Abstract
Background: Dietary calcium and vitamin D intakes may be inversely associated with cardiovascular disease (CVD) risk, possibly because of their potential beneficial effects on circulating lipids. Clinical trials that have evaluated the effect of calcium supplementation on lipids are limited by a short follow-up, and data on vitamin D are scarce.
Objective: The objective was to evaluate the effect of a longer-term effect (over 5 y) of calcium and vitamin D (CaD) supplementation on changes in the concentrations of several lipids: LDL, HDL, non-HDL, total cholesterol, triglycerides, and lipoprotein(a) [Lp(a)].
Design: The study was conducted in 1259 postmenopausal women in the Calcium plus Vitamin D Trial (1 g elemental Ca as carbonate plus 400 IU vitamin D3/d compared with placebo) of the Women's Health Initiative. Analyses were conducted by intention-to-treat. Repeated measurements on lipids during follow-up were analyzed by linear mixed-effects models.
Results: Overall, the change in lipids was relatively small [≤5% except for Lp(a), which was 20–25%], and there was no significant difference in the mean change of any lipid variable between the active and placebo groups.
Conclusions: Our results indicate that CaD supplementation is not associated with lipid changes over 5 y. Existing and future CaD trials should consider evaluating this association for different doses of supplements. This study was registered at clinicaltrials.gov as NCT00000611.
INTRODUCTION
The role of diet in the prevention of cardiovascular disease (CVD) is well known (1). In this regard, existing research has focused mainly on macronutrients and dietary composition. Micronutrients, however, may also play a role in CVD prevention. Specifically, limited data suggest an inverse association between a relatively high dietary intake of calcium and vitamin D and risk of CVD (2–4). One potential mechanism that may explain this inverse association is an effect of these nutrients on the concentrations of circulating lipids—an established risk factor for CVD.
Several (5–11), but not all (12–15), randomized, placebo-controlled, clinical trials have suggested that supplementation with 1–2 g elemental Ca/d may lower total and LDL-cholesterol concentrations by ≈5% and increase HDL by 5%. However, all of these studies evaluated the effect of short-term (≤1 y) calcium supplementation. In addition, these studies were also limited by relatively small sample sizes; the largest study thus far had only 223 participants. In terms of the effect of vitamin D supplementation on concentrations of lipids, the results from the 3 small studies conducted so far are inconsistent (16–18). Furthermore, only one study has evaluated the effect of the combined supplementation of calcium and vitamin D on the lipid profile, and it reported a null effect (15). Using data from the Women's Health Initiative (WHI), we conducted the current study to evaluate the long-term effect of calcium and vitamin D supplementation on circulating concentrations of lipid variables, including total cholesterol, LDL cholesterol, HDL cholesterol, non-HDL cholesterol, triglycerides, and lipoprotein(a) [Lp(a)].
SUBJECTS AND METHODS
The WHI consists of a set of clinical trials and a parallel observational study among ethnically diverse women from different parts of the United States, which was designed to address some of the major causes of morbidity and mortality in postmenopausal women. Details of the scientific rationale, eligibility requirements, and other aspects of the design of the WHI were published elsewhere (19). In brief, the WHI clinical trials (WHI-CT) were designed to evaluate the benefits and risks of dietary modification (DM), hormone therapy (HT), and supplementation with calcium and vitamin D (CaD) (19). Overall, a total of 68,132 women aged 50–79 y were randomly assigned into the DM and HT trials. At the first or second annual visits, eligible participants from these trials were invited to be randomly assigned further to CaD supplementation (n = 18,176) or placebo (n = 18,106) (20, 21). Women were eligible to participate in the CaD trial if they 1) were postmenopausal volunteers of any race or ethnicity, 2) were aged 50–79 y inclusive at the first screening, 3) were likely to reside in the study area for ≥3 y after randomization, and 4) provided written informed consent. The exclusion criteria for the CaD component included current daily use of ≥600 IU supplemental vitamin D or calcitriol, inadequate adherence to the DM component during the first or second year of follow-up, a history of renal calculi, hypercalcemia, current use of oral corticosteroids for >6 mo, or a previous osteoporosis-related fracture being treated with CaD. Women in the CaD trial were randomly assigned to take either 2 tablets for a total of 1 g elemental Ca (as calcium carbonate) and 400 IU vitamin D3/d or 2 identical-looking placebo tablets.
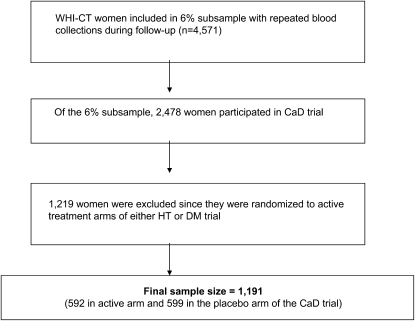
The current analysis was conducted within the 6% subsample of the WHI-CT (n = 4571) women with repeated blood sample collections at baseline and years 1, 3, and 6 y and in whom a number of core analytes, including lipids, were measured at each time point. Of these women, 2478 participated in the CaD trial, of whom we excluded 1259 women who were in the active treatment arms of either the DM or the HT trial. We chose to exclude women in the active arms of the other trials to eliminate any potential bias due to the effect of the other interventions on lipid concentrations. The final sample size for the analysis was 1191 women (Figure 1). Because the CaD trial was initiated after 1 y of the other WHI-CT trials, the year 1 follow-up of the WHI-CT women was considered as the baseline for this analysis, and repeated measurements of lipids were available at years 2 and 5. Lipid measures were obtained from frozen stored (at −70°C) samples and assayed at Medical Research Laboratories Inc (Highland Heights, KY). The Friedewald formula was used to calculate the concentration of LDL cholesterol from the concentrations of total cholesterol, HDL cholesterol, and triglycerides for those women who had a triglyceride value <400 mg/dL.
FIGURE 1.
Study population and sample size of the current study. WHI-CT, Women's Health Initiative clinical trials; DM, dietary modification; HT, hormone therapy, CaD, Calcium plus Vitamin D.
The active and placebo groups were compared in terms of baseline (year 1 of the WHI-CT was baseline for the CaD trial) characteristics, including sociodemographic data (eg, age and race), anthropometric variables (BMI and waist circumference), and lifestyle factors (eg, smoking and physical activity) All analyses were conducted by using the intention-to-treat approach, ie, data from each study participant were analyzed as per her initial assignment to the active or the placebo arm.
We calculated mean changes in the concentration of each biomarker from baseline to a specified follow-up time (year 2 or 5) within the active and placebo arms. We also calculated the difference in mean change between the active and placebo groups at years 2 and 5 separately. Furthermore, using data on lipid biomarkers from both the follow-up visits together, we conducted an analysis with a linear mixed-effects model to evaluate change in lipid biomarker concentrations over time from baseline with a random intercept to account for correlations between repeated observations for the same woman. Time since randomization was included in the model as a categorical variable (year 2 compared with year 5). An interaction term between time since randomization and intervention group was also included to allow the effect of intervention to be different at year 2 and year 5. A Wald's test was used to assess whether the intervention effect was statistically different from the placebo. The baseline concentration of each lipid biomarker was also included as a covariate to account for the potential effect due to "regression to the mean" (22). Because weight change may contribute to the changes in lipids, we also evaluated the effect of additional adjustment for the corresponding change in weight between baseline and follow-up time. In a sensitivity analysis, we evaluated the effect of adjustment of average compliance over the follow-up as a covariate. We used likelihood-ratio tests to test for interactions. All statistical analyses were conducted by using SAS software (SAS Institute, Cary, NC), and 2-sided P values ≤0.05 were considered statistically significant. Missing data were handled by the complete case method by using observations without any missing data (23).
RESULTS
The baseline characteristics of the study participants, by intervention group, are shown in Table 1. The treatment and placebo groups were similar with respect to their sociodemographic characteristics, lifestyle factors, anthropometric variables, medical history, and biochemical variables at baseline. The mean lipid values at baseline and at the end of years 2 and 5 and the associated mean changes by intervention group are shown in Table 2. Overall, the change in all the lipid factors was relatively small; for example, the mean decrease in LDL-cholesterol concentrations was 6.5 ± 33.0 mg/dL (−5.0%) in the intervention group and 6.3 ± 35.2 mg/dL (−4.7%) in the placebo group at the end of 5 y of the intervention. Similarly, the mean changes in HDL-cholesterol and triglyceride concentrations corresponded to a change of <5% in both trial arms at the end of the study. In general, compared with the change at the end of 2 y, the mean change at 5 y was of a larger magnitude and in the same direction. However, the concentrations of Lp(a) decreased at the end of 2 y (3.5% in the active arm and 7.9% in the placebo arm) but increased by 25.8% in the active arm and 17.3% in the placebo arm at the end of 5 y. Importantly, the differences in mean change between the active and placebo groups were not statistically significant at the end of year 2 or year 5 for any of the lipid variables. The lipid estimates (β coefficient) from the linear mixed-effects model with repeated measurements are shown in Table 3. These estimates represent the mean change in lipid variables between active and placebo groups at year 2 or year 5 after control for the baseline concentration of the lipid variable. We found no statistically significant differences in the changes of any lipid variables. Furthermore, the intervention effects did not vary over time (ie, the interaction was not significant). In addition, the adjustment for weight change during follow-up did not change the results.
TABLE 1.
Baseline characteristics of the study population in the Calcium Plus Vitamin D Trial, by intervention group1
| Characteristics | Active arm | Placebo arm | P value2 |
| No. of subjects | 592 | 599 | |
| Age (y) | 61.6 ± 6.83 | 62.1 ± 7.1 | 0.27 |
| Race [n (%)] | 0.62 | ||
| White | 290 (49) | 302 (50) | |
| Other | 302 (51) | 297 (50) | |
| Smoking status [n (%)] | 0.25 | ||
| Never smoked | 298 (51) | 329 (56) | |
| Past smoker | 232 (40) | 211 (36) | |
| Current smoker | 53 (9) | 48 (8) | |
| Missing | 9 (1.5) | 11 (1.8) | |
| Hormone use status [n (%)] | 0.40 | ||
| Never used | 316 (53) | 342 (57) | |
| Past user | 110 (19) | 107 (18) | |
| Current user | 165 (28) | 149 (25) | |
| BMI (kg/m2) | 29.7 ± 6.4 | 29.3 ± 6.1 | 0.83 |
| Waist (cm) | 89.3 ± 14.0 | 88.8 ± 13.8 | 0.64 |
| Total METs per week | 9.8 ± 11.9 | 10.4 ± 11.9 | 0.41 |
| Hypertension [n (%)] | 214 (36) | 205 ± 35 | 0.55 |
| Diabetes [n (%)] | 46 (8) | 33 ± 6 | 0.12 |
| Glucose (mg/dL) | 103.6 ± 32.4 | 103.5 ± 32.9 | 0.65 |
| Insulin (μIU/mL) | 12.7 ± 8.1 | 12.1 ± 7.7 | 0.60 |
| Alcohol intake (g/d) | 2.9 ± 6.9 | 3.6 ± 9.2 | 0.29 |
| Total fat intake (% of energy) | 35.7 ± 7.0 | 35.9 ± 6.6 | 0.85 |
| Dietary calcium intake (mg) | 707.7 ± 403.2 | 734.8 ± 424.4 | 0.29 |
| Calcium supplement use [n (%)] | 90 (15) | 74 (13) | 0.17 |
| Vitamin D use [n (%)] | 26 (4) | 21 (4) | 0.45 |
METs, metabolic equivalent tasks.
Chi-square test was used for categorical variables, and Kruskal-Wallis test was used for continuous variables.
Mean ± SD (all such values).
TABLE 2.
Means and mean changes (in mg/dL) in lipid variables in the Calcium Plus Vitamin D Trial, by intervention group
| Total cholesterol |
LDL cholesterol |
HDL cholesterol |
Non-HDL cholesterol |
Triglycerides |
Lipoprotein(a) |
|||||||
| n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | n | Mean ± SE | |
| Mean1 | ||||||||||||
| Active arm | ||||||||||||
| Baseline | 569 | 217.2 ± 1.6 | 565 | 130.3 ± 1.4 | 569 | 57.6 ± 0.6 | 569 | 159.6 ± 1.6 | 569 | 148.8 ± 3.8 | 569 | 25.9 ± 1.0 |
| Year 2 | 507 | 213.4 ± 1.6 | 500 | 127.3 ± 1.5 | 506 | 56.7 ± 0.7 | 506 | 156.8 ± 1.7 | 507 | 149.8 ± 3.5 | 507 | 25.1 ± 1.1 |
| Year 5 | 472 | 208.8 ± 1.7 | 466 | 123.5 ± 1.6 | 470 | 56.4 ± 0.6 | 470 | 152.6 ± 1.7 | 472 | 148.4 ± 3.5 | 472 | 32.5 ± 1.2 |
| Placebo arm | ||||||||||||
| Baseline | 569 | 222.7 ± 1.6 | 554 | 133.9 ± 1.6 | 569 | 58.6 ± 0.7 | 569 | 164.2 ± 1.7 | 569 | 151.4 ± 3.6 | 569 | 27.7 ± 1.2 |
| Year 2 | 513 | 218.5 ± 1.7 | 505 | 131.6 ± 1.6 | 510 | 57.6 ± 0.7 | 510 | 161.0 ± 1.7 | 513 | 148.4 ± 3.2 | 513 | 26.1 ± 1.1 |
| Year 5 | 477 | 213.1 ± 1.8 | 473 | 127.1 ± 1.6 | 477 | 57.4 ± 0.7 | 477 | 155.7 ± 1.8 | 477 | 145.8 ± 3.5 | 477 | 31.8 ± 1.2 |
| Mean change2 | ||||||||||||
| Active arm | ||||||||||||
| Year 2: baseline | 488 | −2.6 ± 1.3 | 479 | −1.8 ± 1.1 | 487 | −1.2 ± 0.4 | 487 | −1.4 ± 1.3 | 488 | 1.5 ± 3.3 | 488 | −0.9 ± 0.6 |
| Year 5: baseline | 458 | −8.5 ± 1.7 | 450 | −6.5 ± 1.6 | 456 | −1.4 ± 0.4 | 456 | −6.8 ± 1.7 | 458 | −2.4 ± 3.5 | 458 | 6.7 ± 0.7 |
| Placebo arm | ||||||||||||
| Year 2: baseline | 494 | −3.4 ± 1.3 | 478 | −1.3 ± 1.3 | 491 | −1.4 ± 0.4 | 491 | −2.1 ± 1.3 | 494 | −3.7 ± 2.5 | 494 | −2.2 ± 0.7 |
| Year 5: baseline | 458 | −8.7 ± 1.8 | 442 | −6.3 ± 1.7 | 458 | −1.6 ± 0.4 | 458 | −7.1 ± 1.8 | 458 | −3.2 ± 3.7 | 458 | 4.8 ± 0.7 |
| Difference in mean change between the 2 arms3 | ||||||||||||
| Year 2 | 982 | 0.8 ± 1.9 | 987 | −0.5 ± 1.7 | 978 | 0.2 ± 0.5 | 978 | 0.7 ± 1.9 | 982 | 5.2 ± 4.1 | 938 | 1.3 ± 0.9 |
| Year 5 | 916 | 0.2 ± 2.4 | 892 | −0.2 ± 2.3 | 914 | 0.1 ± 0.6 | 914 | 0.3 ± 2.5 | 916 | 0.8 ± 5.1 | 889 | 1.8 ± 1.0 |
Means at year 2 or year 5 were not significantly different (P > 0.05) from baseline, and no significant difference between treatment arms was observed for the lipids.
Mean change at year 2 and year 5 was not different from zero, and no significant difference between treatment arms was observed.
Difference in mean change was calculated as the mean change in the active arm minus the mean change in the placebo arm.
TABLE 3.
Difference in mean changes (in mg/dL) in lipid variables between the active and placebo arms of the Calcium Plus Vitamin D Trial1
| Year 2 | Year 5 | |
| Total cholesterol | −1.31 ± 1.90 | −1.67 ± 1.96 |
| LDL | −1.68 ± 1.77 | −1.51 ± 1.82 |
| HDL | −0.01 ± 0.52 | −0.05 ± 0.54 |
| Non-HDL cholesterol | −1.15 ± 1.88 | −1.30 ± 1.93 |
| Triglyceride | 3.69 ± 3.65 | 1.43 ± 3.77 |
| Lipoprotein(a) | 0.76 ± 0.90 | 1.79 ± 0.92 |
All values are βs ± SEs. The β coefficient represents the mean change in lipid variables between the active and placebo arms at year 2 or year 5 after control for baseline lipid concentrations.
The results for changes in lipids at the end of the study differed little in the sensitivity, analysis which excluded women who reported current use of postmenopausal hormones, women who were <60% compliant with the study medications, or women who self-administered calcium or vitamin D supplements. However, the statistical power for these analyses was limited.
DISCUSSION
To our knowledge, this was the first randomized controlled trial to evaluate the effect of CaD supplementation on lipid concentrations over a 5-y period. Our results indicate that CaD supplementation is not associated with a significant change in important lipid variables between postmenopausal women.
Only a few studies of the effects of dietary calcium and vitamin D on the risk of CVD in humans have been conducted. Although some of these studies have suggested an inverse association of calcium and vitamin D with CVD risk, the overall results have been inconsistent (2–4, 24–26). Analysis of the CaD trial of the WHI (26), in which our current study was conducted, reported a null effect for the association between CaD and risk of developing CVD. One mechanism by which these nutrients might potentially exert a beneficial effect on CVD risk in humans is through an effect on circulating lipids (27, 28). Several animal experimental studies have suggested that calcium supplementation has beneficial effects on circulating concentrations of lipoproteins (29–32). Mechanistically, a high calcium intake may inhibit the absorption of dietary fatty acids by promoting the formation of indigestible calcium-lipid complexes in the gastrointestinal tract (8, 33). In addition, calcium supplementation may also affect circulating lipid concentrations by its effect on concentrations of parathyroid hormones and vitamin D, which also regulate adipocyte activity (34, 35). Although the exact mechanism by which vitamin D affects lipid concentrations is not known, it is possibly related to its potential benefit with respect to insulin sensitivity (36).
Bhattacharrya et al (5) conducted the first randomized clinical trial to evaluate the association between calcium intake and concentration of circulating cholesterol. In this study of 11 healthy men, which was conducted in 1969, investigators reported a 5% greater decrease in total cholesterol concentrations among those supplemented with 2 g/d of calcium carbonate or gluconate for 2 wk compared with those in the placebo group. However, lipid subfractions were not evaluated. Several randomized clinical trials conducted after this initial study, however, reported inconsistent results (7, 8, 10, 12–15, 37–39). The sample size across these clinical trials ranged from 13 to >200 participants, and follow-up time ranged from 4 wk to 1 y. Of the 10 placebo-controlled trials conducted so far, 4 found no significant change in serum cholesterol concentrations in the calcium supplementation arm compared with placebo (12–14, 37). The largest and the longest trial that evaluated this association was conducted in New Zealand, among 223 healthy postmenopausal women, in a study primarily designed to investigate the effect on bone fractures. The results from this study indicated that women who were randomly assigned to receive 1 g elemental Ca (as calcium citrate) per day had a significantly greater decrease in LDL (6%) and increase in HDL (7%) compared with the placebo group at the end of 1 y (38). The change in triglyceride concentrations, however, was similar in the 2 intervention groups.
Women randomly assigned to the active arm of the CaD trial in the WHI also received 400 IU vitamin D3/d in addition to calcium carbonate. Only a few studies have evaluated the effects of vitamin D supplementation on concentrations of circulating lipids. In a Finnish randomized trial of 464 postmenopausal women, supplementation with 300 IU vitamin D3/d had detrimental effects on the lipid profile, resulting in an increase in LDL-cholesterol and a decrease in HDL-cholesterol concentrations after 3 y of follow-up (16). However, a few other studies found no significant change in lipids in the intervention arm compared with placebo (17, 18), which may possibly be due to a short follow-up time (range: 6 wk to 1 y). Only one small clinical trial has previously evaluated the effect of combined supplementation with calcium and vitamin D, as in our current study. In this clinical trial of 39 healthy postmenopausal women, supplementation with 1 g elemental Ca as citrate along with 800 IU vitamin D3 was not associated with any significant difference in lipid concentrations compared with placebo after a 3-mo period (15), which is consistent with our results.
The strengths of the present study included its randomized design, large sample size, long follow-up time, and availability of repeated lipid measurements. A few limitations of this study, however, also warrant consideration. The study intervention included combined supplementation with calcium and vitamin D, so that we were not able to evaluate the effect of calcium and vitamin D supplementation alone. Furthermore, given that, in contrast with calcium, vitamin D supplementation may result in an increase in LDL-cholesterol and a decrease in HDL-cholesterol concentrations (16), the null association observed in this study may have resulted from the potentially opposing effects of calcium and vitamin D on lipids. In addition, we cannot rule out the possibility that an effect of calcium or vitamin D on lipids may occur at doses higher than that used in the present study. Finally, compliance with treatment may have been an additional limitation. During year 1, 60% of the participants took ≥80% of their study medication, and this percentage remained stable during follow-up, with small differences between groups. In addition, ≥70% took ≥50% of their study medication. An additional limitation of the study was the use of over-the-counter prescriptions of calcium and vitamin D supplements. However, our results were similar to those of a sensitivity analysis that excluded noncompliers and those who self-administered calcium and vitamin D supplements.
In conclusion, this large clinical trial, the first study to evaluate the association of calcium plus vitamin D supplementation on changes in circulating lipids over 5 y, found no significant effects of CaD supplementation on changes in lipid concentrations. Existing and/or future trials of calcium and vitamin D with adequate sample size, long-term follow-up, and repeated blood collections should also consider evaluating the effects of different doses of calcium and vitamin D supplements, both separately and together, on circulating lipid concentrations.
Acknowledgments
The authors’ responsibilities were as follows—SNR and TER: study concept and design; and SNR, XX, SW-S, and TER: data analysis. All authors contributed to the writing and editing of the manuscript. The authors thank Dan Wang for her assistance with the data analysis. No conflicts of interest were reported.
REFERENCES
- 1.Hu FB, Willett WC. Optimal diets for prevention of coronary heart disease. JAMA 2002;288:2569–78 [DOI] [PubMed] [Google Scholar]
- 2.Bostick RM, Kushi LH, Wu Y, Meyer KA, Sellers TA, Folsom AR. Relation of calcium, vitamin D, and dairy food intake to ischemic heart disease mortality among postmenopausal women. Am J Epidemiol 1999;149:151–61 [DOI] [PubMed] [Google Scholar]
- 3.Umesawa M, Iso H, Date C, et al. Dietary intake of calcium in relation to mortality from cardiovascular disease: the JACC Study. Stroke 2006;37:20–6 [DOI] [PubMed] [Google Scholar]
- 4.Michos ED, Blumenthal RS. Vitamin D supplementation and cardiovascular disease risk. Circulation 2007;115:827–8 [DOI] [PubMed] [Google Scholar]
- 5.Bhattacharyya AK, Thera C, Anderson JT, Grande F, Keys A. Dietary calcium and fat. Effect on serum lipids and fecal excretion of cholesterol and its degradation products in man. Am J Clin Nutr 1969;22:1161–74 [DOI] [PubMed] [Google Scholar]
- 6.Groot PH, Grose WF, Dijkhuis-Stoffelsma R, Fernandes J, Ambagtsheer JJ. The effect of oral calcium carbonate administration on serum lipoproteins of children with familial hypercholesterolaemia (type II-A). Eur J Pediatr 1980;135:81–4 [DOI] [PubMed] [Google Scholar]
- 7.Bell L, Halstenson CE, Halstenson CJ, Macres M, Keane WF. Cholesterol-lowering effects of calcium carbonate in patients with mild to moderate hypercholesterolemia. Arch Intern Med 1992;152:2441–4 [PubMed] [Google Scholar]
- 8.Denke MA, Fox MM, Schulte MC. Short-term dietary calcium fortification increases fecal saturated fat content and reduces serum lipids in men. J Nutr 1993;123:1047–53 [DOI] [PubMed] [Google Scholar]
- 9.Reid IR.Effects of calcium supplementation on circulating lipids: potential pharmacoeconomic implications. Drugs Aging 2004;21:7–17 [DOI] [PubMed] [Google Scholar]
- 10.Ditscheid B, Keller S, Jahreis G. Cholesterol metabolism is affected by calcium phosphate supplementation in humans. J Nutr 2005;135:1678–82 [DOI] [PubMed] [Google Scholar]
- 11.Major GC, Alarie F, Dore J, Phouttama S, Tremblay A. Supplementation with calcium + vitamin D enhances the beneficial effect of weight loss on plasma lipid and lipoprotein concentrations. Am J Clin Nutr 2007;85:54–9 [DOI] [PubMed] [Google Scholar]
- 12.Bostick RM, Fosdick L, Grandits GA, Grambsch P, Gross M, Louis TA. Effect of calcium supplementation on serum cholesterol and blood pressure. A randomized, double-blind, placebo-controlled, clinical trial. Arch Fam Med 2000;9:31–8, discussion 39 [DOI] [PubMed] [Google Scholar]
- 13.Karandish M, Shockravi S, Jalali MT, Haghighizadeh MH. Effect of calcium supplementation on lipid profile in overweight or obese Iranian women: a double-blind randomized clinical trial. Eur J Clin Nutr 2007;63:268–72 [DOI] [PubMed] [Google Scholar]
- 14.Karanja N, Morris CD, Illingworth DR, McCarron DA. Plasma lipids and hypertension: response to calcium supplementation. Am J Clin Nutr 1987;45:60–5 [DOI] [PubMed] [Google Scholar]
- 15.Gannage-Yared MH, Azoury M, Mansour I, Baddoura R, Halaby G, Naaman R. Effects of a short-term calcium and vitamin D treatment on serum cytokines, bone markers, insulin and lipid concentrations in healthy post-menopausal women. J Endocrinol Invest 2003;26:748–53 [DOI] [PubMed] [Google Scholar]
- 16.Heikkinen AM, Tuppurainen MT, Niskanen L, Komulainen M, Penttila I, Saarikoski S. Long-term vitamin D3 supplementation may have adverse effects on serum lipids during postmenopausal hormone replacement therapy. Eur J Endocrinol 1997;137:495–502 [DOI] [PubMed] [Google Scholar]
- 17.Carlson LA, Derblom H, Lanner A. Effect of different doses of vitamin D on serum cholesterol and triglyceride levels in healthy men. Atherosclerosis 1970;12:313–7 [DOI] [PubMed] [Google Scholar]
- 18.Lips P, Wiersinga A, van Ginkel FC, et al. The effect of vitamin D supplementation on vitamin D status and parathyroid function in elderly subjects. J Clin Endocrinol Metab 1988;67:644–50 [DOI] [PubMed] [Google Scholar]
- 19.The Women's Health Initiative Study Group Design of the Women's Health Initiative clinical trial and observational study. Control Clin Trials 1998;19:61–109 [DOI] [PubMed] [Google Scholar]
- 20.Jackson RD, LaCroix AZ, Cauley JA, McGowan J. The Women's Health Initiative calcium-vitamin D trial: overview and baseline characteristics of participants. Ann Epidemiol 2003;13:S98–106 [DOI] [PubMed] [Google Scholar]
- 21.Hays J, Hunt JR, Hubbell A, et al. The Women's Health Initiative recruitment methods and results. Ann Epidemiol 2003;13:S18–77 [DOI] [PubMed] [Google Scholar]
- 22.Barnett AG, Van Der Pols JC, Dobson AJ. Regression to the mean: what it is and how to deal with it. Int J Epidemiol 2005;34:215–20 [DOI] [PubMed] [Google Scholar]
- 23.Greenland S, Finkle WD. A critical look at methods for handling missing covariates in epidemiologic regression analyses. Am J Epidemiol 1995;142:1255–64 [DOI] [PubMed] [Google Scholar]
- 24.Wang TJ, Pencina MJ, Booth SL, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation 2008;117:503–11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Van der Vijver LP, van der Waal MA, Weterings KG, Dekker JM, Schouten EG, Kok FJ. Calcium intake and 28-year cardiovascular and coronary heart disease mortality in Dutch civil servants. Int J Epidemiol 1992;21:36–9 [DOI] [PubMed] [Google Scholar]
- 26.Hsia J, Heiss G, Ren H, et al. Calcium/vitamin D supplementation and cardiovascular events. Circulation 2007;115:846–54 [DOI] [PubMed] [Google Scholar]
- 27.Cappuccio FP, Elliott P, Allender PS, Pryer J, Follman DA, Cutler JA. Epidemiologic association between dietary calcium intake and blood pressure: a meta-analysis of published data. Am J Epidemiol 1995;142:935–45 [DOI] [PubMed] [Google Scholar]
- 28.Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr 2004;79:820–5 [DOI] [PubMed] [Google Scholar]
- 29.Jolma P, Koobi P, Kalliovalkama J, et al. Increased calcium intake reduces plasma cholesterol and improves vasorelaxation in experimental renal failure. Am J Physiol Heart Circ Physiol 2003;285:H1882–9 [DOI] [PubMed] [Google Scholar]
- 30.Vaskonen T, Mervaala E, Sumuvuori V, Seppanen-Laakso T, Karppanen H. Effects of calcium and plant sterols on serum lipids in obese Zucker rats on a low-fat diet. Br J Nutr 2002;87:239–45 [DOI] [PubMed] [Google Scholar]
- 31.Appleton GV, Owen RW, Williamson RC. The effect of dietary calcium supplementation on intestinal lipid metabolism. J Steroid Biochem Mol Biol 1992;42:383–7 [DOI] [PubMed] [Google Scholar]
- 32.Shi H, Dirienzo D, Zemel MB. Effects of dietary calcium on adipocyte lipid metabolism and body weight regulation in energy-restricted aP2-agouti transgenic mice. FASEB J 2001;15:291–3 [DOI] [PubMed] [Google Scholar]
- 33.Welberg JW, Monkelbaan JF, de Vries EG, et al. Effects of supplemental dietary calcium on quantitative and qualitative fecal fat excretion in man. Ann Nutr Metab 1994;38:185–91 [DOI] [PubMed] [Google Scholar]
- 34.Zemel MB, Shi H, Greer B, Dirienzo D, Zemel PC. Regulation of adiposity by dietary calcium. FASEB J 2000;14:1132–8 [PubMed] [Google Scholar]
- 35.Kelly KA, Gimble JM. 1,25-Dihydroxy vitamin D3 inhibits adipocyte differentiation and gene expression in murine bone marrow stromal cell clones and primary cultures. Endocrinology 1998;139:2622–8 [DOI] [PubMed] [Google Scholar]
- 36.Lind L, Hanni A, Lithell H, Hvarfner A, Sorensen OH, Ljunghall S. Vitamin D is related to blood pressure and other cardiovascular risk factors in middle-aged men. Am J Hypertens 1995;8:894–901 [DOI] [PubMed] [Google Scholar]
- 37.Karanja N, Morris CD, Rufolo P, Snyder G, Illingworth DR, McCarron DA. Impact of increasing calcium in the diet on nutrient consumption, plasma lipids, and lipoproteins in humans. Am J Clin Nutr 1994;59:900–7 [DOI] [PubMed] [Google Scholar]
- 38.Reid IR, Mason B, Horne A, et al. Effects of calcium supplementation on serum lipid concentrations in normal older women: a randomized controlled trial. Am J Med 2002;112:343–7 [DOI] [PubMed] [Google Scholar]
- 39.Heaney RP, Recker RR, Lappe JM. Effects of calcium supplementation on serum lipid levels in postmenopausal women. Am J Med 2003;114:620–1, author reply 621 [DOI] [PubMed] [Google Scholar]