ABSTRACT
BACKGROUND
Non-adherence to essential medications represents an important public health problem. Little is known about the frequency with which patients fail to fill prescriptions when new medications are started (“primary non-adherence”) or predictors of failure to fill.
OBJECTIVE
Evaluate primary non-adherence in community-based practices and identify predictors of non-adherence.
PARTICIPANTS
75,589 patients treated by 1,217 prescribers in the first year of a community-based e-prescribing initiative.
DESIGN
We compiled all e-prescriptions written over a 12-month period and used filled claims to identify filled prescriptions. We calculated primary adherence and non-adherence rates for all e-prescriptions and for new medication starts and compared the rates across patient and medication characteristics. Using multivariable regressions analyses, we examined which characteristics were associated with non-adherence.
MAIN MEASURES
Primary medication non-adherence.
KEY RESULTS
Of 195,930 e-prescriptions, 151,837 (78%) were filled. Of 82,245 e-prescriptions for new medications, 58,984 (72%) were filled. Primary adherence rates were higher for prescriptions written by primary care specialists, especially pediatricians (84%). Patients aged 18 and younger filled prescriptions at the highest rate (87%). In multivariate analyses, medication class was the strongest predictor of adherence, and non-adherence was common for newly prescribed medications treating chronic conditions such as hypertension (28.4%), hyperlipidemia (28.2%), and diabetes (31.4%).
CONCLUSIONS
Many e-prescriptions were not filled. Previous studies of medication non-adherence failed to capture these prescriptions. Efforts to increase primary adherence could dramatically improve the effectiveness of medication therapy. Interventions that target specific medication classes may be most effective.
Electronic supplementary material
The online version of this article (doi:10.1007/s11606-010-1253-9) contains supplementary material, which is available to authorized users.
KEY WORDS: adherence, non-adherence, electronic prescribing, health information technology
INTRODUCTION
Underuse of prescription medicines constitutes a large problem for the United States healthcare system.1–6 Some underuse is due to under-diagnosis, some to under-treatment, but at least part may be attributed to the fact that many patients do not take medications that they have been prescribed, a phenomenon referred to as medication non-adherence.7–13 Medication non-adherence is related to greater morbidity and mortality in chronic disease,14–16 and has been estimated to increase healthcare costs by over $170 billion annually in the United States.17,18 The public health consequences of medication non-adherence have led providers and health plans to aspire to measure its frequency, assess its root causes, and develop and implement interventions to address it.
Prior research has demonstrated that many patients stop taking medications soon after filling the first prescription.19 These studies generally rely on claims data and begin tracking adherence when the patient first fills a prescription, in effect measuring “persistence” on a medication.7–13 The rate at which patients fill new prescriptions has been defined as “primary adherence,”20,21 and is an important phenomenon since timely initiation of medications is critical for treating both acute and chronic conditions. The study of primary medication adherence and non-adherence is limited in the United States by the difficulty and expense of tracking fill rates of initial prescriptions which until recently were almost always hand-written. Thus, prior research generally consists of small samples,8 experiences in countries other than the United States,21,22 or the use of patient reports via surveys.23,24 Electronic prescribing (e-prescribing) creates an electronic record of the written prescription, and so its use provides an opportunity to calculate primary non-adherence,25–27 and to examine correlates of different rates.
METHODS
Data Sources and Study Sample
We used three sources of data—e-prescribing transactions, pharmacy claims files, and provider characteristic files. Data were drawn from the eRx Collaborative in Massachusetts, which was initiated in October 2003 by Blue Cross Blue Shield of Massachusetts (BCBSMA), Tufts Health Plan (THP) and Zix Corporation (ZixCorp). Under the program, PocketScript™ software from ZixCorp was distributed to Massachusetts outpatient providers. Clinicians began enrolling during the second quarter of 2004. The program subsequently expanded to include additional insurers and e-prescribing companies; however, the data for this study were drawn exclusively from BCBSMA, THP and ZixCorp.
The e-prescribing data recorded all electronic prescriptions issued, regardless of whether they were eventually filled or not. Each transaction record included information on prescribing clinician, patient, prescription date, drug name, dosage, form(pill, tablet, etc.), and insurance plan.
Pharmacy insurance claims included data on prescriptions that were filled and reimbursed (i.e. picked up by the patient), and therefore represent a subset of prescriptions written either electronically or by hand. The claims data included encoded patient ID, prescription fill date, and insurance plan. Drugs were identified by national drug code (NDC), which specifies the medication, dosage, form, package size, and manufacturer for each filled prescription. The claims data files included fields for the brand name and generic name of the medication dispensed corresponding to the NDC. The claims files included fields for patient age and gender that had been linked from insurance enrollment files.
Provider characteristics were included in the insurance companies′ provider files and included clinician specialty, gender, and age, although data were missing for a subset of providers. We calculated the practice size based on the number of providers at each practice location as identified in the e-prescribing data during the study period.
The study sample included all patients who received at least one e-prescription using the PocketScript system in Massachusetts during the first year of the eRx Collaborative, from April 1 2004 through March 31 2005. For these patients we included data on all e-prescriptions written during the study period. All identifiable individual characteristics were removed from the data before transfer to the researchers. Claims data from the insurance companies were provided for the 12-month study period and for the 6 months prior (i.e. beginning 10/1/2003). Crosswalks, using encrypted patient and clinician identifiers, were created by ZixCorp and the insurance plans so that patient and clinician records could be linked across the datasets while preserving confidentiality. The Partners IRB approved the study.
Linking Pharmacy Claims to E-Prescribing Transactions
Although prescription claims data include NDC numbers, there is no corresponding code for the e-prescriptions as written, requiring us to use drug names to match individual prescriptions. If the drug name from the e-prescriptions file matched either the brand or generic name from the claims file, then we defined the e-prescription as filled by that claim. For combination medications the naming conventions sometimes differed between the two files, so we broke the combinations down to the individual agents and checked if all the individual agents matched before defining those as filled prescriptions. In all cases, we required that the prescription fill date was on or after the date of e-prescribing.
We counted an e-prescription as filled if a corresponding paid claim appeared at any time prior to the end of our data(3/31/2005). We then restricted the population of prescriptions to newly initiated medications. To do this we used the same matching strategy as described above, but this time looking for filled claims before the date of the e-prescription. We examined the claims for up to 12 months back(claims data began 10/1/2003, so 12 months were not always available). If no prior claims were found, we considered the e-prescription to represent a newly prescribed medication.
Analyses
The rate of primary adherence is expressed as the number of prescriptions filled divided by the total number of prescriptions written. Thus, the unit of analysis was the prescription. We compared primary adherence rates across drug classes, physician characteristics, patient characteristics, and the month in which an e-prescription was written.
We then developed generalized estimating equation(GEE) models, with an exchangeable correlation structure for the physician. Effect estimates measured the log odds ratio of a filled prescription. All measured prescriber and patient characteristics were included as covariates in the model. We also included medication therapeutic class in the model, using antimicrobials as the reference group. In preliminary analyses the month in which an e-prescription was written had no statistically significant effect, so month was dropped from the analyses. We stratified by patient age, specifying the model separately for children and adults.
RESULTS
A total of 195,930 e-prescriptions were written for 75,589 patients during our study period. The top half of Table 1 shows the gender and age distribution for these patients. There were 1,217 prescribers who wrote e-prescriptions and the bottom half of Table 1 shows their characteristics. Data on characteristics were missing for 12–14% of the prescribers. The majority of prescribers were in primary care specialties, specifically internal medicine, pediatrics, and family practice. The overall primary adherence rate was 77.5%, corresponding to 151,837 of the e-prescriptions being filled, corresponding to 22.5% primary non-adherence. There were 82,245 e-prescriptions that were for new medications and 58,984 (71.7%) of these were filled, or 28.3% primary non-adherence.
Table 1.
Characteristics of Prescribers using the E-Prescribing System and Patients Receiving E-Prescriptions
| Patient characteristics | |
|---|---|
| Overall | N=75,589 |
| Gender | |
| Male | 32,142 (42.5%) |
| Female | 43,447 (57.5%) |
| Age | |
| zero to 18 | 9,417 (12.5%) |
| 19 to 44 | 24,381 (32.3%) |
| 45 to 64 | 32,359 (42.8%) |
| 65 and up | 9,432 (12.5%) |
| Prescriber characteristics | |
| Overall | N=1,217 |
| Gender | |
| Male | 595 (48.9%) |
| Female | 461 (37.9%) |
| missing | 161 (13.2%) |
| Age | |
| under 35 | 161 (13.2%) |
| 36 to 54 | 685 (56.3%) |
| 55 and up | 203 (16.7%) |
| missing | 168 (13.8%) |
| Specialtya | |
| internal medicine | 366 (30.1%) |
| pediatrics | 296 (24.3%) |
| family practice | 188 (15.4%) |
| other | 230 (18.9%) |
| missing | 137 (11.3%) |
| Practice Size | |
| 1–3 | 348 (27.9%) |
| 4–8 | 398 (32.7%) |
| 9–15 | 205 (16.8%) |
| 16+ | 266 (21.9%) |
a As clinicians may have multiple specialties, categories for specialty are not mutually exclusive. Column percentages for this section do not total to 100%
Table 2 shows adherence rates by physician characteristics. Primary adherence rates were higher for e-prescriptions from primary care specialists (internal medicine, primary care, pediatrics) than from other specialties. Adherence rates were higher for male physicians and older physicians but did not differ greatly across practice sizes. When prescriptions were examined by patient characteristics (Table 3), e-prescriptions were filled for children at a much higher rate (87.3%) than any other age group. Men filled e-prescriptions at a slightly higher rate than women.
Table 2.
Primary Adherence, by Prescriber Characteristics
| All e-prescriptions | New e-prescriptions | |||
|---|---|---|---|---|
| Number of e-prescriptions | Number ever filled (%) | Number of e-prescriptions | Number ever filled (%) | |
| TOTAL | 195,930 | 151,837 (77.5%) | 82,245 | 58,984 (71.7%) |
| Specialty | ||||
| Internal medicine | 92,721 | 77,413 (83.5%) | 34,035 | 27,162 (79.8%) |
| Pediatrics | 13,712 | 11,579 (84.4%) | 7,804 | 6,410 (82.1%) |
| Family practice | 51,885 | 42,974 (82.8%) | 21,290 | 17,026 (80.0%) |
| Other | 22,467 | 12,794 (57.0%) | 10,651 | 5,036 (47.3%) |
| Missing | 15,145 | 7,077 (46.7%) | 8,465 | 3,350 (39.6%) |
| Gender | ||||
| Male | 122,908 | 102,293 (83.2%) | 47,088 | 37,492 (79.6%) |
| Female | 55,752 | 40,853 (73.3%) | 25,763 | 17,516 (68.0%) |
| Missing | 17,270 | 8,691 (50.3%) | 9,394 | 3,976 (42.3%) |
| Age | ||||
| Under 35 | 16,318 | 12,344 (75.7%) | 8,376 | 6,116 (73.0%) |
| 35–54 | 122,909 | 99,071 (80.6%) | 50,376 | 38,253 (75.9%) |
| 55 and over | 37,781 | 30,795 (81.5%) | 13,431 | 10,326 (76.9%) |
| Missing | 18,922 | 9,627 (50.9%) | 10,062 | 4,289 (42.6%) |
| Practice size | ||||
| 1–3 | 59,460 | 46,538 (78.3%) | 24,944 | 18,179 (72.9%) |
| 4–8 | 59,713 | 45,911 (76.9%) | 25,369 | 17,946 (70.7%) |
| 9–15 | 41,172 | 31,983 (77.7%) | 16,689 | 11,949 (71.6%) |
| 16+ | 35,585 | 27,405 (77.0%) | 15,243 | 10,910 (71.6%) |
Table 3.
Primary Adherence, by Patient Characteristics
| All e-prescriptions | New e-prescriptions | |||
|---|---|---|---|---|
| Number of e-prescriptions | Number ever filled (%) | Number of e-prescriptions | Number ever filled (%) | |
| TOTAL | 195,930 | 151,837 (77.5%) | 82,245 | 58,984 (71.7%) |
| Age | ||||
| 0–18 | 17,921 | 15,636 (87.3%) | 10,024 | 8,571 (85.5%) |
| 19–44 | 56,055 | 41,248 (73.6%) | 29,010 | 19,948 (68.8%) |
| 45–64 | 92,022 | 71,340 (77.5%) | 34,436 | 24,339 (70.7%) |
| 65+ | 29,932 | 23,613 (78.9%) | 8,775 | 6,126 (69.8%) |
| Gender | ||||
| Male | 81,648 | 65,230 (79.9%) | 32,705 | 24,533 (75.0%) |
| Female | 114,282 | 86,607 (75.8%) | 49,540 | 34,451 (69.5%) |
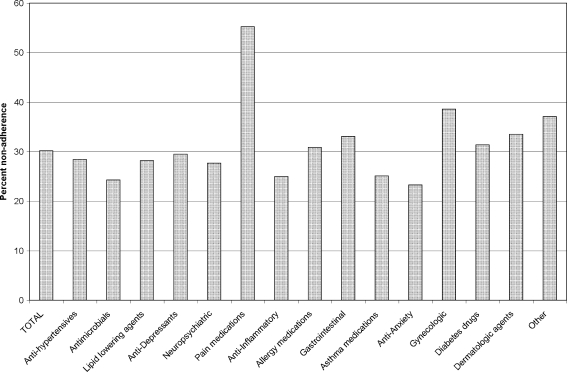
Table 4 shows the primary adherence rates for the major drug classes among patients over age 18, the corresponding values for non-adherence are displayed in Fig. 1. Patients aged 0-18 accounted for 9.1% of the e-prescriptions written and the drug classes prescribed for them differed from the overall population, so they are listed separately in the lower panels of Table 4. Among adults, anti-hypertensives (19.5% primary non-adherence) and antimicrobials (22.9% primary non-adherence) were the most commonly prescribed medications. Pain medications (34.5%) had noticeably higher primary non-adherence than other classes. For all medication classes the primary non-adherence rates were higher when the sample was limited to newly prescribed medications. A high proportion of antimicrobial medications were new prescriptions, consistent with their use for acute symptoms. For chronic medications such as lipid-lowering agents, antihypertensives, and diabetes medications the primary non-adherence rate was about 9% higher for newly prescribed medications than for all e-prescriptions. For children the prescribing and adherence patterns were quite different. Among patient 0-18, 49% of e-prescriptions were for antimicrobials and the primary non-adherence rate for that class was only 5.8%.
Table 4.
Primary Adherence, by Medication Class
| All e-prescriptions | New e-prescriptions | |||
|---|---|---|---|---|
| Number of e-prescriptions | Number ever filled (%) | Number of e-prescriptions | Number ever filled (%) | |
| Patients aged 19 and over | ||||
| TOTAL | 178,009 | 136,201 (76.5%) | 72,221 | 50,413 (69.8%) |
| Drug class | ||||
| Anti-hypertensives | 30,211 | 24,332 (80.5%) | 6,145 | 4,401 (71.6%) |
| Antimicrobials | 22,208 | 17,112 (77.1%) | 16,292 | 12,338 (75.7%) |
| Lipid lowering agents | 12,963 | 10,380 (80.1%) | 3,242 | 2,329 (71.8%) |
| Anti-Depressants | 11,767 | 9,251 (78.6%) | 3,476 | 2,452 (70.5%) |
| Neuropsychiatric | 10,941 | 8,382 (76.6%) | 4,046 | 2,926 (72.3%) |
| Pain medications | 10,555 | 6,911 (65.5%) | 3,594 | 1,610 (44.8%) |
| Anti-Inflammatory | 10,333 | 8,060 (78.0%) | 5,892 | 4,419 (75.0%) |
| Allergy medications | 10,123 | 7,221 (71.3%) | 6,324 | 4,368 (69.1%) |
| Gastrointestinal | 8,689 | 6,587 (75.8%) | 3,516 | 2,353 (66.9%) |
| Asthma medications | 7,368 | 5,898 (80.1%) | 3,489 | 2,614 (74.9%) |
| Anti-Anxiety | 4,668 | 4,897 (81.9%) | 1,756 | 1,346 (76.7%) |
| Gynecologic | 5,980 | 3,972 (71.9%) | 1,750 | 1,075 (61.4%) |
| Diabetes drugs | 5,525 | 4,316 (78.1%) | 1,032 | 708 (68.6%) |
| Dermatologic agents | 5,525 | 3,211 (68.8%) | 3,598 | 2,393 (66.5%) |
| Other | 21,153 | 15,671 (74.1%) | 8,069 | 5,081 (62.9%) |
| Patients aged 0–18 | ||||
| TOTAL | 17,921 | 15,636 (87.3%) | 10,024 | 8,571 (85.5%) |
| Drug class | ||||
| Antimicrobials | 8,732 | 8,227 (94.2%) | 4,881 | 4,609 (94.4%) |
| Neuropsychiatric | 1,476 | 1,256 (85.1%) | 182 | 144 (79.1%) |
| Asthma medications | 2,295 | 2,033 (88.6%) | 1,225 | 1,087 (88.7%) |
| Dermatologic agents | 1,439 | 1,195 (83.0%) | 1,149 | 941 (81.9%) |
Figure 1.
Primary non-adherence to newly prescribed medications. Patients aged 19 and over.
The results of the models for adult patients are presented in Table 5, which shows the odds ratio of a prescription being filled for a given characteristic of the prescription, prescriber, or patient, as compared to the reference group. The second and third columns show results for all e-prescriptions and the right-most two columns show results for newly prescribed medications. Model results for children are presented in the Online Appendix.
Table 5.
Results of Multivariate Models: Impact of Medication, Clinician, and Patient Characteristics on Primary Adherence to E-Prescriptions; Patients Aged 19+
| All Medications | New medications only | |||||
|---|---|---|---|---|---|---|
| Variable | Odds ratio | 95% CI | Odds ratio | 95% CI | ||
| Drug class | ||||||
| Lipid lowering agents | 0.79 | 0.73 | 0.86 | 0.58 | 0.52 | 0.65 |
| Anti-hypertensives | 0.84 | 0.79 | 0.90 | 0.60 | 0.55 | 0.66 |
| Diabetes drugs | 0.73 | 0.65 | 0.81 | 0.55 | 0.47 | 0.65 |
| Asthma medications | 1.02 | 0.93 | 1.11 | 0.90 | 0.82 | 0.99 |
| Pain medications | 0.40 | 0.36 | 0.44 | 0.20 | 0.17 | 0.22 |
| Dermatologic agents | 0.53 | 0.48 | 0.58 | 0.52 | 0.47 | 0.58 |
| Neuropsychiatric | 0.75 | 0.70 | 0.80 | 0.72 | 0.66 | 0.78 |
| Anti-anxiety | 0.99 | 0.91 | 1.08 | 0.92 | 0.82 | 1.03 |
| Anti-depressants | 0.88 | 0.82 | 0.94 | 0.68 | 0.62 | 0.75 |
| Gynecologic | 0.72 | 0.66 | 0.79 | 0.53 | 0.47 | 0.60 |
| Allergy medications | 0.62 | 0.56 | 0.68 | 0.62 | 0.54 | 0.70 |
| Anti-inflammatory | 0.83 | 0.77 | 0.89 | 0.80 | 0.74 | 0.87 |
| Gastrointestinal | 0.68 | 0.63 | 0.74 | 0.50 | 0.45 | 0.56 |
| Other classes | 0.62 | 0.58 | 0.67 | 0.42 | 0.38 | 0.46 |
| Physician specialty | ||||||
| Family practice | 1.02 | 0.90 | 1.17 | 1.13 | 0.99 | 1.30 |
| Other specialty | 0.26 | 0.23 | 0.30 | 0.25 | 0.21 | 0.30 |
| Missing specialty | 0.19 | 0.12 | 0.32 | 0.17 | 0.09 | 0.30 |
| Physician gender | ||||||
| Female | 0.70 | 0.62 | 0.80 | 0.72 | 0.62 | 0.83 |
| Missing | 0.89 | 0.49 | 1.59 | 0.91 | 0.44 | 1.85 |
| Physician age | ||||||
| Under 35 | 0.81 | 0.67 | 0.96 | 0.88 | 0.72 | 1.08 |
| 55 and over | 0.98 | 0.83 | 1.15 | 0.95 | 0.80 | 1.13 |
| Missing | 0.71 | 0.41 | 1.23 | 0.61 | 0.34 | 1.10 |
| Practice size | ||||||
| 4–8 | 0.87 | 0.75 | 1.01 | 0.84 | 0.72 | 0.98 |
| 9–15 | 0.80 | 0.67 | 0.95 | 0.79 | 0.65 | 0.95 |
| 16 and over | 0.82 | 0.71 | 0.95 | 0.86 | 0.73 | 1.01 |
| Patient age | ||||||
| 45–64 | 1.05 | 1.01 | 1.09 | 1.02 | 0.97 | 1.06 |
| 65+ | 0.99 | 0.90 | 1.09 | 0.86 | 0.76 | 0.98 |
| Patient gender | ||||||
| Male | 1.03 | 0.99 | 1.07 | 1.05 | 1.00 | 1.09 |
The top panel of Table 5 shows results for medication class, with antimicrobials serving as the referent. All other medication classes except asthma medications and anti-anxiety medications were less likely to be filled than antimicrobials. Medications for chronic conditions including hypertension, diabetes, and hyperlipidemia were less likely to be filled for all prescriptions and strikingly less likely to be filled when the medications were newly prescribed. The drug class least likely to be filled was pain medications. Of note, this class includes mostly narcotic medications that require a paper prescription.
Among the major primary care specialties represented in this sample, there were not significant differences between internists and family practitioners. Prescriptions written by other specialists were much less likely to be filled than those written by internists. Female prescriber gender, young prescriber age, and larger practice sizes were associated with lower primary adherence. Male patients were 5% more likely to fill a new prescription; this result was borderline statistically significant.
DISCUSSION
Medication non-adherence has been widely recognized as limiting the effectiveness of prescription treatment. However, assessment of adherence and interventions to improve adherence have been largely conditional on patients filling their initial prescriptions, and have failed to accurately account for primary non-adherence. The costs for pharmacies and insurers from patients not picking up medications has been recognized and defined in the industry as “leakage” of prescriptions, but this phenomenon has not been quantified in the medical literature.28 The potential of e-prescribing for accurate measurement of primary non-adherence should create opportunities to improve medication adherence. In this study we found that 22% of e-prescriptions were never filled, with an increase to 28% never filled when we restricted the sample to newly prescribed medications. Several factors were associated with lower primary adherence.
To date there has been a limited body of research addressing primary adherence. Beardon and colleagues tracked over 20,000 prescriptions written in 1989 for patients in general practice in the UK and found 5.2% primary non-adherence,21 while Matsui and colleagues tracked 1,014 prescriptions written in a pediatric ED in 1997 and found 7.3% primary non-adherence.8 Getting copies of actual prescriptions is very cumbersome, so most other studies of primary adherence relied on surveys, finding non-adherence rates ranging from 4% to 21.6%.23,24
The increasing use of e-prescribing creates the opportunity to measure primary non-adherence in larger populations, but very few such studies have been published to date. Ekedahl and Mansson evaluated over 91,000 e-prescriptions in a Swedish population with universal drug coverage and found a non-adherence rate of 2.4%.22 Two recent studies done at the Geisinger clinic in Pennsylvania used electronic data to study the care of patients with single conditions. One found that patients being started on treatment for hypertension failed to fill new prescriptions 17% of the time27 and another found that those being started on treatment for diabetes failed to fill new prescriptions 15% of the time.26 Our study found slightly higher rates of primary non-adherence. We evaluated patients treated in mostly smaller practices using stand-alone e-prescribing systems while the Geisinger clinic is a large integrated system with a full electronic health record. In addition, our data evaluated the first year of a new e-prescribing program during which e-prescribing use was increasing slowly, only approaching 50% of prescriptions at the end of the study period.29 We cannot say for certain if those differences in study settings account for the higher rate of non-adherence in our study. In either case, non-adherence in US studies was higher than in other countries; it is not clear whether this is due to differences between populations and health care systems or is due to differences in the ability to ascertain prescription filling in the United States; additional studies will be needed to verify these results.
From a policy perspective, the high rate of non-adherence to medications for hypertension, diabetes, and hyperlipidemia is an especially alarming finding; these three conditions contribute greatly to the burden of mortality and morbidity from cardiovascular disease in the United States. It has previously been shown that many patients with these conditions either lack awareness of their diagnoses or are not receiving treatment.30,31 If over one-quarter of such patients do not fill the medications prescribed by their physicians, the potential health gains from these medications will not be realized. In a study of patients being discharged after myocardial infarction, Jackevicius and colleagues found that lower adherence with discharge medications was associated with increased 1-year mortality.32 Whether these findings would hold in outpatient treatment has not yet been established. Interventions aimed at improving the quality of chronic disease management must address the needs and challenges of patients who are first initiated on essential medications.
Interventions to reduce primary non-adherence will be most effective if targeted towards those who are least likely to fill prescriptions. Higher patient cost-sharing has been shown to delay initiation of treatment for chronic conditions.33 Correspondingly, prescription of medications with lower copayments appeared to be associated with better primary adherence in two recent studies of single drug classes.26,27 These results highlight the importance of prescribing in compliance with a patient’s formulary, which was previously shown to affect refill adherence.34
We had limited patient-specific information, but did have a borderline significant finding that women were less likely than men to fill prescriptions, as found in an earlier study of hypertension medications,27 but not in a study of diabetes.26 Prescriptions from primary care clinicians were more likely to be filled. While some physician characteristics (female gender, young age) were associated with lower rates of primary adherence, our ability to explain non-adherence in this population is relatively limited. Some physicians may be more likely to prescribe lower-tier medications from patients′ formularies.35 Unmeasured patient and physician factors, such as the extent of physician–patient communication and education about prescriptions are likely to influence adherence. Further research will be needed to confirm and understand the causes of these findings and to develop interventions to improve primary adherence. The potential to identify primary non-adherence rapidly and accurately may allow for such interventions to be targeted specifically towards patients likely to benefit from education about the importance of their prescribed medications.
There are limitations that must be considered when interpreting these results. Our population is drawn from early adopters of e-prescribing and e-prescribing was not used for all prescriptions issued,29 so the physicians and patients may be atypical, limiting the generalizability of our findings. We have limited data on patient and physician characteristics, which limits our ability to explain the causes of non-adherence. Since we do not have data on the number of prescriptions written for patients who did not get e-prescriptions, we cannot extrapolate these findings to more general populations. Actions taken by patients, prescribers, or pharmacists that were not captured in our data may lead us to underestimate the rate of adherence. For example, if patients pay cash for inexpensive prescriptions (e.g. $4 generics),36 or fill medications at another location (e.g. VA) we would misclassify the prescription as unfilled. Any other data errors in the process of matching e-prescribing data to filled claims data could lead to a patient to being falsely labeled as non-adherent–this type of misclassification of the outcome could lead us to overestimate non-adherence. There are not standard approaches for performing these types of matches, so there is no benchmark against which we can compare our matching results; the methods that we employed will need to be evaluated further in other settings.
Telephone contacts between the pharmacy and the prescriber that lead to verbal changes in the medication prescribed would also cause us to misclassify prescriptions as unfilled. Our claims data ended on March 31, 2005, so we may have misclassified some e-prescriptions written in the final month but filled later. Non-adherence was only 4% higher for the final month and excluding it did not change any of the effect estimates in our models, so we did not exclude those data. Prescriptions given for possible but not definite use (e.g. antibiotics prescribed to be filled only if culture results are positive) would lead us to underestimate primary adherence. Although these errors may occur, we suspect they would not account for a large portion of the e-prescriptions.
These findings highlight the need to reprioritize efforts when trying to improve the quality of prescription drug care in the United States. We must continue to support patients who have already filled prescriptions for essential medication to enhance their persistence. However, our results suggest that relying solely on such a strategy to improve medication use will lead us to miss the potentially large number of patients who received a prescription but never initiate therapy. Our ability to link e-prescribing data to filled claims allows us to measure primary non-adherence, which was not possible previously. As more physicians adopt e-prescribing, the methods we describe here can be used to understand the predictors of non-adherence, explore barriers to appropriate medication use, and potentially provide adherence information back to prescribers. This research will be instrumental in developing interventions that encourage patients to initiate medications when prescribed, and to adhere to a full course of chronic therapy.
Electronic supplementary materials
Below is the link to the electronic supplementary material.
(DOC 43 kb)
Acknowledgements
We acknowledge the assistance of BCBSMA, Tufts HP, and ZixCorp in providing data. The investigators retained control over all aspects of the analyses and presentation of results.
The research was supported by AHRQ grant R01 HS15175.
Dr. Brookhart is supported by a career development grant from NIH (AG12084).
Dr. Shrank is supported by a career development grant from NIH (HL090505).
Conflict of Interest None disclosed.
References
- 1.Burwen DR, Galusha DH, Lewis JM, et al. National and state trends in quality of care for acute myocardial infarction between 1994-1995 and 1998-1999: the medicare health care quality improvement program. Arch Intern Med. 2003;163:1430–9. doi: 10.1001/archinte.163.12.1430. [DOI] [PubMed] [Google Scholar]
- 2.Ganz DA, Glynn RJ, Mogun H, et al. Adherence to guidelines for oral anticoagulation after venous thrombosis and pulmonary embolism. J Gen Intern Med. 2000;15:776–81. doi: 10.1046/j.1525-1497.2000.91022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Higashi T, Shekelle PG, Solomon DH, et al. The quality of pharmacologic care for vulnerable older patients. Ann Intern Med. 2004;140:714–20. doi: 10.7326/0003-4819-140-9-200405040-00011. [DOI] [PubMed] [Google Scholar]
- 4.Jencks SF, Huff ED, Cuerdon T. Change in the quality of care delivered to Medicare beneficiaries, 1998-1999 to 2000-2001. JAMA. 2003;289:305–12. doi: 10.1001/jama.289.3.305. [DOI] [PubMed] [Google Scholar]
- 5.McGlynn EA, Asch SM, Adams J, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–45. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 6.Shrank WH, Asch SM, Adams J, et al. The quality of pharmacologic care for adults in the United States. Med Care. 2006;44:936–45. doi: 10.1097/01.mlr.0000223460.60033.79. [DOI] [PubMed] [Google Scholar]
- 7.Benner J, Glynn R, Mogun H, Neumann P, Weinstein M, Avorn J. Long-term persistence in use of statin therapy in elderly patients. JAMA. 2002;288:455–61. doi: 10.1001/jama.288.4.455. [DOI] [PubMed] [Google Scholar]
- 8.Matsui D, Joubert G, Dykxhoorn S, Rieder M. Compliance with prescription filling in the pediatric emergency department. Arch Pediatr Adolesc Med. 2000;154(2):195–8. doi: 10.1001/archpedi.154.2.195. [DOI] [PubMed] [Google Scholar]
- 9.O’Connor PJ. Improving medication adherence: challenges for physicians, payers, and policy makers. Arch Int Med. 2006;166:1802–4. doi: 10.1001/archinte.166.17.1802. [DOI] [PubMed] [Google Scholar]
- 10.Osterberg L, Blaschke T. Drug therapy-adherence to medication. N Engl J Med. 2005;353(5):487–97. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 11.Partridge A, Wang P, Winer E, Avorn J. Non-adherence to adjuvant tamoxifen therapy in women with primary breast cancer. J Clin Oncol. 2003;21:602–6. doi: 10.1200/JCO.2003.07.071. [DOI] [PubMed] [Google Scholar]
- 12.Partridge AH, Avorn J, Wang PS, Winer EP. Adherence to therapy with oral antineoplastic agents. J Natl Cancer Inst. 2002;94:652–61. doi: 10.1093/jnci/94.9.652. [DOI] [PubMed] [Google Scholar]
- 13.Siegel D, Lopez J, Meier J. Antihypertensive medication adherence in the department of veterans affairs. Am J Med. 2007;120:26–32. doi: 10.1016/j.amjmed.2006.06.028. [DOI] [PubMed] [Google Scholar]
- 14.Ho PM, Rumsfeld JS, Masoudi FA, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–41. doi: 10.1001/archinte.166.17.1836. [DOI] [PubMed] [Google Scholar]
- 15.Ho PM, Spertus JA, Masoudi FA, et al. Impact of medication therapy discontinuation on mortality after myocardial infarction. Arch Intern Med. 2006;166:1842–7. doi: 10.1001/archinte.166.17.1842. [DOI] [PubMed] [Google Scholar]
- 16.Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS. Impact of medication adherence on hospitalization risk and healthcare cost. Med Care. 2005;43:521–30. doi: 10.1097/01.mlr.0000163641.86870.af. [DOI] [PubMed] [Google Scholar]
- 17.Caro JJ, Salas M, Speckman JL, Raggio G, Jackson JD. Persistence with treatment for hypertension in actual practice. CMAJ. 1999;160(1):31–7. [PMC free article] [PubMed] [Google Scholar]
- 18.Enhancing Prescription Medicine Adherence: A National Action Plan. 2007. (Accessed January 5, 2010, at http://www.talkaboutrx.org/documents/enhancing_prescription_medicine_adherence.pdf. .)
- 19.Adherence to long-term therapies: evidence for action. Geneva: WHO; 2003. [PubMed] [Google Scholar]
- 20.Andrade SE, Kahler KH, Frech F, Chan KA. Methods for evaluation of medication adherence and persistence using automated databases. Pharmacoepidemiol Drug Saf. 2006;15:565–74. doi: 10.1002/pds.1230. [DOI] [PubMed] [Google Scholar]
- 21.Beardon PHG, McGilchrist MM, McKendrick AD, McDevitt DG, MacDonald TM. Primary non-compliance with prescribed medication in primary care. Br Med J. 1993;307(6908):846–8. doi: 10.1136/bmj.307.6908.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ekedahl A, Mansson N. Unclaimed prescriptions after automated prescription transmittals to pharmacies. Pharm World Sci. 2004;26:26–31. doi: 10.1023/B:PHAR.0000013464.09197.41. [DOI] [PubMed] [Google Scholar]
- 23.Wamala S, Merlo J, Bostrom G, Hogstedt C, Agren G. Socioeconomic disadvantage and primary non-adherence with medication in Sweden. Int J Qual Health Care. 2007;19:134–40. doi: 10.1093/intqhc/mzm011. [DOI] [PubMed] [Google Scholar]
- 24.Wroth TH, Pathman DE. Primary medication adherence in a rural population: the role of the patient-physician relationship and satisfaction with care. J Am Board Fam Med. 2006;19:478–86. doi: 10.3122/jabfm.19.5.478. [DOI] [PubMed] [Google Scholar]
- 25.Bell DS, Marken RS, Meili RC, et al. Recommendations for comparing electronic prescribing systems: results of an expert consensus process. Health Affairs 2004;Jan-Jun;Suppl Web Exclusives:W4-305-17. [DOI] [PubMed]
- 26.Shah NR, Hirsch AG, Zacker C, Taylor S, Wood GC, Stewart W. Factors associated with first-fill adherence rates for diabetic medications: a cohort study. J Gen Intern Med. 2008;24:233–7. doi: 10.1007/s11606-008-0870-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shah NR, Hirsch AG, Zacker C, et al. Predictors of first-fill adherence for patients with hypertension. Am J Hypertens. 2009;22:392–6. doi: 10.1038/ajh.2008.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lapane KL, Dubé C, Schneider KL, Quilliam BJ. Patient perceptions regarding electronic prescriptions: is the geriatric patient ready? J Am Geriatr Soc. 2007;55:1254–9. doi: 10.1111/j.1532-5415.2007.01248.x. [DOI] [PubMed] [Google Scholar]
- 29.Fischer MA, Stedman MR, Vogeli C, Ferris TG, Weissman JS. Uptake of electronic prescribing in community-based practices. J Gen Intern Med. 2008;23:358–63. doi: 10.1007/s11606-007-0383-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Total prevalence of diabetes in the United States, all ages, 2005. 2005. (Accessed January 5, 2010, at http://www.cdc.gov/diabetes/pubs/estimates05.htm#prev, at
- 31.Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. JAMA. 2003;289(19):2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 32.Jackevicius CA, Li P, Tu JV. Prevalence, predictors, and outcomes of primary nonadherence after acute myocardial infarction. Circulation. 2008;117(8):1028–36. doi: 10.1161/CIRCULATIONAHA.107.706820. [DOI] [PubMed] [Google Scholar]
- 33.Solomon MD, Goldman DP, Joyce GF, Escarce JJ. Cost sharing and the initiation of drug therapy for the chronically Ill. Arch Intern Med. 2009;169(8):740–8. doi: 10.1001/archinternmed.2009.62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shrank WH, Hoang T, Ettner SL, et al. The implications of choice: prescribing generic or preferred pharmaceuticals improves medication adherence for chronic conditions. Arch Int Med. 2006;166:332–7. doi: 10.1001/archinte.166.3.332. [DOI] [PubMed] [Google Scholar]
- 35.Shrank WH, Fox SA, Kirk A, et al. The effect of pharmacy benefit design on patient-physician communication about costs. J Gen Intern Med. 2006;21:334–9. doi: 10.1111/j.1525-1497.2006.00402.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Barbaro M, Abelson R. Relief for Some but Maybe Not Many in Wal-Mart Plan for $4 Generic Drugs The New York Times 2006 September 22, 2006.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Below is the link to the electronic supplementary material.
(DOC 43 kb)