Abstract
Background
The timely and accurate identification of symptoms of ACS is a challenge for patients and clinicians. It is unknown whether response times and clinical outcomes differ with specific symptoms. We sought to identify which acute coronary syndrome (ACS) symptoms are related—symptom clusters—and to determine if sample characteristics, response times, and outcomes differ among symptom cluster groups.
Methods
In a multisite randomized clinical trial, 3522 patients with known cardiovascular disease were followed for two years. During follow-up, 331 (11%) had a confirmed ACS event. In this group, eight presenting symptoms were analyzed using cluster analysis. Differences in symptom cluster group characteristics, delay times, and outcomes were examined.
Results
The sample was predominately male (67%), older (mean 67.8, S.D. 11.6 years), and white (90%). Four symptom clusters were identified: Classic ACS characterized by chest pain; Pain Symptoms (neck, throat, jaw, back, shoulder, arm pain); Stress Symptoms (shortness of breath, sweating, nausea, indigestion, dread, anxiety), and Diffuse Symptoms, with a low frequency of most symptoms. Those in the Diffuse Symptoms cluster tended to be older (p=.08) and the Pain Symptoms group was most likely to have a history of angina (p=.01). After adjusting for differences, the Diffuse Symptoms cluster demonstrated higher mortality at two years (17%) than the other three clusters (2–5%, p<.001), even though prehospital delay time did not differ significantly.
Conclusion
Most ACS symptoms occur in groups or clusters. Uncharacteristic symptom patterns may delay diagnosis and treatment by clinicians even when patients seek care rapidly. Knowledge of common symptom patterns may facilitate rapid identification of ACS.
Keywords: acute coronary syndrome, delay in seeking treatment, mortality
Introduction
In ACS, symptoms are an important early indicator of the need to seek care. Patients have great difficulty determining the importance of their symptoms, however, and prehospital delay in seeking care continues to be a problem in this population.1 Clinicians also struggle to diagnose ACS in the early hours before cardiac biomarkers rise. We reasoned that if clusters of ACS symptoms that patient experience could be identified, early recognition of ACS, early diagnosis, and outcomes might be improved.
The National Heart, Lung and Blood Institute and the American Heart Association publicize typical symptoms of AMI, which include chest discomfort (e.g., pressure, squeezing, fullness, or pain) that radiates to the arms, back, neck, jaw, or “stomach”, shortness of breath, sweating, nausea, and light-headedness.2 No mention is made, however, of symptom patterns or the likelihood of these symptoms occurring simultaneously.
A symptom cluster is defined as two or more symptoms that are related to each other and that occur together.3 Symptom clusters have been examined in other illnesses, most commonly cancer,4, 5 and found to aid in assessment by enhancing pattern recognition.6 Cardiac symptom clusters are just beginning to be investigated.7
Only three studies using cluster analysis in ACS patients were located. In a sample of 212 patients admitted with acute chest pain, Eslick8 clustered chest pain characteristics and locations using k-means cluster analysis in an attempt to differentiate cardiac from non-cardiac chest pain. They concluded that there is considerable overlap in patients with cardiac and non-cardiac chest pain and discouraged providers from making a diagnosis based on pain location and patient description. In a secondary analysis of 1,073 people having an acute myocardial infarction (AMI), Ryan and colleagues 9 identified five symptom clusters using latent class cluster analysis. They concluded that none of their five symptom clusters included all the classic symptoms of ACS (chest discomfort, diaphoresis, shortness of breath, nausea, and lightheadedness) and recommended that symptom clusters be communicated to the public to help them assess their symptoms more effectively. Lindgren et al10 clustered cardiac symptoms occurring prior to hospitalization for ACS in 247 elderly patients. Using cluster analysis to categorize patients with similar symptom profiles, they identified three symptom clusters: classic ACS symptoms, diffuse symptoms, and a “weary” (severe fatigue, sleep disturbance, and shortness of breath) pattern in patients most likely to have a history of heart failure. They concluded that further research was needed to clarify the relationships among symptoms and health outcomes.
In this study we identified ACS symptom clusters. Then we compared the cluster groups to identify demographic and clinical differences among the groups. Finally, differences in the number of emergency department (ED) visits, prehospital delay time, and mortality were compared in the cluster groups.
Methods
The data for this study were obtained from the randomized, controlled PROMOTION clinical trial (Clinical Trial Registration: URL http://clinicaltrials.gov/ct2/show/NCT00734760#NCT00734760), details of which have been published elsewhere.11 Briefly, the PROMOTION trial tested a secondary prevention intervention of education and counseling intended to reduce prehospital delay in response to ACS symptoms. Patients were eligible for the study if they had a history of CAD (e.g., prior AMI), clinical atherosclerotic disease of the aorta or peripheral arteries, or clinical cerebrovascular disease, based on the recommendations of the National Heart Attack Alert Program12, 13 and lived in the community. Exclusion criteria were: 1) complicating serious comorbidity such as a major psychiatric illness, 2) untreated malignancy or neurological disorder that impaired cognition, 3) inability to understand spoken or written English, and 4) major and uncorrected hearing loss. Between 2001 and 2004, subjects were enrolled from five centers; three in the United States and one each in Australia and New Zealand and followed for two years. The local Institutional Review Board at each site approved the study and all participants gave informed consent.
Sample
A convenience sample of 3522 persons was enrolled into the parent trial. Over the two year follow-up period, 565 (16%) patients visited an ED. The main outcome of interest in the parent trial was time from ACS symptom onset to arrival at the ED (i.e., prehospital delay time) during the two year follow-up period. Prehospital delay time was measured as the time from symptom onset to hospital presentation and obtained from the hospital medical record. If no notation was found in the medical record, delay time was obtained from the emergency medical system (EMS) prehospital medical reports.
Intervention
Experimental group subjects received a face-to-face educational intervention of approximately 40 minutes duration, administered by a cardiovascular nurse.11 The intervention addressed informational, emotional, and social factors known to increase delay in response to symptoms. Any negative events associated with prior experience in seeking care were discussed in the context of the current informational message. Patients were asked to bring to the intervention session their spouse, a significant other, or the person most likely to be called upon to help. Supporters were “deputized” to act as the decision maker if the patient hesitated to call EMS. Scenarios, role-playing, and rehearsal were used to accomplish the intervention goals.
Few significant group (experimental or control) differences were found in subject characteristics at baseline.14 After two years of follow-up, no significant group differences were found in the number of ED visits, mortality, or prehospital delay time; median prehospital delay time was 2.20 hours in the experimental group vs. 2.25 in the control group.
Procedure
In the current study, all participants who sought care at an ED and were subsequently hospitalized for a documented ACS event were included (N=331; 9% of sample). Comparability of the experimental and control groups at baseline and in outcomes supported our decision to combine the groups for this analysis.
During follow-up in the parent trial, participants were identified as having sought care for ACS symptoms after patients called the research office to report an event, through routine review of affiliated hospital records, and during routine telephone follow-up calls. All ACS events were verified the medical records by registered nurse research assistants. Participants who sought care were interviewed by research assistants, usually within days of hospital discharge, to identify which cardiac symptoms prompted them to seek care.
Symptoms were measured by scripted telephone interview with items adapted from the REACT Trial.15 Patients were asked about seven symptoms: 1) chest pain, discomfort or pressure; 2) left arm pain or discomfort; 3) shortness of breath; 4) sweating; 5) upset stomach; 6) discomfort in the area between the breastbone and navel; and 7) a sense of dread. An open-ended question about “other” symptoms generated 135 unique responses. The primary investigator used content analysis to classify these responses.16 No attempt was made to reconcile patient reports with the medical record.
On content analysis, some symptoms occurred in so few and differed so much from others, that they could not be grouped (e.g., difficulty urinating; feeling cold). Others were similar to those suggested to patients and were added to existing categories (e.g., right arm pain was added to the left arm discomfort category and named arm pain or discomfort). The rest were grouped into these seven categories: 1) dizzy, lightheaded, feeling faint, passed out; 2) fatigued, tired, weak; 3) headache; 4) numbness, tingling; 5) back or shoulder pain; 6) neck, throat, or jaw pain; and 7) palpitations. All of these categories had at least five responses each.
When these 14 symptoms (7 suggested to patients and 7 from the content analysis) were analyzed, six occurred in fewer than 5% (n=17) and were not used further in analysis. One deleted symptom was from the list of suggested symptoms, discomfort in the area between the breastbone and navel (n=12); the other five came from the content analysis of patient responses: dizzy, lightheaded, feeling faint, passed out (n=12); fatigued, tired, weak (n=8); headache (n=5); numbness, tingling (n=7); and palpitations (n=13).
Analysis
Two approaches to symptom clustering have been used.17 The first approach involves the grouping of symptoms by factor or cluster analytic techniques, or a combination of the two.18 The second approach involves identifying subgroups of patients at risk for specific symptom clusters. Cluster analysis or latent class analysis can be used to identify patient subgroups. In this study, the eight symptoms were analyzed using two-step cluster analysis, which accommodates categorical variables. The log-likelihood distance measure was used, with subjects categorized under the cluster associated with the largest log-likelihood.19 No prescribed number of clusters was suggested. The Bayesian Information Criterion was used to judge adequacy of the final solution.
Associations between symptoms reported were assessed using bivariate Chi-square tests of association. Univariate differences in sample characteristics were compared according to cluster membership using one-way ANOVA models and chi-square statistics for continuous and categorical variables, respectively. For the analysis of continuous variables, the model assumption for variance homogeneity was assessed using Levine’s tests. Outcome measures included number of ED visits at two years among subjects with at least 24 months follow-up, pre-hospital delay time on a logarithmic scale, and mortality. Simple Poisson, general linear, and Cox regression models were used to assess cluster membership as an independent predictor of ED visits, pre-hospital delay time (transformed on the log scale or categorized as < 2 hours or ≥ 2 hours)20, and mortality, respectively; multivariate models were also generated for outcome, with adjustment for variables significant in preliminary analyses, as well as primary ED admission diagnosis. Age was included in the multivariate models of outcome due to its known prognostic importance. Statistical significance was demonstrated on the basis of a p-value less than 0.05.
Results
The sample of 331 patients was predominately male (67%), older (mean 67.8, SD 11.6 years), white (91%), educated beyond high school (61%), married (63%), and retired (80%). Most had a history of prior AMI (61%) and most were under the care of a cardiologist (84%). Most were admitted with a diagnosis of unstable angina (60%).
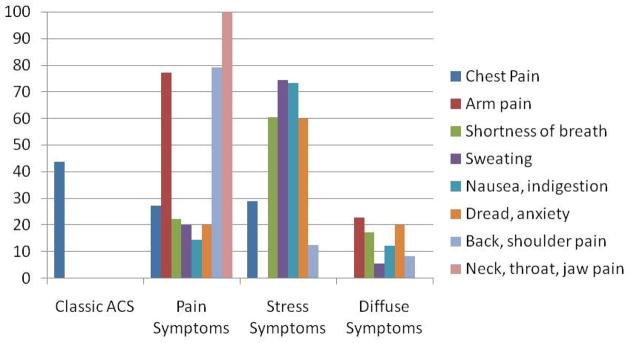
Frequencies for each of the eight symptoms analyzed are shown in Table 1. When the eight symptoms were examined for association, six symptom pairs were significantly related (Table 2). Based on the BIC criterion and log-likelihood distance, four clusters were identified (Figure 1). For four clusters, the BIC ratio of change was 0.581, which was maximum among clusters of four or higher, and the ratio of distances was 1.557, maximum among all solutions.
Table 1.
Frequency of Individual Symptoms Reported by the Sample of Acute Coronary Syndrome Patients (N = 331)
| Symptom | Frequency | Percent |
|---|---|---|
| Chest pain, discomfort or pressure | 259 | 78% |
| Shortness of breath | 81 | 24% |
| Arm pain or discomfort | 70 | 21% |
| Upset stomach, nausea, indigestion | 41 | 12% |
| Sweating | 35 | 11% |
| Sense of dread, anxious | 25 | 8% |
| Pain in the back or shoulder | 24 | 5% |
| Pain in the neck, throat, or jaw | 23 | 5% |
Table 2.
Associations between Symptoms Reported by the Patients with Acute Coronary Syndrome (N=331)
| Chest pain, discomfort or pressure | Arm pain or discomfort | Shortness of breath | Sweating | Upset stomach, nausea, indigestion | Dread, anxiety | Back, shoulder pain | |
|---|---|---|---|---|---|---|---|
| Arm pain or discomfort | χ2 = 0.34 P = 0.56 |
||||||
| Shortness of breath | χ2 = 0.25 P = 0.62 |
χ2 = 1.47 P = 0.23 |
|||||
| Sweating | χ2 = 0.49 P = 0.49 |
χ2 = 0.03 P = 0.86 |
χ2 = 22.60 P < .0001 |
||||
| Upset stomach, nausea, indigestion | χ2 = 0.00 P = 0.97 |
χ2 = 0.08 P = 0.78 |
χ2 = 0.58 P = 0.45 |
χ2 = 6.41 P = 0.01 |
|||
| Dread, anxiety | χ2 = 0.62 P = 0.43 |
χ2 = 0.76 P = 0.38 |
χ2 = 14.54 P < .0001 |
χ2 = 18.49 P < .0001 |
χ2 = 3.36 P = 0.07 |
||
| Back or shoulder pain | χ2 = 0.16 P = 0.69 |
χ2 = 1.00 P = 0.32 |
χ2 = 0.31 P = 0.58 |
χ2 = 0.14 P = 0.71 |
χ2 = 0.00 P = 0.99 |
χ2 = 0.43 P = 0.51 |
|
| Neck, throat or jaw pain | χ2 = 1.10 P = 0.29 |
χ2 = 4.79 P = 0.03 |
χ2 = 3.33 P = 0.07 |
χ2 = 1.01 P = 0.31 |
χ2 = 1.47 P = 0.23 |
χ2 = 2.02 P = 0.16 |
χ2 = 7.72 P = 0.01 |
Bolding highlights significant associations.
Figure 1. Differences in the Distribution of Symptoms within Each Symptom Cluster.
Patients with Classic ACS had chest pain. Those in the Pain Symptoms cluster presented primarily with arm, back, shoulder, neck, throat, and jaw pain. Those with the Diffuse Symptoms cluster had a wide variety of symptoms.
Chest pain loaded independently and was called Classic ACS (n=113). The second cluster contained primarily arm, back, shoulder, neck, throat, and jaw pain; this cluster was named Pain Symptoms (n=75). In the third cluster, shortness of breath, sweating, nausea, indigestion, dread, and anxiety were predominant, so this cluster was named Stress Symptoms (n=80). A fourth cluster contained most of the symptoms, but since none was highly represented, this factor was named Diffuse Symptoms (n=63).
When differences among the cluster groups were examined, those in the Diffuse Symptoms cluster tended to be older (p=.08) (Table 3). There were no gender differences in symptom clusters. The only clinical characteristic that differed among the clusters was a history of angina; those in the Pain Symptoms cluster group were most likely to have a history of angina (p=.01). The proportion of patients delaying 2 hours or more was comparable and not significantly different among the groups.
Table 3.
Demographic and Clinical Comparisons by Cluster Groups
| Characteristic | Cluster 1 | Cluster 2 | Cluster 3 | Cluster 4 |
|---|---|---|---|---|
| Classic ACS | Pain Symptoms | Stress Symptoms | Diffuse Symptoms | |
| N=113 | N=75 | N=80 | N=63 | |
| Age | 67.1 (SD 11.7) | 67.0 (SD 11.1) | 66.7 (SD 12.7) | 71.2 (SD 10.4) |
| Females | 27% | 39% | 37% | 32% |
| Caucasian ethnicity | 90% | 89% | 94% | 90% |
| Married | 64% | 51% | 62% | 67% |
| High school education or less | 36% | 53% | 40% | 33% |
| Household income ≤ $30,000 annually | 46% | 62% | 53% | 42% |
| Insured for emergency use | 96% | 97% | 92% | 98% |
| Insured for ambulance use | 93% | 92% | 93% | 100% |
| Current smoker | 3% | 12% | 8% | 5% |
| Sedentary lifestyle | 33% | 28% | 36% | 35% |
| History of angina (p=.01) | 79% | 85% | 71% | 62% |
| History of myocardial infarction | 58% | 61% | 64% | 65% |
| History of diabetes | 29% | 16% | 31% | 27% |
| Has attended cardiac rehabilitation | 47% | 46% | 53% | 40% |
| Admission diagnosis | ||||
| • Unstable angina | 64% | 65% | 64% | 43% |
| • Acute myocardial infarction | 11% | 8% | 12% | 24% |
| Delayed ≥ 2 hours before seeking care | 61% | 51% | 55% | 57% |
Groups were compared using one-way ANOVA model for age and Chi-square statistics for the remaining variables.
Significant differences are highlighted.
Multivariate models with adjustment for age, angina history, and specific ACS diagnosis are in Table 4. In both simple and multivariate models, the number of ED visits and prehospital delay time did not differ significantly among the groups. Multivariate Cox proportional hazards modeling demonstrated that symptom cluster was a significant predictor of mortality (Table 5); with adjustment for history of angina and ED diagnosis as AMI, those in the Diffuse Symptoms cluster had significantly higher mortality than those with Classic ACS (p=.002), Pain Symptoms (p=.017), and Stress Symptoms (p=.037). Figure 2 displays Kaplan-Meier estimates of mortality according to the four symptom cluster groups, illustrating significantly higher two-year mortality estimates in the Diffuse Symptoms cluster (17% versus 2–5% in the other three clusters, log rank p<.001).
Table 4.
Multivariate Regression Modeling of Emergency Department Visits (n=229) and Prehospital Delay Time (n=331) by Symptom Cluster Group, with adjustment for age and history of angina
| β | SE | p |
CI |
||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Emergency Department Visit (Poisson Model) | |||||
| Age | −0.01 | 0.01 | 0.123 | −0.02 | 0.00 |
| No History of angina | −0.30 | 0.11 | 0.006 | −0.51 | −0.08 |
| Primary ED diagnosis-Unstable Angina | 0.07 | 0.12 | 0.586 | −0.18 | 0.31 |
| Primary ED diagnosis-AMI | 0.30 | 0.13 | 0.028 | 0.03 | 0.56 |
| Classic ACS Cluster | −0.19 | 0.17 | 0.249 | −0.52 | 0.13 |
| Pain Symptoms Cluster | 0.05 | 0.19 | 0.783 | −0.32 | 0.43 |
| Stress Symptoms Cluster | −0.15 | 0.18 | 0.420 | −0.50 | 0.21 |
| Prehospital Delay Time (GLM) | |||||
| Age | 0.01 | 0.01 | 0.755 | −0.01 | 0.01 |
| No History of angina | 0.02 | 0.07 | 0.821 | −0.12 | 0.15 |
| Primary ED diagnosis-Unstable Angina | −0.04 | 0.07 | 0.604 | −0.17 | 0.10 |
| Primary ED diagnosis-AMI | 0.06 | 0.11 | 0.610 | −0.16 | 0.27 |
| Classic ACS Cluster | −0.02 | 0.08 | 0.791 | −0.19 | 0.14 |
| Pain Symptoms Cluster | −0.03 | 0.09 | 0.758 | −0.21 | 0.15 |
| Stress Symptoms Cluster | −0.09 | 0.10 | 0.344 | −0.28 | 0.10 |
Note: Baseline for History of angina is “Yes”; baseline for primary ED diagnosis is “Not Unstable Angina” or “Not AMI”; baseline for Symptom Cluster is “Diffuse Symptoms”.
Table 5.
Stepwise Cox Proportional Hazards Regression Modeling of Mortality by Symptom Cluster Group, with adjustment for age, history of angina, primary ED diagnosis for unstable angina and AMI
| β | SE | HR | p |
CI |
||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| No History of angina | −1.72 | 0.77 | .18 | .025 | .04 | .80 |
| Symptom cluster | .002 | |||||
| Classic ACS vs. Diffuse Symptoms | −3.12 | 1.05 | .04 | .002 | .01 | .32 |
| Pain Symptoms vs. Diffuse Symptoms | −1.86 | 0.78 | .16 | .017 | .03 | .72 |
| Stress Symptoms vs. Diffuse Symptoms | −1.24 | 0.60 | .29 | .037 | .09 | .93 |
| Primary ED diagnosis of AMI | −2.37 | 0.49 | .09 | .000 | .04 | .25 |
HR=Hazard Ratio or Exp(B)
Age and primary ED diagnosis for unstable angina not significant at 0.05 level
Note: Baseline for History of angina is “Yes”; baseline for primary ED diagnosis is “Not Unstable Angina” or “Not AMI”; baseline for Symptom Cluster is “Diffuse Symptoms”.
Figure 2. Kaplan-Meier estimates of mortality according to the four symptom cluster groups.
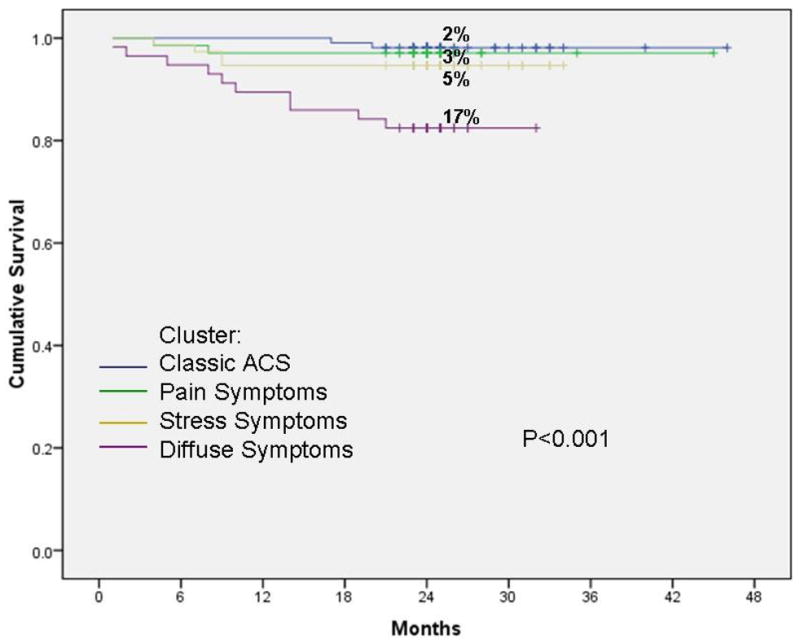
Patients with the Diffuse Symptoms cluster had significantly higher mortality rates during the two year follow-up compared to patients admitted to the hospital with one of the other three symptom profiles.
This work was funded by the National Institute of Nursing Research grant R01 NR05323. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Discussion
Four symptom clusters were identified in this sample of patients with known CAD who were hospitalized with a diagnosis of ACS. Although prehospital delay time and number of ED visits did not differ among the symptom cluster groups, those with the Diffuse Symptoms pattern had significantly higher mortality rates within the two years of follow-up.
One explanation for the increase in mortality among those with Diffuse Symptoms, in spite of comparable prehospital delay times, is that clinicians may have difficulty diagnosing ACS with an atypical presentation. It may be that patients presenting with this cluster are not treated as rapidly as those with the other symptom patterns, and they may receive less aggressive treatment of symptoms or have ischemic episodes that are missed by clinicians.21 Attention to this cluster of symptoms may heighten suspicion and facilitate early diagnosis and treatment of these patients.
The clusters identified are similar to those found by Lindgren et al10 in that they also identified a Classic ACS cluster and a Diffuse Symptoms cluster. However, their Classic ACS cluster included fatigue, which was one of the symptoms reported by so few in our sample that it could not be used in the cluster analysis. Their cluster of Diffuse Symptoms was characterized by low symptom intensity. We did not measure intensity, just the occurrence of various symptoms. So, in our study the diffuse pattern reflected a low frequency, diffuse pattern of symptoms. The Diffuse Symptoms cluster is also similar to a cluster described by Ryan et al,9 who identified one cluster without any high probability symptoms.
The Stress Symptoms cluster of shortness of breath, sweating, dread, and anxiety is difficult to diagnose because the symptoms are similar to those experienced during a panic attack.22 The challenge for clinicians is to attribute the symptom cluster to the correct diagnostic category. Some guidance is found in the study by Meuret and colleagues22 who evaluated clusters of panic attack symptoms and identified three factors. Importantly, shortness of breath, sweating, and anxiety all loaded on different factors, suggesting that when these symptoms are combined, they signal ACS, not panic disorder. Thus, ACS should be suspected when encountering this cluster of symptoms until proven otherwise.
It was surprising that no gender differences were found in the symptom clusters, based on prior research,23 but this may be due to the fact that fatigue, the primary symptom in women,24 was not able to be included in the analysis. Others have found a higher rate of arm, neck, throat, and jaw pain in women than men,25 so we expected to find that women were more likely to experience the Pain Symptoms cluster more than men. The difference in our results may reflect differences in the manner in which symptoms were measured.
A notable finding is the high percentage of both men and women in the current study who experienced chest pain, discomfort or pressure associated with ACS. Others have found that patients hospitalized for AMI and presenting with symptoms other than chest pain were most likely to be female and older.26 Our results suggest that high percentages of both men and women report chest pain. These results are consistent with those of prior investigators who found that chest pain is a major symptom of ACS in both men and women.26, 27
Limitations
Limitations of this study include the retrospective nature of data collection. Participants were interviewed as quickly as possible following hospitalization, but we asked about the symptoms that brought them into the hospital and some period of time had passed since the event. Another limitation is the method used to collect data on symptoms. Although standardized scripts and procedures were used to elicit symptoms, a longer list of possible symptoms and one that measured intensity rather than just incidence would have been useful. We also combined some symptoms to allow them to be included (e.g., dread was combined with anxiety) and our combinations could be questioned by others. The Diffuse Symptoms cluster, the cluster associated with higher mortality, had the smallest number of patients and requires further investigation to confirm whether or not the trend is consistent with others. However, a similar cluster has been found in two prior studies, lending more credence to this result.9, 10
The results of this study are limited by the participants enrolled: individuals with prior CVD who chose to sit through a 40 minute educational session. Most participants were white, limiting analyses of racial/ethnic group differences. Further research is needed to replicate these results, test the veracity of the clusters, and to determine if these symptom clusters are found in other racial/ethnic groups.
In summary, we have identified four ACS symptom clusters. Some of the symptoms that grouped together could be interpreted as vague (e.g., shortness of breath) or nonspecific (e.g., neck pain) in isolation, but in the context of the other symptoms in the cluster, patients and clinicians may identify ACS more readily. Mortality was higher in those experiencing the Diffuse Symptoms cluster. Based on these results we advocate an increased index of suspicion for patients with an atypical symptom presentation. Patients with more than one vague symptom should be suspected to have ACS.
Acknowledgments
This work was funded by the National Institute of Nursing Research grant R01 NR05323.
Abbreviations list
- ACS
acute coronary syndrome
- AMI
acute myocardial infarction
- BMI
body mass index
- CAD
coronary artery disease
- ED
emergency department
- EMS
emergency medical system
- SD
standard deviation
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Barbara Riegel, Professor, School of Nursing, University of Pennsylvania, Philadelphia, PA.
Alexandra L. Hanlon, Research Associate Professor of Biostatistics, School of Nursing, University of Pennsylvania, Philadelphia, PA.
Sharon McKinley, Professor of Critical Care Nursing, Faculty of Nursing Midwifery and Health, University of Technology Sydney and Northern Sydney Central Coast Health.
Debra K. Moser, Professor, College of Nursing, University of Kentucky, Lexington, KY.
Hendrika Meischke, Professor, Department of Health Services, University of Washington, Seattle, WA.
Lynn V. Doering, Professor, School of Nursing, University of California, Los Angeles, CA.
Patricia Davidson, Professor, Curtin University, Australia.
Michele M. Pelter, Assistant Professor, Orvis School of Nursing, University of Nevada, Reno, NV.
Kathleen Dracup, Professor and Dean, School of Nursing, University of California, San Francisco, CA.
References
- 1.Moser DK, Kimble LP, Alberts MJ, Alonzo A, Croft JB, Dracup K, Evenson KR, Go AS, Hand MM, Kothari RU, Mensah GA, Morris DL, Pancioli AM, Riegel B, Zerwic JJ. Reducing delay in seeking treatment by patients with acute coronary syndrome and stroke: a scientific statement from the American Heart Association Council on Cardiovascular Nursing and Stroke Council. J Cardiovasc Nurs. 2007;22(4):326–343. doi: 10.1097/01.JCN.0000278963.28619.4a. [DOI] [PubMed] [Google Scholar]
- 2.American Heart Association. Heart Attack, Stroke and Cardiac Arrest Warning Signs. [Accessed July 30, 2009.];American Heart Association. Available at: http://www.americanheart.org/presenter.jhtml?identifier=3053#Heart_Attack.
- 3.Kim HJ, McGuire DB, Tulman L, Barsevick AM. Symptom clusters: concept analysis and clinical implications for cancer nursing. Cancer Nurs. 2005;28(4):270–282. doi: 10.1097/00002820-200507000-00005. quiz 283-274. [DOI] [PubMed] [Google Scholar]
- 4.Gift AG. Symptom clusters related to specific cancers. Semin Oncol Nurs. 2007;23(2):136–141. doi: 10.1016/j.soncn.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Dodd M, Janson S, Facione N, Faucett J, Froelicher ES, Humphreys J, Lee K, Miaskowski C, Puntillo K, Rankin S, Taylor D. Advancing the science of symptom management. Journal of Advanced Nursing. 2001;33(5):668–676. doi: 10.1046/j.1365-2648.2001.01697.x. [DOI] [PubMed] [Google Scholar]
- 6.Miaskowski C, Dodd M, Lee K. Symptom clusters: the new frontier in symptom management research. J Natl Cancer Inst Monogr. 2004;(32):17–21. doi: 10.1093/jncimonographs/lgh023. [DOI] [PubMed] [Google Scholar]
- 7.Zimmerman L. Foreword: Cluster Analysis. Journal of Cardiac Nursing. 2010 [Google Scholar]
- 8.Eslick GD. Usefulness of chest pain character and location as diagnostic indicators of an acute coronary syndrome. Am J Cardiol. 2005;95(10):1228–1231. doi: 10.1016/j.amjcard.2005.01.052. [DOI] [PubMed] [Google Scholar]
- 9.Ryan CJ, DeVon HA, Horne R, King KB, Milner K, Moser DK, Quinn JR, Rosenfeld A, Hwang SY, Zerwic JJ. Symptom clusters in acute myocardial infarction: a secondary data analysis. Nurs Res. 2007;56(2):72–81. doi: 10.1097/01.NNR.0000263968.01254.d6. [DOI] [PubMed] [Google Scholar]
- 10.Lindgren TG, Fukuoka Y, Rankin SH, Cooper BA, Carroll D, Munn YL. Cluster analysis of elderly cardiac patients’ prehospital symptomatology. Nurs Res. 2008;57(1):14–23. doi: 10.1097/01.NNR.0000280654.50642.1a. [DOI] [PubMed] [Google Scholar]
- 11.Dracup K, McKinley S, Riegel B, Mieschke H, Doering LV, Moser DK. A nursing intervention to reduce prehospital delay in acute coronary syndrome: a randomized clinical trial. J Cardiovasc Nurs. 2006;21(3):186–193. doi: 10.1097/00005082-200605000-00006. [DOI] [PubMed] [Google Scholar]
- 12.Dracup K, Alonzo AA, Atkins JM, Bennett NM, Braslow A, Clark LT, Eisenberg M, Ferdinand KC, Frye R, Green L, Hill MN, Kennedy JW, Kline-Rogers E, Moser DK, Ornato JP, Pitt B, Scott JD, Selker HP, Silva SJ, Thies W, Weaver WD, Wenger NK, White SK. The physician’s role in minimizing prehospital delay in patients at high risk for acute myocardial infarction: recommendations from the National Heart Attack Alert Program. Working Group on Educational Strategies To Prevent Prehospital Delay in Patients at High Risk for Acute Myocardial Infarction. Ann Intern Med. 1997;126(8):645–651. doi: 10.7326/0003-4819-126-8-199704150-00010. [DOI] [PubMed] [Google Scholar]
- 13.Lenfant C, LaRosa JH, Horan MJ, Passamani ER. Considerations for a national heart attack alert program. Clin Cardiol. 1990;13(8 Suppl 8):VIII9–11. [PubMed] [Google Scholar]
- 14.Dracup K, McKinley S, Riegel B, Moser DK, Meischke H, Doering LV, Davidson P, Paul S, Baker H, Pelter M. A Randomized Clinical Trial to Reduce Patient Prehospital Delay to Treatment in Acute Coronary Syndrome. Circulation. doi: 10.1161/CIRCOUTCOMES.109.852608. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Simons-Morton DG, Goff DC, Osganian S, Goldberg RJ, Raczynski JM, Finnegan JR, Zapka J, Eisenberg MS, Proschan MA, Feldman HA, Hedges JR, Luepker RV. Rapid early action for coronary treatment: rationale, design, and baseline characteristics. REACT Research Group. Acad Emerg Med. 1998;5(7):726–738. doi: 10.1111/j.1553-2712.1998.tb02492.x. [DOI] [PubMed] [Google Scholar]
- 16.Sandelowski M. Combining qualitative and quantitative sampling, data collection and analysis techniques in mixed-methods studies. Research in Nursing and Health. 2000;23:246–255. doi: 10.1002/1098-240x(200006)23:3<246::aid-nur9>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 17.Miaskowski C, Aouizerat BE, Dodd M, Cooper B. Conceptual issues in symptom clusters research and their implications for quality-of-life assessment in patients with cancer. J Natl Cancer Inst Monogr. 2007;(37):39–46. doi: 10.1093/jncimonographs/lgm003. [DOI] [PubMed] [Google Scholar]
- 18.Eslick GD, Howell SC, Hammer J, Talley NJ. Empirically derived symptom sub-groups correspond poorly with diagnostic criteria for functional dyspepsia and irritable bowel syndrome. A factor and cluster analysis of a patient sample. Aliment Pharmacol Ther. 2004;19(1):133–140. doi: 10.1046/j.1365-2036.2003.01805.x. [DOI] [PubMed] [Google Scholar]
- 19.Melia M, Heckerman D. An experimental comparison of several clustering and initialization methods. 1998. [Google Scholar]
- 20.Goldstein P, Wiel E. Management of prehospital thrombolytic therapy in ST-segment elevation acute coronary syndrome (<12 hours) Minerva Anestesiol. 2005;71(6):297–302. [PubMed] [Google Scholar]
- 21.Booker KJ, Holm K, Drew BJ, Lanuza DM, Hicks FD, Carrigan T, Wright M, Moran J. Frequency and outcomes of transient myocardial ischemia in critically ill adults admitted for noncardiac conditions. Am J Crit Care. 2003;12(6):508–516. discussion 517. [PubMed] [Google Scholar]
- 22.Meuret AE, White KS, Ritz T, Roth WT, Hofmann SG, Brown TA. Panic attack symptom dimensions and their relationship to illness characteristics in panic disorder. J Psychiatr Res. 2006;40(6):520–527. doi: 10.1016/j.jpsychires.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 23.Milner KA, Vaccarino V, Arnold AL, Funk M, Goldberg RJ. Gender and age differences in chief complaints of acute myocardial infarction (Worcester Heart Attack Study) Am J Cardiol. 2004;93(5):606–608. doi: 10.1016/j.amjcard.2003.11.028. [DOI] [PubMed] [Google Scholar]
- 24.McSweeney JC, Cody M, O’Sullivan P, Elberson K, Moser DK, Garvin BJ. Women’s early warning symptoms of acute myocardial infarction. Circulation. 2003;108(21):2619–2623. doi: 10.1161/01.CIR.0000097116.29625.7C. [DOI] [PubMed] [Google Scholar]
- 25.Kosuge M, Kimura K, Ishikawa T, Ebina T, Hibi K, Tsukahara K, Kanna M, Iwahashi N, Okuda J, Nozawa N, Ozaki H, Yano H, Nakati T, Kusama I, Umemura S. Differences between men and women in terms of clinical features of ST-segment elevation acute myocardial infarction. Circ J. 2006;70(3):222–226. doi: 10.1253/circj.70.222. [DOI] [PubMed] [Google Scholar]
- 26.Arslanian-Engoren C, Patel A, Fang J, Armstrong D, Kline-Rogers E, Duvernoy CS, Eagle KA. Symptoms of men and women presenting with acute coronary syndromes. Am J Cardiol. 2006;98(9):1177–1181. doi: 10.1016/j.amjcard.2006.05.049. [DOI] [PubMed] [Google Scholar]
- 27.DeVon HA, Ryan CJ. Chest pain and associated symptoms of acute coronary syndromes. J Cardiovasc Nurs. 2005;20(4):232–238. doi: 10.1097/00005082-200507000-00006. [DOI] [PubMed] [Google Scholar]