Abstract
About 15 years have gone by since Strachan first proposed the idea that infections and unhygienic contact may confer protection from the development of allergic illnesses. The so-called ‘hygiene hypothesis’ has since undergone numerous modifications in the field of epidemiology, clinical science and immunology. Three main areas of research have been brought forward: to explore the role of overt viral and bacterial infections for the inception of allergic diseases; to investigate the significance of environmental exposure to microbial compounds on the development of allergies; and to study the effect of both exposures on underlying innate and adaptive immune responses. A concept unifying these various aspects has not been found, but various pieces of a complex interplay between immune responses of the host, characteristics of the invading microorganism, the level and variety of the environmental exposure and the interactions between an exposed subject's genetic background and the environmental exposures becomes apparent. A natural experiment relating to the hygiene hypothesis is the recurrent observation of a protective effect of growing up on a farm for asthma and allergies. This has been shown in a large number of epidemiological studies across the world among children and adults. The timing and duration of exposure are likely to play a critical role. The largest reduction in risk has been demonstrated for those exposed prenatally and continuously thereafter until adulthood. The protective factors in these farming environments have not been unravelled completely. Findings from various studies suggest that the contact with farm animals, at least in childhood, confers protection. Also the consumption of unprocessed cow's milk directly from the farm has been shown to protect from childhood asthma and allergies. Increased levels of microbial substances may, at least in part, contribute to the ‘farm effect’. However, only few studies have measured microbial exposures in these environments and the results obtained so far suggest that the underlying protective microbial exposure(s) have not been identified, but a number of studies using metagenomic approaches are currently under way. The mechanisms by which such environmental exposures confer protection from respiratory allergies are also not well understood. There is good evidence for the involvement of innate immune responses, but translation into protective mechanisms for asthma and allergies is lacking. Furthermore, a number of gene × environment interactions have been observed.
Keywords: allergy, asthma, farm life style, ‘hygiene hypothesis’
Introduction
In recent years, the ‘hygiene hypothesis’ has received much attention [1]. This field of allergy research investigates the potential link between exposure to microbial sources and the development of allergic and autoimmune diseases. At least three distinct claims on the underlying nature of the hygiene hypothesis have been brought forward. First, the potential role of overt and unapparent infections with viruses and bacteria has been discussed; secondly, the relevance of non-invasive microbial exposures in the environment has been shown to influence the development of allergic and also autoimmune diseases; and thirdly, the influence of such exposures and infections on a subject's innate and adaptive immune response is being discussed.
Before addressing these various aspects of the hygiene hypothesis, one must consider the complex nature of the problem. In clinical practice allergic illnesses may appear somewhat uniform because most patients present with a limited variety of symptoms, yet the underlying mechanisms and causes are likely to be numerous. Asthma and allergies are complex diseases determined by genetic variation interacting with environmental exposures. There is increasing evidence that it is not one single gene that causes, for example, asthma, but that many genes with small effects contribute to new-onset asthma. Moreover, several environmental determinants have been identified for different allergic illnesses which interact with an exposed subject's genetic background.
Furthermore, when considering the various environmental exposures and potential underlying mechanisms, one must bear in mind that the effect of an exposure has been shown to depend upon the timing. At least during infancy, childhood and adolescence the human organism is in a constant stage of development and maturation. These predefined processes display windows of accessibility and vulnerability to intrinsic and extrinsic influences only at certain stages of development. Most studies suggest that for asthma and allergies, early life, i.e. pregnancy and the first 1–3 years, plays the most important role, either through mechanisms acting in utero or as epigenetic modulation of subsequent developmental trajectories. Environmental exposures may, however, also modify health outcomes postnatally by affecting the innate and adaptive immune responses. Moreover, genetic factors are clearly of importance for the incidence of asthma and allergies, but our journey into the discovery of relevant genes for allergic diseases has just begun. It seems likely that no single gene will be responsible for the clinical manifestation of any allergic illness. Rather, polymorphisms in many genes interacting with environmental influences at various time-points of development are likely to contribute to the mechanisms underlying the various atopic conditions.
Several immunological concepts have been proposed to account for the hygiene hypothesis. First, the skewing of the T helper type 1 (Th1)/Th2 balance away from allergy-promoting Th2 towards Th1 cells has been at the centre of attention [2]. The link between the Th1/Th2 balance and allergic diseases is mediated in part by immunoglobulin (Ig)E: Th2 cells, by secreting interleukin (IL)-4 and IL-13, promote immunoglobulin class switch recombination to IgE [3]. This notion has, however, been debated and conflicting data cannot be disregarded. Not only has the prevalence of Th2-related diseases such as allergies been increasing during recent decades, but so also has the prevalence of autoimmune diseases such as Crohn's disease and diabetes mellitus [4,5]. Furthermore, helminthic infections favouring Th2-type immune responses have been shown to be protective for the development of allergic diseases [6]. In vitro and animal data have shown that activation of the innate immune system does not necessarily promote a Th1 response, but that Th2 responses may also occur, depending upon the experimental conditions [7]. Therefore, regulation of the Th1/Th2 balance through regulatory T cells and Th17 cells may contribute to the development of both allergic and autoimmune illnesses. Not only effector cells, but also cells of the innate immune response recognizing microbial signals such as dendritic cells may occupy a central role in controlling immune responses. Their importance for the development of allergies has been well documented [8,9].
Infections as intermediary of the hygiene hypothesis
A number of surveys have suggested that infections with hepatitis A might protect from the development of allergy [11–13], but others could not confirm these results [14–16]. All studies used a positive serology to hepatitis A as a marker of past disease. However, a positive serology and an inapparent hepatitis A infection may simply be a proxy of other unhygienic environmental exposures. However, immunological characteristics of hepatitis A virus may suggest a truly allergy-modulating effect. The receptor for the hepatitis A virus is TIM-1 (T cell, immunoglobulin and mucin) [10]. This receptor and its ligand TIM-4 belong to a family of proteins which are involved in the regulation of CD4 T cell differentiation, airway inflammation and airway hyperresponsiveness [17].
Few other viruses have been investigated in population-based studies. Two reports have suggested a protective role for herpes infections [11,18], but confirmation in other populations is needed. Even fewer studies have investigated the association between the occurrence of bacterial infections and the development of asthma and allergies. In Italy, children hospitalized for salmonellosis had a lower prevalence of allergic rhino-conjunctivitis and asthma compared to children who had been hospitalized with non-bacterial enteritis [19]. These findings, however, need confirmation in other populations. A number of other reports suggest that infections with oro-faecal pathogens such as Helicobacter pylori and Toxoplasma gondii may affect the development of asthma and allergic disorders. Several studies have shown an inverse relation between a positive serology to H. pylori and T. gondii and atopic sensitization, allergic rhinoconjunctivitis and allergic asthma [14,20,21]. A dose–response relationship has been observed in these studies: the more infections these subjects have encountered as assessed by positive serology, the lower was the observed prevalence of atopy, allergic rhinitis and asthma. These findings suggest that it is not one single microorganism which may confer protection, but most probably a number of different agents.
The evidence regarding a potential protective effect of exposure to Mycobacteria in population-based surveys is conflicting. These microorganisms, however, show remarkable immunomodulatory characteristics in experimental studies. In murine models of allergic asthma, treatment with Mycobacteria resulted in the suppression of several allergic features [22–25]. In westernized societies, parasitic infections are likely to play a minor role in the protection from asthma and allergies. In endemic areas such as Africa or Latin America parasitic infections are, however, related strongly inversely to the development of atopy. These findings have been reviewed in detail in [26,27].
Environmental exposure as intermediary of the hygiene hypothesis
A number of studies have been performed in rural areas in Europe, contrasting the prevalence of asthma and allergies in children and adults living on farms to the prevalence of these illnesses in subjects living in rural areas but not on farms. A large body of evidence suggests that the prevalence of hay fever, allergic rhinoconjunctivitis and atopic sensitization is reduced significantly among farm children compared to non-farm children. Similar figures have been observed for adult farming populations. In the European farmers study, for example, the prevalence of allergic rhinitis was significantly lower in 20–44-year-old animal farmers compared to other participants of the European Community Respiratory Health Survey [28]. The prevalence of asthma was also significantly lower among these farmers when compared to the general population.
Sources of protective exposures in farming environments
Two studies conducted outside Europe [29,30] suggested that an important component of the farm environment is livestock exposure, as no protective effect of farming was observed among children living in a primarily crop-farming region in Australia. This notion is supported by findings from the European studies, where exposure to livestock has been identified as an important contributor to the protective ‘farm effect’[31–34]. Children not living on a farm but being exposed regularly to farm animals also had a lower prevalence of allergic sensitization and allergic rhinitis compared to non-exposed non-farm children. Another consistently identified source of protection is the consumption of unprocessed cow's milk, as shown in a number of studies [30,31,34]. As with livestock exposure, the protective effect from the consumption of raw milk was not restricted to children living on a farm, but was also seen among non-farm populations consuming unpasteurized cow's milk [34]. Among adult farmers, the protective effect of farming on atopic diseases has also been shown to be more pronounced among animal farmers, with the strongest effect among pig and cattle farmers [35–37]. This observation, however, is not consistent across studies.
Timing of farm exposures
In the ALEX (Allergen and Endotoxin) study, a multi-centre, cross-sectional survey in rural alpine areas in Switzerland, Austria and Germany, children exposed to animal sheds and the consumption of unprocessed cow's milk in the first year of life (Fig. 1) but not thereafter were protected significantly from the development of asthma, hay fever and atopic sensitization. In the PARSIFAL study (Prevention of Allergy – Risk Factors for Sensitization Related to Farming and Anthroposophic Lifestyle), the risk of atopic sensitization was influenced not only by a child's exposure to the farming environment, but also determined strongly by maternal exposure to animal sheds during pregnancy [38]. Since then a prospective birth cohort in rural populations of farming and non-farming women has been initiated. The notion of a prenatal maternal influence on the development of allergic diseases has been corroborated by showing that maternal exposure to animal sheds and unpasteurized cow's milk influences the production of specific IgE antibodies in the cord blood of the neonate [39]. Furthermore, the production of interferon-γ and tumour necrosis factor-α by neonatal cord blood cells differed according to maternal exposure to animal sheds and unprocessed cow's milk [39].
Fig. 1.
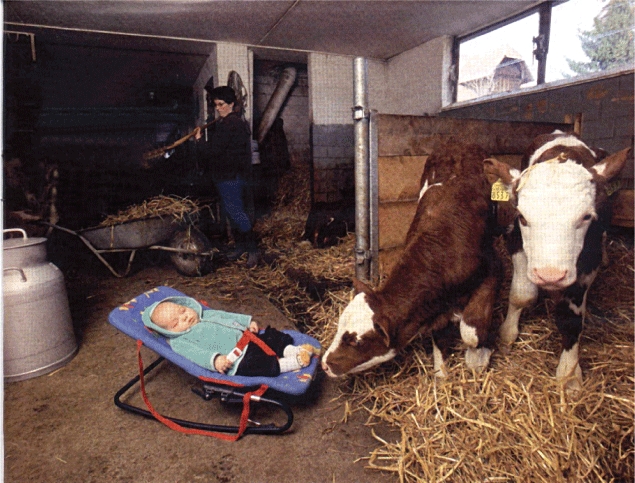
Growing up on a farm protects from childhood asthma and allergy. Timing: during pregnancy and first years of life, continued exposure is best. Protective exposures: farm animals, farm milk and animal fodder. Microbial exposures: bacteria, fungi. Mechanisms: activation of innate immunity. Gene–environment interactions.
In studies of adult farmers, the relevance of the timing of exposures has also been addressed. The protective effect of farming environments and respiratory allergies were strongest when farm contact started during childhood, and was sustained until adulthood [35,40–45]. A study among 137 university employees, of whom approximately one-third were working with laboratory animals, indicated that those with farm contact during infancy were protected from sensitization to occupational allergens later in life [46]. Many of the subjects exposed in early childhood to a farm environment may already have been exposed during pregnancy. Thus, the effect of prenatal to postnatal exposure in early life cannot be disentangled in the surveys of adult populations. With respect to asthma, the findings across studies among adult farmers have been less clear-cut. These inconsistencies may, in part, be attributable to the difficulties in the diagnosis of asthma versus the ‘asthma-like syndrome’ in adults. Also, long-term exposure to endotoxin has been shown clearly to be a risk factor for non-atopic asthma in adults, as discussed below [42,44,47–51].
Microbial exposures
It seems likely that children exposed to animal sheds encounter more allergens, bacteria, viruses and fungi than children without such exposures, but only few of these potential protective exposures have been assessed in farming environments. Bacterial substances such as endotoxin from Gram-negative bacteria and muramic acid, a component of peptidoglycan from the cell wall of all types of bacteria, have been found to be more abundant in mattress dust from farm children compared to non-farm children [52]. Similarly, a marker for fungal exposures, i.e. extracellular polysaccharides from Penicillium and Aspergillus spp., is more prevalent in farming households than in non-farming households. Endotoxin levels in children's mattress dust have been shown to relate inversely to the prevalence of hay fever, atopic asthma and atopic sensitization [53]; yet high levels of endotoxin were associated positively with non-atopic wheeze. In turn, levels of muramic acid in mattress dust were associated with a lower frequency of wheezing and asthma among rural children in the ALEX study [54]. These findings are comparable to studies among adult farmers. In the Netherlands, a job exposure matrix was designed to assign individual occupational exposures to endotoxin [55]. Using this job exposure matrix, endotoxin exposure was related inversely to self-reported symptoms of allergic rhinitis. However, the prevalence of asthma was augmented with increasing exposure. Similar findings have been reported from an earlier case–control study among Dutch pig farmers [51]. While higher endotoxin levels were associated with a reduced risk for atopic sensitization, farmers with higher levels of endotoxin were more likely to show airway hyperresponsiveness and to have reduced lung function. Therefore, endotoxin may have both beneficiary effects (atopic sensitization, allergic rhinitis) while simultaneously being a risk factor for non-atopic asthma and wheeze.
Mechanisms of protection in farming environments
Little is known about immune responses in farm as compared to non-farm children. The Swiss arm of the ALEX study investigated whether growing up on a farm affects the expression of receptors for microbial compounds. Pathogen-associated molecular patterns, evolutionarily highly conserved structural components of microbes, are recognized by similarly conserved receptors of host innate immune systems such as the human Toll-like receptors and CD14. Peripheral blood leucocytes from children in the ALEX population living on a farm were found to display increased expression of the genes for CD14, TLR2 and TLR4 compared to non-farm children [56]. These results were confirmed in the PARSIFAL study [38], suggesting that environmental exposures, in particular to microbial components, affect the expression of genes encoding microbial ligand receptors [56]. A number of individual characteristics were related to the up-regulation of distinct TLR genes [57]. Interestingly, gene-expression correlated with prenatal exposure to farm factors. Maternal exposure to animal sheds during pregnancy correlated significantly with an increase in the expression of TLR2, TLR4 and CD14[38]. Also, a dose–response relationship was seen. Expression of TLR2, TLR4 and CD14 increased with the number of different farm animal species with which the mother had contact during her pregnancy.
Genetic studies performed in farm children further support the notion that Toll-like receptors are involved in a mechanism contributing to the protection from asthma and allergies. Polymorphisms in the genes for TLR4, TLR2 and NOD2 have been shown to interact with the farm environment, modulating the asthma and allergy protective effect [58]. Furthermore, a significant interaction between genetic variation in CD14 and unprocessed cow's milk consumption was found. These findings suggest that a protective effect of various farm exposures is modified by an individual's genetic make-up. In adults, gene–environment interactions between genes for CD14 have also been shown in adult farmers and the general population with respect to childhood farm exposure [59,60].
In conclusion, there is convincing evidence that a farm childhood confers protection from respiratory allergies with a sustained effect into adulthood, particularly with continued exposure. The nature of individual protective exposures has not been elucidated completely. Studies suggest that at least in childhood contact with farm animals, their fodder and their products, such as milk consumed directly from the farm, contribute to the ‘farm effect’. The underlying mechanisms are still ill-defined, but are likely to involve a number of steps in innate and adaptive immunity. An individual's genetic background modifies the effects of the environmental exposures.
Disclosure
The author is consultant to UCB, Protectimmun and GSK.
References
- 1.Okada H, Kuhn C, Feillet H, Bach J-F. The ‘hygiene hypothesis’ for autoimmune and allergic diseases: an update. Clin Exp Immunol. 2010;160:1–9. doi: 10.1111/j.1365-2249.2010.04139.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Martinez FD, Holt PG. Role of microbial burden in aetiology of allergy and asthma. Lancet. 1999;354(Suppl. 2):SII12–15. doi: 10.1016/s0140-6736(99)90437-3. [DOI] [PubMed] [Google Scholar]
- 3.Geha RS, Jabara HH, Brodeur SR. The regulation of immunoglobulin E class-switch recombination. Nat Rev Immunol. 2003;3:721–32. doi: 10.1038/nri1181. [DOI] [PubMed] [Google Scholar]
- 4.Platts-Mills TA, Woodfolk JA, Sporik RB. Con: the increase in asthma cannot be ascribed to cleanliness. Am J Respir Crit Care Med. 2001;164:1107–8. doi: 10.1164/ajrccm.164.7.2107130b. discussion 8–9. [DOI] [PubMed] [Google Scholar]
- 5.Bach JF. The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med. 2002;347:911–20. doi: 10.1056/NEJMra020100. [DOI] [PubMed] [Google Scholar]
- 6.Yazdanbakhsh M, van den Biggelaar A, Maizels RM. Th2 responses without atopy: immunoregulation in chronic helminth infections and reduced allergic disease. Trends Immunol. 2001;22:372–7. doi: 10.1016/s1471-4906(01)01958-5. [DOI] [PubMed] [Google Scholar]
- 7.Eisenbarth SC, Piggott DA, Huleatt JW, Visintin I, Herrick CA, Bottomly K. Lipopolysaccharide-enhanced, toll-like receptor 4-dependent T helper cell type 2 responses to inhaled antigen. J Exp Med. 2002;196:1645–51. doi: 10.1084/jem.20021340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akdis CA, Blaser K, Akdis M. Genes of tolerance. Allergy. 2004;59:897–913. doi: 10.1111/j.1398-9995.2004.00587.x. [DOI] [PubMed] [Google Scholar]
- 9.Belkaid Y, Piccirillo CA, Mendez S, Shevach EM, Sacks DL. CD4+CD25+ regulatory T cells control Leishmania major persistence and immunity. Nature. 2002;420:502–7. doi: 10.1038/nature01152. [DOI] [PubMed] [Google Scholar]
- 10.Umetsu DT, DeKruyff RH. 99th Dahlem Conference on Infection, Inflammation and Chronic Inflammatory Disorders: Microbes, apoptosis and TIM-1 in the development of asthma. Clin Exp Immunol. 2010;160:125–9. doi: 10.1111/j.1365-2249.2010.04136.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matricardi PM, Rosmini F, Panetta V, Ferrigno L, Bonini S. Hay fever and asthma in relation to markers of infection in the United States. J Allergy Clin Immunol. 2002;110:381–7. doi: 10.1067/mai.2002.126658. [DOI] [PubMed] [Google Scholar]
- 12.Matricardi PM, Rosmini F, Ferrigno L, et al. Cross sectional retrospective study of prevalence of atopy among Italian military students with antibodies against hepatitis A virus. BMJ. 1997;314:999–1003. doi: 10.1136/bmj.314.7086.999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Linneberg A, Ostergaard C, Tvede M, et al. IgG antibodies against microorganisms and atopic disease in Danish adults: the Copenhagen Allergy Study. J Allergy Clin Immunol. 2003;111:847–53. doi: 10.1067/mai.2003.1335. [DOI] [PubMed] [Google Scholar]
- 14.Jarvis D, Luczynska C, Chinn S, Burney P. The association of hepatitis A and Helicobacter pylori with sensitization to common allergens, asthma and hay fever in a population of young British adults. Allergy. 2004;59:1063–7. doi: 10.1111/j.1398-9995.2004.00539.x. [DOI] [PubMed] [Google Scholar]
- 15.Bodner C, Anderson WJ, Reid TS, Godden DJ. Childhood exposure to infection and risk of adult onset wheeze and atopy. Thorax. 2000;55:383–7. doi: 10.1136/thorax.55.5.383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cullinan P, Harris JM, Newman Taylor AJ, et al. Can early infection explain the sibling effect in adult atopy? Eur Respir J. 2003;22:956–61. doi: 10.1183/09031936.03.00039102. [DOI] [PubMed] [Google Scholar]
- 17.Kaplan G, Totsuka A, Thompson P, Akatsuka T, Moritsugu Y, Feinstone SM. Identification of a surface glycoprotein on African green monkey kidney cells as a receptor for hepatitis A virus. EMBO J. 1996;15:4282–96. [PMC free article] [PubMed] [Google Scholar]
- 18.Illi S, von Mutius E, Lau S, et al. Early childhood infectious diseases and the development of asthma up to school age: a birth cohort study. BMJ. 2001;322:390–5. doi: 10.1136/bmj.322.7283.390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pelosi U, Porcedda G, Tiddia F, et al. The inverse association of salmonellosis in infancy with allergic rhinoconjunctivitis and asthma at school-age: a longitudinal study. Allergy. 2005;60:626–30. doi: 10.1111/j.1398-9995.2005.00747.x. [DOI] [PubMed] [Google Scholar]
- 20.Kosunen TU, Hook-Nikanne J, Salomaa A, Sarna S, Aromaa A, Haahtela T. Increase of allergen-specific immunoglobulin E antibodies from 1973 to 1994 in a Finnish population and a possible relationship to Helicobacter pylori infections. Clin Exp Allergy. 2002;32:373–8. doi: 10.1046/j.1365-2222.2002.01330.x. [DOI] [PubMed] [Google Scholar]
- 21.Matricardi PM, Rosmini F, Riondino S, et al. Exposure to foodborne and orofaecal microbes versus airborne viruses in relation to atopy and allergic asthma: epidemiological study. BMJ. 2000;320:412–17. doi: 10.1136/bmj.320.7232.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Abbas AK, Murphy KM, Sher A. Functional diversity of helper T lymphocytes. Nature. 1996;383:787–93. doi: 10.1038/383787a0. [DOI] [PubMed] [Google Scholar]
- 23.Herz U, Gerhold K, Gruber C, et al. BCG infection suppresses allergic sensitization and development of increased airway reactivity in an animal model. J Allergy Clin Immunol. 1998;102:867–74. doi: 10.1016/s0091-6749(98)70030-2. [DOI] [PubMed] [Google Scholar]
- 24.Zuany-Amorim C, Sawicka E, Manlius C, et al. Suppression of airway eosinophilia by killed Mycobacterium vaccae-induced allergen-specific regulatory T-cells. Nat Med. 2002;8:625–9. doi: 10.1038/nm0602-625. [DOI] [PubMed] [Google Scholar]
- 25.Sayers I, Severn W, Scanga CB, Hudson J, Le Gros G, Harper JL. Suppression of allergic airway disease using mycobacterial lipoglycans. J Allergy Clin Immunol. 2004;114:302–9. doi: 10.1016/j.jaci.2004.03.057. [DOI] [PubMed] [Google Scholar]
- 26.Yazdanbakhsh M, Kremsner PG, van Ree R. Allergy, parasites, and the hygiene hypothesis. Science. 2002;296:490–4. doi: 10.1126/science.296.5567.490. [DOI] [PubMed] [Google Scholar]
- 27.Cooper PJ. Intestinal worms and human allergy. Parasite Immunol. 2004;26:455–67. doi: 10.1111/j.0141-9838.2004.00728.x. [DOI] [PubMed] [Google Scholar]
- 28.Radon K, Danuser B, Iversen M, et al. Respiratory symptoms in European animal farmers. Eur Respir J. 2001;17:747–54. doi: 10.1183/09031936.01.17407470. [DOI] [PubMed] [Google Scholar]
- 29.Downs SH, Marks GB, Mitakakis TZ, et al. Having lived on a farm and protection against allergic diseases in Australia. Clin Exp Allergy. 2001;31:570–5. doi: 10.1046/j.1365-2222.2001.01070.x. [DOI] [PubMed] [Google Scholar]
- 30.Wickens K, Lane JM, Fitzharris P, et al. Farm residence and exposures and the risk of allergic diseases in New Zealand children. Allergy. 2002;57:1171–9. doi: 10.1034/j.1398-9995.2002.t01-1-23644.x. [DOI] [PubMed] [Google Scholar]
- 31.Riedler J, Braun-Fahrlaender C, Eder W, et al. Early life exposure to farming environment is essential for protection against the development of asthma and allergy: a cross-sectional survey. Lancet. 2001;358:1129–33. doi: 10.1016/S0140-6736(01)06252-3. [DOI] [PubMed] [Google Scholar]
- 32.Von Ehrenstein OS, von Mutius E, Illi S, et al. Reduced risk of hay fever and asthma among children of farmers. Clin Exp Allergy. 2000;30:187–93. doi: 10.1046/j.1365-2222.2000.00801.x. [DOI] [PubMed] [Google Scholar]
- 33.Remes ST, Iivanninen K, Koskela W, et al. Which factors explain the lower prevalence of atopy amongst farmers' children? Clin Exp Allergy. 2003;33:427–34. doi: 10.1046/j.1365-2222.2003.01566.x. [DOI] [PubMed] [Google Scholar]
- 34.Perkin MR, Strachan DP. Which aspects of the farming lifestyle explain the inverse association with childhood allergy? J Allergy Clin Immunol. 2006;117:1–374. doi: 10.1016/j.jaci.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 35.Smit LA, Zuurbier M, Doekes G, et al. Hay fever and asthma symptoms in conventional and organic farmers in the Netherlands. Occup Environ Med. 2007;64:101–7. doi: 10.1136/oem.2006.028167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Monso E, Schenker M, Radon K, et al. Region-related risk factors for respiratory symptoms in European and Californian farmers. Eur Respir J. 2003;21:323–31. doi: 10.1183/09031936.03.00070803. [DOI] [PubMed] [Google Scholar]
- 37.Monso E, Magarolas R, Radon K, et al. Respiratory symptoms of obstructive lung disease in European crop farmers. Am J Respir Crit Care Med. 2000;162:1246–50. doi: 10.1164/ajrccm.162.4.9912093. [DOI] [PubMed] [Google Scholar]
- 38.Ege MJ, Bieli C, Frei R, et al. Prenatal farm exposure is related to the expression of receptors of the innate immunity and to atopic sensitization in school-age children. J Allergy Clin Immunol. 2006;117:817–23. doi: 10.1016/j.jaci.2005.12.1307. [DOI] [PubMed] [Google Scholar]
- 39.Pfefferle PI, Büchele G, Blümer N, et al. Cord blood cytokines are modulated by maternal farming activities and consumption of farm dairy products during pregnancy – the PASTURE study. J Allergy Clin Immunol. 2010;125:108–15. doi: 10.1016/j.jaci.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 40.Portengen L, Sigsgaard T, Omland O, et al. Low prevalence of atopy in young Danish farmers and farming students born and raised on a farm. Clin Exp Allergy. 2002;32:247–53. doi: 10.1046/j.1365-2222.2002.01310.x. [DOI] [PubMed] [Google Scholar]
- 41.Dimich-Ward H, Chow Y, Chung J, et al. Contact with livestock – a protective effect against allergies and asthma? Clin Exp Allergy. 2006;36:1122–9. doi: 10.1111/j.1365-2222.2006.02556.x. [DOI] [PubMed] [Google Scholar]
- 42.Douwes J, Travier N, Huang K, et al. Lifelong farm exposure may strongly reduce the risk of asthma in adults. Allergy. 2007;62:1158–65. doi: 10.1111/j.1398-9995.2007.01490.x. [DOI] [PubMed] [Google Scholar]
- 43.Hoppin JA, Umbach DM, London SJ, et al. Pesticides and atopic and nonatopic asthma among farm women in the Agricultural Health Study. Am J Respir Crit Care Med. 2008;177:1–8. doi: 10.1164/rccm.200706-821OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Schulze A, van Strien RT, Praml G, et al. Characterisation of asthma among adults with and without childhood farm contact. Eur Respir J. 2007;29:1169–73. doi: 10.1183/09031936.00127906. [DOI] [PubMed] [Google Scholar]
- 45.Radon K, Schulze A, Nowak D. Inverse association between farm animal contact and respiratory allergies in adulthood: protection, underreporting or selection? Allergy. 2006;61:443–6. doi: 10.1111/j.1398-9995.2006.00995.x. [DOI] [PubMed] [Google Scholar]
- 46.Dorevitch S, Tharenos L, Demirtas H, et al. Inverse association between rural environment in infancy and sensitization to rodents in adulthood. Ann Allergy Asthma Immunol. 2007;98:440–6. doi: 10.1016/S1081-1206(10)60758-2. [DOI] [PubMed] [Google Scholar]
- 47.Radon K, Ehrenstein V, Praml G, et al. Childhood visits to animal buildings and atopic diseases in adulthood: an age-dependent relationship. Am J Ind Med. 2004;46:349–56. doi: 10.1002/ajim.20000. [DOI] [PubMed] [Google Scholar]
- 48.Radon K, Monso E, Weber C, et al. Prevalence and risk factors for airway diseases in farmers – summary of results of the European Farmers' Project. Ann Agric Environ Med. 2002;9:207–13. [PubMed] [Google Scholar]
- 49.Radon K. The two sides of the ‘endotoxin coin’. Occup Environ Med. 2006;63:73–8. doi: 10.1136/oem.2004.017616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Eduard W, Douwes J, Omenaas E, et al. Do farming exposures cause or prevent asthma? Results from a study of adult Norwegian farmers. Thorax. 2004;59:381–G. doi: 10.1136/thx.2004.013326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Portengen L, Preller L, Tielen M, et al. Endotoxin exposure and atopic sensitization in adult pig farmers. J Allergy Clin Immunol. 2005;5:797–802. doi: 10.1016/j.jaci.2004.11.046. [DOI] [PubMed] [Google Scholar]
- 52.Schram D, Doekes G, Boeve M, et al. Bacterial and fungal components in house dust of farm children, Rudolf Steiner school children and reference children – the PARSIFAL study. Allergy. 2005;60:611–8. doi: 10.1111/j.1398-9995.2005.00748.x. [DOI] [PubMed] [Google Scholar]
- 53.Braun-Fahrlander C, Riedler J, Herz U, et al. Environmental exposure to endotoxin and its relation to asthma in school-age children. N Engl J Med. 2002;347:869–77. doi: 10.1056/NEJMoa020057. [DOI] [PubMed] [Google Scholar]
- 54.van Strien RT, Engel R, Holst O, et al. Microbial exposure of rural school children, as assessed by levels of N-acetyl-muramic acid in mattress dust, and its association with respiratory health. J Allergy Clin Immunol. 2004;113:860–7. doi: 10.1016/j.jaci.2004.01.783. [DOI] [PubMed] [Google Scholar]
- 55.Smit LA, Heederik D, Doekes G, et al. Exposure–response analysis of allergy and respiratory symptoms in endotoxin-exposed adults. Eur Respir J. 2008;31:1241–8. doi: 10.1183/09031936.00090607. [DOI] [PubMed] [Google Scholar]
- 56.Lauener RP, Birchler T, Adamski J, et al. Expression of CD14 and Toll-like receptor 2 in farmers' and non-farmers' children. Lancet. 2002;360:465–6. doi: 10.1016/S0140-6736(02)09641-1. [DOI] [PubMed] [Google Scholar]
- 57.Ege MJ, Frei R, Bieli C, et al. Not all farming environments protect against the development of asthma and wheeze in children. J Allergy Clin Immunol. 2007;119:1140–7. doi: 10.1016/j.jaci.2007.01.037. [DOI] [PubMed] [Google Scholar]
- 58.Eder W, Klimecki W, Yu L, et al. Toll-like receptor 2 as a major gene for asthma in children of European farmers. J Allergy Clin Immunol. 2004;113:482–8. doi: 10.1016/j.jaci.2003.12.374. [DOI] [PubMed] [Google Scholar]
- 59.Leynaert B, Guilloud-Balaille M, Soussan D, et al. Association between farm exposure and atopy, according to the CD14C-159T polymorphism. J Allergy Clin Immunol. 2006;118:65845. doi: 10.1016/j.jaci.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 60.Smit LA, Bongers SI, Ruven HJ, et al. Atopy and new-onset asthma in young Danish farmers and CD14, TLR2, and TLR4 genetic polymorphisms: a nested case–control study. Clin Exp Allergy. 2007;37:1602–8. doi: 10.1111/j.1365-2222.2007.02831.x. [DOI] [PubMed] [Google Scholar]


