Abstract
Objective To describe the epidemiology of 2009 A/H1N1 influenza in critically ill pregnant women.
Design Population based cohort study.
Setting All intensive care units in Australia and New Zealand.
Participants All women with 2009 H1N1 influenza who were pregnant or recently post partum and admitted to an intensive care unit in Australia or New Zealand between 1 June and 31 August 2009.
Main outcome measures Maternal and neonatal mortality and morbidity.
Results 64 pregnant or postpartum women admitted to an intensive care unit had confirmed 2009 H1N1 influenza. Compared with non-pregnant women of childbearing age, pregnant or postpartum women with 2009 H1N1 influenza were at increased risk of admission to an intensive care unit (relative risk 7.4, 95% confidence interval 5.5 to 10.0). This risk was 13-fold greater (13.2, 9.6 to 18.3) for women at 20 or more weeks’ gestation. At the time of admission to an intensive care unit, 22 women (34%) were post partum and two had miscarried. 14 women (22%) gave birth during their stay in intensive care and 26 (41%) were discharged from an intensive care unit with ongoing pregnancy. All subsequently delivered. 44 women (69%) were mechanically ventilated. Of these, nine (14%) were treated with extracorporeal membrane oxygenation. Seven women (11%) died. Of 60 births after 20 weeks’ gestation, four were stillbirths and three were infant deaths. 22 (39%) of the liveborn babies were preterm and 32 (57%) were admitted to a neonatal intensive care unit. Of 20 babies tested, two were positive for the 2009 H1N1 virus.
Conclusions Pregnancy is a risk factor for critical illness related to 2009 H1N1 influenza, which causes maternal and neonatal morbidity and mortality.
Introduction
Pregnant women are at increased risk of influenza and its complications.1 The effects of influenza during pregnancy have been noted in previous pandemics, particularly the increased mortality in pregnant women compared with the general population.2 3 4 The 2009 influenza A/H1N1 pandemic was the first influenza pandemic to occur in the era of modern obstetric and intensive care management,5 and pregnancy is a risk factor for critical illness due to 2009 H1N1 infection.6 7 8 Information is, however, limited on medical and obstetric management and maternal and infant outcomes when pregnancy is complicated by 2009 H1N1 related critical illness.
We describe the characteristics, obstetric and intensive care management, and birth outcomes of all pregnant and recently pregnant women with confirmed 2009 H1N1 nfection admitted to Australian and New Zealand intensive care units during the winter of 2009.
Methods
Using the Australian and New Zealand Intensive Care (ANZIC) Influenza Investigators registry,7 we identified all women admitted to an intensive care unit between 1 June and 31 August 2009 with confirmed 2009 H1N1 infection who were either pregnant or post partum (completion of pregnancy within the past 28 days). All 187 intensive care units in Australia and New Zealand have been screening patients for this registry, which documents all patients admitted to an intensive care unit with confirmed influenza A.7 Registry data were last updated on 18 November 2009. Definitions, including the diagnosis of H1N1 influenza, secondary bacterial pneumonia, and other influenza syndromes, have been described previously.7 We report our findings according to strengthening the reporting of observational studies in epidemiology guidelines.9
Additional data on obstetric history, management of the current pregnancy, and birth outcomes were collected using the Australian Maternity Outcomes Surveillance System and a case report form based on one developed by the United Kingdom Obstetric Surveillance System. We collected data on the mothers’ height and weight at time of booking for maternity services, any coexisting illness, gravidity, parity (previous pregnancies with a birth at ≥20 weeks’ gestation), estimated date of delivery, plurality, miscarriage (fetal loss before 20 weeks’ gestation), vaccination against seasonal influenza during this pregnancy, and any medical or obstetric problems that developed during the current pregnancy. We documented the date and time of delivery, the occurrence of labour and whether it was spontaneous or induced, the indications for induction of labour or surgical delivery (categorised as one or more of maternal hypoxia or difficult ventilation, maternal haemodynamic instability, and fetal compromise), the use of corticosteroids to induce fetal lung maturation, and postpartum haemorrhage with more than 1500 ml of blood loss. For each baby we recorded the method of birth (unassisted vaginal, assisted vaginal, or surgical delivery), gestation, birth weight, live born or stillborn (fetal death ≥20 completed weeks of gestation), Apgar score at five minutes, admission and duration of admission to a neonatal intensive care unit or special care nursery, infant infection with 2009 H1N1 influenza, the occurrence of any complication, and survival status at time of hospital discharge. Maternal and neonatal outcomes were last updated on 22 February 2010 or last hospital discharge after delivery.
We estimated the population at risk from publicly available data. As gestational status changes with time, we considered the unit of risk to be each week of gestation from conception to four weeks post partum. From the most recently available registrations of births and stillbirths we estimated the prevalence of pregnant women at 20 weeks or more of gestation or who were post partum, between 1 June and 31 August, after adjustment for multiple births and preterm delivery, as reported by the Australian Bureau of Statistics and Statistics New Zealand.10 11 12 We estimated the prevalence of pregnant women at less than 20 weeks of gestation using the same most recently available registrations of births and stillbirths, with the addition of pregnant women who had therapeutic or spontaneous abortions or an ectopic pregnancy. We obtained the number of women who had therapeutic abortions from registrations in New Zealand13 and from published estimates in Australia.14 The number of pregnant women who have a spontaneous abortion between six and 20 weeks after the last menstrual period was estimated to be 10.9% of all pregnancies and the ectopic pregnancy rate was estimated to be 2.3%, with allowance for estimated gestation at the time of fetal loss.15 No additional allowance was made for pregnancy loss less than six weeks after the last menstrual period. We determined the population of women of childbearing age (15-44 years) in 2008 in Australia16 and 2009 in New Zealand.17 We obtained the annual number of births in Aboriginal and Torres Strait Islander women and the total number of births in Australia 2008 from the Australian Bureau of Statistics.18 The number of births in Maori or Pacific Islander women and the total number of births in New Zealand in 2007 were obtained from the New Zealand Ministry of Health.19
Statistical analysis
We analysed the data using SPSS for Windows, version 17.0. We calculated descriptive statistics for all study variables. We report continuous variables as medians (ranges) and categorical variables as percentages or relative risk ratios (95% confidence intervals), where appropriate.
Results
During the study period, 209 women of childbearing age (15-44 years) were admitted to an intensive care unit with confirmed 2009 H1N1 infection. Of these, 64 (31%) were either pregnant or post partum; 57 were admitted to an intensive care unit in Australia and seven to an intensive care unit in New Zealand.
At the time of onset of symptoms of influenza, 10 of these 64 women were at less than 20 weeks’ gestation, 49 were at 20 weeks or more, and five were post partum. The estimated number of women of childbearing age in Australia and New Zealand during the study period was 5 426 000, giving 70 533 000 women weeks—that is, weeks of potential pregnancy over the 13 weeks of the pandemic. Overall, there were 1 899 000 women weeks of gestation at less than 20 weeks, 1 704 000 women weeks of gestation at 20 weeks or more, and 358 000 women weeks post partum.
The overall risk of admission to an intensive care unit for non-pregnant women of childbearing age was 1 in 35 300 compared with 1 in 14 600 for gestations less than 20 weeks, 1 in 2700 for gestations of 20 weeks or more, and 1 in 5500 for the postpartum period. Compared with non-pregnant women of childbearing age, pregnant women with a gestation of 20 weeks or more had a 13-fold greater risk of admission to an intensive care unit as a result of 2009 H1N1 infection (relative risk 13.2, 95% confidence interval 9.6 to 18.3). The corresponding risk for postpartum women was 6.4 (2.6 to 15.7) and for women with a gestation of less than 20 weeks was 2.4 (1.3 to 4.6). Overall, compared with non-pregnant women of childbearing age the relative risk of women who were pregnant or post partum being admitted to an intensive care unit with 2009 H1N1 infection was 7.4 (5.5 to 10.0).
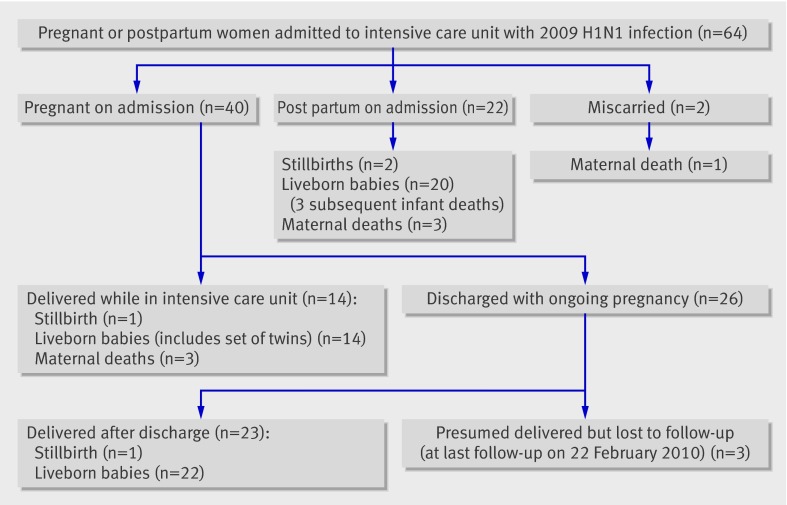
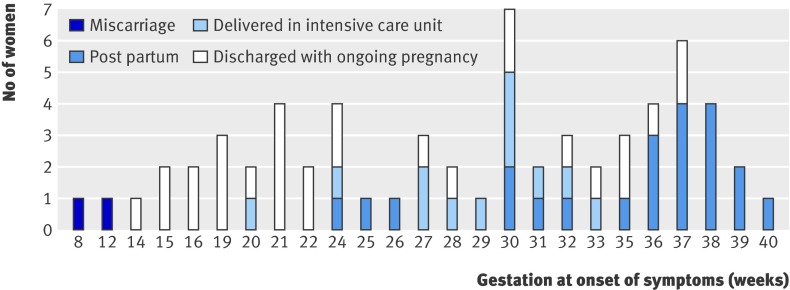
Figure 1 summarises the maternal and perinatal outcomes after admission to an intensive care unit. Of the 64 women admitted to an intensive care unit, 40 (63%) were pregnant, 22 (34%) were post partum, and 2 (3%) had miscarried. Twenty six women (41%) were discharged from the intensive care unit with ongoing pregnancy, of whom 23 (36%) had given birth at last follow-up. Three women should have delivered according to dates but could not be followed up as of 22 February 2010. Admission to an intensive care unit post partum or after miscarriage occurred a median of 0 (range 0-8) days after delivery, and 19 of 24 women (79%) had onset of influenza symptoms while pregnant. Figure 2 shows the duration of gestation at onset of influenza symptoms for women categorised as having had a miscarriage, being post partum at admission to an intensive care unit, delivering while in the unit, or being discharged from the unit with an ongoing pregnancy.
Fig 1 Outcomes after admission to intensive care unit
Fig 2 Gestation at onset of influenza symptoms in women, according to pregnancy status
Tables 1 and 2 list the characteristics, influenza syndromes and onset of symptoms, management in intensive care, and outcome of pregnant or postpartum women admitted to an intensive care unit with 2009 H1N1 infection. Thirteen of 57 patients (20%) in Australia were Australian Aboriginal or Torres Strait Islanders. Admission to an intensive care unit was more common in this group than in non-indigenous women (relative risk 6.2, 95% confidence interval 3.8 to 9.9). Admission to an intensive care unit was also more common among Maori and Pacific Islander women compared with other pregnant women (2.3, 1.4 to 3.7). Of 59 women with available data, 25 (39%) had a body mass index of more than 30 and 13 (20%) an index or more than 35. Overall, 36 women (56%) had a documented coexisting illness, of whom 21 (33% of total) had asthma. Other coexisting illnesses included documented valvular or congenital heart disease in four women (6%), depression requiring drugs in three (5%), and diabetes and essential hypertension in two women (3%). Sixteen women (25%) developed a new obstetric problem during their pregnancy, of whom six (9%) developed gestational diabetes and seven (11%) pregnancy induced hypertension or pre-eclampsia. No women had been immunised against seasonal influenza.
Table 1.
Characteristics of pregnant or postpartum women admitted to intensive care units with 2009 H1N1 infection. Values are numbers (percentages) unless stated otherwise
| Characteristics | Pregnant or postpartum women |
|---|---|
| Age (years) at admission to intensive care unit: | n=64 |
| Median (range) | 27 (16-42) |
| <20 | 7 (11) |
| 20-34 | 41 (64) |
| ≥35 | 16 (25) |
| Ethnicity: | |
| White | 37 (58) |
| Aboriginal or Torres Strait Islanders | 13 (20) |
| Maori or Pacific Islanders | 8 (13) |
| Other | 6 (9) |
| Gravidity: | n=63 |
| 1 | 15 (24) |
| 2-4 | 33 (52) |
| >5 | 15 (24) |
| Parity: | n=63 |
| Nulliparous | 19 (30) |
| 1 previous | 19 (30) |
| ≥2 previous | 25 (40) |
| Body mass index (kg/m2): | n=59 |
| <25.0 | 19 (32) |
| 25.0-29.9 | 15 (25) |
| 30.0-34.9 | 12 (20) |
| ≥35.0 | 13 (22) |
| Documented coexisting illness | |
| Present: | 36 (56) |
| Asthma | 21 (33) |
| Valvular or congenital heart disease | 4 (6) |
| Depression (receiving treatment) | 3 (5) |
| Diabetes | 2 (3) |
| Essential hypertension | 2 (3) |
| Absent | 28 (44) |
| Onset of any new obstetrical problem during pregnancy*: | 16 (25) |
| Gestational diabetes | 6 (9) |
| Pregnancy induced hypertension or pre-eclampsia | 7 (11) |
| Chorioamnionitis | 2 (3) |
| Other problem | 3 (5) |
*Some women had more than one obstetrical problem.
Table 2.
Influenza syndromes and onset of symptoms, intensive care management, and outcome of pregnant or postpartum women admitted to intensive care unit with 2009 H1N1 infection. Values are numbers (percentages) unless stated otherwise
| Variables | Pregnant or postpartum women (n=64) |
|---|---|
| Influenza syndrome: | |
| Viral pneumonitis or acute respiratory distress syndrome | 35 (55) |
| Secondary bacterial pneumonia | 18 (28) |
| Asthma or exacerbation of chronic obstructive pulmonary disease | 6 (9) |
| Intercurrent infection | 5 (8) |
| Median (range) interval from onset of symptoms to admission to intensive care unit (days) | 6 (0-35) |
| Median (range) interval from onset of symptoms to first positive test result for 2009 H1N1 (days) | 5 (1-39) |
| Median (range) gestation at onset of symptoms of influenza (weeks): | |
| <20 | 16 (8-19) |
| ≥20 | 31 (20-40) |
| Median (range) gestation at time of admission to intensive care unit, or delivery if post partum (weeks): | |
| Total cohort | 31 (8-41) |
| Pregnant | 29 (14-38) |
| Post partum | 38 (26-41) |
| Treatment in intensive care unit: | |
| Invasive mechanical ventilation | 44 (69) |
| Median (range) duration of ventilation (days) | 9 (1-45) |
| Extracorporeal membrane oxygenation | 9 (14.1) |
| Renal replacement therapy | 5 (8) |
| Vasopressors | 22 (34) |
| Antiviral drugs | 52 (81) |
| Median (range) duration of antiviral treatment (days) | 5 (0-22) |
| Corticosteroids prescribed for fetal lung maturation (n=44) | 15 (34) |
| Corticosteroids for any maternal indication | 20 (31) |
| Median (range) interval from symptom onset to antiviral treatment (days) | 6 (0-37) |
| Median (range) duration of stay in intensive care unit | 8 (1-50) |
| Died in intensive care unit | 7 (11) |
Forty four women (69%) were mechanically ventilated for a median of nine days (range 1-45 days), and nine (14%) were treated with extracorporeal membrane oxygenation. Eighteen women (28%) received corticosteroids for reasons other than fetal lung maturation and 81% received oseltamivir in the intensive care unit (no other neuraminidase inhibitors were used).
Seven women (11%) died from 2009 H1N1 influenza. All seven had viral pneumonitis or acute respiratory distress syndrome secondary to 2009 H1N1 infection. In addition, two had pulmonary haemorrhage and one each had septic shock, viral encephalitis, and the syndrome of haemolysis, elevated liver enzymes, and low platelets. All were mechanically ventilated and three were treated with extracorporeal membrane oxygenation. Four received corticosteroids. All were treated with oseltamivir. Six of the nine women (67%) treated with extracorporeal membrane oxygenation survived.
As of 22 February 2010, 59 of the women were known to have given birth to 60 babies of at least 20 weeks’ gestation; 56 were live born and four were stillbirths. There was one set of liveborn twins. Of the 22 postpartum women, 14 (64%) had had an emergency caesarean section and eight (36%) had spontaneous vaginal deliveries. Fourteen women (26%) gave birth during their stay in an intensive care unit, 13 (93%) by emergency caesarean section. Non-mutually exclusive indications for delivery that occurred in women while in an intensive care unit were maternal hypoxaemia in 13 (93%), maternal haemodynamic instability in 8 (57%), and concern for fetal wellbeing in 3 (21%). Three of the 14 women (21%) requiring caesarean section while in the intensive care unit died. In only one case was concern for fetal wellbeing the sole indication for delivery while in the intensive care unit. Of 23 women who delivered after discharge from intensive care, 17 (74%) had vaginal deliveries and six (26%) caesarean sections, of which three were elective and three were during labour. Seven women (16%) had postpartum haemorrhage (blood loss >1500 ml).
Table 3 describes the perinatal outcomes of the 60 babies. Eleven (18%) had gestations between 32 and 37 weeks, and 11 (18%) between 20 and 32 weeks. Ten (17%) weighed between 1500 g and 2500 g at birth, whereas eight (13%) weighed less than 1500 g. The birth weight of three male neonates (5%) was below the 10th centile for gestational age for males. Thirty two (57% of 56 liveborn babies) were admitted to a neonatal intensive care unit or special care nursery, including three babies born after the mother was discharged from the intensive care unit, for a median stay of 18 days (range 1-79 days). Twenty one (38% of 56 liveborn babies) required continuous positive airway pressure ventilation or endotracheal intubation with positive pressure ventilation. Of 20 neonates tested, two were positive for 2009 H1N1 virus infection. Three infants died (two neonates and one post-neonatal infant), all related to complications of prematurity, hypoxic encephalopathy, or both.
Table 3.
Perinatal outcomes. Values are numbers (percentages) unless stated otherwise
| Outcome measures | Babies (n=60*) |
|---|---|
| Gestation (completed weeks): | |
| 32-36 | 11 (18) |
| 20-31 | 11 (18) |
| Birth weight (g): | |
| Median (range) | 2806 (640-4260) |
| 1500 to 2499 | 10 (17) |
| <1500 | 8 (13) |
| Apgar score <4 at five minutes | 8 (13) |
| Admission to NICU or SCN (of 56 live borns) | 32 (57) |
| Use of assisted ventilation in NICU or SCN (n=32): | |
| None | 11 (34) |
| Continuous positive airway pressure ventilation only | 5 (16) |
| Endotracheal intubation or ventilation | 16 (50) |
| Median (range) duration of admission to NICU or SCN (days) | 18 (1-79) |
| Documented infection with 2009 H1N1† | 2 (10) |
| Hospital outcome: | |
| Still birth | 4 (7) |
| Discharged | 53 (88) |
| Infant death‡ | 3 (5) |
NICU=neonatal intensive care unit; SCN=special care nursery.
*Includes one set of twins. Denominators vary.
†Of 20 babies tested.
‡Two neonatal and one post-neonatal.
Discussion
Pregnancy is a risk factor for 2009 H1N1 related critical illness. Of the 64 pregnant and postpartum women who were admitted to an intensive care unit in Australia and New Zealand with confirmed 2009 H1N1 infection, the risk of critical illness was much greater later in the pregnancy, at over 13 times the risk in the non-pregnant population. 2009 H1N1 infection was associated with substantial maternal and perinatal morbidity and mortality.
Our results show that indigenous pregnant women in Australia and New Zealand were at higher risk of critical illness due to 2009 H1N1 influenza than non-indigenous pregnant women, consistent with the observation that women from indigenous populations are at higher risk for a variety of complications of pregnancy associated with poor maternal and neonatal outcomes.20 21 22 Over half of the women had a coexisting illness. Pre-existing asthma occurred in 21% of these women compared with 12% in the general Australian birthing population.23 Among the critically ill women, 42% had a body mass index of more than 30 and 22% of more than 35; the corresponding proportions in the Australian birthing population are 24% and 10%.24 This is consistent with a preliminary report that identifies obesity as a risk factor for 2009 H1N1 related critical illness in pregnant women in the United Kingdom.25
Most of the women admitted to an intensive care unit were treated with mechanical ventilation and 14% were treated with extracorporeal membrane oxygenation.26 As seen in the general intensive care unit population, severe 2009 H1N1 infection was predominantly single system respiratory failure with only a few women requiring support for multiorgan failure. The time from the onset of symptoms to the receipt of antivirals was long for many of the women in this study, with antiviral drugs started a median of six days after onset of symptoms. The recommended timing for starting antiviral treatment is less than 48 hours from the onset of symptoms.27 Whether earlier treatment with an antiviral agent could have modified the severity of illness is unknown.
Overall, seven women (11%) died. Generally, influenza has been an extremely rare cause of maternal death. Between 1997 and 2005 in Australia, 24 maternal deaths occurred as a result of any infection, or 1.1 deaths per 100 000 births.21 28 29 Only one of these deaths was due to influenza.29 No maternal deaths were attributed to influenza in the United Kingdom between 1997 and 2005.30 31 32 Other descriptions of 2009 H1N1 influenza during pregnancy in the United States have also documented substantial mortality, including an 8% mortality among pregnant women with severe 2009 H1N1 infection in California.6 8 Although a mortality of 11% seems low when compared with usual outcomes of respiratory failure in intensive care (such as 30-40% mortality for the acute respiratory distress syndrome in a general intensive care population),33 a maternal mortality of 11% is high when compared with any other obstetric condition.
Operative births and preterm delivery were common. Most of the caesarean sections were carried out for maternal hypoxia or haemodynamic instability. Concern for the fetus was the primary indication for only one delivery. The proportion of women who had a caesarean section before or during their stay in an intensive care unit was 75%, compared with 30% for the general birthing population in Australia.20 Caesarean delivery for maternal hypoxia has generally not been recommended in the literature as it has been thought not to improve maternal outcome,34 but in our series only three (21%) of these women died despite critical hypoxaemia.
No woman in this cohort had been immunised against seasonal influenza despite established recommendations that pregnant women should be immunised.35 A specific 2009 H1N1 vaccine has recently been made available and is recommended for pregnant women.35 36 The availability of H1N1 vaccine and antiviral treatment may modify the epidemiology and alter the course of the disease in the future.
Infection with 2009 H1N1 had a substantial impact on neonatal outcomes. Most neonates born to the critically ill women in this study were admitted to a neonatal intensive care unit or special care nursery, compared with less than 15% of the total newborn population in Australia.20 Few neonates were small for gestational age, consistent with the acute onset of the illness. Overall, seven perinatal deaths occurred, four of them stillbirths. Whether earlier delivery in women at over 30 weeks’ gestation with severe disease could improve neonatal outcome is currently unknown.
Strengths and limitations of the study
This study was population based and, to the best of our knowledge, included all pregnant or postpartum woman with confirmed 2009 H1N1 infection admitted to any intensive care unit in Australia and New Zealand. Overall, our numbers were small, which limits the conclusions that can be drawn. The incidence, infection rate, and virulence of influenza infection may be different at other locations and at different stages of the pandemic, and this may limit generalisability.
Conclusion
Pregnant women, particularly in the second half of pregnancy, are more likely than non-pregnant women to develop critical illness associated with 2009 H1N1 influenza. Among women who developed critical illness, the outcomes were poor, including death of the mother or baby.
What is already known on this topic
Pregnant women are at an increased risk of complications from influenza
Other risk factors include obesity and respiratory problems such as asthma
What this study adds
A disproportionate number of pregnant or postpartum women were admitted to intensive care with 2009 H1N1 influenza, particularly after 20 weeks’ gestation
Overall, 11% of mothers and 12% of babies died
Intensive management for maternal hypoxia, including caesarean section and extracorporeal membrane oxygenation, led to better than expected outcomes
The Australian and New Zealand Intensive Care (ANZIC) Influenza Investigators are a collaboration of the ANZIC Society Clinical Trials Group, the ANZIC Research Centre, the Australasian Society for Infectious Diseases Clinical Trials Group, the Paediatric Study Group of the ANZIC Society, and the ANZIC Society Centre for Outcome and Resource Evaluation. We thank Ville Pettilä for the provision of data from the ANZIC Influenza Investigators registry and assistance with some analysis, and the research coordinators and research midwives in all sites, who collected data. The study was coordinated by the Australian and New Zealand Intensive Care Research Centre, Monash University, Melbourne and the Australasian Maternity Outcomes Surveillance System, Perinatal and Reproductive Epidemiology Research Unit, University of New South Wales, Sydney, Australia.
Contributors: All members of the writing committee (see web extra on bmj.com for details) contributed equally to the collection and analysis of the data and drafting the manuscript, and take responsibility for the content of this manuscript.
Funding: The ANZIC Influenza Investigators registry is supported by the Department of Health and Ageing, Commonwealth Government of Australia; New South Wales Health, Government of New South Wales; Department of Health, Government of Victoria; the Australian and New Zealand Intensive Care Research Centre; the Australian and New Zealand Intensive Care Society; and an unrestricted grant from CSL, Melbourne, Victoria. The Australasian Maternity Outcomes Surveillance System is supported by National Health and Medical Research Council (Australia) project grant, No 510298. None of the funders had any role in the study design and the collection, analysis, and interpretation of data, or in the writing of the article and the decision to submit it for publication. The researchers confirm their independence from funders and sponsors. All researchers had access to all the data.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare that (1) no authors have support from any company for the submitted work; (2) no authors have any relationships with any companies that might have an interest in the submitted work in the previous 3 years; (3) their spouses, partners, or children have no financial relationships that may be relevant to the submitted work; and (4) no authors have non-financial interests that may be relevant to the submitted work.
Ethical approval: This study was approved by the institutional ethics committee of each centre and the requirement for individual subject informed consent was waived at all sites.
Data sharing: No additional data available.
Cite this as: BMJ 2010;340:c1279
Web Extra. Extra material supplied by the author
Details of the writing committee and collaborators
References
- 1.Rasmussen S, Jamieson D, Bresee J. Pandemic influenza and pregnant women. Emerg Infect Dis 2008;14:95-100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Harris JW. Influenza occurring in pregnant women. JAMA 1919;72:978-80. [Google Scholar]
- 3.Freeman DW, Barno A. Deaths from Asian influenza associated with pregnancy. Am J Obstet Gynecol 1959;78:1172-5. [DOI] [PubMed] [Google Scholar]
- 4.Neuzil KM, Reed GW, Mitchel EF, Simonsen L, Griffin MR. Impact of influenza on acute cardiopulmonary hospitalizations in pregnant women. Am J Epidemiol 1998;148:1094-102. [DOI] [PubMed] [Google Scholar]
- 5.Webb SAR, Seppelt IM. Pandemic (H1N1) 2009 influenza (“swine flu”) in Australian and New Zealand intensive care. Crit Care Resusc 2009;11:170-2. [PubMed] [Google Scholar]
- 6.Jamieson DJ, Honein MA, Rasmussen SA, Williams JL, Swerdlow DL, Biggerstaff MS, et al. H1N1 2009 influenza virus infection during pregnancy in the USA. Lancet 2009;374:451-8. [DOI] [PubMed] [Google Scholar]
- 7.The ANZIC Influenza Investigators. Critical care services and 2009 H1N1 influenza in Australia and New Zealand. N Engl J Med 2009;361:1925-34. [DOI] [PubMed] [Google Scholar]
- 8.Louie JK, Acosta M, Jamieson DJ, Honein MA, for the California Pandemic (H1N1) Working Group. Severe 2009 H1N1 influenza in pregnant and postpartum women in California. N Engl J Med 2010;326:27-35. [DOI] [PubMed] [Google Scholar]
- 9.Von Elm E, Egger M, Altman DG, Pocock SJ, Gøtzsche PC, Vandenroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ 2007;335:806-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Australian Bureau of Statistics. 3301.0 Births, Australia, 2008. Canberra: 2009. www.abs.gov.au/AUSSTATS/abs@.nsf/mf/3301.0.
- 11.Australian Bureau of Statistics. 3304.0 Perinatal deaths, Australia, 2007. Canberra: 2009. www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3304.02007?OpenDocument.
- 12.Statistics New Zealand. Births and deaths: June 2009 quarter. Wellington: 2009. http://search.stats.govt.nz/nav/ct2/population_births/ct1/population/0.
- 13.Statistics New Zealand. Abortion statistics: 2008. Wellington: 2009. http://search.stats.govt.nz/nav/ct1/health/0.
- 14.Chan A, Sage LC. Estimating Australia’s abortion rates 1985-2003. Med J Aust 2005;182:447-52. [DOI] [PubMed] [Google Scholar]
- 15.Nybo Andersen AM, Wohlfahrt J, Christens P, Olsen J, Melbye M. Maternal age and fetal loss: population based register linkage study. BMJ 2000;320:1708-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Australian Bureau of Statistics. 3235.0 Population by age and sex, regions of Australia, 2008. Canberra: 2009. www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3235.02008?OpenDocument.
- 17.Statistics New Zealand. National population estimates June 2009 quarter. Wellington: 2009. www.stats.govt.nz/methods_and_services/access-data/tables/national-pop-estimates.aspx.
- 18.Australian Bureau of Statistics. Table 9 Aboriginal and Torres Strait Islander births, Summary, Australia, states and territories, 2008. Canberra: 2009. www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3301.02008?OpenDocument.
- 19.New Zealand Ministry of Health. Maternity Snapshot 2007. Wellington: Ministry of Health, 2009.
- 20.Laws PJ, Hilder L. Australia’s mothers and babies 2006. Perinatal statistics series No 22. Catalogue No PER 46. Sydney: AIHW National Perinatal Statistics Unit, 2008.
- 21.Sullivan EA, Hall B, King JF. Maternal deaths in Australia 2003-2005. Maternal death Series No 3. Catalogue No PER 42. Sydney: AIHW National Perinatal Statistics Unit, 2006. www.preru.unsw.edu.au/PRERUWeb.nsf/resources/MD3/$file/md3a.pdf.
- 22.Knight M, Kurinczuk J, Spark P, Brocklehurst P, on behalf of UKOSS. Inequalities in maternal health: national cohort study of ethnic variation in severe maternal morbidities. BMJ 2009;338:b542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Clifton V, Engel P, Smith R, Gibson P, Brinsmead M, Giles W. Maternal and neonatal outcomes of pregnancies complicated by asthma in an Australian population. Aust NZ J Obstet Gynaecol 2009;49:619-26. [DOI] [PubMed] [Google Scholar]
- 24.Chan A, Scott J, Nguyen A-M, Sage L. Pregnancy outcome in South Australia 2007. Adelaide: SA Health, 2008. www.dh.sa.gov.au//pehs/PDF-files/090210-pregnancy-outcome-report-2007.pdf.
- 25.H1N1 in pregnancy interim report No 1, UK Obstetric Surveillance System. 2009. www.npeu.ox.ac.uk/downloads/ukoss/UKOSS-H1N1v-Interim-Report-1.pdf.
- 26.The Australia and New Zealand Extracorporeal Membrane Oxygenation (ANZ ECMO) Influenza Investigators. Extracorporeal membrane oxygenation for 2009 influenza A(H1N1) acute respiratory distress syndrome. JAMA 2009;302:1888-95. [DOI] [PubMed] [Google Scholar]
- 27.Cheng A, Dwyer R, Kotsimbos A, Starr M, Korman TM, Buttery JP, et al. ASID/TSANZ guidelines: treatment and prevention of H1N1 influenza 09 (human swine flu) with antiviral agents. Med J Aust 2009;191:1-8. [DOI] [PubMed] [Google Scholar]
- 28.Slaytor EK, Sullivan EA, King JF. Maternal deaths in Australia 1997-1999. Catalogue No PER 24. Sydney: AIHW National Perinatal Statistics, 2004. www.preru.unsw.edu.au/PRERUWeb.nsf/resources/MD_94_97_00/$file/Final+MD+report+August+24+2004.pdf.
- 29.Sullivan EA, King JF. Maternal deaths in Australia 2000-2002, maternal deaths series No 2. Catalogue No PER 32. Sydney: AIHW National Perinatal Statistics Unit, 2006. www.preru.unsw.edu.au/PRERUWeb.nsf/resources/MD_94_97_00/$file/MD2002_02.pdf.
- 30.Lewis G, Drife JO, eds. Why mothers die. Confidential Enquiries into Maternal Deaths in the United Kingdom 1997-1999. RCOG Press, 2001.
- 31.Lewis G, ed. Why mothers die. Confidential Enquiries into Maternal Deaths in the United Kingdom 2000-2002. RCOG Press, 2005.
- 32.Lewis G, ed. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer—2003-2005. The seventh report on Confidential Enquiries into Maternal Deaths in the United Kingdom. RCOG Press, 2007.
- 33.Bersten AD, Edibam C, Hunt T, Moran J, the Australian and New Zealand Intensive Care Society Clinical Trials Group. Incidence and mortality of acute lung injury and the acute respiratory distress syndrome in three Australian states. Am J Respir Crit Care Med 2002;165:443-8. [DOI] [PubMed] [Google Scholar]
- 34.Tomlinson MW, Caruthers TJ, Whitty JE, Gonik B. Does delivery improve maternal condition in the respiratory-compromised gravida? Obstet Gynecol 1998;91:108-11. [DOI] [PubMed] [Google Scholar]
- 35.The Australian immunisation handbook 9th ed. Australian Government, 2008. www.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook-influenza.
- 36.Australian national vaccine program priority groups. www.health.gov.au/internet/healthemergency/publishing.nsf/Content/national-vaccination-program#priority.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Details of the writing committee and collaborators