Abstract
Purpose
This pilot study investigated the acceptability of whole grain and legume foods in youths with type 1 diabetes and determined demographic and behavioral factors associated with their acceptability.
Methods
Youths with type 1 diabetes (7.0 to 16.9 years) were recruited during a diabetes camp and completed self-report measures of food acceptability, eating behaviors, and demographics. An overall acceptability score for whole grains and for legumes was calculated as the sum of foods in each category rated as either “tried and liked” or “not tried and willing to try.” Correlations of whole grain and legume acceptability with demographic characteristics were examined.
Results
One hundred twenty-eight youths participated (70% females, mean age 11.6 ± 2.3 years). Whole grain foods with the highest acceptability were corn bread (85% tried/liked and 11% willing to try) and whole wheat bread (72% tried/liked and 3% willing to try). Total whole grain acceptability was negatively associated with days per week of fast food consumption (r =−0.21; P < .02) and living in an urban environment (r = −0.24; P < .01). Chili with beans (66% tried/liked and 8% willing to try) and baked beans (57% tried/liked and 19% willing to try) were the legume-containing foods with the highest acceptability. There were no significant associations between demographic factors and total legume acceptability.
Conclusions
These findings demonstrate the variability in acceptability among whole grains and legumes in youths with type 1 diabetes and the importance of addressing acceptability when counseling youths or designing nutrition interventions to improve consumption of these foods.
The current dietary recommendation is that half of all carbohydrates consumed from grain products come from whole grains1; however, actual whole grain intake in children in the United States falls well below the recommended amounts.2,3 The 1994–1996 United States Department of Agriculture (USDA) Continuing Survey of Food Intake demonstrated low consumption of whole grains in children ages 2 to 18 years. Based on these findings, one of the goals of Healthy People 2010 is to “increase the proportion of persons aged 2 years and older who consume at least 6 daily servings of grain products, with at least 3 being whole grains.”4 The recommendation for legume intake is not as well defined. The USDA recommends choosing legumes as a main dish or part of a meal often1; however, little is known about actual legume intake in children.
Whole grain and legume consumption is associated with decreased risk of a variety of chronic diseases. In adults, whole grain intake has been positively associated with enhanced insulin sensitivity,5 better weight control,6,7 reduced risk of stroke,8 prevention of coronary heart disease,9,10 and reduced risk of certain types of cancers.11 Although fewer studies have addressed the health benefits of legumes, intake has been inversely associated with cancer,12,13 cardiovascular disease,14 and type 2 diabetes.15 Unfortunately, much less is known about the effects of whole grain and legume consumption on health outcomes in children. However, 1 study conducted with 5th to 8th graders demonstrated that whole grain intake was associated with greater insulin sensitivity and lower BMI.16
Although adequate whole grain and legume intake is recommended for all individuals, it may have particular benefit for those with type 1 diabetes. As cardiovascular disease is the most common complication in persons with diabetes17 the cardioprotective aspects of whole grains and legumes may be particularly relevant. In addition, while the current American Diabetes Association’s dietary recommendations emphasize the amount rather than the source of carbohydrates,18 it is increasingly recognized that blood glucose response to the ingestion of carbohydrate-containing foods may vary substantially.19 The presence of dietary fiber, along with the lesser degree of processing often occurring in whole grains and legumes, may decrease the glycemic response to these foods.20,21 Thus, in addition to the cardiovascular and other health benefits observed in the general population, whole grain and legume consumption may improve glycemic control in people with diabetes, which is associated with both increased quality of life and reductions in long-term complications.22,23 Unfortunately, youths with type 1 diabetes consume well below the recommended amount of whole grains. The SEARCH for Diabetes study reported that no youth with type 1 diabetes met whole grain intake recommendations.24
While there is a need for efforts to improve whole grain and legume consumption in youths, little is known about the relative acceptability of whole grain and legume containing foods. Because these foods are not currently a regular part of most youths’ diets, acceptability data are critical for informing diabetes educators about which foods to recommend to their patients and for designing programs to increase their consumption. Such information would allow nutrition education efforts to build on existing food preferences to enhance acceptability of less-preferred or less-familiar foods.
The purpose of this study was to determine the acceptability of whole grain and legume foods among youths with type 1 diabetes and to determine demographic and behavioral factors associated with their acceptability.
Methods
Setting and Participants
This study was conducted at a diabetes camp in Southern Maryland offering 3 consecutive 5-day summer sessions. All eligible campers were invited to participate. A total of 157 youths attended; of these, 141 consented to participate, 12 declined, and 4 were ineligible, resulting in a consent rate of 92% of those eligible. Reasons for ineligibility included extensive dietary restrictions (n = 1), no parent available to provide consent (n = 2), and not diagnosed with diabetes (n = 1). Youths with type 2 diabetes were not included in this data analysis because of the small sample (n = 7). Two participants did not complete data collection, resulting in a total sample of 128. Mean participant age was 11.6 ± 2.3 years (range, 7.0 to 16.9 years), with 70% females. Seventy-five percent of the sample was Caucasian, 17% African American, 2% Asian, 2% American Indian, and 4% mixed race. The mean age at diagnosis was 6.7 ± 3.2 years; 60% of the sample used insulin injections and 40% used insulin pumps. Informed assent and consent were obtained from participants and their parents. The study protocol was approved by the National Institutes of Health Institutional Review Board.
Measures
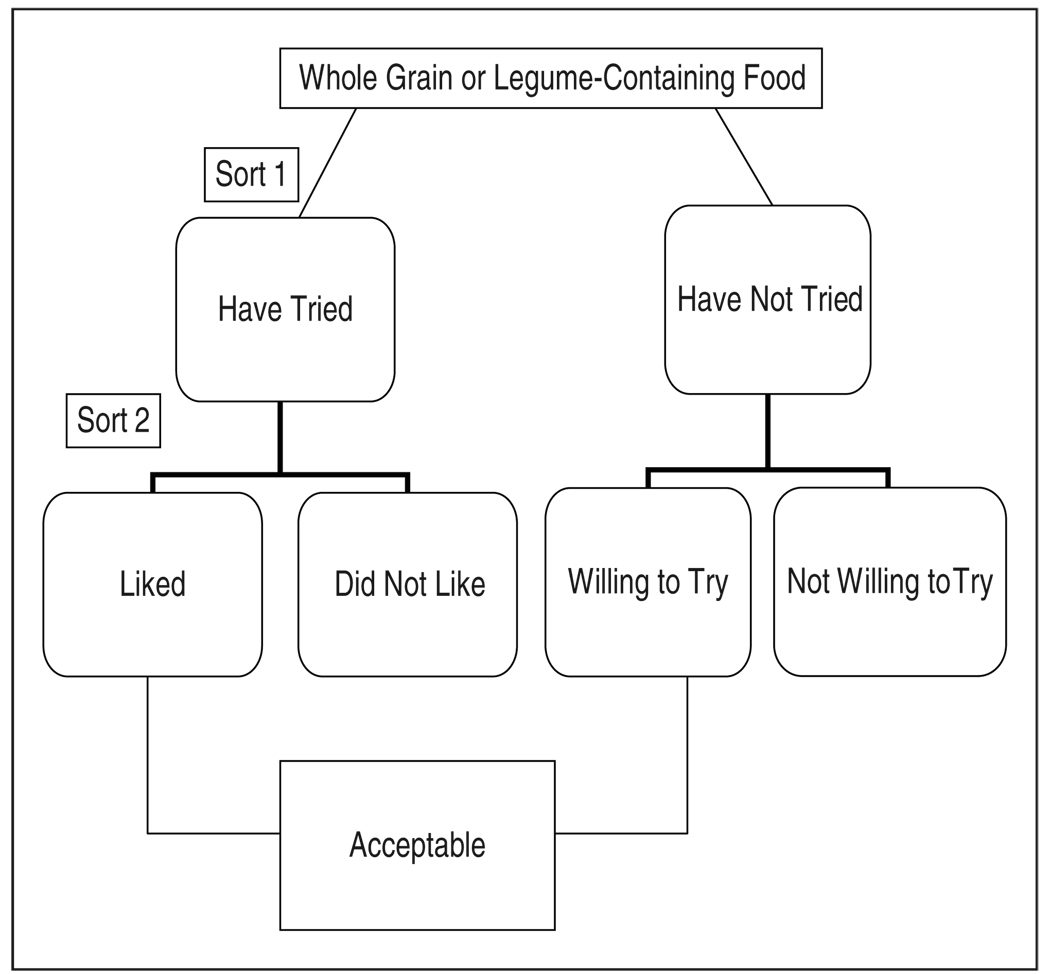
Participants completed self-report measures of food acceptability, eating-related behaviors (frequency of eating together as a family, eating at restaurants, and eating fast food), and demographic characteristics. The food acceptability measure, created for this study, was designed to assess the youth’s cognitive reaction (acceptance versus avoidance) to the presentation of healthy food items. Administered as a Q-sort, each subject received a package of 66 cards, each having the name of 1 food item. A picture and description of each food item was provided. Foods were selected to represent a range of healthful foods that are widely accessible and potentially acceptable. Processed foods of unclear whole grain content (such as whole grain crackers or snack bars) were not included, because respondents would be unlikely to be able to adequately differentiate between primarily whole grain and primarily refined counterparts. Research assistants provided standardized responses to questions. Subjects first sorted the cards into “Have Tried” and “Have Not Tried.” Each grouping then underwent a second sort, resulting in 4 categories. The “Have Tried” grouping was sorted into “Liked” and “Did not Like.” The “Haven’t Tried” grouping was sorted into “Willing to Try” and “Not Willing to Try” (Figure 1). A subset of 13 whole grain food items and 14 legume food items were analyzed.
Figure 1.
Q-sort measure flow chart.
Statistical Analyses
Descriptive analyses were performed including evaluation of means, standard deviations, and ranges of continuous variables and distributions of categorical variables. An overall acceptability score was calculated for whole grains and for legumes as the sum of foods in each category rated as either “tried and liked” or “not tried and willing to try.” Correlations of whole grain and legume acceptability with demographic characteristics were examined using Pearson correlation coefficient. Statistical significance was defined as P < .05. All analyses were performed using STATA 9.0 (Stata Corp, College Station, Texas).
Results
Whole Grain Acceptability
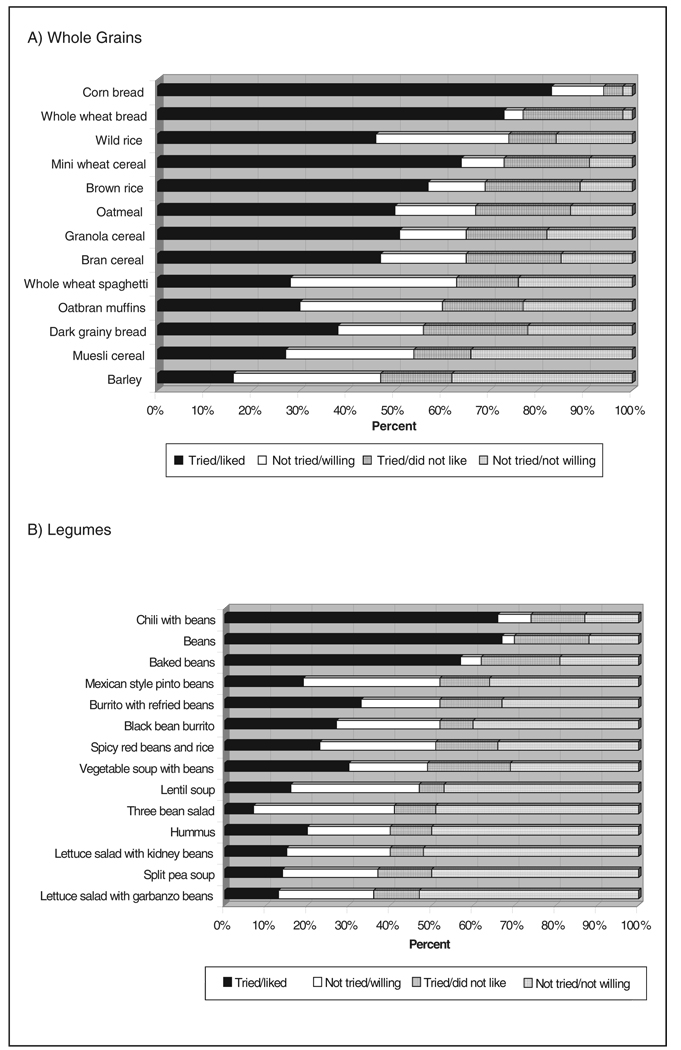
Acceptability of whole grain foods varied widely (Figure 2a). The whole grain foods with the highest acceptability were corn bread (85% tried/liked and 11% willing to try) and whole wheat bread (72% tried/liked and 3% willing to try). Barley (16% tried/liked and 31% willing to try) and muesli cereal (27% tried/liked and 12% willing to try) demonstrated the lowest acceptability. The mean number of whole grains that were acceptable to children was 8.7 ± 3.4 of 13 possible. Total whole grain acceptability was negatively associated with number of days per week of fast food consumption (r = −0.21; P < .02) and with living in an urban environment (r = − 0.24; P < .01). There were no associations between total whole grain acceptability and age, parent’s level of education, gender, frequency of restaurant dining, or frequency of eating family meals together.
Figure 2.
Acceptability of whole grain and legume foods.
Legume Acceptability
Acceptability of legumes also varied greatly (Figure 2b). Acceptability of the general category of “beans” was 79% (67% tried/liked and 12% willing to try). Chili with beans (66% tried/liked and 8% willing to try) and baked beans (57% tried/liked and 19% willing to try) were the legume-containing foods with the highest acceptability. Lettuce salad with garbanzo beans (13% tried/liked and 23% willing to try) and split pea soup (14% tried/liked and 23% willing to try) demonstrated the lowest acceptability. The mean number of legumes that were acceptable to children was 7.1 ± 4.5 of 14 possible. There were no associations between legume acceptability and fast food consumption, living in an urban environment, age, parent’s level of education, gender, frequency of restaurant dining, or frequency of eating family meals together.
Discussion
Despite low whole grain and legume consumption among US youths, findings from this study indicate that a substantial percentage of youth with type 1 diabetes report a willingness to eat various whole grains and legumes. Current low consumption, then, may be related less to an unwillingness to eat these foods and more to their competition with highly accessible and palatable refined carbohydrate foods. Familiarity may be an important consideration in whole grain and legume acceptability. More common whole grain foods such as corn bread, brown rice, and whole wheat bread were more acceptable to youths, whereas less common foods such as muesli cereal and barley were less acceptable. Similarly, less common legume containing foods such as three bean salad and lentil soup were less acceptable, whereas baked beans, a more commonly consumed legume containing food, was more acceptable.
The main limitation of this study was that it was conducted at a single diabetes camp; thus, participants were from a limited geographic range. Although the camp served urban, suburban, and rural areas, and included youth from a broad range of socioeconomic status, this study did not address cultural, geographic, and socioeconomic differences in acceptability of whole grain and legume containing foods. Acceptability may be influenced by race, ethnicity, and cultural factors; however, this study did not involve sufficient participants of varying races or ethnicity to address these issues. Additionally, all participants had type 1 diabetes; thus, results are not necessarily generalizable to healthy youths or youths with type 2 diabetes.
Given the documented relationship of whole grain and legume consumption with health outcomes in adults, as well as findings from this study suggesting sufficient acceptability of many whole grain and legume foods, efforts to increase whole grain and legume consumption among youth with type 1 diabetes should be undertaken. In addition, future research examining the effects of consuming more whole grains and legumes on glycemic control and other diabetes-related health outcomes is warranted.
Implications for Practice
Diabetes education regarding dietary intake requires finding a balance between assisting families to incorporate diabetes management into existing dietary patterns and promoting improvements in dietary intake where needed. Given extremely low rates of whole grain and legume consumption, these foods merit particular attention. When counseling patients on nutrition, diabetes educators should focus on helping patients increase their exposure to whole grains and legumes, and enhancing their ability to identify these foods in their current food environment. Information on usual dietary intake and food preferences can be used to inform suggestions for whole grain and legume alternatives for more highly processed foods in the current diet. Given the varied acceptability of whole grain and legume foods, youths may need to be offered a variety of different foods to allow them to select the foods that are most acceptable to them. It is important to note that gradual behavior change and flexibility are recommended when attempting to increase intake of new foods or foods that are infrequently consumed. For example, the diabetes educator can suggest that whole grain pasta be partially substituted for regular pasta and the ratio of whole grain pasta to regular pasta can be gradually increased over time. Taste preference is a well-documented mediating factor of food choice25; therefore, efforts to increase consumption should incorporate the most acceptable whole grain and legume containing foods to foster behavior change, and then build on these initial changes to promote consumption of the less familiar whole grain and legume foods. Families may not be aware that multiple exposures are often needed for new foods to become acceptable, and so they should be provided with education about how taste and food preferences can be changed with repeated exposure. In addition, efforts to increase whole grain and legume consumption are likely to be more successful if these foods are served as a substitute for highly refined foods rather than in direct competition with such foods. Nansel and colleagues demonstrated high satisfaction for 100% whole grain bread when it was the only bread served for that meal.26
Monitoring food intake for blood glucose management primarily focuses on carbohydrate consumption; therefore, diabetes educators can build on carbohydrate counting education to guide youths toward healthier carbohydrate choices. When teaching youths with type 1 diabetes about carbohydrate counting, the educator should emphasize that while different carbohydrates are counted the same, they are not all equal in terms of their nutritional value and so healthier carbohydrates such as legumes and whole grains should be consumed more frequently than refined foods. Because most whole grains and legumes are less commonly consumed than refined grain products, diabetes educators should provide specific suggestions for foods to consume and ideas for incorporating these foods into the family’s usual diet. Results from this study suggest that whole grains and legumes can in fact be acceptable to youths with type 1 diabetes. Promoting consumption of these foods should be an integral part of diabetes nutrition education.
Acknowledgments
The authors acknowledge the contribution of Robert Rainey, camp administrator, Linda Zeitzoff, camp nurse practitioner, and the staff of Lions Camp Merrick for their assistance in the conduct of this study. This research was supported by the Intramural Research Program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development.
References
- 1.Department of Health and Human Services (HHS) and the Department of Agriculture (USDA) Washington, DC: United States Government Printing Office; Dietary Guidelines for Americans. 2005
- 2.Cleveland LE, Moshfegh AJ, Albertson AM, Goldman JD. Dietary intake of whole grains. J Am Coll Nutr. 2000;19:331S–338S. doi: 10.1080/07315724.2000.10718969. [DOI] [PubMed] [Google Scholar]
- 3.Harnack L, Walters SA, Jacobs DR., Jr Dietary intake and food sources of whole grains among US children and adolescents: data from the 1994–1996 Continuing Survey of Food Intakes by Individuals. J Am Diet Assoc. 2003;103:1015–1019. doi: 10.1016/s0002-8223(03)00470-x. [DOI] [PubMed] [Google Scholar]
- 4.Department of Health and Human Services (HHS) Healthy People 2010. Washington, DC: Office of Disease Prevention and Health Promotion; 2006. [Google Scholar]
- 5.Liese AD. Whole-grain intake and insulin sensitivity: the Insulin Resistance Atherosclerosis Study. Am J Clin Nutr. 2003;78:965–971. doi: 10.1093/ajcn/78.5.965. [DOI] [PubMed] [Google Scholar]
- 6.Melanson KJ, Angelopoulos TJ, Nguyen VT, et al. Consumption of whole-grain cereals during weight loss: effects on dietary quality, dietary fiber, magnesium, vitamin B-6, and obesity. J Am Diet Assoc. 2006;106:1380–1388. doi: 10.1016/j.jada.2006.06.003. [DOI] [PubMed] [Google Scholar]
- 7.Koh-Banerjee P, Franz M, Sampson L, et al. Whole grain consumption and weight gain: a review of the epidemiological evidence, potential mechanisms and opportunities for future research. Am J Clin Nutr. 2004;80:1237–1245. doi: 10.1079/PNS2002232. [DOI] [PubMed] [Google Scholar]
- 8.Liu S, Manson J, Stampfer M, et al. Whole grain consumption and risk of ischemic stroke in women: a prospective study. JAMA. 2000;284:1534–1540. doi: 10.1001/jama.284.12.1534. [DOI] [PubMed] [Google Scholar]
- 9.Jensen MK, Koh-Banerjee P, Hu FB, Sampson L, Gronbaek M, Rimm EB. Intakes of whole grains, bran, and germ and the risk of coronary heart disease in men. Am J Clin Nutr. 2004;80:1492–1499. doi: 10.1093/ajcn/80.6.1492. [DOI] [PubMed] [Google Scholar]
- 10.Liu S, Stampfer MJ, Hu FB, et al. Whole-grain consumption and risk of coronary heart disease: results from the Nurses’ Health Study. Am J Clin Nutr. 1999;70:412–419. doi: 10.1093/ajcn/70.3.412. [DOI] [PubMed] [Google Scholar]
- 11.Jacobs DR, Slavin J, Marquart L. Whole grain intake and cancer: a review of the literature. Nutr Cancer. 1995;24:221–299. doi: 10.1080/01635589509514411. [DOI] [PubMed] [Google Scholar]
- 12.Lanza E, Hartman TJ, Albert PS, et al. High dry bean intake and reduced risk of advanced colorectal adenoma recurrence among participants in the polyp prevention trial. J Nutr. 2006;136:1896–1903. doi: 10.1093/jn/136.7.1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Adebamowo CA, Cho E, Sampson L, et al. Dietary flavonols and flavonol-rich food intake and the risk of breast cancer. Int J Cancer. 2005;114:628–633. doi: 10.1002/ijc.20741. [DOI] [PubMed] [Google Scholar]
- 14.Flight I, Clifton P. Cereal grains and legumes in the prevention of coronary heart disease and stroke: a review of the literature. Eur J Clin Nutr. 2006;60:1145–1159. doi: 10.1038/sj.ejcn.1602435. [DOI] [PubMed] [Google Scholar]
- 15.Dilaware JB, Kumar A, Khurana S, Bhatnagar R, Dash RJ. Effect of legumes on blood sugar in diabetes mellitus. Indian J Med Res. 1987;85:184–187. [PubMed] [Google Scholar]
- 16.Steffen LM, Jacobs DR, Murtaugh MA, et al. Whole grain intake is associated with lower body mass and greater insulin sensitivity among adolescents. Am J Epidemiol. 2003;158:243–250. doi: 10.1093/aje/kwg146. [DOI] [PubMed] [Google Scholar]
- 17.American Diabetes Association. [Accessed April 28];Complications of Diabetes in the United Status. 2008 http://www.diabetes.org/diabetes-statistics/complications.jsp.
- 18.American Diabetes Association. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care. 2007;30 Suppl 1:S48–S65. doi: 10.2337/dc07-S048. [DOI] [PubMed] [Google Scholar]
- 19.Ludwig DS. The glycemic index: physiological mechanisms relating to obesity, diabetes, and cardiovascular disease. JAMA. 2002;287:2414–2423. doi: 10.1001/jama.287.18.2414. [DOI] [PubMed] [Google Scholar]
- 20.Baumer JH, Drakeford JA, Wadsworth J, Savage DCL. Effects of dietary fibre and exercise on mid-morning diabetic control: a controlled trial. Arch Dis Child. 1982;57:905–909. doi: 10.1136/adc.57.12.905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kinmonth AL, Angus RM, Jenkins PA, Smith MA, Baum JD. Whole foods and increased dietary fibre improve blood glucose control in diabetic children. Arch Dis Child. 1982;57:187–194. doi: 10.1136/adc.57.3.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoey H, Aanstoot HJ, Chiarelli F, et al. Good metabolic control is associated with better quality of life in 2,101 adolescents with type 1 diabetes. Diabetes Care. 2001;24:1923–1928. doi: 10.2337/diacare.24.11.1923. [DOI] [PubMed] [Google Scholar]
- 23.The Diabetes Control and Complications Trial Research Group. The Effect of Intensive Treatment of Diabetes on the Development and Progression of Long-Term Complications in Insulin-Dependent Diabetes Mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 24.Mayer-Davis EL, Liese NM, Bell RA, et al. Dietary intake among youth with diabetes: the SEARCH for Diabetes in Youth Study. J Am Diet Assoc. 2006;106:689–697. doi: 10.1016/j.jada.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 25.Neumark-Sztainer D, Story M, Perry C, Casey MA. Factors influencing food choices of adolescents: findings from focus-group discussions with adolescents. J Am Diet Assoc. 1999;99:929–937. doi: 10.1016/S0002-8223(99)00222-9. [DOI] [PubMed] [Google Scholar]
- 26.Nansel TR, Gellar L, Zeitzoff L. Acceptability of lower glycemic index foods in the diabetes camp setting. J Nutr Educ Behav. 2006;38:143–150. doi: 10.1016/j.jneb.2006.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]