Abstract
The spread of avian H5N1 influenza viruses around the globe has become a worldwide public health concern. To evaluate the pathogenic potential of reassortant viruses between currently cocirculating avian H5N1 and human H3N2 influenza viruses, we generated all the 254 combinations of reassortant viruses between A/chicken/South Kalimantan/UT6028/06 (SK06, H5N1) and A/Tokyo/Ut-Sk-1/07 (Tok07, H3N2) influenza viruses by reverse genetics. We found that the presence of Tok07 PB2 protein in the ribonucleoprotein (RNP) complex allowed efficient viral RNA transcription in a minigenome assay and that RNP activity played an essential role in the viability and replicative ability of the reassortant viruses. When the pathogenicity of 75 reassortant H5 viruses was tested in mice, 22 were more pathogenic than the parental SK06 virus, and three were extremely virulent. Strikingly, all 22 of these viruses obtained their PB2 segment from Tok07 virus. Further analysis showed that Tok07 PB1 alone lacked the ability to enhance the pathogenicity of the reassortant viruses but could do so by cooperating with Tok07 PB2. Our data demonstrate that reassortment between an avian H5N1 virus with low pathogenicity in mice and a human virus could result in highly pathogenic viruses and that the human virus PB2 segment functions in the background of an avian H5N1 virus, enhancing its virulence. Our findings highlight the importance of surveillance programs to monitor the emergence of human H5 reassortant viruses, especially those containing a PB2 segment of human origin.
Keywords: influenza reassortants, pathogenicity, pandemic
The genome of influenza A virus is composed of eight single-stranded, negative-sense RNA segments. This unique genome arrangement allows the exchange of gene segments between two influenza viruses that coinfect a single host cell, a process known as “reassortment.” Reassortment is one mechanism by which pandemic viruses emerge and spread in immunologically naïve human populations (i.e., by introducing HA or HA and NA genes of avian virus origin into a human virus background), as occurred with the 1957 H2N2 “Asian flu” and the 1968 H3N2 “Hong Kong flu” (1, 2).
The H5N1 influenza virus was first isolated from geese in 1996 in China (3, 4). Soon afterwards, it infected 18 people in Hong Kong, six of whom died as a result of the infection (5, 6). Since the H5N1 influenza outbreak in Asian poultry in 2003 (8), H5N1 influenza viruses have spread to wild birds and poultry in several continents (7) and have resulted in 442 confirmed human cases and 262 deaths (World Health Organization; http://www.who.int). Fortunately, the H5N1 viruses still lack the ability to transmit efficiently among humans. However, this obstacle may be overcome by reassortment with cocirculating human H1N1 or H3N2 influenza viruses. The next pandemic then will be inevitable. It therefore is important to evaluate the pathogenicity of such reassortants. Chen et al. (9) attempted to generate 63 (26 − 1 parent virus) reassortant viruses between A/Thailand/16/04 (H5N1) and A/Wyoming/3/03 (H3N2) viruses containing the H5N1 HA and NA genes, together with an additional virus that had H5 HA and N2 NA genes and tested the virulence in mice of 39 of the reassortant viruses generated. They found that these reassortant viruses displayed a broad spectrum of pathogenicity in the mouse model. However, all these reassortants demonstrated attenuated pathogenicity compared with the wild-type A/Thailand/16/04 virus. These findings might suggest that, even though reassortment between H5N1 and human H3N2 viruses is likely in nature, the generation of competitive and highly pathogenic viruses may not be as likely as presently feared.
We therefore asked whether the findings of Chen et al. (9) could be generalized to all the avian H5N1 and human H3N2 influenza viruses currently cocirculating. To answer this question, we systematically generated all 254 (28 − 2 parent viruses) combinations of reassortant viruses between the avian H5N1 (A/Chicken/South Kalimantan/UT6028/06, SK06) and human H3N2 (A/Tokyo/Ut-Sk-1/07, Tok07) influenza viruses and tested the pathogenicity in mice of 75 reassortant viruses with H5 HA genes, which potentially would pose the greatest threat to humans. Here, we report that reassortment between avian H5N1 and human H3N2 influenza viruses indeed can generate hybrid viruses with substantial virulence and demonstrate that the human PB2 gene is necessary but not sufficient for the conversion of H5 viruses to a highly pathogenic phenotype.
Results
Phenotyping of the Replicative Abilities of the Reassortant Viruses Between SK06 and Tok07.
To understand how pathogenic the reassortant viruses could be to humans, we attempted to generate all of the 254 combinations of reassortants between the SK06 and Tok07 viruses by reverse genetics. Forty-eight hours posttransfection of plasmids in 293T cells, the supernatant was inoculated into Madin-Darby canine kidney (MDCK) cells to make virus stocks. Based on the titers of the virus stocks, the reassortant viruses were categorized into four groups: (i) Highly replicative viruses (Table S1). Numbers in the virus names denote the gene segments derived from Tok07 virus as follows: 1, PB2; 2, PB1; 3, PA; 4, HA; 5, NP; 6, NA; 7, M; 8, NS; for example, “r2,3” stands for the reassortant virus containing Tok07 PB1, Tok07 PA, and its other six segments from SK06 virus. The segments derived from SK06 virus are not shown. These viruses grew efficiently in MDCK cells with titers >107 pfu/mL. This group contained 96 viruses, 62 containing the SK06 HA gene and 34 that possessed the Tok07 HA gene. (ii) Moderately replicative viruses (Table S2). The virus titers in this group ranged from 104 to 106 pfu/mL and comprised 68 reassortant viruses: 26 H5 and 42 H3 viruses. (iii) Low replicative viruses (Table S3). The viruses in this group grew poorly in MDCK cells with titers ranging from 101 to 103 pfu/mL. This group contained 20 viruses: 12 H5 and 8 H3 viruses. (iv) Nonviable viruses (Table S4). The viruses in this group produced no visible cytopathic effects (CPE) and did not form visible plaques in MDCK cells. Of the total 254 combinations of reassortant viruses, 70 belonged to this nonviable group. It is noteworthy that 55 of these viruses derived their NP gene from the Tok07 virus, and 36 derived their NS segment from the SK06 virus, suggesting possible incompatibility between the human NP and avian NS genes.
Minigenome Assay to Determine Ribonucleoprotein Complex Activities in Vitro.
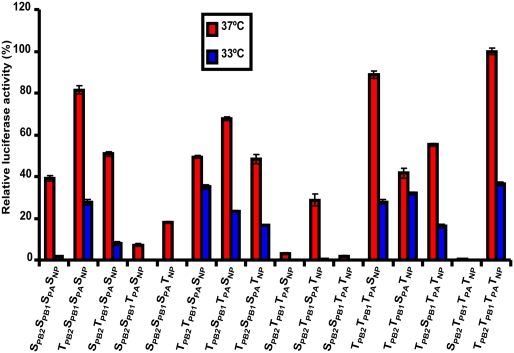
Previously, by using a minigenome assay, we demonstrated that the replication and transcription activity of the ribonucleoprotein (RNP) complex is a restricting factor for influenza virus reassortment (10). Therefore, to evaluate the possible relationship between RNP activity and the differences in viability and replicative ability of our reassortant viruses, we determined the activity of the 16 combinations of RNP complex between the SK06 and Tok07 viruses by measuring the activity of luciferase, which was encoded by a virus-like genome. As shown in Fig. 1, at 37 °C the RNP complex of the wild-type Tok07 virus, TPB2TPB1TPATNP (“T’ indicates Tok07 virus) exhibited the highest activity of all of the 16 combinations tested. The RNP activity of the wild-type SK06 virus, SPB2SPB1SPASNP (“S” indicates SK06 virus) was ≈40% of that of TPB2TPB1TPATNP. It is noteworthy that all the seven hybrid RNP combinations containing Tok07 PB2 protein showed higher activity than the RNP combination SPB2SPB1SPASNP. Strikingly, the RNP activity of combinations SPB2SPB1TPASNP, SPB2TPB1TPASNP, SPB2SPB1TPATNP, and SPB2TPB1TPATNP, all of which contained SK06 PB2 and Tok07 PA proteins, were significantly reduced compared with those of TPB2TPB1TPATNP and even SPB2SPB1SPASNP. These findings mirror our previous findings with A/equine/Prague/1/56 (H7N7) and A/Yokohama/2017/03 (H3N2) reassortants, suggesting that compatibility among polymerase subunits is a determinant of RNP activity and reassortment (10). At 33 °C, the RNP activity of SPB2SPB1SPASNP dropped substantially compared with its actvity at 37 °C. However, even at 33 °C, the RNP complex of TPB2TPB1TPATNP still exhibited 36% of the activity observed at 37 °C. Of note, except for TPB2TPB1TPATNP, the seven RNP combinations containing Tok07 PB2 protein retained considerable RNP activity at 33 °C. We then further analyzed our virus rescue data by correlating them with the RNP activity. All 96 viruses in the highly replicative group possessed RNP complexes with high activity in the minigenome assay (see the RNP combinations SPB2SPB1SPASNP and SPB2TPB1SPASNP and the eight RNP combinations containing human PB2 protein), with only three exceptions (see viruses r2,3, r5,7,8, and r2,5,7,8 in Table S1) that could grow up to 107 pfu/mL after 72-h incubation on MDCK cells. By contrast, the RNP activity for most of the viruses in the nonviable group was low. For example, none of the 32 viruses with the RNP combinations SPB2SPB1TPATNP or SPB2TPB1TPATNP could be rescued (Table S4), and these two combinations had the lowest RNP activity in the minigenome assay. These results confirm our previous finding that RNP activity plays an important role in the viability and replicative ability of reassortant viruses (10).
Fig. 1.
Luciferase activity of the 16 RNP combinations between the SK06 and Tok07 viruses. The minigenome reporter, pPolWSNNA F-Luc, together with 1 of the 16 combinations of RNP complex protein plasmids (pCAGGS-PB2, pCAGGS-PB1, pCAGGS-PA, and pCAGGS-NP) between the SK06 and Tok07 viruses, was transfected into 293 cells. The transfected cells were maintained separately at both 33 °C and 37 °C. After 48-h incubation, a dual-luciferase assay was performed in which the relative firefly luciferase activity was normalized to the internal control, Renilla luciferase. The values shown are means ± SDs of three independent experiments and are standardized to the activity of TPB2TPB1TPATNP (Tok07 PB2, Tok07 PB1, Tok07 PA, and Tok07 NP) at 37 °C.
Pathogenicity of Reassortant Viruses in Mice.
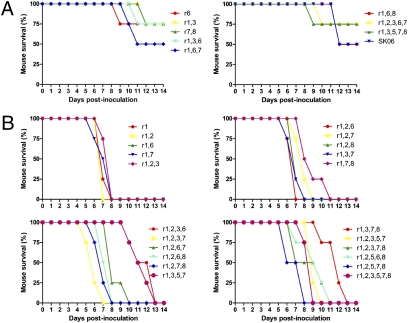
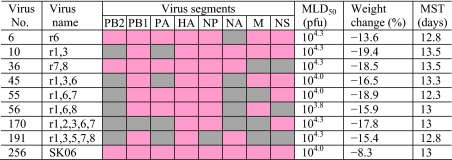
First, we tested the pathogenicity of the parental viruses in mice. SK06 virus was not highly pathogenic [mouse LD50 (MLD50) = 104.0 pfu], and, of note, human Tok07 virus did not kill any mice even when they were infected with 106.5 pfu of viruses. We then performed pathogenicity testing in mice for all the 75 reassortant viruses that met the two criteria of possessing SK06 HA and having a virus stock titer higher than 106 pfu/mL. A total of 62 viruses in the highly replicative group and 13 viruses in the moderately replicative group met these criteria. We chose the reassortant viruses with the SK06 H5 HA because a pandemic is most likely to be caused by an HA subtype to which humans do not have immunity. For each virus, four mice were inoculated intranasally with 104.0 pfu of virus and were observed daily for 14 days for body weight changes and survival. The viruses were divided into three groups based on their pathogenicity in mice. (i) Less pathogenic viruses (Table 1): All four mice inoculated with this group of viruses survived the infection. Therefore, the MLD50 was ≥ 104.5 pfu. Mice infected with most of the viruses in this group experienced an increase in body weight at the end of the observation period (with a few exceptions; see viruses r3, r7, r1,8, r2,3, r3,7, and r1,3,6,7). Among the 75 viruses tested, 32 viruses in the highly replicative group and all 13 viruses in the moderately replicative group were less pathogenic than the SK06 virus. (ii) Viruses with pathogenicity similar to that of SK06 (Table 2 and Fig. 2A): This group comprised eight viruses that were as pathogenic as the SK06 virus. One, two, or three of the four mice died after infection with 104.0 pfu of these viruses. The MLD50 was determined further to be between 103.8 and 104.3 pfu. All mice infected with these viruses demonstrated various degrees of weight loss by the end of the observation period. The mean survival times were >10 days for all mice infected with viruses from this group. (iii) Viruses more pathogenic than SK06 (Table 3 and Fig. 2B): All four mice died when infected with 104.0 pfu of one of these 22 viruses. Substantial body weight loss was observed for all mice infected with these viruses, and the mean survival times were <10 days for most of the viruses (with three exceptions: r1,2,3,6, r1,3,5,7, and r1,3,7,8). Importantly, 10 viruses were lethal to mice with an MLD50 ≤100 pfu. Of these viruses, r1, r1,2, and r1,2,8 killed mice with ≤10 pfu. All these more pathogenic viruses belonged to the highly replicative group that had a titer >107 pfu/mL on MDCK cells (Table S1). A common feature of these viruses is that their PB2 segment was derived from the Tok07 virus. Although the introduction of Tok07 PB2 into the SK06 virus backbone did not necessarily result in a more pathogenic phenotype, our data suggest that human PB2 is a prerequisite for the emergence of substantially virulent reassortant viruses. For the 10 reassortant viruses with MLD50 ≤100 pfu, we fully sequenced the virus stocks to ensure that there were no mutations that might be responsible for the highly pathogenic phenotype. No such mutations were found. Therefore, our data suggest that the components of these reassortant viruses are compatible at both the viral RNA and protein levels and that the highly pathogenic phenotype is an intrinsic property of these viruses.
Table 1.
Reassortant viruses of lower pathogenicity than that of SK06
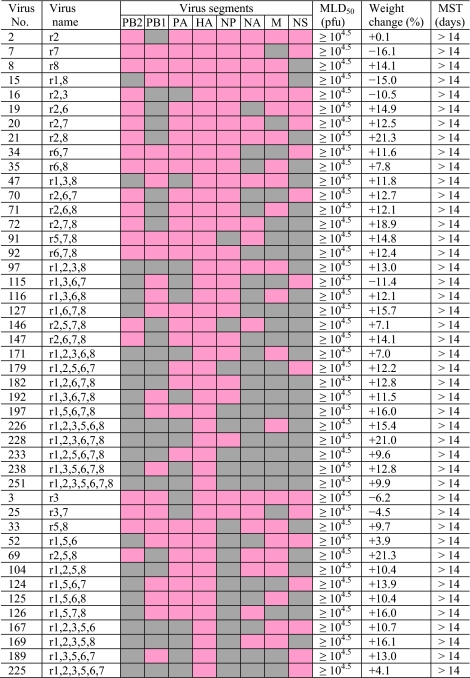 |
In the virus name “r” denotes “reassortant.” The numbers in the virus name indicate segments derived from the Tok07 virus as follows: 1, PB2; 2, PB1; 3, PA; 4, HA; 5, NP; 6, NA; 7, M; and 8, NS. The virus segments derived from the SK06 virus were not assigned numbers. Gene segments derived from Tok07 and SK06 viruses are shown in gray and rose, respectively. The last 13 viruses from r3 to r1,2,3,5,6,7 were derived from the moderately replicative group; all other viruses were from the highly replicative group. The pathogenicity of the reassortant viruses was determined as described in Materials and Methods. The weight change was determined from four mice in each group infected with 104 pfu of virus [relative weight change from days postinoculation (dpi) 0 to the weight at dpi 14]. None of these viruses killed mice at 104 pfu. Therefore, the MLD50 was assigned as ≥ 104.5 pfu and was not determined further. +, mice had increased body weight; −, mice had body weight loss; MST, mean survival time of the mice infected with 104 pfu.
Table 2.
Reassortant viruses with pathogenicity similar to that of SK06
 |
Symbols and nomenclature of the viruses are as in Table 1. The weight change was determined from four mice in each group infected with 104 pfu of virus (relative weight change from dpi 0 to the weight of the mice on the day they started to die or were euthanized). The MLD50 was further determined from groups of four mice.
Fig. 2.
Survival of mice inoculated with 104 pfu of reassortant viruses. Groups of four mice were anesthetized with isoflurane and were inoculated intranasally with 104 pfu of virus. Body weight and survival status were checked daily. (A) Viruses with pathogenicity similar to that of SK06. (B) Viruses more pathogenic than SK06.
Table 3.
Reassortant viruses of higher pathogenicity than that of SK06
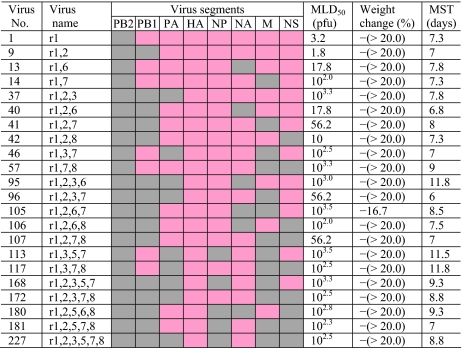 |
Symbols and nomenclature of the viruses are as in Table 1. The weight change was determined from four mice in each group infected with 104 pfu of virus (relative weight change from dpi 0 to the weight of the mice on the day they started to die or were euthanized). The MLD50 was further determined from groups of four mice. − (> 20.0) denotes that the mice lost >20% of their body weight.
All the 75 reassortant viruses we examined for pathogenicity possessed HA from SK06 virus, which has a series of basic amino acids at the cleavage site. The high cleavability of H5 HA protein has been well established as a prerequisite for the high-virulence phenotype of H5N1 influenza viruses in mammals (11). Our data clearly demonstrated that human PB2 is the principal determinant for the pathogenicity of these reassortant viruses. Therefore, to achieve a better understanding of the contributions to pathogenicity made by the other human virus genes of the reassortant viruses, we analyzed pathogenicity data of single-gene reassortant viruses each containing one gene from the human virus and found that, except for PB2, none of the human virus genes in isolation could increase the pathogenicity of the virus (see viruses r2, r3, r7, and r8 in Table 1; r6 in Table 2; and r1 in Table 3). With respect to the specific role of each human virus gene, we found that human PB1 alone did not increase the pathogenicity of the reassortant viruses, because all 11 viruses containing Tok07 PB1 with SK06 PB2 (see viruses r2, r2,3, r2,6, r2,7, r2,8, r2,5,8, r2,6,7, r2,6,8, r2,7,8, r2,5,7,8, and r2,6,7,8) exhibited low pathogenicity in mice with MLD50 ≥104.5 pfu (Table S5). Without exception, however, the viruses containing Tok07 PB1 as well as Tok07 PB2 exhibited enhanced pathogenicity or pathogenicity similar to that of corresponding viruses possessing SK06 PB1 and Tok07 PB2. For example, the pathogenicity was increased when the virus pair r1,3/r1,2,3 was compared and was similar for virus pair r1/r1,2 (Table S5), suggesting a close partnership between PB1 and PB2 proteins in forming the RNP complex and in overall functioning.
Human virus NP in the SK06 background usually attenuated the viruses in mice. Of the 75 reassortant viruses tested, 25 viruses contained Tok07 NP (Table S6). The MLD50 was ≥ 104.5 for 19 of these viruses. The other six viruses were attenuated when compared with the corresponding viruses that derived their NP from SK06 virus (with only one exception, virus pair r1,2,3,7,8/r1,2,3,5,7,8, in which both viruses had an MLD50 of 102.5 pfu; Table S6). By analyzing other human virus segments in the same way, we found that Tok07 PA (Table S7), Tok07 NA (Table S8), and Tok07 NS (Table S9) also attenuated the pathogenicity of the reassortant viruses, with a few exceptions (for Tok07 PA, see the MLD50 of virus pairs r1,7,8/r1,3,7,8 and r1,5,7,8/r1,3,5,7,8; for Tok07 NA, see virus pairs r1,3/r1,3,6, r1,8/r1,6,8, r1,2,3/r1,2,3,6, and r1,2,5,8/r1,2,5,6,8; and for Tok07 NS, see virus pair r1,2,3,5,7/r1,2,3,5,7,8).
The influence of Tok07 M on pathogenicity was largely dependent on the specific combination of reassortant viruses (Table S10). In the absence of Tok07 PB2, all 11 viruses containing Tok07 M were of low pathogenicity (MLD50 ≥104.5 pfu) or showed pathogenicity similar to that of the parental SK06 virus. In the presence of Tok07 PB2, however, the pathogenicity was increased in some reassortant viruses (e.g., r1,3/r1,3,7) but was attenuated in others (e.g., r1,2/r1,2,7).
Taken together, our data suggest that human PB2 is indispensible for reassortant viruses to be virulent to mice. Human PB1 alone lacks the ability to increase virus pathogenicity in mice but could do so in cooperation with human PB2. Other human segments, including PA, NP, NA, and NS, usually attenuated the reassortant viruses, whereas the influence of the human M segment varied depending on the specific gene combination of the reassortant virus.
Discussion
We systematically attempted to generate all of the 254 combinations of reassortant viruses between two currently cocirculating avian H5N1 and human H3N2 influenza viruses to evaluate their pathogenic potential. Our data demonstrate that the gene segments of these two viruses are largely compatible, resulting in 184 reassortant viruses with different replicative abilities and 70 nonviable viruses. Pathogenicity experiments performed with 75 H5 reassortant viruses showed that 22 viruses were more pathogenic for mice than the parental SK06 virus. Strikingly, three viruses exhibited substantial lethality for mice with MLD50s of ≤10 pfu. Our data suggest that of the eight segments in the human virus, Tok07 PB2 is indispensible for the conversion of reassortant H5 viruses into the highly pathogenic phenotype and that, in contrast to the findings of Chen et al. (9), viruses with substantial virulence indeed can be generated by reassortment of avian H5N1 and human H3N2 viruses. Our study thus provides valuable information for preparedness for future pandemics that could be caused by reassortants between avian H5N1 and human influenza viruses, including the recently emerged pandemic H1N1 virus.
While we were working on this study, Chen et al. (9) published data on reassortment between A/Wyoming/3/03 (H3N2) and A/Thailand/16/04 (H5N1) viruses, both of which are human isolates. They attempted to generate the 63 reassortant viruses bearing the H5 HA and N1 NA genes with the remaining segments as combinations of the two parental viruses plus one extra single gene reassortant virus, r6, possessing the A/Wyoming/3/03 NA in the background of the A/Thailand/16/04 virus. For the 39 viruses they generated, pathogenicity was assessed in a mouse model. The MLD50 for the wild-type A/Thailand/16/04 virus was 101.8 pfu. Surprisingly, the most virulent reassortant virus in their study was the r6 virus (MLD50 = 102.2 pfu), whereas the corresponding r6 virus (see virus r6 in Table 2 and Fig. 2A) in our study exhibited pathogenicity similar to that of the wild-type SK06 virus. Most importantly, in the Chen et al. study (9), none of their reassortant viruses were more virulent than the wild-type H5N1 virus.
The differences between our data and those of Chen et al. (9) may stem partly from the choice of parental H5N1 viruses in the two studies. The H5N1 viruses have been shown to acquire enhanced pathogenicity by a glutamic acid-to-lysine mutation at position 627 in the PB2 protein (11, 12). Unlike Chen’s study (9), we demonstrate that H5 viruses with increased pathogenicity in mice can be generated by reassortment between low-pathogenic avian H5N1 and human H3N2 influenza viruses and that the human virus PB2 segment functions in the background of an avian H5N1 virus and enhances its virulence.
We used an H5N1 virus of avian origin in this study because most of the current human cases of H5N1 virus infection have been characterized by contact with sick poultry or poultry products (13, 14). Therefore, the emergence of reassortant H5 viruses with pandemic potential most likely will occur through reassortment when a person infected with a seasonal human influenza virus comes into contact with H5N1 virus-infected poultry or poultry products. This scenario is more likely now because of the cocirculation of multiple lineages of avian H5N1 and human H3N2 influenza viruses around the world (15–18).
Previously, we selected two genetically distinct viruses, A/equine/Prague/1/56 (H7N7) and A/Yokohama/2017/03 (H3N2), to define the restricting factors for influenza virus reassortment and found that the activity of the RNP complex is one of the most important determinants for influenza virus reassortment (10). This finding extends to the current study. We found that almost all 96 reassortant viruses in the highly replicative group possessed high RNP activity in the minigenome assay, and all 32 reassortant viruses containing the two RNP combinations with the lowest activity (SPB2SPB1TPATNP and SPB2TPB1TPATNP) were nonviable. The cotransfection procedure used in our previous study reflected the competitiveness of the progeny viruses in the reassortment process; however, the current study provides specific information about the viability and replicative ability of all 254 combinations of reassortant viruses between the two parental viruses.
It is noteworthy that the activities of the RNP complexes containing SK06 PB2 protein decreased dramatically when the minigenome assay was performed at 33 °C rather than at 37 °C, probably because of the presence of glutamic acid (a known determinant of temperature sensitivity in RNA replication of avian influenza viruses) at position 627 in the PB2 protein of SK06 virus (19). The presence of human Tok07 PB2 protein in 8 of the 16 RNP combinations led to sustained replication and transcription activity in the minigenome assay at 33 °C, without exception. Therefore, we anticipate that the introduction of the human PB2 segment into a reassortant virus could confer efficient growth at the lower temperature of the upper respiratory tract of humans, an ability that is critical for efficient transmission of pandemic viruses among humans (20). To initiate pandemics, influenza viruses also need to acquire human-like receptor-binding specificity with α2,6-linked sialic acid (21–23), an ability that has been partially achieved by some H5N1 human isolates (7, 24, 25).
In summary, we attempted to generate all the possible 254 combinations of reassortant viruses between human H3N2 and avian H5N1 influenza viruses that could pose a threat to public health. Our study elucidated the specific role of each human virus segment in the pathogenicity of reassortant H5 viruses and found that the introduction of the human PB2 segment into the reassortant viruses is crucial to convert them to a highly pathogenic phenotype. Our findings suggest that high pathogenicity, an important viral property in determining the magnitude of a pandemic, could occur as a result of reassortment between avian H5N1 and human H3N2 influenza viruses and highlight the importance of vaccination programs against both avian H5N1 and human H3N2 influenza viruses, at least for people at high risk of exposure to avian H5N1 influenza viruses, such as poultry workers and medical personnel.
Materials and Methods
Cells and Viruses.
293 and 293T human embryonic kidney cells were maintained in DMEM supplemented with 10% FBS. MDCK cells were grown in MEM containing 5% newborn calf serum. After infection with influenza virus, the MDCK cells were maintained in MEM containing 0.3% BSA and 0.5 μg/mL L-(tosylamido-2-phenyl) ethyl chloromethyl ketone-trypsin. The H5N1 (SK06) virus was isolated from a sample collected in South Kalimantan province, Indonesia, in November 2006 (26) and was grown in 10-day-old embryonated eggs. The H3N2 (Tok07) virus was isolated during the 2006–2007 influenza season and was propagated in MDCK cells.
Construction of Plasmids.
Reverse genetics systems for the SK06 and Tok07 viruses were established by the method described by Neumann et al. (27). Briefly, the cDNAs of the SK06 and Tok07 viruses were synthesized from viral RNAs by reverse transcription with Uni12 primer (28), amplified by PCR with gene-specific primers, and then were inserted into the pHH21 vector. The ORFs for PB2, PB1, PA, and NP of both the SK06 and Tok07 viruses were inserted into the pCAGGS/BsmBI vector for protein expression, as described previously (10).
The generation of plasmids expressing the three polymerase and NP proteins of the WSN virus and the minigenome firefly luciferase reporter, pPolWSNNA F-Luc, was described previously (10, 27).
Reverse Genetics.
All reassortant viruses and the parental SK06 and Tok07 viruses were generated from plasmids as described by Neumann et al. (27). Briefly, the eight plasmids for the synthesis of viral RNA and the four expression plasmids for WSN PB2, PB1, PA and NP proteins were transfected into 293T cells. Forty-eight hours later, aliquots of the transfection supernatant were used to inoculate MDCK cells to produce stock viruses. With two exceptions [r1,2,3,7,8 and r1,2,6,7,8, which were harvested 24 hours post infection (hpi)], the viruses were harvested 48 hpi when obvious CPE were observed or were harvested 72 hpi if the MDCK cells showed no CPE or only unobvious CPE at 48 hpi. The titers of the stock viruses were determined by plaque assay on MDCK cells. All experiments with live viruses and with transfectants generated by reverse genetics were performed in an enhanced biosafety level 3 containment laboratory approved for such use by the Centers for Disease Control and Prevention and the US Department of Agriculture.
Luciferase Assay.
A dual-luciferase reporter assay system (Promega) was used to compare the activities of viral RNP complexes. Briefly, the construct pPolWSNNA F-Luc (0.05 μg) was transfected into 2 × 105 293 cells together with 0.5 μg each of the four protein expression plasmids, pCAGGS-PB2, pCAGGS-PB1, pCAGGS-PA and pCAGGS-NP, for each of the 16 possible RNP combinations between the SK06 and Tok07 viruses. The assay was performed at both 33 °C and 37 °C. At 48 hours post-transfection, luciferase activities were measured on a GloMax 96 microplate luminometer (Promega). As an internal control, pGL4.74[hRluc/TK] (Promega) was used (29).
Mouse Experiments.
Reassortant H5 viruses whose HA gene was derived from the SK06 virus and which grew to titers >106 pfu/mL in MDCK cells were tested for pathogenicity in 6-week-old Balb/C mice (Jackson Laboratory). For each virus, four mice were lightly anesthetized with isoflurane and inoculated intranasally with 104 pfu of virus in 50 μL PBS. The mice were observed for 14 days after inoculation, and their body weight and survival status were checked daily. Mice that lost >20% of their body weight were euthanized. If the test virus did not reduce the body weight of any of the mice by >20%, the MLD50 was designated as ≥104.5 pfu. For viruses that killed mice at 104 pfu, the MLD50 was refined further by testing additional groups of four mice.
Supplementary Material
Acknowledgments
We thank Martha McGregor, Krisna Wells, Kelly Moore, and Rebecca Moritz for technical assistance and Susan Watson for editing the manuscript. This work was supported by Public Health Service research grants from the National Institute of Allergy and Infectious Diseases, by a Grant-in-Aid for Specially Promoted Research, by the program of Founding Research Centers for Emerging and Reemeraging Infectious Diseases from the Ministry of Education, Culture, Sports, Science and Technology, and by an Exploratory Research for Advanced Technology grant from Japan Science.
Footnotes
The authors declare no conflict of interest.
This article is a PNAS Direct Submission.
Data deposition: The sequences reported in this paper have been deposited in the GenBank database (accession nos.CY049745–CY049752).
This article contains supporting information online at www.pnas.org/cgi/content/full/0912807107/DCSupplemental.
References
- 1.Kawaoka Y, Krauss S, Webster RG. Avian-to-human transmission of the PB1 gene of influenza A viruses in the 1957 and 1968 pandemics. J Virol. 1989;63:4603–4608. doi: 10.1128/jvi.63.11.4603-4608.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lindstrom SE, Cox NJ, Klimov A. Genetic analysis of human H2N2 and early H3N2 influenza viruses, 1957-1972: Evidence for genetic divergence and multiple reassortment events. Virology. 2004;328:101–119. doi: 10.1016/j.virol.2004.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Xu X, Subbarao K, Cox NJ, Guo Y. Genetic characterization of the pathogenic influenza A/Goose/Guangdong/1/96 (H5N1) virus: Similarity of its hemagglutinin gene to those of H5N1 viruses from the 1997 outbreaks in Hong Kong. Virology. 1999;261:15–19. doi: 10.1006/viro.1999.9820. [DOI] [PubMed] [Google Scholar]
- 4.Chen H, et al. The evolution of H5N1 influenza viruses in ducks in southern China. Proc Natl Acad Sci USA. 2004;101:10452–10457. doi: 10.1073/pnas.0403212101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Claas EC, et al. Human influenza A H5N1 virus related to a highly pathogenic avian influenza virus. Lancet. 1998;351:472–477. doi: 10.1016/S0140-6736(97)11212-0. [DOI] [PubMed] [Google Scholar]
- 6.Subbarao K, et al. Characterization of an avian influenza A (H5N1) virus isolated from a child with a fatal respiratory illness. Science. 1998;279:393–396. doi: 10.1126/science.279.5349.393. [DOI] [PubMed] [Google Scholar]
- 7.Kongchanagul A, et al. Positive selection at the receptor-binding site of haemagglutinin H5 in viral sequences derived from human tissues. J Gen Virol. 2008;89:1805–1810. doi: 10.1099/vir.0.2008/002469-0. [DOI] [PubMed] [Google Scholar]
- 8.Li KS, et al. Genesis of a highly pathogenic and potentially pandemic H5N1 influenza virus in eastern Asia. Nature. 2004;430:209–213. doi: 10.1038/nature02746. [DOI] [PubMed] [Google Scholar]
- 9.Chen LM, et al. Genetic compatibility and virulence of reassortants derived from contemporary avian H5N1 and human H3N2 influenza A viruses. PLoS Pathog. 2008;4:e1000072. doi: 10.1371/journal.ppat.1000072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Li C, et al. Compatibility among polymerase subunit proteins is a restricting factor in reassortment between equine H7N7 and human H3N2 influenza viruses. J Virol. 2008;82:11880–11888. doi: 10.1128/JVI.01445-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hatta M, Gao P, Halfmann P, Kawaoka Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science. 2001;293:1840–1842. doi: 10.1126/science.1062882. [DOI] [PubMed] [Google Scholar]
- 12.Subbarao EK, London W, Murphy BR. A single amino acid in the PB2 gene of influenza A virus is a determinant of host range. J Virol. 1993;67:1761–1764. doi: 10.1128/jvi.67.4.1761-1764.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beigel JH, et al. Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353:1374–1385. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- 14.Gambotto A, et al. Human infection with highly pathogenic H5N1 influenza virus. Lancet. 2008;371:1464–1475. doi: 10.1016/S0140-6736(08)60627-3. [DOI] [PubMed] [Google Scholar]
- 15.Zhao ZM, et al. Genotypic diversity of H5N1 highly pathogenic avian influenza viruses. J Gen Virol. 2008;89:2182–2193. doi: 10.1099/vir.0.2008/001875-0. [DOI] [PubMed] [Google Scholar]
- 16.Rambaut A, et al. The genomic and epidemiological dynamics of human influenza A virus. Nature. 2008;453:615–619. doi: 10.1038/nature06945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schweiger B, Bruns L, Meixenberger K. Reassortment between human A(H3N2) viruses is an important evolutionary mechanism. Vaccine. 2006;24:6683–6690. doi: 10.1016/j.vaccine.2006.05.105. [DOI] [PubMed] [Google Scholar]
- 18.Vijaykrishna D, et al. Evolutionary dynamics and emergence of panzootic H5N1 influenza viruses. PLoS Pathog. 2008;4:e1000161. doi: 10.1371/journal.ppat.1000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Massin P, van der Werf S, Naffakh N. Residue 627 of PB2 is a determinant of cold sensitivity in RNA replication of avian influenza viruses. J Virol. 2001;75:5398–5404. doi: 10.1128/JVI.75.11.5398-5404.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hatta M, et al. Growth of H5N1 influenza A viruses in the upper respiratory tracts of mice. PLoS Pathog. 2007;3:1374–1379. doi: 10.1371/journal.ppat.0030133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Suzuki Y, et al. Sialic acid species as a determinant of the host range of influenza A viruses. J Virol. 2000;74:11825–11831. doi: 10.1128/jvi.74.24.11825-11831.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Matrosovich M, et al. Early alterations of the receptor-binding properties of H1, H2, and H3 avian influenza virus hemagglutinins after their introduction into mammals. J Virol. 2000;74:8502–8512. doi: 10.1128/jvi.74.18.8502-8512.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Tumpey TM, et al. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- 24.Auewarakul P, et al. An avian influenza H5N1 virus that binds to a human-type receptor. J Virol. 2007;81:9950–9955. doi: 10.1128/JVI.00468-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Yamada S, et al. Haemagglutinin mutations responsible for the binding of H5N1 influenza A viruses to human-type receptors. Nature. 2006;444:378–382. doi: 10.1038/nature05264. [DOI] [PubMed] [Google Scholar]
- 26.Takano R, et al. Phylogenetic characterization of H5N1 avian influenza viruses isolated in Indonesia from 2003-2007. Virology. 2009;390:13–21. doi: 10.1016/j.virol.2009.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Neumann G, et al. Generation of influenza A viruses entirely from cloned cDNAs. Proc Natl Acad Sci USA. 1999;96:9345–9350. doi: 10.1073/pnas.96.16.9345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Katz JM, Wang M, Webster RG. Direct sequencing of the HA gene of influenza (H3N2) virus in original clinical samples reveals sequence identity with mammalian cell-grown virus. J Virol. 1990;64:1808–1811. doi: 10.1128/jvi.64.4.1808-1811.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ozawa M, et al. Contributions of two nuclear localization signals of influenza A virus nucleoprotein to viral replication. J Virol. 2007;81:30–41. doi: 10.1128/JVI.01434-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.