Abstract
Many studies showed abnormal serotonin transporter (5-HTT) function and heart rate variability (HRV) in panic disorder patients. The present study investigated the relationship between HRV power spectral analysis findings and platelet serotonin uptake in panic disorder patients. Short-term HRV over 5 min and platelet serotonin transporter uptake parameters (Vmax and Km) were measured both in 45 patients with panic disorder and in 30 age-matched normal healthy control subjects. Low frequency power (LF) normalized unit (nu) and LF/high frequency power (HF) were significantly higher, whereas HF and HF nu were lower in the patient group than in the control group. Vmax and Km were all significantly lower (i.e., reflects decreased 5-HTT function) in patients with panic disorder than in normal controls. In the patient group, Km was negatively correlated with LF/HF and LF nu whereas no such correlations between them were found in the control group. By multivariate analysis based on multiple hierarchical linear regression, a low Km independently predicted an increased LF nu even after controlling for age, sex, and body mass index in the patient group. These results suggest that impaired 5-HTT function is closely related to dysregulation of autonomic nervous system in panic disorder.
Keywords: Panic Disorder, Heart Rate Variability, Platelet Serotonin Uptake
INTRODUCTION
Panic disorder (PD) is a chronic and often disabling psychiatric condition (1). Some researches even reported increased cardiac mortality rate in patients with PD, and autonomic dysregulation has been suggested to link between PD and increased cardiac mortality (2, 3). Heart rate variability (HRV) is known to be a noninvasive and useful method to assess autonomic control of cardiac activity (4). HRV has attracted considerable interest in clinical research (5, 6), and altered HRV has been repeatedly found in patients with panic disorder (5-8). Short-term spectral power analysis of HRV is typically characterized by 3 major components: high frequency power (HF), low frequency power (LF), and very low frequency power (VLF). HF is known to reflect parasympathetic nervous activity, whereas LF is associated with both sympathetic and parasympathetic nervous activity (9). The absolute values of HF and LF can be transformed into normalized units (nu) that represent the relative values of each power component in proportion to total power minus VLF component (9). LF/HF and LF in normalized units are considered to mirror sympathovagal balance (9). Yeragani et al. (10) reported a decrease in the HF component and an increase in the LF component in panic disorder patients compared with normal controls. They also reported a significant increase in the sympathovagal ratio in the patient group after isoproterenol administration (8). These findings suggest an overall dysregulation of autonomic activity in panic disorder.
It remains unclear what the role of neural substrates is in the relationship between HRV and serotonin transporter function. Catecholamines, such as norepinephrine and epinephrine, have been assumed to be implicated in altered HRV in patients with PD. However, Alvarenga et al. (11) reported no significant correlation between norepinephrine spillover rate and HRV indexes. Abnormalities of serotonin transporter (5-HTT) have been found in panic disorder, although results about the synaptic serotonin state are still conflicting (12-14). Lesch et al. (15) reported that hyperserotonergic state, resulting from impaired 5-HTT function, can lead to stimulation of amygdala, and finally bring about anxiety or fear response. In addition, serotonergic agents are known to relieve panic-related symptoms effectively (16). Thus, the exploration of relationship between 5-HT system and HRV may shed light on the neural substrate of HRV and autonomic imbalance in patients with PD. Although some studies have shown that successful pharmacotherapy to affect 5-HTT function has been associated with improved HRV findings in patients with panic disorder, no data are available on the association between HRV and a measureable index of serotonin uptake in panic patients.
The human platelet has been used as a useful peripheral markers of central serotonergic neurons (17) because of the difficulties of access to central nervous system. We aimed to compare patients with panic disorder and normal healthy controls in terms of HRV as well as platelet serotonin uptake, and to determine the relationship between them in panic disorder patients.
MATERIALS AND METHODS
Particicipants
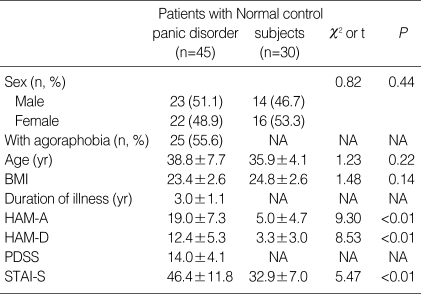
The study cohort consisted of 45 patients (23 men and 22 women) with panic disorder with/without agoraphobia, aged from 20 to 55 yr (mean±SD, 38.8±7.70 yr). Sample characteristics are listed in Table 1. Patients who met the DSM-IV criteria for panic disorder with/without agoraphobia, were diagnosed using the Structured Clinical Interview for DSM-IV (SCID) (18). Panic disorder patients with a current major medical or psychiatric illnesses, including heart disease, liver or renal disease, diabetes mellitus, severe asthma, cerebrovascular disease, mood disorder, other anxiety disorder, psychosis, and current drug or alcohol abuse were excluded. The patients in our study had a relatively short duration of illness (mean±SD, 3.0±1.1 yr). To be eligible for the study, patients with panic disorder should not have received any psychotropic medications (except medication of benzodiazepines p.r.n.) for at least 2 months before participating in the study. Thirty age-matched normal healthy subjects (14 men and 16 women) were recruited as control subjects using local advertisements and referrals. All study subjects underwent a physical examination, electrocardiography, a complete blood count, blood chemistry, and urinalysis. Subjects completed the Hamilton Rating Scale for Anxiety (HAM-A) (19), the 17-item Hamilton Rating Scale for Depression (HAM-D) (20), and the Panic Disorder Severity Scale (PDSS)-Korean version (21). After being given a complete description of the study, subjects provided written informed consent. The study was approved by the Institutional Review Board of Samsung Medical Center.
Table 1.
Demographic and clinical characteristics
BMI, body mass index; HAM-A, the Hamilton Rating Scale for Anxiety; HAM-D, the 17-item Hamilton Rating Scale for Depression; PDSS, the Panic Disorder Severity Scale; STAI-S, the Spielberger State Anxiety Inventory; NA, not, applicable.
Platelet [3H]5-HT uptake assays
Venous blood was sampled from all 75 subjects into vacutainer tubes containing acid citrate dextrose (ACD)-A between 8:00 and 10:00 a.m. after overnight fasting. 5-HT uptake parameters were measured within 2 hr of sample collection. Platelet-rich plasma (PRP) was prepared by centrifugation at 250 g for 15 min at a room temperature. Platelets for [3H]-serotonin uptake assays were isolated by centrifuging PRP twice at 3,000 g for 10 min, and then suspended in original blood volumes of Ca2+ free Krebs-Hensleit buffer (pH 7.4). Numbers of platelets were determined using an automatic cell-counter in the impedance mode (Sysmex XE-2100, Kobe, Japan). Aliquots of PRP were incubated in the presence of [3H]5-HT (from 0.1 to 1.6 µM; final volume 500 µL) at 37℃ for 10 min, and the blocking of the binding reaction by 100 µM paroxetine was followed rapidly using INOTECH Glass fiber filters (typeG-7). Filters were then washed twice with 5 mL of ice-cold saline (150 mM NaCl and 2% ethylene diamine tetraacetic acid [EDTA]) and filter mat discs were distributed into vials containing 4 mL Ultima Gold F cocktail solution (Perkin Elmer, Norwalk, CT). Radioactivities were measured using a liquid scintillation in a Beckman L6500 Scintillation Counter. Platelet 5-HT uptake parameters were calculated using the Michaelis-Menten equation using KELL ver. 6.0 and Enzfitter for Windows (Biosoft®, Cambridge, UK).
Heart rate variability
Subjects were instrumented with an ProComp+ with electrocardiogram (ECG) (Thought Technology Ltd., Quebec, Canada) and rested for 30 min. Five-minutes of data were collected at rest in a comfortable chair and stored in a computer for subsequent review, artifact rejection, and calculation. CardioPro program version 2.1 (Thought Technology Ltd.) was used to perform time-domain analysis as well as spectral power analyses by fast fourier transformation. Frequency domains including HF power (>0.15 Hz), LF power (0.05-0.15 Hz), VLF power (<0.05 Hz) were obtained. LF/HF ratio, and HF nu and LF nu were also calculated.
Statistical analysis
The Student's t-test and the Mann-Whitney U test were used to analyze differences between groups in terms of HRV indexes and platelet 5-HT uptake kinetic parameters. Categorical variables were analyzed using the chi-square test. Pearson correlation was used to examine the relationship between HRV and platelet serotonin uptake parameters. We also performed hierarchical multiple linear regression analysis of HRV indexes (HF, LF/HF, and LF nu), which were viewed as dependent measures, to determine whether 5-HT uptake parameters predict HRV, after controlling for age, sex, and body mass index. Analyses were run on the SPSS version 14.0 software. The criterion for statistical significance was set at P<0.05.
RESULTS
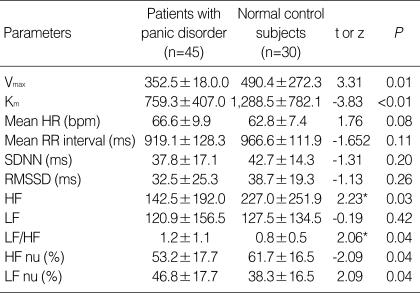
Demographic and clinical characteristics of the subjects were presented in the Table 1. As expected, the HAM-A, HAM-D, and STAI-S scores were higher in panic patients than those in controls (Table 1). In terms of HRV, LF/HF ratio was higher (1.2±1.1 vs. 0.8±0.5, Z=2.06, P=0.039; by the Mann-Whitney U test) whereas HF was lower in the patients (142.5±192.0 vs. 227.0±251.8 ms2, Z=2.23, P=0.03; by the Mann-Whitney U test). The Student's t-test also revealed that LF nu was higher and HF nu was lower in the patients (46.8±17.7 vs. 38.3±16.5, t=-2.09, P=0.04 and t=-2.09, P=0.04, respectively) (Table 2). There were no significant differences in the means of HR, RR interval, SDNN, and RMSSD between the patient group and healthy controls (all P values >0.1). Respiration rates were not different between the two groups (P=0.59).
Table 2.
Platelet 5-HT uptake parameters and HRV indexes
*by Mann-Whitney U test.
Vmax, Platelet 5-HT uptake maximum velocity=pM 5-HT/107 platelet×min 37℃; Km, Michaelis-Mentens constant=nM; HR, heart rate per minutes; SDNN, Standard deviation of normal to normal beat intervals (ms); RMSSD, Root mean square of successive differences; LF, low frequency component (ms2); HF, high frequency component (ms2); LF nu, LF normalized unit; HF nu, HF normalized unit.
The Student's t-test revealed that Vmax and Km values were significantly lower in the patients than in normal controls (352.5±180.0 vs. 490.4±272.3 pMol 5-HT/107 platelet×min 37℃, t=-3.31, P=0.01 and 759.3±407.0 vs. 1,288.5±782.1 nM, t=-3.83, P=0.001, respectively).
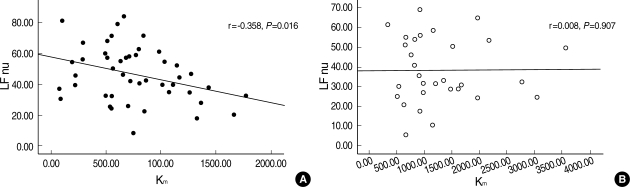
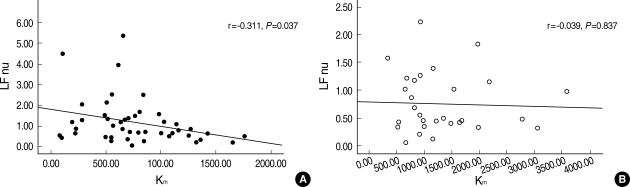
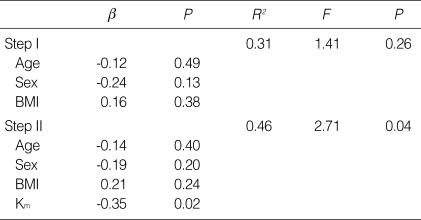
Pearson correlation analyses were performed between HRV indexes and 5-HT uptake parameters in both groups. In the patient group, Km was found to be negatively correlated with LF nu (r=-0.358, P=0.016; Fig. 1A) and LF/HF (r=-0.311, P=0.037; Fig. 2A). There was no significant correlation between Km and HF in the patient group (P>0.2). By multivariate analysis using multiple hierarchical linear regression, a low Km was found to independently predict an elevated LF nu after controlling for age, sex, and body mass index (ΔR2=0.15, β=-0.35, P=0.02; Table 3). The significance of association between LF/HF and Km disappeared after controlling for such confounding variables (P>0.1). On the other hand, no significant correlations were found between 5-HT uptake parameters and HRV indices in the control group (all P values >0.1). We also examined the relationship between emotional states (scores of the HAM-A, HAM-D, and STAI-S) and HRV indices as well as Km since emotional states might affect HRV parameters. However, we did not find any significant correlation between them (all P values >0.1).
Fig. 1.
Correlation between Km and LF nu in patients with panic disorder and in normal control subjects. (A) Patients with panic disorder. (B) Normal control subjects.
Fig. 2.
Correlation between Km and LF/HF in patients with panic disorder and in normal control subjects. (A) Patients with panic disorder. (B) Normal control subjects.
Table 3.
Hierarchical multiple linear regression analysis and the prediction of sympathovagal index LF nu using Km in the patients with panic disorder (n=45)
BMI, body mass index; Km, Michaelis-Mentens constant=nM; LF, low frequency component (ms2); HF, high frequency component (ms2).
DISCUSSION
Many researches have concluded that altered 5-HTT function and abnormalities in heart rate variability (HRV) are characteristics of panic disorder (5, 6, 10, 12, 13, 22). However, the relationship between platelet 5-HTT function and HRV in panic disorder has yet to be known. To the best of our knowledge, the present study is the first one to investigate the relationship between platelet 5-HT uptake function and HRV in panic disorder.
There have been contradictory findings on the 5-HTT function in panic disorder (12, 13, 23). In the present study, platelet 5-HT uptake maximal velocity (Vmax) and its associated affinity constant (Km) were found to be lower (i.e. increased affinity) in panic disorder patients than in normal control subjects. In terms of HRV indexes, decreased HF and increased LF/HF and LF nu were noted in the panic patients, which suggests that parasympathetic activity decreases and sympathovagal balance increases in panic disorder patients. These findings are consistent with some previous reports (8, 10). With respect to 5-HTT function, recent genetic studies have shown that anxiety disorder is associated with gene variants related to reduced expression of 5-HTT both in the brain and on the platelets, and reduced expression of 5-HTT leads to decreased 5-HT uptake (15, 24, 25). In line with these results, low Vmax in this study can be considered to reflect a primary pathophysiological mechanism in panic disorder, resulting in serotonergic overactivity in the synapses, whereas the low Km in this study may be the result of secondary and compensatory processes to the serotonergic overactivity.
Some preclinical studies provide an explanation for the interactions between 5-HTT and the sympathoadrenal system. Fox et al. (26) reported that 5-HTT knockout mice showed exaggerated serotonin syndrome behavior and physiological responses because of impaired 5-HT uptake function. Other researchers have shown that decreased 5-HTT function is also related to exaggerated sympathoadrenal and neuroendocrine responses to stress (27, 28), and one function of 5-HTT is to restrain adrenomedullary activation in response to stress (27). Our results extend the relationship between the impaired 5-HTT and dysregulation of autonomic nervous function to panic disorder patients.
Our results suggest that decreased 5-HTT function is related to HRV abnormalities in patients with PD, and that Km could be a quantitative predictor of autonomic dysfunction in panic patients. Impaired HRV has been known to be associated with increased cardiac morbidity and mortality, and some researchers have reported that PD is related to increased cardiac risk (2, 3). In the present study, panic disorder patients showed decreased parasympathetic and increased sympathovagal tones in terms of HRV indices. Taken together, abnormalities of 5-HTT function, specifically low Km, would be a cardiac risk factor in patients with PD.
There are some limitations in this study. This was a cross-sectional study, limiting our inference on the causal direction. And the sample size was relatively small to generalize our hypothesis in panic disorder. In addition, the healthy controls were just age-matched subjects, although gender difference may affect the results. Several studies have reported conflicting results (29, 30) of HRV measures regarding gender difference. However, sex distribution of the two groups was not statistically different in this study, and gender did not affect HRV indices in the regression model (Table 3).
In conclusion, patients with panic disorder showed abnormalities in platelet 5-HTT function and HRV indexes, and low affinity of 5-HTT could independently predict increased sympathovagal activity in panic patients. Thus, we suggest that impaired 5-HTT function may be closely related to dysregulation of autonomic nervous system in panic disorder.
ACKNOWLEDGEMENT
This study was supported by Samsung Biomedical Research Institute (SBRI) grant CA6-218-3 and Samsung Medical Center Clinical Research Development Program (CRDP) grant CRS107-48-2. The authors would like to express their gratitude to Dr. Seonwoo Kim for her valuable support and advice on the statistical analyses in this research.
References
- 1.Son SJ, Kim SJ, Kim CH. Quality of life for patients with obsessive-compulsive disorder and panic disorder. J Korean Neuropsychiatr Assoc. 2006;45:438–443. [Google Scholar]
- 2.Kawachi I, Colditz GA, Ascherio A, Rimm EB, Giovannucci E, Stampfer MJ, Willett WC. Prospective study of phobic anxiety and risk of coronary heart disease in men. Circulation. 1994;89:1992–1997. doi: 10.1161/01.cir.89.5.1992. [DOI] [PubMed] [Google Scholar]
- 3.Smoller JW, Pollack MH, Wassertheil-Smoller S, Jackson RD, Oberman A, Wong ND, Sheps D. Panic attacks and risk of incident cardiovascular events among postmenopausal women in the Women's Health Initiative Observational Study. Arch Gen Psychiatry. 2007;64:1153–1160. doi: 10.1001/archpsyc.64.10.1153. [DOI] [PubMed] [Google Scholar]
- 4.Akselrod S, Gordon D, Ubel FA, Shannon DC, Berger AC, Cohen RJ. Power spectrum analysis of heart rate fluctuation: a quantitative probe of beat-to-beat cardiovascular control. Science. 1981;213:220–222. doi: 10.1126/science.6166045. [DOI] [PubMed] [Google Scholar]
- 5.Lavoie KL, Fleet RP, Laurin C, Arsenault A, Miller SB, Bacon SL. Heart rate variability in coronary artery disease patients with and without panic disorder. Psychiatry Res. 2004;128:289–299. doi: 10.1016/j.psychres.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 6.Klein E, Cnaani E, Harel T, Braun S, Ben-Haim SA. Altered heart rate variability in panic disorder patients. Biol Psychiatry. 1995;37:18–24. doi: 10.1016/0006-3223(94)00130-U. [DOI] [PubMed] [Google Scholar]
- 7.Yeragani VK, Tancer M, Uhde T. Heart rate and QT interval variability: abnormal alpha-2 adrenergic function in patients with panic disorder. Psychiatry Res. 2003;121:185–196. doi: 10.1016/s0165-1781(03)00235-x. [DOI] [PubMed] [Google Scholar]
- 8.Yeragani VK, Pohl R, Srinivasan K, Balon R, Ramesh C, Berchou R. Effects of isoproterenol infusions on heart rate variability in patients with panic disorder. Psychiatry Res. 1995;56:289–293. doi: 10.1016/0165-1781(95)02608-y. [DOI] [PubMed] [Google Scholar]
- 9.Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Heart rate variability: standards of measurement, physiological interpretation and clinical use. Circulation. 1996;93:1043–1065. [PubMed] [Google Scholar]
- 10.Yeragani VK, Pohl R, Berger R, Balon R, Ramesh C, Glitz D, Srinivasan K, Weinberg P. Decreased heart rate variability in panic disorder patients: a study of power-spectral analysis of heart rate. Psychiatry Res. 1993;46:89–103. doi: 10.1016/0165-1781(93)90011-5. [DOI] [PubMed] [Google Scholar]
- 11.Alvarenga ME, Richards JC, Lambert G, Esler MD. Psychophysiological mechanisms in panic disorder: a correlative analysis of noradrenaline spillover, neuronal noradrenaline reuptake, power spectral analysis of heart rate variability, and psychological variables. Psychosom Med. 2006;68:8–16. doi: 10.1097/01.psy.0000195872.00987.db. [DOI] [PubMed] [Google Scholar]
- 12.Iny LJ, Pecknold J, Suranyi-Cadotte BE, Bernier B, Luthe L, Nair NP, Meaney MJ. Studies of a neurochemical link between depression, anxiety, and stress from [3H]imipramine and [3H]paroxetine binding on human platelets. Biol Psychiatry. 1994;36:281–291. doi: 10.1016/0006-3223(94)90625-4. [DOI] [PubMed] [Google Scholar]
- 13.Norman TR, Judd FK, Gregory M, James RH, Kimber NM, McIntyre IM, Burrows GD. Platelet serotonin uptake in panic disorder. J Affect Disord. 1986;11:69–72. doi: 10.1016/0165-0327(86)90062-5. [DOI] [PubMed] [Google Scholar]
- 14.Kang EH, Shim HB, Kim KJ, Park JE, Lee IS, Yu BH. Platelet serotonin transporter function after short-term paroxetine treatment in patients with panic disorder. Psychiatry Res. doi: 10.1016/j.psychres.2008.12.007. (In Press) [DOI] [PubMed] [Google Scholar]
- 15.Lesch KP, Bengel D, Heils A, Sabol SZ, Greenberg BD, Petri S, Benjamin J, Muller CR, Hamer DH, Murphy DL. Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science. 1996;274:1527–1531. doi: 10.1126/science.274.5292.1527. [DOI] [PubMed] [Google Scholar]
- 16.Ballenger JC. Remission rates in patients with anxiety disorders treated with paroxetine. J Clin Psychiatry. 2004;65:1696–1707. doi: 10.4088/jcp.v65n1216. [DOI] [PubMed] [Google Scholar]
- 17.Camacho A, Dimsdale JE. Platelets and psychiatry: lessons learned from old and new studies. Psychosom Med. 2000;62:326–336. doi: 10.1097/00006842-200005000-00006. [DOI] [PubMed] [Google Scholar]
- 18.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders. New York: New York State Psychiatric Institute; 1996. [Google Scholar]
- 19.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 20.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lim YJ, Yu BH, Kim JH. Korean panic disorder severity scale: construct validity by confirmatory factor analysis. Depress Anxiety. 2007;24:95–102. doi: 10.1002/da.20206. [DOI] [PubMed] [Google Scholar]
- 22.Esler M, Lambert E, Alvarenga M, Socratous F, Richards J, Barton D, Pier C, Brenchley C, Dawood T, Hastings J, Guo L, Haikerwal D, Kaye D, Jennings G, Kalff V, Kelly M, Wiesner G, Lambert G. Increased brain serotonin turnover in panic disorder patients in the absence of a panic attack: reduction by a selective serotonin reuptake inhibitor. Stress. 2007;10:295–304. doi: 10.1080/10253890701300904. [DOI] [PubMed] [Google Scholar]
- 23.Maron E, Shlik J. Serotonin function in panic disorder: important, but why? Neuropsychopharmacology. 2006;31:1–11. doi: 10.1038/sj.npp.1300880. [DOI] [PubMed] [Google Scholar]
- 24.Lin PY. Meta-analysis of the association of serotonin transporter gene polymorphism with obsessive-compulsive disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2007;31:683–689. doi: 10.1016/j.pnpbp.2006.12.024. [DOI] [PubMed] [Google Scholar]
- 25.Kim SJ, Seok JH, Kim CH. Serotonin transporter and pharmacotherapy. Korean J Psychopharmacol. 2006;17:263–272. [Google Scholar]
- 26.Fox MA, Jensen CL, French HT, Stein AR, Huang SJ, Tolliver TJ, Murphy DL. Neurochemical, behavioral, and physiological effects of pharmacologically enhanced serotonin levels in serotonin transporter (SERT)-deficient mice. Psychopharmacology (Berl) 2008;201:203–218. doi: 10.1007/s00213-008-1268-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murphy DL, Lesch KP. Targeting the murine serotonin transporter: insights into human neurobiology. Nat Rev Neurosci. 2008;9:85–96. doi: 10.1038/nrn2284. [DOI] [PubMed] [Google Scholar]
- 28.Tjurmina OA, Armando I, Saavedra JM, Goldstein DS, Murphy DL. Exaggerated adrenomedullary response to immobilization in mice with targeted disruption of the serotonin transporter gene. Endocrinology. 2002;143:4520–4526. doi: 10.1210/en.2002-220416. [DOI] [PubMed] [Google Scholar]
- 29.Kuo TB, Lin T, Yang CC, Li CL, Chen CF, Chou P. Effect of aging on gender differences in neural control of heart rate. Am J Physiol. 1999;277:H2233–H2239. doi: 10.1152/ajpheart.1999.277.6.H2233. [DOI] [PubMed] [Google Scholar]
- 30.Ramaekers D, Ector H, Aubert AE, Rubens A, Van de Werf F. Heart rate variability and heart rate in healthy volunteers. Is the female autonomic nervous system cardioprotective? Eur Heart J. 1998;19:1334–1341. doi: 10.1053/euhj.1998.1084. [DOI] [PubMed] [Google Scholar]