Abstract
Loneliness is a prevalent social problem with serious physiological and health implications. However, much of the research to date is based on cross-sectional data, including our own earlier finding that loneliness was associated with elevated blood pressure. In this study, we tested the hypothesis that the effect of loneliness accumulates to produce greater increases in SBP over a four-year period than are observed in less lonely individuals. A population-based sample of 229 50–68 year-old White, Black, and Hispanic men and women in the Chicago Health, Aging, and Social Relations Study was tested annually for each of five consecutive years. Cross-lagged panel analyses revealed that loneliness at study onset predicted increases in SBP 2, 3, and 4 years later (B = 0.152, SE = 0.091, p < .05, one-tailed). These increases were cumulative such that higher initial levels of loneliness were associated with greater increases in SBP over a 4-year period. The effect of loneliness on SBP was independent of age, gender, race/ethnicity, cardiovascular risk factors, medications, health conditions, and the effects of depressive symptoms, social support, perceived stress, and hostility.
Keywords: loneliness, blood pressure, aging, social isolation
Loneliness is a prevalent and serious social and public health problem (Cacioppo & Patrick, 2008). At any given time, up to thirty-two percent of adults over the age of 55 report feeling lonely (De Jong Gierveld & Van Tilburg, 1999), and from five to seven percent report feeling intense or persistent loneliness (Steffick, 2000; Victor, Scambler, Bowling, & Bond, 2005). Socially isolated individuals tend to feel lonely, but loneliness is not synonymous with being socially isolated. Loneliness is more accurately defined as the distressing feeling that accompanies discrepancies between one’s desired and actual social relationships. Number of relationships can be important, but perceived shortcomings in the quality of one’s relationships are particularly closely linked to loneliness (Hawkley et al., 2008; Peplau & Perlman, 1982; Pinquart & Sőrensen, 2003). Prospective studies have shown that feelings of loneliness predict depressive symptoms (Cacioppo, Hughes, Waite, Hawkley, & Thisted, 2006; Heikkinen & Kauppinen, 2004), impaired sleep and daytime dysfunction (Cacioppo, Hawkley, Berntson et al., 2002), impaired mental health and cognition (Wilson et al., 2007), nursing home admission (Russell, Cutrona, De La Mora, & Wallace, 1997), and mortality (Penninx et al., 1997). At the biological level, loneliness is associated with increased vascular resistance (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley, Burleson, Berntson, & Cacioppo, 2003), increased systolic blood pressure (Hawkley, Masi, Berry, & Cacioppo, 2006), increased hypothalamic pituitary adrenocortical activity (Adam, Hawkley, Kudielka, & Cacioppo, 2006; Steptoe, Owen, Kunz-Ebrecht, & Brydon, 2004), under-expression of genes bearing anti-inflammatory glucocorticoid response elements (GREs), over-expression of genes bearing response elements for pro-inflammatory NF-κB/Rel transcription factors (Cole et al., 2007), and altered immunity (Kiecolt-Glaser et al., 1984; Pressman et al., 2005).
Evidence is mounting that feelings of loneliness have serious physiological and health implications, but much of the research to date is based on cross-sectional data, including our own earlier finding that loneliness was associated with elevated blood pressure in a population-based sample of 50–68 year-old adults (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley et al., 2006). In the present study, we use longitudinal data to examine the degree to which loneliness explains increases in blood pressure over a four-year follow-up period in the same sample of aging adults. We posit a potentially causal role for loneliness because an experimental and an observational field study among young adults indicated that loneliness was associated with chronically elevated total peripheral resistance (TPR) (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley et al., 2003), and loneliness did not modulate the degree to which TPR increased in response to acute laboratory stress or ubiquitous daily stress. TPR levels behaved like a trait that varied as a function of individual differences in loneliness. Loneliness is relatively stable over time (3 year test-retest > .70) (Cacioppo, Hughes et al., 2006), and if the elevation in TPR in young adults contributes to higher SBP until age 55 years, then stable individual differences in loneliness should cumulate to influence SBP into middle adulthood. Our finding that loneliness was associated with increased SBP in a population-based sample of 50–68 year-old White, Black, and Hispanic men and women (Chicago Health, Aging, and Social Relations Study, CHASRS) was consistent with this logic. Moreover, the association between loneliness and SBP was greater in older than younger individuals in this cohort (Hawkley et al., 2006), suggesting that the effects of loneliness accrue to accelerate age-related increases in SBP (Hawkley & Cacioppo, 2007). In general, SBP increases slowly with age, averaging approximately 1 mm/year in individuals over 50 years of age (Diez Roux et al., 2002; Goldstein, Shapiro, & Guthrie, 2003). In the present study, we used longitudinal data to formally test the hypothesis that the effect of loneliness on blood pressure accumulates to produce greater increases in SBP over a four-year period in 50–68 year-old adults. Higher levels of baseline SBP tend to predict faster rates of increase in SBP (Whelton, 1994), and because loneliness was associated with elevated SBP in our sample (Hawkley et al., 2006), we simultaneously tested whether loneliness predicts increases in SBP over a one-, two-, or three-year period.
In our examination of the cross-sectional association between loneliness and SBP, we observed a sizeable relationship (an increase of one standard deviation in loneliness was associated with a 5 mm Hg increase in SBP) that was net of demographics (i.e., age, gender, ethnicity, education, income), behavioral and physical risk factors (i.e., smoking, body mass index, alcohol use), and use of blood pressure medications (Hawkley et al., 2006). We also found that depressive symptoms, perceived stress, hostility, and low social support--psychosocial risk factors that are related to loneliness and have been associated with cardiovascular disease and hypertension (Orth-Gomer et al., 2005; Rosengren et al., 2004; Rozanski, Blumenthal, & Kaplan, 1999; Steptoe, 2000)--did not account for the association between loneliness and SBP (Hawkley et al., 2006). Loneliness behaved as though it is a unique health risk factor in its own right. In testing the role of loneliness in predicting increases in blood pressure over a four-year period, we examine the degree to which the prospective association is unique to loneliness net of demographic characteristics, traditional cardiovascular risk factors, cardiovascular medications, depressive symptoms, perceived stress, hostility, and social support.
Method
Participants
Data for this study were collected annually between 2002 and 2006, as part of the Chicago Health, Aging, and Social Relations Study (CHASRS). CHASRS is a longitudinal, population-based study of non-Hispanic White, African American, and non-Black Latino American persons born between 1935 and 1952, and living in Cook County, IL. The sample was selected using a multistage probability design in which the first stage involved identifying a subset of households estimated to have high probability of containing at least one adult aged 50–65 years (24 percent of the total frame). A stratified, equal-probability-of-selection sample was drawn from this subset. The three strata were (1) households from census tracts in which at least 80 percent of the residents were African American, (2) households for which the associated surname was identified by the U.S. Census Department as "Hispanic", and (3) all remaining households. The second stage involved selecting one age-eligible individual per household, and screening selected individuals to include only those who belonged to one of the three racial/ethnic groups of interest and were sufficiently ambulatory to come to the University and participate in the study. A quota sampling strategy was used at both the household and individual levels to achieve an approximately equal distribution of participants across the six gender by racial/ethnic group combinations. Response rates approached 45% overall, an impressive rate given that participation in our study involved predominantly working adults spending an entire day at the University. The final sample consisted of 229 individuals who ranged from 50–68 years of age on the first testing occasion. The study was approved by the Institutional Review Board of the University of Chicago, and all participants gave informed consent.
The distribution of our sample on a number of characteristics compares quite closely to that obtained from the national population-based Health and Retirement Survey (HRS). For instance, self-rated health was rated as “excellent” or “very good” in 48% of 55–64 yr-olds in HRS (NIH Publication No. 07-5757, 2007), and in 40% of the 50–68 yr-olds in CHASRS (which over-sampled Blacks and Hispanics with known poorer self-rated health status than Whites). In the U.S. population, 83–87% of those aged 50–64 years are high school graduates or more (Stoops, 2004), and in our sample, 84% are high school graduates or more.
Sample attrition over the course of the 5-year study averaged 7.2% annually, resulting in a sample size of 163 in Year 5 (2006). Attriters over this time period had fewer years of education and more chronic health conditions at study onset, and were more likely to be Black or Hispanic than White. Attriters and non-attriters did not differ in age, gender, marital status, household income, religious participation, number of voluntary group memberships, SBP, BMI, cardiovascular or antihyperlipidemia medications, smoking, alcohol ingestion, probability and duration of physical activity, loneliness, depressive symptoms, perceived stress, hostility, or social support.
Procedures
For each of five annual visits to our laboratory, participants arrived between 8:00 and 9:00 a.m., whereupon informed consent was obtained before beginning a day of assessments that included standard psychological surveys, health and medication interviews, anthropometric measurements, and a cardiovascular protocol that included blood pressure measurement. All psychological measures reported in this paper, including loneliness, were obtained in the first survey packet of the day. During the health interview, participants were asked whether they had ever been diagnosed with a series of twenty health conditions, including heart attack, congestive heart failure, stroke, chronic obstructive pulmonary disease, ulcers, diabetes, and kidney disease. Participants were asked to bring their medications with them to the laboratory, and experimenters recorded drug name, dosage, and frequency for subsequent coding. Height and weight were obtained using a standard medical scale.
Cardiovascular measures were obtained prior to lunch for all participants. Sensors for electrocardiograph, impedance cardiograph, and blood pressure recording were attached to participants. Participants were then seated in a comfortable padded chair. During a 15-minute adaptation period, participants completed questionnaires while experimenters established good signal quality. Participants then sat quietly for an additional five minutes prior to recording of baseline cardiovascular activity. For the purposes of the present study, only blood pressure measurements are reported.
Blood Pressure Measurement
A Colin Vital Statistics Monitor (Model BP-508; Vital Signs, Minster, OH) was used to obtain beat-by-beat systolic, diastolic, and mean arterial blood pressure readings from the non-dominant arm which was supported at heart level by a cushion resting on the arm of the participant’s chair. The Colin Monitor records a pulse wave tonometrically by partial occlusion of the radial artery against the radius at the wrist, allowing for beat-to-beat measurement of blood pressure. The tonometer was calibrated against an initial blood pressure reading obtained using an oscillometric cuff and was periodically recalibrated either automatically or on experimenter initiation. Systolic blood pressure was defined as the mean SBP during a four-minute seated, resting baseline.
As we did in our earlier cross-sectional study (Hawkley et al., 2006), we focus on SBP because it is superior to DBP in predicting cardiovascular disease (Chobanian et al., 2003), especially in adults over the age of 50 yrs (Franklin et al., 1997). After about 50 years of age, DBP gradually decreases (see, for example, Diez Roux et al., 2002) while SBP continues to increase. According to Franklin et al. (1997), “Age-related stiffening of the aorta is associated with a decreased capacity of the elastic reservoir and hence a greater peripheral runoff of stroke volume during systole. Thus, with less blood remaining in the aorta at the beginning of diastole, and with diminished elastic recoil, diastolic pressure decreases with increased steepness of diastolic decay.” These physiological changes and the superiority of SBP in predicting health outcomes support our focus on SBP in this age group.
Loneliness Measurement
UCLA Loneliness Scale-Revised (UCLA-R)
The UCLA-R has been shown to possess construct validity (Russell, Peplau, & Cutrona, 1980) as a measure of general loneliness and degree of satisfaction with one’s social network. Examples of the items are, “I lack companionship” and “I feel in tune with the people around me.” Each of the 20 items is rated on a scale of 1 (never), 2 (rarely), 3 (sometimes), and 4 (often). Cronbach’s alpha across all 20 items ranged from .90 to .92 across all 5 years of CHASRS (mean = .91). After reverse scoring appropriate items, loneliness scores are calculated by summing all items. The range of possible scores is 20 to 80, with higher scores signifying greater loneliness.
Covariates
Demographic covariates were age at study onset, gender, race/ethnicity, and education (high school diploma or GED). Social network size was included as a covariate to determine the degree to which objective social isolation/integration accounted for the effect of subjective isolation (i.e., loneliness) on SBP. Social network scores were based on a weighted combination of marital status (62% of the sample was married or living with a partner), number of relatives and friends with whom the participant reported interacting at least once every two weeks, voluntary group membership, and religious group affiliation. Following as closely as possible the procedures described by Berkman (Berkman, 1977), we collapsed the 12 possible social network scores into four categories: low, medium, medium-high, and high.
Current smoking status, alcohol consumption, body mass index (BMI; weight in kg/(height in m)2), physical activity, cardiovascular medications, and chronic health conditions were included as covariates because of their known associations with blood pressure and/or loneliness. Smoking and alcohol consumption were dummy-coded to contrast current smokers and drinkers with non-smokers and non-drinkers respectively (the reference categories). Physical activity was measured using a modified version of the Minnesota Leisure Time Physical Activity Questionnaire that asks about activities performed in the last 14 days (Mcphillips, Pellettera, Barrett-Connor, Wingard, & Criqui, 1989). Physical activity was defined as present or absent as has been described previously (Hawkley, Thisted, & Cacioppo, In Press). Cardiovascular medications were coded using a standardized scheme available from www.multum.com. The Multum database permits coding of generic and brand name drugs by pharmacologic and therapeutic categories. For the present study, two medication categories—anti-hyperlipidemia agents (e.g., simvastatin), and a broad range of cardiovascular agents (e.g., beta blockers, ACE-inhibitors, diuretics, etc.)—were defined as present (i.e., prescribed) or absent. Chronic conditions (e.g., diabetes, stroke) were assessed by interview, and the Charlson comorbidity index (Charlson, Pompei, Ales, & Mackenzie, 1987) was derived as the sum of chronic conditions weighted by severity (Katz, Chang, Sangha, Fossel, & Bates, 1996). Although we asked subjects whether they had ever been told by a physician that they had hypertension or high blood pressure, hypertension is not included in the Charlson index.
In a final model, we added depressive symptoms, perceived stress, hostility, and social support as covariates to assess whether reciprocal lagged relationships between loneliness and SBP were independent of the lagged effects of these related psychosocial variables on SBP. Loneliness is associated with, and plays a causal role in, depressive symptoms, perceived stress, hostility, and perceptions of poor social support (Cacioppo, Hawkley, et al., 2006). Nevertheless, loneliness is conceptually distinct from these related psychosocial variables. For instance, whereas loneliness is a painful and aversive condition that is marked by a sense of emptiness, worthlessness, lack of control, and personal threat in one’s social relationships (Cacioppo & Patrick, 2008), depressive symptoms are painful, aversive feelings that dominate all aspects of life, not only social relationships (Booth, 2000; Weiss, 1973). Perceived stress is a percept that the strain of life circumstances requires more time and energy than one is prepared or able to give. Feeling stressed is only one of the “symptoms” of loneliness. Hostility is another “symptom” of loneliness, but neither stress nor hostility is unique to loneliness, nor is loneliness subsumed by stress or hostility. Perceived social support is the percept that others are or will be available to provide instrumental, tangible, or emotional support in times of need. Feelings of loneliness extend beyond perceptions of available support and color social cognitions about social relationships past, present, and future (Cacioppo, Hawkley et al., 2006; Cacioppo & Patrick, 2008).
Depressive symptoms were measured using the Center for Epidemiological Studies Depression Scale (Radloff, 1977), and the item about loneliness was dropped before calculating a total depressive symptoms score (referred to as CESDML, range=0–56). Perceived stress was measured using the Perceived Stress Scale (PSS, range=0–40) (Cohen & Williamson, 1988), hostility with the Cook-Medley Hostility Scale (CMHo, range=0–50) (Cook & Medley, 1954), and social support with the Interpersonal Support Evaluation List (ISEL, range=4–16) (Cohen, 2008). The psychometric characteristics of these scales in the CHASRS study have been reported elsewhere (Hawkley et al., 2006).
Data Analysis
Analyses were conducted using a cross-lagged panel model approach (Curran, 2000) to simultaneously address reciprocal influences on loneliness and SBP. The substantive research question under investigation in the present study is the degree to which loneliness has long- and short-term effects on SBP independent of any reciprocal effects of SBP on loneliness. Cross-lagged panel analysis is the most practical analytic solution for this question because it allows modeling of chronic and transient effects of loneliness. For short-term effects, we examined the degree to which loneliness explained changes in SBP over a one-year period holding constant prior year loneliness and SBP. In other words, we asked whether changes in loneliness over a one-year period predicted changes in SBP over the subsequent one-year period. For long-term effects, we examined the degree to which a stable aspect of loneliness explained changes in SBP over a two-, three-, and four-year period. We posited that short-term changes in loneliness would not exert a noticeable influence on SBP, but that a chronic trait-like component of loneliness would influence SBP over a longer time interval independent of any short-term effects. Specifically, we tested long-term effects by examining the degree to which annual changes in SBP were predicted by initial loneliness levels that had been measured two, three, or four years earlier.1
The cross-lagged panel analyses were conducted with MPlus (version 5) (Muthen & Muthen, 2002). All analyses were conducted using full information maximum likelihood estimation with robust standard errors (Little & Rubin, 1987). In the present study, covariance coverage values, which indicate the proportion of data present to estimate each pairwise relationship, ranged from 53% to 90%. The degree of model fit was assessed using the chi-square goodness of fit statistic and the root mean square error of approximation (RMSEA) (Browne & Cudeck, 1992). Models with an RMSEA of .05 or less have been characterized as having a good fit, .10 or more as a poor fit (Hu & Bentler, 1999), and .08 or less as having adequate fit (Maccallum, Browne, & Sugawara, 1996). We report unstandardized regression coefficients (B) and correlations (r, obtained as standardized regression coefficients), with an alpha level of .05 throughout. Loneliness has been associated with increased SBP, and exhibited a stronger association with SBP with increasing age (Hawkley et al., 2006), so we hypothesized that loneliness will predict an increase in SBP over time in this longitudinal study. Accordingly, we employed a directional (one-tailed) test of significance for this effect.
Results
Table 1 provides sample characteristics of the CHASRS cohort. Table 2 lists means, standard deviations, and intercorrelations for SBP and UCLA-R values at each annual assessment. SBP showed moderate temporal reliability, r’s = .42–.47. UCLA-R showed moderate to high temporal reliability, r’s = .63–.79. For cases providing SBP data in Years 1 and 5 (N = 150), the age-adjusted 4-year increase in SBP was 2.49 mm Hg, equivalent to an annual age-adjusted increase of approximately 0.6 mm Hg.
Table 1.
Characteristics of the CHASRS sample at study onset (N=229, unless otherwise indicated).
| Characteristic | Statistic |
|---|---|
| Age (mean yrs) | 57.4 (SD = 4.5) |
| Female (%) | 52.4 |
| Ethnicity (%) | |
| White | 35.8 |
| African American | 35.4 |
| Latino Americana | 28.8 |
| Education (mean years, N = 223) | 13.3 (SD = 3.1) |
| Household income (median $, N = 216) | 50,000–75,000 |
| Social network index (%, N = 225) | |
| Low | 7.9 |
| Medium | 19.2 |
| Medium-high | 43.2 |
| High | 27.9 |
| Smoking status (%, N = 223) | |
| Current smoker | 15.2 |
| Alcohol (%, N = 223) | |
| Current drinker | 65.9 |
| Body mass index (mean kg/m2) | 31.4 (SD = 6.7) |
| Exercise, any during last 14 days (%, N = 226) | 88.9 |
| Anti-hyperlipidemia medications (%, N = 228) | 18.9 |
| Cardiovascular medications (%, N = 228) | 43.0 |
| Charlson Comorbidity Index (mean, N = 214) | 0.53 (SD = 1.43) |
| Depressive symptoms, CESDML (mean, N = 225) | 9.8 (SD = 8.5) |
| Perceived Stress, PSS (mean, N = 223) | 13.3 (SD = 6.4) |
| Hostility, CMHo (mean, N = 216) | 17.4 (SD = 7.7) |
| Social support, ISEL (mean, N = 218) | 12.9 (SD = 2.2) |
The greatest majority of these individuals are Mexican (72%), with the remaining individuals representing a wide range of ethnicities (e.g., Puerto Rican, Cuban, Chilean, Colombian, Dominican, etc.).
CESDML = Center for Epidemiological Studies Depression Scale, minus the loneliness item; PSS = Perceived Stress Scale; CMHo = Cook-Medley Hostility Scale; ISEL = Interpersonal Support Evaluation List.
Table 2.
Means, standard deviations, and intercorrelations among SBP and UCLA loneliness scores.
| Variable (N) | M | SD | SBP 1 |
SBP 2 |
SBP 3 |
SBP 4 |
SBP 5 |
UCLA 1 |
UCLA 2 |
UCLA 3 |
UCLA 4 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| SBP, Year 1 (223) | 130.6 | 19.6 | - | ||||||||
| SBP, Year 2 (202) | 129.7 | 18.4 | .59** | - | |||||||
| SBP, Year 3 (187) | 129.7 | 17.7 | .43** | .60** | - | ||||||
| SBP, Year 4 (170) | 129.7 | 15.3 | .44** | .48** | .44** | - | |||||
| SBP, Year 5 (154) | 132.2 | 15.1 | .42** | .50** | .47** | .56** | - | ||||
| UCLA Loneliness, Year 1 (225) | 36.0 | 9.8 | .19** | .17* | .003 | .09 | .12 | - | |||
| UCLA Loneliness, Year 2 (206) | 35.4 | 9.7 | .16* | .09 | −.03 | .10 | −.05 | .76** | - | ||
| UCLA Loneliness, Year 3 (191) | 35.6 | 9.5 | .14 | .03 | −.03 | .05 | −.01 | .74** | .84** | - | |
| UCLA Loneliness, Year 4 (177) | 38.1 | 8.6 | .03 | .02 | .004 | −.04 | −.09 | .65** | .75** | .79** | - |
| UCLA Loneliness, Year 5 (162) | 36.8 | 8.1 | .03 | .03 | −.03 | −.01 | −.08 | .63** | .78** | .79** | .83** |
SBP = systolic blood pressure
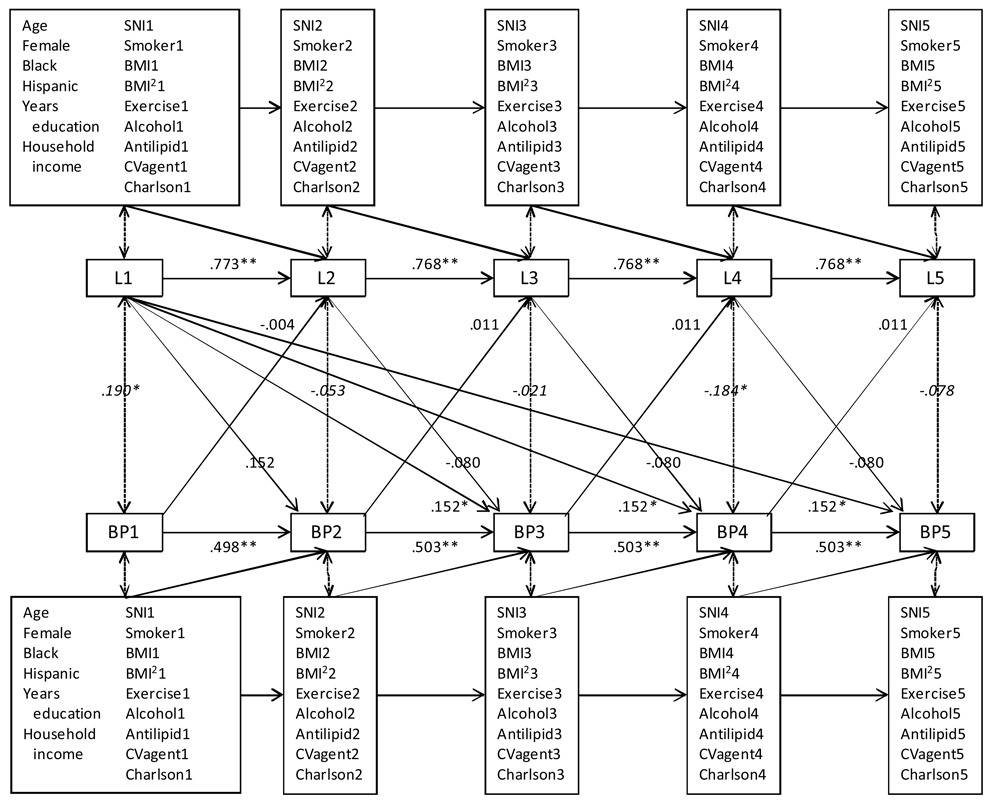
A cross-lagged panel model was specified to examine reciprocal relationships between SBP and loneliness over the course of the five-year study. The model is depicted in Figure 1. Our theoretical model holds that the one-year autoregressive paths (i.e., autocorrelations that represent stability of each of the variables over time) and lagged effects of loneliness, SBP, and covariates do not differ from year to year, but because we cannot model the predecessors of Year 1, we expected Year 1 lagged effects to be somewhat different. This model was specified by allowing the autoregressive paths (single-headed arrows from a given variable at one time point to the same variable at the next time point) and one-year lagged effects (diagonal single-headed arrows) of Year 1 predictors and covariates to be freely estimated. For subsequent years, we applied equality constraints to the autoregressive paths and one-year lagged paths. In addition, long-lagged pathways from loneliness in Year 1 to SBP in Years 3, 4, and 5 were constrained to equality. The application of equality constraints imposes stationarity on the relationships among variables in the model and the resulting model fit can be compared to a model in which these relationships are freely estimated. Demographic characteristics at study onset were treated as covariates predicting only Year 2 UCLA-R and SBP, under the assumption that any subsequent influence of these static individual differences operates through their association with intervening covariates in the model.
Figure 1.
Cross-lagged panel model showing that loneliness has a long-lag effect on blood pressure net of demographic, behavioral, health, and medication covariates. Regression weights for unidirectional pathways are unstandardized. Bidirectional pathways are standardized and equivalent to correlations.
L = UCLA Loneliness; BP = Systolic Blood Pressure; Age = age at study onset, in years; Female = female gender; Black = non-Hispanic black race/ethnicity; Hispanic = Hispanic race/ethnicity; SNI = Social network index; Smoker = current smoker, yes/no; Exsmoker = former smoker, yes/no; BMI = body mass index; Exercise = any activity in past 14 days, yes/no; Alcohol = current drinker, yes/no; Antilipid = anti-lipid medication, yes/no; CVagent = cardiovascular medication, yes/no; Charlson = Charlson comorbidity index. Digit suffixes refer to study year.
* p < .05, ** p < .01.
The partially stationary model fit the data adequately, χ2(1403) = 2713.282, p < .0001; RMSEA = .064, 90% CI: .060, .067. A second model was tested in which the equality constraints were lifted from the lagged effects of covariates and long-lagged effects of loneliness on SBP in Years 3, 4, and 5. The nonstationary model fit the data no better than the stationary model, χ2(1365) = 2679.280, p < .0001, χ2 difference (38) = 34.002, p >.6, and the stationary model was therefore preferred for its parsimonious representation of associations in the data. Figure 1 depicts this model and the results. The autoregressive coefficients for loneliness were significant, B’s > 0.7, SE’s < .06, p’s < .001, as were the autoregressive coefficients for SBP, B’s ≥ 0.49, SE’s < .07, p’s < .001. Loneliness did not exhibit significant one-year lagged effects on SBP, Byear 2 = 0.152, SE = 0.146, p = .3; Byears 3–5 = −0.080, SE = 0.104, p > .4, and SBP did not exhibit significant one-year lagged effects on loneliness, Byear 2 = −0.004, SE = 0.027, p > .8; Byears 3–5 = 0.011, SE = 0.014, p>.4. Net of autoregressive effects, and consistent with our hypothesis, loneliness at study onset had a significant effect on SBP two, three, and four years later, B = 0.152, SE = 0.091, p < .05, one-tailed. In other words, one year is insufficient to capture the influence of loneliness on SBP. Instead, the longer-lagged effects reveal the durable influence of loneliness on annual SBP changes two or more years later, holding constant its short-term effects. If we compare two subjects who at study onset differ only by a 10-point difference in loneliness, this model predicts that the lonelier person’s SBP would be 2.1 mm higher in Year 5 than that of the less lonely person. Loneliness is also associated with higher SBP at Year 1, however, and when we take that into account, the model predicts that the lonelier person’s baseline SBP would be 3.7 mm higher at study onset and 2.3 mm higher in Year 5 than that of the less lonely person.
Table 3 lists correlations of covariates with SBP and UCLA-R at study onset. Prospective effects of covariates are provided by the cross-lagged panel model. Among the demographic covariates, the cross-lagged analysis showed that years of education predicted decreases in loneliness between Years 1 and 2, but none of the demographic covariates predicted changes in SBP. Net of demographic variables, cardiovascular medication use and chronic health conditions tended to predict increases in SBP between Years 1 and 2. Neither cardiovascular medication use (B = 1.743, SE = 1.287, p > .1) nor chronic health conditions (B = 0.71, SE = 0.61, p > .2) predicted further increases in SBP subsequent to Year 2, likely due to the relative stability of cardiovascular medication use (rYears 2–5 > 0.80, p < .001) and chronic conditions (rYears 2–5 > 0.72, p < .001) over the duration of the study. No other covariates showed prospective associations with either loneliness or SBP. Importantly, the long-term effect of loneliness on SBP persisted net of the relationships of demographic and cardiovascular risk factor covariates with loneliness and SBP.
Table 3.
Pearson correlations of covariates with SBP and UCLA loneliness scores at study onset.
| Covariate | SBP | UCLA |
|---|---|---|
| Age | .11 | −.07 |
| Female | −.02 | −.13 |
| Black (vs. White & Hispanic) | .13† | .04 |
| Hispanic (vs. White & Black) | −.02 | .14* |
| Years education | −.26** | −.11 |
| Household income | −.18** | −.19** |
| Social network size | −.16* | −.19** |
| Current smoker | .06 | .06 |
| Current drinker | −.15* | −.06 |
| Body mass index | .13† | .02 |
| Any exercise | −.12 | −.16* |
| Anti-hyperlipidemia medication | .10 | −.03 |
| Cardiovascular medication | .18** | −.05 |
| Charlson comorbidity index | .14* | .17* |
| Depressive symptoms, CESDML | .14* | .57** |
| Perceived stress, PSS | .20** | .48** |
| Hostility, CMHo | .22** | .34** |
| Social support, ISEL | −.10 | −.58** |
p < .01,
p < .05,
p < .06
CESDML = Center for Epidemiological Studies Depression Scale, minus the loneliness item; PSS = Perceived Stress Scale; CMHo = Cook-Medley Hostility Scale; ISEL = Interpersonal Support Evaluation List.
A second panel model examined whether the effects of loneliness on SBP persisted net of the one-year lagged effects of depressive symptoms, perceived stress, hostility, or social support. As was done for all time-varying covariates, Year 1 effects of these psychosocial variables were unconstrained, and Years 2–5 effects were constrained to equality. Adding the psychosocial variables to the original model resulted in a reasonable fit, χ2(2515) = 4796.569, p < .001; RMSEA = .063, 90% CI: .060, .066. Of the psychosocial variables, social support had a one-year lagged effect on loneliness, Byear 2 = −0.56, SE = 0.27, p < .05; Byears 3–5 = −.83, SE = 0.16, p < .001, but none of the psychosocial covariates exhibited a one-year lagged effect on SBP, p’s > .1. The long-lagged effect of loneliness on SBP was only modestly reduced in size, B = 0.130, SE = 0.085, p < .1, one-tailed. Given the absence of longitudinal effects of the psychosocial covariates on SBP, the model depicted in Figure 1 provides the most parsimonious depiction of the lagged relationship between loneliness and SBP.
Discussion
Over a nine-year follow-up in the Atherosclerosis Risk in Communities Study, an age-adjusted SBP increase of approximately 1 mm Hg per year was observed in a sample of 8,555 adults 45–64 years old (Diez Roux et al., 2002). We tested a much smaller sample of 229 adults 50–68 years old over a shorter follow-up period of four years, and we found a somewhat smaller age-adjusted increase in SBP of approximately 0.6 mm Hg per year. Estimates of SBP change over a longer follow-up period would be expected to provide somewhat different estimates of age-related trends in SBP. In addition, attrition in CHASRS claimed less healthy adults at a higher rate than healthy adults, and the loss of just a few such subjects from our relatively small sample could result in underestimates of change in SBP over time.
Importantly, increases in SBP were not homogeneous across the sample. By way of example, individuals differing by one standard deviation in their loneliness level differed in SBP such that the lonelier individual was predicted to have a 2.3 mm greater increase in SBP over four years on top of a 3.7 mm higher SBP at study onset. Across the full range of loneliness scores (20–80, SD ≃ 10), these estimates predict that the most lonely individuals will exhibit SBP increases of 3.6 mm/year (0.6*6 SDs), or a 14.4 mm greater increase in SBP than their least lonely counterparts over the course of 4 years. Faster rates of increases in SBP translate into higher rates of clinical hypertension at a younger age. Hypertension is the most common primary diagnosis in the U.S., is the primary or contributing cause of about 18% of U.S. deaths, and is estimated to cost $73.4 billion in 2009 (Lloyd-Jones et al., 2009). Our data indicate that lonelier individuals may be over-represented in the hypertensive segment of the population, and at a younger age. The economic cost of hypertension and the price it exacts in quality and quantity of life suggest that loneliness has significant clinical and public health implications. In addition, special national advisory committees encourage physicians to heed even small differences in SBP because the risk for cardiovascular disease is continuous across the range of SBP from 115 – 185 mm Hg (Chobanian et al., 2003). We conclude that the risk for high and more rapidly increasing SBP associated with loneliness warrants clinical attention.
Loneliness did not have a significant short-term (i.e., one year) lagged effect of loneliness on SBP, but when the short-term effect of loneliness on SBP was held constant, loneliness was revealed to have a durable influence that was evident in larger increases in SBP over a four-year period. We have posited that the physiological effects of chronic loneliness accrue gradually to accelerate increases in SBP (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley & Cacioppo, 2007), and a one-year lag may not be sufficient to capture the effect of this accrual on SBP. High measurement reliability is important when examining long-term influences, so we ensured at each annual assessment that participants were well-habituated to the laboratory setting prior to the initiation of blood pressure readings. SBP was determined by averaging over hundreds of beat-by-beat readings to obtain a reliable and internally consistent measurement. These procedures revealed a cumulative long-term effect of loneliness on SBP in a population-based sample of 50–68 year-old adults.
The long physiological shadow cast by chronic loneliness may begin earlier in life than middle age, however. First, the SBP levels of lonely and nonlonely adults were already distinguishable at study onset. Physiological processes yet to be delineated, but possibly including increases in TPR, could have been operative for years prior to our study for us to observe higher SBP in lonelier 50–68 year-old adults. Second, evidence for an early accrual onset includes the finding that, among 26-year-old adults in the longitudinal Dunedin Multidisciplinary Health and Development Study, chronic social isolation, rejection, and/or feelings of loneliness in early childhood, adolescence, and young adulthood had a dose-response association with number of risk factors for poor cardiovascular health, including elevated blood pressure (Caspi, Harrington, Moffitt, Milne, & Poulton, 2006).
The strength of the association between loneliness and SBP could be expected to diminish in the elderly, however. Until the fifth decade of life, total peripheral resistance is the primary determinant of increases in SBP, after which arterial stiffening plays a growing role (Franklin et al., 1997). In prior research, we observed that lonely young adults exhibited chronically elevated levels of TPR relative to their age-matched nonlonely counterparts (Cacioppo, Hawkley, Crawford et al., 2002; Hawkley et al., 2003). Faster rates of increase in TPR and blood pressure foster earlier development of arterial stiffening and further increases in SBP (Franklin et al., 1997). By this logic, loneliness may be associated with earlier or larger structural changes in resistance arteries that favor collagen deposition and the loss of elastic fiber content, but may no longer be associated with changes in blood pressure that derive from arterial stiffening.
Second, pharmaceutical treatment for high blood pressure increases with age. Some evidence suggests that loneliness motivates people to visit their physician (Cheng, 1992) and the emergency department (Geller, Janson, McGovern, & Valdini, 1999), perhaps for the social contact as much if not more than for medical reasons, and this may result in a greater probability of being prescribed medications. To the extent that SBP is more likely to be treated by medication in lonely than nonlonely individuals, loneliness may exhibit an attenuated association with SBP in elderly adults. A treatment effect would depend on comparable adherence to medication regimens across the range of loneliness feelings, and in support of this assumption, compliance was not associated with loneliness in an earlier study of the CHASRS sample (Kudielka, Hawkley, Adam, & Cacioppo, 2007). Future research should examine whether differential healthcare utilization and treatment explain loneliness differences in SBP.
Finally, loneliness and high blood pressure have been associated with higher rates of mortality (Penninx et al., 1997). If poor health or death result in earlier attrition of lonely than nonlonely individuals, the association between loneliness and SBP will diminish with time. Indeed, in older adults, loneliness-related attrition may have already occurred if poor health compelled individuals to discontinue participation, or if it prevented their participating in the study in the first place. Attrition in our sample was not associated with loneliness, but we cannot rule out loneliness-related recruitment failures. Additional longitudinal research on older adults is needed to evaluate the extent to which differential experimental mortality attenuates the association between loneliness and SBP.
We note that high BMI, smoking, and lack of physical activity, factors that are typically considered risk factors for elevated SBP, did not explain the effects of loneliness on SBP over the 4-year follow-up period. Our dichotomous measure of physical activity is rudimentary, however, and measures of activity duration and frequency may be more relevant to changes in SBP over time. In supplementary analyses of a subset of the sample with activity duration data, we found no change in the pattern of results when we substituted activity duration for the dichotomous measure of activity. Additional research is needed to replicate this effect and determine the role of alternative measures of physical activity in explaining loneliness differences in the rate of increase in SBP over time. There may be other unmeasured or omitted covariates that account for the prospective influence of loneliness on SBP. Dietary intake is one possibility. In supplementary analyses, we failed to find an association between caloric intake and SBP either at study onset or prospectively. Intake of specific nutrients or non-nutritive food may nevertheless contribute to SBP, and it remains an open question whether loneliness influences food choices that affect SBP. A second example is alcohol consumption. Although we controlled for differences between drinkers and non-drinkers, the prospective effect of loneliness on SBP may be better explained by taking into consideration the amount of alcohol consumed and the effects of binge drinking. A third example is access to healthcare. Health insurance coverage is uneven in the U.S., and to the extent that loneliness is associated with a lower probability of having health insurance, this factor may contribute to loneliness differences in healthcare utilization relevant to SBP. Future research should consider the role not only of health insurance, but also of neighborhood factors that influence access to healthcare resources (e.g., location of healthcare facilities, public transportation) in explaining loneliness differences in rates of SBP increase over time.
The effects of loneliness on SBP may differ as a function of chronic disease status, cardiovascular medication use, hypertension, and obesity. In supplementary analyses of subsets of participants who were initially healthy (i.e., no chronic conditions), unmedicated (i.e., no anti-hyperlipidemic or cardiovascular medications), and normotensive (i.e., not on cardiovascular medications and SBP <140), loneliness persisted in its lagged effects on SBP two, three, and four years later. In initially healthy individuals and unmedicated individuals, the long-lagged effects of loneliness were comparable to that observed in the full sample (B = 0.136 and B = 0.165, respectively, vs. 0.152). In initially normotensive participants, the long-lagged effect of loneliness was larger in magnitude, B = 0.243, SE = 0.144, p < .1, one-tailed, than in the full sample. On the other hand, in initially non-obese participants (i.e., BMI below the 80th percentile within each racial/ethnic group), the long-lagged effect of loneliness was reduced from B = 0.152 to B = 0.115. Additional research is needed to examine whether health status, medication use, hypertension, and obesity moderate the prospective effect of loneliness on SBP.
What physiologic mechanisms might explain loneliness differences in age-related SBP increases? As reviewed above, we hypothesize that elevated levels of total peripheral resistance contribute to loneliness-related SBP increases at least until 50 years of age. This hypothesis would ideally be tested in a study of individuals from young adulthood to age 55 or more to establish TPR as a contributor to loneliness differences in SBP later in life. Physiologic pathways leading to elevated TPR may involve increased activation of the sympathetic nervous system. We have observed an association between loneliness and epinephrine concentrations in overnight urine samples (Hawkley et al., 2006) that is consistent with this possibility. Loneliness has also been associated with increased activity of the hypothalamic-pituitary-adrenocortical axis as reflected in higher levels of circulating cortisol (Pressman et al., 2005) and an elevated salivary cortisol response to awakening (Adam et al., 2006; Steptoe et al., 2004). Cortisol operates through the vascular nitric oxide system to affect blood pressure, and we posit that loneliness may influence TPR and SBP through its influence on cortisol and vascular endothelial function. Additional research is needed to determine the degree to which neuroendocrine pathways and endothelial function contribute to loneliness-related increases in SBP.
Among possible psychosocial mediators of the effect of loneliness, we found no evidence that depressive symptoms, perceived stress, hostility, or low social support accounted for the influence of loneliness on SBP. Another potential mediator is inhibited temperament. Loneliness is correlated with shyness, and in our sample, the correlation was r(210) = .39, p < .001. However, we saw no correlation between shyness and SBP, r(206) = −.03, p > .6. It is worth noting that temperament is not as stable across the life course as is often assumed. For instance, a recent meta-analysis found decreases in one aspect of introversion (i.e., social submission) across the life course (Roberts, Walton, & Viechtbauer, 2006). This is not to say that inhibited temperament does not influence physiology and health over the long term. To the best of our knowledge, however, evidence for an association between inhibited temperament and blood pressure in the extant literature is limited to a single study that found higher SBP in high- than low-shy older adults (Bell, et al., 1993). Whereas shyness is often characterized by avoidance of social interactions due to lack of confidence and awkwardness, loneliness is characterized by a motivational impulse to connect with others but also a fear of negative evaluation, rejection, and disappointment. We hypothesize that threats to one’s sense of safety and security with others are the toxic component of loneliness, and that hypervigilance for social threat (conscious or unconscious) may contribute to alterations in physiological functioning, including elevated blood pressure.
Do effective interventions for loneliness exist? We recently completed a meta-analysis examining the effectiveness of interventions for loneliness published between 1970 and April 2009 (Masi, Chen, Hawkley, & Cacioppo, under review). Our assumption when we began the study was that our analyses would support the general conclusion found in qualitative reviews, namely that group interventions (i.e., providing people with opportunities to interact and form relationships with others) effectively reduce loneliness. To our surprise, our quantitative literature review revealed that studies with the highest quality design (randomized control group design) showed absolutely no intervention effect, regardless of intervention type and numerous other potential moderators. We believe the failure of prior interventions is based in part on a faulty understanding of loneliness; loneliness is not synonymous with being alone or isolated. We are in the process of designing an intervention based on our theory that loneliness is a subjective state of perceived isolation that, without our awareness, colors attention, cognition, and behavior in self-defeating ways (Cacioppo & Hawkley, 2009). Accordingly, an effective intervention would be expected to include cognitive-behavioral training and practice in (1) extending oneself socially, (2) increasing one’s awareness of qualities of good relationships, (3) selecting relationship partners carefully to optimize synergies, (4) being more optimistic and expecting the best from relationship partners, and (5) synchronizing affect and behavior with a relationship partner (Cacioppo & Patrick, 2008).
Most medical practitioners have neither the time nor the training to follow-up on psychosocial risk factors for high blood pressure or health more generally. However, a simple assessment of loneliness by questionnaire or interview could be sufficient to determine whether the patient should be referred to a clinical psychologist for therapy. Although no effective therapy for loneliness has yet been documented, a cognitive-behavioral therapist should be able to identify and address specific sources of problems in patients’ social experiences. Of course, even if loneliness is reduced, we have no evidence that blood pressure will also be reduced. Given that the physiological changes that lead to high blood pressure are often irreversible (e.g., arteriosclerosis), a reasonable goal may be to attenuate the subsequent rate of SBP increase. The more important goal may be to detect and treat loneliness early in life, before it has an opportunity to take a toll on physical and mental health and well-being.
Patterns of social integration have been transformed in late modern United States, and the implications for loneliness and its role in health and well-being are profound. Dramatic changes in the family have been noted in higher divorce rates and a higher proportion of adults living alone (Casper & Bianchi, 2002). Greater heterogeneity in life paths, increasing income inequality, and a more diverse population may be eroding the basis for feeling connected with others (Hughes & O'Rand, 2004). A recent study supports this view, finding that Americans’ discussion networks shrank significantly between 1985 and 2004, with the modal number of confidants reported by Americans across the past two decades declining from three to zero (McPherson, Smith-Lovin, & Brashears, 2006). Social isolation has been linked to broad-based morbidity and mortality (House, Landis, & Umberson, 1988), but perceived social isolation (i.e., loneliness) has received less attention. Our results show that loneliness, not social network size, predicts changes in SBP. Moreover, independent of social network size, age, gender, race/ethnicity, traditional cardiovascular risk factors (BMI, poor health behaviors), cardiovascular medications, chronic health conditions, and a set of related psychosocial variables (depressive symptoms, perceived stress, social support, hostility), loneliness appears to be a unique risk factor for elevated SBP and increases in SBP over time.
Acknowledgments
This research was supported by Grant R01-AG036433-01 and R01-AG034052 from the National Institute on Aging, and by the John Templeton Foundation.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/pag
Parallel models that treated Year 2 or Year 3 loneliness as the initial measurement point rendered comparable results to those reported here, albeit with reduced statistical power and potentially different values on all initial time-varying covariates. Because the longer-lagged effect of Year 1 loneliness on SBP is estimated three times, it is more reliable than the estimates for the longer-lagged effects of Year 2 or Year 3 loneliness (which are estimated only twice and once, respectively).
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience-cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Science USA. 2006;103(45):17058–17063. doi: 10.1073/pnas.0605053103. PMCID: PMC1636578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell IR, Martino GM, Meredit KE, Schwartz GE, Siani MM, Morrow FD. Vascular disease risk factors, urinary free cortisol, and health histories in older adults: Shyness and gender interactions. Biological Psychology. 1993;35:37–49. doi: 10.1016/0301-0511(93)90090-u. [DOI] [PubMed] [Google Scholar]
- Berkman LF. Ph.D. dissertation. Berkeley: University of California; 1977. Social networks, host resistance and mortality: A follow-up study of Alameda County residents. [Google Scholar]
- Booth R. Loneliness as a component of psychiatric disorders. Medscape General Medicine. 2000;2(2):1–7. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological Methods Research. 1992;21(2):230–258. [Google Scholar]
- Cacioppo JT, Hawkley LC. Perceived social isolation and cognition. Trends in Cognitive Science. 2009 doi: 10.1016/j.tics.2009.06.005. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Berntson GG, Ernst JM, Gibbs AC, Stickgold R, et al. Do lonely days invade the nights? Potential social modulation of sleep efficiency. Psychological Science. 2002;13(4):384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Crawford LE, Ernst JM, Burleson MH, Kowalewski RB, et al. Loneliness and health: Potential mechanisms. Psychosomatic Medicine. 2002;64(3):407–417. doi: 10.1097/00006842-200205000-00005. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Hawkley LC, Ernst JM, Burleson M, Berntson GG, Nouriani B, Spiegel D. Loneliness within a nomological net: An evolutionary perspective. Journal of Research in Personality. 2006;40(6):1054–1085. [Google Scholar]
- Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA. Loneliness as a specific risk factor for depressive symptoms: Cross-sectional and longitudinal analyses. Psychology and Aging. 2006;21(1):140–151. doi: 10.1037/0882-7974.21.1.140. [DOI] [PubMed] [Google Scholar]
- Cacioppo JT, Patrick B. Loneliness: Human nature and the need for social connection. New York: W. W. Norton & Company; 2008. [Google Scholar]
- Casper LM, Bianchi SM. Continuity & Change in the American Family. Thousand Oaks, Calif.: Sage Publications; 2002. [Google Scholar]
- Caspi A, Harrington H, Moffitt TE, Milne BJ, Poulton R. Socially isolated children 20 years later: Risk of cardiovascular disease. Archives of Pediatrics and Adolescent Medicine. 2006;160(8):805–811. doi: 10.1001/archpedi.160.8.805. [DOI] [PubMed] [Google Scholar]
- Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: Development and validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Cheng S-T. Loneliness-distress and physician utilization in well-elderly females. Journal of Community Psychology. 1992;20(1):43–56. [Google Scholar]
- Chobanian A, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 Report. Journal of the American Medical Association. 2003;289:2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed]
- Cohen S. Basic psychometrics for the ISEL 12-item scale. [Retrieved September 2, 2008];2008 from http://www.psy.cmu.edu/~scohen/ [Google Scholar]
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health: Claremont symposium on applied social psychology; Sage; Newbury Park, CA. 1988. [Google Scholar]
- Cole SW, Hawkley LC, Arevalo JM, Sung CY, Rose RM, Cacioppo JT. Social regulation of gene expression in human leukocytes. Genome Biology. 2007;8(9):R189.181–R189.113. doi: 10.1186/gb-2007-8-9-r189. PMCID: PMC2375027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook WW, Medley DM. Proposed hostility and pharisaic-virtue scales for the MMPI. Applied Psychology. 1954;38(6):414–418. [Google Scholar]
- Curran PJ. A latent curve framework for the study of developmental trajectories in adolescent substance use. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Mahwah, NJ: Lawrence Erlbaum Associates; 2000. pp. 1–4. [Google Scholar]
- de Jong Gierveld J, van Tilburg T. Living arrangements of older adults in the Netherlands and Italy: Coresidence values and behaviour and their consequences for loneliness. Journal of Cross-Cultural Gerontology. 1999;14(1):1–24. doi: 10.1023/a:1006600825693. [DOI] [PubMed] [Google Scholar]
- Diez Roux AV, Chambless L, Merkin SS, Arnett D, Eigenbrodt M, Nieto FJ, et al. Socioeconomic disadvantage and change in blood pressure associated with aging. Circulation. 2002;106(6):703–710. doi: 10.1161/01.cir.0000025402.84600.cd. [DOI] [PubMed] [Google Scholar]
- Franklin SS, Gustin WI, Wong ND, Larson MG, Weber MA, Kannel WB, Levy D. Hemodynamic patterns of age-related changes in blood pressure: The Framingham heart study. Circulation. 1997;96(1):308–315. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- Geller J, Janson P, McGovern E, Valdini A. Loneliness as a predictor of hospital emergency department use. Journal of Family Practice. 1999;48(10):801–804. [PubMed] [Google Scholar]
- Goldstein IB, Shapiro D, Guthrie D. A 5-year follow-up of ambulatory blood pressure in healthy older adults. American Journal of Hypertension. 2003;16(8):640–645. doi: 10.1016/s0895-7061(03)00906-3. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Burleson MH, Berntson GG, Cacioppo JT. Loneliness in everyday life: Cardiovascular activity, psychosocial context, and health behaviors. Journal of Personality and Social Psychology. 2003;85(1):105–120. doi: 10.1037/0022-3514.85.1.105. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Cacioppo JT. Aging and loneliness: Downhill quickly? Current Directions in Psychological Science. 2007;16(4):187–191. [Google Scholar]
- Hawkley LC, Hughes ME, Waite LJ, Masi CM, Thisted RA, Cacioppo JT. From social structure factors to perceptions of relationship quality and loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology: Social Sciences. 2008;63B:S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley LC, Masi CM, Berry JD, Cacioppo JT. Loneliness is a unique predictor of age-related differences in systolic blood pressure. Psychology and Aging. 2006;21(1):152–164. doi: 10.1037/0882-7974.21.1.152. [DOI] [PubMed] [Google Scholar]
- Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts reduced physical activity: Cross-sectional and longitudinal analyses. Health Psychology. 2009;28:354–363. doi: 10.1037/a0014400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heikkinen R-L, Kauppinen M. Depressive symptoms in late life: A 10-year follow-up. Archives of Gerontology and Geriatrics. 2004;38(3):239–250. doi: 10.1016/j.archger.2003.10.004. [DOI] [PubMed] [Google Scholar]
- House JS, Landis KR, Umberson D. Social relationships and health. Science. 1988;241(4865):540–545. doi: 10.1126/science.3399889. [DOI] [PubMed] [Google Scholar]
- Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1. [Google Scholar]
- Hughes ME, O'Rand AM. The Lives and Times of the Baby Boomers. New York and Washington, DC: Russell Sage Foundation and Population Reference Bureau; 2004. [Google Scholar]
- Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Ricker D, George J, Messick G, Speicher CE, Garner W, et al. Urinary cortisol levels, cellular immunocompetency, and loneliness in psychiatric inpatients. Psychosomatic Medicine. 1984;46(1):15–23. doi: 10.1097/00006842-198401000-00004. [DOI] [PubMed] [Google Scholar]
- Kudielka BM, Hawkley LC, Adam EK, Cacioppo JT. Compliance with ambulatory saliva sampling in the Chicago Health, Aging, and Social Relations Study and associations with social support. Annals of Behavioral Medicine. 2007;34:209–216. doi: 10.1007/BF02872675. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Lloyd-Jones D, et al. Heart disease and stroke statistics 2009 update: A report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2009;119:e21–e181. doi: 10.1161/CIRCULATIONAHA.108.191261. [DOI] [PubMed] [Google Scholar]
- MacCallum RC, Browne MW, Sugawara HM. Power analysis and determination of sample size for covariance structure modeling. Psychological Methods. 1996;1(2):130–149. [Google Scholar]
- McPherson M, Smith-Lovin L, Brashears ME. Social isolation in America: Changes in core discussion networks over two decades. American Sociological Review. 2006;71:353–375. [Google Scholar]
- McPhillips JB, Pellettera KM, Barrett-Connor E, Wingard DL, Criqui MH. Exercise patterns in a population of older adults. American Journal of Preventive Medicine. 1989;5(2):65–72. [PubMed] [Google Scholar]
- Masi CM, Chen H-Y, Hawkley LC, Cacioppo JT. A meta-analysis of interventions to reduce loneliness. doi: 10.1177/1088868310377394. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen B, Muthen L. Mplus: The comprehensive modeling program for applied researchers. Los Angeles: Muthen & Muthen; 2002. [Google Scholar]
- Orth-Gomer K, Albus C, Bages N, DeBacker G, Deter HC, Herrmann-Lingen C, et al. Psychosocial considerations in the European guidelines for prevention of cardiovascular diseases in clinical practice: Third joint task force. International Journal of Behavioral Medicine. 2005;12(3):132–141. doi: 10.1207/s15327558ijbm1203_2. [DOI] [PubMed] [Google Scholar]
- Penninx BW, van Tilburg T, Kriegsman DM, Deeg DJ, Boeke AJ, van Eijk JT. Effects of social support and personal coping resources on mortality in older age: The Longitudinal Aging Study Amsterdam. American Journal of Epidemiology. 1997;146(6):510–519. doi: 10.1093/oxfordjournals.aje.a009305. [DOI] [PubMed] [Google Scholar]
- Peplau LA, Perlman D. Loneliness: A Sourcebook of Current Theory, Research, and Therapy. New York: Wiley; 1982. [Google Scholar]
- Pinquart M, Sőrensen S. Risk factors for loneliness in adulthood and old age - a meta-analysis. 2003;Vol. 19:111–143. In. [Google Scholar]
- Pressman SD, Cohen S, Miller GE, Barkin A, Rabin BS, Treanor JJ. Loneliness, social network size, and immune response to influenza vaccination in college freshmen. Health Psychology. 2005;24(3):297–306. doi: 10.1037/0278-6133.24.3.297. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- Roberts BW, Walton KE, Viechtbauer W. Patterns of mean-level change in personality traits across the life course: A meta-analysis of longitudinal studies. Psychological Bulletin. 2006;132:3–27. doi: 10.1037/0033-2909.132.1.1. [DOI] [PubMed] [Google Scholar]
- Rosengren A, Hawken S, Ôunpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): Case-control study. The Lancet. 2004;364(9438):953–962. doi: 10.1016/S0140-6736(04)17019-0. [DOI] [PubMed] [Google Scholar]
- Rozanski A, Blumenthal JA, Kaplan J. Impact of psychological factors on the pathogenesis of cardiovascular disease and implications for therapy. Circulation. 1999;99(16):2192–2217. doi: 10.1161/01.cir.99.16.2192. [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, Cutrona CE. The revised UCLA loneliness scale: Concurrent and discriminant validity evidence. Journal of Personality and Social Psychology. 1980;39(3):472–480. doi: 10.1037//0022-3514.39.3.472. [DOI] [PubMed] [Google Scholar]
- Russell DW, Cutrona CE, de la Mora A, Wallace RB. Loneliness and nursing home admission among rural older adults. Psychology and Aging. 1997;12(4):574–589. doi: 10.1037//0882-7974.12.4.574. [DOI] [PubMed] [Google Scholar]
- Steffick DE. Documentation on affective functioning measures in the Health and Retirement Study. Ann Arbor: University of Michigan, Survey Research Center; 2000. [Google Scholar]
- Steptoe A. Psychosocial factors in the development of hypertension. Annals of Medicine. 2000;32(5):371–375. doi: 10.3109/07853890008995940. [DOI] [PubMed] [Google Scholar]
- Steptoe A, Owen N, Kunz-Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle-aged men and women. Psychoneuroendocrinology. 2004;29(5):593–611. doi: 10.1016/S0306-4530(03)00086-6. [DOI] [PubMed] [Google Scholar]
- Victor CR, Scambler SJ, Bowling ANN, Bond J. The prevalence of, and risk factors for, loneliness in later life: A survey of older people in Great Britain. Ageing & Society. 2005;25(06):357–375. [Google Scholar]
- Weiss RS. Loneliness: The experience of emotional and social isolation. Cambridge, MA: MIT Press; 1973. [Google Scholar]
- Whelton PK. Epidemiology of hypertension. Lancet. 1994;344(8915):101–106. doi: 10.1016/s0140-6736(94)91285-8. [DOI] [PubMed] [Google Scholar]
- Wilson RS, Krueger KR, Arnold SE, Schneider JA, Kelly JF, Barnes LL, et al. Loneliness and risk of Alzheimer disease. Archives of General Psychiatry. 2007;64(2):234–240. doi: 10.1001/archpsyc.64.2.234. [DOI] [PubMed] [Google Scholar]