Abstract
We investigated associations between personality and health cognitions and behaviors related to preparation for future care among 355 primary care patients who were 65 years of age and older. Path analyses examined the effects of the personality traits of neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness on health cognitions about future care (avoidance, awareness), health-planning behaviors (gathering information, decision making, and planning), and beliefs about planning, while covarying age, gender, education, medical burden, functional status, and depression-symptom severity. Higher levels of neuroticism, openness, and agreeableness were associated with greater awareness of care needs; higher openness was also associated with more gathering of information and less avoidance. Extraversion and conscientiousness were not related to future-oriented health cognitions. Depression was inversely associated with the gathering of information. Age and education were related to more positive beliefs about the planning. Neither concrete planning nor decision making were related to personality variables. Health professionals should consider the impact of individual differences when addressing preparation for future care with older adults.
Keywords: Long-term care planning, Personality traits, Primary care, Future care needs, Decision-making, Health cognitions
As Populations age worldwide, the need to plan for future health care and residential adjustments will continue to grow. For example, 21% of persons aged 70 years and older who have no functional limitations can be expected to develop disabling limitations over a 2-year period (Anderson, James, Miller, Worley, & Longino, 1998), and 30% are likely to become disabled over a 6-year period (Sonn, Grimby, & Svanborg, 1996). Because planning enhances access to choices and helps individuals to gain control over their environment, the extent to which older adults prepare for future care needs will likely play a role in their ability to enhance their health-related quality of life and could even prevent disease progression. Nevertheless, surprisingly few older adults engage in care-planning behaviors (Sörensen & Pinquart, 2000a, 2000c), and there is little awareness among aged adults that failure to plan may lead to crisis decision making (Maloney, Finn, Bloom, & Andresen, 1996) and negative mental health outcomes, such as worry and depression symptoms (Pinquart & Sörensen, 2002b; Steele, Pinquart, & Sörensen, 2003). Thus one public health challenge in aging services may be to help older adults overcome their reluctance to engage in preventive health behaviors. Engaging in behaviors that promote or protect health requires an awareness of the risks for disease-related disability (Gerrard, Gibbons, Benthin, & Hessling, 1996; Harrison, Mullen, & Green, 1992), such as by understanding that one’s vision loss may limit independent living, and willingness to act on these and other health cognitions, such as by choosing a more supportive living environment.
The proactive coping model suggests that preparation for future stressors by mobilizing resources and considering responses in advance may help people cope with age-related stressors and improve well-being (Aspinwall, 1997a, 1997b). Preparation for future care (PFC) is a type of health-promotion activity that combines thoughts and actions (Sörensen & Pinquart, 2001; Sörensen & Pinquart, 2000b). Individuals who have made concrete plans are more likely to be satisfied with the level of discussion and planning in their family (Sörensen & Zarit, 1996), are less likely to suffer health problems that are due to loss of control over care arrangements (Reinardy, 1992), and are less likely to end up “scrambling” to find new living arrangements after they have experienced a crisis (Maloney et al., 1996). Proposed explanations of planning processes have emerged from theories of reasoned action (Heckhausen, 1989; Kuhl, 1981) and planning in everyday situations (Scholnick & Friedman, 1993). Most involve a series of steps, including (a) gathering information about the present situation, (b) gathering information about future goals, (c) evaluating options for reaching these goals, (d) making and choosing plans for how to reach the goals, and (e) implementing plans.
Three types of studies on care planning and related constructs exist: research on general planfulness (e.g., “I like to plan for the future”) and future-oriented thinking; studies on awareness of long-term-care choices; research on PFC and on thoughts, beliefs, and actions regarding expectable health care needs. Prenda and Lachman (2001)showed that planful older adults report greater life satisfaction. Furthermore, future-oriented thinking enhances subsequent health-promotion behaviors, such as exercise (Kahana, Kahana, & Zhang, 2005). Prospective research shows that older adults with greater awareness of long-term-care preferences tend to have better subjective well-being at follow-up (Brechling & Schneider, 1993; Coulton, Dunkle, Haug, Chow, & Vielhaber, 1989; Reinardy, 1995). PFC research suggests that older individuals who engage in concrete care planning report greater subjective well-being in concurrent analyses (Pinquart & Sörensen, 2002b; Steele et al., 2003).
Andersen and colleagues (Andersen, 1995; Andersen & Newman, 1973) suggest that three factors are related to health service use: predisposing, enabling, and need characteristics. These characteristics are important in PFC as well. Predisposing characteristics for PFC are female gender, higher education, more advanced age (Sörensen & Pinquart, 2000a), and social integration—through its enhancement of beliefs in the usefulness of planning (Sörensen & Pinquart, 2000b). Need characteristics that affect PFC include greater limitations in instrumental activities of daily living, which are likely to alert older adults to the necessity of receiving future care (Sörensen & Pinquart, 2000b), and medical burden. Enabling factors for service awareness and future care planning include higher income (Sörensen & Pinquart, 2000a), nonkin advisers, membership in clubs, contacts with other community agencies, and availability of transportation (Chapleski, 1989). Enabling factors include sociocultural variables: For example, middle-aged Americans are more likely than their German age peers to say that they invest thought and effort into their health (Staudinger, Fleeson, & Baltes, 1999). Compared with German seniors, American elders report greater awareness of their future care needs, more preparatory activities, and more knowledge about services (Pinquart, Sörensen, & Davey, 2003), perhaps as a result of national differences in resources.
In his 1995 revision of The Behavioral Health Model, Andersen (1995) suggests that individual psychological and genetic factors may affect health cognitions and health behaviors, independent of other predisposing factors. Indeed, personality traits contribute to health behaviors and cognitions (Roberts, Walton, & Bogg, 2005) and may also be related to preparing for future care needs. Consistent with this view, social-cognitive processes such as rational and avoidant decision styles (Scott & Bruce, 1995) as well as internal locus of control have been shown to be related to preparation for future health care needs (Sörensen, 1998; Sörensen & Pinquart, 2001). Qualitative studies suggest individual differences in styles of planning (Maloney et al., 1996; Sörensen & Pinquart, 2000c). Such individual differences are perhaps based in long-standing dispositions, such as personality traits.
This study aims to investigate whether Five Factor Model personality traits (McCrae & Costa, 1997) are significantly related to health cognitions and behaviors identified in previous studies as processes of PFC (Sörensen & Pinquart, 2001). PFC consists of five subscales: Awareness of Future Care Needs, Gathering Information (about care needs and options), Decision Making (about preferences), Concrete Planning, and (active) Avoidance (of future care planning). We also include a scale measuring beliefs about the usefulness of care planning. To our knowledge, personality trait correlates of older adults’ future care planning have not been assessed previously in the literature.
Because depression is associated with neuroticism (Lyness et al., 1998; Ormel, Oldehinkel, & Brilman, 2001) but also with a stronger orientation toward the present and with negative views of the future (Linden, Hautzinger, & Hoffman, 1983; Wertheim & Schwarz, 1983), depression symptoms can also affect future care planning. Individuals with more severe depression symptoms may be predisposed to more negative thoughts about future care needs, and therefore have higher levels of awareness, but are less likely to gather information or make concrete plans aimed at meeting these needs. In order to disentangle stable personality traits from depression, we include depression-symptom severity as a covariate.
Hypotheses
Neuroticism
Higher neuroticism levels have been associated with more worry and anxiety about health (Peltzer, 2004). Therefore, we hypothesized that neuroticism would be associated with more awareness of future care needs. Individuals with high levels of neuroticism tend to be less effective at problem solving (Watson & Hubbard, 1996) and therefore less likely to gather information or make concrete plans; in addition, their overall planfulness is below average (Prenda & Lachman, 2001) and they engage in fewer preventive health behaviors (Peltzer). Consequently, we expected neuroticism to be associated with lower scores on the Gathering Information and Concrete Planning subscales, as these activities require active problem solving in the presence of anxiety-provoking thoughts. Although no studies on neuroticism and decision making exist for older adults, the literature suggests that neuroticism is related to indecision in young and middle-aged adults (Jackson, Furnham, & Lawty-Jones, 1999; Meyer & Winer, 1993). Thus, we hypothesized that older adults with high levels of neuroticism would be more likely to avoid decision making and less likely to believe that planning is useful.
Multiple aspects of extraversion lead to contradictory conclusions about its relationship to health cognitions. Extraversion is related to indicators of social support or activity (Cutrona, Hessling, & Suhr, 1997; Von Dras & Siegler, 1997). Thus, one might hypothesize that extraversion would be related to more information gathering, which is partially dependent on social resources (Sörensen & Pinquart, 2000b). Extraversion is associated with positive affect and optimism (Costa & McCrae, 1992), as well as more positive health behaviors (Kressin, Spiro, Bosse, & Garcia, 1999) and more positive health behavior outcome expectancies (Williams, O’Brien, & Colder, 2004), all associated with more PFC. Conversely, extraversion is related to greater hope fur the future (Tellegen, 1985) and positive views of future health (Chapman, Duberstein, Sörensen, & Lyness, 2006). An overly positive view of the future could inhibit planning for future frailty. Although we expected extraversion to be associated with more information gathering, we did not examine extraversion’s constituent components and thus did not hypothesize directional relationships to the other PFC scales.
Openness
Greater tolerance of ambiguity may be one aspect of high openness that allows individuals to consider a variety of future health-planning scenarios. Empirical work documents that greater general planfulness (Prenda & Lachman, 2001) and death preparation are both related to greater openness (Cappeliez & O’Rourke, 2002). Thus, we expected openness to be associated with more awareness of future care needs, more gathering of information, and more decision making. Because openness is positively associated with planful problem solving in couples (Bouchard, 2003) as well as creativity and cognitive flexibility (McCrae, 1987), processes indispensable to the cognitive aspects of PFC, we also expected greater openness to be related to higher scores on the Concrete Planning subscale and less avoidance of future care considerations.
Agreeableness
We did not expect agreeableness to be related to PFC, because there is no theoretical reason to believe that individuals high in agreeableness would be more or less likely to engage in making plans. More agreeable individuals may be more easily influenced by relatives, but this influence can lead to more or less planning, depending on the relatives’ attitudes and preferences.
Conscientiousness
Individuals who are conscientious tend to be dutiful, orderly, and goal oriented in trying to get their plans implemented (Costa & McCrae, 1992; McCrae & Costa, 2003). Conscientiousness is empirically associated with fewer risky health behaviors, such as smoking, risky driving, and excessive alcohol use (Roberts et al., 2005), and lower overall medical burden (Chapman, Lyness, & Duberstein, 2007); this suggests that conscientious individuals may reflect upon the future consequences of health choices. We expected conscientiousness to be associated with more information gathering, decision making, and concrete planning.
METHODS
Participants
We drew our sample from 710 adults who were 65 years of age or older and who were participating in an ongoing, naturalistic study of primary care patients. We recruited participants from private internal medicine practices and hospital-affiliated clinics. Practice physicians provided permission to recruit, a letter of support to use during recruitment, and access to participants’ medical files. Office staff identified eligible participants, who were approached in the waiting room and invited to participate by study staff. Some physicians and nurses mentioned the study to their patients, but this was infrequent and typically occurred after the patients had already been approached by our research personnel. The study attempted to recruit all patients aged 65 years and older who presented for care on selected days and were capable of giving consent. Study staff interviewed individuals in their homes and asked them to complete and mail back the PFC and personality questionnaires; 355 (50%) completed the interview and both questionnaires (see Table 1 for sample characteristics). Median income, measured in six categories of $20,000 increments, was $40,000 (Category: $30,000–$50,000); modal income was $20,000. Among respondents with complete data, 5.3% had a diagnosis of current major depression and 6.6% had a diagnosis of minor depression according to criteria from the appendix of the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders(DSM-IV).
Table 1.
Demographic Information for Participants With Complete NEO and PFC Data
| Information | n (%) M (SD) |
|---|---|
| Gender | |
| Female | 215 (60.6) |
| Male | 140 (39.4) |
| Race | |
| White | 342 (96.4) |
| African American | 7 (1.9) |
| Other | 6 (1.7) |
| Marital status | |
| Married or living with partner | 207 (58.3) |
| Widowed | 94 (26.6) |
| Single, separated, or divorced | 53 (15.0) |
| Missing | 1 (.02) |
| Preretirement occupation codes (Hollingshead Occupational Scale) | |
| Higher executives, proprietors, and major professionals | (16) |
| Business manager, medium-size business proprietor, and lesser professional | (25.6) |
| Administrative personnel, small business owners, and minor professionals | (15) |
| Clerical or sales workers, technicians, and owners of very small businesses | (22.5) |
| Age (65–95 years) | 74.76 (6.44) |
| Education (4–17 years) | 14.28 (2.34) |
| HDRS (0–37) | 8.54 (6.26) |
| CIRS (1–19) | 7.41 (2.91) |
| IADL (0–19) | 1.51 (3.26) |
Note: N = 355; CIRS = Cumulative Illness Rating Scale, IADL = instrumental activity of daily living, HDRS = Hamilton Depression Rating Scale; NEO = neuroticism, extraversion, and openness to experience (as well as agreeableness and conscientiousness); PFC = preparation for future care.
Procedures
Study staff interviewed participants for 2 hours in their homes; they used the Structured Clinical Interview for DSM-IV (Spitzer, Williams, & Gibbon, 1994) to assess mood disorders. Staff asked the participants detailed questions about health, medication use, social support, life events, religiosity, medical service use, instrumental activities of daily living, personal self-maintenance, cerebrovascular risk factors, and anxiety. Participants’ mental status was tested using the Mini-Mental State Examination (Folstein, Folstein, & McHugh, 1975). A psychiatrist, who was not affiliated with the practices from which the participants were recruited, reviewed all medical charts. Participants completed the PFC and the NEO-FFI survey after the interview (FFI stands for Five Factor Inventory and NEO is defined in the following paragraph).
Measures in the Current Analysis
Personality traits
The NEO-FFI is a 60-item, self-report questionnaire measuring each of the traits that constitute the Five Factor Inventory: neuroticism, extraversion, openness to experience, agreeableness, and conscientiousness (Costa & McCrae, 1992). Individuals high in neuroticism are prone to worry, nervousness, and feelings of insecurity (e.g., “I often feel inferior to others”). Those low in extraversion are shy and socially avoidant. Those high in extraversion tend to be outgoing and optimistic and prefer high stimulation and social situations (e.g., “I like to have a lot of people around me”). Individuals high in openness to experience are prone to fantasy, interested in aesthetics, and open to a variety of ideas, values, feelings, and unfamiliar experiences (e.g., “I have a lot of intellectual curiosity”). Persons high in agreeableness are compliant, trusting, straightforward, altruistic, modest, and caring (e.g., “I would rather cooperate with others than compete with them”). Those high in conscientiousness tend to be orderly, dutiful, self-disciplined, and deliberate (e.g., “I try to perform all the tasks assigned to me conscientiously”). The NEO-FFI has been validated (Costa & McCrae) across age groups (Weiss et al., 2005), and its utility in gerontological research and health research has been extensively documented (Hooker, Monahan, Bowman, Frazier, & Shifren, 1998; Lang, Staudinger, & Carstensen, 1998; Lyness et al., 1998; Patrick & Hayden, 1999; Schmutte & Ryff, 1997). In the current sample, the reliability estimates (Cronbach’s alpha measuring internal consistency) were acceptable: neuroticism = .81, extraversion = .75, openness to experience = .81, agreeableness = .78, and conscientiousness = .69.
Depression-symptom severity
We assessed the severity of the symptoms of depression by using the 24-item Hamilton Depression Rating Scale (HDRS), which is administered in a semistructured format in accordance with Williams (1988). We interspersed the HDRS probe questions from the Williams interview with corresponding symptom questions in the Structured Clinical Interview for DSM-IV. The HDRS is both self-report and examiner rated; scores are based on participants’ responses and nonverbal presentation (e.g., facial expression; psychomotor behavior). The severity of depressive symptoms in the week prior to interview, based on nine common symptoms, is assessed. The HDRS has been used in gerontological research (e.g., Lyness et al., 1995) and shows acceptable internal consistency for our data (α = .80). Interrater reliability (intraclass correlation) for the reliability of the individual ratings, based on six raters and five participants, was .93 (Shrout & Fleiss, 1979). The HDRS score served as a covariate in all analyses.
Functional status
We assessed functional status by using instrumental activities of daily living (IADLs; Lawton & Brody, 1969). The interviewer asked whether the participant was able to use the telephone, shop, do housekeeping, prepare food, take medications, do laundry, travel independently, and handle finances. Options ranged from 0 (can complete independently) to 3 (cannot do this at all). The alpha level was α = .91.
Medical burden
We assessed medical burden with the Cumulative Illness Rating Scale (CIRS; Linn, Linn, & Gurel, 1968). Completed by a physician on the basis of information from the participant interview and from review of the medical record, the CIRS quantifies the pathology in 13 organ systems. Its validity is well established (Royall, Cabello, & Polk, 1998). CIRS scores derived from reviews of physical examination findings in medical charts are highly correlated with CIRS scores derived from postmortem autopsy performed by a pathologist or medical examiner (Conwell, Forbes, Cox, & Caine, 1993). The CIRS score served as a covariate in all analyses.
Preparation for future care
A recently developed short form of Sörensen and Pinquart’s (2001) Preparation for Care Needs measure assesses two health cognitions (avoidance, awareness) and three health-planning behaviors (gathering information, decision making, and concrete planning) with items rated on a 5-point Likert scale. In a separate study, our confirmatory factor analysis showed that the items load as expected, and the five-factor solution has the best fit (χ2 = 281.4, df = 80, p < .000; Comparative Fit Index or CFI = 0.94; root mean square error of approximation or RMSEA = 0.058; standardized root mean residual or SRMR = 0.046) compared with more parsimonious factor solutions (Sörensen, Chapman, Lyness, Duberstein, & Pinquart, 2008). The three-item subscales have acceptable internal consistency in the current sample: the Awareness of Future Care Needs subscale (three items, α = .77; e.g., “Talking to other people has made me think about whether I might need help or care in the future”); the Avoidance subscale (three items, α =.71; e.g., “I try not to think about things like future loss of independence”); the Gathering Information subscale (three items, α = .75; e.g., “I have been following the public discussion in the media to learn more about care options”); the Decision Making subscale (three items, α = .74; e.g., “I have compared different options of obtaining help or care in the future and have decided which would work for me and which would not”); and the Concrete Planning subscale (three items, α =.68; e.g., “I have identified how I want to be cared for and taken concrete steps to ensure that those options are available”). Retest reliabilities for the longer PFC subscales ranged from rtt = .44 to rtt = .63. Evidence for validity is suggested in the finding that perceived knowledge of services among community-dwelling older adults is correlated with the Gathering Information subscale (Sörensen & Pinquart, 2001). In addition, higher baseline levels on all PFC subscales except awareness were significantly related to having long-term care insurance during the following four year period (Sörensen et al, 2008).
Beliefs about planning
The belief that planning is not useful (7 items; α = .86; “Since I can’t predict whether I will need care in the future, it’s not worth making plans for that occasion” is an attitude measure developed and validated by Sörensen and Pinquart (2001).
Analyses
We tested a path model to assess the effect of personality traits on PFC. The initial model included the five PFC factors and a PFC beliefs factor as outcome variables, the five personality traits as predictors, and age, gender, decrements in function (IADL), education, medical burden, and depression severity (HDRS) as covariates. We modeled directional effects between PFC factors (as suggested by Sörensen & Pinquart, 2000b) and correlations between the belief variable and the other PFC factors as well.
RESULTS
Participants
Multivariate analyses showed that, compared with participants who did not return the surveys, those who did were more educated (14.33 vs 13.66 years; F = 10.97, p < .01), had lower IADL scores (1.52 vs 2.63; F = 13.33, p < .001), and were more likely to be White (96.4% vs 87.6%; χ2 = 19.06, df = 1, p < .001).
Hypothesized Relationships
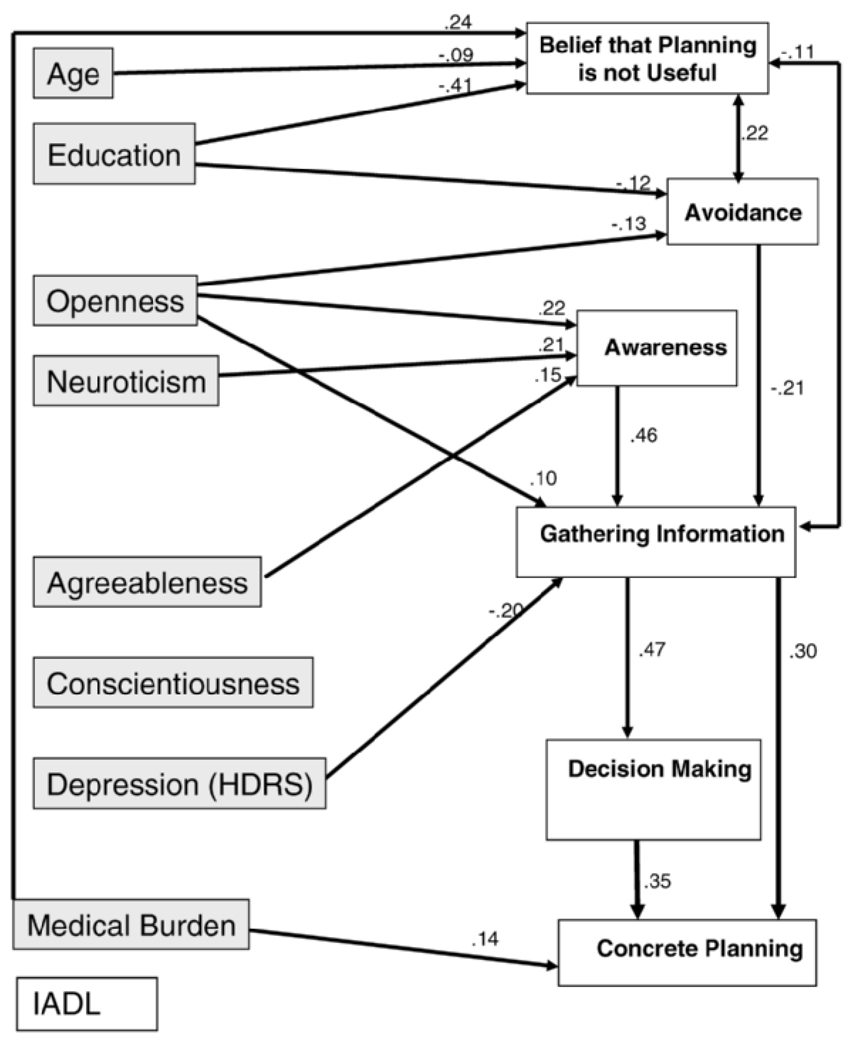
Bivariate correlations are shown in Table 2. Our initial path model included paths from all personality traits to all PFC subscales and to the beliefs about planning, as well as from age, gender, education, the CIRS, IADL decrements, and depression severity to all outcomes. The initial model had an excellent fit (χ2 = 3.29, df = 3, p = .35; CFI = 0.999, RMSEA = 0.018, SRMR = 0.007), despite a number of nonsignificant paths. Eliminating the variables with no relationships to PFC and the nonsignificant paths resulted in a slightly (not significantly) poorer fit (χ2 = 49.39, df = 38, p = .1020; CFI = 0.98, RMSEA = 0.03, SRMR = 0.04). Both models included directional relationships between the PFC variables. Figure 1 shows the final model, including only significant paths.
Table 2.
Means, Standard Deviations, and Bivariate Correlations of Study Variables (Listwise N = 350)
| Variable | Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Age | 74.6 | 6.44 | — | |||||||||||||||
| 2. | Gender | −.11* | — | ||||||||||||||||
| 3. | Education | 14.30 | 2.35 | −.17** | .23** | — | |||||||||||||
| 4. | CIRS | 7.45 | 2.93 | .27** | −.09* | −.09* | — | ||||||||||||
| 5. | HDRS | 8.45 | 6.24 | .07 | −.26** | −.19** | .37** | — | |||||||||||
| 6. | IADL | 1.51 | 3.26 | .20** | −.10* | −.23** | .37** | .39** | — | ||||||||||
| 7. | N | 14.99 | 7.69 | .05 | −.23** | −.27** | .27** | .61** | .33** | — | |||||||||
| 8. | E | 28.43 | 6.05 | −.04 | .03 | .11* | −.25** | −.36** | −.22** | −.49** | — | ||||||||
| 9. | O | 26.91 | 5.92 | −.13* | .00 | .45** | −.10* | −.08 | −.12* | −.18** | .22** | — | |||||||
| 10. | A | 35.17 | 4.96 | −.01 | −.18** | .14* | −.13** | −.20** | −.14** | −.37** | .29** | .06 | — | ||||||
| 11. | C | 34.23 | 5.79 | −.02 | .05 | .03 | −.22** | −.34** | −.19** | −.44** | .43** | .01 | .34** | — | |||||
| 12. | AW | 2.87 | .97 | .05 | −.05 | .01 | .08 | .17** | .12* | .21** | −.14** | .15** | .02 | −.14** | — | ||||
| 13. | AV | 2.92 | .92 | .10* | −.12* | −.19** | −.05 | .04 | .01 | .11* | −.02 | −.19** | −.07 | −.01 | −.06 | — | |||
| 14. | GI | 2.68 | 1.02 | −.10 | −.04 | .13** | .02 | −.09 | .02 | −.03 | .05 | .23** | .05 | .02 | .46** | −.26** | |||
| 15. | DM | 3.24 | .99 | .02 | −.11* | .06 | .12* | .07 | .08 | .06 | .05 | .19** | .01 | −.01 | .29** | −.11* | .49** | ||
| 16. | CP | 2.55 | 1.11 | .16** | −.10* | −.04 | .18** | .03 | .11* | .01 | .06 | .03 | .00 | .01 | .19** | −.14** | .45** | .48** | |
| 17. | No use | 2.1 | .90 | −.27** | .15** | .43** | −.23** | −.28** | .17** | −.34** | .13** | −.29** | −.21** | −.19** | −.03 | −.33** | −.27** | −.11* | −.03 |
Notes Gender uses a point-biserial correlation, with 1 = female, 2 = male; education uses Spearman’s rho. CIRS = Cumulative Illness Rating Scale, HDRS = Hamilton Depression Rating Scale, IADL = instrumental activity of daily living, N = neuroticism, E = extraversion, O = openness, A = agreeableness, C = conscientiousness, AW = awareness of future care needs, AV = avoidance of future care thoughts, GI = gathering information, DM = decision making, CP = concrete planning, No use = belief that planning is not useful. Higher scores indicated more of the characteristic for all variables.
p < .05;
p < .01.
Figure 1.
Path model of the relationship between personality traits, covariates, and preparation for future care (IADL = instrumental activity of daily living; HDRS = Hamilton Depression Rating Scale). All variables were treated as observed variables, as their factor structure has been established in previous research; higher scores indicated more of the characteristic for all variables. Model fit: χ2 = 49.39, df = 38, p = .102, Comparative Fit Index = 0.98, root mean square error of approximation = 0.03, standardized root mean residual = 0.04.
Neuroticism was positively related to greater awareness of future care, but no other PFC variables. Openness was positively associated with greater awareness, less avoidance, and more gathering of information, but not with decision making or concrete planning. Agreeableness predicted greater awareness. Conscientiousness and extraversion were not related to any PFC variables.
With regard to covariates, more education predicted less avoidance, and fewer negative beliefs about planning. Depression severity was negatively related to the gathering of information. Medical burden was positively related to concrete planning and to more negative beliefs about planning. Older participants were more likely to believe that planning is useful. Negative planning beliefs were inversely related to the gathering of information and positively correlated with avoidance.
The variance explained by the model for each outcome variable is as follows: awareness, R2 = .11; avoidance, R2 = .07; gathering information, R2 = .31; decision making, R2 = .27; concrete planning, R2 = .34; belief that planning is useless, R2 = .33.
DISCUSSION
To the best of our knowledge, this is the first study to investigate the role of personality traits in explaining variations in health cognitions and behaviors aimed at future care needs, specifically PFC. Consistent with our hypotheses, several personality traits are independently related to variations in health cognitions and behaviors aimed at future care needs, but only those occurring early in the planning process. In particular, awareness of future care needs is related to high openness, agreeableness, and neuroticism, and avoidance of future care thoughts is associated with lower openness. Furthermore, people with greater openness are more likely to gather information about care needs and options. Concrete planning and decision making are not related to personality traits, but they are associated with medical burden and the other PFC variables (i.e., awareness of care needs and gathering information). Although it cannot be tested here, the sequence of PFC behaviors suggested by Sörensen and Pinquart (2000a) is supported by our model. The emerging pattern suggests that Gathering Information is a central element in the overall progression of PFC. It is associated with personality traits, depression severity, early-stage awareness, and avoidance of care thoughts, and it is also a predictor of decision making and concrete planning activities.
Neuroticism
Individuals high in neuroticism tend to be more aware of future care needs. Both high awareness (Steele et al., 2003) and high neuroticism are linked to worry and anxiety (McCrae, 1990; Morris & Carden, 1981), especially for those with low scores on the Concrete Planning subscale (Steele et al.). Thus, those high in neuroticism may experience more distress during the planning process, especially in the early stages. Because awareness of future needs is also closely related to information gathering about needs and options, the lack of awareness associated with high neuroticism may stall the entire planning process.
Extraversion
The lack of findings for extraversion underscores the complex effect that extraversion may have on planning. An overly positive view of the future (Chapman et al., 2006; Tellegen, 1985; Williams et al., 2004) may thwart care planning, whereas being interested in social interaction (Sörensen & Pinquart, 2000b), its potential access to information, as well as a tendency toward more positive health behaviors (Kressin et al., 1999) could have a positive effect on planning.
Openness to Experience
Our results suggest that greater openness is important to the development of future care plans, as it is associated with both greater awareness of future care needs and more information gathering. This is consistent with the research by Prenda and Lachman (2001) suggesting that openness is related to more positive attitudes toward overall planfulness. Individuals who are relatively open to new experiences may be more likely to explore possible future events, even unpleasant ones, which makes it easier to think through possible scenarios of frailty and care.
Open individuals are also more creative, cognitively flexible, and skilled at divergent thinking (McCrae, 1987). These aspects of openness probably aid in future planning and the behavioral execution of such plans because they facilitate problem solving and permit the negotiation of obstacles in the planning process. Openness may be an important predisposing characteristic for the initiation of PFC, because it is related particularly to the early stages of the planning process, which have a strong relationship to later stages.
It is possible that lower levels of openness are associated with “negative arousal,” a type of heightened anxiety that leads to avoidance of problem solving (Aspinwall, 1997a). Low openness may confer risk for adverse health outcomes by means of the avoidance of problem solving and other preventive measures for unknown future dependence scenarios. Thus, individuals with low openness may be in need of interventions to encourage awareness of future care needs. They may also need assistance in following through to gather more information. However, once individuals who are low in openness are encouraged to make plans and gather information, other factors may play a more central role in determining PFC follow-through. In fact, the nonsignificant relationship of openness to making decisions about preferences and taking concrete planning steps may be ascribed to the possibility that people high in openness also prefer staying flexible and not committing to any particular plan.
Conscientiousness
Conscientiousness was not independently related to any future-care-related health cognitions or behaviors, even though previous research suggests that conscientiousness is linked to a more deliberate and planful pursuit of goals resulting in the achievement of greater financial security (Roberts, Caspi, & Moffitt, 2003); to fewer risky health behaviors, such as smoking, risky driving, and excessive alcohol use (Roberts et al., 2005); and to lower morbidity (Chapman et al., 2007).
One explanation for this null finding is that conscientiousness is linked to diligent and regular adherence to everyday routines in the present, rather than the creative development and exploration of future plans. The health cognitions and health behaviors of interest here are all future oriented. Even information gathering, a task requiring persistence and diligence, which we hypothesized to be associated with conscientiousness, primarily requires the individual to ponder expectable future health problems or possible care and residential choices. Gathering and reviewing health data may require openness-related cognitive functions, such as cognitive flexibility and curiosity. Future research might explore the possibility that everyday routinized behaviors related to future care needs, such as checking in daily with home-monitoring health care services, are more a function of conscientiousness than the explorative and intellectual aspects of PFC.
Our results are consistent with the health service use framework (Andersen, 1995). Our indicators of predisposing characteristics, need characteristics, and enabling factors were, for the most part, related to PFC. The finding that personality traits were independently associated with planning behaviors is consistent with the revisions of the Newman–Andersen model.
Other Findings
Individuals high in agreeableness are more likely to be aware of future care needs. Agreeable individuals may be more aware of future needs because they are more altruistic and would like to protect potential caregivers from being overburdened by care (Pinquart & Sörensen, 2002a). Agreeable individuals perceive and provide greater social support (Bowling, Beehr, & Swader, 2005), potentially improving their information resources, and may be more readily influenced by relatives, leading them to think more about future care.
Null findings with regard to the Decision Making and Concrete Planning subscales were unexpected. The personality traits studied here may be more influential in the initiation stages of planning. When it comes to making concrete decisions, such as putting one’s name on a waiting list for assisted living, older adults may be reluctant to act until frailty becomes more salient. Interestingly, people with greater medical burden have more negative beliefs about planning, which in turn appear to inhibit the gathering of information about future care. Perhaps the concrete steps of the PFC process are not activated before a still unidentified threshold of medical burden is reached,. With regard to conscientiousness, as well as the Concrete Planning subscale, low internal consistency (α = .68 and α = .69, respectively) also may have attenuated the relationships.
Limitations and Strengths
One limitation of this study is the cross-sectional design. Prospective studies are required to establish the PFC sequence definitively as well as to support a causal role for personality dispositions in planning processes. Recent research suggests the possibility of change in some personality variables (Terracciano, McCrae, Brant, & Costa, 2005). Future research might explore whether PFC is affected by changes in personality traits.
Our conclusions are also limited by the lack of ethnic and socioeconomic diversity in our sample. What little research exists does suggest that older African Americans and Latinos may differ from Whites in their approach to future care needs (Delgadillo, Sörensen, & Costner, 2004; Groger, 1994a, 1994b; Pinquart et al., 2003). Future research is also needed to understand the interplay of individual-level psychological variables beyond the personality traits examined here (e.g., control beliefs, needs and motives, defenses, information-seeking styles, and preferred decision strategies) and sociocultural variables (e.g., socioeconomic gradients, individualism vs collectivism, and cultural beliefs about family obligations) in the initiation and completion of future care plans. In addition, research with individuals who are not presenting for care at their primary care physician’s office, have no health insurance, or do not accept medical care may shed more light on the challenges of late-life planning.
One strength of this study is that it includes covariate coverage of current depression severity, using a measure that involves not only self-report but also interviewer ratings. Thus we are able to detect an effect of personality traits, even after accounting of the effects of depression. Furthermore, the presence of a physician-rated measure of medical burden (CIRS), rather than self-reported health, allowed for control of actual medical burden.
In sum, our research suggests that people with high neuroticism and agreeableness are more likely to think about their future care needs but not more likely to take behavioral steps toward planning. Those high in openness are less likely to avoid the sometimes unpleasant thoughts about future care and more likely to gather information about care options. Depression is likely to inhibit information gathering. Health care and social service providers may benefit from considering whether dispositional characteristics as well as situational mood factors will impede or enhance their older patients’ consideration of future care needs. Our research points to the need to approach the planning process differently for older adults varying in disposition. Taking into account personality differences in creating programs that encourage or teach future planning efforts may lead to better preparation for future care.
Personality traits affect responses to questions about subjective health, especially as people get older (Duberstein et al., 2003): Older people who are low in extraversion are more likely to believe that their health will get worse (Chapman et al., 2006). Furthermore, conscientiousness is independently associated with physician-rated morbidity (Chapman et al., 2007). Assessing personality in primary care may help physicians understand patients’ health cognitions, behaviors, and treatment decisions. Although such assessments may be difficult in the context of a primary care office, the use of existing very brief personality assessments, for example, the Ten-Item Personality Inventory (Gosling, Rentfrow, & Swann, 2003), allows the physician to recognize trait-associated health cognitions, behaviors, and outcomes, and this could facilitate more effective doctor–patient communication.
Historically, the social system in the United States has to some extent been based on consumer choice and the idea that people will take care of themselves. However, some people, by virtue of their traits, may not do this, making them vulnerable to receiving inadequate care. One solution is to develop individual-level interventions tailored to individual traits; another might be to design social programs that ensure quality care for all older adults, so that the adverse effects of certain personality traits will be minimized, if not eliminated.
ACKNOWLEDGMENTS
This research was supported by the following grants: K24MH072712 (Duberstein), T32 MH073452 (Lyness and Duberstein), K01 AG 022072-01 (Sörensen), R01 MH61429 (Lyness), and P20 MH071897 (Caine). An earlier version of this manuscript was presented in November 2004 at the 57th Annual Meeting of the Gerontological Society of America, Washington, DC.
Many thanks to Ebiere Okah and Larry Medici for assistance with data entry and management and to the seniors who kindly volunteered to participate in the study.
REFERENCES
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Andersen RM. Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior. 1995;36:1–10. [PubMed] [Google Scholar]
- Andersen RM, Newman DL. Societal and individual determinants of medical care utilization in the United States. Milbank Memorial Fund Quarterly—Health & Society. 1973;51:95–124. [PubMed] [Google Scholar]
- Anderson RT, James MK, Miller ME, Worley AS, Longino CF. The timing of change: Patterns in transitions in functional status among elderly persons. Journal of Gerontology: Psychological Sciences. 1998;53B:17–27. doi: 10.1093/geronb/53b.1.s17. [DOI] [PubMed] [Google Scholar]
- Aspinwall LG. Where planning meets coping: Proactive coping and the detection and management of potential stressors. In: Friedman SL, Scholnick EK, editors. The developmental psychology of planning: Why, how, and when do we plan? Mahwah, NJ: Erlbaum; 1997a. pp. 285–319. [Google Scholar]
- Aspinwall LG. Future-oriented aspects of social comparisons: A framework for studying health-related comparison activity. In: Buunk BP, Gibbons FX, editors. Health, coping, and well-being: Perspectives from social comparison theory. Mahwah, NJ: Erlbaum; 1997b. pp. 125–165. [Google Scholar]
- Bouchard G. Cognitive appraisals, neuroticism, and openness as correlates of coping strategies: An integrative model of adaptation to marital difficulties. Canadian Journal of Behavioural Science. 2003;35:1–12. [Google Scholar]
- Bowling NA, Beehr TA, Swader WM. Giving and receiving social support at work: The roles of personality and reciprocity. Journal of Vocational Behavior. 2005;67:476–489. [Google Scholar]
- Brechling B, Schneider C. Preserving autonomy in early stage dementia. Journal of Gerontological Social Work. 1993;20:17–33. [Google Scholar]
- Cappeliez P, O’Rourke N. Personality traits and existential concerns as predictors of the functions of reminiscence in older adults. Journal of Gerontology: Psychological Sciences. 2002;57:P116–P123. doi: 10.1093/geronb/57.2.p116. [DOI] [PubMed] [Google Scholar]
- Chapleski EE. Determinants of knowledge of services to the elderly: Are strong ties enabling or inhibiting? The Gerontologist. 1989;29:539–545. doi: 10.1093/geront/29.4.539. [DOI] [PubMed] [Google Scholar]
- Chapman BP, Lyness JM, Duberstein P. Personality and medical illness burden among older adults in primary care. Psychosomatic Medicine. 2007;69:277–282. doi: 10.1097/PSY.0b013e3180313975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman BP, Duberstein PR, Sörensen S, Lyness JM. Personality and perceived health in older adults: The five factor model in primary care. Journal of Gerontology: Psychological Sciences. 2006;61B:P362–P365. doi: 10.1093/geronb/61.6.p362. [DOI] [PubMed] [Google Scholar]
- Conwell Y, Forbes NT, Cox C, Caine ED. Validation of a measure of physical illness burden at autopsy: The cumulative illness rating scale. Journal of the American Geriatrics Society. 1993;41:38–41. doi: 10.1111/j.1532-5415.1993.tb05945.x. [DOI] [PubMed] [Google Scholar]
- Costa PT, Jr, McCrae RR. Revised NEO Personality Inventory and NEO Five Factor Inventory: Professional manual. Odessa, FL: Psychological Assessment Resources; 1992. [Google Scholar]
- Coulton CJ, Dunkle RE, Haug M, Chow J, Vielhaber DP. Locus of control and decision making for post-hospital care. The Gerontologist. 1989;29:627–632. doi: 10.1093/geront/29.5.627. [DOI] [PubMed] [Google Scholar]
- Cutrona CE, Hessling RM, Suhr JA. The influence of husband and wife personality on marital social support interactions. Personal Relationships. 1997;4:379–393. [Google Scholar]
- Delgadillo L, Sörensen S, Costner DC. An exploratory study of factors related to preparation for future care among older Latinos in Utah. Journal of Family and Economic Issues. 2004;25:51–79. [Google Scholar]
- Duberstein PR, Sörensen S, Lyness JM, King DA, Conwell Y, Seidlitz L, et al. Personality is associated with perceived health and functional status in older primary care patients. Psychology and Aging. 2003;18:25–37. doi: 10.1037/0882-7974.18.1.25. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. Mini-Mental State: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Gerrard M, Gibbons FX, Benthin AC, Hessling RM. A longitudinal study of the reciprocal nature of risk behaviors and cognitions in adolescents: What you do shapes what you think, and vice versa. Health Psychology. 1996;15:344–354. doi: 10.1037//0278-6133.15.5.344. [DOI] [PubMed] [Google Scholar]
- Gosling SD, Rentfrow PJ, Swann WB., Jr A very brief measure of the Big Five personality domains. Journal of Research in Personality. 2003;37:504–528. [Google Scholar]
- Groger L. Decision as process: A conceptual model of Black elders’ nursing home placement. Journal of Aging Studies. 1994a;8:94–104. [Google Scholar]
- Groger L. Limit of support and reaction to illness: An exploration of Black elders’ pathways to long-term care settings. Journal of Cross-Cultural Gerontology. 1994b;9:369–387. doi: 10.1007/BF00975005. [DOI] [PubMed] [Google Scholar]
- Harrison JA, Mullen PD, Green LW. A meta-analysis of studies of the Health Belief Model with adults. Health Education Research. 1992;7:107–116. doi: 10.1093/her/7.1.107. [DOI] [PubMed] [Google Scholar]
- Heckhausen H. Motivation und Handeln [Motivation and action] Berlin, Germany: Springer; 1989. [Google Scholar]
- Hooker K, Monahan D, Bowman SR, Frazier LD, Shifren K. Personality counts for a lot: Predictors of mental and physical health of spouse caregivers in two disease groups. Journal of Gerontology: Psychological Sciences. 1998;53B:P73–P85. doi: 10.1093/geronb/53b.2.p73. [DOI] [PubMed] [Google Scholar]
- Jackson CJ, Furnham A, Lawty-Jones M. Relationship between indecisiveness and neuroticism: The moderating effect of a tough-minded culture. Personality and Individual Differences. 1999;27:789–800. [Google Scholar]
- Kahana E, Kahana B, Zhang J. Motivational antecedents of preventive proactivity in late life: Linking future orientation and exercise. Motivation and Emotion. 2005;29:443–464. doi: 10.1007/s11031-006-9012-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kressin NR, Spiro A, III, Bosse R, Garcia RI. Personality traits and oral self-care behaviors: Longitudinal findings from the normative aging study. Psychology and Health. 1999;14:71–85. [Google Scholar]
- Kuhl J. Motivational and functional helplessness: The moderating effect of state versus action orientation. Journal of Personality and Social Psychology. 1981;19:448–468. [Google Scholar]
- Lang FR, Staudinger UM, Carstensen LL. Perspectives on socioemotional selectivity in late life: How personality and social context do (and do not) make a difference. Journal of Gerontology: Psychological Sciences. 1998;53B:P21–P30. doi: 10.1093/geronb/53b.1.p21. [DOI] [PubMed] [Google Scholar]
- Lawton MP, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Linden M, Hautzinger M, Hoffman N. Discriminant analysis of depressive interactions. Behavior Modification. 1983;7:402–422. doi: 10.1177/01454455830073007. [DOI] [PubMed] [Google Scholar]
- Linn BS, Linn MW, Gurel L. Cumulative illness rating scale. Journal of the American Geriatrics Society. 1968;16:622–626. doi: 10.1111/j.1532-5415.1968.tb02103.x. [DOI] [PubMed] [Google Scholar]
- Lyness JM, Cox C, Curry J, Conwell Y, King DA, Caine ED. Older age and the underreporting of depressive symptoms. Journal of the American Geriatrics Society. 1995;43:216–221. doi: 10.1111/j.1532-5415.1995.tb07325.x. [DOI] [PubMed] [Google Scholar]
- Lyness JM, Duberstein PR, King DA, Cox C, Caine ED. Medical illness burden, trait neuroticism, and depression in primary care elderly. American Journal of Psychiatry. 1998;155:969–971. doi: 10.1176/ajp.155.7.969. [DOI] [PubMed] [Google Scholar]
- Maloney SK, Finn J, Bloom D, Andresen J. Personal decision making styles and long-term care choices. Health Care Financing Review. 1996;18:141–156. [PMC free article] [PubMed] [Google Scholar]
- McCrae RR. Creativity, divergent thinking, and openness to experience. Journal of Personality & Social Psychology. 1987;52:1258–1265. [Google Scholar]
- McCrae RR. Controlling neuroticism in the measurement of stress. Stress Medicine. 1990;6:237–241. [Google Scholar]
- McCrae RR, Costa PT., Jr Personality trait structure as a human universal. American Psychologist. 1997;52:509–516. doi: 10.1037//0003-066x.52.5.509. [DOI] [PubMed] [Google Scholar]
- McCrae RR, Costa PT., Jr . Personality in adulthood: A five-factor theory perspective. 2nd ed. New York: Guilford Press; 2003. [Google Scholar]
- Meyer BW, Winer JL. The career decision scale and neuroticism. Journal of Career Assessment. 1993;1:171–180. [Google Scholar]
- Morris LW, Carden RL. Relationship between locus of control and extraversion-introversion in predicting academic behavior. Psychological Reports. 1981;83:799–806. [Google Scholar]
- Ormel J, Oldehinkel AJ, Brilman EI. The interplay and etiological continuity of neuroticism, difficulties, and life events in the etiology of major and subsyndromal, first and recurrent depressive episodes in later life. American Journal of Psychiatry. 2001;158:885–891. doi: 10.1176/appi.ajp.158.6.885. [DOI] [PubMed] [Google Scholar]
- Patrick JH, Hayden JM. Neuroticism, coping strategies, and negative well-being among caregivers. Psychology and Aging. 1999;14:273–283. doi: 10.1037//0882-7974.14.2.273. [DOI] [PubMed] [Google Scholar]
- Peltzer K. Preventive health behavior, personality, and religiosity among Black and White South Africans. Studia Psychologica. 2004;46:37–48. [Google Scholar]
- Pinquart M, Sörensen S. Factors that promote and prevent preparation for future care needs: Perceptions of older Canadian, German, and U. S. women. Health Care for Women International. 2002a;23(6–7):729–741. doi: 10.1080/07399330290107467. [DOI] [PubMed] [Google Scholar]
- Pinquart M, Sö rensen S. Psychological outcomes of preparation for future care needs. Journal of Applied Gerontology. 2002b;21:452–470. [Google Scholar]
- Pinquart M, Sörensen S, Davey A. National and regional differences in preparation for future care needs: A comparison of the United States and Germany. Journal of Cross-Cultural Gerontology. 2003;18:53–78. doi: 10.1023/a:1024878512547. [DOI] [PubMed] [Google Scholar]
- Prenda KM, Lachman ME. Planning for the future: A life management strategy for increasing control and life satisfaction in adulthood. Psychology and Aging. 2001;16:206–216. [PubMed] [Google Scholar]
- Reinardy JR. Decisional control in moving to a nursing home: Postadmission adjustment and well-being. The Gerontologist. 1992;32:96–103. doi: 10.1093/geront/32.1.96. [DOI] [PubMed] [Google Scholar]
- Reinardy JR. Relocation to a new environment: Decisional control and the move to a nursing home. Health and Social Work. 1995;20:31–38. doi: 10.1093/hsw/20.1.31. [DOI] [PubMed] [Google Scholar]
- Roberts BW, Caspi A, Moffitt TE. Work experiences and personality development in young adulthood. Journal of Personality and Social Psychology. 2003;84:582–593. [PubMed] [Google Scholar]
- Roberts BW, Walton KE, Bogg T. Conscientiousness and health across the life course. Review of General Psychology. 2005;9:156–168. [Google Scholar]
- Royall DR, Cabello M, Polk MJ. Executive dyscontrol: An important factor affecting the level of care received by older retirees. Journal of the American Geriatrics Society. 1998;49:1519–1524. doi: 10.1111/j.1532-5415.1998.tb01536.x. [DOI] [PubMed] [Google Scholar]
- Schmutte PS, Ryff CD. Personality and well-being: Reexamining methods and meanings. Journal of Personality and Social Psychology. 1997;58:549–559. doi: 10.1037//0022-3514.73.3.549. [DOI] [PubMed] [Google Scholar]
- Scholnick EK, Friedman SL. Planning in context: Developmental and situational considerations. International Journal of Behavioral Development. 1993;16:145–167. [Google Scholar]
- Scott SG, Bruce RA. Decision-making style: The development and assessment of a new measure. Educational and Psychological Measurement. 1995;55:818–831. [Google Scholar]
- Shrout PE, Fleiss JL. Intraclass correlations: Uses in assessing rater reliability. Psychological Bulletin. 1979;86:420–428. doi: 10.1037//0033-2909.86.2.420. [DOI] [PubMed] [Google Scholar]
- Sonn U, Grimby G, Svanborg A. Activities of daily living studied longitudinally between 70 and 76 years of age. Disability and Rehabilitation. 1996;18:91–100. doi: 10.3109/09638289609166023. [DOI] [PubMed] [Google Scholar]
- Sörensen S. Predictors of anticipating caregiving in multigeneration families: An exploratory study. Journal of Applied Gerontology. 1998;17:499–520. [Google Scholar]
- Sörensen S, Chapman B, Lyness JM, Duberstein PR, Pinquart M. The preparation for future care (PFC) measure: Development of a short form for the planning process. 2008 Manuscript submitted for publication. [Google Scholar]
- Sörensen S, Pinquart M. Vulnerability and access to resources as predictors of preparation for future care needs in the elderly. Journal of Aging and Health. 2000a;12:275–300. [Google Scholar]
- Sörensen S, Pinquart M. Preparation for future care needs by West and East German older adults. Journal of Gerontology: Social Sciences. 2000b;55B:S357–S367. doi: 10.1093/geronb/55.6.s357. [DOI] [PubMed] [Google Scholar]
- Sörensen S, Pinquart M. Preparation for future care needs: Styles of preparation used by older Eastern German, United States, and Canadian women. Journal of Cross-Cultural Gerontology. 2000c;15:349–381. doi: 10.1023/a:1006778627518. [DOI] [PubMed] [Google Scholar]
- Sörensen S, Pinquart M. Developing a measure of older adults’ preparation for future care needs. International Journal of Aging and Human Development. 2001;53:137–165. doi: 10.2190/1R0D-30TC-F4K1-F0DW. [DOI] [PubMed] [Google Scholar]
- Sörensen S, Zarit SH. Preparation for caregiving: A study of multigeneration families. International Journal of Aging and Human Development. 1996;42:43–63. doi: 10.2190/A8H1-W8BD-W6XL-2V2E. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M. Structured clinical interview for DSM-IV (SCID) New York: New York State Psychiatric Institute, Biometrics Research; 1994. [Google Scholar]
- Staudinger UM, Fleeson W, Baltes PB. Predictors of subjective physical health and global well-being: Similarities and differences between the United States and Germany. Journal of Personality and Social Psychology. 1999;76:305–319. [Google Scholar]
- Steele M, Pinquart M, Sörensen S. Preparation dimensions and styles in long term care. Clinical Gerontologist. 2003;26(3–4):105–122. [Google Scholar]
- Tellegen A. Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report. In: Tuma AH, Maser JD, editors. Anxiety and the anxiety disorders. Hillsdale, NJ: Erlbaum; 1985. pp. 681–706. [Google Scholar]
- Terracciano A, McCrae RR, Brant L, Costa PT. Hierarchical linear modeling analyses of the NEO-PI-R scales in the Baltimore longitudinal study of aging. Psychology and Aging. 2005;20:493–506. doi: 10.1037/0882-7974.20.3.493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Dras DD, Siegler IC. Stability in extraversion and aspects of social support at midlife. Journal of Personality and Social Psychology. 1997;72:233–241. doi: 10.1037//0022-3514.72.1.233. [DOI] [PubMed] [Google Scholar]
- Watson D, Hubbard B. Adaptational style and dispositional structure: Coping in the context of the five-factor model. Journal of Personality. 1996;64:737–774. [Google Scholar]
- Weiss A, Costa PT, Jr, Karuza J, Duberstein PR, Friedman B, McCrae RR. Cross-sectional age differences in personality among Medicare patients aged 65 to 100. Psychology and Aging. 2005;20:182–185. doi: 10.1037/0882-7974.20.1.182. [DOI] [PubMed] [Google Scholar]
- Wertheim E, Schwarz JC. Depression, guilt, and self-management of pleasant and unpleasant events. Journal of Personality and Social Psychology. 1983;45:884–889. doi: 10.1037//0022-3514.45.4.884. [DOI] [PubMed] [Google Scholar]
- Williams JBW. A structured interview guide for the Hamilton Depression Rating Scale. Archives of General Psychiatry. 1988;45:742–747. doi: 10.1001/archpsyc.1988.01800320058007. [DOI] [PubMed] [Google Scholar]
- Williams PG, O’Brien CD, Colder CG. The effects of neuroticism and extraversion on self-assessed health and health-relevant cognition. Personality and Individual Differences. 2004;37:83–94. [Google Scholar]