Abstract
The use of cocaine and other drugs during pregnancy may have serious public health consequences. The objective of this study was to determine if the use of cocaine prenatally identifies women for ongoing risk of psychological symptoms. Four hundred and two women (207 cocaine using [C], 195 non-cocaine using [NC]) were assessed for rates of clinically elevated psychological symptoms shortly after childbirth, 6.5 months and 1, 2, 4 and 6 years after using the Brief Symptom Inventory (BSI). Generalized estimating equation modeling (GEE) was used to compare psychological symptom severity, controlling for confounding factors including early childhood trauma. Results indicated that women identified as having used cocaine during pregnancy had clinically elevated psychological distress (OR=1.76, 95%CI=1.15–2.71, p=0.01), psychoticism (OR=1.97, 95%CI=1.41–2.76, p=0.001), interpersonal sensitivity (OR=2.34; 95%CI=1.65–3.34; p<0.0001) and phobic anxiety (OR=1.86; 95%CI=1.24– 2.79) across all assessments compared to NC women. Childhood emotional abuse was also independently associated with psychological distress. Women who use cocaine during pregnancy should be recognized as at very high risk of ongoing clinically elevated psychological symptoms and should receive early and regular assessments and intervention for mental health and substance use problems.
Keywords: Psychological distress, Childhood trauma, Longitudinal, Prenatal cocaine use
Introduction
The use of cocaine and other drugs among pregnant women (Kuczkowski 2002) can have significant negative public health consequences for both mothers and children. Among the recognized consequences, maternal cocaine use has been related to increased rates of postpartum maternal psychological distress compared to similar, non-cocaine using women (Singer et al. 1995, 1997). A history of early childhood trauma, which is prevalent among women who abuse drugs, has also been linked to higher rates of psychological symptoms (Jantzen et al. 1998). Psychological distress and ongoing substance use among mothers can negatively affect the quality of care giving and child developmental outcomes (Eiden et al. 2006; Hans 2002; Light et al. 2004; Marques et al. 2007; Sheinkopf et al. 2006; Singer et al. 2002a, 2004). An understanding of the severity, characteristics and course of maternal psychological symptoms during the early child rearing years, and their association with prenatal cocaine use and early childhood trauma among women identified as using cocaine during pregnancy, is important for improving mental health interventions services for affected women and children.
The purpose of this study was to compare levels of psychological distress over 6 years in a cohort of women identified as having used cocaine prenatally to the symptoms reported by racially and economically similar women who did not use cocaine during pregnancy, controlling for confounding factors and history of early childhood trauma. It was hypothesized that women identified as cocaine using would be at increased risk for clinically elevated overall psychological distress symptoms, psychoticism, paranoid ideation, and depression, in the immediate post-partum period and over 6 years compared to non-cocaine, polydrug using women of similar socioeconomic status and race. It was also hypothesized that a history of childhood trauma would have an independent effect on the likelihood of increased rates of elevated psychological distress symptoms across the 6-year period.
Cocaine use has been linked to a wide range of symptoms including: irritability, impaired judgment, aggressive, sexual, or impulsive behavior, and manic excitement during acute intoxication and sadness, loss of appetite, insomnia, extreme fatigue, overeating and agitation during the withdrawal phase (APA 1994). Psychological symptoms that occur after chronic use include somatic problems (Johanson et al. 1999; Watson et al. 1992), eating disorders (Ross-Durow and Boyd 2000), anxiety and depression (Beckwith et al. 1999; Falck et al. 2002). Associations between chronic cocaine use and conditions such as obsessive–compulsive disorder (Crum and James 1993), paranoia (Espinosa et al. 2001; Lejoyeux et al. 2000), schizophrenia (Bowers et al. 2001), and antisocial personality disorder (Falck et al. 2004; Ladd and Nancy 2003) have also been identified.
Psychological distress is an important domain to assess in women who have used cocaine prenatally because it is associated with negative maternal behaviors, affect and adverse child rearing environments. Negative effects of psychological symptoms on parenting include less sensitive maternal care giving behavior, experience of parenting stress and poor infant attachment (Eiden et al. 2006; Espinosa et al. 2001; Howard et al. 1195; Minnes et al. 2005; Sheinkopf et al. 2006) and less optimal infant cognitive (Singer et al. 1997) and language outcomes (Marques et al. 2007). Despite the known negative effects of psychological distress on parenting among cocaine using women, very little is known about the natural history of mental health symptoms among cocaine using mothers (Jantzen et al. 1998; Minnes et al. 2000, 2008).
A small number of research studies have assessed psychological symptoms in cocaine using women during the immediate postpartum period but not over the early childhood years. Of those studies, several found elevated mental health symptoms including higher depression and sociopathy (Light et al. 2004; Strickland et al. 1993; Woods et al. 1993; Zuckerman et al. 1989) and clinically elevated interpersonal sensitivity, phobic anxiety and paranoid ideation in cocaine using women compared to non-cocaine using women (Singer et al. 1995, 2002b)
Women with lower levels of education and cognitive abilities, who live in stressed, socioeconomically depressed, urban areas also have a higher incidence of mental health disorders (Costello et al. 2003). Therefore, poor, urban women who are identified as having used cocaine during pregnancy may have additional risk of developing and maintaining high levels of psychological distress over longer periods of time due to multiple biologic and environmental stressors.
Early childhood abuse and neglect is also associated with higher rates and greater severity of cocaine and other substance use (Jantzen et al. 1998), highlighting the importance of understanding the independent, enduring effects of early trauma on psychological symptoms in cocaine using women. In addition, childhood trauma has been associated with changes in neurobiological responses to stress, increasing the risks of negative parenting through increased psychological reactivity (Nemeroff 2004).
Data on mental health symptoms and early childhood trauma of women who used cocaine during pregnancy can provide important information that can be used to develop targeted mental health and substance abuse treatment for women. It can also alert child welfare workers to the types of mental health symptoms experienced by cocaine using women so that adequate measure can be taken to protect children.
Materials and methods
Participants
Participants in the study were 402 high-risk status women who gave birth between September 1994 and June 1996 in a large urban teaching hospital in the Midwest. The participants were primarily African American of low socioeconomic status receiving public assistance. All participants and some infants were screened one time for substance use using urine toxicology due to their high risk status. High-risk status was defined by hospital delivery staff as women who did not receive prenatal care, had behaviors suggesting intoxication, previous involvement with Child Protective Services or who self-admitted drug use to hospital staff. All urine sampling was monitored by trained obstetric nurses. The urine was screened using the Syva Emit method of enzyme immunoassay (Syva Company, Palo Alto, CA), which detects the presence of benzoylecgonine (BZE), meta-hydroxybenzoylecgonine (m-OH-bze), and cocaethylene, the major metabolites for cocaine, as well as metabolites of other drugs of abuse. See Singer et al. (2002a, b) for additional details on urine screening. In addition to urine analysis, infant meconium, the first stool passed by a newborn, was collected shortly after birth by trained research staff to screen the infant for exposure cocaine and other drug metabolites over a 4.5 month period of gestation (Lewis et al. 1994; Ostrea et al. 1989).
Women were identified as cocaine using (C+) based on either self-reported drug use to hospital or research staff, or a positive result on urine or meconium screening. Women in the control group (C−) tested negative for cocaine on all measures including urine and meconium analyses and hospital and research study interviews. Women with confounding conditions such as schizophrenia, bipolar disorder or mental retardation documented in hospital records, age <19, positive HIV status, or who had a child with fetal alcohol syndrome or other serious birth defects, were excluded from the study.
The 402 women included in this study were assessed at least one time point, from post-partum (1 to 4 weeks after birth) through 6-year follow-up in the longitudinal study. The sample at each time point was 382 (95%) (198C+, 184C−) postpartum, 287 (71%) (143C+, 144C−) at 6.5 months, 334 (83%) (165C+, 1,169C−) at 12 months, 360 (90%) (186C+, 174C−) at 24 months, 349 (87%) (173C+, 176C−) at 48 months and 347 (86%) (182C+, 165C−) at 72 months.
Procedure
Women were recruited and screened by a nurse practitioner who obtained signed consent approved by the hospital's Institutional Review Board at the time of delivery. A writ of confidentiality preventing the release of any research data concerning substance abuse histories (Writ # DA-04-03) was obtained from the National Institute on Drug Abuse.
All subsequent assessments were performed at the child development laboratory located at a nearby university at <1 and 6.5 months and 1, 2, 4 and 6 years of age by a trained research assistant. All women, regardless of infant custody status, were contacted regularly for participation. They were paid a stipend of $35 for each visit through 2 years post-partum and $50 for the 4 and 6 years assessments.
Measures
Demographics
Maternal and infant demographic and medical characteristics were taken from hospital birth records and included race, age, parity, number of prenatal care visits, family composition, and school or work history. At each follow-up interview, dates of subsequent births and child placement status were recorded.
Maternal psychological symptoms
The Brief Symptom Inventory (BSI; Derogatis and Melisaratos 1983), a 53-item self-report questionnaire, was used to measure psychological distress at each time point. The BSI is comprised of nine subscales including somatization, obsessive–compulsive, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation, and psychoticism, and a summary measure, the Global Severity Index (GSI). Since the distribution of scores was skewed, all scores on the subscales were dichotomized to depict the borderline/clinical range (>90th percentile) and the normal range (≤90th percentile). Only the GSI, which was normally distributed, was reported using both the mean and dichotomized scores. Test–retest reliability ranged from 0.68 to 0.91, with Chronbach's alpha for this administration 0.96 for GSI and ranging from 0.76 to 0.88 for subscales.
Maternal cognitive ability
The Peabody Picture Vocabulary Test (PPVT-III; Dunn and Dunn 1997) was used to assess maternal verbal ability. The Block Design and Picture Completion subscales of the Wechsler Adult Intelligence test (WAIS-R; Wechsler 1989) were used to assess non-verbal, performance intelligence. Assessments were completed by a trained research assistant at the 1–4 week post-partum assessment.
Maternal substance use
Detailed substance use histories were obtained using an adaptation of the Maternal Post-Partum Interview (Singer et al. 2002b; Streissguth 1986) with the interview completed post-partum for assessment of substance use during pregnancy, and at each follow up assessment point to assess current use. Amount and frequency of use was quantified for cocaine, tobacco, alcohol and marijuana for the month prior to pregnancy and each trimester of pregnancy. At subsequent assessments, this information was collected for the prior 30 day period. For tobacco, the number of cigarettes smoked per day was collected. For marijuana, the number of marijuana joints smoked per day and for alcohol, the number of drinks of beer, wine, or hard liquor per day was acquired. Each drink was equivalent to 0.5 ml of absolute alcohol. Frequency of drug use was recorded on a Likert-type scale with a range of 0 (not at all) to 7 (daily usage). Frequency was converted to an average number of days of drug use each week and multiplied by amount of use per day to yield an average amount of use per week for each follow up period and during pregnancy.
Childhood trauma
The Childhood Trauma Questionnaire (CTQ; Bernstein and Fink 1998; Bernstein et al. 2003), is a 28-item self-report questionnaire used to assess maternal history of childhood emotional, physical and sexual abuse as well as emotional and physical neglect. This assessment requires an individual to recall abuse and neglect from their childhood and was administered to 300 (148C+; 152C−) study participants at one time point (48 month follow-up). The reduced sample size was a result of adding the CTQ after about 1/4 of the sample had been seen. Those not receiving the CTQ were more likely to smoke, use higher average amount of cocaine prenatally and have less prenatal care compared to those who did receive the CTQ. They were the same on all other variables. Cronbach's alpha levels were above 0.83 for emotional neglect, emotional abuse, physical abuse and sexual abuse. For the physical neglect scale, alpha was 0.61.
Statistical analyses
Positively skewed self-report drug data were transformed using loge (X+1) to reduce the influence of outlying values prior to analyses. For ease of interpretation, means and standard deviations are reported for the non-transformed variables. Cocaine effects were examined for demographic, prenatal substance use, and birth outcome measures. Comparisons were made using t tests and Wilcoxon rank sum tests for continuous data and Pearson χ2 tests for categorical variables. The Pearson χ2 test was also used to compare group differences on the percentage of borderline/clinical BSI subscales scores. To evaluate potential covariates, the relationships of dichotomized BSI subscale scores to maternal demographic, drug use, subsequent births, child placement status and early childhood trauma were assessed by t-tests or Wilcoxon rank sum tests for continuous data and Pearson χ2 tests for dichotomous data.
A Generalized Estimating Equation (GEE; Liang and Zeger 1986; Zeger and Liang 1986) for logistic regression was used to compare dichotomous BSI subscale scores by group over the six assessment points, controlling for covariates. Confounding variables were considered in the model stepwise if they were different between C+ and C− groups (p<0.25) and different based on outcome grouping (borderline/clinical vs. non-clinical (p<0.25). Demographic and prenatal factors were entered into the model first, followed by measures of maternal cognitive performance and prenatal/current drug use. If, upon entry, covariates reached p<0.10 significance level, they were retained in the model. Main effects of interest included cocaine status at time of study entry (C vs NC−) and time of assessment. In addition, the interaction between cocaine status and time was considered for all subscales to test for the homogeneity of the cocaine effect over time.
Due to the reduced sample of women with CTQ data, secondary analyses were conducted using this subsample. The final model identified above was extended to include measures from the CTQ to assess whether childhood trauma was also associated with psychological distress.
Results
Demographic characteristics
Tables 1 and 2 reveals that C+ women were older (p< 0.0001), had fewer prenatal care visits (p<0.0001), lower vocabulary (p<0.01) scores, less education (p<0.008) and were less likely to be married (p<0.003) or employed (<0.0001) than C− women. Cocaine-using women were also significantly more likely to have a greater number of children (p<0.0001), lost custody of their child at some time point (p<0.001) and had fewer subsequent births (p< 0.01) over the 6-year assessment period than C− women. Mean GSI scores at the post-partum assessment were higher for cocaine using women compared to non cocaine using women. Self report of childhood emotional, physical and sexual abuse did not differentiate the two groups, although on average, C+ women reported higher scores on emotional (p<0.04) and physical neglect (p<0.05) than women who did not use cocaine prenatally. Table 3 indicates that women who used cocaine during pregnancy also used more tobacco prenatally and during each of the 6-year follow-up assessments. Prenatal cocaine use women also used more alcohol prenatally and during all of the follow-up assessments except 6 years. Use of marijuana was greater prenatally and at the 1- and 6-year assessments. No women who were classified as non cocaine using during pregnancy reported cocaine use at follow-up assessment.
Table 1.
Demographic characteristics by cocaine status
| Cocaine(n=212) | Non-cocaine (n=196) | t-values | p-value | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Maternal demographics | ||||||
| Maternal age at birth | 29.63 | 5.06 | 25.68 | 4.83 | −8.03 | <0.0001 |
| Years of education | 11.56 | 1.66 | 11.96 | 1.43 | 2.67 | 0.008 |
| Parity | 3.54 | 1.91 | 2.71 | 1.84 | −4.46 | <0.0001 |
| Number of prenatal visits | 5.13 | 4.58 | 8.67 | 4.91 | 7.53 | <0.0001 |
| Number subsequent births since start of study | 1.34 | 0.60 | 1.51 | 0.70 | 2.58 | 0.01 |
| Peabody Picture Vocabulary Test-Revised | 73.85 | 15.32 | 77.77 | 14.89 | 2.57 | 0.01 |
| WAIS-R Design Scale | 6.84 | 2.16 | 7.19 | 2.11 | 1.63 | 0.10 |
| WAIS-R Picture Completion | 6.57 | 2.16 | 6.96 | 2.37 | 1.74 | 0.08 |
| Global Severity Index (postpartum assessment) | 0.80 | 0.74 | 0.48 | 0.52 | −4.96 | <0.0001 |
| Childhood trauma | ||||||
| Emotional abuse | 9.76 | 4.86 | 9.02 | 5.24 | −1.27 | 0.20 |
| Physical abuse | 9.02 | 4.78 | 8.39 | 4.63 | −1.15 | 0.25 |
| Sexual abuse | 8.91 | 6.13 | 8.53 | 6.08 | −0.54 | 0.59 |
| Emotional neglect | 12.36 | 5.51 | 11.03 | 5.39 | −2.12 | 0.04 |
| Physical neglect | 8.66 | 3.99 | 7.77 | 3.91 | −1.96 | 0.05 |
Table 2.
Demographic characteristics by cocaine status
| Maternal demographics | Cocaine(n=212) | Non-cocaine (n=196) | χ2 | p-value | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| African American | 171 | 80.66 | 155 | 79.08 | 0.16 | 0.69 |
| Currently employed | 11 | 5.21 | 41 | 21.03 | 22.69 | <0.0001 |
| Married | 16 | 7.55 | 34 | 17.35 | 9.10 | 0.003 |
| Low socioeconomic status | 207 | 98.10 | 191 | 97.45 | 0.20 | 0.65 |
| Lost custody at any time point | 134 | 63.21 | 14 | 7.14 | 138.48 | <0.001 |
Table 3.
Average maternal substance use follow-up assessment
| Maternal substance usea | CE | NCE | p-value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Tobacco (number per day) | |||||
| Prenatal | 11.75 | 10.88 | 4.21 | 7.83 | <0.0001 |
| 6.5 months | 9.79 | 7.97 | 4.86 | 8.54 | <0.0001 |
| 1 year | 10.04 | 9.93 | 4.82 | 8.65 | <0.0001 |
| 2 years | 10.57 | 10.92 | 4.51 | 7.91 | <0.0001 |
| 4 years | 9.46 | 9.33 | 4.32 | 7.00 | <0.0001 |
| 6 years | 9.85 | 10.80 | 4.26 | 7.37 | <0.0001 |
| Alcohol (dose per week) | |||||
| Prenatal | 9.99 | 18.66 | 1.31 | 4.48 | <0.0001 |
| 6.5 months | 5.51 | 11.31 | 1.50 | 2.91 | <0.0001 |
| 1 year | 5.90 | 12.58 | 1.67 | 4.24 | 0.0007 |
| 2 years | 7.98 | 20.44 | 1.81 | 5.01 | <0.0001 |
| 4 years | 4.14 | 9.16 | 2.10 | 7.39 | 0.009 |
| 6 years | 3.43 | 9.36 | 1.70 | 4.17 | 0.34 |
| Marijuana (dose per week) | |||||
| Prenatal | 1.34 | 3.59 | 0.59 | 3.42 | <0.0001 |
| 6.5 months | 1.81 | 9.92 | 2.25 | 16.86 | 0.29 |
| 1 year | 0.83 | 2.55 | 0.72 | 4.64 | 0.02 |
| 2 years | 0.77 | 3.42 | 0.65 | 4.03 | 0.16 |
| 4 years | 0.38 | 1.29 | 0.43 | 3.18 | 0.30 |
| 6 years | 0.53 | 3.02 | 0.13 | 0.83 | 0.03 |
| Cocaine (dose per week) | |||||
| Prenatal | 24.09 | 45.60 | 0.00 | 0.00 | N/A |
| 6.5 months | 10.33 | 51.46 | 0.00 | 0.00 | N/A |
| 1 year | 4.68 | 17.32 | 0.00 | 0.00 | N/A |
| 2 years | 8.43 | 21.97 | 0.00 | 0.00 | N/A |
| 4 years | 6.23 | 45.98 | 0.00 | 0.00 | N/A |
| 6 years | 1.89 | 9.93 | 0.00 | 0.00 | N/A |
Number of drinks, joints, units per day×number of days per week.
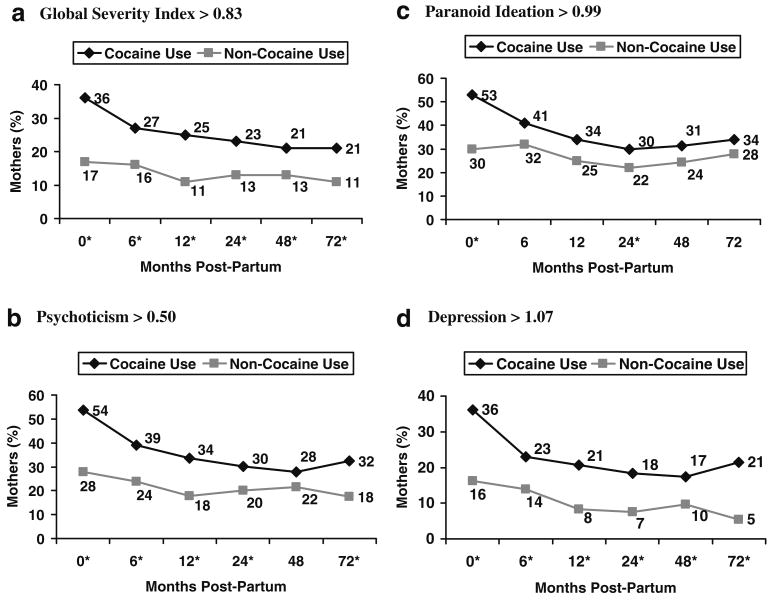
Global severity index
Figure 1a indicates that there were higher percentages of women with clinically elevated GSI scores (>90th percentile) among the C+ use group compared to the non-cocaine use group at each assessment point (ps<0.05). The GEE model presented in Table 4 shows that cocaine using women had significantly higher odds of scoring above the borderline/clinical cutoff than the control group (OR=1.76, 95%CI=1.15–2.71, p=0.01) and the cocaine effect did not significantly vary over the 6-year time period. Current marijuana use, alcohol consumption during pregnancy, and maternal performance IQ were also associated with clinically elevated GSI scores. Women who currently used marijuana at all time points had significantly higher odds of a GSI score above the borderline/clinical cutoff compared to mothers not currently using marijuana (OR=1.60, 95% CI=1.20–2.13, p=0.001). Higher average prenatal alcohol consumption, predicted higher odds of a GSI score above clinical cutoff of the 90th percentile. Prenatal alcohol use had a varied effect over time, with significant differences at birth, 6 months, and at 1 and 6 year follow-up (ps<0.05), but not 24 and 48 months. Lower performance IQ was associated with higher odds of GSI score above the 90th percentile. The relationship between performance IQ and psychological distress varied over time as well, with significant effects at 6, 12, 24 and 48 months follow-up (ps>002).
Fig. 1.
Unadjusted percent above borderline/clinical cut-off scores. *p<0.05; different by cocaine group. a Global Severity Index>0.83. b Psychoticism>0.50. c Paranoid ideation>0.99. d Depression>1.07
Table 4.
Adjusted* association of cocaine use with BSI outcomes above borderline/clinical cut-off
| BSI outcome above borderline/clinical cut-off | Non-time varying cocaine effects [OR (95% CI)] |
Time varying cocaine effects by months post-partum [OR (95% CI)] | |||||
|---|---|---|---|---|---|---|---|
| 0 | 6 | 12 | 24 | 48 | 72 | ||
| Hypothesized associations | |||||||
| GSI>0.83 | 1.76** (1.15–2.71) |
||||||
| Psychoticism>0.50 | 1.97*** (1.41–2.76) |
||||||
| Paranoid ideation>0.99 | 2.03*** (1.43–2.87) |
1.95*** (1.40–2.71) |
1.87*** (1.35–2.57) |
1.72*** (1.26–2.35) |
1.46* (1.03–2.07) |
1.24 (0.80–1.93) |
|
| Depression>1.07 | 1.83* (1.10–3.05) |
2.36*** (1.52–3.65) |
2.64*** (1.60–4.34) |
2.46** (1.40–4.32) |
1.69 (0.89–3.20) |
4.99*** (2.22–11.22) |
|
| Additional BSI subscales | |||||||
| Hostility>0.87 | 1.48 (0.97–2.24) |
1.56* (1.06–2.32) |
1.66** (1.14–2.42) |
1.87*** (1.29–2.71) |
2.36*** (1.48–3.76) |
2.99*** (1.58–5.66) |
|
| Anxiety>1.07 | 1.82 (0.93–3.53) | 2.06* (1.17–3.64) |
2.16** (1.16–4.02) |
1.99 (0.99–4.02) |
1.35 (0.60–3.03) |
1.60 (0.78–3.28) |
|
| Somatization>0.95 | 0.75 (0.52–1.07) |
||||||
| Obsessive compulsive>1.15 | 1.58 (0.96–2.62) |
1.99** (1.30–3.05) |
2.12** (1.32–3.38) |
1.66* (1.00–2.74) |
0.68 (0.37–1.26) |
1.22 (0.66–2.25) |
|
| Interpersonal sensitivity>1.03 | 2.34*** (1.65–3.34) |
||||||
| Phobic anxiety>0.62 | 1.86** (1.24–2.79) |
||||||
Adjustments included the following for BSI models: (1) GSI—WAIS-R Picture Completion scale, log of average prenatal alcohol dose per week, and current marijuana use; (2) psychoticism—log of average prenatal alcohol dose per week; (3) paranoid ideation—WAIS-R Picture Completion scale and log of average current marijuana use; (4) depression—PPVT Standard Score and log of average current alcohol dose per week; (5) hostility—log of average prenatal marijuana dose per week; (6) anxiety—PPVT Standard Score and log of average prenatal alcohol dose per week; (7) somatization— parity, maternal education, WAIS-R Picture Completion scale, log of average prenatal cigarettes per day, log of current caregiver average alcohol dose per week, current marijuana use and custody loss at any time point; (8) obsessive-compulsive—custody loss at any time point; (9) interpersonal sensitivity—no further adjustments; (10) phobic anxiety—WAIS-R Picture Completion scale and maternal prenatal alcohol use.
Cocaine did not vary by time
p<0.05;
p<0.01;
p<0.001
Psychoticism
Figure 1b indicates that a higher percentage of C+ women scored above the 90th percentile on psychoticism at birth, 6, 12, 24 and 72 months than C− women (ps<0.05). Table 4 shows that after adjusting for covariates, the C+ group was more likely to score above the 90th percentile than the C− group (OR=1.97, 95%CI=1.41–2.76, p=0.05) with this effect being elevated over the 6-year period. Higher average prenatal alcohol consumption was also positively associated with borderline/clinical psychoticism scores at birth, 6 months and 6 years (ps<0.05).
Paranoid ideation
Figure 1c indicates that C+ women were more apt to score above the 90th percentile on the paranoid ideation subscale at birth and at 24 month follow-up than C− women. Table 4 indicates that after adjusting for covariates, maternal cocaine use was associated with a higher percentage of borderline/clinical paranoid ideation scores at birth, 6, 12, 24, and 48 months (ps<0.05), but not 72 months. Lower maternal performance IQ scores and higher current marijuana use were also associated with a higher likelihood of paranoid ideation scores above the 90th percentile. These effects were consistent across all time points except birth for performance IQ (ps<0.03), with marijuana effects only emerging at 12, 24, and 48 months (ps<0.03).
Depression
Figure 1d shows that C+ women were more apt to score above the 90th percentile on depression scores at all time points (ps<0.05) as compared to C− women (ps<0.05). This effect remained present even after adjusting for covariates (see Table 4). The association varied over time with significant associations obtained only during the 2 years after infant birth (birth, 6, 12, and 24 months) and at 6 years. Lower verbal IQ scores were associated with higher odds of depression scores exceeding the 90th percentile, but only during the first year of life (6.5, 12, (ps<0.05) and at 24 months (p<0.09). Higher current alcohol consumption increased the odds of depression scores exceeding the 90th percentile with this effect significant at birth, 6.5, 12, 24, and 48 months (ps<0.05).
Summary of other BSI subscales
With the exception of somatization, all remaining BSI subscales (hostility, anxiety, phobic anxiety, interpersonal sensitivity, and obsessive compulsive) revealed a higher percentage of C+ women exceeding the 90th percentile than C− women (ps<0.05). See Table 4 for a summary of these results. The cocaine effects varied over time beginning at 6.5 months (ps<0.05), with the exception of interpersonal sensitivity (OR=2.34; 95%CI=1.65–3.34; p<0.0001) and phobic anxiety ((OR=1.86; 95%CI=1.24–2.79; p<0.003) in which prenatal cocaine use was a significant predictor of symptoms at all time points. The use of marijuana increased the likelihood that hostility scores would exceed the 90th percentile during the first year of life only (ps<0.05). Significant effects of alcohol on rates of anxiety scores >90th percentile were found at birth, 6.5 and 12 months (ps<0.002) and phobic anxiety at 6 years (p<0.03). Effects of lower vocabulary on clinically elevated anxiety were found at 12 and 24 months (ps<0.05). Finally, effects of lower performance IQ on clinically elevated phobic anxiety were found at 6.5–24 months (p<0.002).
Loss of infant custody predicted higher rates of clinically elevated obsessive compulsive symptoms at 48 and 72 months (ps<0.02) and somatization (p<0.0005) across all time points. In addition, elevated somatic symptoms, while not predicted by cocaine use during pregnancy, were predicted by a number of demographic and drug use variables. Having a greater number of children (p<0.01), lower education (p<0.001), lower performance IQ (p< 0.003), current alcohol use (p<0.0008), and current marijuana use (p<0.03) were related to elevated somatic symptoms across all time points.
Effects of early childhood trauma
In a sub-analysis of women who were assessed for early childhood trauma presented in Table 5, emotional abuse was independently related to a higher incidence of overall psychological distress above the 90th percentile at all time points, even controlling for other demographics and substance use variables. The effect of cocaine remained a significant predictor of overall psychological distress. Physical abuse and neglect, emotional neglect, and sexual abuse were not significantly associated with overall psychological distress. Physical neglect was associated with a greater likelihood of paranoid ideation at birth only. When the effects of early childhood trauma on depression were considered, only physical neglect was associated with depression scores above the 90th percentile at 6.5, 12, 24 and 72 months (ps<0.05) (see Table 5).
Table 5.
Adjusted association of Childhood Trauma Questionnaire with BSI outcomes above borderline/clinical cut-off
| BSI outcome above borderline/clinical cut-off | Months post-partum, OR (95%CI) | |||||
|---|---|---|---|---|---|---|
| 0 | 6 | 12 | 24 | 48 | 72 | |
| GSI>0.83 | ||||||
| Emotional abuse | 2.13** (1.17–3.86) | 2.94**** (1.77–4.88) | 3.88**** (2.39–6.31) | 5.91**** (3.41–10.25) | 7.94**** (4.19–15.03) | 5.14**** (2.46–10.71) |
| Paranoid ideation>0.99 | ||||||
| Physical neglect | 1.79** (1.00–3.19) | 1.42 (0.84–2.39) | 1.17 (0.70–1.97) | 0.90 (0.50–1.62) | 0.85 (0.46–1.56) | 1.49 (0.78–2.85) |
| Depression>1.07 | ||||||
| Physical neglect | 1.19 (0.57–2.52) | 2.06** (1.08–3.92) | 2.90*** (1.39–6.05) | 3.61*** (1.62–8.04) | 2.33* (0.90–6.06) | 3.01** (1.06–8.55) |
Adjustments included the following for BSI models: (1) GSI—prenatal cocaine use, WAIS-R Picture Completion scale, log of average prenatal alcohol dose per week, and current marijuana use; (2) psychoticism—prenatal cocaine use and log of average prenatal alcohol dose per week; (3) depression—prenatal cocaine use, PPVT Standard Score, and log of average current alcohol dose per week.
p<0.1;
p<0.05;
p<0.01;
p<0.001
Childhood trauma predicted increased rates of elevated symptoms for all other subscales of the BSI except psychoticism and obsessive compulsive. Physical abuse and/or neglect were the most common predictors of elevated symptoms of anxiety, physical anxiety, interpersonal sensitivity, hostility and somatization. Clinically relevant hostility, while not predicted by emotional neglect, was associated with early emotional abuse at all time points (ps<0.03) as well as sexual abuse at 12 through 72 months (ps<0.03).
Discussion
Findings from this study indicate that women identified as having used cocaine during pregnancy have higher odds of clinically elevated overall psychological distress, as well as specific psychological symptoms including paranoid ideation, psychoticism, depression, hostility, anxiety and interpersonal sensitivity immediately postpartum. The increased risk for psychological symptoms persisted over a 6-year time period, after controlling for confounding demographic, cognitive and drug use factors. Maternal childhood trauma, specifically childhood emotional abuse, was independently associated with higher rates of severe psychological distress. Several specific symptom domains including paranoid ideation, depression, hostility and anxiety, also were associated with a reported history of childhood neglect and abuse. Receptive vocabulary, performance IQ, prenatal alcohol use and current marijuana use were found to be independently associated with clinically elevated psychological distress as well as paranoid ideation.
These data corroborate and extend the association previously found between maternal cocaine use during pregnancy and increased psychological distress immediately postpartum (Singer et al. 1995) in cocaine using compared to non-cocaine using women. Furthermore, these findings document the ongoing risk of continued alcohol and marijuana use and serious mental health symptoms over a 6-year period among mothers identified as having used cocaine prenatally. Given the detrimental effects of psychological symptoms for mothers and their children, particular care by mental health professionals should be paid to the accurate, systematic assessment of mental health symptoms and extremely elevated level of psychological distress among women who use cocaine during pregnancy. Hospital staff, including emergency room physicians, delivering obstetricians, social workers and pediatricians, who may see the mother for obstetric care and the child for well care, should use this unique, limited opportunity to complete symptom assessment and make referrals for mental health interventions.
Significant evidence for prompt assessment and intervention is apparent from the alarmingly high rates of mental health symptoms exceeding the 90th percentile among this prenatal cocaine use group. For example, rates of clinically elevated psychoticism in the first 2 years post partum were (30–54%), paranoid ideation (30–53%), depression (18– 36%), hostility (24–31%) and anxiety (15–27%). Elevation of these symptom domains have the potential for serious consequences for mothers including suicide (Holmstrand et al. 2006), loss of infant custody (Minnes et al. 2008) and increased rates of domestic violence (Nixon et al. 2004; Stuart et al. 2006). High rates of maternal psychopathology pose threats to infant well-being as well. Maternal psychological distress is associated with higher rates of child abuse and neglect (Berger 2005; Burke 2003), lower quality mother infant interaction (Minnes et al. 2005; Singer et al. 1996), lower cognitive and language outcomes (Singer et al. 1997, 1999) and poor attachment and social behavior among infants (Hipwell et al. 2000). Given the nature and severity of these symptoms, and the potential harm to mother and children, targeted interventions for mothers and infants should be started as soon as possible during the post-partum period. The independent effect of early trauma on psychological distress indicates that special attention should be paid to the mental health needs of women who experienced early childhood trauma and use cocaine during pregnancy.
Higher than expected rates of depression (16% and 14% in the first 6 months post-partum) and psychoticism (24–28% in the first 6 months post-partum) were also found for non-cocaine use women. While these symptoms are among the more common postpartum symptoms, they are elevated in this high-risk sample compared to national average rates of 10–12% for depression and 5.5–17% for psychotic symptoms. In addition the findings are also consistent with other studies that have found an association of depression and anxiety with alcohol use among lower risk obstetric samples (Baigent 2005). There is also considerable research which shows an association of lower cognitive abilities with higher rates of depression, anxiety and overall psychological distress (Zammit et al. 2004), similar to the findings of this study.
Current marijuana use was found to be associated with a higher rate of elevated paranoid ideation scores at 24 and 48 months as well as overall psychological distress scores over the entire assessment period. These findings are consistent with studies that report increased psychological symptoms in chronic marijuana users (Laqueille 2005; Raphael et al. 2005) and indicate an independent risk factor for marijuana use on psychological distress symptoms independent of prenatal cocaine use.
Early-life trauma/stress has been found to lead to neurobiological changes that increase the risk of psychopathology in adulthood (Jantzen et al. 1998; Nemeroff 2004). The effects of childhood trauma on psychological symptoms were associated at select time points over the 6-year assessment period but not others and on some symptom domains but not others. This pattern of findings indicates that the associations of early childhood trauma with psychological symptoms may have varying degrees of relevance during different biologic and care giving stress states such as caring for an infant or toddler. Another study of this sample found greater psychological distress and early emotional neglect to be associated with increased likelihood of loss of infant custody among cocaine using women (Minnes et al. 2008). In contrast, this study did not reveal an association of loss of infant custody with increased psychological distress at any time point. This difference may be related to study design. In this study, the whole sample (cocaine using and non cocaine using) was examined over multiple time points whereas the other study (Minnes et al. 2008) was cross sectional (post-partum only) and the sample consisted of only cocaine using women.
Strengths and limitations of the study
One methodological weakness of the study is that the data is based solely on self-report of psychological symptoms and continued drug use. Self-report data were not corroborated with DSM-IV based diagnostic interviews, direct observations of symptoms, family input or biologic drug screening. Despite these limitations, the BSI has been shown to be a reliable, standardized assessment of mental health symptoms. In addition, the BSI data and self reported drug use revealed significant group differences in this racially and economically similar population. Results indicating that prenatal and current use of marijuana is also associated with increased likelihood of psychological distress symptoms should be interpreted cautiously because the cocaine use group used significantly more marijuana prenatally and the results could be confounded with the group cocaine effect.
A second methodological concern is that childhood trauma data were collected at one time point (48 months post partum), on 75% of the sample, and relied on maternal memory of childhood events. Because memory can be influenced by current psychological symptoms including depression or paranoid ideation, the strong associations with current psychological symptoms should also be interpreted carefully. However, the association of specific psychological symptom domains with specific childhood trauma indicates that psychological symptoms may not have influenced responses on the CTQ in a global way. For example clinically elevated depression scores were associated with more physical neglect but not abuse of any type or emotional neglect. In contrast, elevated psychoticism scores were not associated with any type of early trauma and may be regulated to a greater extent by current biological conditions such as acute effects of cocaine. Despite the noted weakness involved in recalling early trauma, and the influence of current symptomatology or events, such as removal of infant custody on accuracy of recall, these data highlight the need for clinicians involved in substance abuse treatment with women of child bearing years to attend to the possible long term affects of early trauma in drug treatment planning.
Third, the present findings must be interpreted cautiously as the sample does not have premorbid data on maternal psychological symptoms and drug use, limiting the interpretation of the results. Finally, sample composition limits the generalizability of our findings to African-American, poly-substance using women of low socioeconomic status.
Despite the noted limitation the present study has significant advantages over previous research. A large sample size, combined with the low attrition rate of subjects, allowed for long-term follow up of psychological symptoms in cocaine/polydrug using women over a 6-year period with adequate statistical power, increasing confidence in the results. A large number of covariates (>30) were evaluated as confounders and controlled for in the longitudinal analyses when criteria were met and include self reported continued use of tobacco, marijuana and alcohol. Control for a large number of unique covariates increased the likelihood that the associations of prenatal cocaine use with higher rates of mental health symptoms were not spurious. Among the covariates two are unique to this study. Removal of infant custody and the birth of additional children, have not been controlled for in previous studies. To our knowledge, no study has described psychological symptoms of a large number of cocaine using women and a control group matched for race and socioeconomic status over a period of 6 years. Multi-determined methods, including biologic and self-report measures, for the assignment of mothers into cocaine/non-cocaine groups assured that group status was accurate, increasing the validity of the results.
Overall, findings from the present study provide strong evidence for the presence of higher rates of psychological distress among women identified as cocaine using during pregnancy compared to women who did not use cocaine during pregnancy, with increased symptoms persisting well after the immediate postpartum period. While the association of cocaine use with psychopathology did not vary over time for most domains, cocaine's effects were most prominent in the first 2 years after initial assessment for several symptom domains including depression, psychoticism and paranoid ideation indicating a time of highest need for targeted intervention. In addition, women who experienced early childhood trauma and use other substances including alcohol and marijuana are also at significant risk for the development of serious psychological symptoms. Clinicians who have regular appointments with infants and new mothers (e.g. obstetricians and pediatricians) should be particularly attentive to the mental health symptoms experienced by cocaine using women post-partum and during the early childhood year in an effort to reduce maternal suffering and protect infants and children from the negative consequences of maternal psychological symptoms. The implementation of standardized assessments of psychological symptom severity including depression, paranoid ideation and psychoticism should become a routine part of obstetric and general medical care for high-risk cocaine using women.
Acknowledgments
The authors would like to acknowledge the efforts of Paul Weishampel, Addie Lang, Nicole Nall and Selena Cook who have interacted with subjects on a daily basis and carefully collected and processed data, our social worker Laurie Ellison who has maintained a high rate of subject retention and our families who continue to be active participants in this study. This study was supported through grant R01 07957 from the National Institute on Drug Abuse.
Contributor Information
Sonia Minnes, Email: sonia.minnes@case.edu, Department of General Medical Sciences, School of Medicine, Case Western Reserve University, The Triangle Building, 11400 Euclid Avenue, Suite 250-A, Cleveland, OH 44106, USA.
Lynn T. Singer, Department of General Medical Sciences, School of Medicine, Case Western Reserve University, The Triangle Building, 11400 Euclid Avenue, Suite 250-A, Cleveland, OH 44106, USA, Department of Pediatrics, School of Medicine, Case Western Reserve University, Cleveland, OH 44106, USA
H. Lester Kirchner, Geisinger Center for Health Research, Geisinger Health System, Danville, PA 17822, USA.
Sudtida Satayathum, Department of Pediatrics, School of Medicine, Case Western Reserve University, Cleveland, OH 44106, USA.
Elizabeth J. Short, Department of Psychology, Case Western Reserve University, Cleveland, OH 44106, USA
Meeyoung Min, Department of Pediatrics, School of Medicine, Case Western Reserve University, Cleveland, OH 44106, USA.
Sheri Eisengart, Department of Pediatrics, School of Medicine, Case Western Reserve University, Cleveland, OH 44106, USA.
John P. Mack, Department of Psychology, Case Western Reserve University, Cleveland, OH 44106, USA
References
- APA. Diagnostic and statistical manual of mental disorders. 4th. American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Baigent MF. Understanding alcohol misuse and comorbid psychiatric disorders. Curr Opin Psychiatry. 2005;18(3):223–228. doi: 10.1097/01.yco.0000165590.68058.b0. [DOI] [PubMed] [Google Scholar]
- Beckwith L, Howard J, Espinosa M, Tyler R. Psychopathology, mother–child interaction, and infant development: substance-abusing mothers and their offspring. Dev Psychopathol. 1999;11(4):715–725. doi: 10.1017/s095457949900228x. [DOI] [PubMed] [Google Scholar]
- Berger LM. Income, family characteristics, and physical violence toward children. Child Abuse Neglect. 2005;29(2):107–133. doi: 10.1016/j.chiabu.2004.02.006. [DOI] [PubMed] [Google Scholar]
- Bernstein DP, Fink L. Psychological. San Antonio, TX: 1998. Childhood trauma questionnaire: a retrospective self-report. [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, et al. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Neglect. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Bowers MB, D'Souza N, Deepak C, Madonick S. Substance abuse as a risk factor for schizophrenia and related disorders. Int J Ment Health. 2001;30(1):33–57. [Google Scholar]
- Burke L. The impact of maternal depression on familial relationships. Int Rev Psychiatry. 2003;15(3):243–255. doi: 10.1080/0954026031000136866. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Compton SN, Keeler G, Angold A. Relationships between poverty and psychopathology: a natural experiment. JAMA. 2003;290(15):2023–2029. doi: 10.1001/jama.290.15.2023. [DOI] [PubMed] [Google Scholar]
- Crum RMA, James C. Cocaine use and other suspected risk factors for obsessive–compulsive disorder: a prospective study with data from the Epidemiologic Catchment Area surveys. Drug Alcohol Depend. 1993;31(3):281–295. doi: 10.1016/0376-8716(93)90010-n. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychol Med. 1983;13(3):595–605. [PubMed] [Google Scholar]
- Dunn LM, Dunn LM. Peabody picture vocabulary test. third. AGS; Circle Pines, MN: 1997. PPVT-III. [Google Scholar]
- Eiden RD, Stevens A, Schuetze P, Dombkowski LE. Conceptual model for maternal behavior among polydrug cocaine-using mothers: the role of postnatal cocaine use and maternal depression. Psychol Addict Behav. 2006;20(1):1–10. doi: 10.1037/0893-164X.20.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Espinosa M, Beckwith L, Howard J, Tyler R, Swanson K. Maternal psychopathology and attachment in toddlers of heavy cocaine-using mothers. Infant Ment Health J. 2001;22(3):316–333. [Google Scholar]
- Falck RS, Wang J, Carlson RG, Eddy M, Siegal HA. The prevalence and correlates of depressive symptomatology among a community sample of crack-cocaine smokers. J Psychoact Drugs. 2002;34(3):281–288. doi: 10.1080/02791072.2002.10399964. [DOI] [PubMed] [Google Scholar]
- Falck RS, Wang J, Siegal HA, Carlson RG. The prevalence of psychiatric disorder among a community sample of crack cocaine users: an exploratory study with practical implications. J Nerv Ment Dis. 2004;192:503–507. doi: 10.1097/01.nmd.0000131913.94916.d5. [DOI] [PubMed] [Google Scholar]
- Hans SL. Studies of prenatal exposure to drugs: focusing on parental care of children. Neurotoxicol Teratol. 2002;24:329–337. doi: 10.1016/s0892-0362(02)00195-2. [DOI] [PubMed] [Google Scholar]
- Hipwell AE, Goossens FA, Melhuish EC, Kumar R. Severe maternal psychopathology and infant–mother attachment. Dev Psychopathol. 2000;12(2):157–175. doi: 10.1017/s0954579400002030. [DOI] [PubMed] [Google Scholar]
- Holmstrand C, Nimeus A, Traskman-Bendz L. Risk factors of future suicide in suicide attempters—a comparison between suicides and matched survivors. Nord J Psychiatry. 2006;60(2):162–167. doi: 10.1080/08039480600583597. [DOI] [PubMed] [Google Scholar]
- Howard J, Beckwith L, Espinosa M, Tyler R. Development of Infants born to cocaine abusing women: biologic/maternal influences. Neurotoxicol Teratol. 1195;17(4):403–411. doi: 10.1016/0892-0362(94)00077-q. [DOI] [PubMed] [Google Scholar]
- Jantzen K, Ball SA, Leventhal JM, Schottenfeld RS. Type of abuse and cocaine use in pregnant women. J Subst Abuse Treat. 1998;15(4):319–323. doi: 10.1016/s0740-5472(97)00198-0. [DOI] [PubMed] [Google Scholar]
- Johanson CE, Timothy R, Schuh K, Warbasse L. The effects of cocaine on mood and sleep in cocaine-dependent males. Exp Clin Psychopharmacol. 1999;7(4):338–346. doi: 10.1037//1064-1297.7.4.338. [DOI] [PubMed] [Google Scholar]
- Kuczkowski K. Cocaine abuse in pregnancy—anesthetic implications. Int J Obstet Anesth. 2002;11(3):204–210. doi: 10.1054/ijoa.2002.0960. [DOI] [PubMed] [Google Scholar]
- Ladd GTP, Nancy M. Antisocial personality in treatment-seeking cocaine abusers: psychosocial functioning and HIV risk. J Subst Abuse Treat. 2003;24(4):323–330. doi: 10.1016/s0740-5472(03)00042-4. [DOI] [PubMed] [Google Scholar]
- Laqueille X. Related, induced and associated psychiatric disorders to cannabis. Rev Prat. 2005;55(1):30–34. [PubMed] [Google Scholar]
- Lejoyeux M, Mourad I, Ades J. Psychiatric disorders induced by drug dependence other than alcohol. Encephale. 2000;26(2):21–27. [PubMed] [Google Scholar]
- Lewis D, Moore C, Leikin J. Cocaethylene in meconium specimens. J Toxicol Clin Toxicol. 1994;32(6):697–703. doi: 10.3109/15563659409017976. [DOI] [PubMed] [Google Scholar]
- Liang K, Zeger S. Longitudinal data analysis using general linear models. Biometrika. 1986;73(1):13–22. [Google Scholar]
- Light KC, Grewen KM, Amico JA, Boccia M, Brownley KA, Johns JM. Deficits in plasma oxytocin responses and increased negative affect, stress, and blood pressure in mothers with cocaine exposure during pregnancy. Addict Behav. 2004;29(8):1541–1564. doi: 10.1016/j.addbeh.2004.02.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marques PR, Pokorni JL, Long T, Teti LO. Maternal depression and cognitive features of 9-year-old children prenatally-exposed to cocaine. Am J Drug Alcohol Abuse. 2007;33(1):45–61. doi: 10.1080/00952990601082647. [DOI] [PubMed] [Google Scholar]
- Minnes S, Singer LT, Farkas K. Psychological distress, violence and infant placement in cocaine using postpartum women. Paper presented at the College for Problems on Drug Dependence; San Juan, Puerto Rico. 2000. [Google Scholar]
- Minnes S, Singer LT, Arendt R, Satayathum S. Effects of prenatal cocaine/polydrug use on maternal–infant feeding interactions during the first year of life. J Dev Behav Pediatr. 2005;26(3):194–200. doi: 10.1097/00004703-200506000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minnes S, Singer LT, Humphrey-Wall R, Satayathum MS. Psychosocial and behavioral factors related to infant placement of post-partum cocaine-using women. Child Abuse Neglect. 2008 doi: 10.1016/j.chiabu.2007.12.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nemeroff CB. Neurobiological consequences of childhood trauma. J Clin Psychiatry. 2004;65(Suppl 1):18–28. [PubMed] [Google Scholar]
- Nixon RD, Resick PA, Nishith P. An exploration of comorbid depression among female victims of intimate partner violence with posttraumatic stress disorder. J Affect Disord. 2004;82(2):315–320. doi: 10.1016/j.jad.2004.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostrea EJ, Brady M, Parks P, Asensio D, Naluz A. Drug screening of meconium in infants of drug-dependent mothers: an alternative to urine testing. J Pediatr. 1989;115(3):474–477. doi: 10.1016/s0022-3476(89)80860-1. [DOI] [PubMed] [Google Scholar]
- Raphael B, Wooding S, Stevens G, Connor J. Comorbidity: cannabis and complexity. J Psychiatr Pract. 2005;11(3):161–176. doi: 10.1097/00131746-200505000-00004. [DOI] [PubMed] [Google Scholar]
- Ross-Durow PL, Boyd CJ. Sexual abuse, depression, and eating disorders in African American women who smoke cocaine. J Subst Abuse Treat. 2000;81(1):79–81. doi: 10.1016/s0740-5472(99)00057-4. [DOI] [PubMed] [Google Scholar]
- Sheinkopf SJ, Lester BM, LaGasse LL, Seifer R, Bauer CR, Shankaran S, et al. Interactions between maternal characteristics and neonatal behavior in the prediction of parenting stress and perception of infant temperament. J Pediatr Psychol. 2006;31(1):27–40. doi: 10.1093/jpepsy/jsj026. [DOI] [PubMed] [Google Scholar]
- Singer LT, Arendt RE, Minnes S, Farkas K, Yamashita T, Kliegman R. Increased psychological distress in post-partum, cocaine-using mothers. J Subst Abuse. 1995;7(2):165–174. doi: 10.1016/0899-3289(95)90002-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Davillier M, Preuss L, Szekely L, Hawkins S, Yamashita T, et al. Feeding interations in infants with very low birth weight and bronchopulmonary dysplasia. J Dev Behav Pediatr. 1996;17(2):69–76. [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Arendt R, Farkas K, Minnes S, Huang J, Yamashita T. The relationship of prenatal cocaine exposure and maternal postpartum psychological distress to child developmental outcome. Dev Psychopathol. 1997;9(3):473–489. doi: 10.1017/s0954579497001259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Salvator A, Guo S, Collin M, Lilien L, Baley J. Maternal psychological distress and parenting stress after the birth of a very low-birth-weight infant. JAMA. 1999;281(9):799–805. doi: 10.1001/jama.281.9.799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Arendt R, Minnes S, Farkas K, Salvator A, Kirchner HL, et al. Cognitive and motor outcomes of cocaine-exposed infants. JAMA. 2002a;287(15):1952–1960. doi: 10.1001/jama.287.15.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singer LT, Salvator A, Arendt R, Minnes S, Farkas K, Kliegman R. Effects of cocaine/polydrug exposure and maternal psychological distress on infant birth outcomes. Neurotoxicol Teratol. 2002b;24(2):127–135. doi: 10.1016/s0892-0362(01)00208-2. [DOI] [PubMed] [Google Scholar]
- Singer LT, Minnes S, Arendt R, Farkas K, Short E, Lewis B, et al. The home environment and cognitive outcomes of cocaine exposed, preschool children. JAMA. 2004;291:2448–2456. doi: 10.1001/jama.291.20.2448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Streissguth AP. The behavioral teratology of alcohol: performance, behavioral, and intellectual deficits in prenatally exposed children. In: West JR, editor. Alcohol and brain development. Oxford University Press; New York: 1986. pp. 3–44. [Google Scholar]
- Strickland TL, James R, Myers H, Lawson W, Bean X, Mapps J. Psychological characteristics related to cocaine use during pregnancy: a postpartum assessment. J Natl Med Assoc. 1993;85(10):755–760. [PMC free article] [PubMed] [Google Scholar]
- Stuart GL, Moore TM, Gordon KC, Ramsey SE, Kahler CW. Psychopathology in women arrested for domestic violence. J Interpers Violence. 2006;21(3):376–389. doi: 10.1177/0886260505282888. [DOI] [PubMed] [Google Scholar]
- Watson R, Bakos L, Compton P, Gawin F. Cocaine use and withdrawal: the effect on sleep and mood. Am J Drug Alcohol Abuse. 1992;8(1):21–28. doi: 10.3109/00952999209001608. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Psychological. San Antonio, TX: 1989. Wechsler adult intelligence scale—revised. [Google Scholar]
- Woods NS, Eyler FD, Behnke M, Conlon M. Cocaine use during pregnancy: maternal depressive symptoms and infant neurobehavior over the first month. Infant Behav Dev. 1993;16:83–98. [Google Scholar]
- Zammit S, Allebeck P, David AS, Dalman C, Hemmingsson T, Lundberg I, et al. A longitudinal study of premorbid IQ score and risk of developing schizophrenia, bipolar disorder, severe depression, and other nonaffective psychoses. Arch Gen Psychiatry. 2004;61(4):354–360. doi: 10.1001/archpsyc.61.4.354. [DOI] [PubMed] [Google Scholar]
- Zeger S, Liang K. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–130. [PubMed] [Google Scholar]
- Zuckerman B, Amaro H, Bauchner H, Cabral H. Depressive symptoms during pregnancy: relationship to poor health behaviors. Am J Obstet Gynecol. 1989;160:1107–1111. doi: 10.1016/0002-9378(89)90170-1. [DOI] [PubMed] [Google Scholar]