Abstract
Objective
Social cognitive models have been used to explain health risk behaviors such as sexual transmission risk behavior (TRB) in a variety of populations, including people with HIV. However, these models generally do not account for the influence of clinically significant psychological problems. Clinical depression is one of the most common comorbid conditions in HIV, and it may affect the ability of social cognitive models to predict TRB.
Design
The current study examined whether a social cognitive model would explain risk of sexual TRB in sexually active HIV-infected men who have sex with men MSM who meet or do not meet screening criteria for major depression.
Main Outcome Measures
Participants (n=403) completed self-report assessments of negative expectancy, social models, and self-efficacy related to condom use, as well as recent sexual TRB and a screening measure for major depression. We used path analysis to examine whether condom use self-efficacy mediated associations between expectancies about condom use and social models of condom use, and recent sexual TRB. Multiple group modeling was conducted to compare the fit of this model in participants who met (n=47) or did not meet (n=356) screening criteria for major depression.
Results
The final multiple group model fit the data well (χ2(36)=30.55, p=.73; CFI=1.00; RMSEA<.01; SRMR=.05). Results indicated that among MSM who screened negative for depression, low condom use self-efficacy explained indirect pathways from negative expectancy about condom use and poor social models for condom use to greater sexual TRB. In contrast, among MSM who screened positive for depression, condom use self-efficacy did not mediate any pathways from risk factors to sexual TRB and was not directly associated with sexual TRB. In this group, only negative expectancy about condom use was associated with greater sexual TRB.
Conclusion
Models of health risk behaviors, including sexual TRB, may not generalize to HIV-infected individuals with a clinical depression. Risk reduction interventions based on these models should account for comorbid mental health conditions to maximize their effectiveness.
Keywords: HIV, secondary prevention, depression, men who have sex with men (MSM)
INTRODUCTION
With the advent of highly active antiretroviral therapy (HAART), HIV-infected individuals who have adequate resources for treatment are now living with a chronic versus a terminal illness. Because new infections have continued at steady or even increasing rates (Center for Disease Control [CDC], 2007), there is a large and growing population of individuals living with HIV in the U.S. and elsewhere. In the absence of a vaccine or cure, reductions in sexual and other HIV transmission risk behaviors (TRB) are the only known ways to reduce HIV transmission. Accordingly, explanatory models of, and interventions for, HIV transmission risk behavior in individuals with HIV are needed. Men who have sex with men (MSM) are the largest risk group with HIV in the United States (CDC, 2007), and for this group the predominant TRB is sex without condoms.
Most models of HIV sexual transmission risk behavior in HIV are based upon social / health psychology theories to predict whether or not individuals will use condoms when having sex. These models include the Theory of Reasoned Action, with attitudes and intentions as key factors (e.g. Azjen & Fishbein, 1980; Albarracin, Johnson, Fishbein, & Muellerliele, 2001), the AIDS Risk Reduction Model, emphasizing behavior change stages of labeling, commitment, and enactment (Catania, Kegeles, & Coates, 1990; Catania, Coates, & Kegeles, 1994), the Information, Motivation, Behavior model (IMB, Fisher & Fisher, 1992), and Social Cognitive Theory, with self-efficacy being a central factor (e.g. Bandura, 1994; Wulfert, Safren, Brown, & Wan, 1999; Wulfert & Wan, 1995). Each of these models, to greater or lesser extents emphasizes the cognitive pathways involved in behavior change. The ARRM model above, however also, allows for a consideration of affective components (condom enjoyment) and sexual communication skills, in addition to purely cognitive constructs to explicate the pathways to sexual risk (Catania, Coates, & Kegeles, 1994).
Social Cognitive Theory is one of the most widely used models of sexual transmission risk behaviors. In brief, this model posits that individuals go through a cognitive process weighing the pros and cons of practicing safer sex (e.g. considering knowledge about HIV, expectancies related to using condoms, and social norms) which influences an individual’s self-efficacy (i.e. confidence in one’s ability to practice safer-sex in difficult situations). Self-efficacy, in turn, then becomes a key factor in determining whether or not one will practice safer sex. Self efficacy models of HIV transmission risk behavior have been successfully tested in a variety of risk groups for sexual acquisition of HIV, including heterosexually active adults (e.g. Wulfert & Wan, 1993), gay men (e.g. Wulfert, Wan, & Backus, 1996), and HIV-infected individuals (e.g. Wulfert et al., 1999).
Based on health psychology models of sexual risk taking, several studies have examined the efficacy of interventions to reduce sexual transmission risk behaviors in individuals with HIV, and have generally seen modest results. Crepaz & Marks (2001) conducted a meta-analysis of the existing 12 studies at the time and although there was, overall, a significant effect across studies, 7 of the 12 did not see a significant effect. Some of the factors associated with stronger effects were those based on a behavioral theory, those that were more intensively delivered, those that promoted and provided skills building, and those that addressed a myriad of issues related to mental health, medication adherence, and HIV risk behavior. Generally, these studies did not assess comorbid depression in the samples, nor did they examine whether clinical depression served as a moderator in outcomes.
Clinical depression is one of the most common comorbid diagnoses in HIV, with prevalence rates up to 37% (e.g. Asch et al., 2003, Atkinson & Grant, 1994; Bing et al., 2007; Dew et al., 1997). In comparison, the most recent U.S. National Comorbidity Study (NCS) estimates only 6.6% for 12 months before the interview in the general population (Kessler, Merikangas, & Wang, 2007). One potential shortcoming of models of health behaviors in general and HIV transmission risk behaviors in HIV-infected individuals in particular, is that generally they do not account for depression. Depression, conceptually, could be associated with almost all of the theorized predictors in various models of HIV transmission risk behavior, and social cognitive models in particular. Cognitive models of depression suggest that individuals with depression are negatively biased in terms of their thoughts and beliefs (A. Beck, 1972; J. Beck, 1995). Accordingly, individuals with depression have a negative view of one’s self, the world, and the future. This could result in more negative views about perceived social models regarding condom use, the degree of difficulty involved in barriers to condom use, as well as perceived benefits. Finally, it could result in having worse self-efficacy, regardless of the other predictors of self-efficacy.
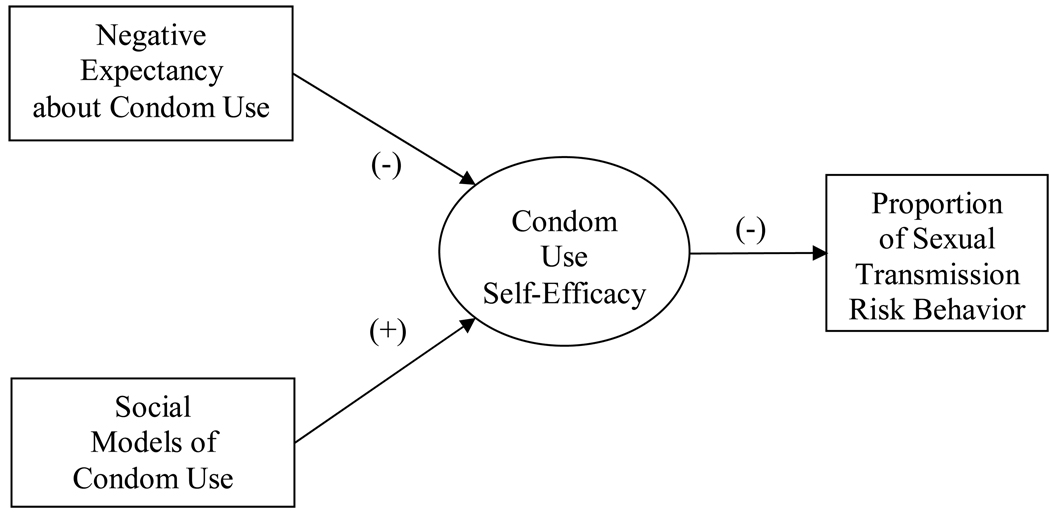
The present study therefore sought to examine the role of depression within the context of a self-efficacy model to predict TRB in MSM with HIV. Following a prior self-efficacy model tested with an HIV-infected sample (e.g. Wulfert et al., 1999), we expected that among MSM without depression, lower condom use self-efficacy would mediate pathways from greater negative expectancy about condom use and poorer social models of condom use, to greater proportions of sexual TRB (see Figure 1). We hypothesized, however, that the magnitude of these associations would be significantly weaker among those who were depressed.
Figure 1.
Proposed model of sexual transmission risk behavior in HIV-infected MSM.
Rectangles represent observed variables. Oval represents the condom use self-efficacy latent variable.
METHODS
Participants and Procedure
The current sample was comprised of 403 sexually active, HIV-infected MSM who received primary care at Fenway Community Health (FCH), the largest ambulatory HIV care provider in New England. Participants were screened for enrollment in one of two parallel secondary HIV behavioral interventions at FCH between 2004 and 2007, which were intended to increase safer sex practices with sexual partners of HIV-uninfected or unknown status (Knauz et al. 2007). Inclusion criteria for screening were men who 1) were HIV-infected, 2) received primary health care at Fenway Community Health, 3) identified as a man who has sex with men. Exclusion criteria were 1) inability to complete informed consent process (e.g. substantial cognitive impairment), and 2) plans to relocate over the upcoming year. All participants (N=503) completed a computer-assisted, extensive psycho-social questionnaire that inquired about their demographic characteristics, mental health, and sexual practices, including condom use and psychosocial correlates of condom use. Consistent with prior research modeling safer sexual behaviors (Wulfert et al., 1999), only individuals who were currently sexually active as defined by having any male sex partners over the past 3 months (n=408) were included in the current analyses. Of these participants, 5 were excluded due to missing data on major depression screening, our main grouping variable, making the final sample 403.
Measures
Sexual transmission risk behavior
Participants were asked to identify the number of times they engaged in receptive or insertive anal intercourse with partners of negative or unknown HIV status during the prior 3 months, and the number of times a condom was used. The primary outcome of this study was the proportion of total instances in which a condom was not used. Higher values reflected a greater proportion of sexual TRB. These are standard HIV transmission risk behavior questions used in HIV prevention research with HIV-infected patients (Morin, Myers, Shade, Koester, Maiorana & Dawson Rose, 2007).
Social Cognitive Variables
Variables related to social-cognitive theory were taken from prior work modeling TRB in HIV-infected individuals (Wulfert et al., 1999). This is because we sought to first replicate prior work with HIV-infected individuals using this model, and secondly sought to examine the degree to which the model worked for both those who screened in for depression and those who did not. Accordingly, condom use self-efficacy (SE) was measured using 4 items ranging from 1 (very unsure) to 5 (very sure), including SE1: ‘How sure are you that you will always use condoms for intercourse in the next 3 months?’; SE2: ‘How sure are you that you will plan to always have a condom available for intercourse in the next 3 months?’; SE3: ‘How sure are you that you will use condoms every time you have intercourse in the next 3 months?”; and SE4: ‘How sure are you that you could resist intercourse unless your partner agreed to using a condom in the next 3 months?’ Two of the items therefore reflected participants’ confidence to actually use a condom during intercourse, one assessed the converse of confidence to resist unprotected intercourse, and one asked about the participants’ self-efficacy to access condoms in anticipation of intercourse, irrespective of intentions to use condoms.
Negative expectations about condom use was measured by one item (‘Condoms make sex less enjoyable’). This item was measured on a 5-point scale from 1 (disagree) to 5 (agree), with higher scores indicating greater negative expectancy. A single item assessed the perceived frequency with which close friends are always using condoms as an indicator of social models of condom use. Responses ranged from 1 (none of them) to 5 (all of them), with higher scores reflecting better social models for condom use.
Depression
The nine-item Depression Severity Scale of the Patient Health Questionnaire (PHQ; Spitzer et al., 1999) was used to screen participants for major depression. This self-report instrument assesses the severity of diagnostic symptoms of depression during the past two weeks. PHQ response criteria were used to group participants by depression status (i.e. 0=negative screen, 1=positive screen). The PHQ has demonstrated relatively good reliability with diagnosis of independent mental health professionals (kappa = 0.65; overall accuracy, 85%; sensitivity, 75%; specificity, 90%) (Spitzer et al., 1999).
Data analyses
The self-efficacy model of sexual TRB was evaluated using structural equation modeling techniques in Mplus (version 4.21; Muthen & Muthen, 1998–2007). Parameters were estimated using the full information maximum likelihood (FIML) approach, which generates unbiased estimates under the assumption of missing at random (Schafer & Graham, 2002). The percentage of missing data across all psychosocial and behavioral model variables ranged from .5% to 6.7%.
Based on current recommendations, overall model fit was evaluated based on multiple indices: chi-square (χ2) statistic, comparative fit index (CFI), root mean square error of approximation (RMSEA), and standardized root mean squared residual (SRMR). Good fit (χ2 pvalue>.05; CFI>.95; RMSEA<.06; and SRMR<.08; Hu & Bentler, 1999) was used to justify interpretation of parameters.
In the hypothesized model of sexual TRB (see Figure 1), all model variables except condom use self-efficacy were tested as observed variables. Condom use self-efficacy was tested as a latent variable with four indicators (SE1–SE4). Using a general two-step procedure (Anderson & Gerbing, 1988), we evaluated the measurement model of condom use self-efficacy prior to including it in the structural model of sexual TRB. The structural model was then tested using a multiple group framework to determine whether major depression screening status (i.e. depression-positive versus depression-negative) moderated relationships between predictors and sexual TRB. Multiple group modeling allowed for the estimation of parameters for each group simultaneously as well as the evaluation of overall model fit.
RESULTS
Demographic, psychosocial and behavioral characteristics
Participants were approximately 42 years of age (SD=8 years) and were primarily Caucasian (77%). Although more than half of the sample (54%) had obtained a college degree, over half (53%) reported an annual income of $40,000 or less. See Table 1 for a summary of sample demographic characteristics.
Table 1.
Sample demographic characteristics (N=403).
| Variable | Mean (SD) or Frequency (%) |
|---|---|
| Age (years) | 41.6 (8.2) |
| Race/Ethnicity | |
| Caucasian | 313 (76.7) |
| Black/African American | 41 (10.0) |
| Hispanic/Latino | 34 (8.3) |
| Other | 20 (5.0) |
| Education | |
| Less than college degree | 186 (45.6) |
| College degree | 222 (54.4) |
| Annual income ($) | |
| ≤ 20,000 | 125 (31.0) |
| 20,001 – 40,000 | 90 (22.3) |
| 40,001 – 60,000 | 70 (17.4) |
| > 60,000 | 118 (29.3) |
In this sample of sexually active HIV-infected MSM (N=403), 12% met screening criteria for major depression. The depressed group reported significantly lower scores on three of four indicators of condom use self-efficacy relative to those who were not depressed (p’s<.05). The depression-positive group also reported marginally higher proportions of recent sexual TRB (M depression positive=.42[SD=.43]; depression-negative=.31[SD=.41]; p=.09). The two groups did not differ statistically on negative expectancy or social models of condom use. Descriptive statistics of all self-efficacy model variables for the total sample and separately by depression status are reported in Table 2. Bivariate correlations between variables are reported in Table 3.
Table 2.
Descriptive statistics for self-efficacy model variables (N=403).
| Variable | Total Sample | Depression- negative |
Depression-positive | ||||
|---|---|---|---|---|---|---|---|
| M(SD) | Range | M(SD) | Range | M(SD) | Range | ||
| 1. | Negative expectancy about condom use |
3.6 (1.4) | 1–5 | 3.6 (1.4) | 1–5 | 3.9 (1.4) | 1–5 |
| 2. | Social models for condom use |
3.1 (1.1) | 1–5 | 3.2 (1.1) | 1–5 | 3.0 (1.1) | 1–5 |
| 3. | Self-efficacy 1: Will always use condoms for intercourse in next 3 mos. |
3.5 (1.8) | 1–5 | 3.5 (1.7) | 1–5 | *3.0 (1.9) | 1–5 |
| 4. | Self-efficacy 2: Will plan to always have condom available for intercourse in next 3 mos. |
4.1 (1.5) | 1–5 | 4.1 (1.5) | 1–5 | 3.8 (1.6) | 1–5 |
| 5. | Self-efficacy 3: Will use condoms every time I have intercourse in next 3 mos. |
3.5 (1.7) | 1–5 | 3.5 (1.8) | 1–5 | *3.0 (1.9) | 1–5 |
| 6. | Self-efficacy 4: Could resist intercourse unless partner agreed to use condom in next 3 mos. |
3.3 (1.8) | 1–5 | 3.6 (1.7) | 1–5 |
**2.6 (1.7) |
1–5 |
| 7. | Proportion of sexual TRB in past 3 mos. |
32.7 (41.6) |
0– 100a |
31.2 (41.2) |
0– 100a |
ŧ42.0 (42.8) |
0–100a |
Interquartile ranges (IQRs): Total sample (0–75.0); Depression-negative group (0–75.0); Depression-positive group (0–81.3).
Mean differences between the depression-negative and -positive groups were tested for significance using independent samples t tests;
p<.10;
p<.05;
p<.01.
Table 3.
Bivariate correlations between self-efficacy model variables (n=403).
| 1 | 2 | 3 | 4 | 5 | 6 | ||
|---|---|---|---|---|---|---|---|
| 1. | Negative expectancy about condom use |
||||||
| 2. | Social models for condom use | **−.22 | |||||
| 3. | Self-efficacy 1: Will always use condoms for intercourse in next 3 mos. |
**−.35 | **.31 | ||||
| 4. | Self-efficacy 2: Will plan to always have condom available for intercourse in next 3 mos. |
**−.26 | **.17 | **.57 | |||
| 5. | Self-efficacy 3: Will use condoms every time I have intercourse in next 3 mos. |
**−.38 | **.34 | **.81 | **.59 | ||
| 6. | Self-efficacy 4: Could resist intercourse unless partner agreed to use condom in next 3 mos. |
**−.36 | **.28 | **.69 | **.48 | **.73 | |
| 7. | Proportion of sexual TRB in past 3 mos. |
**.30 | **−.20 | **−.32 | **−.23 | **−.38 | **−.33 |
p<.01.
Measurement model of condom use self-efficacy
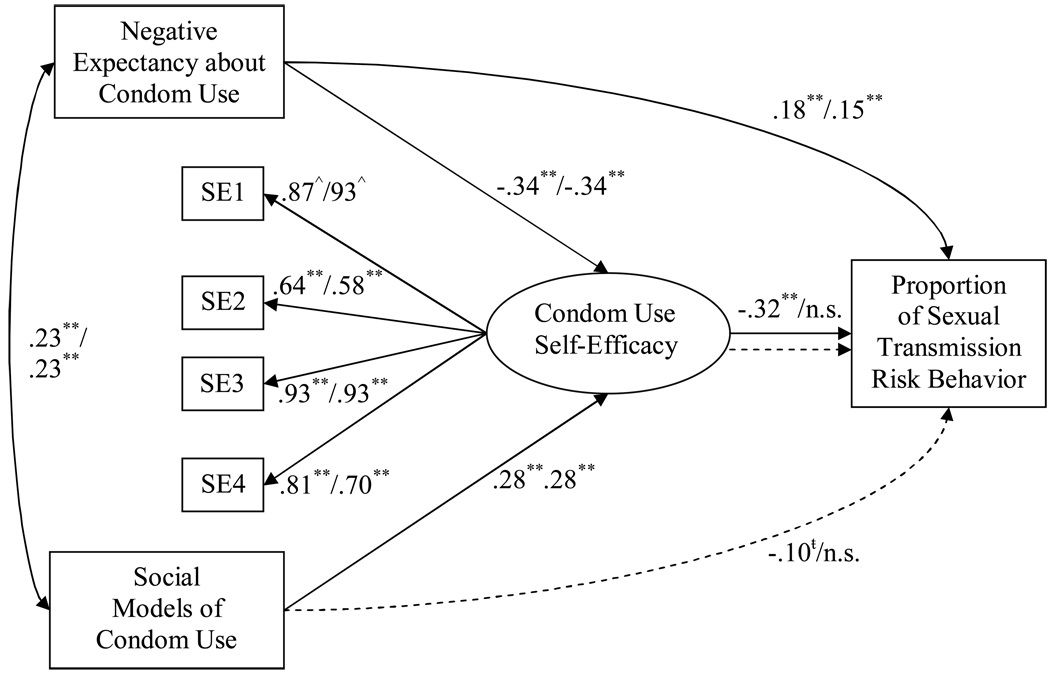
The four indicators of condom use self-efficacy (SE1–SE4) were combined into a self-efficacy latent variable. In preliminary analyses, this variable and all other observed variables in the proposed model (negative expectancy about condom use, social models of condom use, and proportion of sexual TRB) were allowed to freely correlate. This model fit the data (χ2(11)=8.88, p=.63; CFI=1.00; RMSEA<.01; SRMR=.02). Standardized factor loadings for the self-efficacy latent variable are identified in Figure 2. Moderate correlations among all model variables (r’s=.21–.40, p’s<.01) indicated support for testing the hypothesized direct paths.
Figure 2.
Standardized parameter estimates in the final model of sexual transmission risk behavior in HIV-infected MSM by major depression screening status (negative/positive).
Oval represents the condom use self-efficacy latent factor. Small rectangles SE1–SE4 represent observed indicators of the latent factor. Path values represent standardized coefficients for participants who [did not meet/met] screening criteria for major depression.
To maintain presentation clarity, residual terms are not shown.
ŧp<.10; *p<.05; **p<.01; ^fixed to 1 to set metric for latent variable
Model fit statistics: χ 2(36)=30.55, p=.73; CFI=1.00; RMSEA<.01; SRMR=.05.
R2 for the latent factor was 23.5% in both groups. R2 for proportion of sexual transmission risk behavior was 20.3% in the depression-negative group and 7.5% in the depression-positive group.
Structural model of sexual TRB
Per-above, a previously tested model of HIV TRB (Wulfert et al., 1999) was used as a base for testing paths from social cognitive variables to sexual TRB. The current model included direct paths from negative expectancy about condom use and social models of condom use to condom use self-efficacy and from condom use self-efficacy to proportion of sexual TRB (see Figure 1). The addition of direct paths from negative expectancy and social models of condom use to proportion of sexual TRB was also assessed in order to determine the extent to which the associations between these two predictors and proportion of sexual TRB could be explained by direct versus indirect (i.e. self-efficacy-mediated) mechanisms.
Test of moderation by major depression screening status
Modeling was conducted in a multiple group framework to test the hypothesis that direct paths would be weaker in the depression-positive group relative to the depression-negative group. We began with the assumption that model parameters were equal across the two groups. This restrictive model demonstrated relatively good fit (χ2(44)=62.62, p=.03; CFI=.98; RMSEA=.05; SRMR=.06). The model was then used as a baseline to test nested models in which sets of parameters were freed to vary across the two groups. At each step, the χ2difference was evaluated. A significant improvement in model fit (i.e. a significant χ2 difference) would indicate that the parameter values varied significantly by depression status. For non-significant changes in the χ2 value, the parameter values were determined to be statistically equal across groups and the equality constraints were retained in the final model. Figure 2 presents the final model with standardized path coefficients for each pathway, and unstandardized coefficients and z scores are presented in the text below.
Among direct path coefficients, the paths from more negative expectancy (Unstandardized Beta=.37, z=6.94) and poorer social models of condom use (Unstandardized Beta=−.40, z=−5.62) to lower condom use self-efficacy were significant and statistically equal across groups. In contrast, the association between lower condom use self-efficacy and greater proportion of sexual TRB was significant in the depression-negative group (Unstandardized Beta=−8.47, z=−5.38) but nonsignificant in the depression-positive group (Unstandardized Beta=−4.89, z=−1.28).
Additional steps indicated that the addition of direct paths from both negative expectancy and social models of condom use to proportion of sexual TRB improved model fit. The direct path from more negative expectancy to greater proportion of sexual TRB was significant and statistically equal across groups (Unstandardized Beta=4.23, z=2.93). In contrast, the direct path from poorer social models of condom use to greater proportion of sexual TRB was significantly different across groups, such that it was marginally significant in the depression-negative group (Unstandardized Beta=−3.93, z=−1.95) and nonsignificant in the depression-positive group (Unstandardized Beta=7.54, z=1.33). Findings also demonstrated that all four factors loadings for the condom use self-efficacy latent variable were significant and statistically equal across groups, suggesting a homogenous construct across groups (see Figure 2 for standardized values of factor loadings).
The final model fit the data (χ2(36)=30.55, p=.73; CFI=1.00; RMSEA<.01; SRMR=.05). This model explained 23.5% of the variance in condom use self-efficacy in both groups. The model also explained a larger percentage of variance in proportion of sexual TRB for the depression-negative group (20.3%) relative to the depression-positive group (7.5%).
Final model of sexual TRB
Depression-negative group
In the depression-negative group (see Figure 2 for standardized direct path coefficients), lower condom use self-efficacy explained significant indirect paths from more negative expectancy (Unstandardized Beta=3.11, z=4.31) and poorer social models (Unstandardized Beta=−3.35, z=−3.96) to greater proportion of sexual TRB. More negative expectancy was also directly associated with greater proportion of sexual TRB, whereas the direct association between poorer social models and greater proportion of sexual TRB was marginally significant. This pattern of findings supports that among those who screened negative for major depression, associations of negative expectancy and social models of condom use with sexual TRB reflected both direct and indirect (via self-efficacy) mechanisms.
Depression-positive group
In the depression-positive, more negative expectancy about condom use was directly associated with greater proportion of sexual TRB. However, social models of condom use and condom use self-efficacy did not significantly predict sexual TRB. This pattern of findings supports the hypothesis that among those who screened positive for major depression, 1) condom use self-efficacy did not account for the association between more negative expectancy about condom use and greater proportion of sexual TRB, and 2) social models of condom use were not directly or indirectly (via self-efficacy) associated with sexual TRB.
DISCUSSION
This study found that constructs from the Social Cognitive Theory, one of the most frequently used models of sexual TRB for HIV, were particularly useful for explaining pathways to HIV sexual transmission risk behavior in HIV-infected MSM who did not screen in for major depression, but was not useful for explaining pathways to sexual transmission risk behavior in the HIV-infected MSM who did screen in for major depression. Clinically significant symptoms of depression, including persistent sadness and/or loss of interest, worthless feelings, loss of energy, concentration problems, can arguably interfere with the process of making social cognitive judgments, such as self-efficacy perceptions, and could therefore interfere with the ability of important social-cognitive variables to predict health behaviors such as HIV TRB. Because clinical depression is one of the most common conditions comorbid with HIV, models of health behaviors and interventions that are based on such models should address the role of depression to potentially boost their utility. Potentially, this could occur through including screening or referral for medications and/or treatment of depression into the intervention, as has been done for another self-care behavior in HIV, adherence (Safren et al., 2009).
While in some studies symptoms of depression have been shown to be associated with HIV TRB (e.g. Koblin et al., 2006; Stall et al., 2003), this association has not been consistent (Crepaz & Marks, 2001). This may be because those with higher, potentially clinically significant depression may experience loss of interest in sex, a common symptom of depression, and so the association between depression and sexual risk may be curvilinear (see Kalichman &. Weinhardt, 2001). The present study found that those with depression had lower self-efficacy scores across three of the four items assessing self-efficacy, and had a trend toward higher TRB. While the association of depression to sexual risk behavior is worthy of future study, the findings of this analysis are important regardless of the strength or pattern of the direct association of depression to sexual transmission risk behavior. Even if those with depression have similar levels of sexual risk taking as those without depression, depression may moderate the utility of social/health psychology models of sexual risk taking. This finding coupled with data showing that depression is highly comorbid with HIV, points to the need to address depression directly in models and corresponding interventions. Models of behavior change emphasizing Social Cognitive Theory constructs such as self-efficacy models, health beliefs models or Theory of Reasoned Action emphasize cognitive events and appraisals when accounting for the pathways influencing behavior. It is plausible that depression-related behavioral withdrawal and the other neuro-vegetative symptoms of depression (e.g., disturbances of sleep, appetite, concentration, and energy) may overwhelm predominantly cognitive models when attempting to account for HIV transmission risk behavior among men with clinical depression. These models may well be successfully augmented by the specification of behavioral pathways relevant for depression (e.g., avoidant coping or substance use). The success of the ARRM model in accounting for condom use, for example, may well be that is allows for a consideration of both behavioral and affective components (Catania, Coates, & Kegeles, 1994). More recently, this model has been expanded, in the presence of childhood sexual abuse, to accommodate coping and skill set to explain the pathways from childhood sexual abuse to adult sexual risk among MSM (Catania, Paul, Osmond, et al., 2008). Alternatively, cognitive models of depression emphasize strong core cognitions such as negative beliefs about one’s self, the world, and the future (A.T. Beck, 1972, J.S. Beck, 1995), and this might decrease the salience of other social-cognitive variables typically associated with health behaviors. In the current analysis, the relationship between negative expectancies about condom use and TRB was not moderated by depression: the pathway remained significant in all models, which could be thought of as consistent with negative thinking typically characteristic depression and suggesting that negative condom expectancies negatively influence condom use in the presence or absence of major depression.
There are some limitations to the present study. First, a self-report screener was used to assess depression versus clinical interview. The PHQ, however, has demonstrated relatively good reliability with diagnosis of independent mental health professionals (Spitzer et al., 1999). The percentage of individuals who screened in for depression (10%) was higher seen in the U.S. National Comorbidity Study (6.6%; Kessler et al., 2007), and lower than a recent study of HIV infected individuals (36% in Bing et al., 2007). However, the present study was not designed, in terms of sampling, to assess the prevalence of depression in the population of individuals with HIV. Second, the study was cross sectional, and longitudinal designs would be more powerful in demonstrating predictive relationships. However, strengths include the relatively large sample enabling us to have enough individuals who screened in for major depression in the cohort to test the study’s hypotheses and the ability to use SEM as an analytic tool. Third, the study focused on depression but did not consider other non-affective variables that may also interfere with the prediction of TRB from social cognitive variables, and may be related to depression, such as alcohol or other substance use/abuse. People with depression may be more likely to use such substances as a way of coping through escape-avoidance coping, and this may in turn, weaken the association between social cognitive variables and TRB1.
Despite the limitations, the data from this analysis are consistent with the hypothesis that depression may weaken the ability of Social Cognitive Theory to predict condom use in sexually active, HIV-infected MSM. Future research should examine this across other models of transmission risk behavior, and should examine this across other health behaviors in different populations. Because depression is a frequent problem in individuals with HIV, it is possible that interventions based on this model or similar models could increase their potency if they were to account for depression as part of the intervention. In HIV, depression is a treatable condition with medications and/or evidenced-based psychotherapies (Olatunji, Mimiaga, O’Cleirigh, & Safren, 2006). Accounting for comorbid psychosocial problems such as depression and other psychosocial problems has been advocated for in HIV prevention intervention research (Koblin et al., 2006; Stall et al., 2003), and the present study extends this literature, highlighting the importance of depression in developing or applying social-cognitive models to predict health behaviors in individuals with HIV.
Acknowledgments
Funding note: This project was funded by grant 5R01MH068746-05 and HRSA grant H97HA01293 to Drs. Kenneth H Mayer and Steven A Safren.
Footnotes
The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/journals/hea
We wish to thank the anonymous reviewer for articulating this point.
References
- Anderson JC, Gerbing DW. Structural equation modeling in practice: A review and recommended two-step approach. Psychological Bulletin. 1988;103:411–423. [Google Scholar]
- Asch SM, Kilbourne AM, Gifford AL, Burnam MA, Turner B, Shapiro MF The HCSUS Consortium. Underdiagnosis of depression in HIV: Who are we missing? Journal of General Internal Medicine. 2003;18:450–460. doi: 10.1046/j.1525-1497.2003.20938.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson JH, Grant I. Natural history of neuropsychiatric manifestations of HIV disease. The Psychiatric Clinics of North America. 1994;17:17–33. [PubMed] [Google Scholar]
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- Albarracín D, Johnson B, Fishbein M, Muellerleile P. Theories of reasoned action and planned behavior as models of condom use: A meta-analysis. Psychological Bulletin. 2001;127:142–161. doi: 10.1037/0033-2909.127.1.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social cognitive theory and the exercise of control over HIV infection. In: DiClemente R, Peterson J, editors. Preventing AIDS: Theories and methods of behavioral interventions. New York, NY: Plenum; 1994. pp. 25–59. [Google Scholar]
- Bing EG, Burnam MA, Longshore D, Fleishman JA, Sherbourne CD, London AS, Turner BJ, Eggan F, Beckman R, Vitiello B, Morton SC, Orlando M, Bozette SA, Ortiz-Barron L, Shapiro M. Psychiatric disorders and drug use among human immunodeficiency virus-infected adults in the United States. Archives of General Psychiatry. 2001;58:721–728. doi: 10.1001/archpsyc.58.8.721. [DOI] [PubMed] [Google Scholar]
- Beck AT. Cognitive therapy and the emotional disorders. NY: International Universities press; 1972. [Google Scholar]
- Beck JS. In: Cognitive therapy: Basics and Beyond. Catania JA, Kegeles S, Coates TJ, editors. NY: Guildford Press; 1995. [Google Scholar]
- Catania JA, Kegeles S, Coates TJ. Towards an understanding of risk behavior: An AIDS risk reduction model (AARM) Health Education Quarterly. 1990;17:53–72. doi: 10.1177/109019819001700107. [DOI] [PubMed] [Google Scholar]
- Catania J, Coates T, Kegeles S. A test of the AIDS Risk Reduction Model: Psychosocial correlates of condom use in the AMEN cohort survey. Health Psychology. 1994 November;13:548–555. doi: 10.1037//0278-6133.13.6.548. [DOI] [PubMed] [Google Scholar]
- Catania JA, Paul J, Osmond D, Folkman S, Pollack L, Canchola J, Chang J, Neilands T. Mediators of childhood sexual abuse and high-risk sex among men-who-have-sex-with-men. Child Abuse and Neglect. 2008;32:925–940. doi: 10.1016/j.chiabu.2007.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. HIV/AIDS Surveillance Report, 2005. Vol. 17. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2007. 2007. [Google Scholar]
- Crepaz N, Marks G. Are negative affective states associated with HIV sexual risk behaviors? A meta-analytic review. Health Psychology. 2001;20:291–299. doi: 10.1037//0278-6133.20.4.291. [DOI] [PubMed] [Google Scholar]
- Dew MA, Becker JT, Sanchez J, Caldararo R, Lopez OL, Wess J, Dorst SK, Banks G. Prevalence and predictors of depressive, anxiety and substance use disorders in HIV-infected and uninfected men: a longitudinal evaluation. Psychological Medicine. 1997;27:395–409. doi: 10.1017/s0033291796004552. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Changing AIDS-Risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Jaccard JJ, Wan CK. Interaction effects in multiple regression II: Multiple indicator and structural equation approaches. Newbury Park, CA: Sage; 1995. [Google Scholar]
- Kalichman SC, Weindhart L. Negative affect and sexual risk behavior: Comment on Crepaz and Marks (2001) Health Psychology. 2001;20:300–301. [PubMed] [Google Scholar]
- Kessler R, Merikangas K, Wang P. Prevalence, comorbidity, and service utilization for mood disorders in the United States at the beginning of the twenty-first century. Annual Review of Clinical Psychology. 2007;3:137–158. doi: 10.1146/annurev.clinpsy.3.022806.091444. [DOI] [PubMed] [Google Scholar]
- Knauz RO, Safren SA, O’Cleirigh C, Capistrant BD, Driskell JR, Aguilar D, Salomon L, Hobson J, Mayer KH. Developing an HIV-prevention intervention for HIV-infected men who have sex with men: Project Enhance. AIDS Behavior. 2007;5(S):117–126. doi: 10.1007/s10461-007-9257-0. [DOI] [PubMed] [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Barresi PJ, Coates TJ, Chesney MA, Buchbinder S. Risk factors for HIV infection among men who have sex with men. AIDS. 2006;21:731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Morin SF, Myers JJ, Shade SB, Koester K, Maiorana A, Dawson Rose C. Predicting HIV risk behavior among HIV-infected patients seen in clinical settings. AIDS and Behavior. 2007;11:S6–S16. doi: 10.1007/s10461-007-9253-4. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. Fifth Edition. Los Angeles, CA: Muthén & Muthén; 1998–2007. [Google Scholar]
- Olatunji BO, Mimiaga MJ, O’Cleirigh C, Safren SA. A review of treatment studies of depression in HIV. Topics in HIV medicine. 2006;14:112–124. [PubMed] [Google Scholar]
- Safren SA, O’Cleirigh CO, Tan JY, Raminani SR, Reilly LC, Otto MW, Mayer KH. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychology. 2009;28:1–10. doi: 10.1037/a0012715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer JL, Graham JW. Missing data: Our view of the state of the art. Psychological Methods. 2002;7:147–177. [PubMed] [Google Scholar]
- Spitzer RL, Korenke K, Williams JBW The Patient Health Questionnaire Primary Care Study Group. Validation and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. Journal of the American Medical Association. 1999;282:1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Stall R, Mills T, Williamson J, Hart T, Grenwood G, Pollack L, Binson D, Osmond D, Catania JA. Association of co-occurring psychosocial health problems and increased vulnerability to HIV/AIDS among urban men who have sex with men. American Journal of Public Health. 2003;93:939–942. doi: 10.2105/ajph.93.6.939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wulfert E, Safren SA, Brown I, Wan CK. Cognitive, behavioral, and personality correlates of HIV-positive persons’ unsafe sexual behavior. Journal of Applied Social Psychology. 1999;29:223–244. [Google Scholar]
- Wulfert E, Wan C. Condom use: A self-efficacy model. Health Psychology. 1993;12:346–353. doi: 10.1037//0278-6133.12.5.346. [DOI] [PubMed] [Google Scholar]
- Wulfert E, Wan CK, Backus CA. Gay men’s safer sex behavior: An integration of three models. Journal of Behavioral Medicine. 1996;19:345–366. doi: 10.1007/BF01904761. [DOI] [PubMed] [Google Scholar]
- Wulfert E, Wan C. Safer sex intentions and condom use viewed from a health belief, reasoned action, and social cognitive perspective. Journal of Sex Research. 1995;32:299–311. [Google Scholar]