Abstract
The aim of this review was to provide of the current knowledge in pathophysiology, diagnosis and management of spondylolysis based on the authors' experience and the pertinent medical literature.
Spondylolysis represents a weakness or stress fracture in one of the bony bridges that connect the upper with the lower facet joints of the vertebra. It is the most common cause of low back pain in young athletes. One-half of all paediatric and adolescent back pain in athletic patients is related to various disturbances in the posterior elements including spondylolysis. The most common clinical presentation of spondylolysis is low back pain. This is aggravated by activity and is frequently accompanied by minimal or no physical findings. A pars stress fracture or early spondylolysis are common and a misdiagnosis is often made.
Plain radiography with posteroanterior (P - A), lateral and oblique views have proved very useful in the initial diagnostics of low back pain, but imaging studies such as Computed Tomography (CT) and Magnetic Resonance Imaging (MRI) scans are more sensitive in the establishment of the diagnosis.
Several treatment options are available. Surgical treatment is indicated only for symptomatic cases when conservative methods fail. The fact that early and multiple imaging studies may have a role in the diagnosis of pars lesions and the selection of the optimal treatment approaches is also highlighted.
Keywords: spondylolysis, spondylolisthesis, spine, low back pain, pars interarticularis
Spondylolysis is defined as a bony defect in the pars interarticularis of the vertebral arch. It presents a weakness or stress fracture in one of the bony bridges that connects the upper with the lower facet joints. This defect can either be asymptomatic or associated with significant low back pain (LBP). This condition is present in up to 6% of the population1. Although the aetiology of this lesion is still unclear, it has been shown to have both hereditary and acquired risk factors, with an increased prevalence in men and athletes participating in certain high-risk sports. Spondylolysis is indeed, a common cause of low back pain in preadolescent and adolescent athletes (50%) and it particularly presents a clinical problem in this population2. It occurs with higher frequency in people engaged in certain activities that appear to put unusual stress on their lower spine. Gymnasts, football linemen, weightlifters, wrestlers, dancers, and drivers are the most commonly affected individuals. However, primary care practitioners should be familiar with its frequency and the possibility of progression from a pars interarticularis stress fracture to spondylolysis and/or to spondylolisthesis3–5.
The vast majority of spondylolitic defects occur at the L5 level (85 - 95%), with L4 being the second most commonly involved level (5 – 15%) whereas higher lumbar areas are rarely affected6. This defect is seen relatively often in plain radiographic studies with posteroanterior and lateral views, although dynamic and oblique views seem to determine the vertebral stability and lead to the diagnosis7.
Spondylolisthesis occurs in a significant proportion of individuals with bilateral spondylolysis. It appears that approximately 50 - 81% of people suffering from spondylolysis have associated spondylolisthesis1. This is defined as: the complete bilateral fractures of the pars interarticularis resulting in the anterior slippage of the vertebra. Predicting risk factors for progression of the slip to spondylolisthesis has proven to be difficult6,8.
Unfortunately, since a misdiagnosis of spondylolysis is often made, an early recognition of this entity is essential. A complicating factor in the early stages of the disease that leads to a misdiagnosis is the fact that plain radiographs, even with oblique films, may not be helpful at the stress fracture stage. Other imaging techniques, such as bone scan possibly with single photon emission computed tomography (SPECT) or magnetic resonance image (MRI) should be used early in the diagnostic process. In the primary care setting, an early diagnosis of posterior element involvement related to low back pain either at the stage of pars stress fracture or early spondylolysis can prevent progression of the disease and obviate the need for an aggressive intervention of a more significant defect9,10.
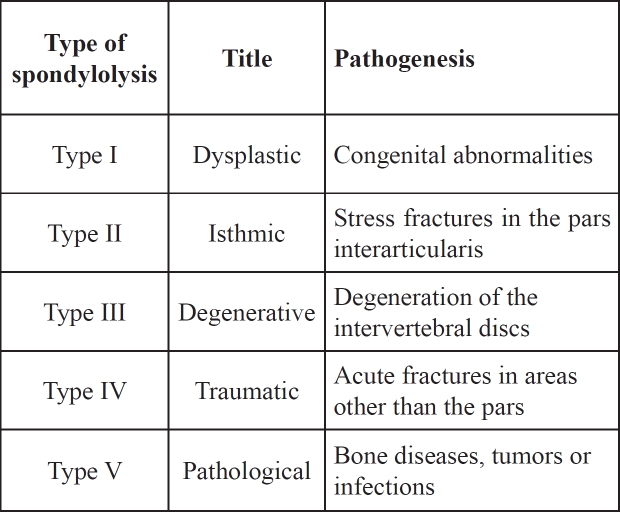
Spondylolysis is subdivided in five categories: dysplastic, isthmic, degenerative, traumatic and pathological - each representing distinct considerations and characteristics for all healthcare providers3,9,11. Dysplastic conditions involve congenital abnormalities (attenuated pars); isthmic conditions are lesions in the pars interarticularis resulting from stress fractures or acute fractures; - Degenerative conditions are related to segmental instability and alterations of the articular processes due to degeneration of the intervertebral discs; - traumatic spondylolysis results from acute fractures in various areas of the neural arch, other than the pars. Finally, pathological conditions involve various bone diseases, tumours or infections and their complications. (Table 1).
Table 1. Types of spondylolysis11.
The present review focuses primarily on isthmic spondylolysis resulting from stress fractures, due to mechanical stress in the pars interarticularis caused by hyperextension and rotation forces, especially during stressful exercises1,3,11,12.
Clinical presentation
In the majority of cases spondylolysis is asymptomatic and identified incidentally. Of the symptomatic individuals, the major complain is the focal low back pain, which frequently radiates into the buttock or proximal lower limb. The onset of pain is acute or gradual, after an intense athletic activity (lumbar spinal rotation or extension). Some patients may also report a recent or old history of local trauma. The pain is intense and restricts everyday activities. Symptoms typically worsen acutely after a particular stressful event5,6,13,14.
Based on the pertinent literature, the only possible pathognomonic finding during physical examination, is the reproduction of pain by performing the one legged hyperextension manoeuvre (the patient stands on one leg and leans backwards). Interestingly, unilateral lesions often produce pain when standing on the ipsilateral leg8,15,16 (Figure 1).
Figure 1. The one legged hyperextension manoeuvre.
Diagnosis
Radiographic studies and other more detailed imaging modalities assist in the diagnosis of spondylolysis. Several imaging modalities may play a role in the identification of a symptomatic pars lesion. The radiographic visualisation of a pars lesion is essential in establishing the diagnosis of symptomatic spondylolysis17.
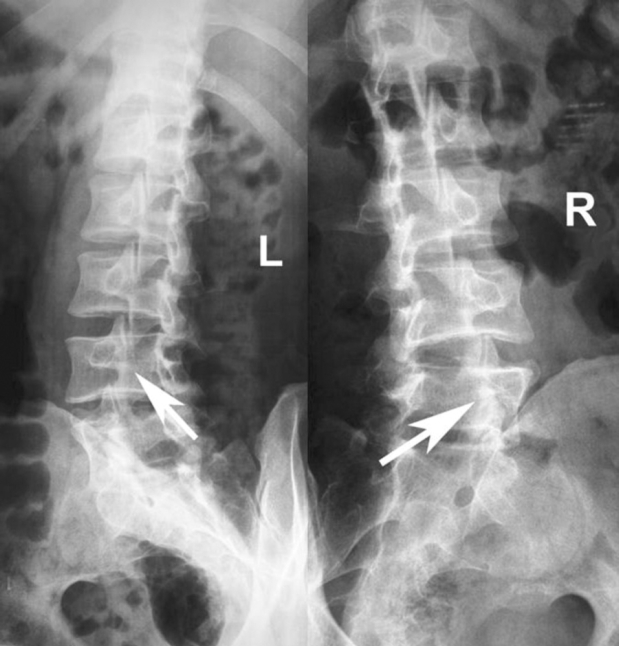
Plain radiographs of the spine are always performed, in symptomatic spondylolysis or not, mainly to rule out underlying specific diagnosis and to describe degenerative spine changes. Plain radiographs with posteroanterior and lateral views are useful in the initial investigation of low back pain, whereas dynamic and oblique views help in the determination of vertebral stability18,19 (Figure 2).
Figure 2. X-ray oblique views of the Lumbar Spine showing the defect in the pars interarticularis at the L4 level.
According to different studies, about 20% of pars defects seen on plain radiographs can be identified on oblique views only6. A common term used for the diagnostic description of the neural arch region defect, is the visualisation of "the collar on the Scottie dog". The collar indicates the non displaced fracture of the pars interarticularis (Figure 3)6,17,18.
Figure 3. Plain radiograph of the lumbar spine. The collar sign on the Scottie dog17.
In the past, most studies have used plain conventional x-rays as the only diagnostic method to determine spondylolysis. It should be noted however that they represented an important diagnostic tool for a long time since the defect in isthmic spondylolysis is visualised as a lucency in the pars interarticularis5. Standard radiographic examinations are still helpful in the diagnosis. They can predict what the prognosis will be in terms of the evolution defect and more importantly indicate what treatment should be applied, according to the degree of the slippage, the slip angle etc. On the other hand, the most significant limitation of plain radiographs is the lack of orientation from the plane of the defect5,15,16.
Over the past decades, other imaging modalities have been increasingly used for diagnosing of spondylolysis. These include the Computed Tomography (CT) scan, the Single Photon Emission Computed Tomography (SPECT) and the magnetic Resonance Imaging (MRI)20. All the above methods have proven to be more sensitive, in identifying pars lesions allowing more complicated angles to be taken to accommodate the complex structure of the lower spine. These techniques can definitely lead with more accuracy to the diagnosis of spondylolysis. A bone scan is useful in the early stages of spondylolysis. In some studies, though, in early spondylolysis, changes in the MRI signal intensity in the pars interarticularis may be detected, even before fracture lines are visible on plain radiographs. Nevertheless, further studies are needed to validate MRI as the imaging modality of choice for the early diagnosis of spondylolysis. Although, the CT scan and in particular high definition multislice devices is the most accurate examination, MRI has also become an indispensable diagnostic tool6. At MRI, most of degenerative disc abnormalities are non-specific and are frequently found in the asymptomatic subjects. On fat-suppressed T2WI images, the presence of oedema in the end-plates in case of degenerative disc disease and in the posterior arches when facet arthropathy and spondylolysis are present is well-correlated to LBP. Such visualised oedema may be useful to direct the treatment approach in these patients. (Figure 4)19,21.
Figure 4. T2-weighted MRI of the Lumbar Spine. Changes on the signal intensity at the L4 - L5 level indicative of spondylolysis.
According to the pertinent literature, CT best demonstrates fracture size and extent, and is the most appropriate modality for the follow-up as a baseline for assessment of healing. MRI is limited in its ability to fully depict the cortical integrity of incomplete fractures in the pars interarticularis, but the presence of marrow oedema on fat-saturated T2-weighted sequences is a useful sign for diagnosing acute spondylolysis9,10,21.
Treatment
The lack of large controlled clinical trials focused on the diagnosis and management of spondylolysis renders the establishment of an optimal treatment algorithm difficult. Recent advances in imaging technology have proven to be useful in the diagnosis and the follow – up in symptomatic patients11.
Conservative methods should be applied to all affected individuals. In fact, most symptomatic cases do well with conservative care. Many pars lesions may heal if managed conservatively, particularly those with early stage defects. According to the classification of Standaert and Herring, pars lesions are divided in early, progressive and terminal stages. The likelihood to heal is much higher in early stage lesions with very few changes of healing or no healing in terminal stages9,17,19,22.
Pharmacological intervention includes the application of pain relief medications. The nonsteroidal anti inflammatory drugs (NSAIDs) should not be ordinarily used because they slow down the bone growth and healing. If the patient is osteoporotic or osteopenic, alendronate sodium is a pharmacological alternative6,15.
Once pain levels are controlled, pulsed ultrasound and therapeutic isometric contractions of surrounding musculature may be initiated to promote additional blood flow, by increasing collagen, neovascular and myofibroblast production in the injured lesion. Through this way, the healing process is also facilitates. Moreover, the use of electrical bone stimulators (internals or externals) seems to promote healing19,23,26.
Surgical treatment is used only for symptomatic cases were all conservative methods failed to show any effect. Approximately 9-15% of cases of symptomatic spondylolysis undergo surgery. The main indications include intractable pain, progressive slip, development of neurological deficits and segmental spine instability. Surgical procedures typically attempt a direct repair of the pars which is sometimes accompanied by a fusion procedure. Specific surgical techniques, such as translaminar screw fixation, cerclage wiring loop and pendiculolaminar hook screws, preserve segmental motion by repairing the isthmic defect24.
Although treating spondylolysis may seem complicated, an uneventful outcome may be experienced. Rehabilitation programmes are strongly recommended for symptomatic and post - surgical patients. It is imperative these programmes to be guided by patients' pain and tolerance and their objectives to be the promotion of bone healing, the relief of pain and the optimization of physical function25–27.
Conclusions
It is very important to obtain a prompt diagnosis of symptomatic spondylolysis so that the disease can be treated properly. The diagnostic approach and the treatment of spondylolysis should be carried out on an individual basis after taking into consideration the patient's clinical status and the results from the diagnostic methods. The management guidelines have remained largely unchanged since earlier recommendations. Most cases are managed conservatively with success. However in special occasions surgery is indicated. The introduction of a bone growth stimulator in the management of chalenging cases is promising for the future of this entity.
References
- 1.Hu SS, Tribus CB, Diab M, Ghanayem AJ. Spondylolisthesis and spondylolysis. Instr Course Lect. 2008;57:431–445. [PubMed] [Google Scholar]
- 2.McTimoney CA, Micheli LJ. Current evaluation and management of spondylolysis and spondylolisthesis. Curr Sports Med Rep. 2003;2:41–46. doi: 10.1249/00149619-200302000-00008. [DOI] [PubMed] [Google Scholar]
- 3.Merbs C. Asymmetrical Spondylolysis. Am J Ph Anthropology. 2002;119:156–174. doi: 10.1002/ajpa.10100. [DOI] [PubMed] [Google Scholar]
- 4.Peer KS, Fascione JM. Spondylolysis: a review and treatment approach. Orthop Nursing. 2007;26:104–111. doi: 10.1097/01.NOR.0000265867.70479.cb. [DOI] [PubMed] [Google Scholar]
- 5.Ralston S. Suspecting lumbar spondylolysis in adolescent lumbar back pain. Cl Paediatr. 1998;37:287–293. doi: 10.1177/000992289803700502. [DOI] [PubMed] [Google Scholar]
- 6.Standaert DC, Herring S. Spondylolysis: a critical review. Br J Sports Med. 2000;34:415–422. doi: 10.1136/bjsm.34.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rodts MF. Disorders of the spine. Orthop Nurs. 2002;3:515–550. [Google Scholar]
- 8.Logroscino G, Mazza O, Aulisa AG, Pitta L, Pola E, Aulisa L. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Child's Nerv Syst. 2001;17:644–655. doi: 10.1007/s003810100495. [DOI] [PubMed] [Google Scholar]
- 9.Bellache L, Petrover D. Imaging in chronic low back pain: which one and when? Rev Prat. 2008;58:273–278. [PubMed] [Google Scholar]
- 10.Campbell RS, Grainger AJ, Hide IG, Papastefanou S, Greenough CG. Juvenile spondylolysis: a comparative analysis of CT, SPECT and MRI. Skeletal Radiol. 2005;34:63–73. doi: 10.1007/s00256-004-0878-3. [DOI] [PubMed] [Google Scholar]
- 11.Wiltse LL, Newman PH, Macnab I. Classification of Spondylolysis and Spondylolisthesis. Clin Orthop. 1976;117:23–29. [PubMed] [Google Scholar]
- 12.Nance DK, Hickey M. Spondylolisthesis in children and adolescents. Orthop Nursing. 1999;18:21–27. [PubMed] [Google Scholar]
- 13.Morita T, Ikata T, Katoh S. Pathogenesis of spondylolysis and spondylolisthesis in young athletes based on a radiological and MRI study. Maui, Hawai: North American Spine Society/Japanese Spine Research Society Spine across the Sea meeting; 1994. [Google Scholar]
- 14.Standaert DC. Practical management: Spondylolysis in the adolescent athlete. Cl J Sports Med. 2002;12:119–122. doi: 10.1097/00042752-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 15.Houglum P. Therapeutic exercise for musculoskeletal injuries. Champaign: Human Kin; 2005. [Google Scholar]
- 16.Standaert DC, Herring S, Halpern B, King O. Spondylolysis. Ph. Med Rehabil Clin North Am. 2000;11:785–803. [PubMed] [Google Scholar]
- 17.Jarvik JG, Deyo R. Diagnostic evaluation of low back pain with emphasis on imaging. Annals of Internal Medicine. 2002;137:588–598. doi: 10.7326/0003-4819-137-7-200210010-00010. [DOI] [PubMed] [Google Scholar]
- 18.Scavone JG, Latshaw RF, Weidner WA. Anteroposterior and lateral radiographs: an adequate lumbar spine examination. AJR. 1980;136:715–717. doi: 10.2214/ajr.136.4.715. [DOI] [PubMed] [Google Scholar]
- 19.Katoh S, Ikata T, Fujii K. Factors influencing on union of spondylolysis in children and adolescents; Proceedings and abstracts from North American Spine Society meeting; New York. 1997. p. 222. [Google Scholar]
- 20.Dutton JAE, Hughes SPF, Peters AM. SPECT in the management of patients with low back pain and spondylolysis. Cl. Nuclear Medicine. 2000;25:93–96. doi: 10.1097/00003072-200002000-00001. [DOI] [PubMed] [Google Scholar]
- 21.Wirtz DC, Wildberger JE, R?hrig H, Zilkens KW. Early diagnosis of isthmic spondylolysis with MRI. Z Orthop Ihre Grenzgeb. 1999;137:508–511. doi: 10.1055/s-2008-1039380. [DOI] [PubMed] [Google Scholar]
- 22.Dunn AJ, Campbell RS, Mayor PE, Rees D. Radiological findings and healing patterns of incomplete stress fractures of the pars interarticularis. Skeletal Radiol. 2008;37:443–450. doi: 10.1007/s00256-008-0449-0. [DOI] [PubMed] [Google Scholar]
- 23.Morita T, Ikata T, Katoh S. Lumbar spondylolysis in children and adolescents. J Bone Joint Surg (Br) 1995;77:620–625. [PubMed] [Google Scholar]
- 24.Starkey C, Ryan J. Evaluation of Orthopaedic and athletic injuries. Philadelphia: FA Davis Co; 2002. [Google Scholar]
- 25.Soler T, Calderon C. The prevalence of spondylolysis in the Spanish elite athletes. Am J Sports Med. 2000;28:57–62. doi: 10.1177/03635465000280012101. [DOI] [PubMed] [Google Scholar]
- 26.Sys J, Michielsen J, Bracke P, Martens M, Verstreken J. Nonoperative treatment of active spondylolysis in elite athletes with normal X-ray findings: literature review and results of conservative treatment. Eur Spine J. 2001;10:498–504. doi: 10.1007/s005860100326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thein-Nissenbaum J, Boissonault W. Differential diagnosis of spondylolysis in a patient with chronic low back pain. J Orthop Sports Ph Ther. 2005;35:319–326. doi: 10.2519/jospt.2005.35.5.319. [DOI] [PubMed] [Google Scholar]