Abstract
Congruence between preferred and actual place of death may be an essential component in terminal care. Most patients prefer a home death, but many patients do not die in their preferred location. Specialized (physician, hospice and palliative) home care visits may increase home deaths, but factors associated with congruence have not been systematically reviewed. This study sought to review the extent of congruence reported in the literature, and examine factors that may influence congruence. In July 2009, a comprehensive literature search was performed using MEDLINE, Psych Info, CINAHL, and Web of Science. Reference lists, related articles, and the past five years of six palliative care journals were also searched. Overall congruence rates (percentage of met preferences for all locations of death) were calculated for each study using reported data to allow cross-study comparison. Eighteen articles described 30% to 91% congruence. Eight specialized home care studies reported 59% to 91% congruence. A physician-led home care program reported 91% congruence. Of the 10 studies without specialized home care for all patients, seven reported 56% to 71% congruence and most reported unique care programs. Of the remaining three studies without specialized home care for all patients, two reported 43% to 46% congruence among hospital inpatients, and one elicited patient preference “if everything were possible,” with 30% congruence. Physician support, hospice enrollment, and family support improved congruence in multiple studies. Research in this important area must consider potential sources of bias, the method of eliciting patient preference, and the absence of a single ideal place of death.
Keywords: Place of death, decision-making, terminal care, palliative care, systematic review
Introduction
Honoring a patient’s choice for place of death has been identified as an essential component in terminal care.1, 2 Congruence is the agreement between a patient’s stated preferred place of death and actual place of death.3 In general population studies of preference, 50–90% of respondents preferred to die at home.4–6 In place of death studies, 10–35% of patients died at home, and 50–60% died in hospitals.7–9 Thus, there may be low levels of congruence between preferred and actual place of death.3, 10
Factors associated with home deaths have been identified in some studies.3, 11–15 A systematic literature review of place of death for cancer patients grouped these factors as environmental, individual and illness-related.16 Environmental factors included health care characteristics (use of home care and availability of inpatient beds), geographic characteristics and social support. Individual factors included patient demographic variables and preferences. Illness factors included tumor type, length of disease and functional status. However, factors associated with congruence have not been systematically reviewed and compared across studies.
Health care and geographic factors have demonstrated stronger associations with place of death than patient preference.10 Actual use of health care resources has previously demonstrated a more powerful influence on place of death than availability of health care resources.3, 10 Receiving physician, hospice, and palliative care home visits have been associated with increased likelihood of home death,12, 16–19 and hospice home care services have been associated with improved congruence between preferred and actual place of death.3 Since the majority of patients prefer home deaths,4–6, 20 these specialized home visit programs would be expected to enhance congruence between preferred and actual home deaths.
This study sought to examine the environmental, individual, and illness factors associated with congruence. First, congruence rates were compared across studies by examining the presence or absence of these factors in the sample populations. Given the importance of health care utilization and home care, the relationship between specialized (including palliative, hospice or physician-led) home care services and congruence was explored. Since studies have demonstrated that the majority of patients prefer home deaths, it was hypothesized that studies with systematic provision of specialized home care would report higher levels of congruence than studies in which these services might be available but not systematically provided to all study patients. Second, the factors associated with congruence among patients within the individual studies were compiled and compared. The results of this review may suggest ways to enhance congruence between preferred and actual place of death.
Methods
Search Strategy
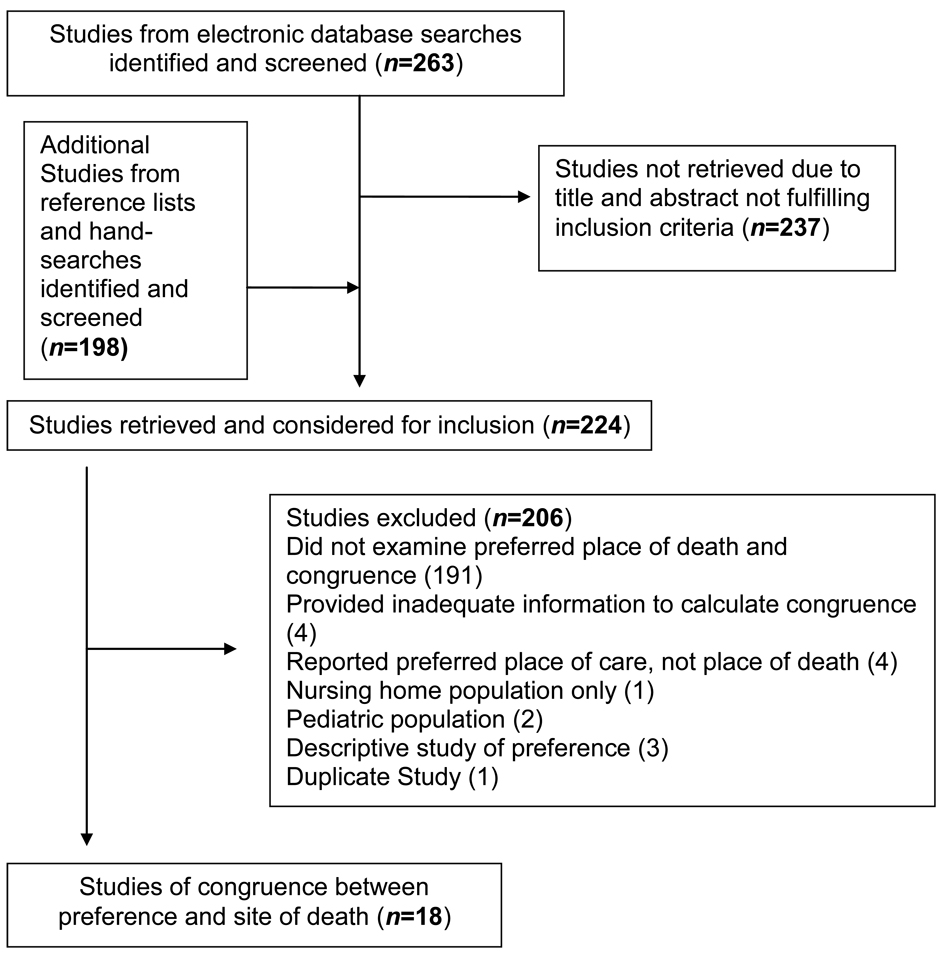
In July 2009, we searched four electronic databases (Medline (1950-present), CINAHL(1983-present), PsychInfo (1987-present) and Web of Science (1980-present)) using the following Medical Subject Heading (MeSH) terms and free text terms: (choice or preference or decision or wish) AND (palliative OR terminal OR end-of-life OR hospice OR elderly OR aged) AND (care or death) AND (place OR location OR site). Reference lists and related articles in Medline were also examined. In addition, indices of the past five years of six palliative care journals were hand-searched. A flowchart of the inclusion and exclusion of studies is shown in Figure 1. Articles were included if they quantitatively compared adult patients’ preferred place of death and actual place of death. Articles which did not report either congruence, or both patients’ preferred place of death and actual place of death, were excluded. Four studies were excluded because preference for place of care was elicited rather than place of death,21–24 as these have been shown to be different outcomes.14 One study which focused exclusively on nursing home patients was excluded.25 In order to compare congruence across as many types of services possible, all studies reporting congruence were included regardless of whether congruence was the primary or secondary purpose of the study. Non-English language articles, methodological reports, editorials, review articles, and case reports were also excluded.
Figure 1.
Flow of studies through review process.
Analysis
Each article was reviewed and the following data were extracted and systematically entered into a matrix table: study purpose, study design and methods, actual place of death, preferred place of death, congruence, sample population characteristics, services described, factors associated with congruence (if reported), and grade of study. The factors associated with congruence for individual patients within the studies, when reported, were grouped according to a model of factors associated with place of death for cancer patients: environmental factors, individual factors, and illness-related factors.16
Comparison of congruence between studies was hampered by four different possible definitions of congruence used in the literature.26 The level of congruence varied significantly depending on the definition of congruence used,26 60% versus 100% in one study.27 This review required comparison of congruence across all locations of death, rather than only home deaths. Overall congruence has been proposed as a single, standard method of reporting congruence to permit cross-study comparison, and consists of the total number of patients whose preferences were met for all locations of death divided by the total number of patients with preferences in the study.26 Overall congruence was reported in nine studies.3, 12, 14, 19, 28–33 Nine other studies reported congruence separately by location of death,10, 17, 18, 27, 34–37 and overall congruence was calculated using the reported data from these studies. In five studies, not all the information was provided to calculate an overall congruence rate that included all possible locations of death. In these cases, congruence for home death was used, 18, 35–37 except for one study which reported congruence for hospital death.10 Kappa statistics for agreement between preferred and actual death were reported in three studies3, 14, 29 and have been proposed as another measure to facilitate cross-study comparison.3, 26 However, inadequate information was provided to determine kappa statistics in 11 studies10, 12, 17–19, 28, 31, 33, 35–37 precluding use of kappa statistics for comparison in this review.
In order to examine the effect of systematic provision of specialized home care on congruence, the studies were placed into two groups depending on the source of the patient sample: patients who universally received specialized home care, and patients who did not universally receive specialized home care. Specialized home care studies were defined as those studies which recruited patients exclusively from physician, palliative, or hospice interdisciplinary home care programs with continuity or coordination of care. The second group of studies recruited patients from other sources, including community palliative care providers or oncologists, hospitals and outpatient study sites, and death certificates and mortality databases. In the second group, specialized home care services may have been available, but universal provision to all patients was not described by these studies.
The studies were graded using quality measures defined previously for preference survey studies.4 These criteria were modified slightly to accommodate the non-survey, prospective studies included in this review: Grade A (strong evidence): longitudinal study with standardized systematic and predefined assessment of preference for place of terminal care or death, more than 80% response rate if survey study, patients not limited to those within one service, (e.g., one palliative care team); Grade B (moderate evidence): longitudinal study that does not meet criteria for A, cross-sectional, observational or retrospective study, more than 60% response rate (if survey study), standardized and systematic assessment of preference for place of terminal care or death; and Grade C (weak evidence): response rate less than 60% or not given if survey study, or inconsistent assessment of preferences.
Results
Characteristics of Studies
Eighteen articles met all the inclusion criteria and were included in the final set of articles reviewed. Nine studies focused on congruence specifically3, 14, 27–32, 34 and nine examined preference as one of many factors associated with place of death.10, 12, 17–19, 33, 35–37 Seven studies were from the U.S.,3, 10, 12, 19, 28, 30, 35 three were from the U.K.,27, 33, 34 and four were from Canada.17, 18, 32, 37 Australia,14 Sweden,36 Taiwan29 and Italy31 each had one study included.
Table 1 summarizes the descriptions, source populations, patient characteristics, service characteristics, home preference, overall congruence, and grade for each study.
Table 1.
Descriptions, Patient and Service Characteristics, Preferences, Congruence, and Grades of Included Studies
| Study Description | Source Population | Patient Diagnosis & Living/ Caregiver Situation |
IDT Home Care with Continuity For all in Study? |
Palliative or Hospice |
Patients Preferring Home (%) |
Congruence (%)a | Grading of Study |
|---|---|---|---|---|---|---|---|
| Agar et al.14 2002–2004 Australia Regional community palliative program, n=71 | Convenience sample (71/320) prospective trial of palliative care outreach. Patients who died within study period with known preferred place of care and death at least twice. | 92% cancer, 14% lived alone | Yes | Palliative | 35% | 59% | A |
| Thomas et al.27 2000–2002 England Terminal cancer patients, n=41 | Terminal cancer patients referred by palliative care professionals in the community (41/69 commenced and 17/69 completed the interview series). | 100% cancer, 41% lived alone | Not described | Specialist palliative care, 73% hospice (inpatient or day care) | 24% b | 71% c | A |
| Pritchard et al.10 1989–1991 5 U.S. teaching hospitals (SUPPORT Study), n=479 | All deaths of patients from observational phase of SUPPORT: survived initial hospitalization, known preferred and actual site of death, subsequent death within 6-month follow-up. | N/A | Not described | Not described d | 82% | 46% for hospital preference only e | A |
| Tang & McCorkle3 2001–2002 Connecticut 6 study sites Terminal cancer patients, n=127 | Convenience sample of terminally ill cancer patients at six study sites in New Haven and Hartford counties in Connecticut. | 100% cancer, 26.8% lived alone | Not described | Not described, 60.6% with high availability of hospice care providers | 87% | 30% | A |
| Leff et al.30 1995–1998 Baltimore, MD Physician-led house call program, n=125 | All patients in Elder House Call Program in a geographically defined catchment area surrounding Johns Hopkins Bayview Medical Center in southeast Baltimore, Maryland. | 36% cancer, 90% had in-home caregiver | Yes, physician-led | No; excluded inpatient hospice patients | 83% | 91% | B, single service |
| Groth-Juncker & McCusker35 1977–1982 New York Physician home health care, n=100 | All home health care team patients followed from referral to death. | 42% cancer, 10% lived alone | Yes, physician-member | No | 68% | 72% home death preference only e | B, single service |
| Brazil et al.32 2000–2002 Canada In-home care service, n=216 | Caregivers of decedents who had received in-home palliative care services through a Community Care Access Center.f | 96% cancer, 6% lived alone | Yes | Palliative | 63% | 70% | B, 70% response rate |
| McWhinney et al.17 1988–1990 Ontario, Canada Palliative Care Home Support Team (PCHST), n=150 | All referred patients (PCHST) who died at home (75/267 referred during study period), and 75 patients randomly chosen out of 192 team patients who died in the hospital. | 93% cancer, 15% lived alone | Yes | Palliative | 39%g | 67% | B, single service |
| Cantwell et al.18 2000 Canada Palliative home care coordinator service, n=73 | Patients consecutively admitted to 10 recruited palliative home care coordinators in the Edmonton region over study period. | 95% with cancer, 67% > 1 caregiver | Yes | Palliative | 56% h | 66% for home preference only e | B, single service |
| Shega et al.12 2000–2001 U.S. Geriatric clinic, n=135 | Caregivers of community-dwelling dementia patients of University of Chicago geriatrics clinics who died during study period. | 100% dementia, 66% lived with caregiver | Not described (home visits were clinic visit alternative) | 43% hospice | N/A | 66% (90% hospice group, 45% non-hospice group) | B, single service; 89% response rate |
| Beccaro et al.31 2000–2002 Italy Population survey of patients who died of cancer, n=1900 | Nationwide, two-stage probability sample mortality follow back caregiver interviews (Italian survey of the dying of cancer). Caregivers of patients who died at home were more likely to participate in interview. | 100% cancer, caregiver interview | No | Services more frequent in North; scarce in South | 94% | 67% | B, 66.9% response rate |
| Hsieh et al.29 2007 Taiwan Palliative care hospital unit, n=46 | Convenience sample of inpatients in the palliative care unit of a metropolitan Taipei hospital. | 100% cancer, 91% lived with caregivers | Not described | Inpatient palliative home services available | 74% | 43% | B, single unit |
| Brazil et al.37 1997–1999 Canada Community palliative care, n=151 | Home palliative care nursing service. | 82% cancer, 86% lived with caregiver | Yes | Palliative | 62% i | 80% for home preference only e | C, 51% response rate |
| Gyllenhammar et al.36 1999 Sweden Palliative home care teams, n=221 | Caregivers of all deceased incurable cancer patients of five palliative home care teams. | 100% cancer, 24% lived alone | Yes | Palliative | 37%j | 77% for spontaneously expressed home preference only e | C, preference not assessed consistently |
| Karlsen & Addington-Hall33 1995–1996 England Cancer death certificates, n=229 | Random sample of cancer deaths. | 100% cancer, caregiver interview | No k | 44% palliative | 73% | 63% | C, 53% response rate |
| Tolle et al.28 1996–1997 Oregon Adult non-traumatic deaths, n=475 | Random sample of adult non-violent deaths (475 of 1458 from random sample). | 24% cancer, caregiver interview | No | 34% used hospice | N/A | 68% | C, 59% response rate |
| Koffman & Higginson34 1999–2000 London Caribbean and UK-born white patients from Death Registry, n=100 | Family caregivers of all black Caribbean ethnicity decedents in inner-London area and stratified random sample of native-born white patients as comparison group. | 69% cancer, caregiver interview | Not described | Not described | 81% | 56% | C, 45–47% response rate |
| Bakitas et al.19 1999–2001 U.S. Outpatient palliative care, n=125 | Consecutive patients with advance family contact persons of deceased patients with breast, gastrointestinal or lung cancer who had participated in Project ENABLE. l | 100% cancer, 73% were married | Not described | Palliative | N/A | 66% | C, 47% response rate |
Overall congruence was calculated using data provided in the studies by dividing the number of subjects with met preferences for any location of death by the number of subjects with a preferred location of death. This overall congruence differed from some studies’ reported congruence value, as many studies reported the met preferences for home death divided either by the number of home deaths or the number of preferences for home death.
In this study, an additional 22% of subjects preferred either home or hospice.
Preference met in this study was reported by place of death, not overall congruence. The study reported home death congruence as 60% (6/10 subjects) and 100% for hospice deaths (4/4subjects). Overall congruence is 6+4/14 = 71%.
Provided information on prognosis to patients and clinicians and provided a highly trained nurse to facilitate communication and to improve pain control.
Data not provided to calculate overall congruence for all locations of death.
CCAC: Community Care Access Center: publicly funded, coordination of services, home palliative care, nursing, social work, personal support, housekeeping, therapy, dietary, equipment.
An additional 16% of patients preferred to die at home “conditional on family’s ability to cope.”
This study reported desire for home death by both the patient and the caregiver; 30/68 patients and caregivers did not both desire home death.
Preference reported as percentage of patients who preferred home death and percentage of patients who did not prefer a home death, not as percentages of patients preferring each site of death.
Percentage of patients who spontaneously expressed a wish to die at home. No other elicitation of preference was reported.
Forty-four percent of caregivers reported palliative care nursing home visits, 47% had community nurse home visits, 9% had GP nurse home visits, and 7% had other nurse home visits. These visits were not mutually exclusive.
Project ENABLE: an outpatient palliative care early intervention demonstration quality improvement project implemented at two oncology care settings.
Grades of Studies and Congruence
Four prospective studies were graded A level. 3, 10, 14, 27 Eight studies were graded B level because of retrospective design, response rates less than 80%, or single service populations.12, 17, 18, 29–32, 35 Six studies were graded C level because of response rates less than 60% or inconsistent assessment of preferences.19, 28, 33, 34, 36, 37 There was no clear trend between level of congruence and grade of study, although the A and B grade studies had wider ranges of overall congruence (30% to 71%, and 43% to 90%, respectively) than the grade C studies (56% to 68%). Two grade C studies reported only home congruence, 77%36 and 80%,37 which is difficult to compare with overall congruence. No grade C studies had less than 50% congruence.
Environmental Factors and Congruence
Specialized Home Care and Congruence
Eight studies were placed in the specialized home care group, with interdisciplinary home care programs and continuity or coordination of care.14, 17, 18, 30, 32, 35–37 Ten studies were placed in the comparison group, and recruited patients from a variety of other sources, including hospital and outpatient sites,3, 10, 12, 29 community palliative care providers and oncologists,19, 27 and death certificates or mortality databases.28, 31, 33, 34 No included studies exclusively sampled hospice patients, and nine studies exclusively sampled palliative care patients. Two studies sampled patients from physician-led home care programs.30, 35
Among the A grade studies, Thomas et al. reported the highest congruence level (71%) and examined specialist palliative care patients who were not all receiving home care (comparison group).27 Agar et al. examined a specialized palliative home care program and reported 59% congruence.14 The lowest congruence (30%) was reported in Tang and McCorkle’s study3 of Connecticut patients who were not all receiving home care (comparison group).
Among the B grade studies, the highest congruence level (91%)30 was reported by a physician-led specialized home care program study. Beyond this study, however, there was not a clear difference between levels of congruence among studies in the specialized home care group and the comparison group. Two Canadian specialized home care programs17, 32 reported similar congruence levels (70% and 67%) to comparison group studies by Shega et al. (66%)12 and Beccaro et al. (67%).31 Shega et al. studied dementia patients followed by the University of Chicago geriatrics clinics in an extension of the PEACE (Palliative Excellence in Alzheimer Care Efforts) program.38 Beccaro et al.’s Italian nationwide probability sample interview study of cancer decedents’ caregivers included more caregivers of patients who died at home than in hospitals.
Among the C grade studies, it was difficult to compare the congruence levels between specialized home care studies and the comparison group. The two specialized home care studies, Brazil et al.37 and Gyllenhammar et al.,36 reported congruence for home deaths only, not overall congruence. The comparison group studies reported congruence levels between 56% and 68%,19, 28, 33, 34 including Bakitas et al.’s study19 of an outpatient palliative care early intervention demonstration project, which reported 66% congruence.
Hospice Utilization and Congruence
Both inpatient and outpatient hospice utilization was associated with higher congruence levels. Thomas et al.’s study reported 71% congruence and 73% of patients had contact with inpatient or day care hospice facilities.27 In Shega et al.’s study, congruence was 90% among patients enrolled in home hospice, and 45% among those not enrolled in home hospice.12 Tolle et al.28 reported 68% congruence in a random sample of all non-violent deaths in Oregon, a U.S. state with higher-than average utilization of hospice. Of the 161 home deaths in the study, 70% reported hospice utilization. In Bakitas et al.’s outpatient palliative care early intervention demonstration project, 81% of patients with congruence used hospice.19
Hospital Availability and Utilization and Congruence
Hospitalized patients had lower levels of congruence. In Tang and McCorkle’s study, patients who received emergency hospital care or lived close to hospitals had lower congruence and patients with congruence had fewer rehospitalizations than patients without congruence.3 Pritchard et al.10 reported 46% congruence for hospital preferences only for SUPPORT study patients from teaching hospitals. Of the patients who preferred home deaths, 55% died in the hospital, but the percentage of patients with congruence for home deaths was not reported. Hsieh et al.’s study29 sampled inpatient palliative care cancer patients and reported 43% congruence. Home death was preferred by 74% of patients but 83% of patients died in the hospital, and attrition was high in this prospective study.
Geographic Factors and Congruence
Geographic areas with higher hospice availability had higher congruence, while areas with higher hospital bed availability had lower congruence. Thomas et al.’s study27 acknowledged a higher than average availability of inpatient hospice beds in Morecambe Bay than in other parts of England. Tang and McCorkle’s study noted that patients who lived in geographic proximity to major hospital centers had lower congruence than patients who lived in areas of lower hospital bed availability.3 Interestingly, Beccaro et al.’s study noted that decedents in areas of the country with fewer hospital and palliative care services had higher rates of home deaths than in areas with greater availability of these services.31
Social Support and Congruence
There was no clear relationship between level of social support reported in the studies and reported congruence levels. Three studies reported that 10% or fewer patients lived alone, and two had higher congruence levels (Leff et al. 91%,30 Groth-Juncker and McCusker 72%,35 Brazil et al. 70%32) while one had a low congruence level (Hsieh et al. 43%29). Three studies reported over 25% of patients lived alone, two with higher congruence levels (Thomas et al. 71%27 and Shega et al. 66%12) and one with the lowest congruence level (Tang and McCorkle 30%3).
Individual Factors and Congruence
Patient Ethnicity
Koffman and Higginson34 sampled all Black Caribbean decedents from an inner-London area and compared congruence with a stratified random sample of native-born white decedents from the area. Overall congruence was 56%, with similar percentages for white and black Caribbean patients. No other studies compared ethnicities and congruence levels.
Preferred Location of Death
In 11 of 18 studies, over 50% of patients preferred home deaths, not including patients without an expressed preference. Four studies reported less than 40% patients who preferred home deaths,14, 17, 27, 36 and three studies did not report percentages of preferences for home death.12, 19, 28 Tang and McCorkle elicited patients’ preferences “if everything were possible” and reported the second highest percentage of preferences for home death (87%), but the lowest congruence of any study (30%).3 Thomas et al. reported 24% of patients preferred home and an additional 22% of patients preferred either home or hospice deaths. Thomas et al. reported high levels of congruence, even when the patients with dual preferences were excluded from congruence calculation.27 McWhinney et al. 17 reported 39% of patients who strongly preferred home deaths and an additional 16% patients preferred home deaths conditional upon families’ ability to cope. In McWhinney et al.’s study, congruence was 67%, not including those with conditional preferences.17 Gyllenhammar et al. reported only the 37% of patients who spontaneously expressed a preference for home death, and did not elicit or report any other preference; the high congruence (77%) in this study was for home only.36 In addition, only three studies reported preferences for every patient in the sample.3, 14, 29 In 13 studies, 18% to 65% of patients did not express a preference for place of death.17, 18, 27, 28, 30–37
Illness Factors and Congruence
There was no clear trend between levels of congruence and the percentage of patients with cancer diagnoses in the studies. In 13 studies, more than 80% of patients had cancer.3, 14, 17–19, 27, 29, 31–33, 36, 37 One study examined dementia patients exclusively,12 and three reported that less than 50% of patients had cancer.28, 30, 35 High levels of congruence were reported in ten of the studies with predominantly cancer patients as well as studies of more mixed populations,12, 28, 30, 34, 35 while two of the studies of cancer patients reported lower levels of congruence.3, 29 Other illness factors were less consistently reported across studies and were not able to be compared.
Study Methods and Congruence
Five studies did not report overall congruence or data to determine overall congruence. 10,18, 35–37 It is unclear in the studies which reported congruence for home deaths only, for example, how many patients preferred and achieved hospital, hospice, or nursing home deaths. Thus, it is difficult to compare these percentages with the rest of the studies. The Thomas et al. and Agar et al. longitudinal studies demonstrated higher congruence rates with final patient wishes than with initial wishes.14, 27
Factors Affecting Congruence
Most of the studies identified factors associated with congruence among individual patients. Table 2 groups these factors as environmental, individual and illness-related, based on the model in Gomes and Higginson’s review of factors associated with cancer home deaths.16 These factors were not mutually exclusive. Several environmental factors improved congruence consistently across studies, including physician support, hospice enrollment, family support and family caregiving ability. Illness-related and environmental factors decreasing congruence consistently across studies included symptom control, rehospitalization, lack of family support, and lack of family caregiving ability. The individual factors, patient characteristics, understanding of illness and resuscitation status, were identified in one study each. Interestingly, preference for inpatient hospice death was associated with increased congruence, while home as the preferred place of death was actually associated with decreased congruence in two studies,27, 31 and was not a factor in other studies.3, 10
Table 2.
Factors Affecting Congruence: Summary of Literature Findings.
| Enhancing Congruence | Decreasing Congruence |
|---|---|
| Environmental Factors | Illness-related Factors |
| Physician support18 | Inability to control symptoms17, 19, 30, 32, 36 |
| Family physician home visits32, 37 | Need for 24-hour nursing care17, 32 |
| Hospice enrollment3, 12, 19, 28 | Unclear prognosis30 |
| Domestic care services33, 36 | Progression/ death prior to admission 17, 30 |
| Palliative home care team36 | Environmental Factors |
| Provision of special equipment 33 | Equipment not available35 |
| More support services17 | Rehospitalization 3, 17, 30, 37 |
| Family caregiver ability3, 37 | Proximity to hospitals3 |
| Family support3, 18, 36 | Hospital palliative care 37 |
| Individual Factors | Individual Factors |
| Hospice as preferred location of death14 | Home as preferred place of death14, 31 |
| Higher social classes33 | Lower patient/ caregiver education levels29 |
| Patient understands illness 36 | Perceived family inability3 17, 29, 35–37 |
| Do Not Resuscitate advance directive30 | Patient changed mind17 |
Discussion
This study systematically reviewed congruence between preferred and actual place of death and examined some of the factors associated with congruence. Overall congruence ranged from 30% to 90%. Within the studies’ reported analyses of individual patients, factors associated with increased congruence included physician support, hospice enrollment and family support, while inadequate symptom control, rehospitalization and lack of family caregiver support decreased congruence. Several of these factors, particularly home care, social support and hospitalization, were noted in a previous systematic review of factors associated with cancer home deaths.16 However, unlike the previous home death review, preference for home death was associated with decreased congruence in at least two studies,27, 31 and preference for inpatient hospice was associated with increased congruence in one study.27
When the overall congruence levels of the studies were compared, environmental factors appeared to be associated with congruence across the studies. Contrary to the hypothesis based on previous studies, studies with systematic provision of specialized home care did not clearly demonstrate higher congruence than the other studies. The studies with specialized palliative home care and physician home care programs30, 35 all reported congruence levels over 59%. Except for the hospital-based studies,3, 10, 29 the studies without specialized home care for all patients reported levels of congruence (56% to 68%) similar to the specialized home care studies (59% to 91%).
Inpatient and home hospice utilization increased congruence in the comparison group, even though not all patients received these services. Thomas et al.27 studied palliative care patients with high utilization of freestanding hospice facilities. Shega et al.12 reported very high congruence (90%) among dementia patients enrolled in hospice compared to those not enrolled in hospice. Bakitas et al. studied an outpatient palliative care demonstration project and noted higher congruence among the hospice patients.19 The study from Oregon28 did not describe special programs or continuity of care, but congruence was most likely enhanced by the state’s high rate of hospice utilization, and 70% of the home deaths had hospice services. The studies by Thomas et al.,27 Shega et al.,12 Bakitas et al.19 and Tolle et al.28 all described a specialized program or level of care beyond usual provision of care. These findings suggest that congruence between preferred and actual place of death is enhanced when patients are given additional skilled care and support in navigating the health care system. This is supported by the studies’ findings that the key factors affecting congruence most consistently in the studies included symptom control, physician support, hospice enrollment, and family support and ability.
Hospitalized patients had lower congruence. Two of the three studies with the lowest congruence rates, the SUPPORT study10 and Hsieh et al.,29 sampled hospital patients. Tang and McCorkle3 reported more rehospitalizations among patients with noncongruence than the patients with congruence.
Geographical factors also played a role in congruence some studies. Thomas et al.27 and Tolle et al.28 noted that regions of higher hospice utilization may have higher congruence levels. Tang and McCorkle3 noted that residence in urban areas with proximity to hospitals reduced congruence. Beccaro et al.31 found higher congruence in areas with lower availability of inpatient hospices and palliative care home services, suggesting that home deaths in some areas may be due to lack of choice.16 The ethnic minority patient caregivers in Koffman and Higginson’s study of inner-London also noted a lack of choice which affected place of death.34
The lowest level of congruence was reported in Tang and McCorkle’s study,3 which elicited preference “if everything were possible.” Comparison of congruence in McWhinney et al.’s and Thomas et al.’s studies excluded patients with conditional17 or dual (“home or hospice”)27 preferences. Gyllenhammar et al.’s study reported only “spontaneously expressed” preferences for home deaths,36 limiting comparison. In order to clearly compare congruence, realistic patient preferences appear to be the most useful.
Overall congruence included patients with place of death matching with preference for hospital, inpatient hospice, and nursing home deaths as well as home deaths. Including all sites of death in congruence avoids the assumption that home deaths are best for every patient. No preference for place of death was expressed by 18% to 65% of patients in 12 of the 18 studies. This is consistent with a previous study which noted heterogeneity in the importance of place of death to terminally ill patients.39 Symptom control, presence of family, and other attributes have been found to be more important to patients than place of death.40
Congruence may have been affected by study methods and designs. It is unclear whether selection bias in retrospective studies, or attrition in prospective studies, affected the congruence. Response rates of the retrospective studies ranged from 46–89%. The Italian retrospective study noted that non-responders were more likely to be caregivers of decedents who died in the hospital, compared to the home.31 This would overestimate the home deaths surveyed and might increase congruence rates for home deaths. Yet some of the prospective studies reported loss of study patients due to attrition,27, 29 which may also result in bias.
The strengths of this study included systematic review methods with clear inclusion and exclusion criteria. The study is limited by the wide heterogeneity of the studies and the different locations of death studied. The study is also constrained by the limited data provided in the original studies. Additional factors enhancing or reducing congruence may have been present but not reported in the original articles. The exclusion of non-English speakers in most U.S., Canadian, and English studies limits generalizability. Additionally, there may be barriers in some settings to asking a patient’s preferred place of death which were beyond the scope of this review.
Implications for Research
Many of the patients in these studies with congruence between preferred and actual place of death did not die at home. Measurements based on a percentage of home deaths alone may not accurately assess the quality of end-of-life care or a model of care’s ability to honor patient preferences. The elicitation of ideal, conditional, or dual site (home or hospice) preferences limits comparison with other studies and interpretation of findings. Both retrospective and prospective study designs have limitations. More study is needed using systematic assessments of preference, and to examine the relationship between congruence and other quality measures of end-of-life care.
Implications for Practice
The key factors affecting congruence most consistently in the studies included symptom control, physician support, hospice enrollment, family support and family caregiving ability. Work to address these areas would likely enhance a care model’s ability to honor patient preferences for place of death. Additionally, providing information and support to help patients understand the demands of dying in a preferred location may improve the congruence between preferred and actual place of death. Home may not be the best location of death for all patients. The best location of death is the one which meets the patient’s needs and is acceptable to the patient and his or her family.
Conclusion
Congruence between preferred and actual place of death is an important goal in end-of-life care. Specialized programs of care and hospice utilization were associated with higher levels of congruence compared to hospital-based programs of care. Geographic variation in hospice and hospital availability affected congruence. Symptom control, physician support, hospice enrollment, and family support are key factors in congruence between patient preferences and place of death. Future studies of congruence should consider potential sources of bias, the method of eliciting patient preference, and the absence of a single ideal place of death.
Acknowledgments
The authors would like to acknowledge Rosanne Harrigan, EdD, APRN-Rx, for her assistance with study concept and design.
This research was supported by: The John A. Hartford Foundation Center of Excellence in Geriatrics, University of Hawaii; and Research Centers in Minority Institutions award 1 R25 RR019321 from the National Center for Research Resources, National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Weitzen S, Teno JM, Fennell M, Mor V. Factors associated with site of death: a national study of where people die. Med Care. 2003;41(2):323–335. doi: 10.1097/01.MLR.0000044913.37084.27. [DOI] [PubMed] [Google Scholar]
- 2.Field M, Cassel C. Approaching death: Improving care at the end of life. Washington DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 3.Tang ST, McCorkle R. Determinants of congruence between the preferred and actual place of death for terminally ill cancer patients. J Palliat Care. 2003;19(4):230–237. [PubMed] [Google Scholar]
- 4.Higginson IJ, Sen-Gupta GJ. Place of care in advanced cancer: a qualitative systematic literature review of patient preferences. J Palliat Med. 2000;3(3):287–300. doi: 10.1089/jpm.2000.3.287. [DOI] [PubMed] [Google Scholar]
- 5.Foreman LM, Hunt RW, Luke CG, Roder DM. Factors predictive of preferred place of death in the general population of South Australia. Palliat Med. 2006;20(4):447–453. doi: 10.1191/0269216306pm1149oa. [DOI] [PubMed] [Google Scholar]
- 6.Braun KL, Onaka AT, Horiuchi BY. Advance directive completion rates and end-of-life preferences in Hawaii. J Am Geriatr Soc. 2001;49(12):1708–1713. doi: 10.1046/j.1532-5415.2001.49284.x. [DOI] [PubMed] [Google Scholar]
- 7.Bruera E, Sweeney C, Russell N, Willey JS, Palmer JL. Place of death of Houston area residents with cancer over a two-year period. J Pain Symptom Manage. 2003;26(1):637–643. doi: 10.1016/s0885-3924(03)00204-5. [DOI] [PubMed] [Google Scholar]
- 8.Gomes B. Where people die (1974–2030): past trends, future projections and implications for care. Palliat Med. 2008;22(1):33–41. doi: 10.1177/0269216307084606. [DOI] [PubMed] [Google Scholar]
- 9.Tang ST, McCorkle R. Determinants of place of death for terminal cancer patients. Cancer Invest. 2001;19(2):165–180. doi: 10.1081/cnv-100000151. [DOI] [PubMed] [Google Scholar]
- 10.Pritchard RS, Fisher ES, Teno JM, et al. Influence of patient preferences and local health system characteristics on the place of death. SUPPORT Investigators. Study to Understand Prognoses and Preferences for Risks and Outcomes of Treatment. J Am Geriatr Soc. 1998;46(10):1242–1250. doi: 10.1111/j.1532-5415.1998.tb04540.x. [DOI] [PubMed] [Google Scholar]
- 11.Chvetzoff G, Garnier M, Perol D, et al. Factors predicting home death for terminally ill cancer patients receiving hospital-based home care: the Lyon comprehensive cancer center experience. J Pain Symptom Manage. 2005;30(6):528–535. doi: 10.1016/j.jpainsymman.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 12.Shega JW, Hougham GW, Stocking CB, Cox-Hayley D, Sachs GA. Patients dying with dementia: experience at the end of life and impact of hospice care. J Pain Symptom Manage. 2008;35(5):499–507. doi: 10.1016/j.jpainsymman.2007.06.011. [DOI] [PubMed] [Google Scholar]
- 13.Izquierdo-Porrera AM, Trelis-Navarro J, Gomez-Batiste X. Predicting place of death of elderly cancer patients followed by a palliative care unit. J Pain Symptom Manage. 2001;21(6):481–490. doi: 10.1016/s0885-3924(01)00283-4. [DOI] [PubMed] [Google Scholar]
- 14.Agar M, Currow DC, Shelby-James TM, et al. Preference for place of care and place of death in palliative care: are these different questions? Palliat Med. 2008;22(7):787–795. doi: 10.1177/0269216308092287. [DOI] [PubMed] [Google Scholar]
- 15.Stajduhar KI, Davies B. Variations in and factors influencing family members' decisions for palliative home care. Palliat Med. 2005;19(1):21–32. doi: 10.1191/0269216305pm963oa. [DOI] [PubMed] [Google Scholar]
- 16.Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ. 2006;332(7540):515–521. doi: 10.1136/bmj.38740.614954.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McWhinney IR, Bass MJ, Orr V. Factors associated with location of death (home or hospital) of patients referred to a palliative care team. CMAJ. 1995;152(3):361–367. [PMC free article] [PubMed] [Google Scholar]
- 18.Cantwell P, Turco S, Brenneis C, et al. Predictors of home death in palliative care cancer patients. J Palliat Care. 2000;16(1):23–28. [PubMed] [Google Scholar]
- 19.Bakitas M, Ahles TA, Skalla K, et al. Proxy perspectives regarding end-of-life care for persons with cancer. Cancer. 2008;112(8):1854–1861. doi: 10.1002/cncr.23381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009;24(6):695–701. doi: 10.1007/s11606-009-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Townsend J, Frank AO, Fermont D, et al. Terminal cancer care and patients' preference for place of death: a prospective study. BMJ. 1990;301(6749):415–417. doi: 10.1136/bmj.301.6749.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tiernan E, O'Connor M, O'Siorain L, Kearney M. A prospective study of preferred versus actual place of death among patients referred to a palliative care home-care service. Ir Med J. 2002;95(8):232–235. [PubMed] [Google Scholar]
- 23.Dunlop R, Davies R, Hockley J. Preferred versus actual place of death: a hospital palliative care support team experience. Palliat Med. 1989;3:197–201. [Google Scholar]
- 24.Fukui S, Kawagoe H, Masako S, et al. Determinants of the place of death among terminally ill cancer patients under home hospice care in Japan. Palliat Med. 2003;17(5):445–453. doi: 10.1191/0269216303pm782oa. [DOI] [PubMed] [Google Scholar]
- 25.Takezako Y, Tamiya N, Kajii E. The nursing home versus the hospital as the place of dying for nursing home residents in Japan. Health Policy. 2007;81(2–3):280–288. doi: 10.1016/j.healthpol.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 26.Bell C, Somogyi-Zalud E, Masaki K. Methodological review: measured and reported congruence between preferred and actual place of death. Palliat Med. 2009;23:482–490. doi: 10.1177/0269216309106318. [DOI] [PubMed] [Google Scholar]
- 27.Thomas C, Morris SM, Clark D. Place of death: preferences among cancer patients and their carers. Soc Sci Med. 2004;58(12):2431–2444. doi: 10.1016/j.socscimed.2003.09.005. [DOI] [PubMed] [Google Scholar]
- 28.Tolle SW, Tilden VP, Rosenfeld AG, Hickman SE. Family reports of barriers to optimal care of the dying. Nurs Res. 2000;49(6):310–317. doi: 10.1097/00006199-200011000-00003. [DOI] [PubMed] [Google Scholar]
- 29.Hsieh MC, Huang MC, Lai YL, Lin CC. Grief reactions in family caregivers of advanced cancer patients in Taiwan: relationship to place of death. Cancer Nurs. 2007;30(4):278–284. doi: 10.1097/01.NCC.0000281728.72243.c4. [DOI] [PubMed] [Google Scholar]
- 30.Leff B, Kaffenbarger KP, Remsburg R. Prevalence, effectiveness, and predictors of planning the place of death among older persons followed in community-based long term care. J Am Geriatr Soc. 2000;48(8):943–948. doi: 10.1111/j.1532-5415.2000.tb06892.x. [DOI] [PubMed] [Google Scholar]
- 31.Beccaro M, Costantini M, Giorgi Rossi P, et al. Actual and preferred place of death of cancer patients. Results from the Italian survey of the dying of cancer (ISDOC) J Epidemiol Community Health. 2006;60(5):412–416. doi: 10.1136/jech.2005.043646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Brazil K, Howell D, Bedard M, Krueger P, Heidebrecht C. Preferences for place of care and place of death among informal caregivers of the terminally ill. Palliat Med. 2005;19(6):492–499. doi: 10.1191/0269216305pm1050oa. [DOI] [PubMed] [Google Scholar]
- 33.Karlsen S, Addington-Hall J. How do cancer patients who die at home differ from those who die elsewhere? Palliat Med. 1998;12(4):279–286. doi: 10.1191/026921698673427657. [DOI] [PubMed] [Google Scholar]
- 34.Koffman J, Higginson IJ. Dying to be home? Preferred location of death of first-generation black Caribbean and native-born white patients in the United Kingdom. J Palliat Med. 2004;7(5):628–636. doi: 10.1089/jpm.2004.7.628. [DOI] [PubMed] [Google Scholar]
- 35.Groth-Juncker A, McCusker J. Where do elderly patients prefer to die? Place of death and patient characteristics of 100 elderly patients under the care of a home health care team. J Am Geriatr Soc. 1983;31(8):457–461. doi: 10.1111/j.1532-5415.1983.tb05116.x. [DOI] [PubMed] [Google Scholar]
- 36.Gyllenhammar E, Thoren-Todoulos E, Strang P, et al. Predictive factors for home deaths among cancer patients in Swedish palliative home care. Support Care Cancer. 2003;11(9):560–567. doi: 10.1007/s00520-003-0487-z. [DOI] [PubMed] [Google Scholar]
- 37.Brazil K, Bedard M, Willison K. Factors associated with home death for individuals who receive home support services: a retrospective cohort study. BMC Palliat Care. 2002;1(1):2. doi: 10.1186/1472-684X-1-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shega JW, Levin A, Hougham GW, et al. Palliative Excellence in Alzheimer Care Efforts (PEACE): a program description. J Palliat Med. 2003;6(2):315–320. doi: 10.1089/109662103764978641. [DOI] [PubMed] [Google Scholar]
- 39.Vig EK, Pearlman RA. Good and bad dying from the perspective of terminally ill men. Arch Intern Med. 2004;164(9):977–981. doi: 10.1001/archinte.164.9.977. [DOI] [PubMed] [Google Scholar]
- 40.Steinhauser KE, Christakis NA, Clipp EC, et al. Factors considered important at the end of life by patients, family, physicians, and other care providers. JAMA. 2000;284(19):2476–2482. doi: 10.1001/jama.284.19.2476. [DOI] [PubMed] [Google Scholar]