Abstract
An efficacious intervention that results in young people living with HIV (YPLH) reducing their transmission risk has been identified. The present study identifies who is most likely to benefit from the intervention. Regression models were used to examine whether background contextual factors moderated the intervention’s success. Percentage of protected sex was moderated by ethnicity, use of antiretroviral medications (ARV), healthcare utilization and mental health. Number of partners was moderated by anxiety and depression. When deciding if an intervention is appropriate and beneficial for an individual young person, consideration must be given to type of services the youth currently accesses and the youth’s mental health.
Keywords: HIV prevention, Youth living with HIV, Intervention
Introduction
Data from the Centers for Disease Control and Prevention (CDC) indicate that despite a decline in the incidence of AIDS among young people, a comparable decline in the number of new HIV infections has not occurred (CDC, 2002). There are currently 33,093 identified AIDS cases among adolescents and young adults (ages 13–24) (CDC, 2001). An additional 27,937 youth who live in areas of the United States that participate in the anonymous HIV surveillance system have been diagnosed with HIV (CDC, 2001). These numbers do not include HIV-positive youth who live in places not participating in the HIV surveillance system, nor do they include youth who are unaware of their seropositive status. Consequently, estimates indicate that between 110,000 and 250,000 youth in the United States are HIV infected (Rotheram-Borus and Futterman, 2000).
While many adults and youth who test positive for HIV reduce their transmission risk, many do not (Crepaz & Marks, 2002; Murphy et al., 2001; Rotheram-Borus et al., 2001; Sturdevant et al., 2001). Given the rising rates of HIV infection among young people, it is clear that secondary prevention targeting HIV-positive youth is needed to reduce transmission of the virus (Rotheram-Borus, O’Keefe, Kracker, & Foo, 2000). A successful intervention for young people living with HIV (YPLH) has shown efficacy in reducing the number of sexual partners, increasing the percentage of protected sexual acts, and increasing disclosure of HIV-positive status to sexual partners (CLEAR intervention) (Rotheram-Borus et al., 2004).
Once an efficacious intervention has been identified, it is important to examine any differential impact of the intervention. Oftentimes an examination of an intervention’s success ends at the outcome analysis. However, in order to facilitate dissemination and inform decision-making regarding the implementation of the intervention, it is important to investigate the factors that moderated the intervention’s impact. This paper will examine the characteristics of the YPLH that influenced the intervention’s success.
The intervention was delivered in either telephone or individual in-person individual sessions. Individual sessions were used as an alternative delivery modality to the traditional small-group implementation of many HIV-prevention interventions. The strengths of an individualized intervention include the ability for it to be implemented by a variety of paraprofessionals in a variety of settings (outpatient medical clinics, sexually transmitted diseases clinics, adolescent health clinics, primary health care clinics). In addition, HIV seroincidence has been reduced by providing individual counseling to serodiscordant couples (de Vincenzi,1994; Padian, O’Brien, Chang, Glass, & Francis, 1993) and STDs have been lowered by interventions delivered in individual sessions (see Rotheram-Borus et al.,1997 for a review). Individual sessions allow the content of the intervention to be tailored to the risk profile of the youth. There are also fewer scheduling problems and the pace of intervention delivery can be tailored, increasing the likelihood that all intervention sessions will be delivered.
Providing intervention via the telephone addresses many of the challenges encountered in conducting traditional small-group, in-person groups. Telephone sessions reduce the wait time for enrolling enough youth to form a group, allow anonymity, reduce transportation and scheduling problems, and reduce the chance of engaging in peer-induced negative behaviors. Telephone sessions offered the youth potential for successfully intervening with seropositive youth, particularly if youth live in rural settings or are, at times, too ill to attend interventions in person.
Telephone-delivered interventions have been successfully used for smoking prevention (Demers, Neale, Adams, Trembath, & Herman, 1990; Ershoff, Quinn, & Mullen, 1995; Rimer et al., 1994) and outreach counseling for battered women (Rubin, 1991). In addition, Roffman and colleagues (Picciano, Roffman, Kalichman, Rutledge, & Berghius, 2001; Roffman, Beadnell, Ryan, & Downey, 1995; Roffman, Picciano, Wickizer, Bolan, & Ryan, 1998) have demonstrated that gay men will participate in telephone interventions with significant reductions in risk acts over time. Therefore, a telephone intervention is a viable means for engaging seropositive young people.
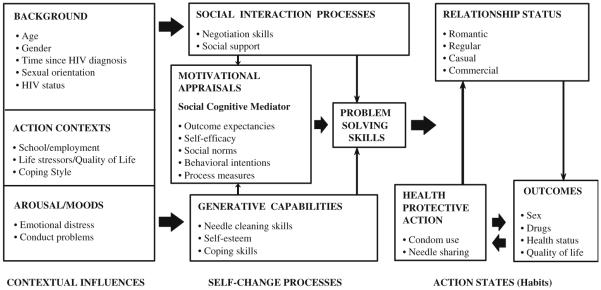
The conceptual basis guiding the intervention is the Social Action Theory (Ewart, 1991, Fig. 1). Social Action Theory postulates that health protective action is a product of three influences: (1) contextual influences (i.e., background variables, action states, and arousal/moods), (2) self-change processes (i.e., social interaction processes, motivational appraisals, problem solving skills, and generative capabilities), and (3) action states (i.e., relationship status and health protective action). While an individual is conceptualized to possess a number of contextual influences such as age and emotional distress, the intervention was developed to target the self-change processes by building skills such as problem-solving and negotiation and addressing motivational factors such as outcome expectancies and self-efficacy.
Fig. 1.
Conceptual framework for an HIV-preventive intervention for youth living with HIV. Note. Modified from “Social Action Theory for a Public Health Psychology,” by C. K. Ewart, 1991, American Psychologist, 46(9), 931–946
While Rotheram-Borus and colleagues (2004) found that the in-person delivery of the intervention was more successful than the telephone delivery, it remains unclear for which youth the telephone or individual sessions worked best or the contexts in which the intervention worked best. Identifying the factors that moderate the success of the intervention is crucial in the dissemination and implementation of any program in a health care or community setting. This paper examines who was most likely to benefit from the intervention and from which delivery modality. Consequently, we examine how those factors that the intervention did not directly target (the contextual influences of background, action contexts and affective arousal states) effect or moderate the intervention’s success.
Method
From 1999 to 2002, 175 YPLH aged 16 to 29 years (26% African American, 42% Latino; 69% gay young men; Table 1) were recruited with voluntary informed consent in Los Angeles, San Francisco, and New York City (Rotheram-Borus et al., 2004). Across cities, YPLH were recruited from medical providers, social service agencies, needle-exchange programs, a drug-treatment center, other research studies, outreach on the street or at special events, and through newspaper advertisements and word-of-mouth. Parental consent was obtained for non-emancipated YPLH under age 18 years. YPLH were randomly assigned to three intervention conditions: (1) a 18-session intervention delivered by telephone, (2) a 18-session intervention delivered in-person, or (3) a delayed-intervention condition where youth did not receive intervention until the completion of their final follow-up assessment.
Table 1.
Baseline characteristics of YPLH by randomly assigned intervention condition
| Telephone (n = 59) % (n) |
In-person (n = 61) % (n) |
Delayed (n = 55) % (n) |
Totala (n = 175) % (n) |
|
|---|---|---|---|---|
| Site | ||||
| Los Angeles | 49% (29) | 51% (31) | 47% (26) | 49% (86) |
| New York | 34% (20) | 33% (20) | 38% (21) | 35% (61) |
| San Francisco | 17% (10) | 16% (10) | 15% (8) | 16% (28) |
| Median age (range) | 23 (16–29) | 23 (16–29) | 22 (17–29) | 23 (16–29) |
| Percent male | 71% (42) | 84% (51) | 78% (43) | 78% (136) |
| Ethnicity | ||||
| Latino | 37% (22) | 46% (28) | 44% (24) | 42% (74) |
| African American | 29% (17) | 26% (16) | 24% (13) | 26% (46) |
| White | 27% (16) | 21% (13) | 22% (12) | 23% (41) |
| Other ethnicities | 7% (4) | 7% (4) | 11% (6) | 8% (14) |
| Have AIDS | 21% (12) | 21% (13) | 26% (14) | 23% (39) |
| HIV symptomatic | 59% (33) | 56% (34) | 51% (28) | 55% (95) |
| ARV medication use | 53% (30) | 51% (31) | 45% (25) | 50% (86) |
| Median CD4 count (range) | 487 (56–1500) | 415 (0–1007) | 555 (22–1128) | 489 (0–1500) |
| Median number of sex partners (range) | ||||
| All sex partners | 1 (0–52) | 1 (0–200) | 1 (0–50) | 1 (0–200) |
| HIV + | 0 (0–15) | 0 (0–140) | 0 (0–34) | 0 (0–140) |
| HIV − | 1 (0–49) | 1 (0–196) | 1 (0–49) | 1 (0–196) |
| Median percent protected sex acts (range) | ||||
| All sex partners | 70.8 (0–100) | 78.3 (0–100) | 62.3 (0–100) | 74.2 (0–100) |
| HIV+* | 53.7 (0–100) | 18.8 (0–100) | 33.3 (0–100) | 29.2 (0–100) |
| HIV− or unknown status partners** | 95.0 (0–100) | 100 (0–100) | 96.0 (0–100) | 100 (0–100) |
| 100% condom use or abstinent | 55% (31) | 56% (34) | 44% (24) | 52% (89) |
| Emotional distress | 1.1 (0–3.8) | 1.2 (.1–2.5) | 1 (.1–3.6) | 1 (0–3.8) |
P < .05
P < .01
n = 173 (n = 57 for telephone) for all measures except site, gender, ethnicity, and age
Procedures
A full description of the study procedures are reported elsewhere (Rotheram-Borus et al., 2004). The intervention consisted of three modules of six sessions each and each session was approximately 2 h long. A detailed manual (available online at http://chipts.ucla.edu/) guided the three intervention modules. YPLH received $10 for each session attended. Intervention sessions were delivered either in-person or via the telephone. The in-person sessions were delivered one-on-one in private rooms available at collaborating sites or other community agencies. Telephone sessions were delivered one-on-one at times and locations convenient for participants. The participant provided a contact phone number for each session.
Module 1 focused on improving health regimens, particularly utilization and adherence to ARV. In addition, the module addressed coping with learning one’s serostatus, implementing new daily routines to stay healthy, issues of disclosure, and participation in health care decisions. Module 2 aimed to reduce unprotected sexual acts and substance use by asking YPLH to identify situations that are likely to elicit risky acts and to adjust their patterns of substance use, as well as increase their skills in condom use self-efficacy, and negotiation skills. Module 3 aimed to reduce emotional distress and to improve the quality of life of YPLH.
For youth randomized into the intervention conditions, 78% (n = 94/120) of young people attended at least one session. YPLH receiving individual sessions completed over half of the 18 sessions (M = 10.0 sessions) whereas in the telephone condition almost half of all sessions were completed (M = 7.5 sessions).
Measures
Retention was high and similar across sites and intervention conditions as YPLH were assessed at 3 months (86%), 6 months (78%), 9 months (86%), and 15 months (82%) after baseline. Each interview lasted approximately 2 h and all YPLH received an incentive of $20 to $25 per assessment. Young people were individually interviewed at a site convenient to them. An ethnically diverse team of trained interviewers assisted by collecting data using audio-computer assisted self-interview (ACASI) assessments. For all assessment domains, activities reported for the previous 3 months are defined as “recent” behaviors.
Main Outcome Variable
Sexual Risk Acts
Using a structured interview protocol (Meyer-Bahlburg, Ehrhardt, Exner, Gruen, 1988), youth reported the total number of partners and sexual acts, specific sexual acts with each partner, and whether condoms were used during each of these sexual acts. A sexual partner was defined as a male or female with whom the youth engaged in vaginal or anal sex. A sexual act was defined as a single session of receptive or insertive vaginal or anal sex. Oral sex was reported, but omitted in all calculations of risk because of its low association with HIV transmission (Carlin, Miller, &Fiano, 1994; Rozenbaum, Gharakhanian, Cardon, Duval, & Couland, 1988). Based on the extensive sexual history data obtained, the following indices were derived: (a) the number of sexual partners and (b) the proportion of vaginal and anal sex acts protected by condoms with all partners and with HIV-negative partners (or partners of unknown status).
Potential Modifying Variables
Based on the theoretical model underpinning the intervention design, those constructs that formed the basis for contextual influences were examined as potential modifying variables.
Background
Demographics
Age of YPLH at each assessment was calculated from youths’ report of their birth date. Youth also reported their main racial or ethnic group, and gender.
Time Since HIV Diagnosis
Youth reported in years and months the time since they learned of their HIV diagnosis.
HIV Health Status
YPLH reported: (1) whether or not symptoms of HIV had been experienced; (2) whether or not AIDS had been diagnosed; (3) medication status: Lifetime and recent antiretroviral medication (ARV) utilization was assessed and categorized as [1] present or [0] not; and (4) health behaviors: positive health behaviors (Rotheram-Borus et al., 2001) documented the frequency of engaging in 12 behaviors to maintain health at least once a week: [1] yes or [0] no (e.g., balanced diet, exercise, vitamins, adequate sleep).
Action Context
Quality of Life
The HIV/AIDS Targeted-QOL scale (HAT-QOL; Holmes and Shea, 1997) was used to measure quality of life. The measure includes 11 items rated on a 1 to 5 scale (all to none of the time) along two domains: being HIV positive (3 items, α = .54) and general life satisfaction (8 items, α = .90).
Coping Style
Coping style was measured with a modified 39-item version of the Dealing with Illness Inventory (Namir, Wolcott, Fawzy, & Alumbaugh, 1987; Murphy, Rotheram-Borus, & Marelich, 2003). The measure asks how often particular coping strategies are used to help deal with knowing that one is HIV positive during the previous three months. The response code was a five point Likert scale (1 = never to 5 = always). Factor analysis resulted in seven subscales that were categorized as positive or negative coping. Positive coping included the subscales of positive action (10 items, α = .87), social support (5 items, α = .76), and spiritual hope (4 items, α = .74). Negative coping included the subscales of depression/withdrawal (5 items, α = .68), self-destructive escape (5 items, α = .81), non-disclosure/problem avoidance (4 items, α = .65), and passive problem solving (6 items, α = .77).
Arousal/Moods
Mental Health
The Brief Symptom Inventory (Derogatis, 1993), a 53-item, reliable index of global severity of mental health symptoms, was administered (α = .97 at baseline). Participants rated the level of severity for each symptom during the previous week on a scale from 0 (not at all) to 4 (extremely). In addition to a global index, three subscales were examined: somatization, depression, and anxiety. Scores are reported as the mean response of the subscale items.
Statistical Methods
The findings of the intervention have been reported elsewhere (Rotheram-Borus et al., 2004). Outcomes included an examination of behavior with all sexual partners, as well as with partners in which transmission of a new HIV infection was possible (i.e., sexual partners whose HIV status was negative or unknown to the participant). In summary, those who experienced the intervention significantly increased the percent of protected sexual acts with their sexual partners and reduced the number of sex partners. In the current analysis, we examined effect modification of the intervention by baseline measures on the intervention outcomes relating to sexual behavior. Guided by the theoretical framework, those constructs that formed the basis of contextual influences were examined as potential modifying variables. Logistic, linear, and Poisson regression models were fit to binomial, continuous, and count outcomes, respectively. In addition to the potential modifying variable, each model included: covariates for time (measured in months), intervention condition, time by intervention condition interaction, time by modifier interaction, intervention condition by modifier interaction, and time by intervention condition by modifier interaction. We report F statistics for significant three-way interactions to indicate effect modification and conduct multiple comparison tests to examine which intervention conditions effect modification occurred between. For continuous measures, we report t-tests for significant multiple comparison tests. For categorical moderators, we report t statistics for multiple comparison tests at levels of the moderator they are significant for. We present interaction plots of estimated outcomes over time by intervention condition and moderator level. For continuous moderators we specify the levels to be the 10th and 90th percentiles of the effect modifiers’ sample distributions to amplify where effect modification is occurring.
Similar to the original data analytic strategy, an Auto-regressive Moving Average (ARMA) covariance structure to account for correlation between repeated measurements over time was used. The ARMA covariance structure provided the best model fit. Analysis was conducted using the SAS Proc Mixed procedure for continuous data and SAS GLIMMIX macro for discrete outcomes.
Due to the large number of regression models, we expected to find a number of significant results just by chance, also known as the multiple testing problem. Consequently, while all intervention condition differences that are significant are reported, we focus our discussion on differences that were significant across at least several regression models. In addition, examination of the correlation matrix (Table 2) found moderating variables of quality of life and negative coping to be highly correlated with emotional distress. However, other moderating variables were not correlated, suggesting independent moderation effects.
Table 2.
Correlations between moderators at baseline
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | 1 | |||||||||||||||
| Male vs Female | 0.14 | 1 | ||||||||||||||
| Black ethnicity | −0.11 | −.24** | 1 | |||||||||||||
| Hispanic ethnicity | −0.03 | 0.1 | − | 1 | ||||||||||||
| Time since HIV diagnosis |
.21** | −0.11 | −0.06 | 0.09 | 1 | |||||||||||
| HIV symptoms | .15* | −0.02 | −0.07 | 0.02 | 0.12 | 1 | ||||||||||
| HAART use | −0.003 | −0.14 | 0.08 | 0.05 | 0.002 | 0.06 | 1 | |||||||||
| QofLa, HIV+ | 0.07 | 0.06 | −0.08 | −0.02 | .23** | −0.05 | 0.05 | 1 | ||||||||
| QofLa, gen life satisfaction |
−0.1 | 0.08 | 0.08 | 0.01 | 0.06 | −0.12 | .17* | .31** | 1 | |||||||
| Positive coping | −0.1 | 0.12 | 0.06 | 0.02 | −0.1 | 0.01 | .28** | 0.03 | .40** | 1 | ||||||
| Negative coping | −0.14 | 0.08 | 0.05 | −0.01 | −.22** | 0.07 | −0.09 | −.42** | −.33** | .27** | 1 | |||||
| BSI GSI | 0.09 | 0.03 | −0.06 | −0.05 | −.15* | 0.12 | −0.06 | −.33** | −.53** | 0.02 | .63** | 1 | ||||
| BSI anxiety | 0.12 | 0.08 | −0.12 | −0.03 | −.17* | 0.09 | −0.09 | −.30** | −.41** | 0.08 | .57** | .88** | 1 | |||
| BSI depression | 0.11 | 0.03 | 0.003 | −0.05 | −.15* | 0.1 | −0.03 | −.34** | −.60** | −0.05 | .57** | .85** | .73** | 1 | ||
| BSI somatization | 0.1 | 0.07 | −0.1 | −0.05 | −0.06 | .17* | −0.11 | −.21** | −.38** | 0.1 | .44** | .81** | .70** | .60** | 1 | |
| Conduct disorder | −0.14 | 0.07 | −0.12 | −0.003 | 0.01 | 0.09 | −0.07 | −0.13 | −.17* | −0.03 | .32** | .43** | .38** | .33** | .32** | 1 |
P < .05
P < .01
Quality of Life
Results
Outcome: Protected Sex Acts
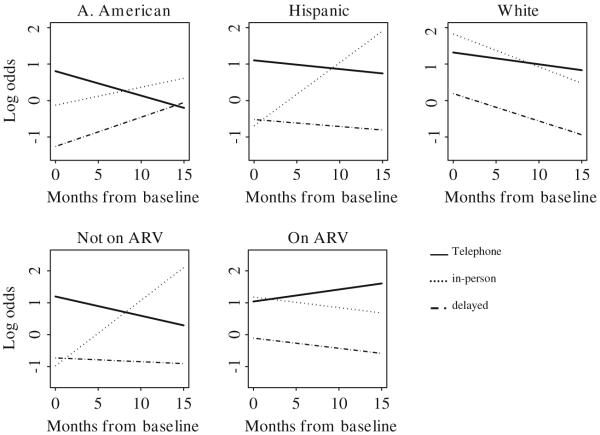
As shown in Fig. 2, ethnicity significantly modified the fraction of protected sex acts with all sexual partners, F(4, 374) = 2.93, P = .02, and HIV-negative sexual partners, F(4, 258) = 2.95, P = .02, over time. The fraction of protected acts with all sexual partners and with HIV-negative sexual partners increased over time in the in-person condition compared to the delayed condition among Hispanics, t(374) = 3.30, P < .01 and t (258) = 3.69, P < .01, respectively. The fraction of protected acts with all sexual partners and with HIV-negative partners increased over time in the in-person condition, compared to the telephone condition, among Blacks, t(374) = 1.93, P = .05, and t(258) = 1.95, P = .05, respectively, and Hispanics, t(374) = 2.09, P < .05, and t(258) = 3.42, P < .01. Therefore, the in-person condition was more successful in reducing transmission risk over time than the telephone condition for Hispanics.
Fig. 2.
Log odds of percent of protected sex acts with HIV-negative partners by ethnicity and ARV use
YPLH use of ARV at baseline also significantly modified the fraction of protected sex acts with all partners, F(2, 375) = 13.26, P < .01, and HIV-negative partners, F(2, 259) = 10.69, P < .01, over time. Participants on ARV in the telephone condition compared to the delayed condition, t(375) = 1.99, P < .05, and compared to the in-person condition, t(375) = 2.45, P < .05, increased their fraction of protected sex acts with all partners over time; significant intervention condition differences were not found for the fraction of protected sex acts with HIV-negative partners over time. Participants not on ARV in the in-person condition compared to the delayed condition, t(375) = 2.48, P < .05, and compared to the telephone condition, t(375) = 4.75, P < .01, increased their fraction of protected sex acts with all sexual partners over time; the same time trends were found for participants not on ARV between intervention conditions for the fraction of protected sex acts with HIV-negative partners, t(259) = 3.30, P < .01, and t(259) = 5.02, p < .01, respectively. Consequently, the telephone condition was more successful for participants on ARV and the in-person condition was more successful for participants not on ARV.
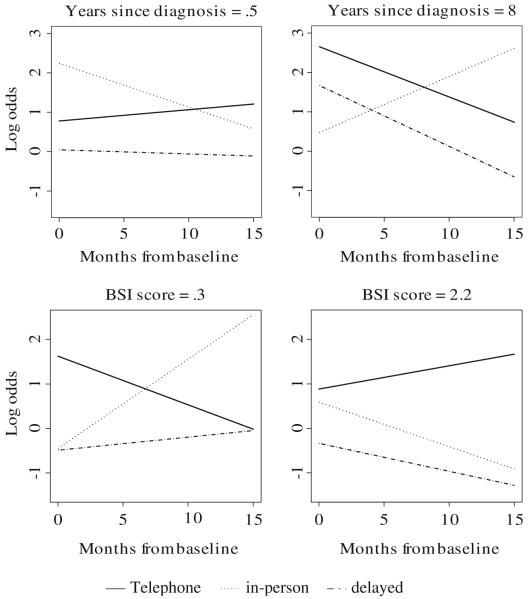
As shown in Fig. 3, mental health was also a significant modifier of the fraction of protected sex acts with all partners, F(2, 375) = 4.01, P < .05, and HIV-negative partners, F(2, 259) = 9.36, P < .01, over time. For youth with higher scores on the BSI global, the telephone condition compared to the in-person condition resulted in increases of protected sex acts with all partners, t(375) = 2.79, P < .01, and HIV-negative partners, t(259) = 4.24, P < .01, over time. For youth with higher scores on the BSI global, the telephone condition compared to the delayed condition, t(259) = 2.84, P < .01, and the delayed condition compared to the in-person condition, t(259) = 2.06, P < .05, resulted in increases of protected sex acts with HIV-negative partners over time. Likewise, in the delayed condition, t(375) = 2.56, P < .05, and telephone condition, t(375) = 4.31, P < .01, compared to the in-person condition, youth with high levels of anxiety increased the fraction of protected sex acts for all partners, F(2, 375) = 9.35, P < .01, over time; time trends were similar for the fraction of protected acts with HIV-negative partners, t(259) = 2.64, P < .01; t(259) = 4.48, P < .01; and F(2, 259) = 10.15, p < .01, respectively. YPLH in the telephone condition compared to the delayed condition, t(259) = 2.49, P < .05, also increased the percentage of protected sex acts with HIV-negative partners over time. YPLH reporting high levels of depression also reported increases over time in the fraction of protected sex acts for HIV-negative partners, F(2, 259) = 4.47, P = .01; significant differences were not found for the fraction of protected sex acts with all partners. YPLH in the telephone condition compared to the delayed condition, t(259) = 2.61, P < .01, and compared to the in-person condition, t(259) = 2.37, P < .05, increased the fraction of protected sex acts with HIV-negative sexual partners over time. Therefore, the telephone condition was more successful for youth who were more generally emotionally distressed.
Fig. 3.
Log odds of percent of protected sex acts with HIV-negative partners by the log number of years since diagnosed with HIV and BSI mean scores, dichotomized at the 10th and 90th percentiles of the sample distribution
Time from HIV diagnosis was a significant modifier of the fraction of protected sex acts with all partners, F(2, 375) = 14.38, P < .01, and HIV-negative partners, F(2, 259) = 16.72, P < .01, over time. YPLH who reported knowing their HIV status longer in the in-person condition compared to the delayed condition, t(375) = 5.17, P < .01, and compared to the telephone condition, t(375) = 3.90, P < .01, increased the fraction of protected sex acts with all partners over time; time trends were similar for the fraction of protected sex acts with HIV-negative partners: t(259) = 5.08, P < .01, and t(259) = 4.61, P < .01, respectively.
Outcome: Number of Sex Partners
The change in the number of sex partners over time between intervention conditions was modified by the BSI global for all partners, F(2, 559) = 3.17, P = .04, and HIV-negative partners, F(2, 549) = 5.61, P < .01. Anxiety also modified the reduction in the number of sexual partners for all partners, F(2, 559) = 5.91, P < .01, and HIV-negative partners, F(2, 549) = 5.93, P < .01). YPLH reporting lower BSI global and anxiety levels in the in-person condition compared to the delayed condition, t(559) = 2.33, P < .05, and t(559) = 3.33, P < .01, respectively, increased the number of sexual partners over time. YPLH reporting lower BSI global and anxiety levels in the telephone condition compared to the delayed condition, t(549) = 2.07, P < .05, and t(549) = 2.25, P < .05, respectively, and in the in-person condition compared to the delayed condition, t(549) = 3.12, P < .01, and t(549) = 3.09, P < .01, respectively, increased the number of HIV-negative partners over time.
Discussion
The initial intervention trial (Rotheram-Borus et al., 2004) was aimed at designing an efficacious intervention to reduce transmission risk and examining whether the delivery format for an intervention makes a difference. This question is particularly important as care providers for this population design and implement programs to improve the health and mental health outcomes, as well as reduce the transmission risk behaviors of this population. Overall, the trial found that the in-person delivery of the intervention resulted in more healthy behavior changes among young people living with HIV. However, it was unclear if this was always the case, or if there were contexts or individuals who would benefit more from the telephone sessions. Given the probable differential costs in delivering the interventions (e.g., convenience, access, transportation, etc.), it is important to determine who is likely to benefit from which delivery modality.
Increasing the amount of condom protected sex that young people living with HIV engage in is an important strategy for reducing HIV transmission risk. When examining the factors that moderate increasing the percentage of protected sex, use of antiretroviral medications (ARV), time since HIV diagnosis, and mental health were important. YPLH who were not taking ARVs, reported lower emotional distress, and had know their HIV diagnosis for a longer period of time were more likely to benefit from the in-person intervention. The in-person intervention appears to be most effective for those youth who may be most difficult to engage in prevention and healthcare services. These youth are likely to be difficult to engage because they are not highly motivated by their current context to seek, help as illustrated by not taking medications, not needing mental health services and having lived with the virus for a long time. However, while difficult to engage, these youth can benefit from preventive interventions. Therefore, increasing the motivation of these youth to attend in-person sessions is crucial. Emphasizing the benefits of in-person sessions, for example, the opportunity to decrease isolation, make a personal connection with someone else, and the opportunity to discuss life challenges with others, are possible techniques for increasing the motivation of youth to attend in-person sessions.
In contrast, while youth not on ARVs and youth that knew their HIV status for longer benefited from the in-person intervention, they did not appear to benefit from the telephone intervention. Given these youth may not be highly motivated to seek help and more difficult to engage, providing services via the telephone is problematic. These youth are likely to be less attentive and engaged by telephone discussions. One of the primary benefits of in-person sessions is the opportunity to personally connect, which is not easily accomplished over the telephone. Further, in an in-person intervention, the personal relationship is fostered by the facilitators’ ability to read the affect of a youth and employ engagement strategies accordingly. This is much more challenging to do over the telephone.
Those YPLH who were taking ARVs and reporting more emotional distress were more likely to benefit from the telephone intervention. YPLH taking medications for their HIV are actively involved in healthcare settings. It might be expected that these youth are more likely to receive preventive information compared to those not regularly seeing their healthcare provider. Consequently, prevention for these youth could easily be overlooked. However, these data suggest that remaining in contact with these youth and providing preventive interventions is important and beneficial when delivered via the telephone. In addition, youth who are emotionally distressed may be more difficult to engage and may not benefit from interventions that require them to come in to an office. It is important to realize that while these youth may not come into an office because of their mental health issues, they can still benefit from intervention that is provided via the telephone.
In contrast, while the telephone intervention was useful for youth recently diagnosed and those taking ARVs, these youth did not benefit from the in-person intervention. This is surprising because it would be expected that recently diagnosed youth would be most in need of in-person communication and interaction. However, recently diagnosed youth may be experiencing heightened affect such as depression or anxiety which could interfere with their ability to engage in an interpersonal setting. This is consistent with the finding that YLPH with heightened emotional distress benefited most from the telephone intervention. It is less clear why those youth taking ARVs did not benefit from the in-person intervention. These youth are already engaged in healthcare settings and are presumably interacting with providers on a one-on-one basis. It may be these youth are overwhelmed or overloaded by the ongoing in-person interaction and conveying preventive information may require less interpersonally demanding modalities.
When examining reductions in the number of sexual partners, these data suggest that mental health status is an important consideration for the success of the intervention. For YPLH who were experiencing high levels of emotional distress or anxiety, the in-person intervention was most effective in reducing the number of sexual partners. However, low levels of emotional distress did not significantly moderate reductions in the number of sexual partners. It appears that the in-person intervention is most beneficial in reducing number of sexual partners for YPLH experiencing high levels of mental distress. This finding contrasts with the results indicating YPLH experiencing high levels of emotional distress benefited from telephone delivery to increase the percentage of protected sex. It may be that for YPLH who become connected to healthcare services or interventions delivered in-person, they reduce contact with potential sex partners. On the other hand, emotionally distressed youth who are not connected to services and who benefit from telephone delivered intervention may seek social support and continue to have sex partners; however, with intervention, they may increase the percentage of protected sex with those partners.
A number of variables were not significant moderators for any of the major intervention outcomes, including age, coping skills, conduct problems, or quality of life. Given that the focus of the intervention included increasing HIV-specific coping and medication adherence, which would positively impact health indicators such as quality of life, these variables may have been mediators rather than moderators of the interventions success. The intervention may have had a positive impact on YPLH by increasing positive coping skills and increased health behaviors, producing mediating rather than moderating effect. Alternatively, both negative coping and quality of life were highly correlated with emotional distress, suggesting these variables were not independent moderators of the effects of the intervention. It would appear that emotional distress exerted the stronger effect on intervention efficacy. In addition, there appears to be a lack of intervention effect for black and white youth. However, this finding is likely due to a lack of power given the small sample size.
The current analysis had several limitations. The main technique for data collection was self-report. Although the self-report outcome of sexual risk acts is subject to demand of social desirability, this potential threat was countered by assurances of confidentiality, careful construction of assessment items, and use of ACASI, as recommended by the National Institutes of Health. There are background characteristics, such as socioeconomic status, that were not included in the analysis that may have moderated the intervention’s success. Unfortunately, this analysis is limited by the data that were collected. While the demographics of our sample closely reflect those of reported AIDS cases in the United States, the sample was not probability-based and was conducted in only three U.S. cities. Thus, generalizability is difficult to assess.
Regardless of these limitations, this analysis provides important knowledge. The intervention was successful in decreasing transmission behavior among YPLH, and illustrates that different delivery strategies are viable. When deciding which delivery strategy is most appropriate and beneficial for an individual young person, consideration must be given to the types of services the youth currently accesses and the youth’s mental health. This research supports the importance of continuing to examine the best modality for engaging youth in prevention activities. While traditional in-person sessions are the most common means of providing services and may be the most beneficial for some youth, in-person sessions may not be the most effective way to provide prevention services for everyone. Further research is needed to examine the possible contexts in which intervention works best.
Acknowledgments
This research was supported by Grant R01 DA-07903 from the National Institute on Drug Abuse.
References
- Carlin E, Miller L, Fiona B. The hazards of oral sex. Sexually Transmitted Disease. 1994;21:241–242. doi: 10.1097/00007435-199407000-00013. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control, Prevention . HIV/AIDS Surveillance Report. 2. Vol. 13. Centers for Disease Control and Prevention; Atlanta, GA: 2001. pp. 1–44. [Google Scholar]
- Centers for Disease Control and Prevention Cases of HIV infection and AIDS in the United States, 2002. HIV/AIDS Surveillance Report. 2002;14 Retrieved May 10, 2005, from http://www.cdc.gov/hiv/stats/hasr1402.htm.
- Crepaz N, Marks G. Towards an understanding of sexual risk behavior in people living with HIV: A review of social, psychological, and medical findings. AIDS. 2002;16(2):135–149. doi: 10.1097/00002030-200201250-00002. [DOI] [PubMed] [Google Scholar]
- Demers RY, Neale AV, Adams R, Trembath C, Herman SC. The impact of physicians’ brief smoking cessation counseling: A MIRNET study. Journal of Family Practice. 1990;31:625–629. [PubMed] [Google Scholar]
- Derogatis LR. Brief symptom inventory: Administration, scoring, and procedures manual. National Computer Systems, Inc.; Minneapolis, MN: 1993. [Google Scholar]
- de Vincenzi I. A longitudinal study of human immunodeficiency virus transmission by heterosexual partners. New England Journal of Medicine. 1994;331:341–346. doi: 10.1056/NEJM199408113310601. [DOI] [PubMed] [Google Scholar]
- Ershoff DH, Quinn VP, Mullen PD. Relapse prevention among women who stop smoking early in pregnancy: A randomized clinical trial of a self-help intervention. American Journal of Preventive Medicine. 1995;11:178–184. [PubMed] [Google Scholar]
- Ewart CK. Social action theory for a public health psychology. American Psychologist. 1991;46(9):931–946. doi: 10.1037//0003-066x.46.9.931. [DOI] [PubMed] [Google Scholar]
- Holmes WC, Shea JA. Performance of a new, HIV/AIDS-targeted quality of life (HAT-QoL) instrument in asymptomatic seropositive individuals. Quality of Life Research. 1997;6:561–571. doi: 10.1023/a:1018464200708. [DOI] [PubMed] [Google Scholar]
- Meyer-Bahlburg HFL, Ehrhardt AA, Exner TM, Gruen RS. Sexual risk behavior assessment schedule–youth. New York State Psychiatric Institute and Department of Psychiatry, College of Physicians and Surgeons of Columbia University; New York: 1988. [Google Scholar]
- Murphy DA, Durako SJ, Moscicki AB, Vermund SH, Ma Y, Schwarz DF, Muenz LR, The Adolescent Medicine HIV/AIDS Research Network No change in health risk behaviors over time among HIV infected adolescents in care: Role of psychological distress. Journal of Adolescent Health. 2001;29S:57–63. doi: 10.1016/s1054-139x(01)00287-7. [DOI] [PubMed] [Google Scholar]
- Murphy DA, Rotheram-Borus MJ, Marelich WD. Factor structure of a coping scale across two samples. Journal of Applied Social Psychology. 2003;33:627–647. [Google Scholar]
- Namir S, Wolcott DL, Fawzy FI, Alumbaugh MJ. Coping with AIDS: Psychological and health implications. Journal of Applied Social Psychology. 1987;17:309–328. [Google Scholar]
- Padian NS, O’Brien TR, Chang Y, Glass S, Francis DP. Prevention of heterosexual transmission of human immunodeficiency virus through couple counseling. Journal of Acquired Immune Deficiency Syndromes. 1993;6:1043–1048. [PubMed] [Google Scholar]
- Picciano JF, Roffman RA, Kalichman SC, Rutledge SE, Berghuis JP. A telephone based brief intervention using motivational enhancement to facilitate HIV risk reduction among MSM: A pilot study. AIDS and Behavior. 2001;5:251–262. [Google Scholar]
- Rimer BK, Orleans CT, Fleisher L, Cristinzio S, Resch N, Telepchak J, Keintz MK. Does tailoring matter? The impact of a tailored guide on ratings and short-term smoking-related outcomes for older smokers. Health Education Research. 1994;9(1):69–84. doi: 10.1093/her/9.1.69. [DOI] [PubMed] [Google Scholar]
- Roffman RA, Beadnell B, Ryan R, Downey L. Telephone group counseling in reducing AIDS risk in gay and bisexual males. Journal of Gay and Lesbian Social Services. 1995;2:145–157. [Google Scholar]
- Roffman RA, Picciano J, Wickizer L, Bolan M, Ryan R. Anonymous enrollment in AIDS prevention telephone group counseling: Facilitating the participation of gay and bisexual men in intervention research. Journal of Social Services Research. 1998;23:5–22. [Google Scholar]
- Rotheram-Borus MJ, Futterman DA. Promoting early detection of human immunodeficiency virus infection among adolescents. Archives of Pediatric and Adolescent Medicine. 2000;154:435–439. doi: 10.1001/archpedi.154.5.435. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Lee MB, Murphy DA, Futterman D, Duan N, Birnbaum JM, Lightfoot M, Teens Linked to Care Consortium Efficacy of a preventive intervention for youths living with HIV. American Journal of Public Health. 2001;91:400–405. doi: 10.2105/ajph.91.3.400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Murphy DA, Coleman CL, Kennedy M, Reid HM, Cline TR, Birnbaum JM, Futterman D, Levin L, Schneir A, Chabon B, O’Keefe Z, Kipke M. Risk acts, health care, and medical adherence among HIV+ youths in care over time. AIDS and Behavior. 1997;1:43–52. [Google Scholar]
- Rotheram-Borus MJ, O’Keefe Z, Kracker R, Foo H. Prevention of HIV among adolescents. Prevention Science. 2000;1:15–30. doi: 10.1023/a:1010071932238. [DOI] [PubMed] [Google Scholar]
- Rotheram-Borus MJ, Swendeman D, Comulada WS, Weiss RE, Lee M, Lightfoot M. Prevention for substance-using HIV-positive young people: Telephone and in-Person delivery. Journal of Acquired Immune Deficiency Syndromes. 2004;37:S68–S77. doi: 10.1097/01.qai.0000140604.57478.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozenbaum W, Gharakhanian S, Cardon B, Duval E, Couland JP. HIV transmission by oral sex. Lancet. 1988;1:1395. doi: 10.1016/s0140-6736(88)92205-2. [DOI] [PubMed] [Google Scholar]
- Rubin A. The effectiveness of outreach counseling and support groups for battered women: A preliminary evaluation. Research on Social Work Practice. 1991;1(4):332–357. [Google Scholar]
- Sturdevant MS, Belzer M, Weissman G, Friedman LB, Sarr M, Muenz LR. The relationship of unsafe sexual behavior and the characteristics of sexual partners of HIV infected and HIV uninfected adolescent females. Journal of Adolescent Health. 2001;29S:64–71. doi: 10.1016/s1054-139x(01)00286-5. [DOI] [PubMed] [Google Scholar]