Abstract
The Emotional Cascade Model proposes that the emotional and behavioral dysregulation of individuals with borderline personality disorder (BPD) may be fundamentally linked through emotional cascades, vicious cycles of intense rumination and negative affect that may induce aversive emotional states. In order to reduce this aversive emotion, dysregulated behaviors such as non-suicidal self-injury may then be used as distractions from intense rumination. This study explored emotional cascades in a sample enriched with subjects meeting diagnostic criteria for BPD. The first part of the study explored a structural equation model that examined the mediational effects of emotional cascades on the relationship between BPD symptoms and dysregulated behavior and found evidence for full mediation, even after controlling for symptoms of depression and other Cluster B disorders. The second part of the study examined the effects of a rumination induction conducted with the intention of eliciting emotional cascades in those diagnosed with BPD. The results demonstrated that individuals with BPD experienced greater reactivity and intensity of negative affect, but not of positive affect, following the procedure – even when controlling for current depressive symptoms. Future directions and clinical implications for the Emotional Cascade Model are discussed.
Keywords: borderline personality disorder, emotion regulation, rumination, suicide attempts, binge-eating
An Exploration of the Emotional Cascade Model in Borderline Personality Disorder
Borderline personality disorder (BPD) is a disorder in which affected individuals experience difficulties with affective instability and regulation (Koenigsberg, et al., 2002; Yen, Zlotnick, & Costello, 2002) as well as dysregulated behaviors, such as non-suicidal self-injury (NSSI) and binge-eating (Brown, Comtois, & Linehan, 2002; Marino & Zanarini, 2001). Yet, the specific nature of this relationship between emotional and behavioral dysregulation has been somewhat elusive. A recent theoretical model, the Emotional Cascade Model (Selby & Joiner, in press; Selby, Anestis, & Joiner, 2008), suggests that the relationship between emotional and behavioral dysregulation in BPD may be explained by rumination. This is because intense rumination may result in “emotional cascades,” which may then lead to dysregulated behaviors for distraction. The purpose of this study was to explore the role of emotional cascades in BPD.
Behavioral Dysregulation in BPD
Individuals with BPD report a wide array of dysregulated behaviors, ranging from interpersonal arguments and fights, to binge-eating and self-injury, and some theories of BPD have attempted to address this relationship. Interpersonal theories of BPD suggest that behavioral dysregulation is used as a way of eliciting desired responses from others or avoiding abandonment (Allen, 1995), or that these behaviors help the individual create boundaries from self and others by affirming one’s identity through cutting and creating scars (see Suyemoto, 1998). Feeling generation/anti-dissociation theories of BPD suggest that behaviors such as NSSI may be used to shock the individual out of dissociative states through the physical sensations produced by the behavior (Gunderson, 1984). Some theories of dysregulated behavior, though not specifically aimed at BPD, suggest that these behaviors serve as ways to escape from aversive perceptions about the self (Heatherton & Baumeister, 1991), or as a way to express anger at and punish oneself (see Klonsky, 2007). Finally, more recent theories have begun to suggest that dysregulated behaviors serve as ways of facilitating emotional avoidance (Chapman, Gratz, & Brown, 2006), although the mechanisms through which these behaviors result in emotional avoidance lack some specificity. For example, the Experiential Avoidance Model (Chapman et al., 2006) suggests that NSSI distracts from negative affect and is negatively reinforcing, yet it is unclear why NSSI is used to distract rather than other behaviors. As can be seen from this brief presentation, the link between BPD and behavioral dysregulation remains at issue (see Selby & Joiner, in press, for a more detailed discussion of how the Emotional Cascade Model compares to and contrasts with other theories). As will be seen, the Emotional Cascade Model not only builds from these theories, but is also consistent with many of them in that most suggest that emotional problems are linked to dysregulated behaviors in fundamental ways.
Emotion Dysregulation in BPD
Linehan (1993) has suggested that individuals with BPD experience emotion dysregulation as: 1) heightened sensitivity to emotional stimuli, 2) experiencing emotions as extremely intense, and 3) a slow return to emotional baseline. Similar to the Experiential Avoidance Model (Chapman et al., 2006), Linehan’s theory also posits that dysregulated behaviors (such as impulsive and self-injurious behavior) result because these behaviors provide a way for an individual to shift attention away from unpleasant emotional states. However, this connection between emotional and behavioral dysregulation spurs the same question that the Experiential Avoidance Model has some difficulty answering: If these behaviors serve as methods of distraction, why don’t individuals with BPD use less problematic forms of distraction such as taking a cold shower, watching television, or talking to a friend to shift attention away from an emotional state?
One potential construct that may provide insight into this unanswered question, as well as into Linehan’s theory more generally, may be rumination. Rumination (Nolen-Hoeksema, 1991) is the tendency to repetitively think about the causes, situational factors, and consequences of one’s negative emotional experience – in other words continuously thinking about and focusing attention on emotionally relevant stimuli. Rumination may be a process that contributes to the heightened sensitivity, increased intensity, and extended duration of emotions in BPD that Linehan’s theory suggests. For example, the tendency to engage in rumination when upset has generally been found to magnify negative affect as well as increase its duration (see Thomsen, 2006 for a review). There is also some indication that multiple ruminative processes may exist (Watkins, 2008), some of which may be relevant to BPD. For example, catastrophizing (Garnefski, Kraaij, & Spinhoven, 2001) is the tendency to continuously think about how terrible a situation is and emphasize the negative implications for the future, and it has also been linked to dysregulated behaviors (Selby, Anestis, & Joiner, 2008).
The Emotional Cascade Model
According to the Emotional Cascade Model (Selby & Joiner, in press; Selby et al., 2008), the reciprocal relationship between negative affect and ruminative processes results in an “emotional cascade,” which is usually initiated by an emotion eliciting event. This event causes the individual to ruminate intensely, which increases the intensity of the emotion. As the intensity of the emotion rises, the individual finds that it is more and more difficult to divert attention away from emotional experience, and as a result he or she pays more attention to emotional stimuli (Carver, Blaney, & Scheier, 1979; Salovey, 1992); this results in a positive feedback loop between rumination and negative affect. In support of this hypothesis, a recent experience sampling study by Moberly and Watkins (2008) found evidence for a reciprocal relationship between rumination and negative affect (in non-BPD participants), such that if an individual had high rumination at one experience signal, he or she was likely to have higher negative affect at the next signal, and vice versa. Thus, there may be a pernicious bi-directional relationship between negative affect and rumination.
Essentially, rumination may contribute to and become part of a subsequent emotional cascade. Rumination in the view of the Emotional Cascade Model differs somewhat from rumination in the sense proposed by other researchers (Nolen-Hoeksema, 1991) in that it is one facet of a dynamic process. While others have mentioned that dysregulated behaviors may be used to escape from ruminative thoughts (Nolen-Hoeksema et al., 2007) the Emotional Cascade Model suggests that rumination is the major driving force in causing dysregulated behaviors. Whereas other models may, in our understanding, tend to view rumination as a static phenomenon, with an individual ruminating and initially increasing, and then maintaining, negative affect at a stable level, the view of the Emotional Cascade Model is that rumination and negative affect interact in a perpetuating and exacerbating cycle that leaves the individual desperate for some form of distraction to interfere with the rumination.
Thus, the end result of an emotional cascade is an extremely high, extremely aversive, state of negative affect. Because of the intensity of this feedback loop, minor distractions may be insufficient to inhibit this cycle – and as a result the individual may search for more potent ways to distract from emotion and short-circuit the emotional cascade. These more potent forms of distraction may be what are thought of as behavioral dysregulation: substance abuse, NSSI, binge-eating, or problematic interpersonal behaviors (i.e. yelling or threatening). These behaviors may inhibit the emotional cascade because they are particularly salient forms of distraction, due to the sensory effects that these behaviors possess (e.g., taste/fullness in binge-eating, or the effects of a substance), as well as the emotion regulatory effects that the individual believes these behaviors have. Whereas other behaviors may help distract someone with low levels of rumination (e.g., a cold shower), those same behaviors may not be distracting enough for an individual ruminating intensely (e.g., continuing to ruminate during a cold shower). Alternatively, behaviors that result in intense physical sensations may be much more distracting, such as pain or the sight of blood during NSSI. For example, cutting and then attempting to control the bleeding may effectively draw attention away from rumination about a problem. Behavioral dysregulation may only have temporary effects, however, and certain behaviors may actually incite another emotional cascade, due to feelings of shame or embarrassment because of the behavior, as in binging and purging, for example.
In general, rumination has been linked to a variety of dysregulated behaviors including NSSI (Armey & Crowther, 2008; Hilt et al., 2008), binge-eating (Nolen-Hoeksema et al., 2007), aggression (Bushman et al., 2001; Bushman et al., 2005), and alcohol use (Nolen-Hoeksema & Harrell, 2002; Nolen-Hoeksema et al., 2007). There is also some evidence that rumination is a problem for individuals with BPD. In one study examining rumination in BPD, Abela et al. (2003) found that participants diagnosed with BPD had significantly higher levels of rumination than individuals diagnosed with major depressive disorder. A second study linking rumination to BPD was conducted by Smith et al. (2006), who examined rumination among all Axis II personality disorders. They found that of all the Axis II disorders, rumination was uniquely related to dimensions of BPD in college students, even after controlling for depression. Thus, rumination may serve as an important link between BPD and behavioral dysregulation.
Although the Emotional Cascade Model is primarily concerned with increases in negative affect, positive affect in individuals with BPD may also be influenced by an emotional cascade. For example, BPD individuals who report feelings of emptiness have been found to have pathologically low levels of positive affect (Klonsky, 2008). One experience sampling study found that, subsequent to daily life stressors, individuals with BPD experienced greater reactivity of both simultaneous decreases in positive affect and increases in negative affect than those with psychotic disorders and control subjects (Glaser, Van Os, Mengelers, & Myin-Germeys, 2008). There is also evidence that some dysregulated behaviors are associated with decreases in positive affect, in addition to increases in negative affect, prior to the behavior, such as in binging and purging (Smyth et al., 2007). Thus, although the Emotional Cascade Model does not specifically predict decreases in positive affect, empirical evidence indicates that both increased negative affect and decreased positive affect may occur prior to a dysregulated behavior.
Current Study
The purpose of this study was to explore the Emotional Cascade Model in BPD, as well as to expand research on rumination in BPD. First, information was collected on BPD symptoms and diagnosis, multiple measures of rumination, and behavioral dysregulation in a sample enriched with individuals diagnosed with BPD, as well as participants with subthreshold symptoms and control subjects. This information was then used to test a structural equation model that evaluated the mediational role of rumination in the relationship between symptoms of BPD and behavioral dysregulation. Second, all participants then engaged in an experimental rumination induction procedure with the intention of eliciting emotional cascades in the BPD group. Individuals with BPD diagnoses were then compared to a group of participants without any symptoms of BPD to determine if the rumination induction had unique effects on the BPD group.
Hypotheses
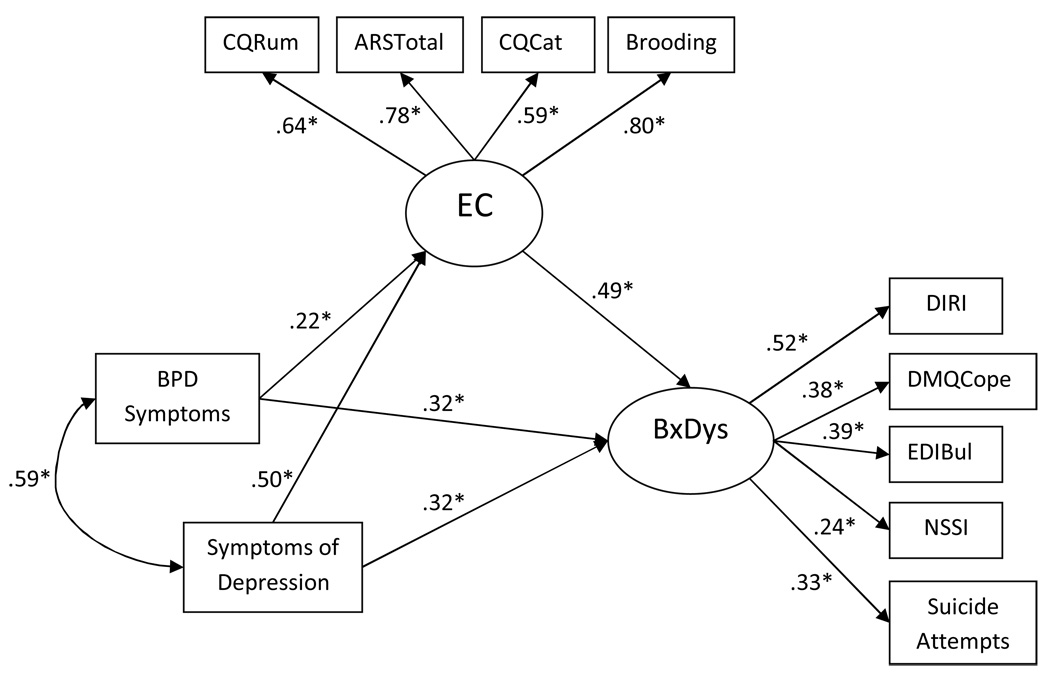
In the structural equation model (see Figure 1) it was hypothesized that the relationship between symptoms of BPD and a latent variable of behavioral dysregulation would be fully mediated by a latent variable of Emotional Cascades (using multiple indicators of rumination). Symptoms of depression were included as a covariate in the model because rumination is highly associated with depression (Just & Alloy, 1997), and demonstrating that BPD symptoms predicted Emotional Cascades when controlling for symptoms of depression was necessary to explore the specificity of Emotional Cascades to BPD. Symptoms of narcissistic and histrionic personality disorders were also used as covariates in the analyses to test the specificity of Emotional Cascades to BPD beyond other Cluster B symptoms, as other Cluster B personality disorders have been found to experience problems with negative emotionality and impulsivity (James & Taylor, 2008), and we desired to identify a relationship between BPD and emotional cascades beyond alternative Cluster B psychopathology.
Figure 1. SEM model testing the mediational effect of rumination on the relationship between symptoms of BPD and behavioral dysregulation.
Note: N=142. CQRum = rumination as measured by the CERQ, ARStot=total of the Anger Rumination Scale, CQCat=catastrophizing as measured by the CERQ, Brooding = the brooding scale of the RRS; DIRI = excessive reassurance seeking, DMQCope = DMQ Drinking to Cope subscale, EDIBul = Bulimia subscale of the EDI, NSSI = frequency of non-suicidal self-injury; EC=Emotional Cascades latent variable, BxDys=Behavioral Dysregulation latent variable. Symptoms of HPD and NPD were included as covariates in the model, but are not displayed in the figure due to no significant paths and for ease of presentation.
Following the testing of the model, the effects of the experimental rumination induction were explored on a group of individuals diagnosed with BPD and compared to a control group that endorsed no symptoms of BPD. This was done to test the hypothesis that the BPD group would experience unique increases in negative affect following the induction, as well as higher levels of baseline negative affect. It was also hypothesized that individuals with BPD would experience unique reductions in positive affect following the induction, as reduction in positive affect may also be associated with emotional cascades.
Methods
Screening Procedure
Approximately 5,000+ Introduction to Psychology students at the Florida State University were screened throughout 2006 as a part of their research requirement for the course. During this screening session all students were given a packet of screening measures for ongoing research throughout the department, and in return for completing the screening process all students received course credit. Students were screened using 9 modified items from the BPD Module of the SCID-II Screening Questionnaire (First et al., 1997). These questions were meant to identify individuals who endorsed symptoms of BPD prior to a structured interview. These questions consisted of forced yes/no answers to questions such as, “Have you ever self-injured?” and “Have you often been frantic when you thought that someone you really cared about was going to leave (abandon) you?”
In order to enrich the sample for participants with features of BPD and BPD diagnoses, “invitation only” phases of data collection were arranged where only those invited to participate were allowed into the study. At all other times the study was open to anyone interested in participating (in order to obtain control subjects). In order to be invited to the study at times that were “invitation only,” an individual had to have endorsed five or more of the screening questions. Individuals identified as meeting screening criteria were emailed with an invitation to participate because of their answers pertaining to “unique emotional experiences” during the screening session. The experimenters who ran the study for each participant were blind as to whether the participants met screening criteria or not, and they did not know when the study was “invitation only” or open participation.
During the spring semester of 2006 participation in the study was open to all students for the first half of the semester; thereafter, participation was restricted to individuals who were invited to participate if they met screening criteria for invitation to the study. This recruitment sequence was reversed for the summer and fall semesters so that individuals meeting screening criteria were invited first, and then participation was opened to all students later in the semester. This alternating of the invitation phase sequence was done in order to control for possible differences in subjects who participated in the study early versus late in the semester.
Participants
Participants consisted of 142 individuals, 33 men (23.2%) and 109 women. Participant ages ranged from 18–24 with the average age of participants being 18.75 (SD=1.05). Ethnicity was 69% Caucasian, 14.1% Hispanic, 10.6% African-American, 2.8% Asian, 2.1% Native American, and 1.4% other. With regard to self-reported socio-economic status (SES), 4.4% of participants reported being from low SES, 72.8% reported being from middle SES, and 22.8% reported being from high SES. This study was approved by the university IRB and all participants provided full, informed, and written consent to participate in all aspects of the study. Following the administration of structured clinical interviews, a total of 39 participants (27% of the sample, which was enriched) met diagnostic criteria for BPD.
Procedures
All participants completed a battery of questionnaires, engaged in a structured clinical interview, and participated in the rumination induction procedure. Each study session was carried out by a trained research assistant or graduate student trained by the primary investigator to competency on the rumination induction procedure and clinical interview. Following the interview, all participants engaged in the rumination induction. All participants were debriefed on the purpose of the study after completion.
Structured Clinical Interview
Structured Clinical Interview for Diagnosis of DSM-IV Axis II Personality Disorders (SCID-II; First et al., 1997). All participants received structured clinical interviews for the borderline personality disorder, histrionic personality disorder, and narcissistic personality disorder modules of the SCID-II; all items from these models were assessed during the interview, regardless of the participants’ responses to the initial screening described above. Due to time constraints, symptoms of antisocial personality disorder and Cluster A and C personality disorders were not assessed in this study. These interviews were completed by trained graduate students in clinical psychology; all interviewers were instructed to take extensive notes for symptoms endorsed by the participants. Individuals were rated 1–3 for each symptom of BPD, NPD, and HPD (1-symptom not present, 2-subthreshold symptom, and 3-symptom present). Upon completion of the structured interviews, all interviews were cross-checked by two masters-level graduate students in clinical psychology. Cross-checking involved examining each SCID-II after the interview was completed and reviewing the evidence for establishing whether each symptom was at threshold level, subthreshold, or absent. If there were disagreements on the initial threshold level for any criterion, the cross-checking student consulted with the interviewer as to whether the participant was appropriately rated for the symptom and a consensus was reached. If needed, the second cross-checking student was brought in for a second opinion. Although no inter-rater reliability information was collected in this study, inter-rater reliability from the use of structured interviews in this lab has previously been demonstrated to range from .79 to .91 for Axis I and II diagnoses (Fink et al., in press).
Scores on each of these modules were calculated so that each individual received a total score of symptoms endorsed for each personality disorder, as well as a dichotomous yes/no diagnosis. Symptom counts for each disorder were created by summing each symptom for the disorder so that subthreshold symptoms were included. The correlation between a formal diagnosis of BPD and the continuous measure of BPD was r=.84 (p<.001), which suggests some validity for the continuous measure of BPD symptoms. The use of a continuous measure of BPD symptoms is also important given that evidence suggests BPD may be non-taxonic (Rothschild, Cleland, Haslam, & Zimmerman, 2003) and there have been suggestions to shift to a dimensional model of personality disorders for DSM-V (Widiger & Trull, 2007). The rate of endorsement for BPD symptoms ranged from 18% of the sample meeting threshold level for the identity disturbance criterion, to 35% of the sample meeting threshold for the affective instability criterion. This suggests that threshold levels for all BPD symptoms were adequately represented in the sample. The alpha for the continuous measure of BPD was α=.80.
Emotional Cascades Measures
The following scales were used to create a latent variable of overall rumination (including anger rumination and catastrophizing) that was referred to as Emotional Cascades.
The Cognitive Emotion Regulation Questionnaire (CERQ; Garnefski, Kraaij, & Spinhoven, 2001) is a 36-item self-report questionnaire that measures the degree to which individuals utilize various cognitive approaches towards regulating negative emotions. Although the CERQ has various subscales, only the eight questions for the Rumination and Catastrophizing subscales were used in this study because they represent ruminative processes. Items utilize a Likert type scale ranging from 1 (Almost never) to 5 (Almost always). The Rumination subscale consists of four items that measure the degree to which individuals engage in perseverative thinking focused entirely upon their own emotions in response to negative affective states (e.g., “I am preoccupied with what I think and feel about what I have experienced.”). The Catastrophizing subscale consists of four items that measure the degree to which individuals tend to believe their negative emotions and experiences will result in highly aversive consequences (e.g., “I often think that what I have experienced is the worst that can happen to a person.”). The Rumination subscale had an alpha of α = .67 and the catastrophizing subscale had an alpha of α = .72 in this sample.
The Anger Rumination Scale (ARS; Sukhodolsky, Golub, & Cromwell, 2001) is a 19-item self-report questionnaire examining the degree to which individuals tend to maintain focus on angry moods rather than engaging in problem solving or re-evaluating the potential value of the situation (e.g. “Whenever I experience anger, I keep thinking about it for a while.”). Items utilize a Likert scale ranging from 1 (Almost never) to 4 (Almost always). In this study the ARS total had an alpha of .94.
The Response Styles Questionnaire (RSQ; Nolen-Hoeksema & Morrow, 1991) is a 71-item self-report measure assessing the manner in which an individual reacts to his/her mood. Items utilize a Likert scale ranging from 1 (Almost never) to 4 (Almost always). The RSQ assesses four response domains: Ruminative Responses, Distracting Responses, Problem-Solving, and Dangerous Activities. The Ruminative Responses Scale (RRS) can be further divided into two subscales: Brooding and Reflection. In this study, only the Brooding subscale of the RRS was used because brooding appears to involve a more intense focus on upsetting thoughts and emotions, while reflection appears to be a calmer analysis of upsetting situations. The Brooding subscale consists of five items assessing an individual’s tendency to focus on the reasons for his or her distress (e.g., “Think ‘What am I doing to deserve this?’”). In this sample, the Brooding scale had an alpha of α = .81.
Reports of Dysregulated Behaviors
The following scales were used to create a latent variable of Behavioral Dysregulation (including alcohol use, binge-eating, NSSI, excessive reassurance seeking, and suicide attempts) in order to represent an overall tendency to engage in dysregulated behaviors.
The Depressive Interpersonal Relationships Inventory – Reassurance Seeking subscale (DIRI-RS; Joiner, Alfano, & Metalsky, 1992) is a four item scale that measures the degree to which individuals seek reassurance from others, as well as the participants’ tendencies to subsequently doubt feedback from peers and seek further reassurance, leading to interpersonal difficulties. This scale may be relevant to BPD in that excessive reassurance seeking may be akin to begging, pleading, or threatening others, behaviors which may distract from emotional cascades, and previous work has shown that it loads on a dysregulated behavior latent variable (Selby et al., 2008). In this sample, the internal consistency was α = .88.
The Eating Disorder Inventory (EDI; Garner, Olmstead, & Polivy, 1983) is a self-report questionnaire that consists of 64 items that measure the degree to which participants exhibit pathological eating behaviors. In additional to a total score, the EDI yields eight subscales; we utilized only the Bulimia subscale, which assesses the degree to which individuals engage in binge-eating and purging. Individual items use a Likert scale (1=strongly agree; 5=strongly disagree) and the internal validity of the measure has been widely reported. Additionally, discriminant validity for Bulimia Nervosa and Anorexia Nervosa diagnoses has been reported (Garner et al., 1983). The alpha for this scale was α = .84.
The Drinking Motives Questionnaire (DMQ; Cooper et al., 1992) is a self-report questionnaire that assesses the degree to which participants consume alcohol for a variety of motives. The scale consists of three dimensions – coping motives, enhancement motives, and social motives. Each dimension is measured with five questions and the individual test items utilize a Likert style format ranging from 1 (almost never/never) to 4 (almost always). In this study, we utilized only the Coping subscale, which assesses the degree to which participants consume alcohol explicitly to reduce sensations of negative affect. The alpha for this scale was α = .84.
The Functional Assessment of Self-Mutilation (FASM; Lloyd et al., 1997) is a self-report questionnaire that assesses the degree to which participants have engaged in a variety of self-injurious behaviors without suicidal intent (e.g. cutting/carving, burning) during the course of the previous year, as well as the reasons for which participants engaged in each of those behaviors. In this study, only the total frequency of engaging in NSSI was used.
The Beck Scale for Suicide Ideation (BSS; Beck, Steer, & Ranieri, 1988) is a 21-item self-report measure used to determine various facets of risk for suicidal behavior. Only question 20 of the BSS was used because it contains the number of previous suicide attempts and is rated as: 0 = no attempts, 1 = one attempt, and 2 = more than one attempt.
Covariates
The Beck Depression Inventory - II (BDI-II; Beck, Steer, & Garbin, 1998) is a 21-item self-report measure of depressive symptoms. A Likert scale (0–3) is used to examine the degree to which depressive symptoms have been present during the previous two weeks. Scores below 10 indicate minimal symptoms, scores 10–18 indicate mild symptoms, and scores greater than 18 indicate moderate to severe symptoms. The internal consistency for this measure was adequate (α=.90).
Histrionic and Narcissistic Personality Disorder Symptoms. The SCID-II was used to assess non-BPD Cluster B psychopathology, excluding symptoms of antisocial personality disorder (ASPD), which were not assessed due to time constraints. Histrionic (HPD) and narcissistic (NPD) personality disorders were included as covariates in the analyses because Cluster B personality disorders have all been shown to have problems with negative emotionality and impulsivity (James & Taylor, 2007). Variables for HPD and NPD were created by summing the respective symptoms of these disorders; symptoms of HPD had an alpha of α=.67 while symptoms of NPD had an alpha of α=.74.
Emotion Measure
The following measure was used in the rumination induction:
Positive Affect Negative Affect Schedule (PANAS; Watson, Tellegen, & Clark, 1988). The PANAS is a commonly used measure of state emotional experience. Participants completed this measure both before and after the rumination induction. On this measure they answered 10 questions pertaining to their current experience of negative emotions and 10 questions pertaining to their current experience of positive emotions using a 5-point Likert scale (1=slightly/not at all, 5=Extremely). The 10 negative emotions to be rated were: upset, distressed, scared, ashamed, afraid, guilty, hostile, irritable, jittery and nervous. At baseline (T1) these items demonstrated an alpha of .89, and following the rumination induction (T2) they demonstrated an alpha of .90. The 10 positive emotions to be rated were: interested, excited, strong, enthusiastic, proud, alert, determined, attentive, inspired, and active. At baseline (T1) these items demonstrated an alpha of .91, and following the rumination induction (T2) they demonstrated an alpha of .92.
Rumination Induction
Prior to the start of the rumination induction all participants completed a baseline measure of positive and negative emotions using the PANAS and were given the instructions. They were informed that people respond to the procedure differently, and that they should be as honest as possible when answering questions before and after the procedure. This was done with the purpose of diminishing potential demand characteristics in the procedure. The instructions for the rumination induction were read verbatim:
Now think about something in your life currently or in the past that is upsetting to you. Try to focus all of your concentration on your feelings about that problem. Consider what these feelings mean and why you feel this way. Analyze the events surrounding this problem and try to understand how they contribute to your feelings. Please do this for the next five minutes.
The rumination induction was purposely kept relatively short in order to demonstrate that rumination could quickly increase negative affect, providing potential support for the experience of an emotional cascade.
Data Analytic Strategy
The first portion of our data analytic approach used structural equation modeling (SEM). This statistical method has advantages over other techniques used to analyze theoretical relationships because it relies on several indicators, rather than a single instrument, to assess a construct of interest, and it allows one to simultaneously assess measurement models (or factor loadings) onto latent variables and relationships (or correlations) between the latent variables. This reduces measurement error and increases construct validity. SEM analyses were conducted with the statistical program AMOS 6.0 (Arbuckle & Wothke, 1999).
The model that was tested using structural equation modeling is displayed in Figure 1. The first latent variable in the model was for Emotional Cascades, and was composed of the following indicators: CERQ Rumination, CERQ Catastrophizing, the total score for the Anger Rumination Scale, and the Brooding subscale of the RRS. The second latent variable in the model was Behavioral Dysregulation, which was created as an overall measure of tendencies to engage in various dysregulated behaviors. This latent variable was composed of the following indicators: excessive reassurance seeking (DIRI), drinking to cope with negative affect (DMQCope), dysregulated eating behaviors (EDIBul), NSSI, and number of previous suicide attempts. Previous SEM analyses have found many of these behaviors to significantly load onto a single latent variable while providing good fit to the data (Selby, Anestis, & Joiner, 2008).
The structural equation model included four observed variables: symptoms of BPD, depressive symptoms, and symptoms of HPD and NPD. The Symptoms of BPD variable was created as a continuous variable so that individuals with subthreshold symptoms of BPD would be accounted for in the model. The HPD and NPD variables were also created as continuous variables.
The model displayed in Figure 1 is recursive, and as such it is an identified model. In order to evaluate the overall model, the maximum likelihood chi-square statistic (χ2) was used (with non-significance indicating that the model fit the data perfectly). Due to the chi-square’s sensitivity to large sample sizes, other fit indices were used including the comparative fit index (CFI), the root mean square error of approximation (RMSEA), and the Tucker-Lewis Fit Index (TLI). Standard cutoff criteria for good fit were used to judge the model as a whole, and consisted of CFI values greater than .95, RMSEA values of less than .06, and TLI values of greater than .90 (Hu & Bentler, 1999). To test individual parameter estimates, a cutoff criterion value for significance was set at p = .05.
The second portion of the study involved the use of repeated measures MANCOVA. This analytic approach was used to assess the effects of the rumination induction on the BPD and control group, and to determine if individuals with BPD reported greater reactivity of negative and positive affect than control subjects, who endorsed no symptoms of BPD. Group differences in baseline negative and positive affect were also examined using MANCOVA analyses. BDI-II total score was used as a covariate in all analyses.
Results
Preliminary Analyses
The means, standard deviations, and inter-correlations for all variables are displayed in Table 1. All variables were examined for the presence of outliers. One outlier was present for the NSSI variable, where one individual reported over 1000 instances of self-injury, while the next highest report was 105. Rather than delete this individual from the analyses, however, the individual’s score on NSSI frequency was brought to the fence and changed to 105. There were no other outliers in the data.
Table 1.
Means and Standard Deviations for, and Inter-correlations Between, All Measures
| 1 | 2 | 3 | 4 | 5 | 6 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. BPD | -- | ||||||||||||
| 2. BDI Tot | .59** | -- | |||||||||||
| 3. ARS Tot | .46** | .48** | -- | ||||||||||
| 4. CQ Rum | .31** | .37** | .46** | -- | |||||||||
| 5. CQ Cat | .30** | .38** | .46** | .50** | -- | ||||||||
| 6. Brooding | .41** | .56** | .66** | .50** | .38** | -- | |||||||
| 8. DIRI | .47** | .44** | .37** | .28** | .32** | .32** | -- | ||||||
| 9. Drinking to Cope | .27** | .26** | .34** | .31** | .28** | .40** | .13 | -- | |||||
| 10. EDI Bulimia | .28** | .37** | .24** | .21** | .24** | .33** | .23** | .30** | -- | ||||
| 11. NSSI | .11 | .15* | .17* | .05 | .11 | .10 | .22** | .05 | .07 | -- | |||
| 12. Suicide Attempts | .34** | .30** | .13 | .087 | .19* | .09 | .18* | .04 | .06 | .04 | -- | ||
| 13. HPD Symptoms | .29** | .15 | .20* | .10 | .21* | .16 | .21* | .17* | .14 | .11 | .06 | -- | |
| 14. NPD Symptoms | .32** | .29** | .26** | .16 | .11 | .13 | .27** | .13 | .20* | .13 | .14 | .46** | -- |
| MEAN | 14.4 | 12.9 | 37.9 | 12.7 | 9.9 | 11.0 | 12.5 | 10.7 | 15.1 | 5.7 | .23 | 9.5 | 11.3 |
| SD | 4.9 | 9.1 | 13.0 | 3.2 | 3.3 | 3.9 | 5.8 | 4.6 | 6.4 | 16.8 | .53 | 2.5 | 3.2 |
| Range | 9–27 | 0–41 | 19–72 | 7–20 | 4–18 | 5–20 | 4–26 | 5–20 | 7–39 | 0–105 | 0–2 | 8–21 | 9–24 |
Note. N=142.
p<.05;
p<0.01
Because SEM can be sensitive to non-normal distributions, all variables were tested for skewness and kurtosis. Both NSSI and number of previous suicide attempts were significantly positively skewed. Square root transformations were applied to both variables and resulted in significant improvement in skewness. No variables demonstrated significant kurtosis.
Gender1 and ethnic differences in all of the variables used in this study were examined using a Bonferroni corrected alpha of .004 to correct for Type 1 error. There were significant gender differences with regard to BPD symptoms, as expected. There were no significant ethnic differences on any of the variables.
Due to missing data for some of the variables (5 individuals were missing data at random; less than 4% of data was missing for the whole sample), full information maximum likelihood estimation (FIML; Anderson, 1957) was used; FIML provides less biased information than ad hoc procedures such as listwise deletion, pairwise deletion or imputation of means (Little & Rubin, 1987; Schafer, 1997).
Measurement Model
Kline (2005) recommends a 2-step approach to the evaluation of a structural equation model where the measurement model is examined first, then the structural model. Accordingly, confirmatory factor analysis was conducted with the latent variables in order to determine if the indicators fit the data well as two latent variables. The measurement model consisted of only the latent variables displayed in Figure 1, Emotional Cascades and Behavioral Dysregulation. The measurement model met criteria for excellent fit (χ2 = 27.8, df = 26, p = ns, CFI = .99, TLI = .99, RMSEA = .02). All factor loadings of the manifest indicators were significant (p<.05) and were between .24 and .78. There was also a significant positive correlation between the two latent variables (r=.90, p<.001). This correlation can be viewed as corroborative of the Emotional Cascade Model, which expects a high association between Emotional Cascades and behavioral dysregulation. Also, as noted below, this correlation is lower (though still substantial) in the structural equation model.
Structural Model
The hypothesized model met criteria for excellent fit (χ2 = 60.64, df = 54, p = ns, CFI = .99, TLI = .99, RMSEA = .03)2. All indicators significantly loaded onto their latent variables (p<.05). The path from Symptoms of BPD to Emotional Cascades was significant (β = .22, p<.05), as was the path from depression to Emotional Cascades (β =.50, p<.05). The path from Symptoms of BPD to Behavioral Dysregulation was significant (β = .32; p<.05), as was the path from depression to Behavioral Dysregulation (β = .32, p<.05). The path from Emotional Cascades to Behavioral Dysregulation was also significant (β =.49, p<.05). The reduction in magnitude of this path from the correlation in the measurement model is likely a result of accounting for variance attributed to depression and BPD. The paths from HPD and NPD symptoms to both Emotional Cascades and Behavioral Dysregulation were not significant. The correlations between the four exogenous observed variables, Symptoms of BPD, depression, HPD, and NPD, were all significant with the exception of the correlation between BDI score and features of HPD (r = .59 for symptoms of BPD and depression, r = .29 for symptoms of BPD and HPD symptoms, r=.32 for Symptoms of BPD and NPD symptoms, and r = .29 for symptoms of depression and NPD symptoms; p<.05 for all correlations).
Given the significant path from BPD symptoms to Behavioral Dysregulation, a partial mediation effect was indicated. This finding may have been a result of the overlap between the continuous measure of BPD symptoms and the Behavioral Dysregulation latent variable, as criteria four and five for BPD involve overt behavioral dysregulation (i.e. impulsivity and NSSI). Approximately 87% of those diagnosed with BPD endorsed at least one of these two symptoms. In order to ensure that this overlap was not overly influencing the model, the model was re-analyzed with criteria four and five removed from the BPD symptoms variable. This model continued to provide excellent fit to the data (χ2 = 59.32, df = 54, p = ns, CFI = .99, TLI = .99, RMSEA = .03), and a positive path was obtained between BPD symptoms and Behavioral Dysregulation (β = .36, p<.01) when the model was analyzed without including the Emotional Cascades mediator. More importantly, in the full model the Emotional Cascades latent variable fully mediated the relationship between BPD symptoms and Behavioral Dysregulation, as the path between these variables was not significant (β = .19, p=.16), when accounting for Emotional Cascades. These findings indicate that when removing the impulsivity and suicidal behavior criteria from the BPD symptoms measure, Emotional Cascades may fully mediate the relationship between the other BPD symptoms and dysregulated behaviors.
The standardized indirect effect of symptoms of BPD on Behavioral Dysregulation was β = .11, p<.05, in the original hypothesized model. This suggests that the effects of BPD symptoms on Behavioral Dysregulation may flow through Emotional Cascades. The PRODCLIN program was used to test the mediational impact of the Emotional Cascades between symptoms of BPD and Behavioral Dysregulation. This program was developed by MacKinnon and colleagues (2007) and tests mediational effects without some of the problems inherent in other methods of testing for mediation (e.g. inflated rates of Type I error, see MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002). In addition, the logic for this method is suited to testing for mediation in structural equation modeling (Bollen, 1987). PRODCLIN examines the product of the unstandardized path coefficients divided by the pooled standard error of the path coefficients (αβ/σαβ) and a confidence interval is generated. If the values between the upper and lower confidence limits include zero, this suggests the absence of a statistically significant mediation effect. The unstandardized path coefficients and standard errors of the path coefficients for the indirect effect of symptoms of BPD on Behavioral Dysregulation via Emotional Cascades were entered into PRODCLIN to yield lower and upper 95% confidence limits of .007 and .15. This suggests that the Emotional Cascades latent variable significantly mediated the association between symptoms of BPD and Behavioral Dysregulation, as predicted.
Because alternate models can also be generated and tested in SEM, two alternative models were also examined: 1) one in which the flow of the model consisted of Emotional Cascades as the source variable, which then led to symptoms of BPD with Behavioral Dysregulation as the mediator, and 2) another in which the flow of the model consisted of Emotional Cascades as the source variable, which then led to Behavioral Dysregulation, with BPD as the mediator. The AIC was used to distinguish differences in model fit, as these were not nested models. An analysis of the alternative models indicated that the first alternative provided similar fit to the hypothesized model (χ2 = 62.50, df = 56, p = ns, CFI = .98, TLI = .97, RMSEA = .03, AIC = 158), but did not fit better (hypothesized model AIC=161, AICdiff =3; a decrease in 10 AIC units is indicative of significantly better model fit [Burnham & Anderson, 2004]), while the second alternate model did not provide excellent fit (χ2 = 88.81, df = 57, p = ns, CFI = .92, TLI = .88, RMSEA = .06, AIC=183), and the hypothesized model provided significantly better fit (AICdiff =22). Because our hypothesized model and the first alternate model provided similar fit to the data, determining which of the two equivalent models is superior cannot be accomplished with these data. Identifying whether BPD causes Emotional Cascades or Emotional Cascades cause BPD is an important question for future work; it has been suggested that BPD and Emotional Cascades may have a bidirectional relationship (Selby & Joiner, in press). Longitudinal studies of these variables may help answer which variable has temporal precedence, Emotional Cascades or symptoms of BPD.
Rumination Induction Comparisons
In order to explore the effects of the rumination induction on those with BPD two groups were created. The first group consisted of the individuals who met full diagnostic criteria for BPD according to the SCID-II, and included 39 participants. The second group was created as a control group, and in order to be placed in this group the participants had to meet zero criteria for BPD so that the results of the analysis would not be confounded by individuals with subthreshold symptoms of BPD. This group consisted of 41 participants who were representative of the larger sample with regard to gender and ethnicity. The BPD and control groups were compared with regard to BDI total score using an ANOVA analysis, and the BPD group endorsed significantly more symptoms of depression than the control group (F(1, 76) = 64.4, p<.01), as would be expected.
The correlations between group status, BDI score, and affect totals are displayed in Table 2. Due to the high correlation between baseline negative affect and post-induction negative affect (r=.62, p<.001), all analyses were corrected using the Greenhouse-Geisser Epsilon Hat statistic. BDI total score was used as a covariate for all analyses in order to demonstrate that the effect of the rumination induction was not due solely to current symptoms of depression.
Table 2.
Correlations between Group, Control, and Affect Variables
| 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|
| 1. BPD Group | -- | |||||
| 2. BDI Total | .67* | -- | ||||
| 3. Baseline NA | .53* | .42* | -- | |||
| 4. Post-Induction NA | .47* | .36* | .63* | -- | ||
| 5. Baseline PA | −.28* | −.36* | −.04 | −.01 | -- | |
| 6. Post-Induction PA | −.28* | −.25* | −.06 | −.15 | .80* | -- |
Note. N=80. BPD Group: 1 = BPD Diagnosis, 0 = Control; BDI Total = Beck Depression Inventory Total; NA = Negative Affect; PA = Positive Affect.
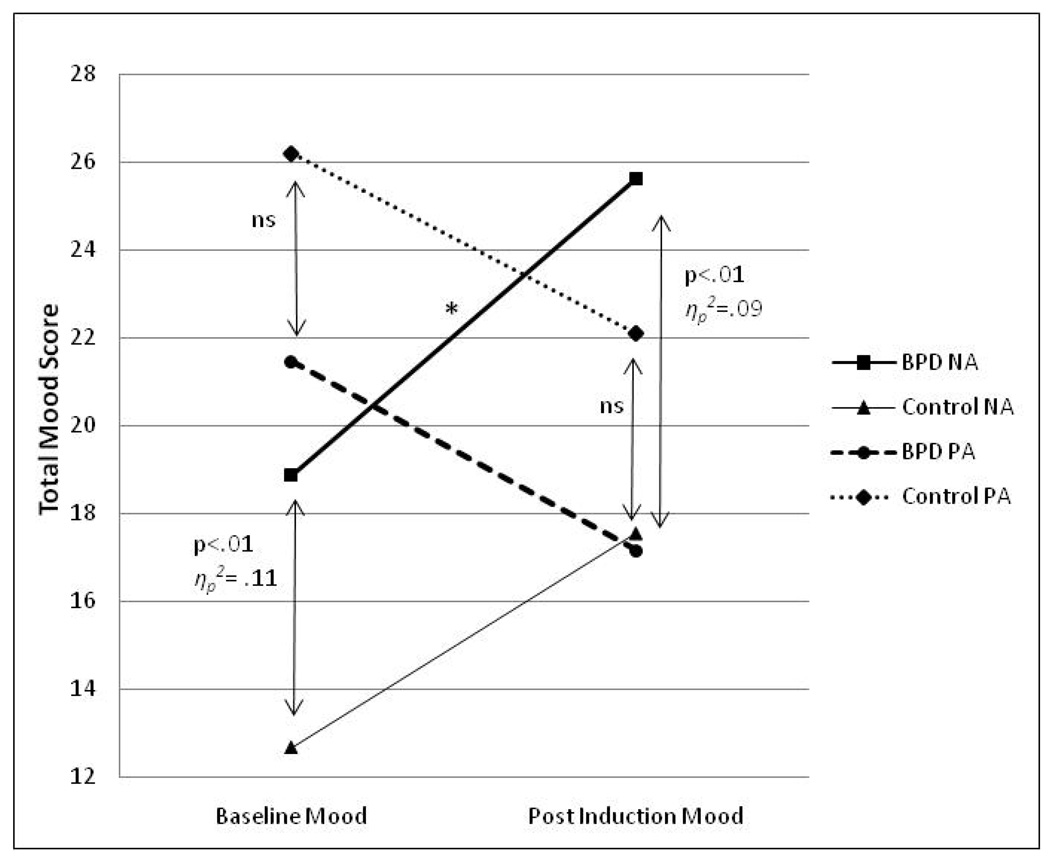
Group differences were then assessed using MANCOVA and repeated measures MANCOVA analyses, the results of which are displayed in Table 3 and graphed in Figure 2. The first hypothesis tested was that the BPD group would have significantly higher baseline negative affect, and significantly lower positive affect at baseline, even after controlling for current symptoms of depression. A MANCOVA analysis indicated that the BPD group had significantly higher baseline negative affect than the control group (F(1, 77) = 9.2, p<.01, ηp2= .11; note that an effect size of partial eta-squared ηp2=.06 is considered a medium effect, while an effect size of ηp2=.14 is considered a large effect according to Cohen, 1977). A significant effect for BDI score was not found on baseline negative affect. Contrary to our first hypothesis, there was not a significant difference in baseline positive affect between groups. Although no BPD effect was found on baseline positive affect, there was a significant effect of BDI score (F(1, 77) = 7.4, p<.01, β =−.31, ηp2=.09) such that higher BDI scores predicted lower levels of baseline positive affect.
Table 3.
Means and Standard Deviations by Group for Rumination Induction
| BPD Group | Control Group | F(df) | Sig. | ηp2 | |
|---|---|---|---|---|---|
| 1. Baseline NA | 18.89 (6.15) | 12.66 (4.25) | 9.2(1, 77) | .003* | .11 |
| 2. Post-Induction NA | 25.63 (7.46)^ | 17.54 (7.80) | 7.7(1, 77) | .007*+ | .09 |
| 3. Baseline PA | 21.46 (8.42) | 26.20 (7.88) | .02 (1, 77) | ns | -- |
| 4. Post-Induction PA | 17.15 (8.00)□ | 22.10 (8.92)□ | .22 (1, 77) | ns | -- |
| 5. BDI-II Total | 20.4 (10.08) | 6.48 (5.20) | 64.4(1, 77) | .001* | .44 |
indicates significant between-group effect, after controlling for BDI-II total.
indicates a significant group*time interaction such that the BPD group experienced greater reactivity of negative affect than the control group [F(1, 77)=5.42, p<.05, ηp2=.07]
indicates significant within-group increase in negative affect (F(1, 37)=12.6, p<.01, ηp2=.25)
indicates a significant within-group decrease of Post-Induction Positive Affect (F(1, 39) = 11.03, p<.01, ηp2=.22)
indicates a significant within-group decrease of Post-Induction Positive Affect (F(1, 37) = 13.7, p<.01, ηp2=.27)
Figure 2. Rumination Induction Procedure.
Note: N=80 (BPD group N = 39). BPD = borderline personality disorder; NA = negative affect; PA = positive affect; * = significant slope test indicating greater reactivity of the BPD group (ηp2=.07); ns = nonsignificant.
The next hypothesis tested was that following the rumination induction, the BPD group would demonstrate unique increases in negative affect from baseline, in addition to unique decreases in positive affect from baseline, when compared to the control group. A repeated measures MANCOVA analysis supported this hypothesis with regard to negative affect (F(1, 77) = 7.65, p<.01, ηp2=.09 – a medium effect)3, but not positive affect (F(1, 77) = .22, p = ns). The BPD group also demonstrated increased reactivity of negative affect, as indicated by a significant group*time interaction (F(1, 77) = 5.42, p<.05, ηp2= .07). There were no significant group differences in positive affect following the induction, and the group*time interaction for positive affect was not significant. There was a significant BDI*time interaction for negative affect (F(1,77) = 10.57, p<.05, ηp2= .12), such that those with higher BDI scores had greater reactivity than those with lower scores. This finding highlights the need for BDI as a covariate in the group comparisons.
In order to test the within-group effects of the rumination induction, the repeated measures MANCOVA analysis was examined according to group. The results of these analyses are listed in Table 3 and displayed in Figure 2. In the BPD group, negative affect was significantly higher following the rumination induction (F(1, 37) = 12.6, p<.01, ηp2=.25), even after controlling for BDI scores. There was not a significant interaction for BDI*time on post-induction negative affect in the BPD group, an interesting finding that lends evidence to the specificity of emotional cascades in BPD. For the BPD group, there was also a significant within-group decrease of positive affect (F(1, 37) = 13.7, p<.01, ηp2=.27). For the control group there was not a significant main effect of the rumination induction increasing negative affect, but there was a significant interaction between baseline negative affect and BDI total score that indicated significantly higher negative affect following the rumination induction (F(1, 39) = 21.7, p<.01, ηp2=.36). This finding replicates previous findings that rumination inductions increase negative affect in individuals experiencing symptoms of depression (Donaldson & Lam, 2004). For the control group, there was also a significant decrease in positive affect following the induction (F(1, 39) = 11.03, p<.01, ηp2=.22).
Discussion
This study provides evidence for the role of emotional cascades in BPD. First, using structural equation modeling, a model in which the relationship between BPD and a latent variable of dysregulated behavior was mediated by emotional cascades provided excellent fit to the data and demonstrated full mediation. The relationship between symptoms of BPD and emotional cascades was robust even when controlling for important covariates such as current symptoms of depression and symptoms of histrionic and narcissistic personality disorders. Second, BPD and control subjects engaged in an experimental rumination induction in which they were asked to think of a problem of personal relevance. The results of this induction provided some evidence for the emotional intensity of individuals with BPD in that they experienced higher levels of negative affect both before and after the procedure. The BPD group also showed evidence of greater reactivity to the induction than the control group because the slope of increases in negative affect was significantly larger than that of the control group (as indicated by the significant group*time interaction for negative affect). Importantly, these effects were found even after controlling for current symptoms of depression. Overall, the findings of this study suggest that rumination is an important cognitive factor that warrants further investigation in individuals with BPD.
BPD and Emotional Cascades
The findings of this study provide some supporting evidence for components of Linehan’s (1993) theory of BPD, especially with regard to the postulated sensitivity and intensity of negative affect in individuals with BPD. The study also provides some preliminary evidence for the Emotional Cascade Model in BPD (Selby & Joiner, in press; Selby et al., 2008). One important consideration with the results of the rumination induction is that the effects were observed by doing nothing more than asking the participants to think about a problem of personal relevance for a few minutes. This provides some evidence for the “hypersensitivity” of individuals with BPD, that even just asking individuals with this disorder to think about something upsetting resulted in increased negative affect relative to controls. This finding suggests that in BPD, emotion dysregulation is not only influenced by the experience of upsetting interpersonal interactions or other problems, but even just thinking about something upsetting (such as a bad memory or worry about the future) might be enough to trigger an emotional cascade.
A strength of this study that should be emphasized is that the results were obtained even when using rigorous covariates. For example, in the SEM model BPD symptoms predicted emotional cascades even after controlling for current symptoms of depression and symptoms of other Cluster B personality disorders (narcissistic and histrionic personality disorders). The inclusion of these stringent covariates is especially important when considering the effect size for reactivity of negative affect during the rumination induction. Although a medium effect size was obtained for the effects of the induction on the BPD group (ηp2=.07), this is taking into account symptoms of current depression, which had a medium-large effect size (ηp2=.14). This means that the BPD group experienced effects of the induction that were unique, and not an artifact of depressive symptoms. This provides some evidence for diagnostic specificity in that the experience of emotional cascades may be specific to BPD within Cluster B, although further research is needed to explore differences in emotional cascades between BPD and antisocial personality disorder and other personality disorders that may involve emotional and behavioral dysregulation (e.g., avoidant personality disorder).
One intriguing finding in this study was that the rumination induction did not have much influence on the positive affect of the BPD group. We hypothesized that the BPD group would have lower positive affect both before and after the rumination induction, and that we would also observe a steeper decline in slope of positive affect for the BPD group after the induction (as indicated by the group*time interaction for positive affect). These hypotheses were not supported, however, as there was not a unique decrease in positive affect for the BPD group after the induction. The failure to find a unique group difference in positive affect between groups indicates that affective lability in individuals with BPD may pertain more to negative affect, and that emotional cascades may specifically influence negative affect. This finding also suggests that reduction of negative affect may be a stronger motivation for behavioral dysregulation in these individuals than increasing positive affect. Positive affect resulting from the behavior may be an added reinforcer of the behavior (as in binge-eating or drug use), however.
Limitations and Future Directions
Despite the promising findings of this study, there are a few limitations that should be considered when interpreting the results. Perhaps the most important limitation to consider is that all of the participants in this study were college students, although the sample was enriched with individuals with BPD and subthreshold symptoms of BPD. Thus, although BPD symptoms were assessed with a structured clinical interview, participants diagnosed with BPD may actually be higher functioning than individuals diagnosed with BPD in clinical settings, reducing the generalizability of these results. This sample has an advantage, however, in that it was not confounded by treatment seeking. Another limitation with this study is that most measures were self-report measures, including self-reported affective experience during the rumination induction. Future research should pair psychophysiological methods (i.e. heart rate, skin conductance) with self-reported affect during a rumination induction to determine if similar results obtained in this study are found with the physiological measures. Another limitation to this study was that it did not explore all forms of behavioral dysregulation that may present in BPD, such as aggressive behaviors (i.e. fights, threatening, throwing things) or other impulsive behaviors (i.e. impulsive shopping, illicit drug use). Thus, the mediational effects of emotional cascades may not hold for other forms of dysregulated behavior.
One final, important limitation to this study was that the rumination induction did not control for differences in what people ruminated about. Individuals with BPD may have ruminated on more intensely negative situations (i.e. past trauma) than those in the control group, who might have had less distressing situations to ruminate about (e.g., a bad test score). This difference in rumination content may be responsible for the reactivity of negative affect in those with BPD. Yet, even if these situations are more painful to think about than a bad test score, we would argue that even simply thinking about that past trauma resulted in increased reactivity of negative affect. Recalling past traumatic memories could be an important trigger for emotional cascades in BPD. Future studies should explore whether thought content serves as a mediator or moderator of emotional cascades. This could be accomplished through the use of two rumination inductions with BPD participants randomly assigned to each condition: 1) a standardized rumination induction where all participants are instructed to think about the same standardized situation, and 2) a more personalized rumination induction, as in this study. Assessing and controlling for thought content during a rumination induction may also help determine if emotional cascades are driving behavioral dysregulation, or if it is primarily the recall of upsetting memories.
Although the findings of this study look promising, future studies should attempt to replicate these results, especially in a sample of BPD individuals in a clinical setting. Additional comparisons should also be made to individuals with clinically diagnosed major depressive disorder in order to provide additional evidence for the specificity of emotional cascades to BPD. Another possible direction for future studies may be to explore the rumination induction paired with a subsequent behavioral proxy (e.g., pain tolerance test), or to assess urges to engage in a behavior, which may test the postulate of the Emotional Cascade Model that emotional cascades are causing the behavioral dysregulation. Future studies may also benefit from exploring emotional cascades and behavioral dysregulation using Ecological Momentary Assessment (EMA; Stone & Shiffman, 1994). Using this methodology, individuals with BPD could be assessed in their daily environment in order to determine if rumination (and potentially emotional cascades) is present during experiences of negative affect and behavioral dysregulation, as well as using cross-lagged analyses to determine if rumination at one daily signal predicts behavioral dysregulation at a subsequent signal. Finally, this study did not explore how long the effects of the rumination induction lasted. Subsequent measurements of negative affect following the rumination induction may have provided support for the slow return to emotional baseline suggested by Linehan (1993).
Clinical Implications
Perhaps the most important clinical application of these findings is that they provide a potential target for therapy and mechanism of change: reduction of emotional cascades. In doing this, a reduction in behavioral dysregulation would most likely be observed as well. Attention control training, or increasing the ability to control one’s attention and shift it away from emotion and onto more productive pursuits, may be the active ingredient in therapies for BPD that have empirical support. The common ground of attention control can be found in the mindfulness and distress tolerance exercises of DBT (Linehan, 1993), enhancement in the patient’s ability to accurately assess his or her moment-to-moment state of mind and affect in mentalization-based treatment (MBT; Bateman & Fonagy, 2008), and improvement of the patient’s reflective functioning through clarification and confrontation of the patient’s in-session relational affects in transference-focused psychotherapy (TFP; Clarkin, Yeomans, & Kernberg, 2006). All of these therapies may teach the patient to disengage from the attention-consuming cycle of an emotional cascade, and instead focus on distraction from negative affect or thinking about the problem in constructive, emotion-detached manner. Although more research is needed to determine if these techniques reduce emotional cascades, mindfulness in particular has been linked to reducing rumination (Broderick, 2005). Another clinical application is that psychoeducation about rumination/emotional cascades and how they may influence dysregulated behaviors may help BPD patients understand their condition and its consequences. Teaching patients to engage in mind-occupying activities (such as Sudoku or other engaging puzzles) when experiencing emotional distress may also help them acquire alternative activities for distraction, which may be most helpful during the initial stages of an emotional cascade.
Acknowledgements
This study was funded by National Institute of Mental Health grant F31MH081396 to E.A. Selby, under mentorship of T.E. Joiner. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/abn.
No significant gender differences were found on the rumination measures, an unexpected finding given that previous studies have identified gender differences in rumination (Nolen-Hoeksema & Jackson, 2001). Because of the significant gender differences in BPD symptoms, we examined the hypothesized model with only female participants included. This model was found to have almost exactly the same fit and all paths were essentially the same, indicating that gender differences did not greatly influence the model.
When this model was tested a negative error variance was obtained for the residual indicator for Behavioral Dysregulation. This was likely a function of the high correlation (r=.90) between the two latent variables. Another possibility was that this residual was near zero, a problem which is minor enough that AMOS was still able to conduct the structural analysis. The recommended way to remedy a negative error variance is to remove the residual indicator and reanalyze the model (Dillon, Kumar, & Mulani, 1987). After running a second analysis where the residual predictor for behavioral dysregulation was removed, the model was empirically identified (i.e. there were no negative error variances) and model fit was the same, all paths and factor loadings remained significant, and the direction and magnitude of all relationships remained the same. Following this second analysis, the empirical identification of the model remains intact and the fit indices and regression weights generated by the model remain valid.
In order to test the specificity of the effects of the rumination induction on BPD further, the analysis was rerun including the HPD and NPD variables along with the BDI as a covariate. The results of the original analysis were essentially unchanged, and neither HPD nor NPD significantly predict increases in negative affect following the rumination induction. This finding provides additional evidence for the specificity of the effects of the BPD diagnosis on the increases in negative affect following the rumination induction.
REFERENCES
- Abela JRZ, Payne AVL, Moussaly N. Cognitive vulnerability to depression in individuals with borderline personality disorder. Journal of Personality Disorders. 2003;17(4):319–329. doi: 10.1521/pedi.17.4.319.23968. [DOI] [PubMed] [Google Scholar]
- Abramowitz JS, Tolin DF, Street GP. Paradoxical effects of thought suppression: A meta-analysis of controlled studies. Clinical Psychology Review. 2001;21:683–703. doi: 10.1016/s0272-7358(00)00057-x. [DOI] [PubMed] [Google Scholar]
- Allen C. Helping with deliberate self-harm: Some practical guidelines. Journal of Mental Health. 1995;4:243–250. [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders, fourth edition. Washington, D.C: Author; 1994. [Google Scholar]
- Arbuckle JL, Wothke W. AMOS 4.0. Chicago, IL: SPSS Inc; 1999. [Google Scholar]
- Armey MF, Crowther JH. A comparison of linear versus non-linear models of aversive self-awareness, dissociation, and non-suicidal self-injury among young adults. Journal of Consulting and Clinical Psychology. 2008;76(1):9–14. doi: 10.1037/0022-006X.76.1.9. [DOI] [PubMed] [Google Scholar]
- Bateman A, Fonagy P. 8-year follow-up of patients treated for borderline personality disorder: Mentalization-based treatment versus treatment as usual. American Journal of Psychiatry. 2008;165:631–638. doi: 10.1176/appi.ajp.2007.07040636. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1998;8:77–100. [Google Scholar]
- Beck AT, Steer RA, Ranieri WF. Scale for suicide ideation: psychometric properties of a self-report version. Journal of Clinical Psychology. 1988;44:499–505. doi: 10.1002/1097-4679(198807)44:4<499::aid-jclp2270440404>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Total, direct, and indirect effects in structural equation models. Sociological Methodology. 1987;17:37–69. [Google Scholar]
- Broderick PC. Mindfulness and coping with dysphoric mood: Contrasts with rumination and distraction. Cognitive Therapy and Research. 2005;29(5):501–510. [Google Scholar]
- Brown MZ, Comtois KA, Linehan MM. Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder. Journal of Abnormal Psychology. 2002;111:198–202. doi: 10.1037//0021-843x.111.1.198. [DOI] [PubMed] [Google Scholar]
- Burnham KP, Anderson DR. Multimodel inference: Understanding AIC and BIC in model selection. Sociological Methods and Research. 2004;33(2):261–304. [Google Scholar]
- Bushman BJ, Baumeister RF, Phillips CM. Do people aggress to improve their mood? Catharsis beliefs, affect regulation opportunity, and aggressive responding. Journal of Personality and Social Psychology. 2001;81(1):17–32. [PubMed] [Google Scholar]
- Bushman BJ, Bonacci AM, Pederson WC, Vasquez EA, Miller N. Chewing on it can chew you up: Effects of rumination on triggered displaced aggression. Journal of Personality and Social Psychology. 2005;88(6):969–983. doi: 10.1037/0022-3514.88.6.969. [DOI] [PubMed] [Google Scholar]
- Carver CS, Blaney PH, Scheier MF. Focus of attention, chronic expectancy, and responses to a feared stimulus. Journal of Personality and Social Psychology. 1979;37:1186–1195. doi: 10.1037//0022-3514.37.7.1186. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy. 2006;44:371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Clarkin JF, Yeomans F, Kernberg OF. Psychotherapy of borderline personality: Focusing on object relations. Washington, DC: American Psychiatric Press; 2006. [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. New York, NY: Academic Press; 1977. [Google Scholar]
- Cooper ML, Russell M, Skinner JB, Windle M. Development and Validation of a Three-Dimensional Measure of Drinking Motives. Psychological Assessment: Journal of Consulting and Clinical Psychology. 1992;4:123–132. [Google Scholar]
- Dillon WR, Kumar A, Mulani N. Offending estimates in covariance structure analysis: Comments on the causes of and solutions to Heywood cases. Psychological Bulletin. 1987;101(1):126–135. [Google Scholar]
- Donaldson C, Lam D. Rumination, mood, and social-problem solving in major depression. Psychological Medicine. 2004;34:1309–1318. doi: 10.1017/s0033291704001904. [DOI] [PubMed] [Google Scholar]
- Fink EL, Smith AR, Gordon KH, Holm-Denoma JM, Joiner TE., Jr Psychological correlates of purging disorder as compared with other eating disorders: An exploratory investigation. International Journal of Eating Disorders. doi: 10.1002/eat.20556. (in press) [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW, Benjamin L. Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) Washington, DC: American Psychiatric Publishing; 1997. [Google Scholar]
- Garfnefski N, Kraaij V, Spinhoven P. Negative life events, cognitive emotion regulation, and emotional problems. Personality and Individual Differences. 2001;30:1311–1327. [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and Validation of a Multidimensional Eating Disorder Inventory for Anorexia Nervosa and Bulimia. International Journal of Eating Disorders. 1983;2:15–19. [Google Scholar]
- Gunderson JG. Borderline personality disorder. Washington, DC: American Psychiatric Press; 1984. [Google Scholar]
- Heatherton TF, Baumeister RF. Binge eating as escape from self-awareness. Psychological Bulletin. 1991;110(1):86–108. doi: 10.1037/0033-2909.110.1.86. [DOI] [PubMed] [Google Scholar]
- Hilt LM, Cha CB, Nolen-Hoeksema S. Nonsuicidal self-injury in young adolescent girls: moderators of the distress-function relationship. Journal of Consulting and Clinical Psychology. 2008;76(1):63–71. doi: 10.1037/0022-006X.76.1.63. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- James LM, Taylor J. Impulsivity and negative emotionality associated with substance use problems and Cluster B personality in college students. Addictive Behaviors. 2007;32:714–727. doi: 10.1016/j.addbeh.2006.06.012. [DOI] [PubMed] [Google Scholar]
- Joiner TE, Alfano MS, Metalsky GI. When depression breeds contempt. Journal of Abnormal Psychology. 1992;101:165–173. doi: 10.1037//0021-843x.101.1.165. [DOI] [PubMed] [Google Scholar]
- Just N, Alloy LB. The response styles theory of depression: Tests and an extension of the theory. Journal of Abnormal Psychology. 1997;106:221–229. doi: 10.1037//0021-843x.106.2.221. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. 2nd Ed. New York: Guildford Press; 2005. [Google Scholar]
- Klonsky ED. The functions of deliberate self-injury: A review of the evidence. Clinical Psychology Review. 2007;27:226–239. doi: 10.1016/j.cpr.2006.08.002. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. What is emptiness? Clarifying the 7th criterion for borderline personality disorder. Journal of Personality Disorders. 2008;22(4):418–426. doi: 10.1521/pedi.2008.22.4.418. [DOI] [PubMed] [Google Scholar]
- Koenigsberg HW, Harvey PD, Mitropoulou V, Schmeidler J, New AS, Goodman M, Silverman J, Serby M, Schopick F, Siever LJ. Characterizing affective instability in borderline personality disorder. American Journal of Psychiatry. 2002;159:784–788. doi: 10.1176/appi.ajp.159.5.784. [DOI] [PubMed] [Google Scholar]
- Leible TL, Snell WE., Jr Borderline personality disorder and multiple aspects of emotional intelligence. Personality and Individual Differences. 2004;37:393–404. [Google Scholar]
- Linehan MM. Cognitive-Behavioral Treatment for Borderline Personality Disorder. New York: Guilford Press; 1993. [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- Lloyd E, Keeley ML, Hope T. Self-mutilation in a sample of community adolescents: Descriptive characteristics and provisional prevalence rates. Poster presented at the Society of Behavioral Medicine; New Orleans. March 17.1997. [Google Scholar]
- Lyubomirsky S, Nolen-Hoeksema S. Effects of self focused rumination on negative thinking and interpersonal problem solving. Journal of Personality and Social Psychology. 1995;69:176–190. doi: 10.1037//0022-3514.69.1.176. [DOI] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behavior Research Methods. 2007;39(3):384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marino MF, Zanarini MC. Relationship between EDNOS and its subtypes and borderline personality disorder. International Journal of Eating Disorders. 2001;29:349–353. doi: 10.1002/eat.1029. [DOI] [PubMed] [Google Scholar]
- Moberly NJ, Watkins ER. Ruminative self-focus and negative affect: An experience sampling study. Journal of Abnormal Psychology. 2008;117(2):314–323. doi: 10.1037/0021-843X.117.2.314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S. Responses to depression and their effects on the duration of depressive episodes. Journal of Abnormal Psychology. 1991;100(4):555–561. doi: 10.1037//0021-843x.100.4.569. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Harrell ZA. Rumination, depression, and alcohol use: Tests of gender differences. Journal of Cognitive Psychotherapy. 2002;16:391–405. [Google Scholar]
- Nolen-Hoeksema S, Jackson B. Mediators in the gender difference in rumination. Psychology of Women Quarterly. 2001;25:37–47. [Google Scholar]
- Nolen-Hoeksema S, Morrow J. A prospective study of depression and posttraumatic stress symptoms after a natural disaster: the 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology. 1991;61(1):115–121. doi: 10.1037//0022-3514.61.1.115. [DOI] [PubMed] [Google Scholar]
- Nolen-Hoeksema S, Stice E, Wade E, Bohon C. Reciprocal relations between rumination and bulimic, substance abuse, and depressive symptoms in female adolescents. Journal of Abnormal Psychology. 2007;116(1):198–207. doi: 10.1037/0021-843X.116.1.198. [DOI] [PubMed] [Google Scholar]
- Rothschild L, Cleland C, Haslam N, Zimmerman M. A Taxometric study of borderline personality disorder. Journal of Abnormal Psychology. 2003;112(4):657–666. doi: 10.1037/0021-843X.112.4.657. [DOI] [PubMed] [Google Scholar]
- Salovey P. Mood-induced self-focused attention. Journal of Personality and Social Psychology. 1992;62(4):699–707. doi: 10.1037//0022-3514.62.4.699. [DOI] [PubMed] [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. London: Chapman & Hall; 1997. [Google Scholar]
- Selby EA, Anestis MD, Joiner TE. Understanding the relationship between emotional and behavioral dysregulation: Emotional Cascades. Behaviour Research and Therapy. 2008;46:593–611. doi: 10.1016/j.brat.2008.02.002. [DOI] [PubMed] [Google Scholar]
- Selby EA, Joiner TE., Jr Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychology. doi: 10.1037/a0015687. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith JM, Grandin LD, Alloy LB, Abramson LY. Cognitive vulnerability to depression and Axis II personality dysfunction. Cognitive Therapy and Research. 2006;30:609–621. [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75(4):629–638. doi: 10.1037/0022-006X.75.4.629. [DOI] [PubMed] [Google Scholar]
- Stone A, Shiffman S. Ecological Momentary Assessment (EMA) in behavioral medicine. Annals of Behavioral Medicine. 1994;16:199–202. [Google Scholar]
- Sukhodolsky DG, Golub A, Cromwell EN. Development and validation of the anger rumination scale. Personality and Individual Differences. 2001;31:689–700. [Google Scholar]
- Suyemoto KL. The functions of self-mutilation. Clinical Psychology Review. 1998;18(5):531–554. doi: 10.1016/s0272-7358(97)00105-0. [DOI] [PubMed] [Google Scholar]
- Thomsen DK. The association between rumination and negative affect: A review. Cognition and Emotion. 2006;20(8):1216–1235. [Google Scholar]
- Watkins ER. Constructive and unconstructive repetitive thought. Psychological Bulletin. 2008;134(2):163–206. doi: 10.1037/0033-2909.134.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watson D, Tellegen A, Clark L. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Widiger TA, Trull TJ. Plate tectonics in the classification of personality disorder: Shifting to a dimensional model. American Psychologist. 2007;62(2):71–83. doi: 10.1037/0003-066X.62.2.71. [DOI] [PubMed] [Google Scholar]
- Yen S, Zlotnick C, Costello E. Affect regulation in women with borderline personality disorder traits. Journal of Nervous and Mental Disease. 2002;190:693–696. doi: 10.1097/00005053-200210000-00006. [DOI] [PubMed] [Google Scholar]