Abstract
Objective
To assess the prospective association between daily feelings of loneliness and subsequent feelings of daytime dysfunction indicative of poor sleep quality.
Design
Three consecutive end-of-day diaries were completed by a population-based sample of 215 adults (mean age = 57.5 years, SD = 4.4). Diary questions probed sleep duration, daytime dysfunction (i.e., fatigue, low energy, sleepiness), loneliness, physical symptoms, and depressed affect experienced that day. Chronic health condition data and body mass index were also obtained. Autoregressive cross-lagged panel models were used to examine the magnitude of reciprocal prospective associations between loneliness and daytime dysfunction.
Main Outcome Measures
Unstandardized path coefficients adjusted for race/ethnicity, sleep duration, marital status, household income, chronic health conditions, and health symptom severity.
Results
Daily variations in loneliness predicted subsequent feelings of daytime dysfunction, B = 0.16, p < .05, and daytime dysfunction predicted subsequent loneliness, B = 0.07, p < .05, adjusted for covariates. Loneliness continued to predict subsequent daytime dysfunction when depressed affect was held constant.
Conclusion
The effect of loneliness on daytime dysfunction was independent of sleep duration, suggesting that the same amount of sleep is less salubrious when individuals feel more socially isolated.
Keywords: loneliness, social isolation, sleep, daytime dysfunction, daily diaries
In his pioneering work, Walter Cannon (1871-1945) noted that physiological responses to contemporary stressors have cumulative health costs because the stress response evolved during a period in which the metabolic requirements for effective coping were greater than required today (Cannon, 1936). Cannon said nothing about anabolic physiology and the reparative and restorative capacity afforded by nightly sleep. The same human physiology that evolved to provide energy to survive stressors also evolved to use the sleep period to recuperate from spent energies and to generate and store energy reserves for future use (Laposky, Bass, Kohsaka, & Turek, 2008).
The role of sleep as a restorative behavior is evident in the dramatic metabolic consequences of as little as six nights of sleep deprivation (Spiegel, Leproult, & Van Cauter, 1999). Sleep deprivation results in a compensatory increase in sleep duration and intensity that speaks to its homeostatic and restorative function (Lesku, Rattenborg, & Almaner, 2006). The restorative effects of sleep appear to be passively acquired, but sleep itself is an active process that plays a constructive role in, for example, the consolidation of learning and memory (Fenn, Nusbaum, & Margoliash, 2003; Stickgold, Hobson, Fosse, & Fosse, 2001). Accompanying the notion of sleep as an active process is an increasing appreciation for the role of nonrestorative sleep (i.e., sleep that is non-refreshing despite normal sleep duration) in daytime fatigue, cognitive and behavioral impairments (Ohayon, 2005) and nighttime insomnia (American Psychiatric Association, 2000).
Throughout human evolution, sleep—and salubrious sleep in particular—has relied on a safe sleeping environment, a need that has typically been met by co-sleeping (Worthman & Melby, 2002). Given this evolutionary history, it is perhaps not surprising that social isolation, real and perceived, is associated with poor sleep quality, whether assessed prospectively as self-reported sleep satisfaction (Jacobs, Cohen, Hammerman-Rozenberg, & Stessman, 2006), or as complaints of poor sleep quality and daytime dysfunction in surveys of national samples, college student populations, and adolescents (Allaert & Urbinelli, 2004; Cacioppo, Hawkley, Crawford et al., 2002; Mahon, 1994). Feelings of loneliness are tantamount to feelings of threat and vulnerability (Cacioppo & Hawkley, 2009), and feeling implicitly unsafe disrupts the sleep of lonely individuals by increasing the number of nightly microawakenings (Cacioppo, Hawkley, Berntson, et al., 2002). Notably, prior research has shown that the greater daytime dysfunction reported by lonely individuals is not attributable to differential sleep duration (Cacioppo, Hawkley, Crawford et al., 2002) or to individual differences in the activities of everyday life (Hawkley, Burleson, Berntson, & Cacioppo, 2003). Given the differences in microawakenings, lonely individuals are posited to feel less rested than nonlonely individuals after an equivalent night's sleep duration.
To date, the finding that daily functioning is impaired to a greater degree in lonely than nonlonely individuals has been studied in convenience samples using cross-sectional designs. In the present study, we use a 3-day diary study to examine whether end-of-day feelings of loneliness are prospectively associated with next day reports of dysfunction (i.e., sleepiness, fatigue, low energy) in a population-based sample of 50-68 year-old adults, and whether these effects are independent of sleep duration. Depressed affect is associated with loneliness and is a known risk factor for poor sleep and daytime dysfunction (Harvey, 2001), so we also tested whether the effect of loneliness on daytime dysfunction was independent of depressed affect. Finally, because prior research has shown that insomnia predicts interpersonal functioning (Roberts, Roberts, & Chen, 2002), we also examine the extent to which dysfunction leads to subsequent feelings of loneliness.
Method
Participants
Data for this study were collected in the first year of CHASRS (Chicago Health, Aging, and Social Relations Study), a longitudinal, population-based study of persons born between 1935 and 1952. The target population was non-Hispanic Caucasian, African American, and non-black Latino American persons living in Cook County, IL, who were English-speaking and sufficiently ambulatory to come to the University of Chicago for a daylong visit to the laboratory. The sampling description and response rates have been described elsewhere (Hawkley et al., 2008). The final sample size of CHASRS is 229. The sample is 35.8% White, 35.4% Black, and 28.8% Hispanic, and 52.4% of the sample are female. The mean age of the sample is 57.5 yrs (SD = 4.4).
Participants were paid $126US for participating in the lab component of the protocol, and an additional $36 for completing the three-day at-home diary component of the protocol. A total of 204 participants completed the entire three-day diary protocol, and 215 participants completed at least one day of the diary protocol.
Procedure
Data from the diary component of the protocol were used to examine the temporal dynamics of the association between daytime dysfunction and loneliness. At the end of each of three consecutive days, Sunday through Tuesday, participants were asked to complete a diary that included questions about sleep duration, time in bed, and time in bed awake the prior night, and questions about daytime dysfunction, loneliness, physical symptoms, and depressed affect experienced that day, as well as measures of daily smoking, drinking, and exercise behaviors. In addition, survey, health, and anthropometric measures completed during the laboratory component of the protocol were used to assess basic demographic information, chronic health conditions, and body mass index.
Measures
Daytime dysfunction
Participants were asked the extent to which they felt sleepy, exhausted, lively, energetic, and fatigued, on a scale of 1 = not at all, to 5 = very much. Cronbach's alpha for this scale was .82. After reverse-scaling the items for “lively” and “energetic,” the mean response across all items was calculated to represent daytime dysfunction. Across all subjects and days, the mean value on this measure was 1.73 (SD = 0.62; range = 1-5).
Loneliness
Participants were asked items from the UCLA loneliness scale (Russell, Peplau, & Cutrona, 1980). We selected six items from this scale that assess feelings of social isolation (e.g., could not find companionship when I wanted it; felt like I didn't belong; felt like no one really knew me well), and one additional item with face validity (“felt lonely”). Participants were asked, “Overall today, to what extent did you feel [like I could not find companionship when I wanted it, etc.],” and responses were made on a scale of 1 = not at all, to 5 = very much. Cronbach's alpha for this measure was .81. After reverse-scaling appropriate items, the mean response across all seven items was calculated to represent loneliness. Collapsed across days, the mean value on this measure was 1.75 (SD = 0.56; range = 1-5).
Covariates
Marital status was dichotomously coded to contrast those with a spouse or live-in partner (61% of sample) versus all other marital status groups. Two dummy-coded variables were used to contrast the Black and the Hispanic with the White racial/ethnic group. Socioeconomic status was represented in measures of education (having completed a high school diploma or equivalent; 79.5% of the sample) and household income (12 categories ranging from less than $5,000 to more than $200,000; median = $50,001 - $75,000). Median household income category values were subjected to a natural log transformation to achieve a more continuous distribution.
Chronic health conditions were quantified by calculating the Charlson Comorbidity Index (Katz, Chang, Sangha, Fossel, & Bates, 1996), a weighted measure of disease burden that takes severity into consideration. The mean score on this index was 0.7 (SD = 1.4; 68% had a score of zero, and 8% had a score of 2 or more; range = 0-14). BMI was calculated as weight in kg/(height in m)2 (M = 31.5, SD = 7.0).
At the diary level, daily reports were obtained for health behaviors. On at least one of the three days, 13% of the sample reported smoking, 35% reported consuming alcohol, and 33% reported exercising ≥ 30 min. Daily reports of physical illness symptom severity (e.g., headache) were obtained on a scale of 1 (not at all) to 5 (very much), and mean symptom severity across subjects and days was 1.54 (SD = 0.84). Self-reported sleep duration averaged 7.1 hours (SD = 1.0; range = 4.5 – 10.2). Self-reported time in bed averaged 7.6 hours (SD = 1.2; range = 4.8 – 12.0), and time in bed awake averaged 31.2 minutes (SD = 56.8; range = 0 – 330). Depressed affect was assessed with two items (sad, discouraged) taken from the Profile of Mood States (POMS) inventory (Shacham, 1983). Collapsed across days, the mean value for depressed affect was 1.42 (SD = 0.66, range = 1-5).
Data Analysis
Stationary autoregressive cross-lagged (ARCL) panel models (Curran, 2000) were used to assess the magnitude and significance of the effect of loneliness on subsequent daytime dysfunction, and the effect of daytime dysfunction on subsequent loneliness, net of a set of covariates. ARCL models are path analysis / structural equation models in which measurements of constructs at time t are treated as predictors of those same constructs at time t + 1, often for several consecutive periods of data collection. Coefficients linking variables are interpretable as regression weights. In addition to estimating time-lagged effects, ARCL models provide information about both the stability of individual differences over time and the stationarity of effects linking two variables across different periods of data collection. Because the model is complex and sample size is small, only measures that were correlated with both loneliness and daytime dysfunction (see Table 1) were included as covariates. Race/ethnicity was also included as a covariate because of known racial/ethnic differences in sleep (Profant, Ancoli-Israel, & Dimsdale, 2002). To rule out sleep duration as an explanation for daytime dysfunction, hours of sleep was treated as a time-varying covariate in all analyses. Models were fit using Mplus 5.2, and confidence intervals were obtained using 5000 bootstrap resamples.
Table 1. Correlations with mean daily feelings of loneliness and daytime dysfunction.
| N | Loneliness | Daytime dysfunction | |
|---|---|---|---|
| Age | 215 | -.17* | -.11 |
| Female | 215 | -.08 | .15* |
| Married/partnered | 215 | -.18** | -.15* |
| High school diploma | 215 | -.13 | -.02 |
| Household income | 215 | -.26** | -.27** |
| Charlson comorbidity index | 215 | .14* | .29** |
| Body mass index | 214 | .05 | .15* |
| Smoke cigarettes | 214 | .13 | -.02 |
| Drink alcohol | 215 | .10 | -.08 |
| Exercise at least 30 min/day | 212 | .08 | .01 |
| Symptom severity | 214 | .29** | .39** |
| Hours of sleep | 215 | .02 | -.08 |
| Time in bed | 215 | .17* | .05 |
| Time in bed awake | 215 | .20** | .14* |
| Depressed affect | 213 | .70** | .46** |
Results
Preliminary analyses of data averaged across three diary days revealed a significant correlation between loneliness and daytime dysfunction, r(215) = .48, p < .001. Sleep duration was not associated with loneliness, r(215) = .02, or daytime dysfunction, r(215) = -.08, p's > .2. These results from a population-based sample replicate prior research based on convenience samples. Unlike sleep duration, time in bed was positively correlated with loneliness, r(215) = .17, p < .05. Moreover, loneliness was positively associated with time spent in bed awake (i.e., poorer sleep efficiency), r(215) = .20, p < .01, a finding that is consistent with previously observed associations between loneliness and poor sleep quality as indicated by more micro-awakenings objectively assessed via Sleep Caps (Cacioppo, Hawkley, Berntson et al., 2002). Average daytime dysfunction was not associated with time spent in bed but, like loneliness, was associated with time spent in bed awake, r(215) = .14, p < .05.
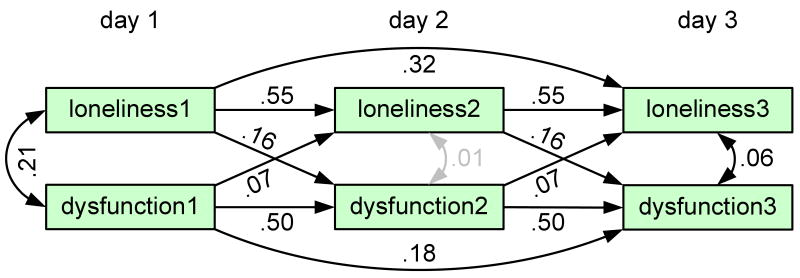
An ARCL panel model supported a fully stationary process (equal lagged and cross-lagged effects over time) showing that loneliness during one day predicted greater daytime dysfunction the next day, controlling for marital status, race/ethnicity, household income, Charlson comorbidity index, physical symptom severity, hours of sleep the prior night, and dysfunction during the previous day. Model fit was good (χ2(48) = 67.05, p = .04; RMSEA = .043, 90% CI: .012, .066; SRMR = .049). The stationary autoregressive effect of loneliness was significant (B = 0.55, 95% CI: 0.39, 0.67), as was the stationary autoregressive effect of daytime dysfunction (B = 0.50, 95% CI: 0.41, 0.60). These coefficients indicate moderate day-to-day stability of feelings of loneliness and daytime dysfunction over a three-day period, leaving substantial day-to-day variability in feelings of loneliness and daytime dysfunction. Importantly, day-to-day variability in loneliness was systematically associated with variability in daytime dysfunction. Net of autoregressive effects, the stationary lagged effect of loneliness on dysfunction was significant (B = 0.16, 95% CI: 0.05, 0.25), as was the stationary lagged effect of dysfunction on loneliness (B = 0.07, 95% CI: 0.001, 0.15), indicating reciprocal influences (see Figure 1). None of the covariates, including sleep duration, exhibited significant lagged effects on loneliness or daytime dysfunction (all CIs included zero). In addition, total time in bed and time spent in bed awake were sequentially substituted for sleep duration as covariates, and analyses showed that neither explained the significant cross-lagged associations between lonely feelings and daytime dysfunction.
Figure 1.
Autoregressive cross-lagged panel model including marital status, household income, Charlson comorbidity index, symptom severity, and sleep duration as covariates. Parameter estimates are unstandardized path coefficients. Grey estimates are n.s. at α = .05.
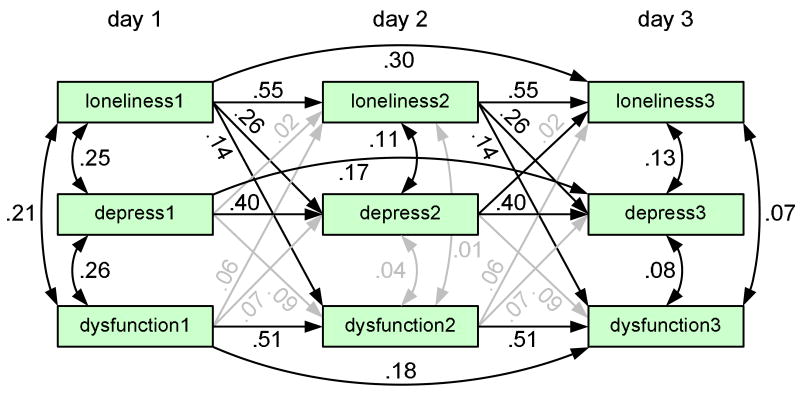
To test whether depressed affect explained the effect of loneliness on daytime dysfunction, the model was simplified by excluding all covariates except sleep duration and race/ethnicity. Model fit was good (χ2(31) = 56.64, p = .003; RMSEA = .062, 90% CI: .035, .087; SRMR = .046). Depressed affect did not exhibit a significant stationary lagged effect on loneliness (B = 0.02, 95% CI: −0.12, 0.14), or on daytime dysfunction (B = 0.09, 95% CI: −0.02, 0.20). Daytime dysfunction did not exhibit a stationary lagged effect on depressed affect (B = 0.07, 95% CI: −0.03, 0.18), or on loneliness (B = 0.06, 95% CI: −0.01, 0.16). Notably, loneliness exhibited a significant stationary lagged effect on daytime dysfunction net of the lagged effects of depressed affect, sleep duration, and the prior day's dysfunction (B = .14, 95% CI: 0.01, 0.27) (see Figure 2). In addition, loneliness exhibited a stationary lagged effect on depressed affect (B = 0.26, 95% CI: 0.10, 0.43), and depressed affect explained a small portion of the prospective association between loneliness and daytime dysfunction (indirect effect = .024, 95% CI: .001, .068).
Figure 2.
Autoregressive cross-lagged panel model including depressed affect as a potential mediator with sleep duration and race/ethnicity as covariates. Parameter estimates are unstandardized path coefficients. Grey estimates are n.s. at α = .05.
Finally, we addressed the possibility that daily events explain differences in daytime dysfunction. Specifically, we used the stacked diary data and multilevel regression to model day-level variability in daytime dysfunction and examine the within-subject association between prior day's loneliness and present day dysfunction holding constant present day loneliness. In the first multilevel model, prior day's loneliness predicted daytime dysfunction, B = 0.34, SE = 0.06, p < .001. In the second model, holding constant same day loneliness (and the daily events and experiences for which this is a proxy), prior day's loneliness continued to predict daytime dysfunction, B = 0.23, SE = 0.07, p = .001.
Discussion
The results of the present prospective study extend prior cross-sectional research and indicate that optimal functioning (i.e., high levels of energy, low levels of sleepiness and fatigue) is not limited solely by sleep duration but is actively altered by the daily experience of social isolation. Given an equal number of hours spent sleeping, a socially contented individual appears to derive greater recovery and restoration of function than his or her lonelier counterpart. Moreover, our data show that daytime dysfunction feeds forward to further increase feelings of loneliness, thus setting in motion a vicious cycle that potentially traps lonely individuals in their lonely state. Finally, the population-based nature of our sample implies that our results are generalizable, more so than results based on the convenience samples that have characterized much of the research on loneliness.
Depressed feelings did not exert a direct effect on daytime dysfunction but explained in small part the influence of loneliness on subsequent dysfunction. Depressed affect may be more potent than loneliness in predicting other indicators of poor sleep (e.g., latency, efficiency), but present data indicate that the direct effect of loneliness on daily functioning outweighs its indirect effect through depressed affect.
Reports of daytime dysfunction must, of necessity, be obtained retrospectively at the end of the day, and this raises the possibility that events of the day may be sufficient to explain differences in daytime dysfunction. Ancillary analyses, however, revealed a persistent lagged effect of loneliness on daytime dysfunction even when concurrent loneliness was held constant. These data weaken the argument that events and experiences of the day are responsible for loneliness differences in daytime dysfunction.
In our prior research in which time in bed and sleep duration were measured objectively, we found no bias in the reporting of these variables as a function of loneliness (Cacioppo, Hawkley, Berntson et al., 2002). In this study, we used alternative measures to self-reported sleep duration (i.e., total time in bed, time in bed awake) to evaluate the robustness of the cross-lagged associations between loneliness and daytime dysfunction. In each case, the reciprocal association between loneliness and daytime dysfunction remained intact. Notably, objective sleep characteristics do not correspond well to subjective sleep complaints (American Academy of Sleep Medicine Standards of Practice Committee, 1995), and “it is in fact this complaint that is of primary interest to clinicians and policy makers” (Alapin et al., 2000). Our data indicate that for individuals experiencing day-to-day vacillations in feelings of loneliness, sleep complaints are not ignorable because they may have measurable consequences for daily functioning as indexed by energy levels, fatigue, and sleepiness.
Measures of sleep quality were not assessed directly in this study, but in a study of young adults who wore a “Sleep Cap” for each of seven nights, we observed that sleep quality was indeed altered in lonely individuals as indicated by more micro-awakenings and poorer sleep efficiency (Cacioppo, Hawkley, Berntson et al., 2002). Consistent with these objective results, self-reports of middle-aged adults in the present study revealed that lonely individuals exhibited poorer sleep efficiency (i.e., more time in bed awake), a finding that also replicates prior observations of poor self-reported sleep efficiency in lonely elderly adults (Cacioppo, Hawkley, Crawford et al., 2002). Sleep efficiency did not explain the cross-lagged association between loneliness and daytime dysfunction in the present study, but micro-awakenings remain a plausible mechanism for the effect of feelings of loneliness on next-day dysfunction.
We have posited that loneliness feels unsafe, and that this places lonely people in a heightened state of vigilance for potential threats in the environment (Cacioppo et al., 2006; Cacioppo & Patrick, 2008). Our recent research has revealed that perceptual and attentional differences between lonely and nonlonely individuals are consistent with heightened feelings of threat and danger in lonely relative to nonlonely individuals. In a Stroop study in which participants had competing attentional demands (i.e., color vs. content of verbal stimuli), negative social words (e.g., rejected, alone, disliked) created greater interference for lonely than nonlonely individuals (Egidi et al., 2008). Positive social words did not elicit loneliness differences. These data suggest that loneliness primes people to look for the negative in their social environment. A subsequent fMRI study (Cacioppo, Norris, Decety, Monteleone, & Nusbaum, 2009) showed that activation of the visual cortex is greater in lonely than nonlonely individuals when viewing negative social (compared to nonsocial) stimuli – a significant effect that was not observed for the positive social minus positive nonsocial contrast. These data again suggest that loneliness increases attention to negative social information and potential social threats. This pattern of findings corresponds to well-substantiated characterizations of the lonely individual as distrustful, fearful of negative evaluation, and anxious (Cacioppo et al., 2006; Ernst & Cacioppo, 1999; Rotenberg, 1994). These perceptions and emotions prompt vigilance and self-defense and contribute to the experience of loneliness as threatening and unsafe. Feelings of threat need not be conscious for them to influence everyday life, and even the unconscious state of sleep seems to be affected. With systems on high alert, lonely individuals appear unable to achieve the restoration and recovery afforded individuals who can rest secure in the knowledge, conscious or unconscious, that they are safe and protected.
Recent research has shown that feelings of social isolation and loneliness predict an increased rate of cognitive decline and development of late-life dementia (Wilson et al., 2007), and is associated with increases in blood pressure (Hawkley, Masi, Berry, & Cacioppo, 2006). Given the active role of sleep in cognitive processes (Fenn et al., 2003; Stickgold et al., 2001), and in chronic diseases such as hypertension (Suka, Yoshida, & Sugimori, 2003; Tochikubo, Ikeda, Miyajima, & Ishii, 1996), an important question for future research is whether nonrestorative sleep contributes to the health consequences of loneliness. In this regard, we note that vigor, a construct that is opposite to daytime dysfunction (i.e., feelings of physical strength, emotional energy, and cognitive liveliness) has recently been shown to predict changes in self-rated health (Shirom, Toker, Berliner, Shapira, & Melamed, 2008). Data linking daytime dysfunction and health are beginning to accrue in large population studies. For instance, sleepiness, one component of daytime dysfunction, has recently been shown to moderate the association between sleep apnea and hypertension. Excessive sleepiness is a characteristic of only one-third of moderate-to-severe sleep apnea cases. Whereas apnea patients with infrequent sleepiness had no increase in risk for hypertension, OR = 1.22 (0.89-1.22), frequent sleepiness increased the odds of hypertension significantly, OR = 2.83 (1.33-6.04) (Gottlieb, 2008). Given the greater risk for high blood pressure in lonely individuals (Hawkley et al., 2006), sleepiness is a plausible explanatory mechanism that future research will address.
Public health concerns about sleep duration are not unfounded, of course, but sleep quality is at least as important for optimal daily functioning. Large scale studies have shown that, relative to other insomnia symptoms (i.e., difficulty falling or staying asleep, waking too early), nonrestorative sleep is associated with significantly greater physical and intellectual fatigue, role impairments, difficulty staying alert, irritability, and cognitive and memory problems (Ohayon, 2005; Roth et al., 2006). To the extent that feelings of social connection and belonging alleviate the burden of nonrestorative sleep, developing and maintaining good quality social relationships may serve as an effective treatment for a pervasive public health problem. The challenge for contemporary society is to utilize rather than ignore (McPherson, Smith-Lovin, & Brashears, 2006) our evolutionary design as a social species.
Acknowledgments
This research was funded by the National Institutes on Aging under Program Project Grant No. PO1 AG18911 and RO1 AG034052-01, and by an award from the Templeton Foundation.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/hea
References
- Alapin I, Fichten CS, Libman E, Creti L, Bailes S, Wright J. How is good and poor sleep in older adults and college students related to daytime sleepiness, fatigue, and ability to concentrate? Journal of Psychosomatic Research. 2000;49:381–390. doi: 10.1016/s0022-3999(00)00194-x. [DOI] [PubMed] [Google Scholar]
- Allaert FA, Urbinelli R. Sociodemographic profile of insomniac patients across national surveys. CNS Drugs. 2004;18 1:3–7. doi: 10.2165/00023210-200418001-00003. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Text Revision (DSM-IV-TR) Arlington, VA: American Psychiatric Publishing, Inc; 2000. [Google Scholar]
- American Academy of Sleep Medicine Standards of Practice Committee. Practice parameters for the use of polysomnography in the evaluation of insomnia. Sleep. 1995;18:55–57. [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science. 2002;13:384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, et al. Loneliness and health: potential mechanisms. Psychosomatic Medicine. 2002;64:407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, et al. Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality. 2006;40:1054–1085. [Google Scholar]
- Cacioppo JT, Norris CJ, Decety J, Monteleone G, Nusbaum H. In the Eye of the Beholder: Individual Differences in Perceived Social Isolation Predict Regional Brain Activation to Social Stimuli. Journal of Cognitive Neuroscience. 2009;21:1–10. doi: 10.1162/jocn.2009.21007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Patrick W. Loneliness: Human nature and the need for social connection. New York: W. W. Norton & Company; 2008. [Google Scholar]
- Cannon WB. The role of emotion in disease. Annals of Internal Medicine. 1936;9:1453–1465. [Google Scholar]
- Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance use. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 1–4. [Google Scholar]
- Egidi G, Shintel H, Nusbaum HC, Cacioppo JT. Social isolation and neural correlates of attention control. 20th Annual Meeting of the Association for Psychological Science; Chicago, IL. 2008. [Google Scholar]
- Ernst JM, Cacioppo JT. Lonely hearts: Psychological perspectives on loneliness. Applied & Preventive Psychology. 1999;8:1–22. [Google Scholar]
- Fenn KM, Nusbaum HC, Margoliash D. Consolidation during sleep of perceptual learning of spoken language. Nature. 2003;425:614–616. doi: 10.1038/nature01951. [DOI] [PubMed] [Google Scholar]
- Gottlieb DJ. The Sleep Heart Health Study: A progress report. Current Opinion in Pulmonary Medicine. 2008;14(6):537–542. doi: 10.1097/MCP.0b013e328312ed61. [DOI] [PubMed] [Google Scholar]
- Harvey AG. Insomnia: Symptom or diagnosis? Clinical Psychology Review. 2001;21:1037–1059. doi: 10.1016/s0272-7358(00)00083-0. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Browne MW, Cacioppo JT. How can I connect with thee? Let me count the ways. Psychological Science. 2005;16:798–804. doi: 10.1111/j.1467-9280.2005.01617.x. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality and Social Psychology. 2003;85:105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structural factors to perceptions of relationship quality and loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology: Social Sciences. 2008;63B:S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology & Aging. 2006;21:152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Jacobs JM, Cohen A, Hammerman-Rozenberg R, Stessman J. Global sleep satisfaction of older people: The Jerusalem Cohort Study. Journal of the American Geriatrics Society. 2006;54:325–329. doi: 10.1111/j.1532-5415.2005.00579.x. [DOI] [PubMed] [Google Scholar]
- Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- Laposky AD, Bass J, Kohsaka A, Turek FW. Sleep and circadian rhythms: Key components in the regulation of energy metabolism. FEBS Letters. 2008;582:142–151. doi: 10.1016/j.febslet.2007.06.079. [DOI] [PubMed] [Google Scholar]
- Lesku JA, Rattenborg NC, Almaner JCJ. The evolution of sleep: A phylogenetic approach. In: Lee-Chiong T, editor. Sleep: A Comprehensive Handbook. Hoboken, NJ: John Wiley & Sons; 2006. pp. 49–61. [Google Scholar]
- Mahon NE. Loneliness and sleep during adolescence. Perceptual & Motor Skills. 1994;78:227–231. doi: 10.2466/pms.1994.78.1.227. [DOI] [PubMed] [Google Scholar]
- McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: Changes in core discussion networks over two decades. American Sociological Review. 2006;71:353–375. [Google Scholar]
- Ohayon MM. Prevalence and correlates of nonrestorative sleep complaints. Archives of Internal Medicine. 2005;165:35–41. doi: 10.1001/archinte.165.1.35. [DOI] [PubMed] [Google Scholar]
- Profant J, Ancoli-Israel S, Dimsdale JE. Are there ethnic differences in sleep architecture? American Journal of Human Biology. 2002;14:321–326. doi: 10.1002/ajhb.10032. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. Journal of Psychosomatic Research. 2002;53:561–569. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- Rotenberg K. Loneliness and interpersonal trust. Journal of Social and Clinical Psychology. 1994;13:152–173. [Google Scholar]
- Roth T, Jaeger S, Jin R, Kalsekar A, Stang PE, Kessler RC. Sleep problems, comorbid mental disorders, and role functioning in the national comorbidity survey replication. Biological Psychiatry. 2006;60:1364–1371. doi: 10.1016/j.biopsych.2006.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA Loneliness Scale: concurrent and discriminant validity evidence. Journal of Personality & Social Psychology. 1980;39:472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Shacham S. A shortened version of the Profile of Mood States. Journal of Personality Assessment. 1983;47:305–306. doi: 10.1207/s15327752jpa4703_14. [DOI] [PubMed] [Google Scholar]
- Shirom A, Toker S, Berliner S, Shapira I, Melamed S. The effects of physical fitness and feeling vigorous on self-rated health. Health Psychology. 2008;27:567–575. doi: 10.1037/0278-6133.27.5.567. [DOI] [PubMed] [Google Scholar]
- Spiegel K, Leproult R, Van Cauter E. Impact of sleep debt on metabolic and endocrine function. Lancet. 1999;354:1435–1439. doi: 10.1016/S0140-6736(99)01376-8. [DOI] [PubMed] [Google Scholar]
- Stickgold R, Hobson JA, Fosse R, Fosse M. Sleep, learning, and dreams: Off-line memory reprocessing. Science. 2001;294:1052–1057. doi: 10.1126/science.1063530. [DOI] [PubMed] [Google Scholar]
- Suka M, Yoshida K, Sugimori H. Persistent insomnia is a predictor of hypertension in Japanese male workers. J Occup Health. 2003;45:344–350. doi: 10.1539/joh.45.344. [DOI] [PubMed] [Google Scholar]
- Tochikubo O, Ikeda A, Miyajima E, Ishii M. Effects of insufficient sleep on blood pressure monitored by a new multibiomedical recorder. Hypertension. 1996;27:1318–1324. doi: 10.1161/01.hyp.27.6.1318. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Archives of General Psychiatry. 2007;64:234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]
- Worthman CM, Melby MK. Toward a comparative developmental ecology of human sleep. In: Carskadon MA, editor. Adolescent Sleep Patterns: Biological, Social, and Psychological Influences. Cambridge, United Kingdom: Cambridge University Press; 2002. pp. 69–117. [Google Scholar]