Abstract
Background:
Fatty degeneration of the rotator cuff muscles may have detrimental effects on both anatomical and functional outcomes following shoulder surgery. The purpose of this study was to investigate the relationship between tear geometry and muscle fatty degeneration in shoulders with a deficient rotator cuff.
Methods:
Ultrasonograms of both shoulders of 262 patients were reviewed to assess the type of rotator cuff tear and fatty degeneration in the supraspinatus and infraspinatus muscles. The 251 shoulders with a full-thickness tear underwent further evaluation for tear size and location. The relationship of tear size and location to fatty degeneration of the supraspinatus and infraspinatus muscles was investigated with use of statistical comparisons and regression models.
Results:
Fatty degeneration was found almost exclusively in shoulders with a full-thickness rotator cuff tear. Of the 251 shoulders with a full-thickness tear, eighty-seven (34.7%) had fatty degeneration in either the supraspinatus or infraspinatus, or both. Eighty-two (32.7%) of the 251 full-thickness tears had a distance of 0 mm between the biceps tendon and anterior margin of the tear. Ninety percent of the full-thickness tears with fatty degeneration in both muscles had a distance of 0 mm posterior from the biceps, whereas only 9% of those without fatty degeneration had a distance of 0 mm. Tears with fatty degeneration had significantly greater width and length than those without fatty degeneration (p < 0.0001). Tears with fatty degeneration had a significantly shorter distance posterior from the biceps than those without fatty degeneration (p < 0.0001). The distance posterior from the biceps was found to be the most important predictor for supraspinatus fatty degeneration, whereas tear width and length were found to be the most important predictors for infraspinatus fatty degeneration.
Conclusions:
Fatty degeneration of the rotator cuff muscles is closely associated with tear size and location. The finding of this study suggests that the integrity of the anterior supraspinatus tendon is important to the development of fatty degeneration. Patients with full-thickness tears that extend through this area may benefit from earlier surgical intervention if fatty degeneration has not already occurred. Additionally, the findings suggest the importance of secure fixation and healing of the anterior aspect of the supraspinatus with surgical repair.
Fatty degeneration of the rotator cuff muscles is a well-known sequela of rotator cuff tears, and it has various detrimental effects on the anatomical and functional outcomes of shoulders postoperatively. Fatty degeneration is associated with a high retear rate and poor functional outcome following rotator cuff repair compared with shoulders without fatty degeneration1-4. These muscle changes are known to progress with time and after failure of a tendon repair1,2,5-8, and they do not resolve even after a successful cuff repair1,2,5. However, not all rotator cuff tears lead to fatty degeneration. It has been theorized that fatty degeneration is associated with multiple factors such as the chronicity of the tear, degree of tear retraction, suprascapular nerve retraction, or patient age; however, these theories have not been proved clinically. To our knowledge, no study has clinically investigated the relationship between tear geometry (e.g., tear size and location) and the development of fatty degeneration in the rotator cuff muscles. Knowledge of cuff tear characteristics that are associated with the development of fatty degeneration may be helpful to orthopaedic surgeons in counseling patients with a chronic degenerative cuff tear on the timing of surgical compared with nonsurgical treatment.
Ultrasonography has become a well-established primary diagnostic modality for shoulder abnormalities, especially rotator cuff lesions. Previous studies9-11 have shown that retraction (i.e., length) and anteroposterior extension (i.e., width) of rotator cuff tears can be measured with ultrasonography with an accuracy comparable with that of magnetic resonance imaging. Recent studies have demonstrated that the accuracy of ultrasonography for the detection of fatty degeneration of the rotator cuff muscles was moderate (72%)12 to excellent (100%)13, with magnetic resonance imaging used as the gold standard.
We conducted an observational study to investigate the relationship of tear size and location to the occurrence of fatty degeneration in the rotator cuff muscles. To study this relationship, we examined shoulder ultrasonograms from a large group of patients previously enrolled for a prospective and longitudinal study examining degeneration of the rotator cuff over time.
Materials and Methods
Study Subjects
Ultrasonograms of both shoulders in 262 patients were reviewed for the study after the approval of the institutional review board. This study represents a cross-sectional analysis of a prospective database accumulated as part of an ongoing study funded by the National Institutes of Health, in which standardized assessment of shoulder function and shoulder ultrasonography for cuff tear geometry and fatty degeneration of the muscles were performed annually on patients who had a symptomatic rotator cuff tear in one shoulder and no symptoms in the other shoulder. The symptomatic shoulder received either surgery or conservative management for the cuff tear. By ultrasonography, the asymptomatic shoulder was found to have either an asymptomatic rotator cuff tear or an intact rotator cuff. Inclusion criteria for the study group were patients who (1) presented for shoulder ultrasonography at our institution to investigate unilateral shoulder pain, (2) had a diagnosis of either a full-thickness rotator cuff tear or a partial-thickness cuff tear of >5 mm on the asymptomatic, contralateral shoulder, (3) were verified as having had no symptoms in the study shoulder at the initiation of the study, (4) had no history of trauma to the asymptomatic shoulder and remained free of injury during the duration of the study, and (5) agreed to participate in the study. Exclusion criteria were (1) any substantial pain in the asymptomatic shoulder, (2) sustained use of narcotic pain medication or anti-inflammatory medication, (3) a traumatic episode to the asymptomatic shoulder, (4) inflammatory arthropathy, (5) a history of seeking medical attention for other problems in the asymptomatic shoulder (such as instability, arthritis, or trauma), (6) use of the upper extremity for weight-bearing, and (7) a very small, partial-thickness tear (<5 mm) in the asymptomatic shoulder. Substantial pain was defined as (1) any pain of >3 points on a 10-point visual analog pain scale that lasted for more than six weeks, (2) any pain considered to be greater than that normally experienced as part of daily living, (3) any pain requiring the use of medications such as narcotics or nonsteroidal anti-inflammatories, or (4) any pain that prompted a physician visit for evaluation. Ultrasonograms were included in the study when all of the following criteria were met: (1) a complete assessment for fatty degeneration was performed on both the supraspinatus and infraspinatus muscles, (2) no previous rotator cuff surgery had been performed in the shoulder, (3) the width and length of the cuff tear were measured and recorded in the report when there was a rotator cuff tear in the shoulder, (4) images demonstrating tear width and length were available for review, (5) either the biceps tendon or bicipital groove was clearly visible in the transverse view, and (6) the biceps tendon was located in the groove without subluxation or dislocation when the bicipital groove was not visible.
Shoulder Ultrasonography
All ultrasonography examinations were performed in real time with use of a Siemens Elegra scanner (Siemens Medical Systems, Issaquah, Washington) and a variable high-frequency linear-array transducer (7.5 to 9 MHz) by one of three radiologists who had more than ten years of experience in musculoskeletal ultrasonography. Tissue harmonic imaging was used for all patients. All of the patients had standardized ultrasonography of both shoulders as previously described11,14. The muscles of the supraspinatus and infraspinatus were evaluated with the forearm of the patient supinated and placed in a relaxed position on the ipsilateral thigh. Each muscle was evaluated in two planes: longitudinal and transverse. The transducer was placed parallel to the long axis of each muscle for the longitudinal examination and perpendicular to the long axis of each muscle for the transverse examination. In both planes, the entire bulk of the muscle was assessed by moving the transducer in a medial to lateral orientation while in the transverse plane and in a superior to inferior orientation while in the longitudinal plane. Care was taken to differentiate between muscle and perimuscular fat by performing graded compression during live scanning. To evaluate fatty degeneration, the echogenicity and echotexture of each muscle was examined with use of a 3-point scale as previously described by Strobel et al.12. The echogenicity of the supraspinatus and infraspinatus was determined in comparison with the echogenicity of the overlying trapezius and deltoid, respectively; the echogenicity was graded as normal when the supraspinatus or infraspinatus was isoechoic to the overlying muscle, as mild to moderate when there was slightly increased echogenicity compared with the overlying muscle, and as severe when there was markedly increased echogenicity compared with the overlying muscle. The echotexture was determined on the basis of the visibility of the central tendon and the normal muscle pennate pattern; the echotexture was graded as normal when there was a clearly visible central tendon and identifiable muscle pennate pattern, as mild to moderate when there was mild to moderate blurring of the central tendon and muscle pennate pattern, and as severe when there was no discernable central tendon or muscle pennate pattern. For the purpose of this study (i.e., to investigate the gross relationship between the presence of fatty degeneration and tear characteristics), the 3-point scale was later collapsed into a binary scale, in which only the presence (from a grade of mild to severe on the 3-point scale) or the absence (a grade of normal) of fatty degeneration was reported (Figs. 1 and 2).
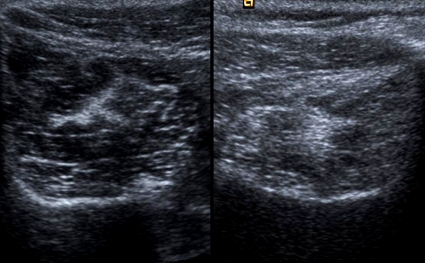
Fig. 1.
Ultrasonographic appearance of the supraspinatus muscle. The muscle without fatty degeneration (left) shows a clear central tendon and hypoechoic surrounding muscle. The muscle with fatty degeneration (right) shows increased echogenicity at the surrounding muscle with a blurred central tendon.
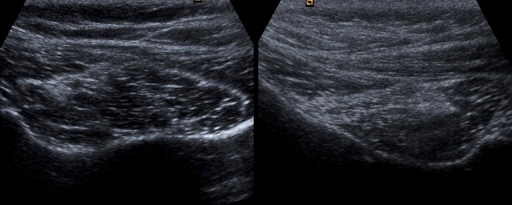
Fig. 2.
Ultrasonographic appearance of the infraspinatus muscle. The muscle without fatty degeneration (left) shows a clear central tendon and hypoechoic surrounding muscle. The muscle with fatty degeneration (right) shows increased echogenicity at the surrounding muscle with a blurred central tendon.
Evaluation of Tear Size and Location with Ultrasonography
The maximum anteroposterior diameter of a tear was measured in transverse views (perpendicular to the long axis of the cuff) and designated as the width of the tear (Fig. 3). When the width of a tear was too large to measure with one straight line over the convex humeral head, more than one straight line was drawn, and the sum of the length of the lines was calculated to obtain the tear width. The maximum degree of retraction (i.e., the mediolateral diameter of a tear) was measured in longitudinal views (parallel to the long axis of the cuff) and designated as the length of the tear (Fig. 4). Tear length was measured from the lateral edge of the rotator cuff footprint on the greater tuberosity. All tears were measured with a digital measuring tool in real time during the ultrasonography examination. When a tear was too large to measure in either of the two views, it was given a fixed value of 50 mm for that measurement and designated as a massive tear. The images that showed the maximum anteroposterior diameter and maximum mediolateral diameter of each tear were saved in the picture archiving and communication system for measurement of tear location. Tear location was assessed by measuring the anteroposterior distance from the posterior margin of the biceps tendon to the anterior extent of a tear in transverse views with use of software for viewing digital radiography (Fig. 5). This measurement was designated as the distance of the tear posterior from the biceps. Distance posterior from the biceps was measured by a radiologist (N.D.) and an orthopaedic surgeon (H.M.K.), who were both blinded to the muscle status and medical history of the patient. The interobserver and intraobserver reliability of the two investigators was obtained for the first thirty measurements. Then, the two investigators determined the distance posterior from the biceps by concurrence.
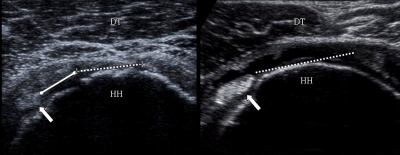
Fig. 3.
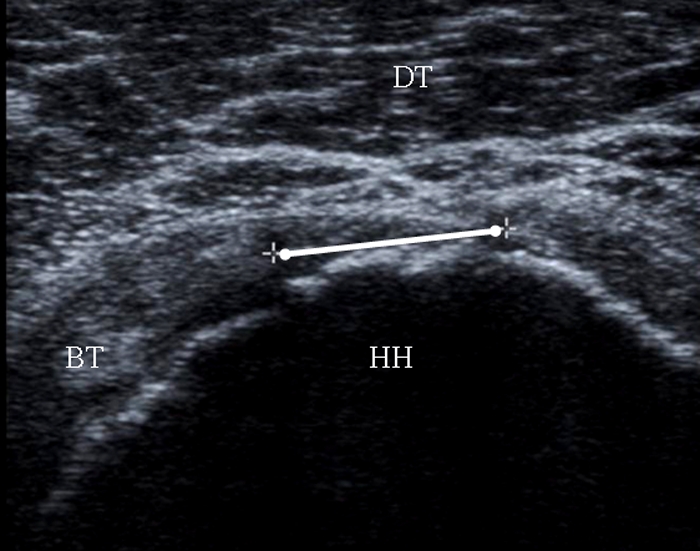
Measurement of the width of the rotator cuff tear in the transverse plane. The width (white line) was defined as the distance between the anterior and posterior tendon stumps. BT = biceps tendon, HH = humeral head, and DT = deltoid muscle.
Fig. 4.
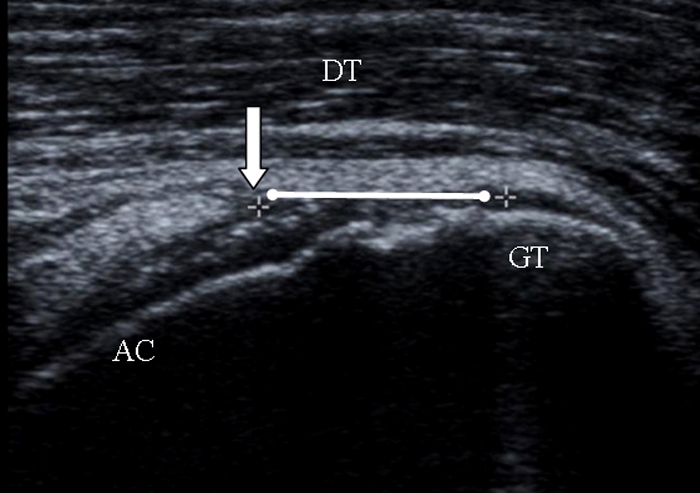
Measurement of the length of the rotator cuff tear in the longitudinal plane. The length (white line) was defined as the distance between the retracted proximal tendon stump (arrow) and the greater tuberosity (GT). AC = articular surface of the humeral head, and DT = deltoid muscle.
Fig. 5.
Measurement of the distance from the biceps tendon in the transverse plane. A tear (dashed white line) whose anterior margin has a measurable distance (solid white line) from the biceps (block arrow) is shown on the left. A fluid-filled full-thickness tear (dashed white line) that extends up to the biceps tendon (block arrow) does not have a measurable distance (right panel). HH = humeral head, and DT = deltoid muscle.
Statistical Methods
Both shoulders of each patient were treated as independent shoulders instead of being treated as a pair. Statistical analyses were performed only on the data obtained from the shoulders with a full-thickness tear. Tear geometry variables (e.g., length, width, and distance) of the shoulders with fatty degeneration were compared with those of the shoulders without fatty degeneration with use of logistic regression. Univariate (unadjusted) odds ratios and corresponding 95% confidence intervals were obtained. Multiple stepwise logistic regression models were utilized to determine the tear characteristic variable(s) most associated with fatty degeneration of the muscles. Adjusted odds ratios and corresponding 95% confidence intervals were obtained for all variables in the model. A p value of <0.05 was considered significant. Data are reported as the mean and the standard deviation.
Source of Funding
This project was funded by a grant from the National Institutes of Health (R01-AR051026-01A1) as part of an ongoing prospective cohort study with a specific aim of describing the natural history of rotator cuff tears.
Results
Study Subjects and Tear Types
Ultrasonograms of 413 shoulders from 237 patients were found to meet all of the inclusion criteria and were included in the study. The mean age of the patients was 64.2 ± 10.4 years. There were 144 male and ninety-three female patients. There were 251 shoulders with a full-thickness rotator cuff tear, ninety-seven with a partial-thickness rotator cuff tear, and sixty-five with an intact rotator cuff. Since fatty degeneration was found almost exclusively in the shoulders with a full-thickness tear, the 251 shoulders with a full-thickness tear were grouped separately for further data collection and analysis. These 251 shoulders were derived from 177 patients (seventy-four patients with bilateral studies and 103 with unilateral studies), and there were 133 symptomatic shoulders and 118 asymptomatic shoulders. The mean age of the patients with full-thickness tear(s) was 64.9 ± 10.1 years, and there were 110 male and sixty-seven female patients.
Tear Size and Location
Statistics for tear size and location are reported only for the 251 full-thickness tears. The mean length of the tears was 18.1 ± 11.2 mm. The mean width was 16.2 ± 10.2 mm. The mean width of the asymptomatic tears was 13.9 ± 10.0 mm, and that of the symptomatic tears was 21.8 ± 13.6 mm (p < 0.0001). There were seventy-seven small tears (a width of <10 mm), 125 medium tears (10 mm ≤ width < 30 mm), thirty-four large tears (30 mm ≤ width < 50 mm), and fifteen massive tears (a width of ≥50 mm).
The intraobserver and interobserver reliability (intraclass correlation coefficient) for the measurement of distance of the anterior extent of tears posterior from the biceps tendon was 0.990 and 0.984, respectively. The mean distance from the biceps tendon was 7.8 ± 5.9 mm. Eighty-two tears (32.7%) had a distance of 0 mm (i.e., the tears extended immediately posterior to the biceps tendon), eighty-eight tears (35.1%) had a distance of >0 mm and ≤10 mm, and eighty-one tears (32.3%) had a distance of >10 mm. The eighty-two tears with a distance of 0 mm included one small tear (1% of seventy-seven small tears), thirty-six medium tears (29% of 125 medium tears), thirty large tears (88% of thirty-four large tears), and all fifteen massive tears (100%) (Fig. 6). The eighty-two tears with a distance of 0 mm were found in twenty-three (20%) of the 118 asymptomatic tears and in fifty-nine (44%) of the 133 symptomatic tears (p < 0.0001).
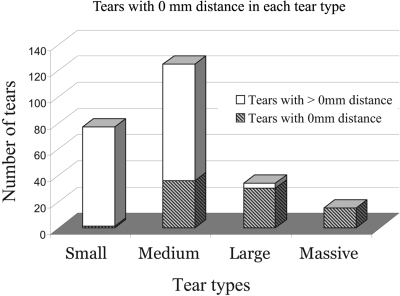
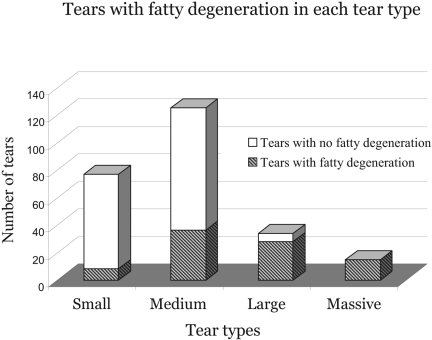
Fig. 6.
The proportion of tears with a 0-mm distance in each tear type increased with increasing size of the tears. Tears with a 0-mm distance were found in one (1%) of seventy-seven small tears, in thirty-six (29%) of 125 medium tears, in thirty (88%) of thirty-four large tears, and in all fifteen massive tears (100%).
Fatty Degeneration of the Rotator Cuff Muscles
Of 413 shoulders, eighty-nine (21.5%) were found to have fatty degeneration in either the supraspinatus or infraspinatus, or both. Fatty degeneration was found exclusively in the shoulders with a full-thickness tear except for two shoulders with a partial-thickness tear. None of the shoulders with an intact rotator cuff had fatty degeneration. Only the 251 shoulders with a full-thickness tear were included for the statistical analysis. Of the 251 shoulders, eighty-seven (34.7%) were found to have fatty degeneration in at least one of the two muscles; twenty-six (10.4%) had fatty degeneration in one muscle and sixty-one (24.3%) had fatty degeneration in both muscles. No fatty degeneration was found in either muscle in 164 shoulders (65.3%). Supraspinatus fatty degeneration was found in seventy-four shoulders (29.5%), and infraspinatus fatty degeneration was found in seventy-four shoulders (29.5%). Fatty degeneration of at least one muscle was found in eight (10%) of the seventy-seven small tears, in thirty-six (29%) of the 125 medium tears, in twenty-eight (82%) of the thirty-four large tears, and in all of the fifteen massive tears (100%) (Fig. 7). Fatty degeneration of at least one muscle was found in twenty-three (19%) of the 118 asymptomatic tears and in sixty-four (48%) of the 133 symptomatic tears (p < 0.0001).
Fig. 7.
The proportion of tears with fatty degeneration in each tear type increased with increasing size of the tears. Tears with fatty degeneration of at least one muscle were found in eight (10%) of the seventy-seven small tears, in thirty-six (29%) of the 125 medium tears, in twenty-eight (82%) of the thirty-four large tears, and in all fifteen massive tears (100%).
Comparisons of Tear Size and Location Between Shoulders with and without Fatty Degeneration
In a comparison of the shoulders with and without supraspinatus fatty degeneration and of the shoulders with and without infraspinatus fatty degeneration, both the length and the width of the tears were significantly greater in the shoulders with fatty degeneration for each muscle (p < 0.0001) (Table I). The odds of having fatty degeneration in the supraspinatus and infraspinatus doubled with every 5-mm increase in either tear length or width. Distance posterior from the biceps was significantly less in the shoulders with supraspinatus fatty degeneration than in those without supraspinatus fatty degeneration (p < 0.0001) (Table II). Eighty-eight percent (sixty-five) of the seventy-four shoulders with supraspinatus fatty degeneration had a distance of 0 mm posterior from the biceps, whereas only 10% (seventeen) of the 177 shoulders without supraspinatus fatty degeneration had a distance of 0 mm. The odds of having supraspinatus fatty degeneration decreased dramatically, by 96%, as the distance posterior from the biceps increased from 0 mm to >0 mm. Similarly, the distance posterior from the biceps was significantly less in the shoulders with infraspinatus fatty degeneration than in the shoulders without infraspinatus fatty degeneration (p < 0.0001) (Table II). Seventy-seven percent (fifty-seven) of the seventy-four shoulders with infraspinatus fatty degeneration had a distance of 0 mm, whereas 14% (twenty-five) of the 177 shoulders without infraspinatus fatty degeneration had a distance of 0 mm. The odds of having infraspinatus fatty degeneration decreased by 84% as the distance posterior from the biceps increased from 0 mm to >0 mm. Tears with isolated supraspinatus fatty degeneration had a significantly shorter distance posterior from the biceps than did tears with isolated infraspinatus fatty degeneration (1.9 ± 3.8 mm and 8.8 ± 6.4 mm, respectively; p = 0.002).
TABLE I.
Tear Geometry of Shoulders with Fatty Degeneration and Those without Fatty Degeneration in the Supraspinatus and Infraspinatus Muscles
| Degeneration |
Odds Ratio (95% Confidence Interval)‡ | |||
| Absent* (N = 177) | Present* (N = 74) | P Value† | ||
| Supraspinatus fatty degeneration | ||||
| Tear length | 14.4 ± 8.3 | 33.2 ± 13.3 | <0.0001 | 2.01 (1.69, 2.39) |
| Tear width | 12.8 ± 7.5 | 30.8 ± 13.5 | <0.0001 | 2.03 (1.70, 2.42) |
| Distance from biceps | 9.9 ± 4.9 | 1.1 ± 3.2 | Bad fit | Bad fit |
| Infraspinatus fatty degeneration | ||||
| Tear length | 14.5 ± 8.1 | 32.8 ± 14.0 | <0.0001 | 1.93 (1.64, 2.27) |
| Tear width | 12.6 ± 6.8 | 31.3 ± 13.8 | <0.0001 | 2.17 (1.79, 2.64) |
| Distance from biceps | 9.4 ± 5.1 | 2.3 ± 4.9 | Bad fit | Bad fit |
The values are given, in millimeters, as the mean and the standard deviation.
P values were derived from univariate logistic regression analysis.
Odds ratios reflect the increased odds of having fatty degeneration for 5-mm increase in each tear geometry variable. Bad fit = Because of the poor distributional properties and poor goodness-of-fit statistics, the distance data could not be incorporated into the regression model.
TABLE II.
Distance from the Biceps of the Shoulders with Fatty Degeneration and Those without Fatty Degeneration in the Supraspinatus and Infraspinatus
| Degeneration |
Odds Ratio (95% Confidence Interval)‡ | |||
| Absent* (N = 177) | Present* (N = 74) | P Value† | ||
| Supraspinatus fatty degeneration | <0.0001 | 0.04 (0.02, 0.09) | ||
| 0 mm | 17 (10) | 65 (88) | ||
| >0 to 10 mm | 82 (46) | 6 (8) | ||
| >10 mm | 78 (44) | 3 (4) | ||
| Infraspinatus fatty degeneration | <0.0001 | 0.16 (0.10, 0.27) | ||
| 0 mm | 25 (14) | 57 (77) | ||
| >0 to 10 mm | 80 (45) | 8 (11) | ||
| >10 mm | 72 (41) | 9 (12) | ||
The values are given as the number of shoulders with the percentage in parentheses.
P value was derived from univariate logistic regression analysis.
Odds ratio reflects the increased odds of having fatty degeneration in the infraspinatus as distance increases from 0 mm to >0 mm.
In comparisons between the shoulders with fatty degeneration in both muscles, those with fatty degeneration in one muscle, and those with no fatty degeneration, there were significant gradual increases of tear length and width with an increasing number of the muscles with fatty degeneration (p < 0.0001) (Table III). The distance posterior from the biceps showed a significant gradual decrease with an increasing number of muscles with fatty degeneration (p < 0.0001) (Table III). Ninety percent (fifty-five) of the sixty-one shoulders with fatty degeneration in both muscles had a distance of 0 mm, whereas 46% (twelve) of the twenty-six with fatty degeneration in one muscle and 9% (fifteen) of the 164 with no fatty degeneration had a distance of 0 mm.
TABLE III.
Tear Length, Width, and Distance from the Biceps in Shoulders with Various Degrees of Fatty Degeneration
| Fatty Degeneration in Supraspinatus and/or Infraspinatus* |
||||
| Tear geometry | Neither (N = 164) | One (N = 26) | Both (N = 61) | P Value† |
| Tear length‡ | 13.8 ± 7.3 | 23.2 ± 12.8 | 35.1 ± 13.0 | <0.0001 |
| Tear width‡ | 12.2 ± 6.7 | 19.1 ± 9.7 | 33.6 ± 13.0 | <0.0001 |
| Distance from biceps‡ | 10.0 ± 4.7 | 5.4 ± 6.2 | 0.9 ± 3.1 | Bad fit |
| Distance category | <0.0001 | |||
| 0 mm§ | 15 (9) | 12 (46) | 55 (90) | |
| >0 to 10 mm§ | 77 (47) | 8 (31) | 3 (5) | |
| >10 mm§ | 72 (44) | 6 (23) | 3 (5) | |
Neither = shoulders with fatty degeneration in neither the supraspinatus nor infraspinatus, one = shoulders with fatty degeneration in either the supraspinatus or infraspinatus, and both = shoulders with fatty degeneration in both the supraspinatus and infraspinatus.
P values were derived from univariate logistic regression analysis. Bad fit = Because of the poor distributional properties and poor goodness-of-fit statistics, the distance data could not be incorporated into the regression model.
The values are given in millimeters as the mean and the standard deviation.
The values are given as the number of shoulders with the percentage in parentheses.
Association of Tear Size and Location with Fatty Degeneration of the Rotator Cuff Muscles
There was a high correlation (r = 0.88) between tear length and width, which precluded simultaneous use of these two variables in a regression model. Instead, a separate logistic regression model was used for each variable. There was a substantial correlation (r = 0.70) between tear width and distance posterior from the biceps. The distribution of the distance data was significantly different from the normal distribution (p < 0.0001) because there were a large number of tears with a distance of 0 mm (33%; eighty-two of 251 tears). Because of the severe non-normal distribution, there was inadequate variability to model this variable as a continuous measure, and it was not possible to perform accurate statistical tests on these data when they were treated as a continuous variable. Therefore, the distance data were categorized into three similarly sized categories instead of being used as a continuous variable. The three categories were (1) 0 mm of distance, (2) a distance of >0 mm and ≤10 mm, and (3) a distance of >10 mm. With stepwise multiple logistic regression models, the distance posterior from the biceps was found to be more important than tear length and width in predicting the presence of supraspinatus fatty degeneration (coefficient of determination R2 = 0.43, p < 0.0001) (Table IV). On the other hand, both length and width were found to be more important than distance posterior from the biceps in predicting the presence of infraspinatus fatty degeneration (R2 = 0.34 and 0.38, respectively; p < 0.0001 for both length and width). With respect to predicting the presence of fatty degeneration in both muscles, length and width were found to be more important (R2 = 0.40 and 0.43, respectively; p < 0.0001 for both length and width) than the distance posterior from the biceps. All of the above results were confirmed with repeated statistical analyses with the massive tears excluded.
TABLE IV.
Association of Tear Geometry Variables with Fatty Degeneration in the Supraspinatus and Infraspinatus
| Variable | Adjusted Odds Ratio (95% Confidence Interval)* | Cumulative R2 (Selection Order)† | P Value |
| Supraspinatus fatty degeneration | |||
| Distance category‡ | 0.11 (0.05, 0.24) | 0.43 (1) | <0.0001 |
| Tear length | 1.40 (1.15, 1.71) | 0.46 (2) | 0.0007 |
| Distance category‡ | 0.10 (0.04, 0.23) | 0.43 (1) | <0.0001 |
| Tear width | 1.35 (1.10, 1.66) | 0.45 (2) | 0.004 |
| Infraspinatus fatty degeneration | |||
| Distance category‡ | 0.50 (0.28, 0.89) | 0.36 (2) | 0.02 |
| Tear length | 1.68 (1.38, 2.03) | 0.34 (1) | <0.0001 |
| Distance category‡ | NS | ||
| Tear width | 2.17 (1.79, 2.64) | 0.38 (1) | <0.0001 |
| Fatty degeneration in both supraspinatus and infraspinatus | |||
| Distance category‡ | 0.27 (0.15, 0.48) | 0.45 (2) | <0.0001 |
| Tear length | 1.56 (1.32, 1.84) | 0.40 (1) | <0.0001 |
| Distance category‡ | 0.30 (0.17, 0.55) | 0.47 (2) | <0.0001 |
| Tear width | 1.72 (1.42, 2.08) | 0.43 (1) | <0.0001 |
Adjusted odds ratios reflect the increased odds of having fatty degeneration, after adjusting for other variables in the model. For continuous variables, adjusted odds ratios were expressed in units of 5 mm. For distance category, adjusted odds ratios were expressed in units of one category. NS = not significant.
Generalized coefficient of determination of the fitted model. The independent variable that is the first in selection order has the strongest association with the dependent variable. Note that the second variable contributes little more information to the model in addition to that provided by the first variable.
Measured on a 0-2 ordinal scale, where 0 = 0 mm distance, 1 = >0 to 10 mm distance, and 2 = >10 mm distance.
Discussion
We investigated the relationship of fatty degeneration in the rotator cuff muscles to the size and location of tendon tears using ultrasonography. Our results indicate that the development of fatty degeneration in the supraspinatus and infraspinatus is strongly associated with both tear size and location. This was supported by the following findings: (1) fatty degeneration was found almost exclusively in the shoulders with a full-thickness tear, whereas shoulders with a partial-thickness tear or an intact rotator cuff did not have fatty degeneration; (2) both tear length and width were significantly greater in shoulders with fatty degeneration than in those without fatty degeneration; (3) both tear length and width gradually increased as the number of fat-infiltrated muscles increased; (4) the distance between the biceps tendon and the anterior margin of a full-thickness tear was significantly smaller in shoulders with fatty degeneration than in those without fatty degeneration; and (5) the distance posterior from the biceps tendon gradually decreased as the number of fat-infiltrated muscles increased.
Our results indicate that the possibility of developing fatty degeneration in the supraspinatus and infraspinatus increases as a tear enlarges in length or width. Since there is a high positive correlation between length and width (r = 0.88), changes in one variable essentially indicate the same directional and proportional changes in the other. This implies that the degree of tear retraction is one of the key factors that are related to the development of fatty degeneration. A small retraction may not usually be associated with the development of fatty degeneration until it progresses to a certain extent. Although the duration of a tear is also an important factor, it was not investigated in the present study because it is nearly impossible to determine when a chronic rotator cuff tear started. Animal studies6-8 have demonstrated that fatty degeneration of the muscle progresses with time after rotator cuff tendon detachment; however, the relationship between fatty degeneration and tendon tear geometry has not been studied clinically. Nakagaki et al.15 reported in their cadaver study that the severity of fatty degeneration in the supraspinatus was associated with tear length. To our knowledge, the present study is the first to investigate the relationship between fatty degeneration and tendon tear geometry in patients.
Our results demonstrate that the probability of fatty degeneration developing in the supraspinatus and infraspinatus increases when a tear involves the more anterior aspect of the supraspinatus tendon. Because there is a substantial correlation (r = 0.70) between size (i.e., width and length) and distance from the biceps tendon, it may not be surprising that a larger tear has a shorter distance from the biceps and, consequently, has a higher probability of developing fatty degeneration than a smaller tear. However, it is notable that 88% of the shoulders with supraspinatus fatty degeneration had a distance of 0 mm from the biceps, whereas only 10% of the shoulders without supraspinatus fatty degeneration had a distance of 0 mm. The odds of supraspinatus fatty degeneration developing decreased dramatically, by 96%, as the distance from the biceps increased from 0 mm to >0 mm. Distance from the biceps was found to be more highly correlated than tear length and width to the presence of fatty degeneration in the supraspinatus. All of these findings suggest that the integrity of the most anterior part of the supraspinatus tendon insertion may be important in preventing the development of fatty degeneration in the supraspinatus muscle.
While the mechanism of these findings is not known, two possible explanations may be considered. First, the most anterior part of the supraspinatus tendon insertion is known as the location where the anterior end of the so-called rotator cable inserts16-18. It has been postulated that the rotator cable stress-shields the rotator crescent, a site where most rotator cuff tears initiate16,18. The rotator cable allows the supraspinatus to transmit its muscle force to the humerus, even in the presence of a tear, by means of its distributed load along the span of the suspension bridge configuration16,19-21. Disruption of one of the two rotator cable insertions may cause a torn tendon end to retract farther and, with time, the muscle may shorten and develop fatty degeneration. In the present study, not only large to massive tears but also many small to medium-sized tears (68%; twenty-five of thirty-seven) were found to have fatty degeneration when they involved the most anterior part of the supraspinatus tendon insertion. These findings are in good concordance with the rotator cable concept. Additionally, two-thirds (169) of the 251 shoulders with full-thickness tears in this study did not have involvement of the most anterior part of the supraspinatus, and only 11% (nineteen) of the 169 shoulders developed fatty degeneration in the supraspinatus. Another possible explanation for our findings is the unique anatomy of the supraspinatus insertion that was recently reported by Mochizuki et al.22. According to that study, the most anterior 1.3 mm of the rotator cuff footprint is composed of purely the supraspinatus. From this point, the next 11.3 mm of the tendon insertion consists of the supraspinatus medially and the infraspinatus laterally. The anterior several millimeters of the supraspinatus is a strong tendinous structure and is thought to perform the main functional role of the tendon by carrying the preponderance of the load23. Disruption of this anterior tendinous structure, especially the most anterior few millimeters, may be associated with more serious changes in the mechanical and biological environment of the muscle than disruption of the posterior portion of the cuff insertion.
We also found that fatty degeneration in the infraspinatus was more closely associated with tear length and width than distance posterior from the biceps tendon. This finding implies that, in contrast to the supraspinatus, fatty degeneration of the infraspinatus is affected by the size and the extent of retraction rather than the location of the tear. Similarly, fatty degeneration of both the supraspinatus and infraspinatus was found to be more closely associated with tear length and width than distance posterior from the biceps tendon.
In the present study, symptomatic tears were found to be significantly larger than asymptomatic tears, which is consistent with the finding in the study of Yamaguchi et al.24. It was also found that the proportion of tears with a distance of 0 mm posterior from the biceps and the proportion of tears with fatty degeneration were both significantly greater for symptomatic tears than for asymptomatic tears.
It is not clear why some shoulders with a tear involving the most anterior part of the supraspinatus insertion did not have supraspinatus fatty degeneration. Likewise, it is not clear either why some shoulders with a tear sparing this portion of the tendon did develop fatty degeneration. It is presumed that there may be a role for tear duration or other unknown factors. Considering the size of large and massive tears included in the present study, there were likely many tears that involved the posterior aspect of the rotator cable, which may have contributed to the development of infraspinatus fatty degeneration. Because there is no distinct landmark in the posterior rotator cuff region like the biceps tendon in the anterior cuff region, an accurate examination was not possible in the posterior cuff region.
The present study has some important, potential limitations. First, ultrasound is a less commonly used imaging modality to assess fatty degeneration than is magnetic resonance imaging or computed tomography. The accuracy of ultrasound in the detection of fatty degeneration of the rotator cuff muscles has not been validated in our institution yet. In addition, the data for interobserver and intraobserver reliability of the three radiologists who performed ultrasonography are not available at this point. A few studies have investigated the accuracy of ultrasound for the detection of fatty degeneration of the rotator cuff muscles. Strobel et al.12 reported only a moderate accuracy of ultrasound (72% to 85%), with magnetic resonance imaging used as the gold standard. They used static ultrasound images for muscle evaluation, which may be the reason for finding only moderate accuracy. Khoury et al.13 evaluated muscles with real-time, dynamic ultrasound scanning, which is the same technique used in our study, and reported an excellent accuracy of ultrasound (98%) in detecting fatty degeneration of the supraspinatus with magnetic resonance imaging used as the gold standard. All ultrasonography in the present study was performed by one of the three radiologists who had more than ten years of experience in musculoskeletal ultrasonography and, in particular, extensive experience in shoulder sonography. Additionally, our institution has a long track record for accuracy with this modality11,14,25,26. Therefore, the accuracy of our institution was expected to be similar to that of Khoury et al.13. Second, although ultrasound has been validated in our institution to be a highly accurate tool for rotator cuff tear geometry11,14,25,26, it should be noted that we did not reassess interobserver and intraobserver reliability for this specific study. Third, only cross-sectional data were analyzed in this study, and no consideration has been given to the chronological aspect of a tear. The duration of a tear is another important factor related to fatty degeneration development; however, it was not investigated in the present study. Fourth, the data derived from both shoulders in patients with bilateral involvement may have introduced bias to the analysis. Data from seventy-four patients with bilateral involvement of the shoulders and from 103 patients with unilateral involvement were used. Each shoulder was treated as an independent shoulder. An ancillary analysis was performed to address this concern by randomly selecting a single shoulder from each patient and repeating the same statistical tests. The results of this analysis confirmed our original conclusions. Fifth, 21% of the initial 524 shoulders were excluded from the study according to the inclusion criteria, which may have introduced additional bias to the data analysis. Sixth, the same radiologist evaluated the rotator cuff tear dimensions and rotator cuff muscles of the subjects at the same time, which also may have introduced bias.
Although multiple comparisons were performed, the levels of significance of statistical tests were not adjusted in the present study for a few reasons. First, this is an observational study testing multiple small hypotheses that are independent of each other rather than a study testing a global null hypothesis. Second, the statistical tests used in the present study had been planned before the study initiation. The p values were small when the tests were significant in the present study; therefore, the result of each test would not have been affected even if an adjustment had been performed.
In summary, we showed that the development of fatty degeneration in the rotator cuff muscles is strongly associated with tear size and location. We found that the disruption of the most anterior part of the supraspinatus tendon is most closely associated with the development of fatty degeneration in the supraspinatus muscle, whereas tear size is most closely associated with the development of fatty degeneration in the infraspinatus. The finding of this study suggests that the integrity of the anterior aspect of the supraspinatus tendon is important to the development of fatty degeneration. Patients with a full-thickness tear that extends through this area may benefit from earlier surgical intervention if fatty degeneration has not already occurred. Additionally, the findings suggest the importance of secure fixation and healing of the anterior part of the supraspinatus with surgical repair.
Footnotes
Disclosure: One or more of the authors received, in any one year, outside funding or grants in excess of $10,000 from the National Institutes of Health (R01-AR051026-01A1). One or more of the authors or members of his or her immediate family received, in any one year, payments or benefits in excess of $10,000 or a commitment or agreement to provide such benefits from commercial entities (Zimmer and Tornier).
References
- 1.Gladstone JN, Bishop JY, Lo IK, Flatow EL. Fatty infiltration and atrophy of the rotator cuff do not improve after rotator cuff repair and correlate with poor functional outcome. Am J Sports Med. 2007;35:719-28 [DOI] [PubMed] [Google Scholar]
- 2.Goutallier D, Postel JM, Bernageau J, Lavau L, Voisin MC. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin Orthop Relat Res. 1994;304:78-83 [PubMed] [Google Scholar]
- 3.Goutallier D, Postel JM, Gleyze P, Leguilloux P, Van Driessche S. Influence of cuff muscle fatty degeneration on anatomic and functional outcomes after simple suture of full-thickness tears. J Shoulder Elbow Surg. 2003;12:550-4 [DOI] [PubMed] [Google Scholar]
- 4.Jost B, Pfirrmann CW, Gerber C. Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg Am. 2000;82:304-14 [DOI] [PubMed] [Google Scholar]
- 5.Gerber C, Fuchs B, Hodler J. The results of repair of massive tears of the rotator cuff. J Bone Joint Surg Am. 2000;82:505-15 [DOI] [PubMed] [Google Scholar]
- 6.Gerber C, Meyer DC, Schneeberger AG, Hoppeler H, von Rechenberg B. Effect of tendon release and delayed repair on the structure of the muscles of the rotator cuff: an experimental study in sheep. J Bone Joint Surg Am. 2004;86:1973-82 [DOI] [PubMed] [Google Scholar]
- 7.Rubino LJ, Stills HF, Jr, Sprott DC, Crosby LA. Fatty infiltration of the torn rotator cuff worsens over time in a rabbit model. Arthroscopy. 2007;23:717-22 [DOI] [PubMed] [Google Scholar]
- 8.Safran O, Derwin KA, Powell K, Iannotti JP. Changes in rotator cuff muscle volume, fat content, and passive mechanics after chronic detachment in a canine model. J Bone Joint Surg Am. 2005;87:2662-70 [DOI] [PubMed] [Google Scholar]
- 9.Bryant L, Shnier R, Bryant C, Murrell GA. A comparison of clinical estimation, ultrasonography, magnetic resonance imaging, and arthroscopy in determining the size of rotator cuff tears. J Shoulder Elbow Surg. 2002;11:219-24 [DOI] [PubMed] [Google Scholar]
- 10.Farin PU, Kaukanen E, Jaroma H, Väätäinen U, Miettinen H, Soimakallio S. Site and size of rotator-cuff tear. Findings at ultrasound, double-contrast arthrography, and computed tomography arthrography with surgical correlation. Invest Radiol. 1996;31:387-94 [DOI] [PubMed] [Google Scholar]
- 11.Teefey SA, Rubin DA, Middleton WD, Hildebolt CF, Leibold RA, Yamaguchi K. Detection and quantification of rotator cuff tears. Comparison of ultrasonographic, magnetic resonance imaging, and arthroscopic findings in seventy-one consecutive cases. J Bone Joint Surg Am. 2004;86:708-16 [PubMed] [Google Scholar]
- 12.Strobel K, Hodler J, Meyer DC, Pfirrmann CW, Pirkl C, Zanetti M. Fatty atrophy of supraspinatus and infraspinatus muscles: accuracy of US. Radiology. 2005;237:584-9 [DOI] [PubMed] [Google Scholar]
- 13.Khoury V, Cardinal E, Brassard P. Atrophy and fatty infiltration of the supraspinatus muscle: sonography versus MRI. AJR Am J Roentgenol. 2008;190:1105-11 [DOI] [PubMed] [Google Scholar]
- 14.Teefey SA, Hasan SA, Middleton WD, Patel M, Wright RW, Yamaguchi K. Ultrasonography of the rotator cuff. A comparison of ultrasonographic and arthroscopic findings in one hundred consecutive cases. J Bone Joint Surg Am. 2000;82:498-504 [PubMed] [Google Scholar]
- 15.Nakagaki K, Ozaki J, Tomita Y, Tamai S. Fatty degeneration in the supraspinatus muscle after rotator cuff tear. J Shoulder Elbow Surg. 1996;5:194-200 [DOI] [PubMed] [Google Scholar]
- 16.Burkhart SS, Esch JC, Jolson RS. The rotator crescent and rotator cable: an anatomic description of the shoulder's “suspension bridge”. Arthroscopy. 1993;9:611-6 Erratum in: Arthroscopy. 1994;10:239 [DOI] [PubMed] [Google Scholar]
- 17.Clark JM, Harryman DT., 2nd Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713-25 [PubMed] [Google Scholar]
- 18.Lo IK, Burkhart SS. Current concepts in arthroscopic rotator cuff repair. Am J Sports Med. 2003;31:308-24 [DOI] [PubMed] [Google Scholar]
- 19.Burkhart SS. Fluoroscopic comparison of kinematic patterns in massive rotator cuff tears. A suspension bridge model. Clin Orthop Relat Res. 1992;284:144-52 [PubMed] [Google Scholar]
- 20.Burkhart SS. Reconciling the paradox of rotator cuff repair versus debridement: a unified biomechanical rationale for the treatment of rotator cuff tears. Arthroscopy. 1994;10:4-19 [DOI] [PubMed] [Google Scholar]
- 21.Burkhart SS. Shoulder arthroscopy. New concepts. Clin Sports Med. 1996;15:635-53 [PubMed] [Google Scholar]
- 22.Mochizuki T, Sugaya H, Uomizu M, Maeda K, Matsuki K, Sekiya I, Muneta T, Akita K. Humeral insertion of the supraspinatus and infraspinatus. New anatomical findings regarding the footprint of the rotator cuff. J Bone Joint Surg Am. 2008;90:962-9 [DOI] [PubMed] [Google Scholar]
- 23.Itoi E, Berglund LJ, Grabowski JJ, Schultz FM, Growney ES, Morrey BF, An KN. Tensile properties of the supraspinatus tendon. J Orthop Res. 1995;13:578-84 [DOI] [PubMed] [Google Scholar]
- 24.Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA. The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Joint Surg Am. 2006;88:1699-704 [DOI] [PubMed] [Google Scholar]
- 25.Middleton WD, Teefey SA, Yamaguchi K. Sonography of the rotator cuff: analysis of interobserver variability. AJR Am J Roentgenol. 2004;183:1465-8 [DOI] [PubMed] [Google Scholar]
- 26.Teefey SA, Middleton WD, Payne WT, Yamaguchi K. Detection and measurement of rotator cuff tears with sonography: analysis of diagnostic errors. AJR Am J Roentgenol. 2005;184:1768-73 [DOI] [PubMed] [Google Scholar]