Abstract
Recent work exploring the relationship between socioeconomic status and health has employed a psychosocial concept called perceived social position as a predictor of health. Perceived social position is likely the “cognitive averaging” (Singh-Manoux, Marmot, & Adler, 2005) of socioeconomic characteristics over time and, like other socioeconomic factors, is subject to interplay with health over the life course. Based on the hypothesis that health can also affect perceived social position, in this paper we used structural equation modeling to examine whether perceived social position and three different health outcomes were reciprocally related in the Wisconsin Longitudinal Study, a longitudinal cohort study of older adults in the United States. The relationship between perceived social position and health differed across health outcomes—self-reported health, the Health Utilities Index, and depressive symptoms—as well as across operationalizations of perceived social position—compared to the population of the United States, compared to one’s community, and a latent variable of which the two items are indicators. We found that perceived social position affected self-reported health when operationalized as latent and US perceived social position, yet there was a reciprocal relationship between self-reported health and community perceived social position. There was a reciprocal relationship between perceived social position and the Health Utilities Index, and depressive symptoms affected perceived social position for all operationalizations of perceived social position. The findings suggest that the causal relationship hypothesized in prior studies—that perceived social position affects health—does not necessarily hold in empirical models of reciprocal relationships. Future research should interrogate the relationship between perceived social position and health rather than assume the direction of causality in their relationship.
Keywords: USA, Perceived social position, Subjective social status, socioeconomic status (SES), Self-reported health, Health Utilities Index, CES-D, Older adults
Introduction
The relationship between socioeconomic status (SES) and health has been explored in multiple ways, revealing a positive relationship between SES and health (Adler, Boyce, Chesney, & Cohen, 1994; Haan, Kaplan, & Syme, 1989; House & Williams, 2000; Kitigawa & Hauser, 1973; Link & Phelan, 1995; Marmot, Shipley & Rose, 1984). SES has been operationalized in several ways when investigating its relationship with health, such as educational attainment, occupational status, income, and combinations thereof (Duncan et al., 2002). Recent work has focused on perceived social position (also called “subjective social status”) as a socioeconomic predictor of health that mediates in part the effect of other measures of socioeconomic status on health (Singh-Manoux, Adler and Marmot, 2003). Perceived social position is often measured by asking respondents to assess their social status relative to others in their country or community using the pictorial representation of a ladder (Adler et al., 2000).
Several studies have found that lower perceived social position predicts a variety of health outcomes even after controlling for the more objective indicators of SES. Self-reported health is often the health outcome of interest, but researchers have examined other health outcomes such as mortality (Kopp et al., 2004), long-standing illness (Demakakos et al., 2008), composite indicators of physical health (Singh-Manoux, Marmot, & Adler, 2005), physical functioning status (Hu et al., 2005), cortisol response to awakening (Wright & Steptoe, 2005), reports of stress (Adler et al., 2000; Goodman et al., 2005), psychological distress (Singh-Manoux, Marmot, & Adler, 2005), depressive symptoms (Collins & Goldman, 2008; Demakakos et al., 2008; Singh-Manoux, Adler, & Marmot, 2003), angina (Singh-Manoux, Adler, & Marmot, 2003), diabetes (Demakakos et al., 2008; Singh-Manoux, Adler, & Marmot, 2003), high-density lipoprotein cholesterol (Demakakos et al., 2008), respiratory illness (Singh-Manoux, Adler, & Marmot, 2003), susceptibility to respiratory infection (Cohen et al., 2008), and reduced gray matter in the anterior cingulated cortex, which indicates physiological reactivity to psychosocial stress (Gianaros et al., 2007). The link between perceived social position and health has been established across a variety of populations, such as national samples of adults in the United States (Operario, Adler, & Williams, 2004) and Hungary (Kopp et al., 2004), the Whitehall II study of British social servants (Singh-Manoux, Adler, & Marmot, 2003; Singh-Manoux, Marmot, & Adler, 2005), pregnant women in the United States (Adler et al., 2000), White and Chinese women in the United States (Ostrove et al., 2000), older Taiwanese (Hu et al., 2005; Collins & Goldman, 2008), older British adults (Demakakos et al., 2008), adolescents in the Midwestern United States (Goodman et al., 2005), Mexican-origin individuals in Texas (Franzini & Fernandez-Esquer, 2006), and Canadian adults (Dunn, Veenstra, & Ross, 2006).
One prominent argument is that the perceived social position items capture the “cognitive averaging” of socioeconomic and other social characteristics that in theory could be objectively observed (Singh-Manoux et al., 2005). In other words, asking respondents for their judgment of their SES allows respondents to account for more nuanced facets of their unique socioeconomic position as well as their past and future prospects. Another explanation is that perceived social position encompasses perceptions of inequality or subordination. Wilkinson (1996, 1999) made the compelling claim that income inequality is a more consistent predictor of morbidity and mortality than absolute income, based on his finding that countries with more social inequality have relatively low life expectancies. Wilkinson finds that some poor countries with little social inequality can have higher life expectancies than rich countries with more social inequality, and posits that the psychological perception of increased inequality damages health outcomes. Animal models have demonstrated that lower social rankings can lead to biomarkers of chronic stress (Sapolsky, 2004).
I choose to call the construct “perceived social position” rather than “subjective social status” because it is more in line with prominent “cognitive averaging” explanation of what perceived social position captures. “Subjective” is an adjective and coupled with “social status” implies that individuals have an inherent social status that exists in their psyche. On the other hand, “perceived” is a verb that indicates that once individuals are provided a stimulus that asks about their social status, they become aware of, recognize, or discern their social status to answer the question, but it is not assumed a priori that everyone has an inherent social status existing in their mind. In short, “subjective social status” is a characteristic of the individual, while “perceived social position” acknowledges that everyone may not have this characteristic, but will use the evidence at hand—their life history—to identify their social status once the perceived social position items are posed.
While previous studies have assumed that perceived social position affects health outcomes, it is possible that health also affects perceived social position. In addition to the idea that SES is a fundamental cause of disease (Link and Phelan, 1995), there is an interplay between SES and health over the life course in that social selection is a “nonignorable” mechanism through which health in part can affect socioeconomic outcomes (Palloni, 2006). Given that perceived social position likely constitutes a “cognitive averaging” of socioeconomic characteristics over time (Singh-Manoux, Marmot, & Adler, 2005), perceived social position may be considered another component of SES that is subject to interplay with health, and not just a cause of health, at different points across the life course.
The present study uses structural equation models of reciprocal relationships to empirically investigate the hypothesis that perceived social position and health mutually affect one another at a given point in time. Structural equation modeling will allow for models of reciprocal relationships to be compared to the alternative unidirectional model specifications using model fit statistics to determine the model that best fits the data. Self-reported health is examined as one health outcome of interest because it is often used in studies analyzing the relationship between perceived social position and health. The Health Utilities Index (HUI) is another health outcome of interest used because, to my knowledge, no study has examined the relationship between HUI and perceived social position. Having depressive symptoms is the mental health outcome of interest, again because depressive symptoms are often used in studies investigating the relationship between perceived social position and health. Notably, other health outcomes were considered and found to not be associated with measures of perceived social position in this sample: body mass index, the number of physical symptoms reported, and the number of health conditions or illnesses reported.
Methods
Participants
The analytic sample includes participants in the Wisconsin Longitudinal Study (WLS), a one-third random sample of 10,317 men and women who graduated from Wisconsin high schools in 1957. Survey data were collected by phone and mail from the original respondents or their parents in 1957, 1964, 1975, 1993, and 2004 (Sewell et al., 2004). The analytic sample was restricted to those WLS respondents who were working in 1993, so that all respondents are on the same metric with regard to the measures of occupation. (The distance from no occupation to the lowest occupation is qualitatively different from the distance from the lowest occupation to the second lowest occupation when using a linear scale like occupational education, which is employed here.) The sample was also restricted to those who answered the items comprising the health dependent variables (n=5731). Table 1 contains the descriptive statistics for the full WLS sample and the final analytic sample.
Table 1.
Descriptive statistics for full and analytic sample, Wisconsin Longitudinal Studya
| Analytic sample (N=5731) |
Full sample |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Year | Mean or % | s.d. | Min | Max | % imputed | Mean or % | s.d. | N | |
| Self-reported health | 2004 | 4.03 | 0.67 | 1.00 | 5.00 | 0.00% | 4.03 | 0.67 | 5833 |
| Self-reported health comparison | 2004 | 4.12 | 0.74 | 1.00 | 5.00 | 0.00% | 4.12 | 0.75 | 6143 |
| Health utilities index | 2004 | 0.83 | 0.20 | −0.22 | 1.00 | 0.00% | 0.83 | 0.21 | 6751 |
| Depressive symptoms (natural log) | 2004 | 6.59 | 5.92 | 0.00 | 41.46 | 0.00% | 6.44 | 5.78 | 6114 |
| US perceived social position | 2004 | 6.68 | 1.43 | 1.00 | 10.00 | 2.32% | 6.71 | 1.43 | 5713 |
| Community perceived social position | 2004 | 6.58 | 1.70 | 1.00 | 10.00 | 2.51% | 6.60 | 1.69 | 5703 |
| Self-reported health | 1993 | 4.18 | 0.65 | 1.00 | 5.00 | 10.59% | 4.16 | 0.67 | 6583 |
| Self-reported health comparison | 1993 | 4.19 | 0.71 | 1.00 | 5.00 | 11.60% | 4.16 | 0.73 | 6514 |
| Smoking status | 1993 | 0.71 | 0.74 | 0.00 | 2.00 | 11.85% | 0.73 | 0.74 | 6495 |
| Body mass index | 1993 | 1.95 | 0.86 | 1.00 | 4.00 | 12.56% | 1.96 | 0.86 | 6441 |
| Depressive symptoms (natural log) | 1993 | 7.75 | 6.27 | 0.00 | 41.59 | 11.25% | 7.77 | 6.20 | 6531 |
| Marital status (1=married) | 1993 | 0.84 % | 0.00 | 1.00 | 0.02% | 0.82 % | 8122 | ||
| Gender (1=female) | 1993 | 0.53 % | 0.00 | 1.00 | 0.00% | 0.51 % | 8124 | ||
| Education (parent report) | 1964 | 13.42 | 1.78 | 12.00 | 18.00 | 10.63% | 13.40 | 1.79 | 7192 |
| Education (respondent report) | 1975 | 13.46 | 2.09 | 12.00 | 18.00 | 0.02% | 13.41 | 2.07 | 8123 |
| Occupational education in 1993 | 1993 | 0.64 | 1.32 | −4.62 | 4.52 | 0.00% | 0.58 | 1.32 | 8124 |
| Occupational education in 1993 | 2004 | 0.62 | 1.32 | −4.62 | 4.93 | 6.53% | 0.65 | 1.33 | 6318 |
| Household income (natural log) | 1993 | 10.85 | 0.94 | 8.52 | 16.12 | 0.05% | 10.78 | 0.99 | 8119 |
| Work success | 1993 | 3.52 | 0.56 | 1.00 | 4.00 | 0.30% | 3.52 | 0.56 | 8094 |
| Financial success | 1993 | 3.21 | 0.56 | 1.00 | 4.00 | 0.19% | 3.21 | 0.57 | 8104 |
Analytic sample averaged across the five imputed datasets
Measures
The present study used data mainly from the 1993 and 2004 waves of the WLS. The outcome variables came from the 2004 wave and included perceived social position, self-reported health, HUI, and depressive symptoms.
Perceived social position
Perceived social position in 2004 was assessed using two items from the MacArthur Scale of Subjective Social Status that ask respondents to rank their social position compared to others in the United States and others in their community. A picture of a ladder with 10 rungs was given as part of the following item: "Think of this ladder as representing where people stand in America. At the top of the ladder are the people who are the best off—those who have the most money, the most education and the most respected jobs. At the bottom are the people who are the worst off—who have the least money, least education and the least respected jobs or no jobs. The higher you are on this ladder, the closer you are to the people at the very top; the lower you are, the closer you are to the people at the very bottom. If you consider your current situation and compare it with all other people in America [your community], where would you place yourself on this ladder?” The items were coded so that a higher score indicates better perceived social position.
The US and community comparison items yielded a Cronbach’s alpha value of .753, were highly correlated (r=.613, p<.001), and appeared to load relatively well on the same underlying factor (unstandardized: US=1.00, community=.79; standardized: US=.91, community=.72. A common rule of thumb is that the standardized loadings should be .7 or higher, because .7 corresponds to almost half of the variance in the indicator being explained by the factor.) However, it is possible that one of the comparison items is more relevant than the other for this population, and that the inclusion of the other item as loading on the same underlying factor could dilute the relationship between the perceived social position and health observed in the data. Therefore, analyses were conducted using the US and community comparison items as indicators of latent perceived social position, then replicated using the US and community comparison items as distinct measures of perceived social position.
Self-reported health
This study used self-reported health in 2004 as one health outcome of interest, because it is a consistent predictor of subsequent mortality (Idler and Benyamini, 1997) and is often used in studies analyzing the relationship between perceived social position and health. Self-reported health in 2004 was analyzed as a latent variable with two indicators loading on it: “How would you rate your health at the present time [compared to other people your age and sex]? Very poor, poor, fair, good or excellent?” These responses were coded from 1=very poor to 5=excellent. The same items were asked in the 1993 wave of the survey and used as indicators of latent self-reported health in 1993. Self-reported health in 1993 was included in the analysis as one control for baseline health status.
Health Utilities Index Mark 3 (HUI)
HUI score in 2004 was another health outcome of interest in this study. HUI is a health-status classification system that describes the health status and health-related quality of life of individuals across a wide range of domains using one summary score, and has been used across a variety of populations in population health and clinical studies (Horsman et al., 2003). The domains in HUI include vision, hearing, speech, ambulation, dexterity, emotion, cognition, and pain. The score for each domain was derived from community preference (utility) measures for each health state, where dead=0 and perfect health=1, and the compilation of scores across domains yields a HUI with a theoretical range between 1 (perfect health) and -.36 (living in a state worse than death) (Horsman et al., 2003).
Depressive symptoms
Having depressive symptoms in 2004 was the mental health outcome of interest in this study, and was constructed as a summary score of twenty items from the Center for Epidemiological Studies Depression scale (Radloff, 1977). The questions about positive affect were reverse coded to match the negativity of the rest of the scale so that a higher score on the scale indicates more depressive symptoms exhibited by the respondent. The natural log of the summary score was used for analysis because the raw summary score was skewed toward having fewer depressive symptoms.
Having depressive symptoms in 1993 was included as a control variable in this study for two reasons. First, depressive symptoms are associated with perceived social position and some other health outcomes (e.g., Collins & Goldman, 2008), so a baseline measure of depressive symptoms was included in the analysis as a potential confounder. Second, controlling for baseline depressive symptoms in part helps to control for a predisposition to self-report positively or negatively about one’s circumstances, which may create a response bias that drives the correlation between perceived social position and the health outcomes.
Success
Success in 1993 was included in the analysis as a variable that only affected perceived social position in 2004 in order to help satisfy the rank and order conditions required to ensure that the parameter estimates in the reciprocal model could be estimated as distinct from one another (see discussion under Data analyses). Two items served as indicators of latent success in 1993: “To what extent have you been successful in work [finances]? Not at all successful, not very successful, somewhat successful, or very successful?” The responses were coded as 1=not at all successful through 4=very successful, so a higher score indicates that respondents perceive themselves as more successful.
Health characteristics
Smoking status and body mass index (BMI) in 1993 were included as controls for baseline health. Smoking status in 1993 was coded as 0=never smoked, 1=former smoker, and 2=current smoker. BMI in 1993 was calculated by weight (kg)/[height (m)] 2 (Centers for Disease Control and Prevention website, www.cdc.gov). The standard groupings are as follows: persons below 18.5 are underweight, 18.5 to 24.9 is normal weight, 25–29.9 is overweight, 30–34.9 is obese I, 35–39.9 is obese II, and 40 or more is obese III. There were very few persons who were underweight in this sample, so they were grouped with those in the normal weight range. There were also few respondents in the obese III category, so they were grouped with the obese II category, leaving four groups for analysis: 1=underweight/normal weight, 2=overweight, 3=obese I, and 4=obese II/III.
Socioeconomic Status
Educational attainment by 1975, occupation in 1993, and income in 1993 were included as controls for the more objective components of socioeconomic status. In order to help correct for measurement error, two indicators of respondent education were used to load on a latent education variable. These indicators were truncated at 18 years of schooling and came from reports of respondent educational attainment from respondents’ parents (1964) and respondents (1975). Occupation in 1993 was operationalized as occupational education, which is the proportion of an occupation’s incumbents who had one or more years of college education in the 1990 Census (Hauser and Warren, 1997). The proportion was transformed into a started logit in order to reduce heteroscedasticity in the variable without creating extreme outliers (Hauser and Warren, 1997; Mosteller and Tukey, 1977). Latent occupational education in 1993 was estimated with two indicators in order to account for measurement error: current occupational education in 1993 and respondent confirmation of their occupation in 1993 during the 2004 survey. Household income in 1993 was re-expressed as the natural log of the 1993 household income of the respondent after the addition of a small constant.
Demographic variables
Gender and marital status were included in the model as control variables. Gender was coded as 1=female and 0=male. Marital status in 1993 was coded as 1=married and 0=not married.
Data analyses
The values for missing data were derived from the multiple imputation technique of multivariate imputation by chained equations (MICE). Given that the analysis required use of several ordinal variables that were also not normally distributed, MICE was chosen to fill in missing data rather than other techniques (e.g., full information maximum likelihood) (see Allison [2003] for a review of these techniques). In order to account for the departures from multivariate normality associated with ordinal variables, the five imputed datasets were transformed into polychoric correlation and asymptotic covariance matrices and the models were estimated using weighted least squares estimation in Lisrel (Bollen, 1989; Jöreskog, 2005).
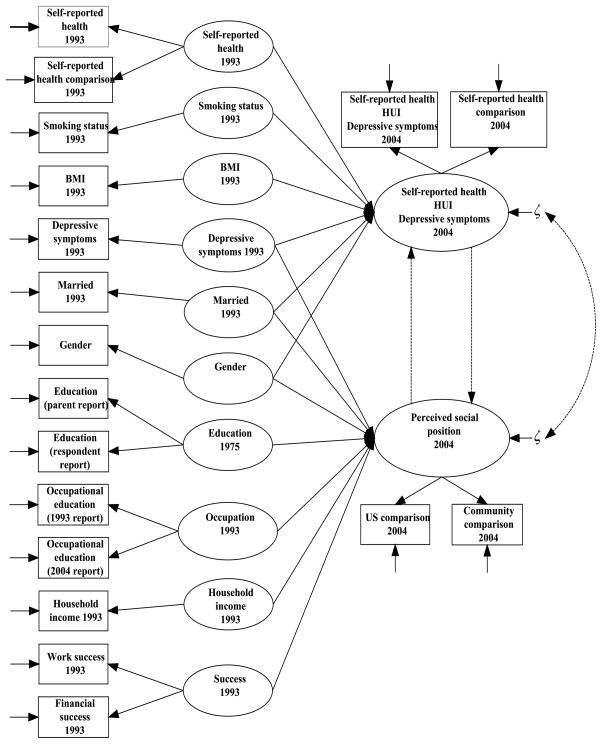
Figure 1 shows the structural equation models estimated in this analysis. All of the exogenous variables covaried with one another, and indicators for the endogenous variables varied depending on the health outcome and operationalization of perceived social position being modeled. When there was only one indicator for a latent variable, the error variance of the indicator was constrained to be zero and the path from the indicator to the factor was constrained to be 1 so that the properties of the indicator were transferred to the factor (Loehlin, 2004).
Figure 1.
Model of proposed relationships between health and perceived social position
In order to identify nonrecursive models for estimation, two conditions must be satisfied. The order condition requires that the number of unestimated direct effects on each endogenous variable is equal to or greater than the number of endogenous variables minus 1; the rank condition requires that each variable in a feedback loop has a unique pattern of direct effects on it from variables outside of the loop (Kline, 2005). In other words, at least one exogenous variable that affects one of the endogenous variables cannot affect the other endogenous variable, so that the parameters estimates in the feedback loop can be estimated as distinct from one another. Self-reported health and success in 1993 were included as exogenous variables in the model that affected only their 2004 counterparts, ensuring that the parameter estimates in the feedback loop could be estimated as distinct from one another.
The other health characteristics—smoking status and BMI in 1993—were included in the model in order to help control for baseline health status, and the socioeconomic characteristics—education, occupation, and income—were included in the model in order to control for baseline socioeconomic status, and it was expected that these variables would be free to affect both perceived social position and the health outcome of interest as controls. However, there was no improvement in model fit when the health characteristics from 1993 were allowed to affect perceived social position in 2004 and when the socioeconomic characteristics from 1993 were allowed to affect the health outcomes in 2004, so the baseline and subsequent models used in the analysis did not estimate these effects.
The baseline model (Model 1) estimated the relationships as described above but did not estimate a relationship between perceived social position and the health outcomes (none of the dashed paths in Figure 1 were estimated). Models 2–5 extended from Model 1 as indicated by the dashed paths: Model 2 estimated the effect of perceived social position on the health outcome, Model 3 estimated the effect of the health outcome on perceived social position, Model 4 estimated the effect of perceived social position on the health outcome and the health outcome on perceived social position as well as a disturbance covariance between the two constructs, and Model 5 estimated the same effects as Model 4 but constrained the reciprocal effects to be of equal size. The disturbance is the error/residual of each endogenous latent variable in the model, and a covariance between the disturbances of perceived social position and each health outcome represents a relationship between the two endogenous variables from at least one common cause that is not present in the model. The reciprocal models (Models 4 and 5) were estimated with a disturbance covariance between the two endogenous variables because if perceived social position and the health outcomes are presumed to mutually cause each other, it is expected that they have at least one common cause that is not present in the model in addition to the direct influence they have on one another (Kline, 2005; Loehlin, 2004; Wong and Law, 1999).
The Akaike Information Criterion (AIC) and hierarchical chi-square tests were used to choose the best-fitting model for each health outcome of interest and operationalization of perceived social position. AIC is a goodness-of-fit indicator that penalizes for sample size as well as model complexity and is used to compare nested and non-nested models; among models being compared, lower values of AIC indicate a better fit to the data (Loehlin, 2004; Kline, 2005). Hierarchical chi-square tests compare the chi-square goodness-of-fit statistics between two nested models (Loehlin, 2004).
Fit indices for each model and each path coefficient in the model were averaged across the five datasets. The coefficients yielded by the models are partial regression coefficients that indicate the change in the dependent variable per one unit change in the independent variable holding constant the relationships between variables as specified by the model. Because multiple imputation leads to the underestimation of the standard errors, the standard errors of the coefficients were averaged using Rubin’s (1987) formula that combines the estimated variability within replications and across replications with a small correction factor to the variance.
Results
This study explored the reciprocal relationship between three operationalizations of perceived social position and three health outcomes. Table 2 contains the fit statistics for the models being discussed. All of the models discussed had a root mean square error of approximation (RMSEA) between .03 and .04, one indication that globally, the models were a good fit to the data (Loehlin, 2004).
Table 2.
| Self-Reported Health |
Health Utilities Index |
Depressive Symptoms |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Chi-sqc | df | AIC | RMSEA | Chi-sq | df | AIC | RMSEA | Chi-sq | df | AIC | RMSEA | |
| Latent PSP | ||||||||||||
| Baseline | 613.29 | 83 | 846.49 | 0.031 | 493.61 | 68 | 697.61 | 0.032 | 503.32 | 68 | 705.32 | 0.032 |
| PSP→health | 571.97 | 82 | 785.97 | 0.031 | 475.13 | 67 | 681.13 | 0.032 | 489.29 | 67 | 693.29 | 0.032 |
| Health→PSP | 601.67 | 82 | 815.67 | 0.032 | 480.68 | 67 | 686.68 | 0.032 | 459.38 | 67 | 663.38 | 0.031 |
| Reciprocal | 560.54 | 80 | 778.54 | 0.031 | 465.89 | 65 | 675.89 | 0.032 | 457.75 | 65 | 665.75 | 0.031 |
| Equal reciprocal | 574.29 | 81 | 790.29 | 0.031 | 466.45 | 66 | 674.45 | 0.031 | 461.05 | 66 | 667.05 | 0.031 |
| US PSP | ||||||||||||
| Baseline | 594.21 | 68 | 798.21 | 0.036 | 428.05 | 54 | 624.05 | 0.034 | 432.89 | 54 | 626.89 | 0.033 |
| PSP→health | 514.69 | 67 | 720.69 | 0.033 | 414.12 | 53 | 612.12 | 0.033 | 424.83 | 53 | 620.83 | 0.033 |
| Health→PSP | 538.57 | 67 | 744.57 | 0.034 | 417.62 | 53 | 615.62 | 0.033 | 398.52 | 53 | 594.52 | 0.032 |
| Reciprocal | 496.72 | 65 | 706.72 | 0.033 | 403.57 | 51 | 605.57 | 0.034 | 397.16 | 51 | 597.16 | 0.033 |
| Equal reciprocal | 508.92 | 66 | 716.92 | 0.033 | 403.84 | 52 | 603.84 | 0.033 | 399.47 | 52 | 597.47 | 0.033 |
| Community PSP | ||||||||||||
| Baseline | 575.97 | 68 | 779.97 | 0.035 | 421.42 | 54 | 617.42 | 0.033 | 440.94 | 54 | 634.94 | 0.034 |
| PSP→health | 515.85 | 67 | 721.85 | 0.033 | 410.71 | 53 | 608.71 | 0.033 | 427.75 | 53 | 623.75 | 0.034 |
| Health→PSP | 525.48 | 67 | 731.48 | 0.033 | 409.32 | 53 | 607.32 | 0.033 | 388.27 | 53 | 584.27 | 0.032 |
| Reciprocal | 483.37 | 65 | 693.37 | 0.032 | 394.48 | 51 | 596.48 | 0.033 | 384.34 | 51 | 584.34 | 0.032 |
| Equal reciprocal | 501.37 | 66 | 709.37 | 0.033 | 396.19 | 52 | 596.19 | 0.033 | 385.27 | 52 | 583.27 | 0.032 |
Averaged across the five imputed datasets
Best-fitting models according to AIC are in bold
Chi-sq=Chi-square goodness-of-fit statistic, df= degrees of freedom, AIC=Akaike information criterion, RMSEA=root mean square error of approximation
AIC was used to determine the best-fitting model among the five models estimated for each health outcome and operationalization of perceived social position, and the chi-square difference tests were used to confirm that the model chosen by AIC was significantly different from hierarchically-related models. The lowest AIC value for a set of models is bolded in Table 2; the bolded values in Table 3 are the chi-square difference tests containing the model with the lowest AIC value in Table 2. In Table 3, a positive difference greater than the critical (p<.05) chi-square value listed denotes improvement in model fit when using the latter—less parsimonious—model; a positive difference less than the critical chi-square value means that the more parsimonious model should be retained.
Table 3.
| Model Comparisons | df difference | Latent PSP | US PSP | Community PSP |
|---|---|---|---|---|
| Self-reported health | ||||
| Baseline vs. PSP→health | 1 | 41.32 | 79.51 | 60.12 |
| PSP→health vs. reciprocal | 2 | 11.44 | 17.98 | 32.47 |
| PSP→health vs. equal reciprocal | 1 | −2.32 | 5.78 | 14.48 |
| Baseline vs. health→PSP | 1 | 11.63 | 55.64 | 50.48 |
| Health→PSP vs. reciprocal | 2 | 41.13 | 41.85 | 42.11 |
| Health→PSP vs. equal reciprocal | 1 | 27.37 | 29.65 | 24.12 |
| Equal reciprocal vs. reciprocal | 1 | 13.76 | 12.20 | 17.99 |
| Health utilities index | ||||
| Baseline vs. PSP→health | 1 | 18.48 | 13.93 | 10.71 |
| PSP→health vs. reciprocal | 2 | 9.24 | 10.55 | 16.23 |
| PSP→health vs. equal reciprocal | 1 | 8.68 | 10.28 | 14.52 |
| Baseline vs. health→PSP | 1 | 12.93 | 10.43 | 12.10 |
| Health→PSP vs. reciprocal | 2 | 14.79 | 14.05 | 14.84 |
| Health→PSP vs. equal reciprocal | 1 | 14.22 | 13.78 | 13.13 |
| Equal reciprocal vs. reciprocal | 1 | 0.57 | 0.27 | 1.71 |
| Depressive symptoms | ||||
| Baseline vs. PSP→health | 1 | 14.04 | 8.06 | 13.19 |
| PSP→health vs. reciprocal | 2 | 31.54 | 27.67 | 43.41 |
| PSP→health vs. equal reciprocal | 1 | 28.23 | 25.37 | 42.48 |
| Baseline vs. health→PSP | 1 | 43.94 | 34.38 | 52.67 |
| Health→PSP vs. reciprocal | 2 | 1.64 | 1.35 | 3.93 |
| Health→PSP vs. equal reciprocal | 1 | −1.67 | −0.95 | 3.00 |
| Equal reciprocal vs. reciprocal | 1 | 3.31 | 2.30 | 0.93 |
Chi-square critical value for 1 df difference is 3.84; 2 df difference 5.99 (p<.05). A positive difference greater than the critical (p<.05) chi-square value listed denotes improvement in model fit when using the latter—less parsimonious—model; a positive difference less than the critical chi-square value means that the more parsimonious model should be retained.
Important differences based on results from Table 2 are bolded (e.g., if Model 4 has lowest AIC, all difference tests with Model 4 are bolded)
Averaged across the five imputed datasets
Model 4 was the best-fitting model when the outcome of interest was self-reported health, indicating a reciprocal relationship between perceived social position and self-reported health where the reciprocal effects were not equal (Tables 2 and 3). However, this model appeared to be empirically underidentified when perceived social position was operationalized as latent or US perceived social position, meaning that the total effects (not shown) of self-reported health, smoking status and BMI in 1993 on perceived social position were substantively small and not significant, where it is expected that these variables should have significant total effects on perceived social position if the relationship between perceived social position and self-reported health in 2004 were truly reciprocal (Kenny, 1979; Kline, 2005). The empirical underidentification of the model was driven by the effect of self-reported health on latent and US perceived social position being close to zero and not significant. As a result, Model 2 was chosen as the model that best explains the relationship between self-reported health and latent and US perceived social position, because Model 2 does not estimate the path from self-reported health to perceived social position that led to the empirical underidentification in Model 4.
The endogenous effects of each best-fitting model are given in Table 4. For example, a one-unit increase in the community perceived social position (i.e., moving up one rung on the ladder) led to a .34 increase in self-reported health while a one-unit increase in self-reported health (i.e., moving from “good” to “very good,” for example) led to a .12 increase in community perceived social position, controlling for the rest of the model.
Table 4.
Estimated coefficients and R2 for perceived social position and health from each best-fitting modelab
| Health → PSP |
PSP → Health |
Disturbance Covariance |
Health R2 |
PSP R2 |
|
|---|---|---|---|---|---|
| Self-reported health | |||||
| Latent PSP | -- | 0.167**** | -- | 0.432 | 0.426 |
| US PSP | -- | 0.132**** | -- | 0.435 | 0.371 |
| Community PSP | 0.115** | 0.341**** | −0.280**** | 0.433 | 0.200 |
| Health utilities index | |||||
| Latent PSP | 0.165*** | 0.165*** | −0.177** | 0.158 | 0.395 |
| US PSP | 0.155*** | 0.155*** | −0.194** | 0.158 | 0.348 |
| Community PSP | 0.201*** | 0.201*** | −0.263** | 0.173 | 0.200 |
| Depressive symptoms | |||||
| Latent PSP | −0.210* | -- | -- | 0.635 | 0.420 |
| US PSP | −0.185 | -- | -- | 0.623 | 0.369 |
| Community PSP | −0.174* | -- | -- | 0.668 | 0.229 |
p<.05,
p<.01,
p<.001,
p<.0001
Coefficients averaged across 5 imputed datasets, standard errors adjusted according to Rubin (1987)
A reciprocal relationship best described the relationship between HUI and perceived social position for each operationalization of perceived social position. Model 5 was the best-fitting model when the health outcome was HUI, indicating that the relationship between HUI and perceived social position was reciprocal and the effects of HUI and perceived social position on one another were equal (Tables 2, 3 and 4).
Model 3 was the best-fitting model when the outcome of interest was having depressive symptoms, where having depressive symptoms affected perceived social position rather than the reverse or a reciprocal relationship (Tables 2 and 3). (The Model 5 AIC for depressive symptoms and community perceived social position was slightly lower than the Model 3 AIC, but the chi-square difference tests pointed to Model 3 as the better-fitting model of the two.) The effects of having depressive symptoms in 2004 on perceived social position were similar in magnitude for each operationalization of perceived social position, although not statistically significant for US perceived social position (Table 4).
Discussion
Perceived social position may be considered another component of SES that is subject to interplay with health across the life course. This study used structural equation models to empirically investigate the hypothesis that perceived social position and health are reciprocally related to one another, and found that the relationship between perceived social position and health differed across health outcomes as well as operationalizations of perceived social position.
The relationship between self-reported health and perceived social position depended on how perceived social position was operationalized. Latent and US perceived social position both had direct effects on self-reported health. There was a reciprocal relationship between self-reported health and community perceived social position, where the effect of community perceived social position on self-reported health was stronger than the reverse. Because people in one’s community are more visible and possibly more likely to be used as a frame of reference than the population of the United States in respondent health assessments, it is plausible that the significant reciprocal effect of self-reported health on community perceived social position was driven by a common frame of reference used to answer the items, given that one indicator of self-reported health asked about health compared to others the respondent’s age and sex.
This study is the first to establish that there is a relationship between perceived social position and HUI no matter how perceived social position was operationalized, and found that this association was reciprocal and that the effects of perceived social position and HUI on one another were equal. Finally, having depressive symptoms affected perceived social position, controlling for baseline depressive symptoms. This finding contrasts prior research which suggests that perceptions of social position affect depressive symptoms and that depressive symptoms may be a mediator in the relationship between perceived social position and other health outcomes (Collins & Goldman, 2008; Operario, Adler, & Williams, 2004).
However, having depressive symptoms was very stable across the two waves of data such that the effect of having depressive symptoms in 1993 on the 2004 measure was much larger than the effects of any of the exogenous variables on perceived social position (not shown). This led to an imbalance in the disturbances of the two endogenous variables, which may have allowed random error to have a greater effect on the estimates (Lorenz et al., 1995; Wong and Law, 1999). As a result, the findings for the depressive symptoms models should be interpreted with caution and future research should continue to examine the relationship between having depressive symptoms and perceived social position over multiple waves of data. (The effects of the exogenous variables on the endogenous variables and the disturbances in the self-reported health and HUI models are of the same magnitude.)
The analysis also provided evidence that the US and community comparison items may be indicators of the same underlying factor for this population. The US and community comparison items were highly correlated with one another, had an acceptable value for Cronbach’s alpha, and had adequate factor loadings on the same underlying factor in the model. However, it is important to note that the variance of the community comparison item explained by the models was lower than the variance explained by the US comparison item (Table 4), indicating differences between the US and community comparison items in terms of the variables associated with each item that were included (and not included) in the current set of models. Furthermore, the relationship between self-reported health and perceived social position differed depending on how perceived social position was operationalized. These facts suggest that the US and community comparison items should continue to be examined as distinct constructs before they are combined into an index or as indicators of the same latent construct.
Overall, the findings suggest that the causal relationship hypothesized in prior studies—that perceived social position affects health—does not necessarily hold in empirical models where reciprocal relationships are compared to alternative specifications using model fit criteria. Future studies should attempt to interrogate the relationship between perceived social position and health, rather than assume the direction of causality in their relationship, and should continue to consider the robustness and causal structure of the relationship between perceived social position and health across various health outcomes, populations, and stages of the life course.
Models of reciprocal relationships between cross-sectional constructs like the ones in this analysis require the assumption of equilibrium, meaning that the effects of each construct on the other are done going through the feedback process and in a steady state at the point of data collection (Kline, 2005). To the extent that perceived social position and health are not in a steady state at this time for this population, the results of this study may be tenuous. However, reciprocal relationships—if they exist—could be expected to be in equilibrium for this sample of adults who are close to the end of their working life course compared to a sample of younger adults, although this is an empirical question worthy of future investigation.
Future studies could assess the causal relationship between perceived social position and health using cross-lagged models with panel data where perceived social position and health constructs are measured at two points in time or more. Cross-lagged models may be preferable to reciprocal models in that the causes temporally precede the effects (health at time 1 affects perceived social position at time 2 and perceived social position at time 1 affects health at time 2), although the exact time lag required to see an effect of health on perceived social position or the reverse may be difficult to identify (Wong and Law, 1999). Recent longitudinal studies have found that controlling for baseline health status attenuates the effect of perceived social position on health (Collins & Goldman, 2008; Singh-Manoux, Marmot, & Adler, 2005), but baseline perceived social position has not been considered at the same time in a cross-lagged model. Unfortunately, the perceived social position items are only asked in the 2004 wave of the WLS, but investigation of cross-lagged relationships between perceived social position and health can and should be carried out using other datasets that have measures of perceived social position and health at more than one point in time.
One limitation of this analysis is that the measures of perceived social position and the health outcomes were constructed from respondent self-reports. To the extent that perceived social position and each health outcome were influenced by a predisposition to self-report positively or negatively about one’s circumstances, the correlation between perceived social position and health may have been driven by this response bias. The current analysis reduced this potential response bias in part by controlling for baseline depressive symptoms in 1993, to the extent that depressive symptoms are associated with a predisposition to report negatively about one’s circumstances and a lack of depressive symptoms is associated with a predisposition to report positively about one’s circumstances. This potential response bias could be eliminated by having independently ascertained measures of health (such as mortality), which this analysis does not use.
Finally, it should be noted that the results of this study are generalizable to a select population of white high school graduates who were employed when on the brink of older adulthood in the United States. In the WLS, everyone graduated from high school, whereas it is estimated that only 75 percent of the eligible population graduated from Wisconsin high schools in the late 1950s. Furthermore, roughly 70 percent of the sample currently resides in Wisconsin, and few of the WLS respondents are nonwhite (Sewell & Hauser, 1975; Sewell et al., 2004).
Acknowledgments
This research uses data from the Wisconsin Longitudinal Study (WLS) of the University of Wisconsin-Madison. Since 1991, the WLS has been supported principally by the National Institute on Aging (AG-9775 and AG-21079), with additional support from the Vilas Estate Trust, the National Science Foundation, the Spencer Foundation, and the Graduate School of the University of Wisconsin-Madison. A public use file of data from the Wisconsin Longitudinal Study is available from the Wisconsin Longitudinal Study, University of Wisconsin-Madison, 1180 Observatory Drive, Madison, Wisconsin 53706 and at http://www.ssc.wisc.edu/wlsresearch/data/. The opinions expressed herein are those of the author. The author thanks Theodore Gerber, Robert Hauser, and Nora Cate Schaeffer for their help with earlier versions of this project, and especially thanks three anonymous reviewers for their insightful comments.
Footnotes
Author Comments: An earlier version of this paper was presented at the 2008 meeting of the Population Association of America in New Orleans, Louisiana, US.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL. Socioeconomic status and health: The challenge of the gradient. American Psychologist. 1994;49(1):15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Adler NE, Epel ES, Castellazzo G, Ickovics JR. Relationship of subjective and objective social status with psychological and physiological functioning: Preliminary data in healthy white women. Health Psychology. 2000;19(6):586–592. doi: 10.1037//0278-6133.19.6.586. [DOI] [PubMed] [Google Scholar]
- Allison PD. Missing data techniques for structural equation models. Journal of Abnormal Psychology. 2003;112:545–557. doi: 10.1037/0021-843X.112.4.545. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. New York: Wiley; 1989. [Google Scholar]
- Cohen S, Alper CM, Doyle WJ, Adler N, Treanor JJ, Turner RB. Objective and subjective socioeconomic status and susceptibility to the common cold. Health Psychology. 2008;27(2):268–274. doi: 10.1037/0278-6133.27.2.268. [DOI] [PubMed] [Google Scholar]
- Demakakos P, Nazroo J, Breeze E, Marmot M. Socioeconomic status and health: The role of subjective social status. Social Science & Medicine. 2008;67(2):330–340. doi: 10.1016/j.socscimed.2008.03.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan GJ, Daly MC, McDonough P, Williams DR. Optimal indicators of socioeconomic status for health research. American Journal of Public Health. 2002;92(7):1151–1157. doi: 10.2105/ajph.92.7.1151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn JR, Veenstra G, Ross N. Psychosocial and neo-material dimensions of SES and health revisited: Predictors of self-rated health in a Canadian national survey. Social Science & Medicine. 2006;62(6):1465–1473. doi: 10.1016/j.socscimed.2005.07.038. [DOI] [PubMed] [Google Scholar]
- Franzini L, Fernandez-Esquer ME. The association of subjective social status and health in low-income Mexican-origin individuals in Texas. Social Science & Medicine. 2006;63(3):788–804. doi: 10.1016/j.socscimed.2006.01.009. [DOI] [PubMed] [Google Scholar]
- Gianaros PJ, Horenstein JA, Cohen S, Matthews KA, Brown SM, Flory JD, Critchley HD, Manuck SB, Hariri AR. Perigenual anterior cingulate morphology covaries with perceived social standing. Social Cognitive and Affective Neuroscience. 2007;2:161–173. doi: 10.1093/scan/nsm013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman E, McEwen BS, Dolan LM, Schafer-Kalkhoff T, Adler NE. Social disadvantage and adolescent stress. Journal of Adolescent Health. 2005;37(6):484–492. doi: 10.1016/j.jadohealth.2004.11.126. [DOI] [PubMed] [Google Scholar]
- Haan MN, Kaplan GA, Syme SL. Pathways to health: The role of social factors. Menlo Park, CA: Henry J. Kaiser Family Foundation; 1989. [Google Scholar]
- Hauser RM, Warren JR. Socioeconomic indexes of occupational status: A review, update, and critique. In: Raftery A, editor. Sociological Methodology. Cambridge: Blackwell; 1997. pp. 177–298. [Google Scholar]
- Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index(HUI®): Concepts, measurement properties and applications. Health and Quality of Life Outcomes. 2003;1(1):54–66. doi: 10.1186/1477-7525-1-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- House JS, Williams DR. Understanding and reducing socioeconomic and racial/ethnic disparities in health. In: Smedley BD, Syme SL, editors. Promoting health: Intervention strategies from social and behavioral research. Washington, DC: National Academy Press; 2000. pp. 81–124. [Google Scholar]
- Hu P, Adler NE, Goldman N, Weinstein M, Seeman TE. Relationship between subjective social status and measures of health in older Taiwanese persons. Journal of the American Geriatric Society. 2005;53(3):483–488. doi: 10.1111/j.1532-5415.2005.53169.x. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Jöreskog KG. Structural equation modeling with ordinal variables using LISREL. 2005 http://www.ssicentral.com/lisrel/techdocs/ordinal.pdf.
- Kenny DA. Correlation and causality. New York: Wiley; 1979. [Google Scholar]
- Kitagawa EM, Hauser PM. Differential mortality in the United States: A study in socioeconomic epidemiology. Cambridge, MA: Harvard University Press; 1973. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. New York: The Guilford Press; 2005. [Google Scholar]
- Kopp M, Skrabski A, Rethelyi J, Kawachi I, Adler NE. Self-rated health, subjective social status, and middle-aged mortality in a changing society. Behavioral Medicine. 2004;30(2):65–70. doi: 10.3200/BMED.30.2.65-72. [DOI] [PubMed] [Google Scholar]
- Kroenke C. Socioeconomic status and health: Youth development and neomaterialist and psychosocial mechanisms. Social Science & Medicine. 2008;66(1):31–42. doi: 10.1016/j.socscimed.2007.07.018. [DOI] [PubMed] [Google Scholar]
- Link BG, Phelan J. Social conditions as fundamental causes of disease. Journal of Health and Social Behavior. 1995;(Extra Issue):80–94. [PubMed] [Google Scholar]
- Loehlin JC. Latent variable models: An introduction to factor, path, and structural equation analysis. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- Lorenz FO, Conger RD, Simons RL, Whitbeck LB. The effects of unequal covariances and reliabilities on contemporaneous inference: The case of hostility and marital happiness. Journal of Marriage and the Family. 1995;57:1049–1064. [Google Scholar]
- McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–48. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- Marmot MG, Shipley MJ, Rose G. Inequalities in death--specific explanations of a general pattern? Lancet. 1984;5(1):1003–1006. doi: 10.1016/s0140-6736(84)92337-7. [DOI] [PubMed] [Google Scholar]
- Miech RA, Hauser RM. Working Paper 98–06. Madison, WI: Center for Demography and Ecology; 1998. Social class indicators and health at midlife. [Google Scholar]
- Mosteller F, Tukey JW. Data Analysis and Regression. Reading, MA: Addison-Wesley Publishing Company; 1977. [Google Scholar]
- Operario D, Adler NE, Williams DR. Subjective social status: reliability and predictive utility for global health. Psychology and Health. 2004;19(2):237–246. [Google Scholar]
- Ostrove JM, Adler NE, Kuppermann M, Washington AE. Objective and subjective assessments of socioeconomic status and their relationship to self-rated health in an ethnically diverse sample of pregnant women. Health Psychology. 2000;19(6):614–618. doi: 10.1037//0278-6133.19.6.613. [DOI] [PubMed] [Google Scholar]
- Palloni A. Reproducing inequalities: Luck, wallets, and the enduring effects of childhood health. Demography. 2006;43(4):587–615. doi: 10.1353/dem.2006.0036. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: Wiley; 1987. [Google Scholar]
- Sapolsky RM. Social status and health in humans and other animals. Annual Review of Anthropology. 2004;33(1):393–418. [Google Scholar]
- Sewell WH, Hauser RM. Education, Occupation, and Earnings: Achievement in the Early Career. New York: Academic; 1975. [Google Scholar]
- Sewell WH, Hauser RM, Springer KS, Hauser TS. As we age: The Wisconsin Longitudinal Study, 1957–2001. In: Leicht K, editor. Research in social stratification and mobility. Vol. 20. London: Elsevier; 2004. pp. 3–111. [Google Scholar]
- Singh-Manoux A, Adler NE, Marmot MG. Subjective social status: Its determinants and its association with measures of ill-health in the Whitehall II study. Social Science and Medicine. 2003;56:1321–1333. doi: 10.1016/s0277-9536(02)00131-4. [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot MG, Adler NE. Does subjective social status predict health and change in health better than objective status? Psychosomatic Medicine. 2005;67:855–861. doi: 10.1097/01.psy.0000188434.52941.a0. [DOI] [PubMed] [Google Scholar]
- Snibbe AC, Stewart J, Adler NE. Where do I stand? How people determine their subjective socioeconomic status. 2007 in preparation. http://www.macses.ucsf.edu/Research/Psychosocial/notebook/subjective.html.
- Tourangeau R, Rips LJ, Rasinski K. The psychology of survey response. Cambridge, UK: Cambridge University Press; 2000. [Google Scholar]
- Wilkinson RG. Unhealthy societies: The afflictions of inequality. London: Routledge; 1996. [Google Scholar]
- Wilkinson RG. Health, hierarchy, and social anxiety. In: Adler NE, Marmot M, McEwan BS, Stewart J, editors. Socioeconomic status and health in industrial nations: Social, psychological, and biological pathways. New York: New York Academy of Sciences; 1999. pp. 48–63. [DOI] [PubMed] [Google Scholar]
- Wong CS, Law KS. Testing reciprocal relations by nonrecusrive structural equation models using cross-sectional data. Organizational Research Methods. 1999;2:69–87. [Google Scholar]
- Wright CE, Steptoe A. Subjective socioeconomic position, gender, and cortisol responses to waking in an elderly population. Psychoneuroendocrinology. 2005;30(6):582–590. doi: 10.1016/j.psyneuen.2005.01.007. [DOI] [PubMed] [Google Scholar]