measure. Indeed, one of the strong findings of the initial comparisons of tailored vs. non-tailored interventions has been that recipients are more likely to read “most or all” of tailored printed communications than of similar-looking non-tailored communications [14–17], and that tailored print have more positive reactions, such as perceived relevance [17]. These process evaluations have also been conducted for tailored interventions delivered via interactive computer programs showing, for example, that they are likely to be used by groups such as older people and those with lower education levels as well as those who are more computer savvy [18,19].
In contrast, studies of computerized medical education interventions have often reported process measures such as acceptability or satisfaction [20] but with some notable exceptions [21–23] they have rarely reported on proportion of the intended audience that used the intervention [20]. This may stem from study designs that do not lend themselves to calculating usage rates; most studies either implement computerized interventions into required coursework (therefore usage is nearly universal) or make information available over the web (where usage can often only be reported in absolute numbers rather than proportions due to lack of information about the denominator of potential users). This report contributes to the literature by reporting process outcomes of usage rates and reactions for a computerized medical education intervention that depends on voluntary usage.
2. Methods
2.1. Overview
The SCOPE Trial, described in detail elsewhere [24], is a randomized controlled trial conducted at Duke University and the Durham Veterans Affairs Medical Centers in Durham, NC, and the University of Pittsburgh Medical Center in Pittsburgh, PA. The protocol was approved by each site’s Institutional Review Board. Participants include patients with advanced cancer and the medical, gynecological, or radiation oncologists who provide their care.
2.1.1. Participant recruitment
As has been previously described [24], one of the investigators met face-to-face with each potential oncologist participants to introduce the study. Those who agreed to participate were asked to identify potential patient participants who had Stage IV malignancies and about whom the oncologist “would not be surprised if she (or he) were admitted to an intensive care unit (ICU) or died within one year”. We used this definition to ensure that referred patients had significant disease burdens while avoiding situations in which patients were referred so late in their disease progression that they were too ill for participation.
2.1.2. Participant consent
For patients, participation included giving consent to audio record their outpatient encounters with oncologists and complete face-to-face interviews immediately before the visit and over the phone within 10 days post-visit. Participating oncologists consented to: (1) have their patient encounters audio recorded; (2) attend a lecture on effective physician/patient communication (or view a webcast); (3) be randomly assigned to receive or not receive the SCOPE intervention on a CD-ROM; (4) for those in the intervention group, have their usage of the intervention measured and complete follow-up surveys assessing their reactions to the SCOPE intervention.
2.1.3. Study procedures
Using previously described methods [8], study staff audio-recorded clinical encounters for participating oncologists and up to eight of their participating patients. Participating oncologists understood that these recordings would be analyzed to assess communication quality and that, for those in the intervention arm, examples from recordings of their own conversations would be used to tailor their personal copy of the CD-ROM (described in the following section).
Following the baseline-recording phase, we used the minimization method [25,26] to randomly assign oncologists to the CD-ROM intervention or to a control condition. In contrast to a standard stratified randomization procedure, the minimization method is particularly useful when it is important to balance treatment arms on a larger number of covariates. In SCOPE, we sought to achieve balance on site (two levels: Durham and Pittsburgh) and oncologist gender and specialty (five levels: medical oncology—solid tumor, medical oncology—solid and liquid tumors, hematology oncology, gynecologic oncology, and radiation oncology). We weighted each classification variable equally to achieve an overall balance of the levels of these variables between treatment arms, rather than a balance within each strata. Twenty-four oncologists were randomly assigned to each arm.
Those assigned to the intervention arm received an email notifying them they were selected to receive the SCOPE intervention. Shortly after, a “communication coach” (PhD or masters-level psychologist) e-mailed each oncologist to set up an in-person meeting to deliver his or her personally tailored SCOPE CD-ROM, along with a set of high-quality earphones to facilitate use. In the brief visit, the coach reviewed the format of the CD-ROM, asked oncologists to use it while connected to the internet (or to connect to the internet at some point after using the CD-ROM) so usage data could be tracked, and used motivational interviewing techniques [27] to help the oncologist set goals for using the CD-ROM. If coaches noticed any reluctance from oncologists, they brainstormed about what barriers might impede use and tried to build motivation by asking what role oncologists felt communication played in their practices. Coaches checked in with oncologists weekly until they viewed the CD-ROM or until eight weeks had passed without viewing (at that point, the intervention phase was considered to have concluded).
We assessed oncologists’ reactions to the intervention via a follow-up survey that was hand delivered and then picked up by a research assistant and for which oncologists were offered a $25 gift card for completion. Data regarding oncologists’ use of and reactions to the intervention are the focus of this report.
2.2. Intervention
2.2.1. Theoretical basis
The SCOPE interactive computer intervention was designed to enhance oncologists’ ability to respond effectively to patients’ emotional concerns and to communicate bad news and prognosis. The conceptual model on which the intervention was based was drawn from social cognitive theory [28], and a barriers model proposed by Cabana [29] (see Fig. 1). Specifically, the aim of the intervention was to improve oncologists’ awareness of patient negative emotions, to build skills to address patient concerns, improve beliefs that addressing their concerns would improve patient well-being (outcome expectancies), build confidence to address patient emotional concerns (self-efficacy), and to improve communications skills. Also, the intervention presented information on external barriers such as patient factors (e.g., patients giving indirect rather than direct emotional cues) [30] and environmental factors (e.g., lack of time or resources) that may deter oncologists from addressing emotional concerns.
Fig. 1.
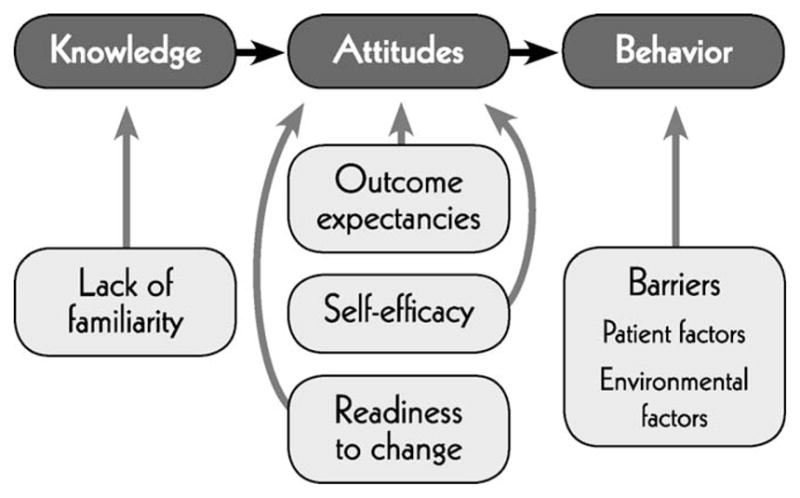
Conceptual model of the SCOPE intervention.
2.2.2. Development process
In developing the CD-ROM’s overall framework, we were guided by previous training programs that had been delivered and had shown effectiveness in seminar formats [13]. Topics selected for the SCOPE intervention’s five teaching modules were: (1) Principles of Effective Communication; (2) Recognizing Empathic Opportunities; (3) Responding to Empathic Opportunities; (4) Conveying Prognosis; (5) Answering Difficult Questions. Module 6 summarized main points from Modules 1–5 and included extra examples.
Having delineated the modules, we next identified important concepts in each. The overall approach was to introduce a concept, include a video clip demonstrating how the concept can be applied, summarize the important teaching points, and give users opportunity to listen to selected portions of their own recorded conversations to hear how they had communicated in regard to the concept. Voice-overs were custom produced using narration by professional actors. However, rather than producing all new video examples, we selected high-quality content from pre-existing programs and received permission to include these clips in the SCOPE CD-ROM (Table 1).1
Table 1.
Modules in the SCOPE CD-ROM.
1. Principles of Effective Communication
|
2. Recognizing Empathic Opportunities
|
3. Responding to Empathic Opportunities
|
4. Conveying Prognosis
|
5. Responding to Difficult Questions
|
6. Summary |
With this overall plan in mind, we created an “intervention development grid” for the introduction section and the five modules. The grid listed each concept to be addressed, the theoretical rationale for including it in the module, the video clip to be included, the script for audio voice-over that would precede and/or follow the clip, and bulleted or summary text that would appear on the screen during the voice-over. Sample cells from the intervention grid appear in Table 2.
Table 2.
Sample cells from SCOPE intervention development grid.
| Theoretical construct | Concept | Visual/audio image | Voiceover wording |
|---|---|---|---|
| Barriers (Module 2: Responding to Patient Emotion) | Oncologists’ own emotions make it hard to deal with patients’ | Video clips from:
|
In situations like this oncologist just described, it’s sometimes easier to avoid engaging patients’ emotions all together. That’s because your own emotions, in response, may feel overwhelming. As painful as your own feelings may be, they are a window to understanding what your patient feels. With this awareness of your own emotions comes the ability to empathize and comfort. The bottom line is that paying attention to your own emotion can help you manage patient distress |
| Skill building (Module 3: Responding to Empathic Opportunities) | Recognizing empathic opportunities | Video clips from:
|
Here are some examples of empathic opportunities that sound similar to things you have heard in your own practice [video clip] Now, here are actual examples from your conversations [audio clip from MD/patient recordings] |
| Skill building (Module 4: Conveying Prognosis) | Use the Ask-Tell-Ask Method | Video clip from:
|
There is almost no more important time to use Ask-Tell-Ask then when conveying prognosis. First, Ask what the patient knows or believes about the prognosis. This can help you know where they are emotionally and cognitively. It helps you understand how they’re doing. Some patients know about survival statistics for their type of cancer. Some have different belief systems to help them understand their prognosis. Knowing this going in will help you communicate most effectively |
The SCOPE CD-ROM was comprised 145 screens and 23 video clips. Each oncologist’s copy of the CD-ROM also included up to 12 audio clips from his or her own recorded encounters with patients. Audio clips to be included were identified via the following steps. First, the audio-recorded data were coded using a software program we developed called ENCOUNTER. In this program, coders marked conversation segments in which our targeted behaviors occurred [8]. For example, coders marked every instance of an empathic opportunity as well as instances in which the oncologist used an emotion handling technique emphasized in the SCOPE CD-ROM. When tailoring a copy of the SCOPE intervention for a particular oncologist, members of the intervention development team searched his or her coded audio recordings to select relevant key segments and, if available, inserted these audio clips so the user could “click to hear your examples of emotion handling skills.” The intervention developers wrote a number of feedback messages (e.g., “next time you might want to try naming the patient’s concern”) that were narrated so that, when oncologists listened to their examples, they also received tailored feedback. Therefore, each user received a version of the CD-ROM tailored to his or her individual audio-recorded data. Oncologists in the intervention group also received a second CD-ROM with full “raw” (uncoded) audios of all their conversations recorded through the study. Audio clips that had been included as their own examples on the SCOPE CD-ROM were identified by time segment from the original conversation available on this second CD-ROM so oncologists could locate and listen to more of the conversation from which the example was selected.
Although the computerized intervention was based on in-person educational interventions that had previously demonstrated success, we assessed its validity further by having drafts of the modules pre-tested and evaluated by three practicing oncologists not enrolled in the trial. Each was asked to evaluate format, content, and sample video clips to ensure the intervention was appropriate for oncologists and communicated clearly. Comments were returned in written form and incorporated into the final CD-ROM.
2.2.3. Format and delivery
The resulting SCOPE program operated as follows. Users launched the program from the CD-ROM and proceeded through the program by clicking to advance from one section to the other. A navigation system was included to allow users to “jump around”, but navigational instructions encouraged users to first use the entire CD-ROM linearly. Consistent with findings from a recent meta-analysis indicating health professionals prefer single-instance rather than ongoing-access internet-based interventions [20], the intent was that oncologists would view the CD-ROM in its entirety once rather than multiple times.
At the end of each of the first four modules, the program asked users to set goals for changing their communications, based on what they had learned in the module, and to enter these goals into a form within the program. Entries were captured in a tracking database and four weekly e-mails from “The SCOPE Project” were sent in follow-up, asking whether the oncologist had tried the skill and how it was working. Sample content from one of these sections appears in Table 3.
Table 3.
Sample content from goals for changing communications.
1. Check the techniques you will try
|
2. Write two things you will do in your next clinic session or hospital rounds to help you recognize or elicit empathic opportunities |
3. Pick two skills to try out over the next week
|
4. What open-ended questions might you use to find out:
|
2.3. Measures
2.3.1. Use of the CD-ROM
There were two techniques for measuring outcomes assessed in this report. First, for oncologists who used the CD-ROM while connected to the internet, usage data were captured and transmitted in real time to a database on a central server. Data captured included start and stop times (users were able to use the CD-ROM as often as they wished), whether each module and section within each module was visited, and data entered in sections that requested user input (such as goals recorded or action steps agreed to be undertaken by the user). We also asked all oncologists how much of the CD-ROM they had reviewed. Response options were: none (did not open it), reviewed some of it, reviewed most of it, and reviewed all of it.
2.3.2. Reactions to the CD-ROM
The follow-up oncologist survey included items measuring reactions to the SCOPE intervention. We developed each of the items to correspond directly to the SCOPE intervention modules and pre-tested them with the same group of oncologists who suggested revisions for the CD-ROM. The question format was modeled on items from our previous research [31]. Oncologists used a 5-point scale to rate helpfulness of the CD-ROM for understanding importance of responding to patients’ emotions and learning how to: use Ask-Tell-Ask when conveying information; identify empathic opportunities; use emotion-handling skills (Name, Understand, Respect, Support, Explore, and Wish statements); use Ask-Tell-Ask when having a discussion about prognosis, and address emotions that underlie difficult questions. Responses were: 1 = not helpful; 2 = a little helpful; 3 = somewhat helpful; 4 = fairly helpful; 5 = very helpful.
Perceived impact was also measured on a 5-point scale via these items developed by the research team and mapping back to the intervention goals: How much impact do you think the CD-ROM will have on your effectiveness in communicating with patients?; How much do you think the CD-ROM will assist you with challenging conversations?; Overall, how much did you feel the CD-ROM was worth your time?; To what degree did you use the skills presented in the CD-ROM before watching the CD-ROM?; After using the CD-ROM; To what degree to you think you will increase the use of skills presented in the CD-ROM? We included 2 items assessing how much oncologists thought it would impact their practice. For all these items, responses were: 1 = none; 2 = a little; 3 = somewhat; 4 = a good amount; 5 = a great deal. Finally, a dichotomous (yes/no) item asked, Since reviewing the CD-ROM, have you made any changes in your clinical practice?
2.4. Analyses procedures
Analyses for this report are descriptive. Usage data were summarized by means, medians, and inter-quartile range. These summaries were used to describe average CD-ROM use at the oncologist level and by module and section level to determine whether oncologists spent more time with certain modules than others. In addition, response frequencies were calculated for the perceived helpfulness and impact measures as well as mean and median response values.
3. Results
3.1. Characteristics of participating oncologists
As shown in Table 4, the 24 participating oncologists who were assigned to the SCOPE intervention group were primarily white and male, with mean age just under 50 and, on average, close to 20 years post-fellowship.
Table 4.
Characteristics of oncologists assigned to receive the SCOPE CD-ROM.
| Variable | Physicians (n = 24) |
|---|---|
| Age | 48.8 (9.3) |
| White (%) | 66.7 |
| Male (%) | 79.2 |
| Years since fellowship | 19.3 (9.6) |
3.2. Use of the CD-ROM
Of these 24 intervention group participants, 18 (75%) used the CD-ROM while connected to the internet, allowing for verification of their CD-ROM use. Among the 6 (25%) for whom we do not have verified data via their computer uploads, 3 (12.5%) reported having used the CD-ROM’s training modules and are thus included in these analyses.
Of the 18 oncologists who used the CD-ROM while logged into the internet, 6 did not log out properly. Therefore, we have data regarding their numbers of logins and which sections they viewed but, without the start and stop times, we are unable to document their total usage. Among the 12 for whom we have documented usage time, median number of minutes spent logged into the CD-ROM was 63.8 (IQR = (58.2, 99.3); mean = 83.6; SD = 36.81).
All 18 oncologists for whom we have verified usage data viewed all five teaching modules. Most (11 of 18) who used the CD-ROM while logged into the internet logged in only once. Five logged in twice, one logged in 3 times and one logged in 4 times.
According to oncologists’ self-reports of how much of the CD-ROM they had reviewed, 8.3% did not review any of the CD, 12.5% reviewed some of it, 20.8% reviewed most of it, and 58.3% reviewed all of it.
3.3. Reactions to the CD-ROM
In the follow-up survey, the 21 oncologists who reported having used the CD-ROM responded to 6 items assessing perceived helpfulness. As shown in Table 5 and explained in Section 2.3.2, these items map directly to the CD-ROM’s modules. For the perceived helpfulness, mean responses were similar for all items, ranging from 3.8 to 4.0 (see Table 5).
Table 5.
Perceptions of the CD-ROM’s helpfulness and impact (n = 21).
| N | Mean (SD) | Median | |
|---|---|---|---|
| Helpfulness of the CD-ROM on: (1 = not at all helpful; 5 = very helpful) | |||
| Understanding importance of responding to emotions | 21 | 3.8. (0.9) | 4.0 |
| Learning to use Ask-Tell-Ask when conveying info | 21 | 4.0 (0.8) | 4.0 |
| Learning to ID empathic opportunities | 21 | 4.0 (0.8) | 4.0 |
| Learning to use Emotion-handling Skills | 21 | 3.8 (1.0) | 4.0 |
| Learning to use Ask-Tell-Ask when discussing prognosis | 21 | 3.8 (1.1) | 4.0 |
| Learning to address emotions that underlie difficult questions | 21 | 3.8 (0.7) | 4.0 |
| Impact of the CD-ROM on: (1 = none; 5 = a great deal) | |||
| Effectiveness in communicating by patients | 21 | 3.1 (0.8) | 3.0 |
| Assistance in challenging conversations | 21 | 3.0 (0.8) | 3.0 |
| Perceived use of skills presented in the CD-ROM: (1 = none; 5 = a great deal) | |||
| Before using the CD-ROM | 21 | 2.8 (0.7) | 3.0 |
| After using the CD-ROM | 21 | 3.2 (0.6) | 3.0 |
The 3 items for which more than half of the oncologists rated the helpfulness in category 4 or 5 were: learning to use Ask-Tell-Ask when conveying information, learning to identify empathic opportunities, and learning to address emotions that underlie difficult questions (76.2%, 76.2%, and 66.7%, respectively; data not shown).
Oncologists’ mean assessment of the CD-ROM’s impact on their effectiveness in communicating with patients was 3.1, on a scale from 1 to 5, and mean assessment of its assistance in their challenging conversations was 3.0. Mean assessment of whether using the CD-ROM was worth their time, also measured on the 5-point scale was 3.6.
The follow-up survey also asked oncologists to indicate their perception of how often they had used the skills before and then after using the CD-ROM. Means of these responses on the 1–5 interval scale were 2.8 before using the CD-ROM and 3.2 afterward (see Table 5). There were 14.3% who said they had used the skills “a good amount” before using the program and 33.3% who said they increased their use of the skills “a good amount” after (data not shown).
When asked whether they had made any changes in their practice since reviewing the CD-ROM, 19 of the 21 oncologists who used the program (90.5%) responded affirmatively.
4. Discussion and conclusion
4.1. Discussion
The SCOPE intervention seeks to take theory-based training that has been successful in seminar classroom-style delivery and use interactive multimedia (voice-overs, video, and print) to provide similar training through a self-directed CD-ROM format that depends on voluntary use. The main outcome evaluation for the SCOPE trial will be is its education impact—whether use of the CD-ROM facilitates changes in oncologist communication with patients as indicated by their conversations recorded pre- and post-intervention. However, an important process evaluation outcome is whether busy oncologists use the CD-ROM and what their reactions are to it.
Exposure is important to assess because use of the CD-ROM is voluntary (much like readership of printed material), and there is no chance for an intervention to have an impact without the intended audience being exposed to it. Indeed, behavior change has been found to be more likely among those with greater intervention exposure [32].
Whether physicians will voluntarily use an intervention is an important factor in the feasibility of dissemination. That very few computer-based medical education intervention studies have reported rates of use may stem from the fact that, for interventions available via the web, the denominator of potential users is rarely known.
The few computerized medical education interventions studies that have tracked use have varied results. A pediatric emergency department education program designed for residents to use on a voluntary basis was used by 29%, with mean usage time being 22 min [33]; in a German study, 87% of medical students voluntarily accessed available web-based programs [22]; an evaluation of a computerized decision support program for physician orders in the U.S. found significantly more change of physician behavior if the program was automatically provided than if intended users had to take the initiative to access it [21]. This study contributes to the literature by reporting usage rates for a CD-ROM-based educational intervention that depends on oncologists’ voluntary usage.
It was encouraging that more than 90% of oncologists assigned to the intervention group reported having reviewed at least some of the CD-ROM, with 58% reporting having reviewed all of it. We had expected that the CD-ROM would take about an hour to review and, indeed, mean confirmed time from those who viewed the CD-ROM while connected to the internet was 63.8 min. However, readers should note that because usage was evaluated in the context of a controlled trial with only 24 oncologists per group and in which oncologists received personalized encouragement to use the CD-ROM, these findings cannot be generalized to predict usage if the CD-ROMS were widely distributed. Also, because not all oncologists used the CD-ROM while connected to the internet, our usage data are incomplete. Although we analyzed responses from 21 of the 24 oncologists in the intervention group who reported having used the CD-ROM, we can only verify use for the 18 who used the CD-ROM while logged onto the internet.
Perception of the helpfulness of the CD-ROM among oncologists who used it was positive—ranging from 3.8 to 4.0 on a 5-point scale. The most highly rated items (receiving a 4 or 5 by 76.2% of users) were Learning to use Ask-Tell-Ask and Learning how to identify empathic opportunities. Impact on practice scores were lower than perceived helpfulness, but this is not surprising given that saying using the CD-ROM would change their practice “a great deal” would require oncologists’ implicit admission that there had been a great deal about their practice that needed to change. That most oncologists stated the intervention would change their practice at all we view as positive.
Finally, responses on the follow-up survey show perception among intervention group participants that their use of the skills taught in the CD-ROM had increased from the beginning of the study to the end and that the CD-ROM was worth their time. 90.5% responded affirmatively when asked whether they had made any change in their practice following use of the CD.
4.2. Conclusion
If ultimately found effective in changing oncologist communication with patients, widespread dissemination of the SCOPE CD-ROM should be explored.
I confirm all patient/personal identifiers have been removed or disguised so the patient/person(s) described are not identifiable and cannot be identified through the details of the story.
4.3. Practice implications
These preliminary findings suggest that the tailored interactive SCOPE CD-ROM has promise for being used and accepted by oncologists. The CD-ROM users in this trial (>90% of those assigned to the intervention) perceived the interventions as being helpful and having an impact on their practice.
Acknowledgments
The authors thank participating oncologists and patients for allowing their conversations to be recorded and oncologists for their willingness to receive feedback. We also thank Sandra Blankenship for her help in preparing this manuscript.
Footnotes
On the Edge of Being, Cerenex Pharmaceuticals, 1993. On Being an Oncologist, The University of Texas M.D. Anderson Cancer Center, 2002. On our own Terms: Moyers on Dying, Films for the Humanities & Sciences®, 2000. A Practical Guide to Communication Skills in Clinical Practice, Medical Audio Visual Communications, Inc., 1998. EPEC-O: Education in Palliative and End-of-life Care—Oncology, Emanuel LL, Ferris FD, von Gunten CF, Von Roenn J., The EPEC TM Project, Chicago, IL, 2005.
This work was funded by a grant from the National Cancer Institute (R01-CA100387-01).
Publisher's Disclaimer: This article appeared in a journal published by Elsevier. The attached copy is furnished to the author for internal non-commercial research and education use, including for instruction at the authors institution and sharing with colleagues.
Other uses, including reproduction and distribution, or selling or licensing copies, or posting to personal, institutional or third party websites are prohibited.
In most cases authors are permitted to post their version of the article (e.g. in Word or Tex form) to their personal website or institutional repository. Authors requiring further information regarding Elsevier’s archiving and manuscript policies are encouraged to visit:
References
- 1.Maguire P. Can communication skills be taught? Brit J Hosp Med. 1990;43:215–6. [PubMed] [Google Scholar]
- 2.Stewart MA. Effective physician–patient communication and health outcomes: a review. CMAJ. 1995;152:1423–33. [PMC free article] [PubMed] [Google Scholar]
- 3.Tulsky JA, Chesney MA, Lo B. See one, do one, teach one? House staff experience discussing do-not-resuscitate orders. Arch Intern Med. 1996;156:1285–9. doi: 10.1001/archinte.156.12.1285. [DOI] [PubMed] [Google Scholar]
- 4.Morita T, Akechi T, Ikenaga M, Kizawa Y, Kohara H, Mukaiyama T, Nakaho T, Nakashima N, Shima Y, Matsubara T, Fujimori M, Uchitomi Y. Communication about the ending of anticancer treatment and transition to palliative care. Ann Oncol. 2004;15:1551–7. doi: 10.1093/annonc/mdh386. [DOI] [PubMed] [Google Scholar]
- 5.Hagerty RG, Butow PN, Ellis PM, Lobb EA, Pendlebury SC, Leighl N, MacLeod C, Tattersall MH. Communicating with realism and hope: incurable cancer patients’ views on the disclosure of prognosis. J Clin Oncol. 2005;23:1278–88. doi: 10.1200/JCO.2005.11.138. [DOI] [PubMed] [Google Scholar]
- 6.Tulsky JA. Beyond advance directives: importance of communication skills at the end of life. J Am Med Assoc. 2005;294:359–65. doi: 10.1001/jama.294.3.359. [DOI] [PubMed] [Google Scholar]
- 7.Foley KM, Gelband H National Cancer Policy Board (U.S.), NRC. Improving palliative care for cancer: summary and recommendations. Washington (DC): National Academy Press; 2001. [PubMed] [Google Scholar]
- 8.Pollak KI, Arnold RM, Jeffreys AS, Alexander SC, Olsen MK, Abernethy AP, Skinner CS, Rodriguez KL, Tulsky JA. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol. 2007;25:5748–52. doi: 10.1200/JCO.2007.12.4180. [DOI] [PubMed] [Google Scholar]
- 9.Anon Approaching death: improving care at the end of life—a report of the Institute of Medicine. Health Serv Res. 1998;33:1–3. [PMC free article] [PubMed] [Google Scholar]
- 10.Levinson W. Physician–patient communication. A key to malpractice prevention. J Am Med Assoc. 1994;272:1619–20. [PubMed] [Google Scholar]
- 11.Turk DC, Feldman CS. Facilitating the use of noninvasive pain management strategies with the terminally ill. Hosp J. 1992;8:193–214. doi: 10.1080/0742-969x.1992.11882725. [DOI] [PubMed] [Google Scholar]
- 12.Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, Eves R. Efficacy of a Cancer Research UK communication skills training model for oncologists: a randomised controlled trial. Lancet. 2002;359:650–6. doi: 10.1016/S0140-6736(02)07810-8. [DOI] [PubMed] [Google Scholar]
- 13.Back AL, Arnold RM, Baile WF, Fryer-Edwards KA, Alexander SC, Barley GE, Gooley TA, Tulsky JA. Efficacy of communication skills training for giving bad news and discussing transitions to palliative care. Arch Intern Med. 2007;167:453–60. doi: 10.1001/archinte.167.5.453. [DOI] [PubMed] [Google Scholar]
- 14.Campbell MK, DeVellis BM, Strecher VJ, Ammerman AS, DeVellis RF, Sandler RS. Improving dietary behavior: the effectiveness of tailored messages in primary care settings. Am J Public Health. 1994;84:783–7. doi: 10.2105/ajph.84.5.783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Strecher VJ, Kreuter M, Den Boer DJ, Kobrin S, Hospers HJ, Skinner CS. The effects of computer-tailored smoking cessation messages in family practice settings. J Fam Pract. 1994;39:262–70. [PubMed] [Google Scholar]
- 16.Skinner CS, Strecher VJ, Hospers H. Physicians’ recommendations for mammography: do tailored messages make a difference? Am J Public Health. 1994;84:43–9. doi: 10.2105/ajph.84.1.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Skinner CS, Campbell MK, Rimer BK, Curry S, Prochaska JO. How effective is tailored print communication? Ann Behav Med. 1999;21:290–8. doi: 10.1007/BF02895960. [DOI] [PubMed] [Google Scholar]
- 18.Gustafson DH, Hawkins RP, Boberg EW, Bricker E, Pingree S, Chan CL. Proc Annu Symp Comput Appl Med Care. 1994. The use and impact of a computer-based support system for people living with AIDS and HIV infection; pp. 604–8. [PMC free article] [PubMed] [Google Scholar]
- 19.Gustafson DH, McTavish FM, Stengle W, Ballard D, Hawkins R, Shaw BR, Jones E, Julesberg K, McDowell H, Chen WC, Volrathongchai K, Landucci G. Use and impact of eHealth system by low-income women with breast cancer. J Health Commun. 2005;10(Suppl 1):195–218. doi: 10.1080/10810730500263257. [DOI] [PubMed] [Google Scholar]
- 20.Cook DA, Levinson AJ, Garside S, Dupras DM, Erwin PJ, Montori VM. Internet-based learning in the health professions: a meta-analysis. J Am Med Assoc. 2008;300:1181–96. doi: 10.1001/jama.300.10.1181. [DOI] [PubMed] [Google Scholar]
- 21.Kawamoto K, Lobach DF. Clinical decision support provided within physician order entry systems: a systematic review of features effective for changing clinician behavior. AMIA Annu Symp Proc. 2003:361–5. [PMC free article] [PubMed] [Google Scholar]
- 22.Schultze-Mosgau S, Zielinski T, Lochner J. Web-based, virtual course units as a didactic concept for medical teaching. Med Teach. 2004;26:336–42. doi: 10.1080/01421590410001679028. [DOI] [PubMed] [Google Scholar]
- 23.Pusic MV, Johnson, Kevin B, Duggan, Anne K. Utilization of a pediatric emergency Department Education Computer. Arch Pediatr Adolesc Med. 2001;155:129–34. doi: 10.1001/archpedi.155.2.129. [DOI] [PubMed] [Google Scholar]
- 24.Koropchak CM, Pollak KI, Arnold RM, Alexander SC, Skinner CS, Olsen MK, Jeffreys AS, Rodriguez KL, Abernethy AP, Tulsky JA. Studying communication in oncologist–patient encounters: the SCOPE Trial. Palliat Med. 2006;20:813–9. doi: 10.1177/0269216306070657. [DOI] [PubMed] [Google Scholar]
- 25.Pocock SJ. Allocation of patients to treatment in clinical trials. Biometrics. 1979;35:183–97. [PubMed] [Google Scholar]
- 26.White SJ, Freedman LS. Allocation of patients to treatment groups in a controlled clinical study. Br J Cancer. 1978;37:849–57. doi: 10.1038/bjc.1978.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Miller JH, Moyers T. Motivational interviewing in substance abuse: applications for occupational medicine. Occup Med. 2002;17:51–65. iv. [PubMed] [Google Scholar]
- 28.Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs (NJ): Prentice Hall, Inc; 1986. [Google Scholar]
- 29.Cabana MD, Rand CS, Powe NR, Wu AW, Wilson MH, Abboud PA, Rubin HR. Why don’t physicians follow clinical practice guidelines? A framework for improvement. J Am Med Assoc. 1999;282:1458–65. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
- 30.Butow PN, Brown RF, Cogar S, Tattersall MH, Dunn SM. Oncologists’ reactions to cancer patients’ verbal cues. Psychooncology. 2002;11:47–58. doi: 10.1002/pon.556. [DOI] [PubMed] [Google Scholar]
- 31.Skinner CS, Rawl SM, Moser BK, Buchanan AH, Scott LL, Champion VL, Schildkraut JM, Parmigiani G, Clark S, Lobach DF, Bastian LA. Impact of the cancer risk intake system on patient–clinician discussions of tamoxifen, genetic counseling, and colonoscopy. J Gen Intern Med. 2005;20:360–5. doi: 10.1111/j.1525-1497.2005.40115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Japuntich SJ, Zehner ME, Smith SS, Jorenby DE, Valdez JA, Fiore MC, Baker TB, Gustafson DH. Smoking cessation via the internet: a randomized clinical trial of an internet intervention as adjuvant treatment in a smoking cessation intervention. Nicotine Tob Res. 2006;8(Suppl 1):S59–67. doi: 10.1080/14622200601047900. [DOI] [PubMed] [Google Scholar]
- 33.Pusic MV. Pediatric residents: are they ready to use computer-aided instruction? Arch Pediatr Adolesc Med. 1998;152:494–8. doi: 10.1001/archpedi.152.5.494. [DOI] [PubMed] [Google Scholar]


