Abstract
Chest pain is the most common complaint among cocaine users who present to the ED seeking care and many hospital resources are applied to stratify cocaine users in regard to future cardiac morbidity and mortality. Little is known about the longitudinal cardiac and non cardiac medical outcomes of cocaine users who have been stratified to an ED observation period following their ED visit.
Objectives
to examine one-year cardiac outcomes in a low-intermediate risk sample of patients with cocaine- associated chest pain in an urban ED, as well as to examine ED recidivism one year for cardiac and non-cardiac complaints.
Methods
Prospective consecutive cohort study of patients (18–60 years) who presented to an urban Level 1 ED with cocaine-associated chest pain and were risk stratified to low-intermediate cardiac risk. Exclusion criteria: EKG suggestive of AMI, elevated serum cardiac markers, history of AMI or CABG, hemodynamic instability, unstable angina. Baseline interviews using validated measures of health functioning, and substance use were conducted during CPOU stay, and 3, 6, and 12 months. ED utilization during the study year was abstracted from medical chart. Zero-Inflated Poisson regression analyses were conducted to predict recurrent ED visits.
Results
219 participants (73% participation) were enrolled, 65% returned to the ED post index visit; 23% returned for chest pain, of these 66% had a positive cocaine urine screen. No patient had an AMI within the one year follow up period. Patients with continued cocaine use were more likely to have a recurrent ED visit (p<0.001) but these repeat visits were most often related to musculoskeletal pain (21%), and injury (30%) rather than potential cardiac complaints.
Conclusions
Patients with cocaine-associated chest pain who are low to intermediate cardiac risk and complete a CPOU protocol have less then 1% rate of MI in the subsequent 12-months.
Keywords: Alcohol, Chest Pain, Cocaine, Emergency Department
Introduction
Background
In 2005, over 800,000 emergency department (ED) visits involved a major substance of abuse; cocaine was involved in over half of such visits.1 Chest pain (CP) is the most common cocaine related ED complaint,2 with up to 20% of chest pain patients in urban cohorts having positive urine drug screens for cocaine.3–5 The incidence of acute myocardial infarction (MI) in patients who present with cocaine- associated chest pain is as high as 6%, and is 24 times more likely than not to occur in the first hour after use.6 Several differences exist between cocaine using chest pain patients vs. traditional patients with chest pain. Patients with cocaine-associated chest pain tend to be more often younger and male, with few traditional risk factors other than smoking, making the diagnosis and management of acute coronary syndrome (ACS) more challenging.7 Chronic cocaine abuse may lead to premature atherosclerosis, left ventricular hypertrophy, cardiomyopathy, and coronary ectasia, thus creating even greater risk for cardiovascular complication in this population7 and prompting a recent statement from the American Heart Association focusing specifically on management of Cocaine-Associated Chest Pain8.
Importance
At this time, the best approach for managing cocaine patients in the ED setting who present with chest pain, and who are at significant risk for myocardial infarction, is appropriate risk stratification. Due to the differing pathophysiology and demographics of cocaine- associated chest pain, classic cardiac risk stratification protocols may not be applicable. Weber and colleagues9 recently validated the safety of a brief observation period for patients specifically with cocaine-associated chest pain. In summary, patients who do not have evidence of ischemia or cardiovascular complications over a 9–12 hour period in a Chest Pain Observation Unit (CPOU) have a very low risk of short term death (30 days) from myocardial infarction. However, little is known about long term outcomes (cardiac or non-cardiac) in a cohort of low-intermediate risk patients with chest pain and recent cocaine use. One prior study has reported long-term (one year) follow-up data on cocaine using chest pain patients; however, this study was limited by the use of a convenience sample.10
In addition to cardiac complications, cocaine users are at elevated risk for other medical complications related to their cocaine use, based on the following factors: (1) IV route of administration (i.e., HIV, hepatitis cellulites, bacterial endocarditis); (2) direct toxicity of cocaine separate from route of administration (i.e., non-cardiac causes including seizure, or stroke); (3) psychological/psychiatric complications (i.e., depression, anxiety disorders, psychosis); and, (4) violent and non-violent related injuries.11 Although many hospital resources have been applied to stratify cocaine users in regard to cardiac risk little is known about the longitudinal outcomes of cocaine users following their ED visit for chest pain, including non-cardiac outcomes, limiting the understanding of how substance use interventions in this group may fully impact both future medical co-morbidities as well as ED service utilization.
Goals of this Investigation
To our knowledge prior research has not examined the longitudinal one-year outcomes among a risk stratified cohort of ED patients with low to intermediate risk for cardiac disease, to asses cardiac and non-cardiac outcomes and rates and correlates of ED recidivism. The first objective of this study was to examine one-year cardiac outcomes in a prospective risk -stratified sample of patients with cocaine- associated chest pain in an urban ED. A second study objective was to examine ED recidivism after one year, for cardiac and non-cardiac complaints, in this same cohort. It was hypothesized that patients with cocaine-associated chest pain (stratified as low/moderate risk for MI) who underwent a negative CPOU stay would have less than 1% risk for death or acute MI over the ensuing year; that ED recidivism and mortality of non cardiac complaints would be higher then that of cardiac complaints; and, ED service utilization over the study year would be positively correlated to ongoing cocaine use.
Methods
Study Design
This study examined a prospective cohort study of patients who presented to a large urban ED with cocaine related chest pain. The detailed methods of this study have been described previously.3, 13
Setting
This study was conducted at a university-affiliated Level I trauma center with an annual ED census of 75,000 patients. All procedures were approved by the university and hospitals' institutional review boards.
CPOU Evaluation
All patients undergoing ED observation for chest pain had cardiac markers measured at the time of presentation in the ED, and three, six, and nine hours after presentation. Continuous 12-lead ST-segment monitoring (Vectra XA, Hewlett–Packard Diagnostics) was performed by physician assistants. For this study, measurement of cardiac troponin I (Access Accu TnI, Beckman Coulter) was selected instead of measurement of the MB fraction of creatine kinase because previously published data suggest that troponin I is the marker protein most specific for myocardial injury in patients who have recently used cocaine.14 The levels of this marker were considered to be elevated if any measurement exceeded the institutional threshold for normal. Following negative enzymes, 9 hours apart, patients were given a referral to their primary care physician for outpatient stress testing.
Selection of Participants
Research staff present in the ED between the hours of 8a.m. and 10p.m., seven days per week, attempted to screen all chest pain patients undergoing a cardiac evaluation for acute coronary syndrome who came to the ED from June 1, 2002 through February 29, 2004. The institutional standard of care in the ED where the study was conducted requires that patients under age 60 who receive a workup for potential acute coronary syndrome (ACS) also undergo urine screening for cocaine metabolites (benzoylecognine) (Synchron® LX Systems).Patients who underwent a cardiac work up overnight (10pm– 8 am) were approached by the research assistant (RA) at 8 am prior to discharge from the CPOU. Patients were assessed for study inclusion based on the criteria below, not on the basis of the decision process of the emergency physicians at this institution on when to use the chest pain observation unit. A two-phase enrollment procedure was used. Consecutive patients age 18–60 with a chief complaint of chest pain (undergoing a cardiac evaluation as demonstrated by ordering of cardiac enzymes) were initially considered eligible for the study and approached by research staff to participate in the screening during the recruitment period. Additional Inclusion Criteria: Patients ages 18–60 with a positive urine screen for cocaine. If urine screen results were incomplete or unavailable, documentation in medical chart by provider that patient was being treated for cocaine-associated chest pain and patient self-reported cocaine use in the 48 hours prior to ED visit. Exclusion Criteria: Patients who were considered too high risk to complete a cardiac evaluation in the CPOU were excluded. Based upon criteria by Weber et al. (2003) patients with cocaine- associated chest pain were identified as high risk and were excluded if their initial electrocardiogram was suggestive of acute ischemia or acute myocardial infarct (MI); ST-segment elevation or depression of 1 mm or more that persisted for at least one minute; elevated serum levels of cardiac markers, or recurrent chest pain deemed to be unstable angina (on anticoagulants or requiring intravenous vasoactive medications (e.g. nitroglycerine). In addition because Weber et al (2003)9 found that patients with clinically significant coronary disease were more likely to have a non- fatal MI in the subsequent study period, patients with a history of prior AMI or coronary artery bypass surgery were also excluded. Patients with hemodynamic instability; and those directly admitted to the ICU from the ED were also deemed high risk (Table1).
Table 1.
Risk Stratification: Criteria For Patients With Cocaine-associated Chest Pain To Be Eligible For CPOU Protocol
| YES |
| ___Physician on evaluation requested cardiac evaluation for chest pain |
| ___Age 18–60 |
| NO |
| ___EKG with changes consistent with acute ischemia or acute myocardial infarct; ST-segment elevation or depression of 1 mm or more that persisted for at least one minute; |
| ___Elevated serum levels of cardiac markers (Troponin or CK- MB) |
| ___History of prior myocardial infarction or coronary artery bypass surgery |
| ___Homodynamic instability |
| ___Unstable angina (as indicated by use of Heperin, Lovanox or IV nitroglycerine) |
| ___Admission directly to the Intensive Care Unit from ED. |
Patients were also ineligible for the study if they did not undergo a cardiac evaluation (i.e., chest pain clearly due to trauma to chest per ED physician judgment with no cardiac enzymes ordered), if they were pregnant, unable to provide informed consent, were acutely suicidal, or demonstrated severe agitation requiring physical restraint. Cocaine use was confirmed with toxicological positive urine screening for cocaine metabolites (sensitivity of 95% and specificity of 100%; Synchron® LX Systems).15 After signing a written consent form, participants eligible for the study completed in a two-hour baseline interview conducted by trained research staff in the ED or CPOU (based on bed availability in the CPOU). Participants who completed the baseline assessment were given a $25 gift certificate to a local retailer (e.g., Wal-Mart, Target) to compensate them for their time.
Interview
Subjects who signed consent for the longitudinal study completed a two hour baseline interview before leaving the CPOU to collect information about socio-demographics, substance use (alcohol and illicit drugs) history, baseline physical and mental health. Measures included an assessment of substance use frequency and consequences from the Substance Abuse Outcomes Module (SAOM).16 The SAOM is designed for evaluation of substance abuse treatment outcomes (www.netoutcomes.net), and measures DSM-IV substance use disorders.17 In addition, the SAOM was used to also measure basic demographic information. The SAOM has been extensively tested and has been found to have excellent psychometric properties.16 The SAOM was administered at 3, 6, and 12 month interviews in person. Finally, the standard Medical Outcomes Study SF-36 Health Survey18 was used to assess health concepts relevant to functional status and well-being.19 For the purposes of this paper, the physical functioning index was used in analyses.
Follow Up Interviews
At baseline, participants were asked to provide locator information that would allow study personnel to contact them for follow-up interviews to be conducted at 3, 6, and 12-month post-baseline. Participants were informed in the consent form about the follow-up contact procedures. Participants were reimbursed $30 for the 3-month, $35 for the 6-month, and $45 for the in person12-month interview. During follow-up visits, participants were also asked to provide a urine specimen voluntarily for which they were provided an extra remuneration of $10. The urine drug screen (UDS) was obtained to encourage more accurate self-report of substance use.20–25
Chart Review
Records at the Hurley Medical Center (HMC), the study site, were reviewed by trained RA's at baseline as well as 12-months after the index ED visit. HMC is the only level 1 trauma center in Flint Michigan, therefore all major trauma/ injury in Flint is routed to HMC. Furthermore, HMC is the provider of choice for most patients treated; for example, 91% of patients who reported that they had any ED visit in the past three months at follow up interview, indicated that they had received ED care at the study site. Furthermore, 98% of patients who completed all follow-up interviews reported that their ED visits for chest pain over the study year occurred at the study site. At start of chart abstraction process there was a training period by physician staff as well as regular auditing of chart reviews to maintain reliability in keeping with the criteria described by Gilbert and Lowenstein26. A second investigator performed a review of a random sample of charts and determined that no discrepancies were found in abstraction of the required variables (i.e., variables to be extracted were clearly defined and not ambiguous). Regular meetings were held with RA staff to review coding rules and chart data. Information was specifically abstracted on: final diagnosis by ED staff (e.g., chest pain, injury, musculoskeletal pain, overdose, seeking detoxification, etc) and ED disposition (e.g., admitted to hospital, admitted to psych facility, discharged home). Details of chest pain related visits, including troponin levels, and results of urine cocaine screens ordered on repeat ED visits, were recorded. RA's verified participant mortality by searching public death record databases.
Data Analysis
We used SAS 9.1 and STATA 9.0 for analyses purposes. First, descriptive statistics were computed for baseline health and past year ED service use for cardiac chief complaint as well as ED visits for any reason. Approximately three-fourths (77%) of participants having zero recurrent ED visits related to chest pain and approximately one-third (35%) of the sample with zero recurrent ED visits for any reason in the study year. To analyze the association between selected variables and recurrent ED visits for chest pain as well as recurrent ED visits for any reason Zero-Inflated Poisson Regression models were performed. STATA's Vuong Test for both count variables (p-value = 0.0008 and p-value = 0.0041 respectively) confirmed that Zero-Inflated Poisson Regression model was a better model for both count variables instead of standard Poisson Regression model. All analyses were performed on the participant level. Independent variables were selected for inclusion in models based on hypotheses and prior literature on ED recidivism and included variables measured at the 12-month follow-up interview. Age, gender, race, education, past month substance use frequency (i.e., days of binge drinking, days of cocaine use), cardiac risk factors (i.e., hypertension, diabetes, tobacco use, prior coronary artery disease), physical functioning index, primary medical doctor (yes/no), and health insurance (yes/no) were the chosen independent variables for both models. The summary substance use variables included in the models were based on substance use over the year following the index ED visit and were computed by summing the number of days (e.g., binge drinking, cocaine use) used for each substance in the month prior to each follow-up interview (3-, 6- and 12 months)
Results
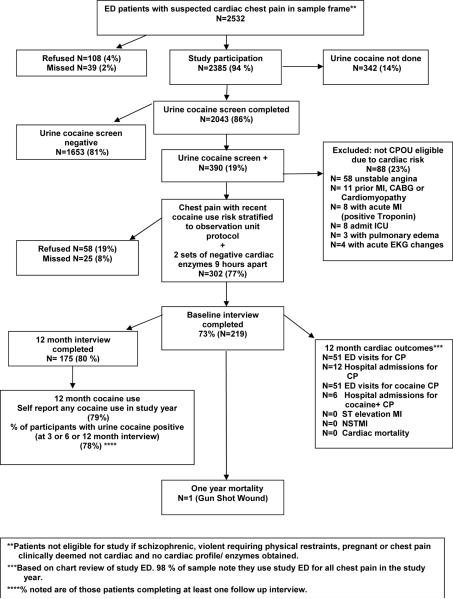
During the recruitment phase 2,532, patients presented to the ED with chest pain that was thought to be potentially cardiac by the ED medical staff. Four percent (n=108) refused to have staff view the urine cocaine results done as part of the ED standard chest pain protocol, and 2% (n=39) were missed by study staff busy with other participants, leaving 94% (n=2385) of patients agreeing to participate in the study. Of these, 86% (n=2043) had urine cocaine screens completed with 19% (n=390) having a positive urine drug screen for recent cocaine use. Eighty-eight (23%) of patients with cocaine- associated chest pain were deemed high risk and thus excluded from the study (see study flow sheet and outcome summary Figure 1). Of the remaining 77% (n= 302) of patients, 73% (n= 219) had 2 sets of negative cardiac enzymes, and agreed to complete a baseline evaluation, chart review, and participate in the study protocol, which included 3-, 6- and 12-month follow-up interviews. All patients were discharged from the ED. The mean length of stay in the CPOU was 12.5 hours (S. D. 4.8). Note that the first cardiac enzymes were usually drawn prior to transfer to CPOU from the ED. Follow-up interview completion rates were: 77%, 82%, and 80%, respectively. Study protocol included urine drug screens at all follow-up interviews; over 90% of participants complied with a urine drug screen (UDS) (91%, 91%, and 94% at each follow-up interview, respectively).
Figure 1.
Overview Of Study Inclusion And Outcomes
The study population (N=219) was predominantly male (65 %) and three-quarters were African-American (78 %). At baseline, participants reported an average number of 7.5 days of cocaine use in the past month (SD=8.5) and 84% reported cigarette use (Table 2). Among participants completing all three follow-up interviews (n=166), 79% (n=131) reported any cocaine use during the year following the ED index visit (e.g., reported at least one day of use during one of the 3, 6 and 12 month follow-up interviews). In addition, 78% (n=127) of participants providing a UDS (n= 163 during at least one of the 3-, 6-, or 12-month follow-up interviews) were positive for cocaine (indicating cocaine use in the previous 48–72 hours).
Table 2.
Selected Self Report Cocaine, Cardiac Risk, Medical History, Service Utilization and Insurance Status at Index ED Visit (for past year).
| Baseline ED Visit | ||
|---|---|---|
| N=219 | % | |
| Cocaine Use | ||
| Mean number days of cocaine use( SD) | 7.5 (8.5) | - |
| Cocaine use at time of presentation for chest pain was same or less then their usual amount of cocaine | 144 | 66% |
| First time they used this much cocaine | 118 | 54% |
| First ever use of cocaine | 13 | 6% |
| ED visits for chest pain prior to index visit | ||
| Participants with at least one visit to ED for chest pain | 81 | 37** |
| Participants with at least one visit to ED for chest pain ever prior to study enrollment | 84 | 39** |
| Have experienced chest pain similar to pain that caused by current ED visit with prior cocaine use (yes) | 56 | 26 |
| Cardiac | ||
| Hypertension | 66 | 30 |
| Diabetes | 13 | 6 |
| Tobacco use | 183 | 84 |
| Coronary artery disease | 6 | 3 |
| Cardiac Risk profile (sum of above 4 factors) (mean, SD) | 1.2 (0.69) | (90) > 1 risk factor |
| Family history of cardiac disease* | 93 | 42 |
| Hyperlipidemia > 220* | 15 | 7 |
| Prior Endocarditis | 2 | 1 |
| Congestive heart failure | 7 | 3 |
| Median # of visits to ED for chest pain past year | 1.0 | 23 |
| Participants with at least one visit to ED for chest pain in past year | 81 | 37** |
| Mean # of visits to ED for chest pain ever prior to study enrollment | 1.44 | 3.6 |
| Participants with at least one visit to ED for chest pain ever prior to study enrollment | 84 | 39** |
| Other medical history | ||
| Kidney trouble | 12 | 5 |
| Migraine headaches | 46 | 21 |
| Repeated stomach problems | 15 | 7 |
| Repeated trouble with neck/ back / spine | 35 | 16 |
| Stroke | 2 | 1 |
| Tuberculosis | 3 | 1 |
| Ulcer | 13 | 6 |
| Hepatitis B, C | 11 | 5 |
| Seizures | 5 | 2 |
| HIV | 1 | 0.5 |
| SF-36 Physical Health Function Index (mean, SD) | 72.6 (32.5) | --- |
| Injury | ||
| Past year sought medical care for unintentional injury | 10 | 5 |
| Past year sought medical care for intentional | 9 | 4 |
| Psychiatric | ||
| Past year mental health treatment/ counseling | 26 | 12 |
| Past year inpatient psychiatric | 8 | 4 |
| Access to Medical Care | ||
| Have a primary medical doctor (YES) | 135 | 62 |
| Have Health Insurance (NO) | 68 | 31 |
as indicated by physician on index visit chart review
have 1 or more ER visits
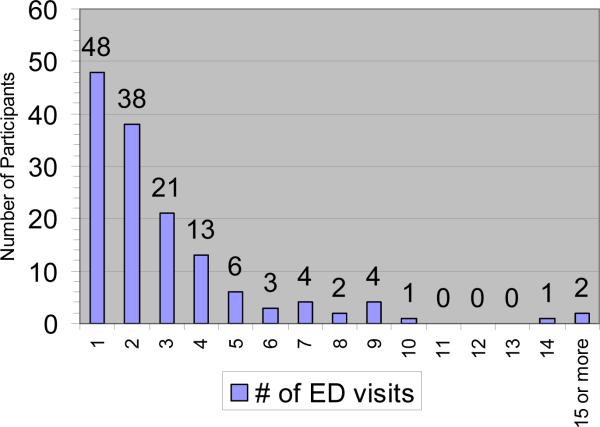
The medical record review showed that all 219 study participants (100%) returned to the study site, HMC, for medical care in the year following the index ED visit; one third (33% n=73) returned to outpatient clinics, 2% (n=4) were directly admitted to hospital from outpatient settings for non cardiac evaluations, 2% (n= 5) were directly admitted to psychiatry inpatient floor from the outpatient setting. The majority of participants 65% (n=143) returned to the study ED in the 12-months following the index ED visit (see Figure 2). Median number of visits, among participant who had any ED visits, was 2 (range of 1– 26, IQ range of 1 – 4). HMC is the provider of choice for most patients treated; 91% of participants, who noted yes on 12-month interview that they had any ED visit in past 3-months, indicated that they had received ED care at the study site. In regard to chest pain, 98% of participants who completed all three follow-up interviews self-reported that their ED visits for chest pain occurred at the study site during the year following their index ED visit.
Figure 2.
Number and frequency of ED visits in study year by 219 study participants. Sixty- Five percent (n=143) returned to ED over study year.
Baseline Health
Few participants noted that they were experiencing medical consequences of their cocaine use at index ED visit (see Table 2). Specifically, 30% of participants reported hypertension, 3.0% report CHF, 5.0% reported positive hepatitis status, and, 0.5% reported positive HIV status.
Cardiac Outcomes Over Subsequent 12 Months (Medical Record Review)
Approximately one quarter of the sample (23%, n=51/219) returned to the study ED for chest pain in the year following the index ED visit (Table 3). Among those participants presenting again to the study ED with chest pain, 66% (n=34/51) had a positive cocaine urine screen at time of presentation to the ED. Five percent of study participants (n=12/219) were hospitalized on repeat chest pain visits from the ED; of these, half had positive cocaine drug screens at time of readmission (Table 4) (see Thapa, et al, In Press27 for detailed longitudinal cocaine/substance use of sample). All patients hospitalized for chest pain were evaluated in the ED initially. However, no study participants had an elevated serum cardiac marker (troponin I) when evaluated for chest pain at the study ED (HMC) during the subsequent year following ED visit. Two patients had outpatient diagnostic cardiac catheterization. One of these patients was noted to have a fixed wall motion defect on outpatient stress testing. This patient, with a history of prior history of coronary artery disease, hypertension, and hyperlipidemia, went on to catheterization showing a single vessel lesion with recommendation for medical management. This same patient re-presented to ED two days following this catheterization with cocaine use and recurrent chest pain and negative cardiac enzymes. A second patient with a history of hypertension underwent outpatient stress testing showing global wall hypokinesis prompting outpatient catheterization which noted diffuse atherosclerosis without further acute intervention beyond medical management.
Table 3.
Reason for ED visit in the 12-months following baseline ED visit for cocaine-associated chest pain
| ED Visit Chief Complaint | Number of participants who returned to the ED N =219 (%) | Number of ED Visits | ED visits resulting in hospitalization |
|---|---|---|---|
| Cardiac | 104 | 15 | |
| Chest pain | 51 (23%) | 100 | 12 |
| Elevated Troponin | 0 | - | - |
| Positive cocaine at ED visit++ | N=34/51 (66%) | N=51/100 (51%) | - |
| Pulmonary Edema/CHF | 3 (1%) | 4 | 3 |
| Non Cardiac | |||
| Other Medical | -- | 178 | 7 |
| Musculoskeletal** | 45 (21%) | 60 | 0 |
| Wound Care /Abscess | 12 (5%) | 13 | 0 |
| Abdominal Pain / Flank | 18 (8 %) | 27 | 2 |
| CVA / TIA | 2 (1%) | 2 | 2 |
| Pulmonary / Asthma / URI | 34 (16%) | 53 | 3 |
| Gynecological/Urological/STDs | 19 (9 %) | 23 | 0 |
| Injury | -- | 83 | 4 |
| Unintentional | 43 (20%) | 53 | 2 |
| Intentional*** | 22(10%) | 30 | 2 |
| Psych | -- | 31 | 6 |
| Depression / Suicidal Ideation Psychosis / Anxiety | 18 (8 %) | 26 | 2 |
| Acute Intoxication / Overdose | (5%) | 15 | 4 |
| Other ** | 12 (5%) | 19 | 2 |
| Total | 143 (65%) | 415 | 34 |
13 visits had a documented negative Urine cocaine screen. 44 visits had incomplete urine drug screens (urine not given). Some patients returned multiple times. Study analysis at subject level(N)
Includes Dental Pain, Headache, and Back Pain.
2 participants were admitted to Surgery after Gun Shot Wounds. One fatality in ED from Gun Shot Wound
Includes Hives, Acute Venous Thrombosis, Medication Refill, Elevated Blood Sugar
Table 4.
Characteristics of Patients Hospitalized Following Return ER Visit For Chest Pain
| Age, gender | Cardiac Co-morbidities | Cocaine positive at repeat visit | EKG |
|---|---|---|---|
| 36yo male | Yes | No abnormalities | |
| 35yo female | Prior CVA | Yes | LVH Non-specific T-wave abnormalities |
| 43yo male | CAD (60–70 stenosis on prior cardiac cath) HTN, HLD |
Yes | Non-specific ST and T-wave abnormalities in multiple leads Setting of Viagra, and nitrates |
| 40yo male (3 admissions) | CAD s/p multiple stents HTN |
No × 3 admissions | 1st admission – no change 2nd,admission - interventricular delay, no ST or T-wave abnormalities 3rd admission – inverted T waves in V2–V3 |
| 45yo female | CHF, Afib, Severe tricuspid and mitral insufficiency | No | No abnormalities |
| 44yo female | DM, HTN | No | No abnormalities |
| 57yo male (2 admissions) | CAD HTN, PSVT |
No × 2 admission | 1st admission – no abnormalities 2nd admission (after angioplasty 1wk PTA) - ST elevations V2–V4 T- wave inversion V4–V6 |
| 41yo female | HTN CHF |
Yes | LBBB (age indeterminate) Negative stress echo prior to discharge |
| 49yo F | Yes | No abnormalities | |
| 41yo F | No | No abnormalities | |
| 42yo F | Yes | Not performed | |
| 39yo M | Aortic stenosis Aortic regurgitation COPD |
Yes | No abnormalities |
* All patients had negative cardiac markers × 3 as part of their inpatient evaluation and were discharged home.
Overall ED Utilization Visits During 12 Month Study Period (Medical Record Review)
The majority of participants (65%; n=143/219) returned to the study ED in the 12 months following the index ED visit (Figure 2). Median number of visits, among participant who had one or more ED visits, was 2 (range of 1– 26 and IQ range of 1 – 4). Among 219 baseline participants, 22% (n=48/219) had one ED visit, 17% (n=38/219) had 2 visits, 10% (n=21/219) had 3 visits, and 16% (n= 36/219) had 4 or more visits (range 4– 26). In the year following the ED index visit, 2 participants (1%) had an ED diagnosis of acute CVA, 5% (n=11/219) presented with non fatal overdose, and 8% (n=18/219) presented with suicidal ideation or major depression (Table 3).
In the year following the index ED visit, slightly more then a quarter (27%, n=60/219),of participants were evaluated in the ED for an injury (median number of visits = 1, range 1 – 4, IQ range 1 – 2). The majority of non-cardiac ED visits were related to musculoskeletal pain (e.g., headache, toothache, low back pain). As confirmed by search of national public death records, during the year following the index ED visit, only one fatality occurred, which was due to a gun shot wound. This patient was treated at HMC prior to death.
Predicting Recurrent ED Visits for Chest Pain
Zero-Inflated Poisson Regression analyses were performed to analyze the association between selected variables and recurrent ED visits for chest pain during the year following the index ED visit. As stated above, independent variables included: age, gender, race, education, past month summary substance use frequency (i.e., days of binge drinking, days of cocaine use), cardiac risk factors (i.e., hypertension, diabetes, tobacco use, prior coronary artery disease), physical health functioning, primary medical doctor (yes), and health insurance (yes). The overall model was significant (Likelihood Ratio Chi-Square = 48.04, DF = 10, p-value < 0.001) with gender, age, cardiac risk factors, medical doctor and health insurance as significant predictors. A greater number of recurrent ED visits for chest pain was reported by females, older patients, participants with less cardiac risk factors, those who did not have a medical doctor, and those with health insurance (Table 5).
Table 5.
Zero-Inflated Poisson Regression To Analyze The Association Between Recurrent ED visits for chest pain using study year and 12 month characteristics
| Characteristics | IRR | CI |
|---|---|---|
| Demographic | ||
| Gender (Male)*** | 0.12 | (0.06, 0.27) |
| Age** | 1.06 | (1.02, 1.10) |
| Race (African-American) | 0.61 | (0.30, 1.21) |
| Education (High School grad or more) | 1.10 | (0.59, 2.03) |
| Substance use frequency ++ | ||
| Total Days binge drinking | 1.00 | (0.98, 1.01) |
| Total Days using crack/cocaine | 1.01 | (0.99, 1.02) |
| Cardiac risk profile*** | 0.36 | (0.21, 0.60) |
| SF-36 Physical Health Functioning Index | 1.00 | (0.99, 1.01) |
| Have a primary medical doctor? (yes)*** | 0.09 | (0.04, 0.20) |
| Have Health Insurance? (yes)*** | 9.43 | (2.44, 36.50) |
p< 0.05
p<0.01
p<0.001
IRR: Incidence rate ratio
summary variables of use over the study year from 3, 6, 12 month survey
Example of clinical interpretation of model in regard to repeat visits for chest pain: males have 0.12 times less recurrent ED visits than females. Those participants who have health insurance have 9.43 times more ED visits for chest pain than those who do not have health insurance.
Predicting ED Utilization over Study Year
Zero-inflated Poisson regression analyses were used were performed to analyze the association between selected variables and frequency of recurrent ED visits (as a count variable) over the 12-month follow-up period based on the independent variables described above. The overall model was significant (Likelihood Ratio Chi-Square = 49.71, DF=10, p-value < 0.001), with race, days of cocaine use, medical doctor and health insurance as significant predictors. A greater number of ED visits in the year following the index ED visit was predicted by non African American race, more days of self-reported cocaine use, lack of a primary medical doctor and those with health insurance (Table 6).
Table 6.
Zero-Inflated Poisson Regression to Analyze the Association of # of ED visits using study year and 12 month characteristics
| Characteristics | IRR | CI |
|---|---|---|
| Demographic | ||
| Gender (Male) | 0.82 | (0.617, 1.08) |
| Age | 1.00 | (0.99, 1.01) |
| Race (African-American)* | 0.70 | (0.52, 0.93) |
| Education (High School grad or more) | 0.90 | (0.70, 1.17) |
| Substance use frequency ++ | ||
| Total Days binge drinking* | 0.99 | (0.99, 1.00) |
| Total Days using crack/cocaine*** | 1.02 | (1.01, 1.02) |
| Cardiac risk profile | 1.00 | (0.80, 1.26) |
| SF-36 Physical Health Functioning Index* | 0.99 | (0.99, 1.00) |
| Have a primary medical doctor? (yes)*** | 0.60 | (0.45, 0.82) |
| Have Health Insurance? (yes)*** | 1.99 | (1.40, 2.85) |
p< 0.05
p<0.01
p<0.001
IRR: Incidence rate ratio
summary variables of use over the study year from 3, 6, 12 month survey
Example of clinical interpretation of model: African-Americans have 0.70 times less ED visits. For every extra day of cocaine use that participants endorsed they had 1.02 times more ED visits. Those with better or higher physical functioning score have 0.99 times less ED visits. Those who have health insurance have 1.99 times more ED visits for than those who do not have health insurance.
Discussion
Data from this prospective longitudinal cohort study of patients with chest pain and recent cocaine use who have been risk stratified to be low or intermediate cardiac risk and discharged following a CPOU protocol (negative cardiac enzymes 9 hours apart) show that these patients are at very low likelihood of having an MI in the subsequent one year. One quarter of these cocaine users with chest pain returned to the study ED for chest pain in the year following the index ED visit, of whom 66% reported recent cocaine use at the time of repeat ED visit. Only 5% were admitted for further cardiac workup on subsequent visit and of these, 64% had recently used cocaine. The majority (79%) of participants completing all follow ups reported recurrent cocaine use at some point over the study year27 and 78% had a positive urine screen at the time of the follow-up interview. Taken together, these findings suggest that self-report of cocaine use appeared to be valid, the cocaine use was often recent, and that that cocaine use is not a rare event following negative CPOU visit for cocaine-related chest pain. These findings are consistent with Hollander et al10 who studied a cohort of 203 patients with cocaine-associated chest pain over one year and found that 60% reported continued cocaine use. However, it is important to note from our prior report that a substantial proportion of the patients (50%)in this cohort were able to abstain from cocaine use at least in the first three months of their index ED visit for cocaine-associated chest pain.27
Data from the current study found that of all 390 patients presenting to the ED with cocaine associate chest pain who were enrolled in the study 23% were classified as high risk, with 8 patients (2%) presenting to the ED with an acute MI and 15 more (4%) with acute pulmonary edema, EKG changes or hemodynamic changes requiring ICU admission on presentation to the ED. These high risk patients were not eligible for study inclusion. No patients completing the CPOU protocol (n= 219), had elevated troponin I or returned to the ED with an acute MI during the study year. Prior literature10 of a non-risk stratified sample of patients with chest pain and recent cocaine use found only 1% returned with a non fatal MI, with 75% returning to the ED for chest pain in a 12-month period, a much higher proportion than the 23% of patients with recurrent ED visits in our study. In a retrospective study of 197 patients only 1 patient (4.5%) developed an MI28. Our findings support previous data that has validated the short term (30 day) mortality in CPOU patients9 and extends the understanding of this risk stratification in a new cohort of patients to one year outcomes. Building on the risk criteria and conclusions for developed by Weber9 (2003) to also exclude those with prior MI or CABG, the non- fatal rate of MI was lower in this sample (zero) compared to prior studies in other cohorts (Weber9 2003, non fatal MI rate was 2%). In addition all patients in this group were discharged home. The lower rates of recurrent ED visits for chest pain than found by Hollander et al,29may reflect an earlier stage of cardiovascular disease occurring in our sample by exclusion of the high risk group. Detailed review of the participants who were hospitalized on repeat ED visit suggests that these patients were older (all but one was in their 40's or 50's) and several had other cardiac disease that was not specifically part of study exclusion criteria (i.e., congestive heart failure, valvular disease, or prior cardiac stents without prior MI).
Somewhat surprisingly, ongoing substance use did not significantly predict recurrent ED visit for chest pain. A greater number of recurrent ED visits for chest pain was reported by females, older patients, those who did not have a medical doctor, and those with health insurance. Those patients with more cardiac risk factors were less likely to return to the ED for chest pain; this somewhat counterintuitive finding may be related to the exclusion of high risk patients. For example, in this sample, the majority of patients had a single cardiac risk factor, namely, tobacco use. In addition, patients who are aware of a diagnosis of hypertension, hyperlipidemia, and coronary heart disease (the other 3 cardiac risk factors listed), may be more likely to have a primary care doctor, which was significantly related to fewer ED visits. It should be noted that although the one year event rate of MI in this sample was low, these patients may have cardiovascular disease (as evidenced by the 2 patients who underwent catheterization), and that disease may be accelerated by their cocaine use.
In addition to cardiac outcomes, this study evaluated the reasons and frequency of ED recidivism other than for chest pain. The majority of participants were treated in the ED in the study year (65%), despite many reporting access to a primary care physician. Cocaine use was a robust predictor of recurrent ED visit for any reason, highlighting the need for interventions and referrals for cocaine use during ED visits to decrease future morbidity, mortality and ED costs. Consistent with prior literature30 participants with health insurance and who do not have a primary doctor were more likely to utilize the ED for care, likely because they had less preventative care and/or undiagnosed co-morbidities, and also were not financially inhibited from a potentially expensive ED visit.
Cocaine use is associated with several other medical complications including but not limited to neurovascular, pulmonary, psychiatric, as well as the association of substance use, specifically cocaine to injury (both unintentional and interpersonal violence). IV injection of cocaine as well as other drugs used in conjunction with cocaine is a well-known risk factor for HIV and hepatitis through needle sharing. However other complications of IV route of administration include cellulitis, local skin infection at the site of injection11 bacterial endocarditis, and granulomatous pulmonary reactions leading to chronic dyspnea.31 The effects of direct toxicity are primarily related to the physiological effect of vasospasm leading to chest pain. More serious neurological side effects such as seizure, stroke or TIA's are common especially with high levels of cocaine.32 Over the past 10 years cocaine has become the most common agent associated with drug-related stroke.33 Indeed in this sample of cocaine users two participants were diagnosed on repeat ED visit with CVA. Common pulmonary consequences of cocaine use include chronic cough, pneumothorax and bacterial pneumonia with 15% of this sample returning to the ED with pulmonary complaints. Psychiatric disorders are common comorbid conditions among cocaine users. Prior work from this sample found 42% reported moderate or severe depression.34 This sample of cocaine users also had high psychiatric co- morbidity with half as many hospitalizations for psychiatric complaints as for recurrent chest pain.
Finally, prior work with this cohort,35 as well in other cohorts (Weber9 2003) found that this group of cocaine users experience high rates violent victimization and perpetration during the year following the index ED visit. After chest pain, the most common presenting complaint in the year following CPOU visit was injury, with the only study fatality related to gun shot wounds. The high rate of injury among this population of cocaine users underscores that while significant time and ED resources are used to identify patients as low to intermediate risk for future cardiovascular events the largest risk for future morbidity and mortality may be injury and violence.
Limitations
Several limitations of this research require acknowledgement. First, data is based on self-report; however, procedures were implemented to increase reliability and validity of self-reports including provision of a research context in which confidentiality was assured; urine samples were obtained for drug testing which may enhance self-report; and, standardized measures were used. Second, ED recidivism is based on chart review from a single hospital and patients may have used other ED's; thus, our reported findings may represent an underreporting of true rates of complications post CPOU visit. However, our prior work and current interview suggests that the study hospital is the preferred ED for participants (98% of ED visits over the study year for complaints of chest pain were at study site) and indeed all participants returned to the study health care system in the one year period. Finally, it should be noted that although the event rate of acute MI during the study year was low, many of these patients have coronary artery disease which other literature suggests8 is accelerated by cocaine use, and may not become evident in a one year study.
Conclusions
Low to intermediate risk patients with cocaine associated chest pain who have a negative CPOU evaluation have less than 1% risk of MI in the subsequent 12 months. However, the majority of patients in this study continue to use cocaine after their ED visit and this cocaine use significantly predicted ED recidivism, highlighting the need for substance use interventions in this population during an ED visit for chest pain
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Substance Abuse and Mental Health Services Administration Office of Applied Studies, Department of Health and Human Services; Rockville, MD: Drug Abuse Warning Network, 2005: National Estimates of Drug-Related Emergency Department Visits. 2007 SMA 07-4256.
- 2.Minor RL, Jr., Scott BD, Brown DD, et al. Cocaine-induced myocardial infarction in patients with normal coronary arteries. Ann Intern Med. 1991 Nov 15;115(10):797–806. doi: 10.7326/0003-4819-115-10-797. [DOI] [PubMed] [Google Scholar]
- 3.Booth BM, Weber JE, Walton MA, et al. Characteristics of cocaine users presenting to an emergency department chest pain observation unit. Acad Emerg Med. 2005 Apr;12(4):329–337. doi: 10.1197/j.aem.2004.11.021. [DOI] [PubMed] [Google Scholar]
- 4.Qureshi AI, Suri MF, Guterman LR, et al. Cocaine use and the likelihood of nonfatal myocardial infarction and stroke: data from the Third National Health and Nutrition Examination Survey. Circulation. 2001 Jan 30;103(4):502–506. doi: 10.1161/01.cir.103.4.502. [DOI] [PubMed] [Google Scholar]
- 5.Hollander JE, Todd KH, Green G, et al. Chest pain associated with cocaine: an assessment of prevalence in suburban and urban emergency departments. Ann Emerg Med. 1995 Dec;26(6):671–676. doi: 10.1016/s0196-0644(95)70035-8. [DOI] [PubMed] [Google Scholar]
- 6.Mittleman MA, Mintzer D, Maclure M, et al. Triggering of myocardial infarction by cocaine. Circulation. 1999 Jun 1;99(21):2737–2741. doi: 10.1161/01.cir.99.21.2737. [DOI] [PubMed] [Google Scholar]
- 7.Hollander JE, Henry TD. Evaluation and management of the patient who has cocaine-associated chest pain. Cardiology clinics. 2006 Feb;24(1):103–114. doi: 10.1016/j.ccl.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 8.McCord J, Jneid H, Hollander JE, et al. Management of cocaine-associated chest pain and myocardial infarction: a scientific statement from the American Heart Association Acute Cardiac Care Committee of the Council on Clinical Cardiology. Circulation. 2008 Apr 8;117(14):1897–1907. doi: 10.1161/CIRCULATIONAHA.107.188950. [DOI] [PubMed] [Google Scholar]
- 9.Weber JE, Shofer FS, Larkin GL, et al. Validation of a brief observation period for patients with cocaine-associated chest pain. N Engl J Med. 2003 Feb 6;348(6):510–517. doi: 10.1056/NEJMoa022206. [DOI] [PubMed] [Google Scholar]
- 10.Hollander JE, Hoffman RS, Gennis P, et al. Cocaine-associated chest pain: one-year follow-up. Acad Emerg Med. 1995 Mar;2(3):179–184. doi: 10.1111/j.1553-2712.1995.tb03191.x. [DOI] [PubMed] [Google Scholar]
- 11.Haverkos HW, Lange WR. From the Alcohol, Drug Abuse, and Mental Health Administration. Serious infections other than human immunodeficiency virus among intravenous drug abusers. The Journal of infectious diseases. 1990 May;161(5):894–902. doi: 10.1093/infdis/161.5.894. [DOI] [PubMed] [Google Scholar]
- 12.Fuda KK, Immekus R. Frequent users of Massachusetts emergency departments: a statewide analysis. Ann Emerg Med. 2006 Jul;48(1):9–16. doi: 10.1016/j.annemergmed.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 13.Cunningham R, Walton MA, Tripathi SP, et al. Past-year violence typologies among patients with cocaine-related chest pain. Am J Drug Alcohol Abuse. 2007;33(4):571–582. doi: 10.1080/00952990701407512. [DOI] [PubMed] [Google Scholar]
- 14.Hollander JE, Levitt MA, Young GP, et al. Effect of recent cocaine use on the specificity of cardiac markers for diagnosis of acute myocardial infarction. American heart journal. 1998 Feb;135(2 Pt 1):245–252. doi: 10.1016/s0002-8703(98)70089-4. [DOI] [PubMed] [Google Scholar]
- 15.Tietz NW. Tietz Fundamentals of Clinical Chemistry. 4th Edition ed. W.B. Saunders Company; Philadelphia, PA: 1996. [Google Scholar]
- 16.Smith GR, Burnam MA, Mosley CL, et al. Reliability and validity of the substance abuse outcomes module. Psychiatr Serv. 2006 Oct;57(10):1452–1460. doi: 10.1176/ps.2006.57.10.1452. [DOI] [PubMed] [Google Scholar]
- 17.American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. Fourth Edition. Fourth ed. American Psychiatric Press; Washington, DC: 1994. [Google Scholar]
- 18.Ware JE. SF-36 Health Survey: Manual and Interpretation Guide. The Health Institute, New England Medical Center; Boston, MA: 1993. [Google Scholar]
- 19.Ware JE, Jr., Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992 Jun;30(6):473–483. [PubMed] [Google Scholar]
- 20.Gray TA, Wish E. Correlates of Underreporting Recent Drug Use in Female Arrestees: A Test of the Literature. J Drug Issues. 1999;29(1):91–106. Winter, 1999. [Google Scholar]
- 21.Hamid R, Deren S, Beardsley M, et al. Agreement between urinalysis and self-reported drug use. Subst Use Misuse. 1999 Sep;34(11):1585–1592. doi: 10.3109/10826089909039416. [DOI] [PubMed] [Google Scholar]
- 22.Hser YI. Self-reported drug use: results of selected empirical investigations of validity. NIDA Res Monogr. 1997;167:320–343. [PubMed] [Google Scholar]
- 23.Hser YI, Maglione M, Boyle K. Validity of self-report of drug use among STD patients, ER patients, and arrestees. Am J Drug Alcohol Abuse. 1999 Feb;25(1):81–91. doi: 10.1081/ada-100101847. [DOI] [PubMed] [Google Scholar]
- 24.Mieczkowski T. The operational styles of crack houses in Detroit. NIDA Res Monogr. 1990;103:60–91. [PubMed] [Google Scholar]
- 25.Mieczkowski T, Newel R, Wraight B. Using hair analysis, urinalysis, and self-reports to estimate drug use in a sample of detained juveniles. Subst Use Misuse. 1998 Jun;33(7):1547–1567. doi: 10.3109/10826089809069812. [DOI] [PubMed] [Google Scholar]
- 26.Gilbert EH, Lowenstein SR, Koziol-McLain J, et al. Chart reviews in emergency medicine research: Where are the methods? Ann Emerg Med. 1996 Mar;27(3):305–308. doi: 10.1016/s0196-0644(96)70264-0. [DOI] [PubMed] [Google Scholar]
- 27.Thapa PB, Walton MA, Cunningham RM, et al. Longitudinal Substance Use Following An Emergency Department Visit for Cocaine-Associated Chest Pain. J Drug Issues. In Press. [Google Scholar]
- 28.Kushman SO, Storrow AB, Liu T, et al. Cocaine-associated chest pain in a chest pain center. Am J Cardiol. 2000 Feb 1;85(3):394–396. A310. doi: 10.1016/s0002-9149(99)00755-9. [DOI] [PubMed] [Google Scholar]
- 29.Hollander JE, Hoffman RS, Burstein JL, et al. Cocaine-associated myocardial infarction. Mortality and complications. Cocaine-Associated Myocardial Infarction Study Group. Arch Intern Med. 1995 May 22;155(10):1081–1086. [PubMed] [Google Scholar]
- 30.Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004 Feb;42(2):176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]
- 31.Stein MD. Medical complications of intravenous drug use. J Gen Intern Med. 1990 May–Jun;5(3):249–257. doi: 10.1007/BF02600544. [DOI] [PubMed] [Google Scholar]
- 32.Levine SR, Brust JC, Futrell N, et al. Cerebrovascular complications of the use of the “crack” form of alkaloidal cocaine. N Engl J Med. 1990 Sep 13;323(11):699–704. doi: 10.1056/NEJM199009133231102. [DOI] [PubMed] [Google Scholar]
- 33.Kaku DA, Lowenstein DH. Emergence of recreational drug abuse as a major risk factor for stroke in young adults. Ann Intern Med. 1990 Dec 1;113(11):821–827. doi: 10.7326/0003-4819-113-11-821. [DOI] [PubMed] [Google Scholar]
- 34.Wryobeck JM, Lippo G, McLaughlin V, et al. Psychosocial aspects of pulmonary hypertension: a review. Psychosomatics. 2007 Nov–Dec;48(6):467–475. doi: 10.1176/appi.psy.48.6.467. [DOI] [PubMed] [Google Scholar]
- 35.Walton MA, Cunningham RM, Chermack ST, et al. Correlates of violence history among injured patients in an urban emergency department: gender, substance use, and depression. J Addict Dis. 2007;26(3):61–75. doi: 10.1300/J069v26n03_07. [DOI] [PubMed] [Google Scholar]