Abstract
Background
Little is known about mortality in nursing home residents with hip fracture. This study examined the effect of pre-fracture characteristics, hospital complications, and post-fracture complications on mortality in residents with hip fracture.
Methods
This is a retrospective cohort study of 195 long-term care residents (153 women, 42 men) with hip fracture (1999–2006) followed for mortality until June 30, 2007. Pre-fracture characteristics (age, sex, cognition, functional status, comorbidities, body mass index), hospital complications (acute myocardial infarction, congestive heart failure, delirium, infection) and 6-month complications (delirium, pneumonia, pressure ulcer, urinary tract infection [UTI]) were evaluated as potential predictors of mortality.
Results
During a median follow-up of 1.4 years, 150 participants (76.9%) died. Male residents were nearly twice as likely to die compared with female residents (hazard ratio [HR] = 1.9, 95% confidence interval [CI] 1.2–3.0). Other pre-fracture characteristics associated with increased mortality included older age (HR per 5 years = 1.3, 95% CI 1.1–1.6), low functional status (HR = 1.7, 95% CI 1.0–3.0), anemia (HR = 1.6, 95% CI 1.1–2.5), and coronary artery disease (HR = 2.0, 95% CI 1.3–2.9). Mortality was 70% greater among residents with a pressure ulcer or pneumonia within 6 months of hip fracture (pressure ulcer, HR = 1.7, 95% CI 1.2–2.6; pneumonia, HR = 1.7, 95% CI 1.1–2.7). Individual hospital complications and post-fracture delirium and UTI were not significant predictors of mortality.
Conclusions
In addition to pre-fracture characteristics, potentially modifiable post-fracture complications including pressure ulcer and pneumonia were associated with increased mortality in nursing home residents with hip fracture. Prevention strategies to reduce pressure ulcers and pneumonia may help reduce mortality in this frail population.
Keywords: Hip fracture, Nursing home, Mortality
HIP fractures occur more frequently and are associated with greater mortality in nursing home residents compared with community dwellers of the same age and sex (1–3). Among community dwellers, pre-fracture characteristics associated with mortality have been well described and include older age, male sex, poor functional status, comorbidities, and nursing home placement (3–7). Few of these factors are modifiable, and thus, it may not be surprising that mortality following hip fracture has improved little over the past few decades (8).
In contrast, complications may occur during as many as 20% of all hospitalizations for hip fracture (9), and many post-fracture complications are potentially modifiable. Little is known about the effect of specific hospital and post-fracture complications on mortality, particularly among nursing home residents. Therefore, we determined the effect of pre-fracture characteristics, hospital complications, and post-fracture complications on mortality among nursing home residents with hip fracture.
METHODS
Study Design
This was a retrospective cohort study of nursing home residents with hip fracture who were followed from the time of hip fracture until death, relocation, or end of follow-up (June 30, 2007) by reviewing medical records. The study was approved by the Institutional Review Board at Hebrew Rehabilitation Center (Boston, MA).
Study Population
Participants included 195 long-term care residents who experienced a baseline hip fracture between January 1, 1999, and December 31, 2006, while living at Hebrew Rehabilitation Center, a 725-bed, long-term care facility. Participants were identified by standardized, comprehensive medical record review of all residents of Hebrew Rehabilitation Center.
Baseline Hip Fracture Ascertainment
Nursing home residents with hip fractures were identified from a review of federally mandated injury files and confirmed with medical records. In cases of uncertainty, a physician (S.D.B.) adjudicated fractures. Fractures associated with Paget's disease (n = 1), periprosthetic fractures (n = 3), and pathological fractures (n = 1) were excluded. Information on the anatomic location of the fracture and type of repair was also obtained from medical records.
Mortality Ascertainment
Vital status was ascertained through a review of the facility's administrative database. The cause of death was determined through a review of physician notes. In less than 10% of deaths, physician notes were unavailable so death certificates were used. Cause of death was classified as infectious, dementia, cardiac related (acute myocardial infarction [AMI] or congestive heart failure [CHF]), cancer, emphysema, stroke, gastrointestinal bleeding, renal failure, other, or unknown.
Pre-fracture Characteristics
We collected information on pre-fracture characteristics using the Minimum Data Set (MDS) assessment within 3 months preceding the baseline hip fracture. The MDS is a federally mandated needs assessment system performed on all nursing home residents at admission and every 3 months thereafter (10).
Weight, to the nearest pound, and height, to the nearest inch, were used to calculate body mass index (BMI) in kg/m2. Cognition was measured using a validated seven-level Cognitive Performance Scale(11) and classified as normal (scores 0–1), mild-moderate impairment (scores 2–4), or severe impairment (scores 5–6). Functional status was assessed using a validated activities of daily living (ADL) short scale (12,13). This scale sums the score of independence (score = 0) or dependence (score = 1) for seven basic ADL items: bed mobility, transfers, locomotion, dressing, eating, toileting, and personal hygiene (14). We classified functional status as high (0–1), moderate (2–3), and low (4–7). Baseline prevalence of active comorbidities including anemia, arrhythmia, coronary artery disease, cancer, CHF, emphysema, and diabetes was determined by a physician. We selected these comorbidities on the basis of having been previously established as predictors of mortality in nursing home residents (15) or having been identified as predictors of mortality among community dwellers with hip fracture (5).
Hospital Complications
Hospital complications were ascertained from discharge summaries. AMI was defined as electrocardiograph changes in the presence of elevated cardiac enzymes. CHF was defined clinically as left ventricular dysfunction with or without radiographic confirmation. Delirium was defined using Diagnostic and Statistical Manual of Mental Disorders-IV criteria (16). Hospital infection included urinary tract infection (UTI), pneumonia, cellulitis, or Clostridium difficile. Pneumonia was defined as the presence of fever or clinical findings suggestive of pneumonia with or without a chest radiograph. UTI was defined as a positive urinalysis with or without culture results. Cellulitis was defined clinically with or without skin cultures but requiring antibiotics. Clostridium difficile was defined with positive toxin result.
Post-fracture Complications
Six-month post-fracture complications including delirium, pneumonia, pressure ulcer, and UTI were determined from a review of the physician's notes. These complications were selected from a list of 13 acute diagnoses as the most frequent diagnoses occurring within 6 months of fracture. Pressure ulcers were defined as a stage II, III, or IV skin ulceration or any nonstageable ulcer in a dependent position.
Reliability
We performed a reliability study in which a physician (S.D.B.) and a research assistant (M.B.) each independently reviewed the medical records from a random sample of 10 patients to determine kappa agreement for hospital and post-fracture complications. The mean kappa interrater agreement was 86% (range, 74%–100%) and intrarater agreement was 96% (range, 78%–100%).
Statistical Analysis
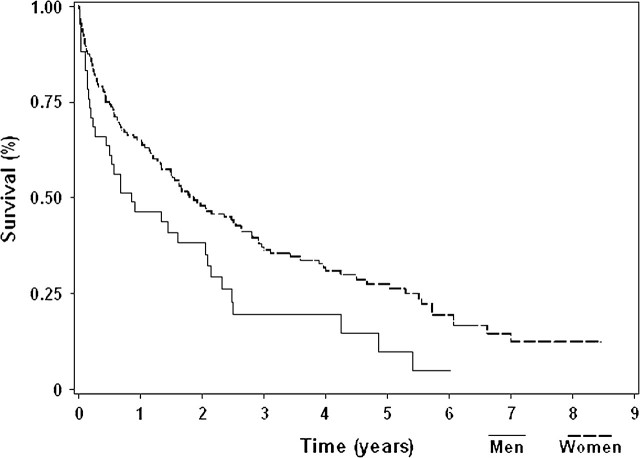
All-cause mortality was calculated using Kaplan–Meier estimates for men and women separately, and a logrank test was used to assess statistical significance.
Cox proportional hazards regression was used to calculate hazard ratios (HRs) and 95% confidence intervals (CIs) for each variable. Variables associated with mortality at a significance level of p ≤ 0.10 were included in multivariable models. We used SAS (version 9.1, 2000; SAS Institute, Cary, NC) for analyses.
RESULTS
Participants included 195 residents (153 women, 42 men) with a hip fracture between 1999 and 2006 (Table 1). Mean age was 88.9 years (range, 65–101 years). At baseline, 19.0% of participants had severe cognitive impairment and 25.8% had low functional status. The most common active comorbidities were coronary artery disease (25.5%) and anemia (21.3%). Sixty-five percent of hip fractures were repaired with internal fixation, whereas 25.8% were repaired with arthroplasty and 9.3% were nonoperatively managed. Among the participants, 26.8% were treated for an infection during hospitalization and 19.0% developed delirium during hospitalization. The most frequent 6-month complications were delirium, UTI, pressure ulcer, and pneumonia (range, 20.5%–34.2%).
Table 1.
Characteristics of Nursing Home Residents With a Hip Fracture Between 1999 and 2006, According to Sex
| Pre-fracture characteristics (%) | Total (N = 195) | Men (N = 42) | Women (N = 153) |
| Age* (y) | 88.9 ± 6.2 | 88.1 ± 7.2 | 89.1 ± 5.9 |
| Body mass index (kg/m2)* | 25.3 ± 5.3 | 25.3 ± 4.7 | 25.3 ± 5.5 |
| Cognitive status | |||
| Normal | 15.8 | 14.6 | 16.1 |
| Mild-moderate impairment | 65.3 | 70.7 | 63.8 |
| Severe impairment | 19.0 | 14.6 | 20.1 |
| Functional status | |||
| High | 23.7 | 31.7 | 21.5 |
| Moderate | 50.5 | 51.2 | 50.3 |
| Low | 25.8 | 17.1 | 28.2 |
| Comorbidities | |||
| Anemia | 21.3 | 25.6 | 20.1 |
| Arrhythmia | 12.0 | 17.1 | 10.6 |
| Cancer | 11.2 | 20.5 | 8.7 |
| Congestive heart failure | 12.0 | 17.1 | 10.7 |
| Coronary artery disease | 25.5 | 35.9 | 22.8 |
| Diabetes | 18.1 | 18.0 | 18.1 |
| Emphysema | 6.9 | 7.7 | 6.7 |
| Fracture characteristics (%) | Total (n = 192)† | Men (n = 41) | Women (n = 151) |
| Anatomic location | 43.8 | 56.1 | 40.4 |
| Femoral neck | 54.7 | 39.0 | 58.9 |
| Intertrochanteric | 1.6 | 4.9 | 0.7 |
| Other | |||
| Type of repair (%) | Total (n = 194)‡ | Men (n = 42) | Women (n = 152) |
| Internal fixation | 65.0 | 56.1 | 67.3 |
| Arthroplasty | 25.8 | 29.3 | 24.8 |
| Immobilization/nonsurgical | 9.3 | 14.6 | 7.9 |
| Length of hospital stay (%) | Total (n = 189)§ | Men (n = 40) | Women (n = 149) |
| No hospitalization | 8.5 | 10.0 | 8.1 |
| 1–2 nights | 9.0 | 5.0 | 10.1 |
| 3–6 nights | 66.7 | 60.0 | 68.5 |
| ≥7 nights | 15.9 | 25.0 | 13.4 |
| Hospital complications (%) | Total (n = 189)§ | Men (n = 40) | Women (n = 149) |
| Infection | 26.8 | 30.0 | 26.0 |
| Delirium | 19.0 | 30.0 | 16.0 |
| Congestive heart failure | 10.6 | 12.5 | 10.1 |
| Acute myocardial infarction | 3.7 | 7.7 | 2.7 |
| 6-month complications (%) | Total (n = 190)| | Men (n = 41) | Women (n = 149) |
| Delirium | 34.2 | 48.8 | 30.2 |
| Urinary tract infection | 32.6 | 19.5 | 36.2 |
| Pressure ulcer | 26.3 | 31.7 | 24.8 |
| Pneumonia | 20.5 | 19.5 | 20.8 |
Notes: *Mean ± standard deviation.
Excludes 3 participants with confirmed hip fracture of unknown type.
Excludes 1 participant with surgical hip fracture repair of unknown type.
Excludes 6 participants without discharge summaries. Nonhospitalized participants were considered to have no hospital complications.
Excludes 4 participants who died during hospitalization and 1 participant who transferred facilities.
During a median follow-up of 1.4 years (range, 2 days to 8.5 years), 145 participants (111 women, 34 men) died and 5 were lost due to relocation. Mortality in men was 1.5 times greater than mortality in women during the first year of follow-up (p = .01), with the highest mortality observed during the first 3 months (Figure 1). Specifically mortality in men was 11.9% at 1 month, 31.5% at 3 months, 36.4% at 6 months, and 53.5% at 1 year, whereas in women mortality was 7.8% at 1 month, 17.7% at 3 months, 25.6% at 6 months, and 35.6% at 1 year.
Figure 1.
Survival among male and female nursing home residents.
Pre-fracture Characteristics
Risk for death in nursing home residents with hip fracture increased by 30% for every 5 years of advancing age (HR = 1.3, 95% CI 1.1–1.6; Table 2). Male nursing home residents were nearly twice as likely to die compared with female residents (HR = 1.9, 95% CI 1.2–3.0). Residents with moderate or low functional status were more likely to die compared with residents with high functional status (moderate versus high, HR = 1.3, 95% CI 0.8–2.1; low versus high, HR = 1.7, 95% CI 1.0–3.0). Anemia (HR = 1.6, 95% CI 1.1–2.5) and coronary artery disease (HR = 2.0, 95% CI 1.3–2.9) were associated with an increased risk for death, whereas BMI, cognition, and other comorbidities were not significant predictors of mortality.
Table 2.
Risk for Death Associated With Pre-fracture Characteristics, Fracture Characteristics, Length of Hospital Stay, Hospital Complications, and Six-Month Post-fracture Complications Among Nursing Home Residents With a Hip Fracture
| Unadjusted HR (95% CI) | Multivariable adjusted HR (95% CI)* | |
| Pre-fracture characteristics | ||
| Age (per 5 y) | 1.3 (1.1–1.5) | 1.3 (1.1–1.6) |
| Male sex | 1.6 (1.1–2.4) | 1.9 (1.2–3.0) |
| Body mass index (per kg/m2) | 1.0 (0.9–1.0) | — |
| Cognitive status | ||
| Moderate impairment vs. normal | 1.2 (0.7–1.9) | 0.9 (0.5–1.5) |
| Severe impairment vs. normal | 2.0 (1.2–3.6) | 1.4 (0.7–2.7) |
| Functional status | ||
| Moderate vs. high | 1.6 (1.0–2.4) | 1.3 (0.8–2.1) |
| Low vs. high | 1.6 (1.0–2.6) | 1.7 (1.0–3.0) |
| Comorbidities | ||
| Anemia | 1.7 (1.2–2.6) | 1.6 (1.1–2.5) |
| Arrhythmia | 1.1 (0.7–1.8) | — |
| Congestive heart failure | 1.7 (1.0–2.7) | 1.2 (0.7–2.0) |
| Coronary artery disease | 2.1 (1.4–3.0) | 2.0 (1.3–2.9) |
| Cancer | 1.3 (0.7–2.2) | — |
| Diabetes | 1.1 (0.7–1.8) | — |
| Emphysema | 1.1 (0.5–2.3) | — |
| Fracture characteristics | ||
| Intertrochanteric vs. other | 0.9 (0.6–1.2) | — |
| Length of hospital stay | ||
| Long hospital stay (≥7 nights) vs. other hospitalization | 1.3 (0.8–2.0) | — |
| Hospital complications | ||
| Acute myocardial infarction | 2.3 (1.0–5.2) | 1.5 (0.6–3.8) |
| Congestive heart failure | 1.3 (0.8–2.3) | — |
| Delirium | 1.2 (0.8–1.9) | — |
| Infection | 1.0 (0.8–1.6) | — |
| 6-month complications (%) | ||
| Delirium | 1.4 (1.0–1.9) | 1.3 (0.9–2.0) |
| Urinary tract infection | 1.1 (0.8–1.5) | — |
| Pressure ulcer | 1.7 (1.2–2.5) | 1.7 (1.2–2.6) |
| Pneumonia | 1.7 (1.1–2.5) | 1.7 (1.1–2.7) |
Notes: CI = confidence interval; HR = hazard ratio. “—” indicates that the variable was not included in the multivariate model based on univariate significance (p > .10).
Final model includes 179 observations.
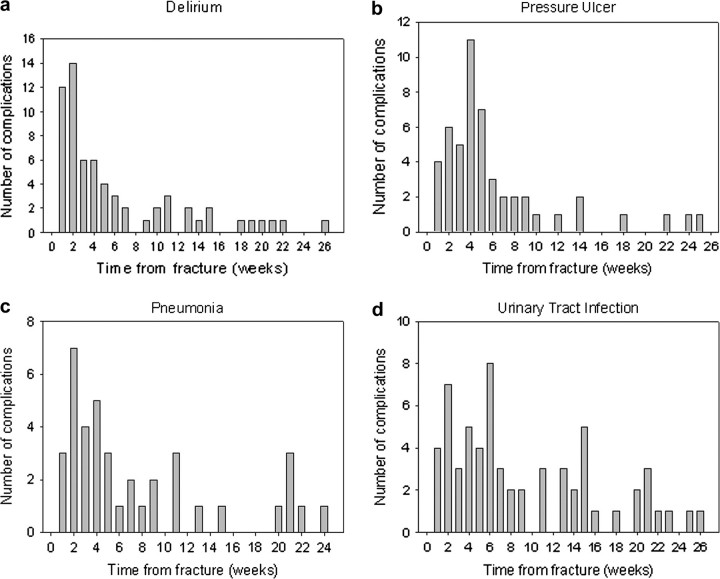
Hospital and Post-fracture Complications
Eighteen percent of participants were rehospitalized within 8 weeks and 25% within 6 months following hip fracture. More than 55% of the 6-month post-fracture complications of pressure ulcer, delirium, pneumonia, and UTI occurred within 8 weeks of the hip fracture (Figure 2). The 6-month complications of pressure ulcer and pneumonia were associated with a 70% increased mortality (pressure ulcer, HR = 1.7, 95% CI 1.2–2.6; pneumonia, HR = 1.7, 95% CI 1.1–2.7; Table 3). Hospital complications and 6-month post-fracture delirium and UTI were not significant predictors of mortality.
Figure 2.
Time to complications among nursing home residents with hip fracture.
Table 3.
Cause of Death Among 145 Nursing Home Residents With Hip Fracture (1999-2006) Who Died by June 2007
| Cause of Death | Total (N = 145), N (%) | Men (N = 34), N (%) | Women (N = 111), N (%) |
| Infection | 54 (37.2) | 13 (38.2) | 41 (36.9) |
| Dementia | 33 (22.8) | 5 (14.7) | 28 (25.2) |
| Cardiac related | 25 (17.2) | 8 (23.5) | 17 (15.3) |
| Cancer | 7 (4.8) | 2 (5.9) | 5 (4.5) |
| Emphysema | 5 (3.4) | 2 (5.9) | 3 (2.7) |
| Stroke | 3 (2.1) | — | 3 (2.7) |
| Gastrointestinal bleeding | 4 (2.8) | 1 (2.9) | 3 (2.7) |
| Renal failure | 4 (2.8) | 2 (5.9) | 2 (1.8) |
| Other | 6 (4.1) | 1 (2.9) | 5 (4.5) |
| Unknown | 4 (2.8) | — | 4 (3.6) |
Cause of Death
The most common cause of death following hip fracture in men and women was infection (37.2%), followed by dementia in women (25.2%) and cardiac related in men (23.5%) (Table 3).
DISCUSSION
We observed that 36% of female and 54% of male nursing home residents died within 1 year of hip fracture. Pre-fracture characteristics including older age, male sex, low functional status, anemia, and coronary artery disease were associated with an increased risk for death in nursing home residents with hip fracture. Complications of delirium, pressure ulcer, pneumonia, and UTI were common among nursing home residents with hip fracture, with the majority occurring during the first 8 weeks. Six-month complications of pressure ulcer and pneumonia were associated with a 70% increase in mortality. Pre-fracture cognition and BMI, individual hospital complications, and 6-month complications of delirium and UTI were not associated with an increased mortality.
Community-based studies have described similar pre-fracture characteristics associated with an increased mortality following hip fracture including older age, low functional status, and certain comorbidities (anemia, arrhythmia, coronary artery disease, CHF, cancer, emphysema, and renal failure) (3–7). Cognition was not a significant predictor of mortality in two large prospective cohort studies after accounting for functional status and other pre-fracture characteristics (4,7). A possible explanation for the lack of association between cognition and mortality is that baseline cognition may be a less important determinant of immobility and complications after hip fracture compared with baseline functional status.
Consistent with studies of community dwellers (3,5,17–19), we found that male nursing home residents with hip fracture had an increased mortality compared with female residents independent of pre-fracture characteristics. A large case-control study suggests that the increased mortality observed in men with hip fracture is explained in part by an increase in deaths from infection (20). Interestingly, we did not find an increase in the frequency of post-fracture pneumonia and UTI in men compared with women, and infections were responsible for a similar proportion of deaths in both sexes. In contrast, men were more likely to experience post-fracture delirium compared with women. The high prevalence of delirium in men after hip fracture may be responsible at least in part for the marked gender difference in survival.
Among individuals with hip fracture, the association between specific hospital complications, such as delirium, and mortality is unclear. One prospective cohort study of community dwellers found that delirium upon hospital admission was associated with a threefold increase in 1-year mortality (3), whereas another study excluding persons with dementia found no such association (21). Nonetheless, perioperative delirium has been associated with poor functional recovery following hip fracture in several studies (21,22). We did not find a statistical association between hospital complications or 6-month post-fracture delirium and mortality; however, we may have been underpowered, particularly if a gender-specific association exists.
Aside from delirium, few studies have examined the association between specific hospital complications following hip fracture and mortality. A prospective Japanese cohort study found that the development of pneumonia during hospitalization for hip fracture was associated with a twofold increased risk for death (23). Another prospective British study found an increased mortality up to 1 year among community dwellers with perioperative heart failure or pneumonia (9). We did not find a statistical association between individual hospital complications and mortality, which again may reflect our small numbers.
Little is known about complications that occur after hospitalization for hip fracture, particularly in the nursing home setting. A prospective study of community dwellers found that the occurrence of hip fracture was associated with a 50% increased risk for pneumonia requiring hospitalization (24). In 1997, an audit of seven British hospitals found that 4.6% of patients with hip fracture repair developed pneumonia within 3 months, and pneumonia was associated with nearly a fivefold increased mortality at 3 months (25). Infections may also be consequential among nursing home residents with fracture as a case-control study found that residents with osteoporotic fractures were 30% more likely to be hospitalized with a UTI compared with residents without fracture (26).
Pressure ulcers are also a common complication among elderly persons with hip fracture (27,28). The same British audit found that 10.0% of patients who underwent hip fracture repair developed a pressure ulcer within 3 months, and the development of a pressure ulcer was associated with 2.2 times increased mortality at 3 months (25).
Compared with the British study, we found an even greater prevalence of the post-fracture complications of pneumonia and pressure ulcer, which is likely a reflection of our frail institutionalized population. Similar to the British study, we found that the development of either pneumonia or a pressure ulcer within 6 months of hip fracture was associated with an increased mortality. The associations were unchanged when we considered post-fracture complications that occurred as recently as 3 months or as long as 1 year following hip fracture (results not shown). These findings are important given that marked variations in the incidence of both pneumonia and pressure ulcers exist between nursing home facilities, suggesting that these complications may be modifiable (29,30). It remains unknown whether aggressive vaccination and skin management strategies might lead to a reduction in pneumonia and pressure ulcers among nursing home residents with hip fracture, and whether these strategies could ultimately lead to the improved survival of this vulnerable population.
We recognize that the most frail residents in our study may have developed a pressure ulcer before the hip fracture, thus explaining the positive association we found between pressure ulcers and mortality. However, using administrative data (MDS), we found only 6% of residents with pressure ulcer had a documented ulcer before the fracture. Therefore, it appears that the majority of these ulcers were caused by immobilization after the fracture and that pressure ulcers are an independent predictor of mortality among nursing home residents with hip fracture.
Mortality among residents who forewent surgical repair is likely to be different compared with residents who underwent surgical repair. We therefore performed a stratified analysis excluding residents without surgical repair (n = 18), and the associations were unchanged.
We did not have information on complication rates or cause of death for residents not experiencing a hip fracture; therefore, we are unable to say whether our results are significantly different from what would be expected in the general nursing home population. However, the prevalence of complications and mortality in our study is much higher than in the general nursing home population, and thus, these factors are likely to be consequential to the hip fracture itself.
There are several limitations to this study. First, our sample size was small, with particularly limited numbers of men. Nonetheless, we were able to identify several pre-fracture characteristics and post-fracture complications that were predictive of mortality. Second, information on predictors was obtained retrospectively using the MDS or medical records. Certain diagnoses, such as delirium, may therefore be underreported resulting in misclassification. We expect that misclassification occurred at random such that it would not greatly influence our results. Third, although autopsy reports would have provided more definitive information on cause of death, they are rarely performed among frail nursing home residents. Finally, this study was conducted in a single nursing home. Individual patient and physician decisions may have influenced the care of these frail elders such that different facilities may have different results.
In conclusion, besides traditional pre-fracture characteristics associated with mortality, this study identified post-fracture complications including pneumonia and pressure ulcer as associated with an increased risk for death among nursing home residents with hip fracture. Post-operative care plans that include prevention strategies to reduce pressure ulcers and increase vaccination and timely treatment of pneumonia may help reduce mortality in this frail population. Larger, multicenter studies should be performed to confirm these risk factors and to identify other predictors of mortality among nursing home residents with hip fracture.
FUNDING
This work was supported by grant T32 AG023480-03 to Beth Israel Deaconess Medical Center, the Hartford Geriatrics Health Outcomes Research Scholars Awards Program, and the Men's Associates of Hebrew SeniorLife.
Acknowledgments
This study was presented in part as an abstract at the 30th Annual Meeting of the American Society for Bone and Mineral Research, Montreal, Canada, September 2008.
References
- 1.Ooms ME, Vlasman P, Lips P, Nauta J, Bouter LM, Valkenburg HA. The incidence of hip fractures in independent and institutionalized elderly people. Osteoporos Int. 1994;4(1):6–10. doi: 10.1007/BF02352254. [DOI] [PubMed] [Google Scholar]
- 2.Rudman IW, Rudman D. High rate of fractures for men in nursing homes. Am J Phys Med Rehabil. 1989;68(1):2–5. doi: 10.1097/00002060-198902000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Survival experience of aged hip fracture patients. Am J Public Health. 1989;79(3):274–278. doi: 10.2105/ajph.79.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hannan EL, Magaziner J, Wang JJ, et al. Mortality and locomotion 6 months after hospitalization for hip fracture: risk factors and risk-adjusted hospital outcomes. JAMA. 2001;285(21):2736–2742. doi: 10.1001/jama.285.21.2736. [DOI] [PubMed] [Google Scholar]
- 5.Jiang HX, Majumdar SR, Dick DA, et al. Development and initial validation of a risk score for predicting in-hospital and 1-year mortality in patients with hip fractures. J Bone Miner Res. 2005;20(3):494–500. doi: 10.1359/JBMR.041133. [DOI] [PubMed] [Google Scholar]
- 6.Marottoli RA, Berkman LF, Leo-Summers L, Cooney LM., Jr. Predictors of mortality and institutionalization after hip fracture: the New Haven EPESE cohort. Established Populations for Epidemiologic Studies of the Elderly. Am J Public Health. 1994;84(11):1807–1812. doi: 10.2105/ajph.84.11.1807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pioli G, Barone A, Giusti A, et al. Predictors of mortality after hip fracture: results from 1-year follow-up. Aging Clin Exp Res. 2006;18(5):381–387. doi: 10.1007/BF03324834. [DOI] [PubMed] [Google Scholar]
- 8.Vestergaard P, Rejnmark L, Mosekilde L. Has mortality after a hip fracture increased? J Am Geriatr Soc. 2007;55(11):1720–1726. doi: 10.1111/j.1532-5415.2007.01420.x. [DOI] [PubMed] [Google Scholar]
- 9.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris JN, Hawes C, Fries BE, et al. Designing the national resident assessment instrument for nursing homes. Gerontologist. 1990;30(3):293–307. doi: 10.1093/geront/30.3.293. [DOI] [PubMed] [Google Scholar]
- 11.Hartmaier SL, Sloane PD, Guess HA, Koch GG, Mitchell CM, Phillips CD. Validation of the Minimum Data Set Cognitive Performance Scale: agreement with the Mini-Mental State Examination. J Gerontol A Biol Sci Med Sci. 1995;50(2):M128–133. doi: 10.1093/gerona/50a.2.m128. [DOI] [PubMed] [Google Scholar]
- 12.Williams BC, Li Y, Fries BE, Warren RL. Predicting patient scores between the functional independence measure and the minimum data set: development and performance of a FIM-MDS “crosswalk. Arch Phys Med Rehabil. 1997;78(1):48–54. doi: 10.1016/s0003-9993(97)90009-5. [DOI] [PubMed] [Google Scholar]
- 13.Frederiksen K, Tariot P, De Jonghe E. Minimum Data Set Plus (MDS+) scores compared with scores from five rating scales. J Am Geriatr Soc. 1996;44(3):305–309. doi: 10.1111/j.1532-5415.1996.tb00920.x. [DOI] [PubMed] [Google Scholar]
- 14.Morris JN, Fries BE, Morris SA. Scaling ADLs within the MDS. J Gerontol A Biol Sci Med Sci. 1999;54(11):M546–553. doi: 10.1093/gerona/54.11.m546. [DOI] [PubMed] [Google Scholar]
- 15.van Dijk PT, Mehr DR, Ooms ME, et al. Comorbidity and 1-year mortality risks in nursing home residents. J Am Geriatr Soc. 2005;53(4):660–665. doi: 10.1111/j.1532-5415.2005.53216.x. [DOI] [PubMed] [Google Scholar]
- 16.American Psychological Association; 1994. American Psychological Association Diagnostic and Statistical Manual of Mental Disorders. 4th ed. [Google Scholar]
- 17.Trombetti A, Herrmann F, Hoffmeyer P, Schurch MA, Bonjour JP, Rizzoli R. Survival and potential years of life lost after hip fracture in men and age-matched women. Osteoporos Int. 2002;13(9):731–737. doi: 10.1007/s001980200100. [DOI] [PubMed] [Google Scholar]
- 18.Bass E, French DD, Bradham DD, Rubenstein LZ. Risk-adjusted mortality rates of elderly veterans with hip fractures. Ann Epidemiol. 2007;17(7):514–519. doi: 10.1016/j.annepidem.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 19.Holt G, Smith R, Duncan K, Hutchison JD, Gregori A. Gender differences in epidemiology and outcome after hip fracture: evidence from the Scottish Hip Fracture Audit. J Bone Joint Surg Br. 2008;90(4):480–483. doi: 10.1302/0301-620X.90B4.20264. [DOI] [PubMed] [Google Scholar]
- 20.Wehren LE, Hawkes WG, Orwig DL, Hebel JR, Zimmerman SI, Magaziner J. Gender differences in mortality after hip fracture: the role of infection. J Bone Miner Res. 2003;18(12):2231–2237. doi: 10.1359/jbmr.2003.18.12.2231. [DOI] [PubMed] [Google Scholar]
- 21.Dolan MM, Hawkes WG, Zimmerman SI, et al. Delirium on hospital admission in aged hip fracture patients: prediction of mortality and 2-year functional outcomes. J Gerontol A Biol Sci Med Sci. 2000;55(9):M527–534. doi: 10.1093/gerona/55.9.m527. [DOI] [PubMed] [Google Scholar]
- 22.Marcantonio ER, Flacker JM, Michaels M, Resnick NM. Delirium is independently associated with poor functional recovery after hip fracture. J Am Geriatr Soc. 2000;48(6):618–624. doi: 10.1111/j.1532-5415.2000.tb04718.x. [DOI] [PubMed] [Google Scholar]
- 23.Muraki S, Yamamoto S, Ishibashi H, Nakamura K. Factors associated with mortality following hip fracture in Japan. J Bone Miner Metab. 2006;24(2):100–104. doi: 10.1007/s00774-005-0654-z. [DOI] [PubMed] [Google Scholar]
- 24.Callahan CM, Wolinsky FD. Hospitalization for pneumonia among older adults. J Gerontol A Biol Sci Med Sci. 1996;51(6):M276–M282. doi: 10.1093/gerona/51a.6.m276. [DOI] [PubMed] [Google Scholar]
- 25.Freeman C, Todd C, Camilleri-Ferrante C, et al. Quality improvement for patients with hip fracture: experience from a multi-site audit. Qual Saf Health Care. 2002;11(3):239–245. doi: 10.1136/qhc.11.3.239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Zimmerman S, Chandler JM, Hawkes W, et al. Effect of fracture on the health care use of nursing home residents. Arch Intern Med. 2002;162(13):1502–1508. doi: 10.1001/archinte.162.13.1502. [DOI] [PubMed] [Google Scholar]
- 27.Hommel A, Bjorkelund KB, Thorngren KG, Ulander K. Nutritional status among patients with hip fracture in relation to pressure ulcers. Clin Nutr. 2007;26(5):589–596. doi: 10.1016/j.clnu.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 28.Margolis DJ, Knauss J, Bilker W, Baumgarten M. Medical conditions as risk factors for pressure ulcers in an outpatient setting. Age Ageing. 2003;32(3):259–264. doi: 10.1093/ageing/32.3.259. [DOI] [PubMed] [Google Scholar]
- 29.Tannen A, Dassen T, Halfens R. Differences in prevalence of pressure ulcers between the Netherlands and Germany—associations between risk, prevention and occurrence of pressure ulcers in hospitals and nursing homes. J Clin Nurs. 2008;17(9):1237–1244. doi: 10.1111/j.1365-2702.2007.02225.x. [DOI] [PubMed] [Google Scholar]
- 30.Tan CG, Ostrawski S, Bresnitz EA. A preventable outbreak of pneumococcal pneumonia among unvaccinated nursing home residents in New Jersey during 2001. Infect Control Hosp Epidemiol. 2003;24(11):848–852. doi: 10.1086/502148. [DOI] [PubMed] [Google Scholar]