Abstract
Background
Older adults with poor functioning preoperatively are at risk for delayed recovery and more impaired outcomes following CABS.
Purpose
To determine if a 6-week early recovery telehealth intervention, designed to improve self-efficacy and management related to symptoms following CABS, was effective in improving outcomes (physical activity, physiological and psychological functioning) for older adults (> 65 years old) with higher disease burden.
Design
A descriptive, repeated measures experimental design was used. Follow-up data was collected at 3- and 6-weeks and 3-months after CABS.
Sample
Subjects were drawn from a larger randomized clinical trial (RCT). Parent study subjects who had high disease burden preoperatively [physical component score of <50 on the Medical Outcome Study Short Form 36 (MOS SF-36) and a RISKO score of > 6], were included (N=55); with 23 subjects in the early recovery intervention group and 31 subjects in the usual care group (n=31). Subjects ranged from 65–85 years old (M=71.6 + 5.1).
Findings
There was a significant main effect by group [F(1,209)=4.66, p<.05), the intervention group had a least square means of 27.9 kcal/kg/day of energy expenditure compared to the usual care group of 26.6 kcal/kg/day per the RT3® accelerometer. Both groups had significantly improved physical [F(2,171)=3.26, p<.05] and role-physical [F(2,171)=6.64, p<.005] functioning over time.
Conclusions
The subgroup of CABS subjects with high disease burden was responsive to an early recovery telehealth intervention. Improving patients’ physical activity and functioning can reduce morbidity and mortality associated with poor functioning after cardiac events.
Keywords: Coronary Artery Bypass Surgery, older adults, physical activity outcomes, functioning outcomes, disease burden
INTRODUCTION
Following coronary artery bypass surgery (CABS), many older adults are able to return to a comparable or improved health-related quality of life (HRQoL) as compared to their preoperative status.1–4 Some older adults do not achieve the beneficial outcomes that can be realized from revascularization due to preexisting pre-procedural factors. Those older adults who are at risk for poor outcomes after revascularization are less physically active;5–8 have coexisting cardiac disease and other comorbidities;9,10 have poor functional capacity11 and have physical functioning impairments prior to their cardiac procedure.12 Regardless, older adults with heart disease and a compromised health status can derive significant cardiovascular benefits and improved HRQoL from physical activity and exercise.13 Several studies have examined interventions, including cardiac rehabilitation participation, to improve outcomes after CABS.14–24 Only a limited number of studies have specifically investigated cardiac patients at risk for poor outcomes, such as multiple comorbidities or multiple cardiovascular risk factors.16,17,25–27 No studies to date have specifically examined the influence of post-CABS interventions on those patients with high coronary artery disease burden (patients with compromised physical functioning and multiple CAD risk factors), who are at risk for impaired functioning and delayed recovery after CABS. It is important to further study patients at risk for poor outcomes after CABS in order to develop interventions that can minimize delays in recovery or avert morbidity and mortality after CABS. Specifically, this paper will examine a subgroup of CABS patients who had high disease burden preoperatively to determine the effects of an early recovery telehealth intervention on physical activity and physical and psychosocial functioning.
RELATED LITERATURE
Functioning improvements after cardiac revascularization appear to improve linearly over time.1,3,28,28–30 However, recent studies indicate that pre-procedural comorbidities9,10,31, illness severity,2,32 daily functioning abilities33 and functional status34,35 can predict health-related quality of life (HRQoL) and recovery of functioning after cardiac revascularization. These findings corroborate the conclusion that there are cardiac patients who do not experience improved health status or HRQoL, and may actually experience impaired or delayed recovery of functioning, as well as have disability after CABS.2,10,28,34,36
Physical activity and exercise are the foundation for improving functioning outcomes for patients after cardiac rehabilitation, particularly for those patients at risk for poor outcomes.23,37,38 Multiple factors are associated with the lack of physical activity and exercise by older adults after CABS. Factors contributing to ongoing physical inactivity after cardiac revascularization include patients’ relatively short hospitalizations, which limits the time for patient education and gaining an understanding of their physical activity prescription. Older adults have lower rate of cardiac rehabilitation (CR) program participation39 related to the lack of physician referral, CR program costs, access, low patient motivation; as well as being physically inactive and having a sedentary lifestyle, disability related to pre-existing comorbidities, caregiving responsibilities and lack of transportation.5–8,40,41 Older adults’ physical activity and exercise are further limited by fatigue,7,42 lack of social support, beliefs that older people cannot change or exercise,43,44 low outcome expectations,45 dislike of exercise, perceptions of physical activity as too strenuous43 and costs (e.g., exercise facility fees).5,46 Interventions that can help high risk older adults initiate a more physically active lifestyle after CABS may reduce the delays in recovery and associated adverse effects associated with poor functioning after CABS.
The purpose of this study was to conduct additional analyses of a randomized clinical trial (RCT) to determine if there were differences in response to an early recovery telehealth intervention among elderly patients (≥ 65 years old) with high disease burden in the early recovery period after CABS (3- and 6-weeks, and 3- and 6-months). The specific aims of this study were to determine if there were differences by group (intervention group or usual care group only) on: a) physical activity and b) physical and psychosocial functioning.
CONCEPTUAL FRAMEWORK
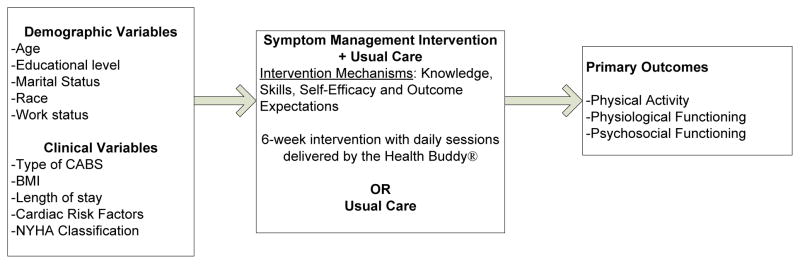
The early recovery telehealth intervention in this study focused on using symptom management strategies to improve physical activity and functioning outcomes after CABS. The conceptual framework used for this study and the development of the intervention was based upon the health outcomes research 47 and the symptom management 48 conceptual models. In the symptom management model, it is assumed that the person, environment and health and illness domains are affected by specific knowledge, skills, self-efficacy and outcome expectations which effect the patient’s ability to manage his/her symptoms and promote improved outcomes. In this study, the early recovery telehealth intervention provided patients with strategies and reinforcement to manage commonly occurring symptoms, and did not just focus on the use of physical activity and exercise after CABS. The outcomes targeted in the study were improving physical activity and functioning (physiological and psychosocial); which are relevant HRQOL outcomes as supported by Donabedian.47 See Figure 1. For example, following CABS, patients need to know how to assess their symptoms such as pain (onset, location, duration, intensity frequency); have the skills to monitor their symptoms; and have self-efficacy in their ability to assess their symptoms accurately and take action (e.g., take analgesic, rest, elevate extremities) based upon their assessment. Outcomes resulting from patients’ use of strategies to manage their symptoms include improved functioning.
Figure 1.
Conceptual framework used for the Study
METHODS
Design
In the parent study, a randomized, two-group (N = 280) repeated measures design was used; with one group receiving the early recovery telehealth intervention plus usual care (UC) and the comparison group received usual care only. Data measurements were obtained prior to discharge (baseline measures), 3- and 6-weeks, and 3- and 6-months postoperatively among older adults (≥ 65 years old) who had undergone CABS. The 6-week symptom management telehealth intervention, developed by the investigators,49 was delivered by a telehealth device, the Health Buddy®, that connected to the subject’s telephone line. The 42-daily sessions of the intervention were designed to improve patients’ self-efficacy and skills related to self-care management of early recovery symptoms and improve outcomes (physical activity and functioning). In the daily intervention sessions, subjects responded to assessment queries and were provided with strategies (e.g., sleep hygiene techniques, relieving anxiety, monitoring individual progress in response to increasing physical activity as per exercise prescription) based upon the subject’s responses of the symptoms he/she was currently experiencing. Information and detail specific to the intervention used in this study has been published and can referenced for further description of the intervention components and how the intervention was tailored based upon subjects’ responses to the daily sessions.49
Sample
In the parent study, 280 subjects, recruited from tertiary, Midwestern hospitals provided written informed consent and participated in the study. Data analysis from the parent study was conducted on 232 subjects; as there were 34 (23.8%) subjects in the intervention group and 15 (11%) subjects in the usual care group that did not receive the allocated intervention or study follow-up as planned, due to: a) subject burden (n=36), b) rehospitalizations or transfer to extended care facility (n=4), c) equipment malfunction (n=3), d) inability to reach subject per telephone for follow-up data collection (n=2); and e) inability to complete the intervention protocol (n=3).
In this study, a sub-analysis was conducted on data from the parent study, and included 55 subjects from the parent study who met the criteria of preoperative high disease burden; and, therefore were included in the data analysis. There were 24 subjects in the early recovery telehealth intervention group, and 31 subjects in the usual care (routine care) group. Criteria for preoperative high disease burden were having a RISKO Heart Hazard Appraisal score ≥ 6 and a MOS SF-36 physical component score < 50. Having a lower than median score on the physical component scale of the MOS SF-36 has been used to predict physical functioning at 6-months after cardiac revascularization (i.e., PCI) by other researchers.50 The RISKO Heart Health Hazard Appraisal51 has been used as a measure of coronary artery disease (CAD) burden; with higher scores associated with more impaired functioning prior to CABS.52 RISKO evaluates the four most modifiable heart disease risk factors (blood pressure, body weight, serum cholesterol level, and use of tobacco). Scores on the RISKO can range from 0 to 27 and risk adjusted if the patient has Diabetes Mellitus, which increases the score; with higher RISKO scores indicating higher risk of heart disease.
The sample in this study was comprised of 84% men (n=46) and 16% women (n=9); with 87% of the sample being married. The mean age of subjects was 71.6 (± 5.1) years. The majority of the sample was Caucasian, with only one non-Caucasian participant. Overall 49% of the subjects reported working outside of the home at the time of their CABS. There were no statistically or clinically significant group differences on demographic (e.g., age, hospital length of stay, marital status) or baseline clinical variables (e.g., body mass index, cardiac risk factors). After hospitalization, 82.4% of the subjects (N=55) participated in a cardiac rehabilitation (CR) program; there were no statistically significant differences in CR program participation by group (treatment group=79.2%, usual care group=85.2%).
Data Collection
Data was obtained by the research nurse while the subjects were hospitalized and included the demographic and clinical characteristics data from subject report and hospital record, as well as per subject interview to complete the baseline measures of the MOS SF-36 and the Modified 7-day activity interview. At the follow-up times of 3-and 6-weeks and 3- and 6-months after CABS, physical activity was measured by having subjects wear an RT3® accelerometer (Stayhealthy, Inc., Monrovia, CA) for three consecutive days (2 weekdays and 1 weekend day) and complete a self-report of activity diary for the same 3-day period. Follow-up survey data were collected by telephone interview conducted by the same research nurse at each time period (6-weeks and 3- and 6-months after CABS) to obtain their responses to the measures of psychosocial and physiologic functioning using the MOS SF-36 tool.
Measurement of Variables
Modified 7- Day Activity Interview measured the subject’s reported baseline physical activity level that they were capable of before undergoing CABS (total kcal/day expended, average kcal/kg/day expended, average minutes/day spent in moderate or greater activity).53 The total kilocalories per kg of body weight expended per day and total calories expended per day were derived from subjects’ reported number of hours per day in sleep and in light, moderate, hard and very hard activity (based on metabolic equivalent [MET] levels). The original 7-day activity interview instrument54 had a reported two-week test-retest reliability of 0.67 for kcal/day.55 Significant differences (z=−6.14, p<.0001) between the measured kcal/kg/day comparing active and inactive groups of older adults demonstrated concurrent validity.53. Construct validity of the instrument was supported by the significant differences (z=−3.06, p<.005) between the kcal/kg/day from week 1 to week 12 during CR participation of older adult subjects; the significant correlation between change in mean kcal/day expended and estimated VO2max (Spearman’s rho=.28, p<.05); and the significant correlation (Spearman’s rho=0.31, p<.05 at week 1 and r=.50, p<.001 at week 12) between the subjects’ global self-estimate of physical activity and their kcal/kg/day measured by the tool.56 In comparing the rank ordering of energy expenditure of active (n=30) and inactive (n=30) older adults using both the original 7-day interview and modified 7-day interview, there was a greater discrimination (a greater dispersion of scores) among the activity levels of the subjects using the modified 7-day interview, due to the inclusion of lower intensity activities included in the modified version of the tool.53
RT3® Accelerometer, a triaxial accelerometer, measures body motion (specifically, the electrical energy of acceleration and deceleration) during activities that involve energy cost. It provided an objective measure of subject’s physical activity. The RT3® is approximately the size and weight of a pager. Subjects wore the accelerometer continuously, except during sleeping times, for three consecutive days each data collection period. Accelerations are detected from three plane (vertical, horizontal, and anterior-posterior) and are internally stored and converted to quantifiable digital signals, referred to as “activity counts”; these counts were converted to kcals expended to derive measures of average daily activity counts, kcals expended/day, and kcal/kg/day expended. Triaxial accelerometers have documented validity, with correlations between the Triaxial accelerometer and indirect calorimetry ranging from .86–.96,57,58 of .85 with SVO 259 and .95 with V02.60 Generalizability coefficients (ICCs) for the RT3® based on a 3-day period of data collection at three data collection points over time were high (.85 – .97).61
Activity Diary was completed by subjects. They recorded the amount of time they spent in various physical activities (light, moderate, hard, very hard) and sleep. Categories to group physical activities were adapted from the Modified 7-Day Activity Interview.53. The diary was used on the same three days that subjects wore the RT3® accelerometer at follow-up times. The diary provided data on: a) mean number of minutes spent in light, moderate, hard, and very hard levels of physical activity, b) types of exercise modes used, c) time of day of exercise sessions and d) duration and distances (if applicable) of exercise sessions. Three-day activity diaries, such as the one used in this study, are commonly used to obtain activity data.62.
Physical and Psychosocial Functioning
The Medical Outcomes Study Short Form-36 (MOS SF-36, version 2.0)63 is comprised of 36-items and was used to measure the physical and psychosocial functioning. It measures eight health concepts, assessing both psychosocial and physical functioning. Physiological subscales include: physical functioning, limitations in role functioning due to physical problems (role physical), bodily pain, and general health. Psychosocial subscales include: limitations in role functioning due to emotional problems (role emotional), vitality, social functioning and mental functioning. Subscale scores have a range of 0 to 100, with higher values indicating better or higher functioning. Satisfactory reliability has been estimated by Cronbach’s alpha between .78–.93.64,65 For 92.5% of all tests, item-scale correlations exceeded correlations with other scales by more than two standard deviations supporting item-discriminant validity .65. In addition to the eight subscale scores, there are also two component summary scores for the MOS SF-36 (one for overall physical health and one for overall mental health). The physical component score (PCS) is derived from physical functioning, role-physical, bodily pain and general health. The mental component score (MCS) is summed from vitality, social functioning, role-emotional, and mental health. The summary scores are standardized to the general United States population (Mean score=50, SD=10).66 The physical component score has demonstrated utility as a preoperative predictor of mortality for patients undergoing CABS.28
In this study, physical functioning was measured using three subscales: physical functioning (10 items), role-physical functioning focused on role limitations due to physical problems (4 items), and vitality functioning evaluating the perceptions of energy and fatigue (4 items). Psychosocial functioning was measured using: mental health (5 items), social (2 items), and role limitations due to emotional problems (3 items) functioning subscales. Cronbach’s alphas in this study for the both physical subscales (physical, role physical and vitality) and the psychosocial subscales (role emotional, mental and social) for all data collection time periods ranged from 89–90.
Data Analysis
Data analyses in this study were conducted using descriptive and using repeated measures analysis of covariance (RM ANCOVA), with the baseline (prior to CABS) measures of the physical activity and functioning variables as the covariates. In this study, it is assumed that the variance-covariance matrix of each outcome is unstructured for the RM ANCOVA analyses. The mixed model was used because each observation is correlated and thus need to take the variance-covariance matrix of each outcome into account for these analyses.
RESEARCH FINDINGS
Physical activity
In this study, physical activity was measured at baseline using the Modified 7-day Activity Interview, which provided baseline data (prior to having CABS) on the subject’s average kcal/kg/day expended, average number of minutes spent exercising/week and average minutes/day spent in moderate or greater activity. At 3- and 6-weeks and 3- and 6-months physical activity and exercise was measured by the RT3® accelerometer (Stayhealthy, Inc.) providing average kcals/kg/day expended, which is an estimate of energy expenditure (EEE). A diary was also completed by subjects during the same follow-up times to collect average daily minutes in activity of moderate or greater intensity, average number of minutes spent exercising/day and the estimate of EEE (average kcals/kg/day).
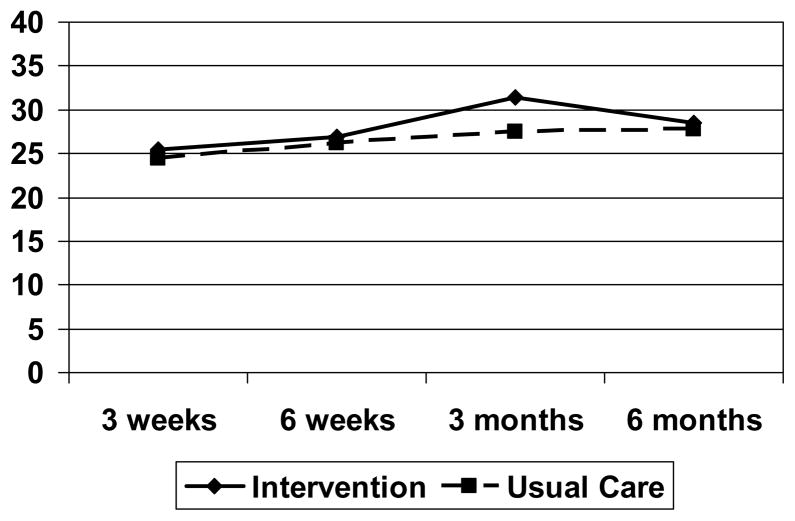
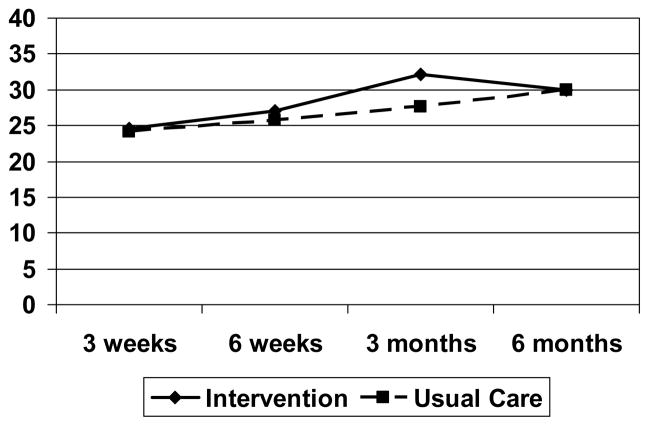
There were no significant interactions for total mean Kcal/Kg/day expended, as measured by the RT3®, using baseline mean number of minutes exercising per day, as measured by the Modified 7-day Activity Interview, as the covariate. Overall, regardless of time, there was a significant main effect by group [F (1,209)=4.66, p=.03]; the least square means of kcal/kg/day expended or estimated energy expenditure (EEE) for the intervention group was 27.9 kcal/kg/day and 26.6 kcal/kg/day for the usual care group. There was also a significant main effect of time [F (3,209)=9.79, p<.0001], with increases in EEE for all subjects, regardless of group. Figure 2 shows the adjusted mean (least mean squares) kcal/kg/day expended by the groups at each follow-up time measured by the RT3® accelerometer. Similarly, the average kcal/kg/day as measured by the Activity Diary demonstrated no significant interactions, but there was a significant main effect by group [F(1,210)=6.43, p<.01]; with the least square means of kcal/kg/day expended of 28.4 kcal/kg/day for the intervention group and 26.7 kcal/kg/day for the usual care group (see Figure 3). Both groups had significantly increased EEE over time [F(3,210)=15.1, p<.0001], as measured by the Activity Diary, regardless of group.
Figure 2.
Adjusted Mean kcal/kg/day Expended by Group as measured by the RT3
Figure 3.
Adjusted Mean kcal/kg/day Expended by Group as measured by the Activity Diary
There were no significant interactions for number of minutes per day spent in moderate or greater intensity of physical activity, as measured by the Activity Diary, using baseline reported levels of physical activity of moderate or greater levels of intensity, as measured by the Modified 7-day Activity Interview, as the covariate. There was a significant main effect by group [F(1,210)=5.99, p<.05]; the least square means of moderate or higher levels of activity per day were 190.6 minutes/day for the intervention group and 148.2 for the usual care group. There was also a significant main effects for time [F (3,210)=14.5, p<.0001] with subjects having increased levels of moderate or higher physical activity over time regardless of group. Figure 4 depicts the moderate and higher levels of activity by group over time.
There were no significant interactions or main effects for intervention group or time for mean number of minutes exercised per day, as measured by the Activity Diary and using baseline mean number of minutes exercised per day, as measured by the Modified 7-day Activity Interview, as the covariate.
The findings for physical activity and exercise in this study, demonstrate some interesting findings. Overall the early recovery telehealth intervention group expended more kcal/kg/day as evidenced by both the RT3® and the activity diary; and additionally had higher levels of physical activity at moderate or greater levels of intensity. Although not significant group by time interactions, it is apparent from Figures 1–3, that most group differences were noted at three months.
Functioning
In this study, physical and psychosocial functioning was measured at baseline (based on preoperative levels of functioning) and follow-up times (6-weeks, and 3- and 6-months) after CABS. There were no significant interactions or group effects for any of the physical functioning measures (physical, role-physical and vitality functioning) or for psychosocial functioning measure (mental, social and role-emotional functioning). There were significant time effects for physical [F(2,171)=3.26, p<.05] and role-physical functioning [F(2,171)=6.64, p<.005], with subjects’ physical and role physical functioning improving over time, regardless of group. The adjusted (least square mean) functioning scores for both physiological and psychosocial functioning at each follow-up time are summarized in Table 1.
Table 1.
Adjusted Mean MOS SF-36 subscale Scores for Physical and Psychosocial Functioning
| Physical Functioning | 6-weeks | 3-months | 6-months | |||
|---|---|---|---|---|---|---|
| Early Recovery Intervention | Usual Care | Early Recovery Intervention | Usual Care | Early Recovery Intervention | Usual Care | |
| Physical | 77.8 | 73.7 | 84.0 | 81.0 | 86.2 | 82.2 |
| Role-Physical | 73.9 | 68.1 | 87.6 | 79.3 | 84.2 | 88.4 |
| Vitality | 64.5 | 66.4 | 70.4 | 71.7 | 68.7 | 71.6 |
| Psychosocial Functioning | 6-weeks | 3-months | 6-months | |||
| Early Recovery Intervention | Usual Care | Early Recovery Intervention | Usual Care | Early Recovery Intervention | Usual Care | |
| Mental | 98.3 | 87.3 | 91.7 | 90.4 | 88.7 | 90.3 |
| Social | 95.4 | 94.7 | 97.4 | 93.9 | 96.7 | 92.8 |
| Role-Emotional | 100 | 96.9 | 98.3 | 99.7 | 99.2 | 97.2 |
DISCUSSION
Physical well-being is very important for patients with chronic conditions such as heart disease; as declines in physical ability and functioning are associated with higher health care utilization, morbidity and mortality.9,67 Cardiac revascularization as compared to medical management can reduce overall mortality among older adults;68 although the beneficial outcomes realized from revascularization may be impeded by persistent physical inactivity and lack of exercise. In this study, those patients with higher disease burden, as reflected by more CAD risk factors and impaired physical functioning prior to CABS, were studied to determine if an early recovery telehealth intervention had an effect on outcomes to improve physical well-being (physical activity, exercise and functioning). Findings indicated that the high disease burden subjects in the intervention group had higher levels of physical activity, as indicated by significantly higher adjusted estimated energy expenditure (kcal/kg/day expended) and higher levels of physical activity at moderate or higher levels of intensity, regardless of time. Subjects in the usual care group reached a plateau in their estimated energy expenditure by 3-months after CABS, while the intervention group was experiencing a peak at this same time period. The estimated energy expenditure patterns among older adults in the usual care group is consistent with findings from Reid and colleagues 27 showing the plateauing of physical activity between 2- to 6-months after surgery.
Older adults have difficulty in maintaining increased exercise after a cardiac event, as only 15–50% of patients are still exercising six months after cardiac rehabilitation.20,69,70 This finding may support the need to consider a booster intervention before the six month period to reinforce the need for physical activity and exercise. Additionally, conclusions by other researchers indicate that there may be more benefits for cardiovascular health by supporting older adults to lead a more physically active lifestyle, rather than just emphasizing the use of exercise alone after a cardiac event.71,72
Other researchers have noted that cardiac patients may have delayed recovery34 or experience disability and have limitations in their functioning after their cardiac events.36. In this study, psychosocial functioning outcomes were similar to findings by other researchers,1,73 and subjects demonstrated very little impairment of mental, social or role-emotional functioning, perhaps reflective of the ceiling effect noted in the findings. Physiological functioning (role-physical, physical, bodily pain and vitality functioning) of study participants also showed a trend of improvement over time; regardless of group.
In this study, the levels of reported physiological functioning for subjects in both groups was very comparable to findings from other studies of older cardiac patients after heart revascularization.1,30 While it might have been assumed that subjects with higher disease burden would have had more impaired functioning after their CABS, perhaps the subjects’ perception that they had such impaired status prior to their CABS and then following CABS their functioning was much improved over preoperative status compelled subjects to respond to their functioning as measured by the MOS SF-36 to be much higher than anticipated based on their preoperative impaired functioning. It should also be noted that the majority of subjects had participated in cardiac rehabilitation, which may also account for the improvements in functioning as reported by subjects in this study.
LIMITATIONS
Findings from this study are limited given this is a sub-analysis of a larger, RCT. In addition, the early recovery intervention examined in this study had not specifically been designed for CABS patients who had higher disease burden; therefore, the effect of the intervention may not have had as much of an impact as a more tailored intervention for this population. Another study limitation is the use of self-report measure of functioning using the MOS SF-36 tool; although this instrument is a robust measure widely used to measure physical and psychosocial functioning reflective of HRQOL.
CONCLUSIONS AND RECOMMENDATIONS
Despite preexisting impairments and higher risk for poor outcomes, older adults with heart disease can derive significant cardiovascular benefits and improved HRQoL from physical activity and exercise.13,74,75 Researchers have previously found a major determinant of the level of physical activity achieved and whether cardiac patients will maintain exercise, is based upon their level of activity and exercise prior to their cardiac event.19 Thus patients with higher disease burden, who have lower levels of physical activity and exercise, may need supportive interventions after their cardiac event to establish and maintain increased levels of physical activity. In summary, findings from this study indicate that after CABS, patients with high disease burden have lower levels of physiological functioning compared to those patients with less impaired preoperative status. In addition, the use of the early recovery telehealth intervention was associated with improvements in estimated energy expenditure from physical activity at 3-months after CABS; albeit the levels of physical activity declined by 6-months after surgery. This finding shows the promise of using such interventions, which could be further tailored to the needs of older adults with high disease burden after cardiac revascularization to integrate the habitual use of physical activity, so that it is an inherent part of daily life.
Acknowledgments
Funded by NIH/NINR R01 NR007759
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Susan Barnason, University of Nebraska Medical Center, College of Nursing-Lincoln Division.
Lani Zimmerman, University of Nebraska Medical Center, College of Nursing-Lincoln Division.
Paula Schulz, University of Nebraska Medical Center, College of Nursing-Lincoln Division.
Chunhao Tu, University of Nebraska Medical Center, College of Nursing-Lincoln Division.
References
- 1.Barnason S, Zimmerman L, Anderson A, Mohr-Burt S, Nieveen J. Functional status outcomes of patients with a coronary artery bypass graft over time. Heart & Lung. 2000;29(1):33–46. doi: 10.1016/s0147-9563(00)90035-9. [DOI] [PubMed] [Google Scholar]
- 2.Hunt JO, Hendrata MV, Myles PS. Quality of life 12 months after coronary artery bypass graft surgery. Heart Lung. 2000;29(6):401–411. doi: 10.1067/mhl.2000.110578. [DOI] [PubMed] [Google Scholar]
- 3.Kiebzak GM, Pierson LM, Campbell M, Cook JW. Use of the SF36 general health status survey to document health-related quality of life in patients with coronary artery disease: Effect of disease and response to coronary artery bypass graft surgery. Heart & Lung. 2002;31(3):207–213. doi: 10.1067/mhl.2002.124299. [DOI] [PubMed] [Google Scholar]
- 4.Ross AC, Ostrow L. Subjectively perceived quality of life after coronary artery bypass graft surgery. American Journal of Critical Care. 2001;10:11–16. [PubMed] [Google Scholar]
- 5.Boyette LW, Lloyd A, Boyette JE, et al. Personal characteristics that influence exercise behavior of older adults. J Rehabil Res Dev. 2002;39(1):95–103. [PubMed] [Google Scholar]
- 6.Brawley LR, Rejeski WJ, King AC. Promoting physical activity for older adults: The challenges for changing behavior. Am J Prev Med. 2003;25(3 Suppl 2):172–183. doi: 10.1016/s0749-3797(03)00182-x. [DOI] [PubMed] [Google Scholar]
- 7.Conn VS. Older women’s beliefs about physical activity. Public Health Nurs. 1998;15(5):370–378. doi: 10.1111/j.1525-1446.1998.tb00362.x. [DOI] [PubMed] [Google Scholar]
- 8.Heath JM, Stuart MR. Prescribing exercise for frail elders. J Am Board Fam Pract. 2002;15(3):218–228. [PubMed] [Google Scholar]
- 9.Bayliss EA, Bayliss MS, Ware JE, Jr, Steiner JF. Predicting declines in physical function in persons with multiple chronic medical conditions: What we can learn from the medical problem list. Health Qual Life Outcomes. 2004;2:47. doi: 10.1186/1477-7525-2-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rumsfeld JS, Ho PM, Magid DJ, et al. Predictors of health-related quality of life after coronary artery bypass surgery. Ann Thorac Surg. 2004;77(5):1508–1513. doi: 10.1016/j.athoracsur.2003.10.056. [DOI] [PubMed] [Google Scholar]
- 11.LaPier TK. Functional status of patients during subacute recovery from coronary artery bypass surgery. Heart & Lung. 2007;36:114–124. doi: 10.1016/j.hrtlng.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 12.Ades PA, Maloney A, Savage P, Carhart RL. Determinants of physical functioning in coronary patients. Archives of Internal Medicine. 1999;159:2357–2360. doi: 10.1001/archinte.159.19.2357. [DOI] [PubMed] [Google Scholar]
- 13.Nelson ME, Rejeski WJ, Blair SN, et al. Physical activity and public health in older adults: Recommendation from the american college of sports medicine and the american heart association. Circulation. 2007;116(9):1094–1105. doi: 10.1161/CIRCULATIONAHA.107.185650. [DOI] [PubMed] [Google Scholar]
- 14.Brennan PF, Caldwell B, Moore SM, Sreenath N, Jones J. Designing HeartCare: Custom computerized home care for patients recovering from CABG surgery. Proc AMIA Symp. 1998:381–385. [PMC free article] [PubMed] [Google Scholar]
- 15.Brennan PF, Moore SM, Bjornsdottir G, Jones J, Visovsky C, Rogers M. HeartCare: An internet-based infromation and support system for patient home recovery after coronary artery bypass graft (CABG) surgery. J Adv Nurs. 2001;35(5):699–708. doi: 10.1046/j.1365-2648.2001.01902.x. [DOI] [PubMed] [Google Scholar]
- 16.Dolansky MA, Moore SM. Effects of cardiac rehabilitation on the recovery outcomes of older adults after coronary artery bypass surgery. J Cardiopulm Rehabil. 2004;24(4):236–244. doi: 10.1097/00008483-200407000-00005. [DOI] [PubMed] [Google Scholar]
- 17.Focht BC, Brawley LR, Rejeski WJ, Ambrosius WT. Group-mediated activity counseling and traditional exercise therapy programs: Effects on health-related quality of life among older adults in cardiac rehabilitation. Ann Behav Med. 2004;28(1):52–61. doi: 10.1207/s15324796abm2801_7. [DOI] [PubMed] [Google Scholar]
- 18.Hartford K, Wong C, Zakaria D. Randomized controlled trial of a telephone intervention by nurses to provide information and support to patients and their partners after elective coronary artery bypass graft surgery: Effects of anxiety. Heart Lung. 2002;31(3):199–206. doi: 10.1067/mhl.2002.122942. [DOI] [PubMed] [Google Scholar]
- 19.Leung YW, Ceccato N, Stewart DE, Grace SL. A prospective examination of patterns and correlates of exercise maintenance in coronary artery disease patients. J Behav Med. 2007;30:411–421. doi: 10.1007/s10865-007-9117-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moore SM, Dolansky MA. Randomized trial of a home recovery intervention following coronary artery bypass surgery. Research in Nursing and Health. 2001;24:93–104. doi: 10.1002/nur.1012. [DOI] [PubMed] [Google Scholar]
- 21.Moore SM, Charvat JM, Gordon NH, et al. Effects of a CHANGE intervention to increase exercise maintenance following cardiac events. Ann Behav Med. 2006;31(1):53–62. doi: 10.1207/s15324796abm3101_9. [DOI] [PubMed] [Google Scholar]
- 22.Moore SM, Primm T. Designing and testing telehealth interventions to improve outcomes for cardiovascular patients. J Cardiovasc Nurs. 2007;22(1):43–50. [PubMed] [Google Scholar]
- 23.Pasquali SK, Alexander KP, Coombs LP, Lytle BL, Peterson ED. Effect of cardiac rehabilitation on functional outcomes after coronary revascularization. Am Heart J. 2003;145(3):445–451. doi: 10.1067/mhj.2003.172. [DOI] [PubMed] [Google Scholar]
- 24.Sniehotta FF, Scholz U, Schwarzer R, Fuhrmann B, Kiwus U, Völler H. Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. Int J Behav Med. 2005;12(4):244–255. doi: 10.1207/s15327558ijbm1204_5. [DOI] [PubMed] [Google Scholar]
- 25.Luszczynska A, Sutton S. Physical activity after cardiac rehabilitation: Evidence that different types of self-efficacy are important in mantainers and relapsers. REHABIL PSYCHOL. 2006;51(4):314–321. [Google Scholar]
- 26.Moore SM, Dolansky MA, Ruland CM, Pashkow FJ, Blackburn GG. Predictors of women’s exercise maintenance after cardiac rehabilitation. J Cardiopulm Rehabil. 2003;23:40–49. doi: 10.1097/00008483-200301000-00008. [DOI] [PubMed] [Google Scholar]
- 27.Reid RD, Morrin LI, Pipe AL, et al. Determinants of physical activity after hospitalization for coronary artery disease: The tracking exercise after cardiac hospitalization (TEACH) study. European Journal of Cardiovascular Prevention and Rehabilitation. 2006;13(4):529–537. doi: 10.1097/01.hjr.0000201513.13343.97. [DOI] [PubMed] [Google Scholar]
- 28.Rumsfeld JS, Magid DJ, O’Brien M, et al. Changes in health-related quality of life following coronary artery bypass graft surgery. Annals of Thoracic Surgery. 2001;72:2026–2032. doi: 10.1016/s0003-4975(01)03213-1. [DOI] [PubMed] [Google Scholar]
- 29.Worcester MUC, Murphy BM, Elliott PC, et al. Trajectories of recovery of quality of life in women after an acute cardiac event. British Journal of Health Psychology. 2007;12(1 1):1–15. doi: 10.1348/135910705X90127. [DOI] [PubMed] [Google Scholar]
- 30.Zimmerman L, Barnason S, Brey BA, Catlin S, Nieveen J. Comparison of recovery patterns for patients undergoing coronary artery bypass grafting and minimally invasive direct coronary artery bypass in the early discharge period. Prog Cardiovasc Nurs. 2002;17(3):132–141. doi: 10.1111/j.0889-7204.2002.00764.x. [DOI] [PubMed] [Google Scholar]
- 31.Bayliss EA, Ellis JL, Steiner JF. Subjective assessments of comorbidity correlate with quality of life health outcomes: Initial validation of a comorbidity assessment instrument. Health Qual Life Outcomes. 2005;3:51–51. doi: 10.1186/1477-7525-3-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yates BC, Heeren BM, Keller SM, Agrawal S, Stoner JA, Ott C. Comparing two methods of rehabilitation for risk factor modification after a cardiac event. Rehabil Nurs. 2007;32(1):15–22. doi: 10.1002/j.2048-7940.2007.tb00144.x. [DOI] [PubMed] [Google Scholar]
- 33.LeGrande MR, Elliott PC, Murphy BM, et al. Health related quality of life trajectories and predictors following coronary artery bypass surgery. Health and Quality of Life Outcomes. 2006;4:49–62. doi: 10.1186/1477-7525-4-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Anderson JA, Petersen NJ, Kistner C, Soltero ER, Willson P. Determining predictors of delayed recovery and the need for transitional cardiac rehabilitation after cardiac surgery. J Am Acad Nurse Pract. 2006;18(8):386–392. doi: 10.1111/j.1745-7599.2006.00152.x. [DOI] [PubMed] [Google Scholar]
- 35.Spadoti Dantas RA, Aparecida Ciol M. Quality of life after coronary artery bypass surgery. West J Nurs Res. 2008;30(4):477–490. doi: 10.1177/0193945907303140. [DOI] [PubMed] [Google Scholar]
- 36.Dolansky MA, Moore SM. Older adults’ early disability following a cardiac event. West J Nurs Res. 2008;30(2):163–180. doi: 10.1177/0193945907303061. [DOI] [PubMed] [Google Scholar]
- 37.Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement?: A critical review of the scientific evidence. American Journal of Preventive Medicine. 2003;25(3 Supplement 2):129–136. doi: 10.1016/s0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- 38.Keysor JJ, Jette AM. Have we oversold the benefit of late-life exercise? J Gerontol A Biol Sci Med Sci. 2001;56(7):M412–23. doi: 10.1093/gerona/56.7.m412. [DOI] [PubMed] [Google Scholar]
- 39.Daly J, Sindone AP, Thompson DR, Hancock K, Chang E, Davidson P. Barriers to participation in and adherence to cardiac rehabilitation programs: A critical literature review. Prog Cardiovasc Nurs. 2002;17(1):8–17. doi: 10.1111/j.0889-7204.2002.00614.x. [DOI] [PubMed] [Google Scholar]
- 40.Aggarwal B, Ades PA. Exercise rehabilitation of older patients with cardovascular disease. Cardiology Clinics. 2001;19(2):525–540. doi: 10.1016/s0733-8651(05)70234-4. [DOI] [PubMed] [Google Scholar]
- 41.Forman DE, Farquhar W. Cardiac rehabilitation and secondary prevention programs for elderly cardiac patients. Clin Geriatr Med. 2000;16(3):619–629. doi: 10.1016/s0749-0690(05)70031-8. [DOI] [PubMed] [Google Scholar]
- 42.Barnason S, Zimmerman L, Nieveen J, et al. Relationships between fatigue and early postoperative recovery outcomes over time in elderly patients undergoing coronary artery bypass graft surgery. Heart Lung. 2008;37(4):245–256. doi: 10.1016/j.hrtlng.2007.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dye CJ, Wilcox S. Beliefs of low-income and rural older women regarding physical activity: You have to want to make your life better. Women Health. 2006;43(1):115–134. doi: 10.1300/J013v43n01_07. [DOI] [PubMed] [Google Scholar]
- 44.Ruppar TM, Schneider JK. Self-reported exercise behavior and interpretations of exercise in older adults. West J Nurs Res. 2007;29(2):140–57. doi: 10.1177/0193945906293805. discussion 158–60. [DOI] [PubMed] [Google Scholar]
- 45.Forkan R, Pumper B, Smyth N, Wirkkala H, Ciol MA, Shumway-Cook A. Exercise adherence following physical therapy intervention in older adults with impaired balance. Phys Ther. 2006;86(3):401–410. [PubMed] [Google Scholar]
- 46.Cohen-Mansfield J, Marx MS, Biddison JR, Guralnik JM. Socio-environmental exercise preferences among older adults. Prev Med. 2004;38(6):804–811. doi: 10.1016/j.ypmed.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 47.Donabedian A. The end results of health care: Ernest codman’s contribution to quality assessment and beyond. Milbank Quarterly. 1989;67:233–256. [PubMed] [Google Scholar]
- 48.Dodd M, Janson S, Facione N, et al. Advancing the science of symptom management. J Adv Nurs. 2001;33(5):668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 49.Zimmerman L, Barnason S. Use of a telehealth device to deliver a symptom management intervention to cardiac surgical patients. Journal of Cardiovascular Nursing. 2007;22(1):32–37. doi: 10.1097/00005082-200701000-00005. [DOI] [PubMed] [Google Scholar]
- 50.Nash IS, Curtis LH, Rubin H. Predictors of patient-reported physical and mental health 6 months after percutaneous coronary revascularization. Am Heart J. 1999;138(3):422–429. doi: 10.1016/s0002-8703(99)70142-0. [DOI] [PubMed] [Google Scholar]
- 51.American Heart Association. RISKO: A Heart Hazard Appraisal. Dallas, TX: American Heart Association; 1985. [Google Scholar]
- 52.Barnason S, Zimmerman L, Nieveen J, et al. Usefulness of RISKO heart hazard appraisal to quantify CAD risk factor burden on the preoperative functioning of coronary artery bypass graft surgery patients. Prog Cardiovasc Nurs. 2007;22(2):81–87. doi: 10.1111/j.0889-7204.2007.05814.x. [DOI] [PubMed] [Google Scholar]
- 53.Hellman EA, Williams MA, Thalken L. Modifications of the 7-day activity interview for use among older adults. Journal of Applied Gerontology. 1996;15(1):116–132. [Google Scholar]
- 54.Blair SN, Haskell WL, Ho P, Paffenbarger RS, Jr, Vranizan KM, Farquhar JW, et al. Assessment of habitual physical acitivity by a seven-day recall in a community survey and controlled experiments. American Journal of Epidemiology. 1985;122(5):794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 55.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the five-city project. Am J Epidemiol. 1985;121(1):91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 56.Hellman EA, Williams MA, Thalken L. Construct validity of the modified 7-day activity interview used with older adults with cardiac problems. REHABIL NURS RES. 1996;5(4):126–133. [Google Scholar]
- 57.Jakicic JM, Winters C, Lagally K, Ho J, Robertson RJ, Wing RR. The accuracy of the tritac-R3D accelerometer to estimate energy expenditure. Medicine & Science in Sports & Exercise. 1999;31(747):754. doi: 10.1097/00005768-199905000-00020. [DOI] [PubMed] [Google Scholar]
- 58.Sherman WM, Morris DM, Kirby TE, Petrosa RA, Smith BA, Frid DJ. Evaluation of a commercial accelerometer (tritrac-R3D) to measure energy expenditure during ambulation. International Journal of Sports Medicine. 1998;19:43–47. doi: 10.1055/s-2007-971878. [DOI] [PubMed] [Google Scholar]
- 59.Rowlands AV, Thomas PW, Eston RG, Topping R. Validation of the RT3 triaxial accelerometer for the assessment of physical activity. Med Sci Sports Exerc. 2004;36(3):518–524. doi: 10.1249/01.mss.0000117158.14542.e7. [DOI] [PubMed] [Google Scholar]
- 60.Welk GJ, Blair SN, Wood K, Jones S, Thompson RW. A comparative evaluation of three accelerometry-based physical activity monitors. Med Sci Sports Exerc. 2000;32(9):S489–S497. doi: 10.1097/00005768-200009001-00008. [DOI] [PubMed] [Google Scholar]
- 61.Hertzog MA, Nieveen JL, Zimmerman LM, et al. Longitudinal field comparison of the RT3 and an activity diary with cardiac patients. J Nurs Meas. 2007;15(2):105–120. doi: 10.1891/106137407782156363. [DOI] [PubMed] [Google Scholar]
- 62.Bouchard C, Tremblay A, Leblanc C, Lortie G, Savard R, Theriault G. A method to assess energy expenditure in children and adults. Am J Clin Nutr. 1983;37(3):461–467. doi: 10.1093/ajcn/37.3.461. [DOI] [PubMed] [Google Scholar]
- 63.Ware JE. The MOS 36-item short form health survey (SF-36). 1. conceptual framework anditem selection. MedCare. 1992;30(6):473–483. [PubMed] [Google Scholar]
- 64.Jette D, Downing J. Health status of individuals entering a cardiac rehabilitation program as measured by the medical outcomes study 36-item short-form study (SF-36) Physical Therapy. 1994;74(6):521–527. doi: 10.1093/ptj/74.6.521. [DOI] [PubMed] [Google Scholar]
- 65.McHorney C, Ware J, Rachel J, Sherbourne C. The MOS 36-item short form health survey (SF-36): III. tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32(1):40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- 66.Ware JE, Snow KK, Kosinski M. SF-36 Health Survey: Manual and Interpretation Guide. Lincoln, R.I: QualityMetric Inc; 2000. [Google Scholar]
- 67.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics--2008 update: A report from the american heart association statistics committee and stroke statistics subcommittee. Circulation. 2008;117(4):e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 68.Jeger RV, Bonetti PO, Zellweger MJ, et al. Influence of revascularization on long-term outcome in patients > or =75 years of age with diabetes mellitus and angina pectoris. Am J Cardiol. 2005;96(2):193–198. doi: 10.1016/j.amjcard.2005.03.042. [DOI] [PubMed] [Google Scholar]
- 69.Ades PA, Savage P, Tischler MD, Poehlman ET, Dee JD, Niggel J. Determininants of disability in older cardiac patients. American Heart Journal. 2002;143(1):151–156. doi: 10.1067/mhj.2002.119379. [DOI] [PubMed] [Google Scholar]
- 70.Bock BC, Carmona-Barros RE, Esler JL, Tilkemeier PL. Program participation and physical activity maintenance after cardiac rehabilitation. Behav Modif. 2003;27(1):37–53. doi: 10.1177/0145445502238692. [DOI] [PubMed] [Google Scholar]
- 71.Houde SC, Melillo KD. Cardiovascular health and physical activity in older adults: An integrative review of research methodology and results. J Adv Nurs. 2002;38(3):219–234. doi: 10.1046/j.1365-2648.2002.02172.x. [DOI] [PubMed] [Google Scholar]
- 72.Reid RD, Dafoe WA, Morrin L, et al. Impact of program duration and contact frequency on efficacy and cost of cardiac rehabilitation: Results of a randomized trial. American Heart Journal. 2005;149:862–868. doi: 10.1016/j.ahj.2004.09.029. [DOI] [PubMed] [Google Scholar]
- 73.Wintz G, LaPier TK. Functional status in patients during the first two months following hospital discharge for coronary artery bypass surgery. CARDIOPULM PHYS THER J. 2007;18(2):13–20. [Google Scholar]
- 74.Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. J Gerontol A Biol Sci Med Sci. 2001;56A:23–35. doi: 10.1093/gerona/56.suppl_2.23. [DOI] [PubMed] [Google Scholar]
- 75.Thompson PD, Buchner D, a IL, et al. AHA scientific statement. exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease: A statement from the council on clinical cardiology (subcommittee on exercise, rehabilitation, and prevention) and the council on nutrition, physical activity, and metabolism (subcommittee on physical activity) Circulation. 2003;107(24):3109–3116. doi: 10.1161/01.CIR.0000075572.40158.77. [DOI] [PubMed] [Google Scholar]