ABSTRACT
Purpose: To investigate the diagnostic accuracy and association to disability of selected functional findings or physical examination tests for patellofemoral pain syndrome (PFPS) in patients with anterior knee pain.
Methods: A sample of 76 consecutive patients with anterior knee pain was further subdivided into PFPS and other diagnoses. Routine physical examination tests were examined in a prospective, consecutive-subjects design for a cohort of patients with anterior knee pain. Diagnostic accuracy findings, including sensitivity, specificity, positive (PPV) and negative (NPV) predictive value, and positive (LR+) and negative (LR−) likelihood ratios, were calculated for each test. PPV and NPV reflect the percentage of time of positive or a negative test (respectively) accurately captures the diagnosis of the condition. LR+ and LR− reflect alterations in post-test probability when the test is positive or negative (respectively). Lastly, associations to disability (International Knee Documentation Committee (IKDC) subjective form) were calculated for each clinical finding.
Results: Diagnostic accuracy analyses of individual functional assessment and situational phenomena suggest that the strongest diagnostic test is pain encountered during resisted muscle contraction of the knee (PPV=82%; LR+=2.2; 95% CI: 0.99–5.2). Clusters of test findings were substantially more diagnostic, with any two of three positive findings of muscle contraction, pain during squatting, and pain during palpation yielding the following values: PPV=89%; LR+=4.0 (95% CI: 1.8–10.3). No individual or clustered test findings were significantly associated with the IKDC score.
Conclusion: Combinations of functional assessment tests and situational phenomena are diagnostic for PFPS and may serve to rule in and rule out the presence of PFPS. Single findings are not related to disability scores (IKDC).
Key Words: diagnostic accuracy, International Knee Documentation Committee, patellofemoral pain syndrome, sensitivity, specificity
RÉSUMÉ
Objectif : Étudier la précision des diagnostics et l'association aux incapacités de résultats fonctionnels sélectionnés ou d'examens physiques dans les cas de syndromes fémoro-rotuliens douloureux (SFR) chez les patients aux prises avec des douleurs à la face antérieure du genou.
Méthodes : Un groupe de 76 patients aux prises avec de la douleur à la face antérieure du genou a été séparé en groupes ayant reçu un diagnostic de SFR ou d'autres problèmes. Les examens courants ont été analysés dans cette étude prospective de modèle séquentiel d'une cohorte de patients souffrant de douleurs à la face antérieure du genou. Les constatations quant à l'exactitude des diagnostics, y compris la sensibilité, la spécificité, les valeurs prédictives positive (VPP) et négative (VPN) et les rapports de vraisemblance positifs (RV+) et négatifs (RV−) ont été établis pour chaque examen. Les VPP et les VPN reflètent le nombre de fois, en pourcentage, où les tests positifs et négatifs (respectivement) reflètent correctement le diagnostic réel de l'état de santé. Les RV+ et les RV− expriment les modifications dans les probabilités après tests, lorsque ceux-ci sont positifs ou négatifs (respectivement). Enfin, les associations aux incapacités (formulaire subjectif de l'International Knee Documentation Committee) ont été calculées pour chaque constatation clinique.
Résultats : Les analyses de la précision diagnostique des évaluations fonctionnelles individuelles et des phénomènes situationnels semblent indiquer que le test le plus probant sur le plan diagnostic est celui de la douleur ressentie au cours de la contraction musculaire du genou, avec résistance (VPP=82 %; RV+=2,2; 95 % IC=0,99–5,2). Les groupes de constatations étaient nettement plus diagnostics, avec deux constatations positives sur trois de contraction musculaire, douleur à l'accroupissement et douleur à la palpation (VPP=89 %; RV+=4,0; 95 % IC=1,8–10,3). Aucun résultat de tests, individuels ou groupés, n'a pu être associé de manière significative au pointage établi selon le formulaire de l'IKDC.
Conclusion : Une combinaison de tests d'évaluation fonctionnelle et phénomènes situationnels constitue des diagnostics d'un SFR et peut être utilisée pour constater la présence ou l'absence de SFR. Les constatations simples ne sont pas liées aux indices d'incapacité (IKDC).
Mots clés : International Knee Documentation Committee, précision des diagnostics, syndrome fémoro-rotulien, syndrome fémoro-patellaire, spécificité
INTRODUCTION
Anterior knee pain is a common musculoskeletal complaint1,2 and is the hallmark clinical manifestation of patellofemoral pain syndrome (PFPS).3,4 Previous diagnostic criteria for PFPS have included anterior knee pain;4 anterior knee pain exacerbated by sitting, stairs, or squatting;5 pain in and around the patella;6 and insidious onset of retropatellar or anterior knee pain of greater than 6 weeks provoked by selected activities.7
At present, there is no consensus on the diagnosis of PFPS, nor is there a consistent use of clinical or functional tests to diagnose the condition.1 In the roughly 25 years of use of the term “patellofemoral pain syndrome,” only three studies have explicitly examined the diagnostic accuracy of PFPS. All three have been published since 2001, signifying that the investigation of the sensitivity and specificity of the components of the physical examination is a relatively new endeavour.
Niskanen et al.8 investigated four individual physical examination tests, all performed in the supine position, and found that only one of these tests, a 45-second hold at end-range of flexion, had a positive likelihood ratio (LR+) above 2.0 (2.33). Unfortunately, the usefulness of even this test in general practice is questionable in light of the limited description of the patient sample in this study.
A more recent study by Nijs et al.5 examined the utility of five physical examination tests in a well-described sample of 45 patients with knee pain. Three tests had a LR+ above 2.0: the vastus medialis coordination test, the patellar apprehension test, and the eccentric step test. However, the ability of any of these three tests to modify post-test probability was minimal (the best LR+ was reported as 2.34).
Another 2006 study by Haim et al.4 examined four individual tests and found two tests, the patellar tilt test (LR+=5.38) and the active instability test (LR+=12.5), that would modify post-test probability of PFPS to a moderate to significant degree. However, the subject sample was limited to 86 male soldiers, and the study used a type of case-control design, subjects with known pathology versus subjects with a known absence of pathology, that is known to lead to the greatest inflation of estimates of diagnostic accuracy.9,10
The limited investigation of the diagnostic accuracy of common physical examination tests and the lack of investigation of the sensitivity and specificity of pain during functional or situational activities such as stair climbing, descending stairs, or prolonged sitting have led some to recommend that the diagnostic approach in PFPS should involve first ruling out other pathologies that may cause anterior knee symptoms.1,11–14 The primary purpose of the present study was to investigate the diagnostic accuracy of common physical examination and functional tests for PFPS, and of clusters of these tests, in a well-described and generalizable sample of patients with anterior knee pain. A secondary purpose was to assess the association to disability in the same sample of patients.
METHODS
Study Design
Procedural guidelines for this prospective, consecutive-subjects-design study followed the Standards for Reporting of Diagnostic Accuracy (STARD) set forth by Bossuyt et al.15 Briefly, these standards are used to improve reporting processes for diagnostic accuracy studies and involve 25 items associated with topics germane to a typical case-control design. Topics are oriented toward description of participants, statistical analysis, results, and conclusions of findings. Prior to designing the study, we used the STARD outline to capture the majority of the procedural requirements suggested by the standards to improve the reporting of findings.
Participants
The study protocol was approved by the Institutional Review Board of Mary Black Healthcare Systems of South Carolina. The study involved 90 consecutive research subjects recruited at a sports medicine practice in Spartanburg, South Carolina. To be included in the study, English-speaking patients over 18 years of age must have been referred for an orthopaedic consult for a report of anterior knee pain. Data recorded for this study were similar to information recorded in customary screening examinations. To reduce the number of potential confounding signs or symptoms associated with post-surgical complications, patients who had had any prior knee surgery were excluded from the study.
Procedures
Participants were consecutive patients, identified by one of three attending surgeons, who were seen for any condition involving anterior knee pain of more than 3 months' duration. Each surgeon had a minimum of 5 years' experience, was board certified in sports medicine or orthopaedics, and was fellowship trained. After consenting to participate in the study, each patient provided a battery of descriptive information such as age, gender, and activity level and the completed the International Knee Documentation Committee (IKDC) subjective knee form. The IKDC contains 18 items designed to measure symptoms associated with pain, stiffness, swelling, joint locking, and joint instability, whereas other items designed to measure knee function assess the ability to perform activities of daily living.16 Patients with bilateral symptoms completed the IKDC form that captures criteria for both knees, whereas those with unilateral symptoms scored the form for a single knee. The IKDC has demonstrated two distinct dimensions, strong internal reliability (Cronbach's α=0.87, 0.88), concurrent validity with the Short Form 12 (SF12) (r=0.45, p<0.01), and item-response validity in a population of patients with various knee pathologies.16 The tool has been successfully translated into and validated in several languages, including Thai and Italian.17,18
Once each patient had completed the IKDC subjective knee form, a physician performed the functional tests or queried the patient about pain with functional activities. Physicians were instructed to identify the most painful knee for the study, and that single knee was considered during testing. The measures were (1) manual compression of the kneecap against the femur at rest or during an isometric knee-extensor contraction; (2) palpation of the postero-medial and postero-lateral borders of the patella; (3) resisted isometric quadriceps femoris muscle contraction; (4) squatting; (5) stair climbing; (6) kneeling; and (7) prolonged sitting.19 Prior to study initiation, all three surgeons underwent a 30-minute educational session with the investigators to standardize collection of the findings. The order of clinician examination was not standardized, and the performance of functional tests and situational phenomena was not consistent across patients.
Diagnosis
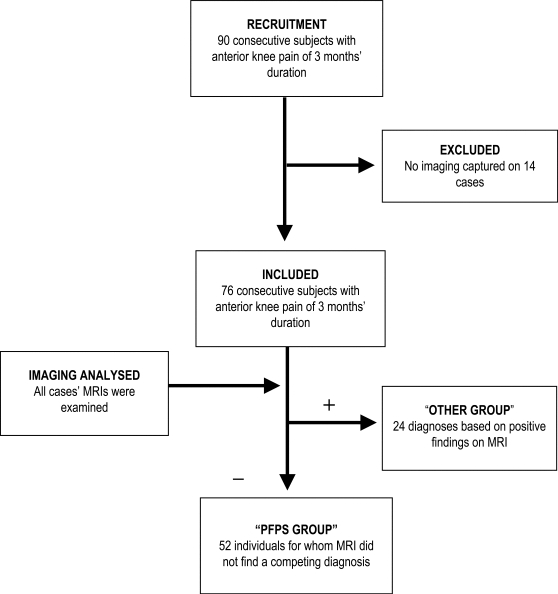
For this study, the clinical diagnosis of PFPS was made by an attending physician (see Figure 1). All patients with anterior knee pain of more than 3 months' duration were initially included. Using this sensitive inclusion strategy, all patients were suspected to have PFPS unless a competing diagnosis was ruled in. A competing diagnosis was any diagnostic condition (e.g., patellar tendonopathy, meniscal injury, medial overload syndrome) identified via magnetic resonance image (MRI). Only after careful evaluation of clinical findings and imaging methods (radiograph, MRI, or CT scan) did the physician make his or her final clinical diagnosis, which was used as the reference standard in this study. In nearly all cases, imaging was performed on the day of the clinical testing, and in all cases it was performed within the week of testing. Imaging was not used to confirm PFPS but, rather, to rule out competing diagnoses. In a number of cases that involved initial clinical suspicion of PFPS, patients with anterior knee pain were found to have a competing diagnosis of another nature, such as degenerative joint disease or osteoarthritis, chondral lesions, medial meniscus tears, medial overload syndrome, Baker's cysts, or an anterior cruciate ligament tear. Participants diagnosed with any of these conditions were assigned to the non-PFPS group. This diagnostic process has been suggested to improve the likelihood of an accurate diagnosis for PFPS, as well as of other pathologies identified as syndromes, and represents a more specific method of diagnosis.13
Figure 1.
The diagnostic flow strategy used in the study
Data Analysis
Descriptive statistics were calculated for each patient. Diagnostic accuracy for each of the functional findings and physical examination tests was determined using STATA 9.0 (StataCorp LP, College Station, TX). Sensitivity, specificity, positive and negative predictive values (PPV and NPV), and positive and negative likelihood ratios (LR+ and LR−) with 95% confidence intervals were calculated, using the physician's diagnosis as a reference standard. PPV and NPV reflect the percentage of time that a positive or a negative test (respectively) accurately captures the diagnosis of the condition; LR+ and LR− reflect alterations in post-test probability when the test is positive or negative (respectively).
Clusters of functional findings and physical examination tests were also tabulated to determine combinations that improved diagnostic accuracy. All possible combinations were examined to capture those with either the strongest sensitivity or the strongest diagnostic accuracy. Post-test probability was calculated using LR+ and the prevalence of PFPS in the study sample (calculated as the number of participants who met the physicians' criteria for diagnosis of PFPS).
Lastly, point biserial correlation was calculated between the functional findings and physical examination tests and the IKDC subjective scores (higher scores indicating better function) for all patients with anterior knee pain and for patients with PFPS only. This analysis allowed an assessment of the association between each individual physical examination test or functional finding and the IKDC score. The level of significance was set a priori at p≤0.05.
RESULTS
Descriptive Data
From June 2007 through August 2008, 90 patients were identified who satisfied the inclusion criteria for this study. Usable data (high-quality MR images) were obtained for 76 of the 90 individuals. Of these 76 cases, 24 were diagnosed with other pathologies and, by exclusion, 52 were classified as having PFPS. No significant differences were found between the two groups in age, gender, painful knee, education level, work status, months of reported pain, marital status, report of participation in sports, exercise level, report of pain in the uninvolved knee, or morphological criteria such as height and weight (see Table 1).
Table 1.
Descriptive Statistics of the Sample (N=76)
| Variable | PFPS n / mean (SD) | Non-PFPS n / mean (SD) | p | |
|---|---|---|---|---|
| Age | 49.3 (13.5) | 50.4 (15.6) | 0.78 | |
| Gender | Male | 25 | 8 | 0.11 |
| Female | 17 | 13 | ||
| Painful knee | Left | 23 | 8 | 0.32 |
| Right | 17 | 12 | ||
| Both | 12 | 4 | ||
| Education level | <High school | 1 | 2 | 0.22 |
| High school | 21 | 6 | ||
| >High school | 30 | 16 | ||
| Work status | Working | 35 | 13 | 0.27 |
| Not working | 17 | 11 | ||
| Months of reported pain | 34.3 (55.6) | 44.5 (97.2) | 0.57 | |
| Marital status | Single | 8 | 5 | 0.80 |
| Married | 34 | 16 | ||
| Separated or divorced | 9 | 3 | ||
| Other | 1 | 0 | ||
| Participation in sports | Yes | 10 | 7 | 0.37 |
| No | 41 | 17 | ||
| Data missing | 1 | 0 | ||
| Exercise level | Very active | 6 | 0 | 0.08 |
| Active | 22 | 17 | ||
| Inactive | 19 | 5 | ||
| Very inactive | 5 | 2 | ||
| Painful uninvolved knee | Yes | 12 | 5 | 0.73 |
| No | 31 | 16 | ||
| Prior history of same knee problems | Yes | 32 | 12 | 0.29 |
| No | 19 | 12 | ||
| Height (") | 67.4 (3.9) | 67 (4.1) | 0.69 | |
| Weight (lb) | 201.6 (47.3) | 187.9 (48.3) | 0.25 |
PFPS=Patellofemoral Pain Syndrome
Table 2 provides the diagnostic accuracy values of seven commonly used functional tests and activities for detection of PFPS. Pain during a resisted quadriceps contraction demonstrated the highest PPV (0.82; 95% CI: 0.67–0.91), the highest LR+ (2.2; 95% CI: 0.99–5.2), and the highest specificity (82%). In addition, pain during a resisted contraction yielded the highest post-test probability (81.7%). The most sensitive tests were pain during squatting (91%) and pain during kneeling (84%). All tests yielded moderate improvements in post-test probability, ranging from a low of 75.3% (pain during palpation and pain during manual compression) to a high of 81.7% (pain during resisted muscle contraction).
Table 2.
Diagnostic Accuracy Values of the Functional Tests and Situational Phenomena
| Sensitivity | Specificity | PPV (95% CI) | NPV (95% CI) | LR+ (95% CI) | LR− (95% CI) | Post-test Probability | |
|---|---|---|---|---|---|---|---|
| Pain during manual compression | 68 | 54 | 0.75 (0.67–0.82) | 0.46 (0.33–0.57) | 1.5 (0.99–2.3) | 0.6 (0.3–1.0) | 75.3 |
| Pain during palpation | 47 | 68 | 0.75 (0.63–0.85) | 0.39 (0.30–0.46) | 1.5 (0.85–2.8) | 0.8 (0.6–1.1) | 75.3 |
| Pain during resisted muscle contraction | 39 | 82 | 0.82 (0.67–0.91) | 0.4 (0.32–0.44) | 2.2 (0.99–5.2) | 0.75 (0.6–1.1) | 81.7 |
| Pain during squatting | 91 | 50 | 0.79 (0.73–0.82) | 0.74 (0.54–0.87) | 1.8 (1.3–2.3) | 0.2 (0.1–0.4) | 78.5 |
| Pain during stair climbing | 75 | 43 | 0.73 (0.66–0.79) | 0.46 (0.3–0.6) | 1.3 (.96–1.9) | 0.6 (0.03–1.1) | 72.5 |
| Pain during kneeling | 84 | 50 | 0.79 (0.71–0.83) | 0.61 (0.44–0.75) | 1.7 (1.2–2.4) | 0.3 (0.2–0.6) | 77.5 |
| Pain during prolonged sitting | 72 | 57 | 0.77 (0.60–0.84) | 0.5 (0.37–0.6) | 1.7 (1.1–2.7) | 0.5 (0.3–0.8) | 77.5 |
PPV=positive predictive value; NPV=negative predictive value; LR+=positive likelihood ratio; LR−=negative likelihood ratio
Combining the test and measures (physical performance tests and/or situational phenomena; see Table 3) yielded marginal improvements in diagnostic accuracy. The strongest combination was any two of three positive findings for pain during a resisted muscle contraction and/or pain during squatting and/or pain during palpation; this combination yielded a LR+ of 4.0 (95% CI: 1.8–10.3) and a post-test probability of 89.1%. Other combinations—two of two positive findings for pain during muscle contraction and pain during squatting and three of three positive findings for pain during muscle contraction, pain during squatting, and pain during kneeling—also exhibited improvements over the use of each situational phenomenon or physical performance test in isolation, increasing the post-test probability to 87.1% and 86.3% respectively.
Table 3.
Diagnostic Accuracy of Best Combinations (Clusters) of Functional Tests and Situational Phenomena
| Sensitivity | Specificity | PPV (95% CI) | NPV (95% CI) | LR+ (95% CI) | LR− (95% CI) | Post-test Probability | |
|---|---|---|---|---|---|---|---|
| Positive findings of muscle contraction and pain during squatting (2 of 2) | 35 | 89 | 0.87 (0.71–0.95) | 0.40 (0.34–0.43) | 3.3 (1.2–9.2) | 0.73 (0.6–0.94) | 87.1 |
| Positive findings of muscle contraction and/or pain during squatting and/or pain during palpation (2 of 3) | 60 | 85 | 0.89 (0.79–0.95) | 0.5 (0.4–0.46) | 4.0 (1.8–10.3) | 0.5 (0.38–0.68) | 89.1 |
| Positive findings of muscle contraction, pain during squatting, and pain during kneeling (3 of 3) | 33 | 89 | 0.86 (0.69–0.95) | 0.39 (0.34–0.43) | 3.1 (1.1–9.5) | 0.7 (0.6–0.9) | 86.3 |
PPV=positive predictive value; NPV=negative predictive value; LR+=positive likelihood ratio; LR−=negative likelihood ratio
Patients with PFPS reported a mean IKDC value of 33.7 (SD=15.9), whereas those diagnosed with conditions other than PFPS scored a mean value of 38.7 (SD=16.30); the two findings were not significantly different (p=0.29). Point biserial correlation with the IKDC subjective form yielded no significant relationships for any of the functional tests or situational phenomena, either for all patients in the anterior knee pain group or for patients in the PFPS-only group (see Table 4).
Table 4.
Point Biserial Correlation of IKDC Subjective Form Values with Functional Finding and Situational Phenomena
| Functional Finding or Situational Phenomenon | Point Biserial Correlation (all patients) | p | Point Biserial Correlation (PFPS only) | p |
|---|---|---|---|---|
| Pain during manual compression | 0.17 | 0.17 | 0.05 | 0.71 |
| Pain during palpation | 0.23 | 0.06 | 0.17 | 0.23 |
| Pain during resisted muscle contraction | 0.01 | 0.96 | −0.01 | 0.92 |
| Pain during squatting | 0.15 | 0.22 | −0.02 | 0.89 |
| Pain during stair climbing | 0.03 | 0.79 | 0.08 | 0.58 |
| Pain during kneeling | 0.06 | 0.64 | 0.004 | 0.98 |
| Pain during prolonged sitting | 0.13 | 0.29 | −0.02 | 0.88 |
DISCUSSION
To our knowledge, this is the first prospective, consecutive-subjects study to explore the diagnostic accuracy of both selected physical examination tests and common functional activities frequently used in the clinical diagnosis of PFPS. We carefully evaluated each patient with a history of anterior knee pain and ruled out the presence of other competing diagnoses through diagnostic tests such as imaging. This approach is recommended for syndromes in general, and specifically for PFPS.13 Our results suggest that no single physical examination test or reported functional activity is helpful in the diagnosis of PFPS. However, any two of three of pain with quadriceps contraction, pain during squatting, and/or pain during palpation of the postero-medial or postero-lateral border results in a moderate shift toward the diagnosis of PFPS after competing sources of anterior knee pain have been ruled out.
We are aware of three studies4,5,8 that have investigated the diagnostic accuracy of selected clinical tests for PFPS. These studies produced similar findings to ours, in that the individual physical examination tests were not helpful in diagnosing PFPS. The exceptions are the active instability and tilt tests, which in Haim et al.'s4 study had LR+ values of 12.5 and 5.4 respectively. However, the case-control design used in this study may have falsely elevated measures of diagnostic accuracy. Further, the fact that the sample was composed exclusively of male soldiers may have elevated the pre-test probability of PFPS to a greater extent than would be observed in the general population. None of these studies evaluated post-test probability or clustered the result findings. As is true of most published reports within the literature, the diagnostic criteria of PFPS were different in all three studies, as were the included tests and measures investigated for diagnostic accuracy.
If PFPS is truly a diagnosis of exclusion,1 it should be considered only after ruling out other contending diagnoses. Consequently, a diagnosis of PFPS requires a high LR+ for ruling in the presence of the disorder. Nijs and colleagues,5 in a prospective sample of convenience that, like our study, used PFPS as a diagnosis of exclusion, found that the eccentric step test yielded the highest LR+ (2.3; 95% CI: 1.9–2.9) of all reported values. This value fell below our calculated clusters of findings, which included two of two positive findings of pain with quadriceps muscle contraction and pain during squatting; any two of three positive findings of muscle contraction, pain during squatting, and pain during palpation; and three of three positive findings of muscle contraction, pain during squatting, and pain during kneeling. Clusters of findings in our study also yielded the highest post-test probability compared to singular uses of the functional tests and physical examination tests.
Worth noting is the poor relationship between results of the functional tests and situational phenomena and IKDC subjective scores in all patients with anterior knee pain and in patients restricted to a diagnosis of PFPS. This suggests that the tests, while somewhat useful for diagnosis, are not useful in determining levels of disability for patients with anterior knee pain. Others have reported similar findings of marginal association between clinical test findings and disability,19 which may reflect the difficulty in identifying pertinent clinical markers for the severity of a patient's PFPS.
LIMITATIONS
There are a number of limitations in this study. First, it is important to note that there is no truly definitive reference standard for PFPS and that the disorder is a clinical diagnosis, often made by ruling out other potential disorders. In some situations, PFPS can occur concomitantly with other diagnoses, and the possibility exists that this occurred in our study, specifically with conditions such as mediopatellar plica syndrome, which was not examined in the study. There is a strong possibility that unknown conditions masquerading as PFPS that were not identified by imaging were actually diagnosed as PFPS. Second, the environment in which the data were collected was a sports medicine centre, and this practice setting generally captures a larger sample of patients with PFPS than may be observed in other orthopaedic settings. Higher pre-test prevalence will lead to increases in post-test probability. Third, a larger sample size would have improved the generalizability of our findings. We did not capture reliability measures of our tests and measures. Lastly, although the diagnosing physician was not always the same physician who performed the tests, the results were available for consideration if the physician chose to explore the findings. Consequently, there is a likelihood of incorporation bias in this study.
CONCLUSIONS
This study complements the body of knowledge on the diagnostic accuracy of the clinical examination of PFPS by using an approach predicated on eliminating other sources of anterior knee pain prior to using clustered tests with higher LR+ to focus on the final diagnosis of PFPS. Further, the clustering of the physical examination findings of pain with quadriceps contraction or with palpation of the posterior edges of the patella with patient report of pain in the functional activity of squatting produces a post-test probability of PFPS of 89.1%. Future studies should use the diagnostic approach outlined in our study and examine the effect on diagnostic accuracy of combining functional activities such as squatting and descending stairs with the best functional tests from the current body of literature (patellar tilt, pain during resisted knee extension, active instability test). To improve the generalizability of the findings, future research should use a larger sample size with data gathered from multiple general orthopaedic sites.
KEY MESSAGES
What Is Already Known on This Subject
The routine measures of (1) manual compression of the knee cap against the femur at rest or during an isometric knee extensor contraction, (2) palpation of the postero-medial and postero-lateral borders of the patella, (3) resisted isometric quadriceps femoris muscle contraction, (4) squatting, (5) stair climbing, (6) kneeling, and (7) prolonged sitting are commonly used to diagnose patellofemoral pain syndrome (PFPS), despite the fact that few of these measures have been investigated for accuracy.
What This Study Adds
This study individually and collectively explores the diagnostic accuracy and relationship to disability of each of the measures listed above. Accuracy of the diagnosis of PFPS is substantiated by use of a rule-out, rule-in probabilistic model, using imaging methods to confirm the competing diagnosis.
Cook C, Hegedus E, Hawkins R, Scovell F, Wyland D. Diagnostic accuracy and association to disability of clinical test findings associated with patellofemoral pain syndrome. Physiother Can. 2010;62:17–24.
REFERENCES
- 1.Naslund J, Naslund UB, Odenbring S, Lundeberg T. Comparison of symptoms and clinical findings in subgroups of individuals with patellofemoral pain. Physiother Theory Pract. 2006;22:105–18. doi: 10.1080/09593980600724246. [DOI] [PubMed] [Google Scholar]
- 2.Urwin M, Symmons D, Allison T, Brammah T, Busby H, Roxby M, et al. Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites, and the relation to social deprivation. Ann Rheum Dis. 1998;57:649–55. doi: 10.1136/ard.57.11.649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arroll B, Ellis-Pegler E, Edwards A, Sutcliffe G. Patellofemoral pain syndrome: a critical review of the clinical trials on nonoperative therapy. Am J Sport Med. 1997;25:207–12. doi: 10.1177/036354659702500212. [DOI] [PubMed] [Google Scholar]
- 4.Haim A, Yaniv M, Dekel S, Amir H. Patellofemoral pain syndrome. Clin Orthop Rel Res. 2006;451:223–8. doi: 10.1097/01.blo.0000229284.45485.6c. [DOI] [PubMed] [Google Scholar]
- 5.Nijs J, van Geel C, van der Auwera C, Van de Velde B. Diagnostic value of five clinical tests in patellofemoral pain syndrome. Man Ther. 2006;11:69–77. doi: 10.1016/j.math.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 6.Houghton KM. Review for the generalist: evaluation of anterior knee pain. Pediatr Rheumatol Online J. 2007;5:a8. doi: 10.1186/1546-0096-5-8. doi: 10.1186/1546-0096-5-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Collins N, Crossley K, Beller E, Darnell R, McPoil T, Vicenzino B. Foot orthoses physiotherapy in the treatment of patellofemoral pain syndrome: randomized controlled trial. Brit Med J. 2008;337:1–8. doi: 10.1136/bmj.a1735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Niskanen RO, Paavilainen PS, Jaakkola M, Korkala OL. Poor correlation of clinical signs with patellar cartilaginous changes. J Arthoscopy Rel Res. 2001;17:307–10. doi: 10.1053/jars.2001.21240. [DOI] [PubMed] [Google Scholar]
- 9.Lijmer JG, Mol BW, Heisterkamp S, Bonsel GJ, Prins MH, van der Meulen JH, et al. Empirical evidence of design-related bias in studies of diagnostic tests. J Am Med Assoc. 1999;282:1061–6. doi: 10.1001/jama.282.11.1061. [DOI] [PubMed] [Google Scholar]
- 10.Rutjes AW, Reitsma JB, Di Nisio M, Smidt N, van Rijn JC, Bossuyt PM. Evidence of bias and variation in diagnostic accuracy studies. Can Med Assoc J. 2006;174:469–76. doi: 10.1503/cmaj.050090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mann G, Constantini N, Hetsroni I, Meidan O, Dolev E, Morgenstern D, et al. Anterior knee-pain syndrome. Adolesc Med State Art Rev. 2007;18:192–220. [PubMed] [Google Scholar]
- 12.Thomee R, Augustsson J, Karlsson J. Patellofemoral pain syndrome: a review of current issues. Sport Med. 1999;28:245–62. doi: 10.2165/00007256-199928040-00003. [DOI] [PubMed] [Google Scholar]
- 13.Witvrouw E, Werner S, Mikkelsen C, Van Tiggelen D, Vanden Berghe L, Cerulli G. Clinical classification of patellofemoral pain syndrome: guidelines for non-operative treatment. Knee Surg Sport Traumatol Arthrosc. 2005;13:122–30. doi: 10.1007/s00167-004-0577-6. [DOI] [PubMed] [Google Scholar]
- 14.Watson CJ, Leddy HM, Dynjan TD, Parham JL. Reliability of the lateral pull test and tilt test to assess patellar alignment in subjects with symptomatic knees: student raters. J Orthop Sport Phys Ther. 2001;31:368–74. doi: 10.2519/jospt.2001.31.7.368. [DOI] [PubMed] [Google Scholar]
- 15.Bossuyt PM, Reitsma JB, Bruns DE, Gatsonis CA, Glasziou PP, Irwig LM, et al. Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. Acad Radiol. 2003;10:664–9. doi: 10.1016/s1076-6332(03)80086-7. [DOI] [PubMed] [Google Scholar]
- 16.Higgins LD, Taylor MK, Park D, Ghodadra N, Marchant M, Pietrobon R, et al. Reliability and validity of the International Knee Documentation Committee (IKDC) Subjective Knee Form. Joint Bone Spine. 2007;74:594–9. doi: 10.1016/j.jbspin.2007.01.036. [DOI] [PubMed] [Google Scholar]
- 17.Lertwanich P, Praphruetkit T, Keyurapan E, Lamsam C, Kulthanan T. Validity and reliability of Thai version of the International Knee Documentation Committee Subjective Knee Form. J Med Assoc Thai. 2008;91:1218–25. [PubMed] [Google Scholar]
- 18.Padua R, Bondi R, Ceccarelli E, Bondi L, Romanini E, Zanoli G, et al. Italian version of the International Knee Documentation Committee Subjective Knee Form: cross-cultural adaptation and validation. Arthroscopy. 2004;20:819–23. doi: 10.1016/j.arthro.2004.06.011. [DOI] [PubMed] [Google Scholar]
- 19.Piva SR, Fitzgerald K, Irrgang J, Jones S, Hando BJ, Browder D, et al. Reliability of measures of impairments associated with patellofemoral pain syndrome. BMC Musculoskelet Dis. 2006;7:a33. doi: 10.1186/1471-2474-7-33. doi: 10.1186/1471-2474-7-33. [DOI] [PMC free article] [PubMed] [Google Scholar]