Abstract
The objectives of this study were to conduct a prevalence survey of trichomoniasis in pregnant women and to evaluate the utility of different methods for its diagnosis. A total of 597 vaginal exudates from pregnant women who were examined at the Hospital de Clinicas in Buenos Aires, Argentina from 1 August 2005 to 31 January 2007, were prospectively and consecutively evaluated. The investigation of Trichomonas vaginalis was made by different microscopic examinations, and culture on liquid medium. The sensitivity and specificity of the microscopic examinations were assessed considering culture on liquid medium as the "gold standard". The prevalence of T. vaginalis obtained by culture on liquid medium was 4.0% (24/597). The prevalence of T. vaginalis obtained by direct wet smear, prolonged May-Grunwald Giemsa staining, and sodium acetate-formalin (SAF)/methylene blue staining-fixing technique was 1.8%, 2.3% and 2.5%, respectively. The sensitivity of the direct wet smear was 45.8%, that of the prolonged May-Grunwald Giemsa staining was 58.3%, and that of the SAF/methylene blue method was 62.5%. Considering the 3 microscopic examinations altogether, the sensitivity rose to 66.7% and the specificity was 100% for all of them. This is the first time that the prevalence data of T. vaginalis by culture in pregnant women are published in Argentina. Due to the low sensitivity obtained by microscopy in asymptomatic pregnant women, the use of the liquid medium is recommended during pregnancy, in order to provide an early diagnosis and treatment.
Keywords: Trichomonas vaginalis, diagnosis, culture, pregnancy, Argentina
Hormone changes produced during pregnancy predispose a higher incidence of infections of the lower genital tract. This leads to maternal and perinatological complications. The diagnosis of Trichomonas vaginalis infection during pregnancy is of great importance as such infections are related to premature rupture of membranes, preterm delivery, and low birth weight [1,2].
Trichomoniasis is a sexually-transmitted disease associated with urethritis, vaginitis, cervicitis, pelvic inflammatory disease, and tubal infertility [3-5], and it is also linked to cervical cancer [6]. Up to 10 to 50% of infected women are asymptomatic and 50% of these women will develop clinical symptoms during the subsequent 6 months [7]. Moreover, reinfection may occur by sexual contact with the man who acts as an asymptomatic carrier [8].
The laboratory diagnosis by microscopic examination has low sensitivity (35-80%) mainly in asymptomatic patients due to the low number of organisms in the sample. This is why it is necessary to implement more sensitive methodologies [9]. In the case of direct microscopic examinations, the detection of T. vaginalis depends on the microscopist's expertise and on the swift transport and processing of the sample, in order to avoid the loss of motility of the parasite [4]. Consequently, the liquid culture medium for T. vaginalis is considered the most accurate method (gold-standard) for the diagnosis of trichomoniasis [6,10-13].
The objectives of this work were to survey the prevalence of infection in asymptomatic and symptomatic pregnant women and to assess the utility of different microscopic methodologies for the diagnosis of trichomoniasis in pregnant women and to compare them with the method using the liquid culture medium.
A total of 597 vaginal exudates from pregnant women were analyzed from 1 August 2005 to 31 January 2007. The patients were examined at the Obstetrics Clinic at the Hospital de Clinicas of the University of Buenos Aires. All the patients underwent clinical and colposcopic examinations. This study was approved by the Hospital Ethics Committee.
The samples of vaginal discharge were taken from the vaginal fornix. The microbiologic study of these samples for the diagnosis of trichomoniasis included a microscopic wet smear examination with 1 ml of physiologic saline solution and smears for Gram and prolonged May-Grunwald Giemsa staining. May-Grunwald-Giemsa staining was performed as follows: each smear was covered with pure May-Grunwald staining solution for 3 min, then rinsed with distilled water for 1 min, and covered with Giemsa solution diluted 1/10 in distilled water for 90 min. Finally, each smear was rinsed with distilled water. Another examination included a microscopic wet smear examination with sodium acetate-formalin (SAF)/methylene blue (methylene blue 0.5 ml and SAF 0.5 ml) [14]. Besides, the liquid medium culture (modified thyoglicolate medium) for T. vaginalis, with 7-day incubation period at 37℃ in an atmosphere of 5% CO2, was performed [13].
Other bedside determinations were pH of vaginal discharge with indicators strips (range 3-7), and fishy-odor test with 1 ml of 10% KOH with posterior microscopic wet smear. T. vaginalis culture was performed at bedside and it was incubated at the corresponding atmosphere not more than 2 hr after collection. The microscopic examinations were also performed within less than 2 hr following collection.
The survey for T. vaginalis was made through direct microscopic examination with physiologic saline solution, SAF/methylene blue, prolonged May-Grumwald Giemsa staining, and modified thyoglicolate medium. The liquid culture medium was examined daily by wet smears for the observation of motile parasites.
Both the sensitivity and specificity for the different microscopic examinations (wet mount with physiologic saline solution, SAF/methylene blue, and prolonged May-Grunwald Giemsa stain) were calculated using the culture on liquid medium as the reference standard. Both the positive and negative predictive values were calculated with their respective 95% confidence intervals (CI) (EPI INFO 6.0). The presence of T. vaginalis was diagnosed by culture in 24 out of 597 (4.0%) of the pregnant patients (95% CI: 2.3-8.3).
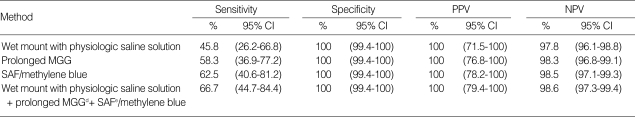
The wet smear with physiologic saline solution detected the parasite in 11 out of 597 (1.8%) patients (95% CI: 1.0-3.4). The prolonged May-Grunwald Giemsa staining detected it in 14 out of 597 (2.3%) (95% CI: 1.3-4.0). Wet smear with SAF/methylene blue detected T. vaginalis in 15 out of 597 (2.5%) (95% CI. 1.5-4.2). Considering the 3 microscopic examinations altogether (wet smear with physiologic saline solution, prolonged May-Grunwald Giemsa staining, and wet smear with SAF/methylene blue), the parasite was detected in 16 out of 597 (2.7%) patients (95% CI: 1.6-4.4). Table 1 shows the sensitivity, specificity, and positive and negative predictive values of each of the methodologies used.
Table 1.
Sensitivities, specificities, and positive and negative predictive values of the different diagnostic methods for the detection of Trichomonas vaginalis in pregnant women
PPV, positive predictive value; NPV, negative predictive value; CI, confidence interval; MGG, May-Grunwald Giemsa; SAF, sodium acetate-formalin.
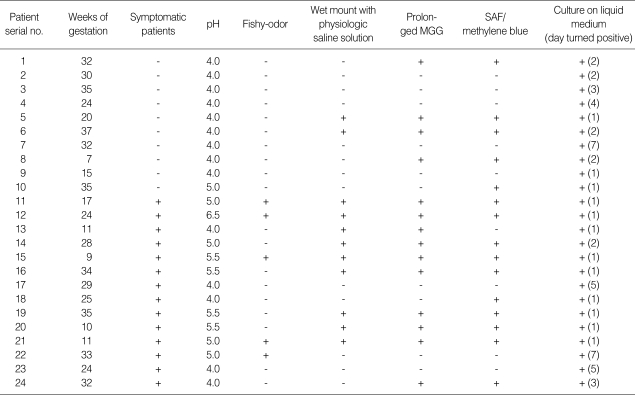
The description of the different characteristics of the patients with trichomoniasis is shown in Table 2. Out of the 24 patients with trichomoniasis, 10 presented with no symptomatology and their colposcopy was normal. The microscopic examinations were negative for T. vaginalis in 5 out of 10 patients. On the other hand, 14 out of 24 patients showed cervicocolpitis and symptomatology. The 3 microscopic examinations altogether of these 14 cases were positive for T. vaginalis in 11 patients (79%).
Table 2.
Characteristics of the pregnant women patients infected with Trichomonas vaginalis
MGG, May-Grunwald Giemsa; SAF, sodium acetate-formalin.
In the present study, a prevalence of 4.0% of T. vaginalis was observed by the liquid culture method in pregnant women. The prevalence values obtained during pregnancy vary in the different published papers according to the populations examined. Germain et al. [15] reported a prevalence of 14.9% by culture in pregnant women of all races with or without symptoms. However, Blackwell et al. [16] described much lower prevalences by culture (0.75%) in symptomatic and asymptomatic pregnant women. Up to the present, no prevalence data of T. vaginalis by culture have been published in Argentina.
It should be highlighted that the solid medium culture (modified Columbia agar) was also used, although it detected only half of the positive cases for T. vaginalis, which shows a low reliability (data not shown). These results differ from the ones reported by Stary et al. [12] who described a sensitivity of 100% for this medium in asymptomatic patients and a value of 97.3% for the symptomatic ones. These differences might be due to the distinct composition of the culture media used. The high agar concentration in the solid medium might hinder the growth and motility of the parasite, as a low number of parasites were observed in this medium. Besides, morphologic alterations (round forms with the presence of vacuoles in their cytoplasm) were observed in this medium.
On the other hand, the prevalences of T. vaginalis vary according to the methodology employed. In other scientific papers, similarly to the findings in the present study, lower prevalences were shown by microscopic examinations, although they presented variations which depend on the population analyzed. Meis et al. [17] reported prevalences of 3.3% and 2.7%, respectively in symptomatic and asymptomatic pregnant women of different races, at the 24th and 28th weeks of gestation, by the wet mount with physiologic saline solution. Simoes et al. [18] in Brazil, described similar prevalences to our results, 2.1% for microscopic examinations in pregnant women with or without symptoms.
It must be also highlighted that the positive rates for T. vaginalis with the different methods appear to have large confidence intervals because the prevalence of infection for this parasite is low in the studied population, in relation to other genital infections, such as vaginal candidiasis (22.4%) and bacterial vaginosis (21.5%) [19].
As described in the literature [10,20,21], the sensitivity of microscopic examinations ranges from 35% to 80%, whereas in our work the sensitivity of the different microscopic examinations varied from 45.8% to 62.5%, and it increased to 66.7% when considering the 3 microscopic examinations altogether, probably due to the low number of parasites present in the group of asymptomatic pregnant women studied. These results were related with the positive predictive values. Similarly, Costamagna [14] reported a sensitivity of 58.3% for the wet mount with physiologic saline solution, and also described a higher efficiency of the wet mount with SAF/methylene blue.
The specificity of the different microscopic examinations was high (100%) in relation with the negative predictive value, as described in the literature [20]. The microscopic examiners of stain smears showed competence and qualification, and examined the preparations as a blind method. It must be taken into account that the sensitivities of the different methods appear to have large confidence intervals while the specificities appear to have tight confidence intervals, in a large part because most of the women were negative for infection. These intervals might be much tighter, probably with a higher number of positive patients for this infection.
Out of the 10 asymptomatic patients studied, the microscopic examinations for T. vaginalis were positive in only half of the cases; and the associated microorganisms were found in conventional cultures in all the patients was Lactobacillus sp. in relation with the low pH (pH: 4.0). These results were similar to the ones described previously by other authors [22]. These patients showed a vaginal pH < 4.5 and the fishy-odor test was negative in all of them. The culture in modified thyoglicolate medium was the only method that allowed the diagnosis of trichomoniasis.
In 11 out of 14 symptomatic patients, the diagnosis of trichomoniasis was performed by means of microscopic examinations and culture in modified thyoglicolate medium. In those 14 patients, absence of Lactobacillus sp. in conventional cultures was observed except in 3 cases. The most frequently found associations in those patients were bacterial vaginosis (4 patients) and Candida albicans (4 patients).
Some authors used PCR for the diagnosis of T. vaginalis and compared the results obtained with the ones obtained with the culture method. In this way, Randonjic et al. [21] reported a sensitivity and specificity of PCR of 81.0% and 97.2%, respectively. Madico et al. [23] described a sensitivity and specificity of PCR of 97% and 98%, respectively, with a substantial agreement between culture and PCR performed with a set of primers targeting a conserved region of the β-tubulin genes of T. vaginalis.
The investigation of T. vaginalis by means of the liquid medium culture requires an exhaustive and laborious daily microscopic observation during 7 days. Nevertheless, this method is recommended routinely for improving diagnosis mainly in asymptomatic pregnant women, and therefore to provide an early and adequate treatment in order to prevent possible maternal and perinatological complications.
ACKNOWLEDGEMENTS
This work was supported by a University of Buenos Aires grant UBACYT B049 project from the Faculty of Pharmacy and Biochemistry.
References
- 1.Cotch MF, Pastorek JG, Nugent RP, Hillier SL, Gibbs RS, Martín DH, Eschenbach DA, Edelman R, Carey JC, Regan JA, Krohn MA, Klebanoff MA, Rao AV, Rhoads GG. Trichomonas vaginalis associated with low birth weight and preterm delivery. The vaginal infections and prematurity study group. Sex Transm Dis. 1997;24:353–360. doi: 10.1097/00007435-199707000-00008. [DOI] [PubMed] [Google Scholar]
- 2.Minkoff H, Grunebaum AN, Schwarz RH, Feldman J, Cummings MC, Crombleholme W, Clark L, Pringle G, McCormack WM. Risk factors for prematurity and premature rupture of membranes: prospective study of the vaginal flora in pregnancy. Am J Obstet Gynecol. 1984;150:965–972. doi: 10.1016/0002-9378(84)90392-2. [DOI] [PubMed] [Google Scholar]
- 3.Sobel JD. Vaginitis. N Engl JMed. 1997;337:1896–1903. doi: 10.1056/NEJM199712253372607. [DOI] [PubMed] [Google Scholar]
- 4.Grodstein F, Goldman MB, Cramer DW. Relation of tubal infertility to a history of sexually transmitted disease. Am J Epidemiol. 1993;137:577–584. doi: 10.1093/oxfordjournals.aje.a116711. [DOI] [PubMed] [Google Scholar]
- 5.Cates W, Joesoef MR, Goldman MB. Atypical pelvis inflammatory disease: can we identify clinical predictors? Am J Obstet Gynecol. 1993;169:341–346. doi: 10.1016/0002-9378(93)90085-w. [DOI] [PubMed] [Google Scholar]
- 6.Zhang Z-F, Begg CB. Is Trichomonas vaginalis a cause of cervical neoplasia? Results from a combined analysis of 24 studies. Int J Epidemiol. 1994;23:682–690. doi: 10.1093/ije/23.4.682. [DOI] [PubMed] [Google Scholar]
- 7.Swygard H, Sena AC, Hobbs MM, Cohen NS. Trichomoniasis: clinical manifestations, diagnosis and management. Sex Transm Infect. 2004;80:91–95. doi: 10.1136/sti.2003.005124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Krieger JN. Trichomoniasis in men: old issues and new data. Sex Transm Dis. 1995;22:83–96. [PubMed] [Google Scholar]
- 9.McCann JS. Comparison of direct microscopy and culture in the diagnosis of trichomoniasis. Br J Vener Dis. 1974;50:450–452. doi: 10.1136/sti.50.6.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Krieger JN, Tam MR, Stevens CE, Nielsen IO, Hale J, Kiviat NB, Holmes KK. Diagnosis of trichomoniasis. Comparison of conventional wet-mount examination with cytologic studies, cultures and monoclonal antibody staining of direct specimens. JAMA. 1988;259:1223–1227. doi: 10.1001/jama.259.8.1223. [DOI] [PubMed] [Google Scholar]
- 11.Garber GE, Sibau L, Ma R, Proctor EM, Shaw CE, Bowie WR. Cell culture compared with broth for detection of Trichomonas vaginalis. J Clin Microbiol. 1987;25:1275–1279. doi: 10.1128/jcm.25.7.1275-1279.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stary A, Kuchinka-Koch A, Teodorowicz L. Detection of Trichomonas vaginalis on modified Columbia agar in the routine laboratory. J Clin Microbiol. 2002;40:3277–3280. doi: 10.1128/JCM.40.9.3277-3280.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poch F, Levin D, Levin S, Dan M. Modified thioglycolate medium: a simple and reliable means for detection of Trichomonas vaginalis. J Clin Microbiol. 1996;34:2630–2631. doi: 10.1128/jcm.34.10.2630-2631.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Costamagna SR. Trichomonas vaginalis. In: Costamagna SR, editor. Parasitosis Regionales, un estudio referido a las principales parasitosis de Bahía Blanca, provincia de Buenos Aires, Argentina. Bahía Blanca, Argentina: Editorial de la Universidad Nacional del Sur; 2004. pp. 197–217. [Google Scholar]
- 15.Germain M, Krohn MA, Hillier SL, Eschenbach DA. Genital flora in pregnancy and its association with intrauterine growth retardation. J Clin Microbiol. 1994;32:2162–2168. doi: 10.1128/jcm.32.9.2162-2168.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blackwell AL, Thomas PD, Wareham K, Emery SJ. Health gains from screening for infection of the lower genital tract in women attending for termination of pregnancy. Lancet. 1993;342:206–210. doi: 10.1016/0140-6736(93)92299-9. [DOI] [PubMed] [Google Scholar]
- 17.Meis PJ, Goldenberg RL, Mercer B, Moawad A, Das A, McNellis D, Johnson F, Tams JD, Thom E, Andrews WW. The preterm prediction study: significance of vaginal infections. Am J Obstet Gynecol. 1995;173:1231–1235. doi: 10.1016/0002-9378(95)91360-2. [DOI] [PubMed] [Google Scholar]
- 18.Simoes JA, Giraldo PC, Faundes A. Prevalence of cervicovaginal infections during gestation and accuracy of clinical diagnosis. Infect Dis Obstet Gynecol. 1998;6:129–133. doi: 10.1002/(SICI)1098-0997(1998)6:3<129::AID-IDOG6>3.0.CO;2-S. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Coppolillo EF, Vay C, Menghi C, Cora Eliseht M, Gatta C, Mendez O, de Torres R, Malamud de Rudavega H, Famiglietti A, Perazzi B. Prevalencia de infecciones vaginales en embarazadas sintomáticas y asintomáticas. Rev Enfer Tract Gen Inf. 2007;1:17–22. [Google Scholar]
- 20.Patel SR, Wiese W, Patel SC, Ohl C, Byrd JC, Estrada CA. Systematic review of diagnostic tests for vaginal trichomoniasis. Infect Dis Obstet Gynecol. 2000;8:248–257. doi: 10.1155/S1064744900000375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Radonjic IV, Dzamic AM, Mitrovic SM, Arsic Arsenijevic VS, Popadic DM, Kranjcic Zec IF. Diagnosis of Trichomonas vaginalis infection: The sensitivities and specificities of microscopy, culture and PCR assay. Eur J Obstet Gynecol Reprod Biol. 2006;126:116–120. doi: 10.1016/j.ejogrb.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 22.Spiegel CA. Microflora associated with Trichomonas vaginalis and vaccination against trichomoniasis. In: Honigberg BM, editor. Trichomonads Parasitic in Humans. New York, USA: Springer-Verlug; 1990. pp. 213–224. [Google Scholar]
- 23.Madico G, Quinn TC, Rompalo A, McKee K, Jr, Gaydos CA. Diagnosis of Trichomonas vaginalis infection by PCR using vaginal swab samples. J Clin Microbiol. 1998;36:3205–3210. doi: 10.1128/jcm.36.11.3205-3210.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]