Abstract
Mutations in the angiopoietin receptor TIE2/TEK have been identified as the cause for autosomal dominantly inherited cutaneomucosal venous malformation (VMCM). Thus far, two specific germline substitutions (R849W and Y897S), located in the kinase domain of TIE2, have been reported in five families. The mutations result in a fourfold increase in ligand-independent phosphorylation of the receptor. Here, we report 12 new families with TEK mutations. Although the phenotype is primarily characterized by small multifocal cutaneous vascular malformations, many affected members also have mucosal lesions. In addition, cardiac malformations are observed in some families. Six of the identified mutations are new, with three located in the tyrosine kinase domain, two in the kinase insert domain, and another in the carboxy terminal tail. The remaining six are R849W substitutions. Overexpression of the new mutants resulted in ligand-independent hyperphosphorylation of the receptor, suggesting this is a general feature of VMCM-causative TIE2 mutations. Moreover, variation in the level of activation demonstrates, to the best of our knowledge for the first time, that widely differing levels of chronic TIE2 hyperphosphorylation are tolerated in the heterozygous state, and are compatible with normal endothelial cell function except in the context of highly localized areas of lesion pathogenesis.
Keywords: angiogenesis, vascular anomaly, VMCM, genetic, TEK, hyperphosphorylation.
Introduction
Venous malformation (VM) is the most frequent malformation referred to specialized vascular anomaly centers.1, 2, 3 Although most VMs are sporadic (95%), they can be inherited as an autosomal dominant trait. Glomuvenous malformation (GVM, OMIM # 138 000) is the most common familial type, histologically characterized by abnormal mural glomus cells. GVM is caused by loss-of-function mutations in glomulin.4, 5 A less common, inheritable form is cutaneomucosal venous malformation (VMCM, OMIM # 600 195).6 VMCMs tend to be multifocal and small.7 They are comprised of grossly dilated vascular spaces that are lined by a single continuous layer of endothelial cells, with areas of relative lack of surrounding mural cells, suggesting a defect in their recruitment.8, 9 A genetic approach led to the identification of a mutation in the endothelial-specific tyrosine kinase, TIE2, in two families with VMCM.8 Later, this same R849W mutation (c.2545C>T) was found in two other families, and a Y897S mutation (c.2690A>C) in a fifth family.9, 10 When overexpressed, both induce a weak (four-to sixfold) increase in ligand-independent tyrosine phosphorylation of the TIE2 receptor.8, 9
We report 12 new families with VMCM. In six, we identified the R849W substitution, whereas in the other six, we discovered new mutations. All new changes resulted in ligand-independent hyperphosphorylation of the receptor when overexpressed in Cos-7 cells. Interestingly, although two mutations showed hyperphosphorylation comparable with R849W, four others had far stronger effects. This demonstrates that a wide range of activating TIE2 mutations cause VMCM, with no apparent correlation between level of hyperphosphorylation and phenotype. Patients typically had small bluish-purple multifocal cutaneous lesions that were soft on palpation and compressible. The frequent presence of mucosal lesions helps to differentiate VMCM from GVM, in which such lesions are rare.
Materials and methods
Patients
Informed consent was obtained from all family members before participation in the study, as approved by the ethics committee of the Medical Faculty of Université catholique de Louvain. We collected 26 blood samples from 12 families with venous malformations. Clinical information was collected by the clinicians responsible for the patients (LMB, JBM, EB, JB, AD, OE, SAI, LK, YL, AST, AP and PR).
DNA screening and mutation segregation
DNA was obtained from whole blood using the Puregene DNA extraction kit (Gentra, Minneapolis, MN, USA). The TEK gene was screened for mutations using denaturing high performance liquid chromatography (DHPLC). In brief, 23 exons and flanking (5′ and 3′) intronic sequences of TIE2 were amplified. PCR products were denatured at 94 °C for 5 min and slowly cooled down to 20 °C. DHPLC screening was performed using WAVE DNA fragment analysis system (Transgenomic, Omaha, NE, USA) with a DnaSep column and a ‘rapid DNA' method. Samples with elution patterns different from controls were purified with Qiaquick PCR purification kit (Qiagen, Valencia, CA, USA) and sequenced using a CEQ 2000 capillary sequencer (Beckman, Fullerton, CA, USA). Segregation of the six novel mutations was assessed by sequencing and/or allele-specific PCR (AS-PCR). Conditions for the c.2545C>T (R849W) AS-PCR have been described previously.8
mRNA analysis
To determine the effect of the 3300G>C nucleotide change (p.K1100N; family VM-55, Figure 1 and Table 1), RNA from lymphoblasts was extracted using Tripure (Roche, Basel, Switzerland) with the recommended protocol. cDNA was synthesized using iScript cDNA Synthesis Kit (Bio-Rad, Hercules, CA, USA) using 1 μg of total RNA. To assay for the expression of the mutant allele in lymphoblast cDNA of patients VM-55.II.1 and VM-55.III.1, a region covering the last six exons was amplified and sequenced, using primers in exon 18 (5′-GATTGTCCCGAGGTCAAGAGG-3′) and the 3′ UTR in exon 23 (5′- CCCTTGACAACTGCTGAGAA-3′), using regular cycling conditions and an annealing temperature of 57 °C.
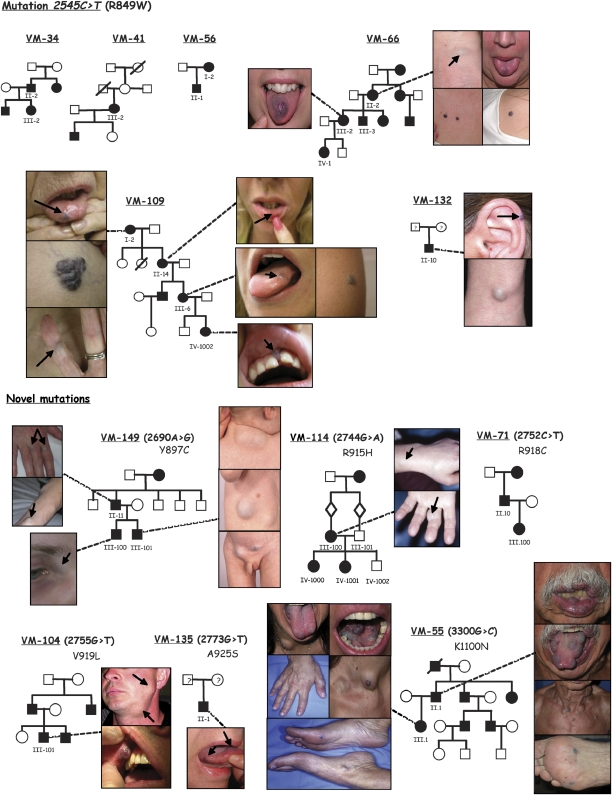
Figure 1.
Pedigrees of 12 families with cutaneomucosal venous malformation (VMCM), in order of occurrence of TIE2 mutations, with the shared c.2545C>T (R849W) mutation shown first. Numbers: participating members; black symbols: affected individuals. Selected clinical pictures show variability in size, number and location of VMCMs. Mucosal lesions (tongue or lip) in VM-66.II.2, VM-66.III.2, VM-109.I.2, VM-109.II.14, VM-109.III.6, VM-109.IV.1002, VM-104.III.101, VM-135.II.1, VM-55.II.1 and VM-55.III.1.
Table 1. Clinical description of patients with a TIE2 mutation, in order of mutated amino acid.
| Size of lesion(s) | Localization of lesion(s) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Family | Individual | Mutation | Sex | No. of lesions | Localized | Extensive | Mucosa | Head/ neck | Trunk | Limbs | Internal organs | D-dimer level | Other anomalies |
| VM-34 | VM-34.II.2 | p.R849W | M | 1 | 1 | 1 | NDa | ||||||
| VM-34.III.2 | p.R849W | F | 4 | 2 | 2 | 1 | 1 | 2 | NDa | ||||
| VM-41 | VM-41.III.2 | p.R849W | F | 11 | 11 | 1 | 7 | 1 | 1 | 2 (lung) | Normal | ||
| VM-56 | VM-56.I.2 | p.R849W | F | 9 | 9 | 2 | 3 | 4 | NDa | ||||
| VM-56.II.1 | p.R849W | M | 3 | 3 | 1 | 2 | NDa | ||||||
| VM-66 | VM-66.II.2 | p.R849W | F | 8 | 8 | 2 | 2 | 3 | 1 | Normal | |||
| VM-66.III.2 | p.R849W | F | 2 | 2 | 1 | 1 | Normal | ||||||
| VM-66.III.3 | p.R849W | M | 1 | 1 | 1 | Normal | |||||||
| VM-66.IV.1 | p.R849W | F | 1 | 1 | 1 | Normal | |||||||
| VM-109 | VM-109.I.2 | p.R849W | F | 6 | 6 | 1 | 2 | 3 | NDa | ||||
| VM-109.II.14 | p.R849W | F | 5 | 5 | 1 | 4 | Brain | NDa | Retro-ocular mass | ||||
| VM-109.III.6 | p.R849W | F | 11 | 11 | 1 | 3 | 7 | NDa | |||||
| VM-109.IV.1002 | p.R849W | F | 2 | 2 | 1 | 1 | 1 | NDa | Facial asymmetry, strabismus | ||||
| VM-132 | VM-132.II.10 | p.R849W | F | 5 | 2 | 1 | 3 | 1 | NDa | ||||
| VM-149 | VM-149.II.11 | p.Y897C | M | > 31 | > 31 | 12 | 3 | 16 | Intestine, kidney, thorax | Elevated | |||
| VM-149.III.100 | p.Y897C | M | > 15 | >15 | 2 | 1 | 11 | Intestine | Elevated | ||||
| VM-149.III.101 | p.Y897C | M | > 30 | 25–30 | 1–2 | 1 | 5–10 | > 28 | Intestine, brain | Elevated | Factor XIII deficiency | ||
| VM-114 | VM-114.III.100 | p.R915H | F | 4 | 4 | 2 | 2 | Elevated | VSDb | ||||
| VM-114.IV.1000 | p.R915H | F | 1 | 1 | 1 | NDa | VSDb | ||||||
| VM-114.IV.1001 | p.R915H | F | 2 | 2 | 1 | 1 | NDa | VSDb | |||||
| VM-71 | VM-71.II.10 | p.R918C | M | 2 | 2 | >1 | 1 | NDa | |||||
| VM-71.III.100 | p.R918C | F | 4 | 4 | 1 | 2 | 1 | NDa | |||||
| VM-104 | VM-104.III.101 | p.V919 L | M | 3 | 3 | 1 | 2 | Elevated | Cardiac murmur (spontaneously converted) | ||||
| VM-135 | VM-135.II.1 | p.A925S | F | 2 | 2 | 2 | Normal | ||||||
| VM-55 | VM-55.II.1 | p.K1100N | M | >25 | all except 1 | 1 | 9–12 | 9 | 6 | Normal | |||
| VM-55.III.1 | p.K1100N | F | >50 | all except 2 | 2 | 5–6 | 5 | 5 | >35 | Normal | Uterine myomas, VSDb | ||
ND=not determined.
VSD=ventricular septal defect.
Haplotype analysis
To determine the haplotypes segregating with the R849W mutation, nine microsatellite markers flanking the TIE2 gene were genotyped (www.genome.ucsc.edu/): D9S171, D9S126, D9S169, D9S161, D9S104 and four new dinucleotide markers (BV724037, BV724038, BV724039 and BV724040) generated in our laboratory. The markers were analyzed radioactively, as described previously.11 Altogether, 18 affected individuals from five unrelated families were analyzed. These included five affected members of family Sa, reported previously.8
Computational analysis
Each nucleotide change identified in the coding regions of TIE2 was assessed as follows: dbSNP and dbEST (http://www.ncbi.nlm.nih.gov/SNP/ and http://www.ncbi.nlm.nih.gov/dbEST/) were searched for corresponding polymorphisms. Mutation-resultant amino-acids changes were submitted to PANTHER (www.pantherdb.org) and POLYPHEN (http://genetics.bwh.harvard.edu/pph/) to estimate the likelihood of a functional impact on the protein, on the basis of position-specific evolutionary conservation in related proteins. RESCUE-ESE (Exonic Splicing Enhancer, http://genes.mit.edu/burgelab/rescue-ese/) was used to predict any splice-alterating effects.
TIE2 expression constructs
The 3.5-kb coding sequence of human TIE2, along with 50 bp of the 5′ and 60 bp of the 3′ UTR, was cloned between the XhoI and NotI sites of the expression vector pcDNA3.1/Zeo(−) (Invitrogen, Carlsbad, CA, USA). To generate mutants in vitro, site-directed mutagenesis was carried out. Briefly, a region of wild-type TIE2 (up to 1 kb, flanked by unique restriction sites) surrounding the mutation was cloned into the pCR-II TOPO vector (Invitrogen). This clone was used as template for a long-range PCR, using a forward primer containing the nucleotide change 7–8 bp from the 5′ end, in combination with a reverse primer located just before the 5′ end of the forward primer, with no gap in sequence between them. After purification (using Qiaquick PCR purification kit, Qiagen), the amplicon was phosphorylated using T4 polynucleotide kinase (forward reaction; Fermentas, Burlington, Canada), and the ends were ligated using T4 DNA ligase (Invitrogen), re-creating a circular construct that was transfected into JM109 competent bacteria (Promega, Madison, WI, USA) by heat shock. The region containing the created mutation was cut and inserted into the full-length TIE2 sequence in the expression vector using unique, flanking restriction sites within TIE2. All constructs were sequence verified.
Cell culture, transfection and western blot analysis
Cos-7 cells were cultured at 37°C under 5% CO2 in Dulbecco's modified Eagle's medium (DMEM; Invitrogen), supplemented with 10% (v/v) fetal bovine serum (Invitrogen), and penicillin G (100 U/ml) and streptomycin (100 μg/ml) (Cambrex Bioscience, Charles City, IA, USA). Transfections were carried out using jetPEI (Polyplus-transfections SA, Illkirch, France), according to manufacturer's instructions. After 24 h, cells were washed with ice-cold PBS, and lysed in cold lysis buffer ((20 m HEPES (pH 7.8), 75 m KCl, 0.1 m EDTA, 2 m MgCl2, 1 m DTT, 10% glycerol, 0.5% Triton-X 100, 1 tablet of Complete Protease Inhibitor and 2 tablets of PhosStop phosphatase inhibitor tablets (Roche) per 20 ml). Lysates were subjected to sonication and spun at 13 000 g to remove debris. Supernatants were resolved by denaturing SDS-polyacrylamide gel electrophoresis and immunoblotted using an anti-phosphotyrosine antibody ((PY99; Santa Cruz Biotechnology, Santa Cruz, CA, USA) at 1:500 dilution, or anti-phospho-Tie2(1102/1108) (Ab-1; Calbiochem, San Diego, CA, USA) at 1:2500 dilution in separate blots for confirmation), and stripped and re-probed with anti-TIE2 antibody (C-20; Santa Cruz Biotechnology) at 1:500 dilution. C-20 is a polyclonal antibody raised against a 20-amino-acid peptide mapping to the 50 most C-terminal residues (1071–1122) of mouse Tie2. Immunoreactive proteins were visualized using goat anti-rabbit-HRP secondary antibody, at 1:25 000 dilution, for C-20 and Ab-1 (Biosource, Carlsbad, CA, USA) or goat anti-mouse-HRP at 1:20 000 dilution for PY99 (Biosource), using a femto-range-sensitive ECL system (Pierce, Rockford, IL, USA). Densitometric image quantification was carried out using ImageJ (http://rsb.info.nih.gov/ij/), and the average fold-difference of TIE2 phosphorylation (normalized to total TIE2) for each mutant over wild-type TIE2, observed across at least three separate blots, were calculated. Each set of mutants, and the wild type to be compared with, were run on the same gel.
Results
Phenotype of patients
Table 1 summarizes the clinical details of individuals with VMCM (n=26). Cutaneous lesions were mostly located in the cervicofacial region (18 of 26) and/or limbs (21 of 26), and less often on the trunk (9 of 26). Lesions on the lip, tongue and buccal mucosa were frequent (15 of 26). Lesions were generally small (< 5 cm), and over 80% of patients had multiple lesions (>2). Some patients had additional anomalies. In three families, affected members had cardiac defects. In VM-114 and VM-55, four patients had a restrictive perimembranous ventricular septal defect (VSD) and two had exertional dyspnea. Doppler ultrasonography showed high velocity from left-to-right ventricle and slight dilatation of the left auricle in all three VM-affected individuals from VM-114. VM-104.III.101 had a spontaneously converted cardiac murmur, and according to family history, his sister had a heart–lung transplantation and his father was operated for a cardiac valve problem.
Some individuals had VMs located in internal organs. In patient 41.III.2, VMs were present in the apex of both lungs, whereas members of family VM-149 had gastro-intestinal, thoracic, renal and brain lesions. Severe and episodic bleeding occurred in patient VM-149.III.101, who had a factor XIII deficiency. Localized intravascular coagulopathy (LIC) was documented in 5 of 13 patients by elevated D-dimers.
Mutational analysis of TIE2
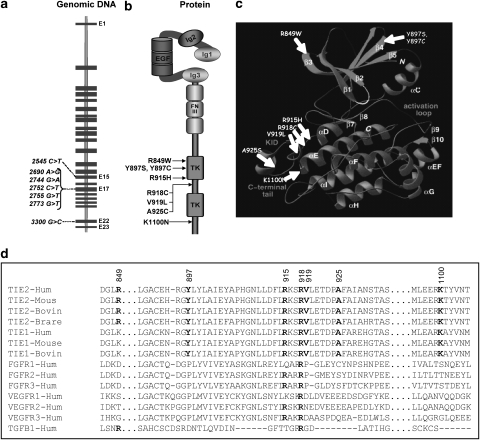
We identified a mutation in 26 of 28 individuals screened from 12 unrelated families with inherited VMs (Figure 1). Unaffected individuals III.101 and IV.1002 from family VM-114 did not have a mutation. The missense mutations were located in exons 15, 17 and 22: c.2545C>T (R849W), c.2690A>G (Y897C), c.2744G>A (R915H), c.2752C>T (R918C), c.2755G>T (V919L), c.2773G>T (A925S) and c.3300G>C (K1100N) (Figure 2a). All mutations were located in the intracellular part of TIE2: R849W, Y897C and R915H in the first tyrosine kinase domain (TK1); R918C, V919L and A925S in the kinase insert domain (KID); and K1100N in the C-terminal tail (Figure 2b–d).
Figure 2.
TIE2 mutations. (a) Genomic structure of TIE2 composed of 23 exons. The c.2545C>T in exon 15; 5 of 6 new mutations in exon 17 and c.3300G>T in the last nucleotide of exon 22. (b) Schematic representation of TIE2 with cutaneomucosal venous malformation (VMCM) mutations: extracellular domain with three immunoglobulin-like loops (Ig1, Ig2 and Ig3) separated by three epidermal growth factor-like repeats (EGF) connected to three fibronectin type III-like repeats (FN III). Intracellular part contains two tyrosine kinase domains (TK) separated by kinase insert domain (KID). (c) Three-dimensional representation of TIE2 intracellular domain with: first TK domain: R849(W), Y897(S) and (C), R915(H); KID: R918(C), V919(L) and A925(S); and C-terminal tail: K1100(N). Figure was prepared using PDB viewer. (d) Conservation of Y897, R915, R918, V919, A925 and K1100 in TK receptors between species (www.ebi.ac.uk/clustalw/).
Predicted effect of mutations
The nucleotide changes are absent in SNP and EST databases. PANTHER and POLYPHEN analyses predicted a deleterious effect for amino-acid changes R849W, Y897C, R915H, R918C, A925S and K1100N, whereas the V919L substitution was predicted to be benign (Table 2). Nucleotide change 3300G>C (K1100N) was located at the end of exon 22. RESCUE-ESE predicted the creation of an exonic splice-enhancer sequence. We re-amplified a region encompassing the K1100N change (spanning several introns: from exons 18 to 23) from lymphoblast cDNA (lesion-derived tissue being unavailable) from both patients: VM-55.II.1 and 55.III.1. No extraneous bands were amplified from patient cDNA, and on sequencing the normal-sized band, we found the mutant allele in both samples (data not shown).
Table 2. Predictions of functional effects of TIE2 mutations.
| Exon | Nt change | AA change | Predicted effect | dbSNP | dbEST | dbESE | POLYPHEN | PANTHER (subPSEC value)b |
|---|---|---|---|---|---|---|---|---|
| 15 | c.2545C>Ta | p.R849W | Missense | Absent | Absent | No change | Possibly damaging | High probability of deleterious effect (−4.93) |
| 17 | c.2690A>Ca | p.Y897S | Missense | Absent | Absent | No change | Probably damaging | High probability of deleterious effect (−3.77) |
| c.2690A>G | p.Y897C | Missense | Absent | Absent | No change | Probably damaging | High probability of deleterious effect (−4.96) | |
| c.2744G>A | p.R915H | Missense | Absent | Absent | No change | Possibly damaging | High probability of deleterious effect (−4.25) | |
| c.2752C>T | p.R918C | Missense | Absent | Absent | No change | Probably damaging | High probability of deleterious effect (−5.33) | |
| c.2755G>T | p.V919 L | Missense | Absent | Absent | No change | Benign | Unlikely deleterious effect (−2.07) | |
| c.2773G>T | p.A925S | Missense | Absent | Absent | No change | Benign | Possible deleterious effect (−2.51) | |
| 22 | c. 3300G>C | p.K1100N | Splicing or missense | Absent | Absent | (+) 1 | Possibly damaging | Possible deleterious effect (−3.4) |
c.2545C>T and c.2690A>C are the inherited mutations identified by Vikkula et al (1996) and Calvert et al (1999), respectively.
SubPSEC=substitution position-specific evolutionary conservation (< −3.5=high probability of deleterious functional effect; −2.5–3.5=possible deleterious functional effect; −2.5–2.5=unlikely functional effect; 2.5–3.5=possible gain-of-function effect; > 3.5=high probability of gain-of-function effect).
Haplotypes around the common R849W mutation
R849W has been described in four families, and was identified in six new families in this study. To establish whether it originates from a common ancestral allele, we determined the haplotype associated with the mutant allele in 18 carriers from six families (patients VM-34.II.2, VM-34.III.2, VM-41.III.2, VM-56.I.2, VM-56.II.2, VM-66.II.2, VM-66.III.2, VM-66.III.3, VM-66.IV.1, VM-109.I.2, VM-109.II.14, VM-109.III.6, VM-109.IV.1002, and the previously described Sa-1, Sa-2, Sa-3, Sa-4 and Sa-5 8). A small, possibly common, haplotype was identified in VM-families 22, 34, 41 and 109 (Supplementary Table 1); however, VM-56 and VM-66 did not share this haplotype.
Ligand-independent hyperphosphorylation of mutant TIE2 receptors
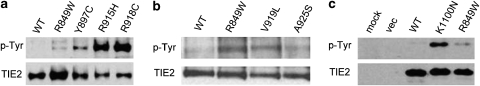
All VMCM-causing substitutions resulted in ligand-independent hyperphosphorylation of TIE2 (Figure 3a–c). The increased autophosphorylation of V919L and A925S mutants was weak (Figure 3b), similar to the increase shown for R849W (two- to fourfold on average), whereas Y897C, R915H and R918C induced much higher levels of receptor hyperphosphorylation (an average of 13-, 29- and 30-fold, respectively; Figure 3a), as did the C-terminal K1100N (an average of sevenfold; Figure 3c).
Figure 3.
Receptor phosphorylation in Cos-7 cells. (a–c) Western blots of lysates from Cos-7 cells overexpressing WT and mutant TIE2 receptors (140 kD): R849W, Y897C, R915H and R918C (a); weakly-phosphorylating mutations V919L and A925S (b); and K1100N (c), probed with anti-phosphotyrosine antibodies (upper panels), and stripped and re-probed with anti-TIE2 antibody for total TIE2 expression (lower panels). Negative control lysates from mock- and empty vector-transfected cells also included.
Discussion
We performed molecular analysis on 12 new families with VMCM. All affected members had cutaneous and/or mucosal venous lesions located in the head and neck, limbs and trunk. Most lesions were multifocal and small (< 5 cm in diameter); a few larger lesions of several centimeters in diameter were observed. The frequent observation of a lesion on the tongue, lip and/or buccal mucosa underscores the importance of lesions in these sites as clues for the correct diagnosis. Localized intravascular coagulopathy (LIC), characterized by elevated D-dimer levels, was observed in some patients. This seems to be associated with the overall lesion volume, similar to sporadic unifocal VMs,12, 13 although rarely, it can accompany smaller lesions.
Most lesions were seen at birth, some appeared during childhood or adulthood. Although symptomatic visceral lesions are uncommon in VMCM, they do occur. One patient carrying the R849W change had a pulmonary malformation. Three others, with the Y897C mutation, had intestinal, thoracic, renal and/or cerebral lesions (Table 1). The Y897C mutation might thus be particularly strong in predisposing to visceral lesions, although a Japanese patient with the R849W mutation was also reported to have cutaneous and intestinal VMs associated with a pancreatic ‘lymphatic malformation'.10
Although cardiac septal defects are frequent in the general population, TIE2 mutations may have a predisposing effect and an important function in cardiac development, as indicated by phenotypes of murine models with altered TIE2 signaling.14 In two families, with R915H and K1100N mutations, respectively, VMCM was associated with restrictive VSD. The VMCM-unaffected, TIE2 mutation-negative members of these families (from whom DNA was available for analysis) did not have VSDs. Another patient (with V919L) had a spontaneously converted cardiac murmur. Nevertheless, screening for germline TIE2 mutations in patients with atrial or ventral septal defects (ASD or VSD) did not identify any changes (Gutierrez-Roelens et al, personal communication).
Our mutational screen identified the activating R849W mutation in six of the new VMCM families. Altogether, 10 families are now known to carry this substitution. Haplotype analysis did not support the hypothesis that this change is due to a single common ancestral allele. The c.2545C>T residue is probably a hot-spot region for mutations, as the C-to-T substitution is the most common single nucleotide change, caused by the deamination of cytosine residues in CpG dinucleotides. We also identified six new amino acid changes. The Y897C mutation induced a ∼13-fold increase in ligand-independent receptor phosphorylation as compared with the wild-type receptor. Another substitution in this residue (Y897S) has been previously reported to induce hyperphosphorylation similar to R849W.8, 9 Tyrosine 897 is a phosphorylation site and negatively regulates TIE2 activation by preventing dimerization of the kinase domains or by recruiting phosphatases.15 This inhibition seems to be lost to differing degrees with various mutations affecting Y897.
Three of the new mutations (R918C, V919L and A925S) are located in the kinase insert domain, a fourth change (R915H) in the last residue of the first tyrosine kinase domain, and the fifth (K1100N) in the C-terminal tail. In the TIE2 crystal structure, all these mutations cluster in the same area (Figure 2c). The function of KID is unknown. It may be essential for protein–protein interactions and signal transduction via autophosphorylation of KID-located tyrosines.16, 17 The C-terminal tail of TIE2 functions as an inhibitory loop,18 and it is possible that K1100N causes a conformational change, releasing this inhibitory effect, as evidenced by increased phosphorylation in our study. None of the mutated residues, with the possible exception of K1100, is located within the short peptide epitope recognized by the anti-TIE2 antibody (see Materials and methods section) used to normalize phosphorylation signal to total TIE2. Although the precise level of K1100N phosphorylation may, therefore, differ from the current estimation, we observe a wide variation in the strength of the in vitro hyperphosphorylation effect characteristic of all VMCM-mutations identified thus far.
As there was no phenotypic difference amongst these patients, and it is thought that TIE2 activity needs to be tightly regulated by positively and negatively acting-angiopoietin ligands, further in vivo studies are needed to elucidate the exact disease-causing mechanisms of these mutations, and the relevance of the level of TIE2 phosphorylation in lesion formation. These data nevertheless suggest that, in the heterozygous state, a wide range of chronically phosphorylated TIE2 mutant alleles are tolerated, and are compatible with normal endothelial cell (EC) function. The pathogenic effect of these mutations is only apparent in highly localized regions despite the uniformity of genetic background (heterozygosity of all patients' cells for inherited TIE2 mutations). We have hypothesized that a somatic second-hit on the wild-type allele could be required for a lesion to appear,19 following Knudson's double-hit mechanism.20 We identified a somatic deletion of a large part of the Ig2 ligand-binding domain of the wild-type receptor, causing a localized loss of its function in one lesion, from a patient carrying the inherited R849W mutation.21 Evidence for local mutations have also been reported in one patient with GVM, and in patients with cerebral cavernous malformations: both dominant and multifocal Mendelian disorders.4, 22, 23, 24 Whether the identities or hyperphosphorylation levels of the new germline TIE2 mutants show any correlation with the requirement for a second-hit, or the nature of such an event, is unknown.
In conclusion, we report 12 new families with VMCM caused by inherited mutations in TIE2/TEK. We show that a mucosal lesion is a strong diagnostic clue. Coagulopathy can occur even when lesions are small, and intestinal lesions that are sometimes seen may be associated with specific mutations. Cardiac septal defects may also be linked to TEK mutations. All of the identified changes induce increased phosphorylation of the receptor, which could lead to chronic activation of TIE2 signaling. Although the level of ligand-independent TIE2 hyperphosphorylation is highly variable, we observed no genotype–phenotype correlation. Thus, the mechanism in VMCM may be altered, rather than simply overactive, signaling by TIE2.
Acknowledgments
We are grateful to all the families for their participation in this study. We thank Antonella Mendola for her expert technical assistance and Liliana Niculescu for secretarial help. This study was partially supported by the Interuniversity Attraction Poles initiated by the Belgian Federal Science Policy, network 5/25 and 6/05; Concerted Research Actions (A.R.C.)—Convention No 02/07/276 and 7/12-005 of the Belgian French Community Ministry; the National Institute of Health, Program Project P01 AR048564; EU FW6 Integrated project LYMPHANGIOGENOMICS, LSHG-CT-2004-503573 and the F.N.R.S. (Fonds national de la recherche scientifique) (to MV, a ‘Maître de recherches honoraire du F.N.R.S.'); and by a fellowship from F.R.I.A. (Fonds pour la formation à la recherche dans l'industrie et dans l'agriculture), and Patrimoine UCL (to VW).
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on European Journal of Human Genetics website (http://www.nature.com/ejhg)
Supplementary Material
References
- Brouillard P, Vikkula M.Genetic causes of vascular malformations Hum Mol Genet 2007. 16(Spec No 2): R140–R149. [DOI] [PubMed]
- Boon LM, Vikkula M.Vascular Malformations Fitzpatrick's Dermatology in General Medecine7th edn, 20081651–1666.Chapter 173.
- Limaye N, Boon LM, Vikkula M. From germline towards somatic mutations in the pathophysiology of vascular anomalies. Hum Mol Genet. 2009;18:R65–R74. doi: 10.1093/hmg/ddp002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouillard P, Boon LM, Mulliken JB, et al. Mutations in a novel factor, glomulin, are responsible for glomuvenous malformations (‘glomangiomas') Am J Hum Genet. 2002;70:866–874. doi: 10.1086/339492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouillard P, Enjolras O, Boon LM, Vikkula M.GLMN and glomuvenous malformationsin Epstein C, Erickson RP, Wynshaw-Boris A (eds): Inborn Errors of Development2nd edn.Oxford: Oxford University Press; 2007 [Google Scholar]
- Wouters V, Boon L, Mulliken JB, Vikkula M.TIE 2 and cutaneomucosal venous malformationin Epstein C, Erickson RP, Wynshaw-Boris A (eds): Inborn Errors of Development2nd edn.Oxford: Oxford University Press; 2007 [Google Scholar]
- Boon LM, Mulliken JB, Enjolras O, Vikkula M. Glomuvenous malformation (glomangioma) and venous malformation: distinct clinicopathologic and genetic entities. Arch Dermatol. 2004;140:971–976. doi: 10.1001/archderm.140.8.971. [DOI] [PubMed] [Google Scholar]
- Vikkula M, Boon LM, Carraway KL, 3rd, et al. Vascular dysmorphogenesis caused by an activating mutation in the receptor tyrosine kinase TIE2. Cell. 1996;87:1181–1190. doi: 10.1016/s0092-8674(00)81814-0. [DOI] [PubMed] [Google Scholar]
- Calvert JT, Riney TJ, Kontos CD, et al. Allelic and locus heterogeneity in inherited venous malformations. Hum Mol Genet. 1999;8:1279–1289. doi: 10.1093/hmg/8.7.1279. [DOI] [PubMed] [Google Scholar]
- Nobuhara Y, Onoda N, Fukai K, et al. TIE2 gain-of-function mutation in a patient with pancreatic lymphangioma associated with blue rubber-bleb nevus syndrome: report of a case. Surg Today. 2006;36:283–286. doi: 10.1007/s00595-005-3138-9. [DOI] [PubMed] [Google Scholar]
- Boon LM, Brouillard P, Irrthum A, et al. A gene for inherited cutaneous venous anomalies (‘glomangiomas') localizes to chromosome 1p21–22. Am J Hum Genet. 1999;65:125–133. doi: 10.1086/302450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dompmartin A, Acher A, Thibon P, et al. Association of localized intravascular coagulopathy with venous malformations. Arch Dermatol. 2008;144:873–877. doi: 10.1001/archderm.144.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dompmartin A, Ballieux F, Thibon P, et al. Elevated D-dimer level is diagnostic for venous malformation Arch Dermatol 2009(In Press). [DOI] [PMC free article] [PubMed]
- Dumont DJ, Gradwohl G, Fong GH, et al. Dominant-negative and targeted null mutations in the endothelial receptor tyrosine kinase, tek, reveal a critical role in vasculogenesis of the embryo. Genes Dev. 1994;8:1897–1909. doi: 10.1101/gad.8.16.1897. [DOI] [PubMed] [Google Scholar]
- Shewchuk LM, Hassell AM, Ellis B, et al. Structure of the Tie2 RTK domain: self-inhibition by the nucleotide binding loop, activation loop, and C-terminal tail. Structure. 2000;8:1105–1113. doi: 10.1016/s0969-2126(00)00516-5. [DOI] [PubMed] [Google Scholar]
- Taylor GR, Reedijk M, Rothwell V, Rohrschneider L, Pawson T. The unique insert of cellular and viral fms protein tyrosine kinase domains is dispensable for enzymatic and transforming activities. EMBO J. 1989;8:2029–2037. doi: 10.1002/j.1460-2075.1989.tb03611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heidaran MA, Pierce JH, Lombardi D, et al. Deletion or substitution within the alpha platelet-derived growth factor receptor kinase insert domain: effects on functional coupling with intracellular signaling pathways. Mol Cell Biol. 1991;11:134–142. doi: 10.1128/mcb.11.1.134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niu XL, Peters KG, Kontos CD. Deletion of the carboxyl terminus of Tie2 enhances kinase activity, signaling, and function. Evidence for an autoinhibitory mechanism. J Biol Chem. 2002;277:31768–31773. doi: 10.1074/jbc.M203995200. [DOI] [PubMed] [Google Scholar]
- Boon LM, Mulliken JB, Vikkula M, et al. Assignment of a locus for dominantly inherited venous malformations to chromosome 9p. Hum Mol Genet. 1994;3:1583–1587. doi: 10.1093/hmg/3.9.1583. [DOI] [PubMed] [Google Scholar]
- Knudson AG., Jr Mutation and cancer: statistical study of retinoblastoma. Proc Natl Acad Sci USA. 1971;68:820–823. doi: 10.1073/pnas.68.4.820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limaye N, Wouters V, Uebelhoer M, et al. Somatic mutations in angiopoietin receptor gene TEK cause solitary and multiple sporadic venous malformations. Nat Genet. 2009;41:118–124. doi: 10.1038/ng.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gault J, Shenkar R, Recksiek P, Awad IA. Biallelic somatic and germ line CCM1 truncating mutations in a cerebral cavernous malformation lesion. Stroke. 2005;36:872–874. doi: 10.1161/01.STR.0000157586.20479.fd. [DOI] [PubMed] [Google Scholar]
- Akers AL, Johnson E, Steinberg GK, Zabramski JM, Marchuk DA. Biallelic somatic and germline mutations in cerebral cavernous malformations (CCMs): evidence for a two-hit mechanism of CCM pathogenesis. Hum Mol Genet. 2009;18:919–930. doi: 10.1093/hmg/ddn430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pagenstecher A, Stahl S, Sure U, Felbor U. A two-hit mechanism causes cerebral cavernous malformations: complete inactivation of CCM1, CCM2 or CCM3 in affected endothelial cells. Hum Mol Genet. 2009;18:911–918. doi: 10.1093/hmg/ddn420. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.