Abstract
Background
We examined whether immigrants were less likely to be covered by a smokefree workplace policy, as well as whether workplace smoking policies garnered comparable associations with smoking for immigrants and the US-born, in the US.
Methods
We applied the 2001/02 Current Population Survey Tobacco Use Supplement among US indoor workers (n=85,784) using multiple logistic regression analyses. First, we examined whether nativity (immigrants vs. US-born) was independently associated with smokefree policy coverage. Second, we examined whether the smokefree policy association with current smoking was differential by nativity (effect modification).
Results
Immigrants were less likely to work in smokefree workplaces than the US-born; however occupation and industry accounted for these disparities. Employment in a workplace that was not smokefree was associated with higher odds of smoking (vs. smokefree workplaces), both before (OR=1.83, 95% CI:1.74–1.92) and after (OR=1.36, (1.29–1.44)) covariate adjustment among the US-born, but associations were weaker among immigrants (OR=1.39(1.20–1.61) unadjusted, OR=1.15(0.97–1.35) adjusted). Worker industry partly explained (16% of) the weaker policy-smoking association among immigrants, while other socioeconomic variables reduced the policy-smoking association without explaining the disparity.
Conclusions
The patchwork of US workplace smoking restriction policy at different governmental levels, combined with a voluntary regime among some employers, generates coverage inequalities. Workplace smokefree policies may be less effective for immigrants, and this is related to differential coverage by such policies due to occupational segregation. Understanding the complex patterns of the social context of smoking is important for understanding how policy interventions might have heterogeneous effects for different demographic groups.
MeSH Keywords: Environmental Tobacco Smoke, Environmental Smoke Pollution, Tobacco, Immigrants, Public Policy, Inequalities
A substantial body of evidence suggests that Environmental Tobacco Smoke (ETS) is a cause of morbidity and mortality.[1,2] Increasing the strength and reach of tobacco control policy is one explicit path to reducing tobacco-related disease,[3] the single leading preventable cause of US deaths.[4] Although workplace smokefree laws were originally enacted to protect workers from ETS, their major benefit is that they discourage smoking among smokers as well.[5]
Tobacco use regulations do not protect everyone equally, however. Those with lower education, and those in blue collar, service or agricultural jobs are less likely to be covered by smokefree policies than college graduates and white collar/professional workers.[5–7] Moreover, smokefree policies may be more weakly enforced in blue-collar occupations.[8] African Americans and Hispanics are also less likely to be covered by a workplace smokefree policy than whites,[5,7] and more likely to experience high smoke exposure.[3,9] As a growing segment of the U.S. population,[1,10] racial/ethnic minorities carry a higher burden compared to whites of developing and dying from cancer and other tobacco-related disease.[1,11–13] Although the causes explaining these racial/ethnic differentials in disease burden remain poorly understood,[11] exposure to second-hand smoke may be one contributing factor.
Although it is often conflated with racial/ethnicity in health analyses, immigrant status (or nativity) is a distinct dimension of social inequality and may partially explain racial/ethnic smoking-related disparities. Together, immigrants and their children comprise over 22% of the US population,[14–16] and disproportionately contribute to the low-wage and low-skilled end of the labor force.[17,18] Immigrants are less likely than the US-born to enjoy workplace benefits including union membership or union contract coverage,[19] or health insurance coverage.[20] Given this evidence, immigrants may also be less likely to be covered by workplace smoking policies.
In this analysis, we explore how tobacco ETS policy is differentially prevalent among, and may differentially affect the smoking behavior of, different nativity groups in the US. We examine two hypotheses: that workplace smokefree policy is (1) less prevalent among immigrants, and (2) less effective for immigrants (with respect to smoking) than for the US-born population. The literature is currently limited for addressing these research questions. Some articles have reported point estimates of workplace smoking policy prevalence for different racial groups,[6,7,21] but have not examined prevalence among nativity subgroups, or have not examined policy associations with smoking. Although a few studies have examined racial differences in smokefree policy-smoking associations with multivariate analyses, they did not control for nativity (immigrant vs. US-born), or model interactions of race/ethnicity and gender.[5,21,22]
Modeling demographic interactions are important since gender, race/ethnicity, and nativity interact powerfully for smoking patterns. For instance, the protective effects of being foreign-born for smoking are much more pronounced for racial minority groups than whites, and for women than men, even after adjusting for demographic and economic covariates.[23] Moreover, whites and the US-born are numerically dominant in nationally representative datasets. If there is heterogeneity of policy effects on smoking, a statistical model that omits demographic interactions produces estimates essentially for US-born whites, masking differential patterns for other groups.
Immigrants may exhibit a weaker effect of smokefree policy than native-born counterparts for four reasons, including confounding by prior common causes (#3–4): (1) if smokefree workplace policies are most influential for groups with the highest prevalence and daily consumption of cigarettes,[5] (2) if other causes are more powerful than workplace policy for influencing smoking among immigrants, such as anti-tobacco socialization and social norms,[23–25] (3) if immigrants have fewer resources to facilitate quitting,[26] or (4) if immigrants are more likely to be in blue collar and service jobs[17] or industries which have lower smokefree policy coverage[5–7] or weaker enforcement.[8]
METHODS
Data
We used the 2001–02 Tobacco Use Supplement (TUS) of the Current Population Survey (CPS) [27,28] which has valid and reliable tobacco use questions, high response rates, yielding nationally-representative estimates for the US non-institutionalized, civilian population aged 15 years and older. The CPS is conducted by the Census Bureau and employs a multistage, stratified probability sample. TUS questions determining smoking status are identical to those used by the National Center for Health Statistics.[6,29,30]
Variables
Current smoking was modeled dichotomously, defined as having smoked 100 cigarettes in lifetime and currently smoking every day or some days; non smokers were referents.[31] We excluded values missing for the smoking variable (n=1512,0.6% of sample).
Workplace smoking policy was a dichotomous variable (smokefree vs. non-smokefree workplace), assessed using 3 items. Those answering no to this question (“Does your place of work have an official policy that restricts smoking in any way?”) had no policy at work regarding smoking, and were coded as non-smokefree. Those answering yes were asked 2 questions to ascertain their workplace’s smoking policy for work areas, and for indoor public or common areas, such as lobbies, rest rooms, lunch rooms. The possible answers to these questions were: smoking is not allowed in any areas; smoking is allowed in some areas; or smoking is allowed in all areas. We classified people in smokefree workplaces if they answered yes to the first question, and “smoking is not allowed in any areas” to the 2 subsequent questions.[5,7] We classified other responses as non-smokefree workplaces. As discussed elsewhere[6,7,32] the TUS asks the workplace smoking policy questions only among indoor workers who were self-respondents, thus this group comprises our sample. We excluded those missing data for these policy questions (n=2192). Our final sample size was 85,784.
Nativity was modeled dichotomously: either foreign-born or US-born. Those born in the US, in Puerto Rico, or born abroad to US citizens were classified as US-born by the TUS. Foreign born is used interchangeably with the term immigrant throughout the manuscript. We modeled two additional immigrant-related variables including language of interview (English or other), and immigrant length of stay in the US (described further in Table 1). Race/ethnicity was self-reported, restricted to the four largest groups in the US (excluding Native Americans, due to few foreign-born), and coded: non-Hispanic (NH) white, NH black, NH Asian/Pacific Islander and Hispanics of any race.
Table 1.
Descriptive Statistics, Tobacco Use Supplement-Current Population Survey 2001–02 Workplace Smoking Policy Sample
| % current smokers |
% in smokefree workplace |
% foreign born |
|||||
|---|---|---|---|---|---|---|---|
| Variable | Category | Category or Sub-category | n | % of sample | (weighted)1 | (weighted)1 | (weighted)1 |
| Total | 85,784 | 100.00% | 21.12% | 70.53% | 12.29% | ||
| Workplace Smoking Policy | Smokefree | 61,302 | 71.46% | 18.17% | -- | 11.94% | |
| Not smokefree | 24,482 | 28.54% | 28.18% | -- | 13.13% | ||
| Nativity | US Born | 77,561 | 90.41% | 22.19% | 70.81% | -- | |
| Foreign Born (Immigrant) | 8,223 | 9.59% | 13.52% | 68.51% | -- | ||
| Immigrant length of stay in the US | US-Born (reference group) | 77,561 | 90.41% | 22.19% | 70.81% | 0.00% | |
| Immigrant, 0–4 years | 1,202 | 1.40% | 18.08% | 66.65% | 100.00% | ||
| Immigrant, 5–9 years | 1,663 | 1.94% | 13.14% | 64.24% | 100.00% | ||
| Immigrant, 10–14 years | 1,195 | 1.39% | 12.23% | 65.81% | 100.00% | ||
| Immigrant, 15–19 years | 1,250 | 1.46% | 10.94% | 69.29% | 100.00% | ||
| Immigrant, 20+ years | 2,913 | 3.40% | 13.57% | 72.69% | 100.00% | ||
| Interview Language | English | 83,908 | 97.81% | 21.31% | 71.03% | 10.09% | |
| Other | 1,794 | 2.09% | 15.15% | 54.06% | 86.03% | ||
| Immigrant generation | 1st generation (foreign born) | 8,223 | 9.59% | 13.52% | 68.51% | 100.00% | |
| 2nd generation (US-born of foreign born | 5,464 | 6.37% | 17.55% | 72.13% | 0.00% | ||
| 3rd generation and higher (US born of US- | 72,097 | 84.04% | 22.58% | 70.70% | 0.00% | ||
| Race/Ethnicity | Non-Hispanic White | 68,254 | 79.56% | 22.76% | 71.32% | 3.90% | |
| Non-Hispanic Black | 7,828 | 9.13% | 18.50% | 69.17% | 9.95% | ||
| Non-Hispanic Asian | 3,181 | 3.71% | 12.47% | 71.94% | 77.80% | ||
| Hispanic | 6,521 | 7.60% | 16.23% | 65.82% | 46.82% | ||
| Sex | Male | 35,789 | 41.72% | 22.12% | 65.81% | 14.53% | |
| Female | 49,995 | 58.28% | 20.27% | 74.58% | 10.37% | ||
| Income | $0–$9,999 | 2,782 | 3.24% | 30.65% | 60.90% | 16.16% | |
| $10,000–$19,999 | 6,233 | 7.27% | 31.19% | 60.35% | 17.40% | ||
| $20,000–$29,999 | 9,379 | 10.93% | 28.22% | 64.62% | 15.93% | ||
| $30,000–$39,999 | 10,346 | 12.06% | 26.06% | 67.83% | 12.77% | ||
| $40,000–$49,999 | 8,608 | 10.03% | 23.12% | 68.41% | 11.08% | ||
| $50,000–$59,999 | 9,075 | 10.58% | 21.08% | 70.88% | 10.14% | ||
| $60,000–$74,999 | 10,118 | 11.79% | 17.97% | 73.70% | 9.61% | ||
| $75,000+ | 22,040 | 25.69% | 13.21% | 77.91% | 10.41% | ||
| Education | Missing | 7,203 | 8.40% | 19.45% | 69.22% | 14.22% | |
| Less than High School Grad | 7,918 | 9.23% | 26.59% | 56.86% | 26.16% | ||
| High School Grad | 24,376 | 28.42% | 29.64% | 63.78% | 9.88% | ||
| Some College/Associates | 25,569 | 29.81% | 22.78% | 70.71% | 8.14% | ||
| Bachelors or Higher | 27,921 | 32.55% | 10.39% | 80.76% | 13.56% | ||
| Occupation | White Collar | Executive, administrative, & managerial | 14,317 | 16.69% | 17.41% | 75.19% | 8.88% |
| Professional specialty | 17,109 | 19.94% | 11.41% | 84.02% | 12.09% | ||
| Technicians & related support | 3,684 | 4.29% | 18.52% | 77.79% | 12.14% | ||
| Sales | 9,521 | 11.10% | 21.59% | 69.21% | 9.63% | ||
| Service | Administrative support including clerical | 15,296 | 17.83% | 21.37% | 76.12% | 8.26% | |
| Private household service | 56 | 0.07% | 13.12% | 44.33% | 43.32% | ||
| Protective service | 1,148 | 1.34% | 21.12% | 69.60% | 7.96% | ||
| Blue Collar | Service, except protective & household | 10,138 | 11.82% | 28.74% | 58.29% | 17.95% | |
| Precision production, craft, & repair | 5,919 | 6.90% | 30.63% | 52.16% | 14.78% | ||
| Machine operators, assemblers, inspectors | 4,776 | 5.57% | 30.71% | 53.65% | 21.76% | ||
| Transportation & material moving | 944 | 1.10% | 31.37% | 50.10% | 16.08% | ||
| Handlers, equipment cleaners, helpers, & laborers | 2,540 | 2.96% | 27.66% | 60.55% | 16.06% | ||
| Agricultural, forestry, fisheries | Farming, forestry, & fishing | 336 | 0.39% | 21.99% | 46.84% | 24.49% | |
| Industry | Agriculture | 462 | 0.54% | 25.26% | 53.39% | 15.37% | |
| Mining | 283 | 0.33% | 19.85% | 63.29% | 6.84% | ||
| Construction | 1,778 | 2.07% | 27.27% | 48.77% | 14.31% | ||
| Manufacturing | Durable Goods | 8,349 | 9.73% | 25.45% | 58.26% | 15.43% | |
| Nondurable Goods | 5,383 | 6.28% | 24.91% | 64.85% | 16.56% | ||
| Transportation, communications, & other public utilitites | Transportation | 2,531 | 2.95% | 23.73% | 67.58% | 12.26% | |
| Communications | 1,405 | 1.64% | 19.29% | 81.95% | 9.55% | ||
| Wholesale trade | Utilities & sanitary service | 752 | 0.88% | 15.00% | 72.46% | 4.34% | |
| Retail trade | 2,742 | 3.20% | 23.29% | 62.61% | 12.63% | ||
| Finance, insurance, & real estate | 15,020 | 17.51% | 26.52% | 60.74% | 12.70% | ||
| Personal services including private households | 6,579 | 7.67% | 18.17% | 77.07% | 9.47% | ||
| Business, auto & repair services | 67 | 0.08% | 13.09% | 41.72% | 41.99% | ||
| Personal services except private households | 4,889 | 5.70% | 24.47% | 65.75% | 17.99% | ||
| Entertainment & recreation services | 2,212 | 2.58% | 29.18% | 55.21% | 24.25% | ||
| Professional & related services | 1,389 | 1.62% | 22.68% | 56.12% | 10.58% | ||
| Hospitals | 4,753 | 5.54% | 15.53% | 85.05% | 12.30% | ||
| Medical services, except hospitals | 5,399 | 6.29% | 21.87% | 80.12% | 11.21% | ||
| Educational services | 10,132 | 11.81% | 10.87% | 90.06% | 8.69% | ||
| Social services | 2,370 | 2.76% | 18.83% | 81.62% | 8.27% | ||
| Other professional services | 4,544 | 5.30% | 12.66% | 76.84% | 9.48% | ||
| Forestry & fisheries | 63 | 0.07% | 18.16% | 79.08% | 0.93% | ||
| Public administration | 4,682 | 5.46% | 16.34% | 81.00% | 5.85% | ||
| Marital Status | Married | 48,660 | 56.72% | 17.05% | 72.72% | 14.03% | |
| Divorced/Separated/Widowed | 15,206 | 17.73% | 30.20% | 71.05% | 9.31% | ||
| Single/Never married | 21,918 | 25.55% | 23.48% | 66.27% | 10.79% | ||
| Age | 15–19 | 3,483 | 4.06% | 17.57% | 62.12% | 6.59% | |
| 20–29 | 16,171 | 18.85% | 24.53% | 65.34% | 12.61% | ||
| 30–39 | 21,883 | 25.51% | 20.88% | 70.90% | 15.29% | ||
| 40–49 | 22,651 | 26.40% | 22.27% | 72.80% | 11.95% | ||
| 50–59 | 15,875 | 18.51% | 18.90% | 75.42% | 10.35% | ||
| 60+ | 5,721 | 6.67% | 13.85% | 72.87% | 11.03% | ||
All P-values were less than 0.01. P values reported using chi-square statistical tests. Sample excludes Native Americans and those with indeterminate smoking status, and those not in universe for determining workplace smoking policy
CPS-TUS self-response weights applied.
Routine labor force questions were used by the Bureau of Labor Statistics to determine employment status, occupation, and worker industry classification.[6,7,27] For regression, we collapsed occupation into 6 standard categories, and collapsed industrial sector into 8 standard categories.[7] Please see the notes in Table 2 for occupation/industry variable detail in regressions. Education was measured as highest level of school completed or degree received. Income was measured as total annual household earnings, modeled in $10,000 groups, including a missing category. We additionally adjusted for gender, age (age, age2, both centered at 45), marital status, and state of residence (fixed effects). Please see Table 1 for additional covariate coding detail.
Table 2.
Relative Odds of working in a Smokefree Workplace (compared to non-smokefree workplace) by nativity. n=85,784
| Model 1: Foreign Born Coefficient 1 |
||||
|---|---|---|---|---|
| Model | Variables in Model | OR | (95% CI) | p |
| Unadjusted model 2 | ||||
| A | Foreign born only | 0.90 | (0.83, 0.96) | ** |
| Models adjusted for one variable at a time 3 | ||||
| B | Foreign born + Occupation 4 | 1.02 | (0.95, 1.10) | |
| C | Foreign born + Industry 5 | 1.02 | (0.94, 1.10) | |
| D | Foreign born + Income | 0.95 | (0.88, 1.02) | |
| E | Foreign born + Education | 0.94 | (0.87, 1.02) | |
| F | Foreign born + Gender | 0.93 | (0.87, 1.00) | # |
| G | Foreign born + Race/ethnicity | 0.95 | (0.88, 1.03) | |
| H | Foreign born + Marital status | 0.88 | (0.82, 0.95) | ** |
| J | Foreign born + Age | 0.90 | (0.84, 0.97) | ** |
| K | Foreign born + Length of stay | 1.09 | (0.93, 1.27) | |
| L | Foreign born + Language of interview | 1.06 | (0.98, 1.15) | |
| M | Foreign born + State fixed effects | 0.77 | (0.71, 0.83) | *** |
| Fully adjusted model 6 | ||||
| P | Foreign born + all other variables (Final Model) | 1.03 | (0.88, 1.21) | |
p-value: p<.10
p<.05
p<.01
p<.001
OR = Odds Ratio
Nativity is modeled as a 2-level variable, foreign born compared to the reference group of USborn.
Model A, the unadjusted model, includes only the nativity variable.
Models B-M include nativity and one other variable at a time.
Occupation was coded in 5 categories for regression: professional specialty; executive administrative & managerial; technicians & related support, sales, and administrative support including clerical; Service; Blue Collar.
Industry was coded in 8 categories for regression: trade; manufacturing; services; professional and related services; finance, insurance, and real estate; public administration; transportation and communications; agricultural, forestry and fishing, mining, and construction.
Model P is the fully adjusted (final) model including nativity, occupation, industry, income, education, gender, race/ethnicity, marital status, age, state fixed effects, length of stay among immigrants, and language of interview.
Analytic Methods
We used SAS 9.1.3 for univariate and bivariate analyses; we used SUDAAN 10.0 for multiple logistic regression analyses to adjust for the complex survey design by applying sample weights and replicate weights, created using a Balanced Repeated Replication method (personal communication, Anne Hartman, NCI, 3/23/05 and 8/12/07). We produced bivariates and calculated chi-squared tests among demographic variables with smoking prevalence, smokefree policy coverage, and immigrant composition. In logistic regression models, we first regressed smokefree policy coverage on nativity, before and after adjusting for covariates (Model 1 A-P). In these models (Models 1), we predicted the odds of being in a smokefree workplace (1) vs. a non-smokefree workplace (0). We next regressed current smoking on smokefree policy (Models 2–6), to test the main effect of policy (Models 2), and to test nativity interactions with policy (Models 3) in unstratified models. We then stratified by nativity (Models 4–5), and then by nativity, race/ethnicity and gender (Model 6), to examine policy associations with smoking. In Models 2–6, smokefree policy was reverse coded from Model 1, so that in Models 2–6 we modeled the association between the odds of smoking for those in a non-smokefree workplace (1) compared with those in a smokefree workplace (0). In model 3, the logit interaction coefficient represents the differential policy effectiveness among foreign born; a negative coefficient denotes a weaker policy association with smoking for immigrants compared to the US born. The 95% confidence intervals were adjusted for design effects. We present parallel models across Models 1–5. Models A were unadjusted. Models B-N built on Model A to add one variable at a time, to examine changes in the nativity (Model 1) and/or policy (Models 2–5) coefficients. Models P adjusted for all covariates simultaneously. Approval to conduct this study was provided by the Harvard School of Public Health Human Subjects Committee (#P11687-101).
RESULTS
Descriptive Analysis
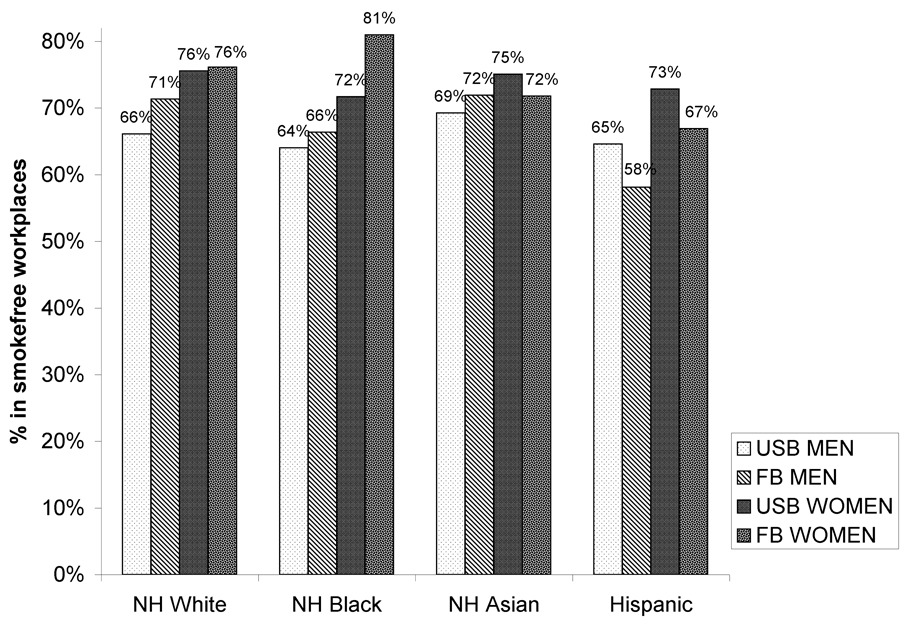
Table 1 presents descriptive statistics. All chi-squared tests of differences were significant at p<.001. Twenty-one percent of US indoor workers were current smokers in 2001–2002. Those born in the US were more likely to smoke than were US immigrants. The majority of US indoor employees worked in smokefree workplaces (70.5%). We observed lower smoking prevalence in smokefree workplaces (18.2%) compared with non-smokefree workplaces (28.2%). Figure 1 presents the variation in prevalence of smokefree policies by employee race/ethnicity, gender, and nativity. Foreign-born Hispanic men are least likely to be covered by a smokefree policy at work – only 58% are in smokefree workplaces vs. 65% for US-born Hispanic men.
Figure 1.
Prevalence of smokefree workplaces by nativity, race/ethnicity, and gender (2001/02 TUS)
NOTES for Figure 1: Sample sizes for each of the demographic subgroups correspond to those listed in Table 4. Racial groups White, Black, and Asian exclude Hispanics. Self-response weights applied.
Table 1 also shows that workers experience differential smokefree policy coverage depending on occupation and industry category, in addition to demographic attributes. For example, workers in professional specialty occupations and professional industries (education, public administration) experience the highest coverage by workplace smokefree policies. These industries also have an underrepresentation of immigrants (compared to the 12.3% prevalence of immigrants in the US). Conversely, service and blue collar occupations, as well as service, construction, manufacturing, and agricultural industries have low coverage of smokefree policies and are overrepresented by immigrants.
Logistic Regression Results
Association of Nativity with Smokefree Policies
Table 2 demonstrates that immigrants have significantly lower odds of workplace smokefree policy coverage compared with the US-born in unadjusted models (Model 1A, OR=.90, 95%CI: 0.83,0.96), and in several models adjusted for certain demographic variables one at a time. However, there are no significant independent associations of nativity with smokefree workplaces after addition of occupation or industry (models 1B–1C), after addition of social class, race, or nativity-related variables, or in models adjusting for all covariates simultaneously (Model 1P). These results suggest that immigrants’ differential employment by occupation and industry category accounts for their lower probability of smokefree policy coverage.
Association of Smokefree Policies with Current Smoking
Table 3 demonstrates that workplace smoking policy was associated with smoking in the expected direction both before and after covariate adjustment, and all smoking policy associations were significant at the .10 level. In unstratified main effect models, we observed higher odds of smoking in non-smokefree workplaces compared to smokefree workplaces in unadjusted models (OR=1.77, 95% CI: (1.69,1.85), Model 2A). The odds ratios of smoking declined with addition of potential confounding variables; addition of occupation, industry, income and education to each model (2–5, C–F) contributed to the largest declines in the smokefree policy-smoking odds ratio. For example, with the addition of occupation (2C), the smoking odds ratio associated with a non-smokefree worksite declined 34% to 1.51 compared to the unadjusted model 2A. In a model adjusted for all factors, the smoking odds ratio associated with working in a non-smokefree worksite was 1.34 (1.27,1.41) (Model 2P). The policy-smoking associations from Model 2 were similar to the results for the US-born in the interaction models (Model 3) and in the stratified models (Model 4).
Table 3.
Odds of current smoking, by workplace smoking policy and nativity.
| Model 2 | Model 3 3 | Model 4 | Model 5 | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unstratified model: Main Effect of Policy |
Unstratified model: Nativity Interaction with Policy | Stratified model: US Born |
Stratified model: Foreign Born |
||||||||||||||||
| unweighted sample size --> | n=85,784 | n=85,784 | n=77,561 | n=8,223 | |||||||||||||||
| Variable reported --> | Policy is Not Smokefree |
Policy is Not Smokefree |
Foreign Born | Non Smokefree Policy*Foreign Born Interaction |
Policy is Not Smokefree |
Policy is Not Smokefree |
|||||||||||||
| Mo del |
Variables in model | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | Logit Coeff |
p | OR 2 | OR | (95% CI) | p | OR | (95% CI) | p |
| A | Policy only | 1.77 | (1.69, 1.85) | *** | -- | -- | -- | -- | -- | -- | -- | -- | -- | 1.83 | (1.74, 1.92) | *** | 1.39 | (1.20, 1.61) | *** |
| One variable added at a time. | |||||||||||||||||||
| Demographic/Socioeconomic Variables | |||||||||||||||||||
| B | Policy + Foreign Born | 1.78 | (1.71, 1.87) | *** | 1.83 | (1.74, 1.92) | *** | 0.60 | (0.55, 0.65) | *** | −0.27 | *** | 1.39 | -- | -- | ||||
| C | Policy + Occupation 1,4 | 1.51 | (1.45, 1.58) | *** | 1.55 | (1.48, 1.63) | *** | 0.55 | (0.50, 0.60) | *** | −0.28 | *** | 1.17 | 1.54 | (1.47, 1.62) | *** | 1.26 | (1.07, 1.47) | ** |
| D | Policy + Industry 1,5 | 1.56 | (1.49, 1.64) | *** | 1.60 | (1.52, 1.68) | *** | 0.55 | (0.50, 0.61) | *** | −0.23 | ** | 1.27 | 1.60 | (1.52, 1.68) | *** | 1.27 | (1.09, 1.47) | ** |
| E | Policy + Income 1 | 1.65 | (1.57, 1.72) | *** | 1.69 | (1.61, 1.78) | *** | 0.56 | (0.51, 0.61) | *** | −0.31 | *** | 1.24 | 1.68 | (1.60, 1.77) | *** | 1.33 | (1.14, 1.55) | *** |
| F | Policy + Education 1 | 1.54 | (1.47, 1.61) | *** | 1.58 | (1.50, 1.66) | *** | 0.60 | (0.55, 0.66) | *** | −0.3 | *** | 1.17 | 1.56 | (1.49, 1.64) | *** | 1.32 | (1.13, 1.55) | *** |
| G | Policy + Gender 1 | 1.77 | (1.69, 1.85) | *** | 1.81 | (1.73, 1.90) | *** | 0.59 | (0.54, 0.65) | *** | −0.27 | ** | 1.38 | 1.83 | (1.74, 1.92) | *** | 1.32 | (1.13, 1.54) | *** |
| H | Policy + Race/ethnicity 1 | 1.80 | (1.72, 1.88) | *** | 1.84 | (1.75, 1.93) | *** | 0.72 | (0.66, 0.80) | *** | −0.27 | ** | 1.41 | 1.84 | (1.75, 1.93) | *** | 1.39 | (1.20, 1.61) | *** |
| J | Policy + Marital 1 | 1.76 | (1.69, 1.84) | *** | 1.81 | (1.78, 1.89) | *** | 0.62 | (0.56, 0.68) | *** | −0.25 | ** | 1.41 | 1.81 | (1.72, 1.89) | *** | 1.39 | (1.20, 1.62) | *** |
| K | Policy + Age 1 | 1.78 | (1.70, 1.86) | *** | 1.82 | (1.74, 1.91) | *** | 0.59 | (0.53, 0.64) | *** | −0.28 | *** | 1.38 | 1.83 | (1.74, 1.91) | *** | 1.38 | (1.19, 1.60) | *** |
| L | Policy + Interview Language | 1.79 | (1.71, 1.87) | *** | 1.83 | (1.74, 1.92) | *** | 0.60 | (0.54, 0.66) | *** | −0.27 | ** | 1.40 | 1.83 | (1.75, 1.92) | *** | 1.37 | (1.18, 1.60) | *** |
| M | Policy + Immigrant Length of Stay 1,6 | 1.79 | (1.71, 1.87) | *** | -- | -- | -- | -- | 1.39 | (1.19, 1.62) | *** | ||||||||
| State Variables | |||||||||||||||||||
| N | Policy + State Dummies 1 | 1.73 | (1.65, 1.81) | *** | 1.77 | (1.69, 1.86) | *** | 0.65 | (0.59, 0.71) | *** | −0.27 | ** | 1.36 | 1.77 | (1.69, 1.86) | *** | 1.36 | (1.16, 1.59) | *** |
| Multivariate Model Building | |||||||||||||||||||
| P | Policy + all covariates | 1.34 | (1.27, 1.41) | *** | 1.37 | (1.30, 1.44) | *** | 0.71 | (0.56, 0.88) | ** | −0.23 | ** | 1.09 | 1.36 | (1.29, 1.44) | *** | 1.15 | (0.97, 1.35) | # |
p-value: p=<.10
p=<.05
p=<.01
p=<.001
OR = Odds Ratio.
For models 2 & 3, all unstratified models (B-P) also contain the variable Nativity.
Odds ratio for the interaction was calculated as the odds ratio of being in a non-smokefree workplace among foreign born (compared to the foreign born in smokefree workplaces).
For model 3, the odds ratios for the main effect of policy is interpreted as the policy association for the US-born, while the interaction logit coefficient is the differential policy association for the foreign born (on the logit scale).
Occupation was coded in 5 categories: professional specialty; executive administrative & managerial; technicians & related support, sales, and administrative support including clerical; Service; Blue Collar.
Industry was modeled in 8 categories: trade; manufacturing; services; professional and related services; finance, insurance, and real estate; public administration; transportation and communications; agricultural, forestry and fishing, mining, and construction.
Immigrant length of stay was included only in Models 2M and 5M to maintain consistency of the meaning of the nativity variable.
The association between workplace policy and smoking was weaker among immigrants compared to the US-born on average (Table 3,Model 5). The smoking odds ratio for immigrant workers in a non-smokefree environment was only 1.39 in unadjusted models (CI:1.20,1.61, Model 5A) compared to 1.83 among the US-born (Model 4A); this policy-smoking association among immigrants declined to 1.15 (0.97,1.35) but remained significant in fully adjusted models (Model 5P), compared to 1.36 among US-born (4P). Although confounding factors (e.g. occupation, income) reduced the odds ratio between policy and smoking among both the US born and the foreign born, the logit interaction for foreign born was affected little across all models (Model 3), except for industry. Addition of industry to the model did reduce the nativity-policy interaction coefficient by 16% (from −27 in Model 3B to −23 Model 3D). This suggests that some of the weaker policy association for foreign born was due to confounding by industry.
In models stratified by nativity, race/ethnicity and gender, (Model 6,Table 4) we found differential associations between smoking and smoking policy across subgroups. Although most US-Born and immigrant groups experienced beneficial smoking associations of being in smokefree workplaces (Models 6P), the associations for immigrants were generally weaker than the associations observed among the US born. We lastly observed some unexpected inverse effects for foreign-born Black women, and null associations for US-born Asians and black men, and for most immigrant groups.
Table 4.
Odds ratios of current smoking for non-smokefree (vs. smokefree) workplaces, stratified by race/ethnicity, gender, and nativity (Models 6).
| US-Born | |||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Women | Men | ||||||||||||||||||||||||
| NH white women | NH black women | NH asian women | hispanic women | NH white men | NH black men | NH asian men | hispanic men | ||||||||||||||||||
| n=38532 | n=4721 | n=557 | n=2113 | n=27447 | n=2371 | n=432 | n=1388 | ||||||||||||||||||
| Model | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | |
| Unadjusted | 6A | 1.88 | (1.74, 2.03) | *** | 1.51 | (1.24, 1.84) | *** | 1.38 | (0.74, 2.57) | 1.54 | (1.16, 2.03) | ** | 2.01 | (1.89, 2.15) | *** | 1.19 | (0.95, 1.49) | 1.27 | (0.68, 2.37) | 1.71 | (1.26, 2.31) | *** | |||
| Adjusted | 6P | 1.41 | (1.30, 1.52) | *** | 1.37 | (1.10, 1.69) | ** | 1.12 | (0.52, 2.41) | 1.56 | (1.16, 2.08) | ** | 1.45 | (1.34, 1.56) | *** | 1.02 | (0.80, 1.30) | 0.76 | (0.36, 1.61) | 1.42 | (1.04, 1.95) | * | |||
| Foreign Born | |||||||||||||||||||||||||
| Women | Men | ||||||||||||||||||||||||
| NH white women | NH black women | NH asian women | hispanic women | NH white men | NH black men | NH asian men | hispanic men | ||||||||||||||||||
| n=1172 | n=409 | n=1107 | n=1384 | n=1103 | n=327 | n=1085 | n=1636 | ||||||||||||||||||
| OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | OR | (95% CI) | p | ||
| Unadjusted | 6A | 0.95 | (0.62, 1.46) | 0.21 | (0.01, 3.21) | 1.98 | (1.01, 3.89) | * | 1.27 | (0.75, 2.14) | 1.74 | (1.19, 2.55) | ** | 0.39 | (0.13, 1.23) | 1.72 | (1.19, 2.47) | ** | 1.27 | (0.95, 1.69) | |||||
| Adjusted | 6P | 0.76 | (0.51, 1.15) | 0.09 | (0.01, 0.85) | * | 1.97 | (0.96, 4.07) | # | 1.30 | (0.75, 2.24) | 1.27 | (0.84, 1.93) | 0.35 | (0.08, 1.47) | 1.49 | (0.98, 2.27) | # | 1.18 | (0.86, 1.63) | |||||
p-value: p<.10
p<.05
p<.01
p<.001
OR = Odds Ratio
NH=Non Hispanic
Unadjusted model includes only workplace smoking policy. Adjusted model includes worksite smoking policy, occupation, industry, age, education, income, marital status. State fixed effects were not included because they made models unstable.
Unweighted sample sizes for each subgroup are listed under the race/gender heading.
DISCUSSION
This study has three principal findings. First, immigrants are less likely to work in jobs where they are covered by a smokefree policy, and this disparity is accounted for by the industries and occupations where immigrants disproportionately work. Second, individuals in non-smokefree workplaces exhibited higher odds of smoking than their counterparts in smokefree workplaces, and ETS policy appeared to be more strongly associated with smoking among the US-born than among immigrants on average. Third, there is heterogeneity of the ETS policy effect with smoking across racial and gender subgroups, signifying that the “average” effect of policy from unstratified models was driven by patterns among US-born whites. We discuss these patterns below.
Our manuscript extends prior literature focusing on workplace smoking policy disparities by race/ethnicity and gender,[6,7,21] to document that immigrants are less likely to be covered by smokefree policies than the US-born on average, and that this disparity is attributable to occupational and industry segregation. Blue collar and service workplaces are less likely to voluntarily enact smokefree policies compared to white collar workplaces. [6] Moreover, clean indoor air policies often exempt jobs with higher concentrations of minorities, e.g. manufacturing jobs [8] or service jobs in restaurants, bars, and hotels.[6,33] Since some workplaces enact their smoking policies based on employee request,[8] doing so may disadvantage employees in industries or occupations dominated by immigrants, since immigrants may be less vocal to advocate for workers’ rights if they are illegal residents and/or not citizens. A voluntary policy regime will therefore be less effective for covering certain minority groups because occupational segregation will induce systematic disparities.
Mandating smokefree workplaces must therefore be a matter of federal policy, rather than relegated to individual states or municipalities, or to voluntary bans by the private sector – the situation which currently describes the US context of tobacco control policy. Such decentralized policy context generates inequalities in smokefree-policy coverage; moreover, when smoking bans are applied across the board nationally, it helps to eliminate race/ethnic and socioeconomic disparities in smokefree workplaces. [34]
We found evidence that tobacco policy exhibits weaker average associations with smoking among foreign-born respondents compared to native born counterparts.[23] Smokefree policies may be more effective for the US-born since they have higher smoking prevalence and consumption than the foreign-born,[35] and these patterns generally held in our study. Among immigrants, other factors may be more influential for smoking than workplace tobacco policy. Family context or cultural norms in an immigrant’s country of origin may play a more important role to influence smoking among immigrants, although we could not test those variables with our data, including family anti-tobacco socialization or norms that smoking is socially unacceptable for women, e.g. among Asian immigrants,[36] gender roles and concomitant access to power or status (e.g. being confined to traditional gender roles),[37] socialization with smoking peers,[38] or the stage of the tobacco epidemic in the sending country.[23,39] Alternately, if immigrants have higher job instability and therefore a shorter duration of coverage by smokefree workplace policies, this may explain their weaker associations with smoking.
Although we posited weaker or null associations among immigrants between workplace tobacco policy and smoking, we did not expect inverse associations, which we found among black immigrant women. We believe that results among black immigrants were due to very small cell sizes (few smokers in non-smokefree workplaces), which is related to the low prevalence of smoking among black immigrants. The heterogeneous policy-smoking associations observed across these demographic subgroups demand further attention in future studies, since our analysis could not sort out the reasons underlying the heterogeneity.
With our data, we could test several hypotheses to explain weaker policy associations with smoking among immigrants. We found immigrant-related variables did not affect policy-smoking associations. We found some evidence that differential industries accounted for 16% of the weaker policy effects among immigrants, but occupational adjustment had little effect on the differential. Adding covariates did, however, reduce the coefficients for the policy main effects, indicating social class and demographic characteristics did confound the association of policy with smoking for both nativity groups. Therefore differential smokefree coverage across certain industries and occupations does contribute to why smokefree policies are associated with current smoking, even if they do not explain the entire association.
Strengths and Limitations
One of the strengths of this analysis is that the CPS data is representative of the US population, which is especially important for examination of health disparities, considering the small populations of some minority/nativity groups. Second, our explicit focus on demographic subgroups builds on the inequality literature aiming to ameliorate disparities in tobacco use and tobacco-related disease. Third, we appropriately accounted for the complex survey design of the CPS by applying survey replicate weights in SUDAAN, which accounted for the differential sampling fractions across states, non-response, and survey-induced clustering.
However, the analysis has several limitations. The cross sectional study design limits the extent to which we may draw causal conclusions. Selection is the most serious threat to validity present in observational studies, although we attempted to minimize this via multiple regression. Selection may confound workplace smoking policy associations with smoking behavior since smokers may be attracted to firms where they can smoke; workplaces with low smoking prevalence may be more likely to enact smokefree policies; or we may misattribute lower smoking to the effect of smoking bans, instead of to other policies or employer-offered programs that may affect smoking.[5,6] However methodologically stronger analyses find that omitted variables do not dramatically alter conclusions from single-equation estimation.[40]
Measurement error may be present in the smokefree policy variable (including because it was self-reported) or occupation-related variables (e.g. duration of employment in smokefree workplaces, or differential enforcement of policies in immigrant workplaces), and such mismeasurement could have been differential by nativity or by smoking status.
With the increasing diversity of the US, understanding smoking patterns and tobacco-control policy disparities among racial minorities and immigrant groups will be crucial for ameliorating smoking disparities.
ACKNOWLEDGEMENTS AND FUNDING
Financial support for this study was provided to Dr. Osypuk by a 2-year Association of Schools of Public Health (ASPH) and American Legacy Foundation (Legacy) STEP-UP to Tobacco Control Dissertation Grant L2010-02. Dr. Acevedo-Garcia was supported by National Cancer Institute grant 1 R03 CA093198-01 and a grant from the ASPH and Legacy (L4002-01/03; Dolores Acevedo-Garcia, PI). The conclusions do not necessarily represent the views of ASPH, Legacy Foundation, Legacy Foundation staff, or Legacy's Board of Directors. Dr. Subramanian was supported by the National Institutes of Health Career Development Award (National Institute Heart Lung and Blood Institute, 1 K25 HL081275). Results from parts of this manuscript were presented at the National Tobacco or Health Conference, May 5, 2005, Chicago IL, as well as at “STEP UP to Tobacco Control: Advancing the Role of Public Health and Public Health Professionals” Meeting, April 14–16, 2004, St. Louis, MO.
Footnotes
"The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive license (or non exclusive for government employees) on a worldwide basis to the BMJ Publishing Group Ltd and its Licensees to permit this article to be published in Journal of Epidemiology & Community Health editions and any other BMJPGL products to exploit all subsidiary rights, as set out in our license (http://jech.bmj.com/ifora/licence.pdf)"
REFERENCES
- 1.U.S. DHHS. Washington DC: U.S. DHHS, Public Health Service, Centers for Disease Control; The Health Consequences in Involuntary Smoking. A Report of the Surgeon General. 1986
- 2.National Cancer Institute. Bethesda, MD: U.S. Department of Health & Human Services; Health Effects of Exposure to Environmental Tobacco Smoke: A Report of the California Environmental Protection Agency, Smoking and Tobacco Control, Monograph 10. 1999
- 3.U.S. Department of Health & Human Services. Washington, DC: Government Printing Office; Healthy People 2010: Understanding and Improving Health. 2000
- 4.CDC. State-Specific Prevalence of Current Cigarette Smoking among Adults and Attitudes about Secondhand Smoke -- United States 2000. MMWR. 2001;50:1101–1106. [PubMed] [Google Scholar]
- 5.Farrelly MC, Evans WN, Sfekas AES. The impact of workplace smoking bans: results from a national survey. Tob Control. 1999;8:272–277. doi: 10.1136/tc.8.3.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gerlach K, Shopland D, Hartman A, et al. Workplace smoking policies in the United States: results from a national survey of more than 100,000 workers. Tob Control. 1997;6:199–206. doi: 10.1136/tc.6.3.199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sweeney CT, Shopland DR, Hartman AM, et al. Sex differences in workplace smoking policies: results from the current population survey. Journal of the American Medical Womens Association. 2000;55:311–315. [PubMed] [Google Scholar]
- 8.Aakko E, Schafer E, Gyarmathy V, et al. Smoking policies in manufacturing and assembly workplaces, Wisconsin 1999. Wis Med J. 2001;100:67–69. [PubMed] [Google Scholar]
- 9.Pirkle JL, Bernert JT, Claudill SP, et al. Trends in the Exposure of Nonsmokers in the U.S. Population to Secondhand Smoke: 1988–2002. Environmental Health Perspectives. 2006;114:853–858. doi: 10.1289/ehp.8850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Smelser N, Wilson W, Mitchell F. American Becoming: Racial Trends and their Consequences. Volumes I and II. Washington DC: National Academy Press; 2001. [Google Scholar]
- 11.Kagawa-Singer M. From genes to social science: impact of the simplistic interpretation of race, ethnicity, and culture on cancer outcome. Cancer. 2001;91:226–232. doi: 10.1002/1097-0142(20010101)91:1+<226::aid-cncr9>3.0.co;2-1. [DOI] [PubMed] [Google Scholar]
- 12.Caraballo RS, Giovino GA, Pechacek TF, et al. Racial and ethnic differences in serum cotinine levels of cigarette smokers: Third National Health and Nutrition Examination Survey, 1988–1991. JAMA. 1998;280:135–139. doi: 10.1001/jama.280.2.135. [comment] [DOI] [PubMed] [Google Scholar]
- 13.Wong MD, Shapiro MF, Boscardin WJ, et al. Contribution of Major Diseases to Disparities in Mortality. N Engl J Med. 2002;347:1585–1592. doi: 10.1056/NEJMsa012979. [DOI] [PubMed] [Google Scholar]
- 14.Dixon D. The Second Generation in the United States. Migration Policy Institute; 2006. [Google Scholar]
- 15.U.S. Census Bureau. 2005. Washington, DC: American Community Survey, Table R0501: Percent of People Who Are Foreign Born: 2005. 2006
- 16.Rumbaut RG, Foner N, Gold SG. Immigration and immigration research in the United States. American Behavioral Scientist. 1999;42:1258–1263. [Google Scholar]
- 17.Capps R, Fortuny K, Fix M. Trends in the Low-Wage Immigrant Labor Force, 2000–2005. Washington, DC: The Urban Institute; 2007. p. 9. [Google Scholar]
- 18.U.S. Department of Commerce, Economics and Statistics Administration, Bureau of the Census. We the American Foreign Born (Report #WE-7) US Census Bureau; 1993. [Google Scholar]
- 19.Grieco E. Migration Policy Institute Immigration Facts. Washington DC: Migration Policy Institute; 2004. Immigrant Union Members: Numbers and Trends; p. 8. [Google Scholar]
- 20.Grieco E. Migration Policy Institute Immigration Facts. Washington DC: Migration Policy Institute; 2004. Health Insurance Coverage of the Foreign BOrn in the United States: Numbers and Trends; p. 9. [Google Scholar]
- 21.Shavers VL, Fagan P, Jouridine Alexander LA, et al. Workplace and home smoking restrictions and racial/ethnic variation in the prevalence and intensity of current cigarette smoking among women by poverty status, TUS-CPS 1998–1999 and 2001–2002. J Epidemiol Community Health. 2006;60:ii34–ii43. doi: 10.1136/jech.2006.046979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shavers VL, Lawrence D, Fagan P, et al. Racial/ethnic variation in cigarette smoking among the civilian US population by occupation and industry, TUS-CPS 1998–1999. Preventive Medicine. 2005;41:597–606. doi: 10.1016/j.ypmed.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 23.Acevedo-Garcia D, Pan J, Jun H-J, et al. The effect of immigrant generation on smoking. Social Science & Medicine. 2005;61:1223–1242. doi: 10.1016/j.socscimed.2005.01.027. [DOI] [PubMed] [Google Scholar]
- 24.Jackson C, Henriksen L. Do as I say: Parent smoking, antismoking socialization, and smoking onset among children. Addictive Behaviors. 1997;22:107–114. doi: 10.1016/0306-4603(95)00108-5. [DOI] [PubMed] [Google Scholar]
- 25.Hoving C, Reubsaet A, de Vries H. Predictors of smoking stage transitions for adolescent boys and girls. Preventive Medicine. 2007;44:485–489. doi: 10.1016/j.ypmed.2007.02.011. [DOI] [PubMed] [Google Scholar]
- 26.Weden MM, Astone NM, Bishai D. Racial, ethnic, and gender differences in smoking cessation associated with employment and joblessness through young adulthood in the US. Social Science & Medicine. 2006;62:303–316. doi: 10.1016/j.socscimed.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 27.U.S. Census Bureau. Current Population Survey, June 2001, November 2001, And February 2002: Tobacco Use Supplement File Technical Documentation CPS-02. Washington DC: U.S. Census Bureau; 2002. [Google Scholar]
- 28.Unicon Research Corporation. CPS Utilities Software. Tobacco Use Supplement. 2001–02 [Google Scholar]
- 29.Trosclair A, Husten C, Pederson LL, et al. Cigarette Smoking Among Adults. Morbidity and Mortality Weekly Report. 2002;51:642–645. [PubMed] [Google Scholar]
- 30.Bang KM, Kim JH. Prevalence of Cigarette Smoking by Occupation and Industry in the United States. American Journal of Industrial Medicine. 2001;40:233–239. doi: 10.1002/ajim.1094. [DOI] [PubMed] [Google Scholar]
- 31.Giovino GA, Pederson LL, Trosclair A. The Prevalence of Selected Cigarette Smoking Behaviors by Occupational Class in the United States. Presented at the Organized Labor, Public Health, and Tobacco Control Policy Conference.2000. [Google Scholar]
- 32.Shopland DR, Gerlach KK, Burns DM, et al. State-Specific Trends in Smoke-Free Workplace Policy Coverage:The Current Population Survey Tobacco Use Supplement, 1993–1999. J Occup Environ Med. 2001;43:680–686. doi: 10.1097/00043764-200108000-00005. [DOI] [PubMed] [Google Scholar]
- 33.Maryland Occupational Safety and Health. COMAR 09.12.23 and Chapter 5, Acts of 1995 Maryland Occupational Safety and Health. Baltimore, MD: 1995. Prohibition on Smoking in an Enclosed Workplace - Compliance Guidelines for the Hospitality Industry. [Google Scholar]
- 34.Edwards R, Thomson G, Wilson N, et al. After the smoke has cleared: evaluation of the impact of a new national smoke-free law in New Zealand. Tob Control. 2008;17:e2. doi: 10.1136/tc.2007.020347. [DOI] [PubMed] [Google Scholar]
- 35.Baluja KF, Park J, Myers D. Inclusion of Immigrant Status in Smoking Prevalence Statistics. Am J Public Health. 2003;93:642–646. doi: 10.2105/ajph.93.4.642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Averbach AR, Lam D, Lam L-P, et al. Smoking behaviours and attitudes among male restaurant workers in Boston's Chinatown: a pilot study. Tob Control. 2002;11 doi: 10.1136/tc.11.suppl_2.ii34. 34ii-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hu S. Osypuk PCwT. ed. Chicago, IL: 2005. [Google Scholar]
- 38.Georgiades K, Boyle MH, Duku E, et al. Tobacco use among immigrant and nonimmigrant adolescents: individual and family level influences. Journal of Adolescent Health. 2006;38:443. doi: 10.1016/j.jadohealth.2005.02.007. e1-e7. [DOI] [PubMed] [Google Scholar]
- 39.Lopez AD, Collishaw NE, Piha T. A descriptive model of the cigarette epidemic in developed countries. Tob Control. 1994;3:242–247. [Google Scholar]
- 40.Evans WN, Farrelly MC, Montgomery E. Do workplace smoking bans reduce smoking? The American Economic Review. 1999;89:728–747. [Google Scholar]