Abstract
Objectives
Although evidence suggests that physical disability and depression may be reciprocally related, questions of causality versus spuriousness and the direction of causality remain to be confidently answered. This study considered the hypothesis of reciprocal influence; the possibility of spuriousness in relation to pain, stress, and lifetime major depression; and the possible mediating effects of pain and social stress.
Methods
We analyzed data from a two-wave panel study of Miami-Dade County residents (n = 1,455) that included a substantial oversampling of individuals reporting a physical disability.
Results
Results indicated that, although prior levels of physical limitations predicted changes in depressive symptoms, there was no evidence of the reverse association. Results also indicated that part of the association between prior physical limitations and changes in depressive symptoms was explained by intervening level of pain and, to a lesser extent, by the day-to-day experience of discrimination.
Discussion
Much of whatever causation may be involved in the linkage between physical limitations and depressive symptomatology flows from limitations to depression rather than in the reverse direction. Results also make clear that this linkage is not an artifact of shared associations with pain, social stress, or lifetime major depression.
Keywords: Physical limitations, Depression, Stress, Pain
THE presence of physical limitations, by definition, implies a circumstance of limited capacity to meet the requirements of core social, familial, and occupational roles and thus to obtain associated rewards and satisfactions. From this perspective the now-abundant evidence linking physical health and depression (Bruce, Seeman, Merrill, & Blazer, 1994; Gurland, Wilder, & Berkman, 1988; Katon & Ciechanowski, 2002; Lenze et al., 2001) might have been anticipated. However, an alternative interpretation has been proposed based on the major correlates and consequences of depression. This perspective suggests that the reduced interest in activities and relationships, sleep problems, and fatigue that characterize depression tend to foster declines in physical performance.
Most prior research has limited consideration to only one of these alternative interpretations, presenting evidence that physical disability is a risk factor for depressive symptoms (Kennedy, Kelman, & Thomas, 1990; Roberts, Kaplan, Shema, & Strawbridge, 1997; Zeiss, Lewinsohn, Rohde, & Seeley, 1996) or that depressive symptomatology is a risk factor for physical disability (Bruce et al., 1994; Penninx, Leveille, Ferrucci, van Eijk, & Guralnik, 1999; Tinetti, Inouye, Gill, & Doucette, 1995). An early exception is the work of Aneshensel, Frerichs, and Huba (1984). In a study of a community-based sample of adults, they found evidence that physical illness and depression exert reciprocal effects over time. More recently, additional studies have considered the temporal and reciprocal associations between physical limitations and depressive symptoms, presenting results largely consistent with those of Aneshensel and colleagues (Geerlings, Beekman, Deeg, Twisk, & Van Tilburg, 2001; Meeks, Murrell, & Mehl, 2000; Ormel, Rijsdijk, Sullivan, van Sonderen, & Kempen, 2002).
Although there are no clear grounds for doubting the reciprocity of associations between physical limitations and depressive symptomatology, several issues of both theoretical and practical significance remain to be resolved. Still in question are (a) whether the observed associations are causal or artifactual and (b) the relative strengths of the directional predictions. Plausible sources of possible spuriousness include pain, social stress, and major depressive disorder. In addition, it is important to evaluate the extent to which intervening levels of pain and stress exposure mediate the physical limitation–depressive symptom relationships over time. This article explores the nature of the association between physical limitations and depressive symptoms over a 3-year interval.
Studies have consistently observed an association between physical limitations and depressive symptoms (Bruce et al., 1994; Everson-Rose et al., 2005; Gurland et al., 1988; Katon & Ciechanowski, 2002; Lenze et al., 2001; Turner, Lloyd, & Taylor, 2006; Turner & McLean, 1989). However, because many of these early investigations were cross-sectional, they could not confidently assess temporal order. Other recent studies have employed longitudinal designs, allowing for the specification of the time ordering of physical functioning and depressive symptoms.
For example, evidence has suggested that the presence and severity of physical disability increases risk for depression over time (Geerlings, Beekman, Deeg, & Van Tilburg, 2000; Kennedy et al., 1990; Schieman & Plickert, 2007; Turner & Noh, 1988; Yang & George, 2005). There is also substantial evidence indicating that depressive symptoms can lead to problems with physical health and functioning (Armenian, Pratt, Gallo, & Eaton, 1998; Bruce et al., 1994; Cronin-Stubbs et al., 2000; Dunlop, Manheim, Song, Lyons, & Chang, 2005; Jiang, Tang, Futatsuka, & Zhang, 2004; Lenze et al., 2005; Penninx, Deeg, van Eijk, Beekman, & Guralnik, 2000; Penninx et al., 1998, 1999). These lagged analyses have provided evidence consistent with the conclusion that physical limitations increase the risk of depression and vice versa. None of these studies, however, specifically considered reciprocal associations between physical limitations and depressive symptoms.
Aneshensel and colleagues (1984) conducted one of the first investigations to evaluate this possibility. They found that physical illness can lead to depression and that depression can lead to physical illness over a 1-year interval, and more recent findings have appeared to confirm such a reciprocal relationship (Geerlings et al., 2001; Ormel et al., 2002). It is of interest to note that prior studies have also found that physical health and limitations are stronger predictors of depressive symptomatology than vice versa (Aneshensel et al., 1984; Meeks et al., 2000; Ormel et al., 2002). An important recent study by Kelley-Moore and Ferraro (2005) examined reciprocal effects across three waves of data, distinguishing disease from disability. They were able to confirm reciprocal effects across both intervals between disease onset and depression. However, in analyses that included assessments of both disability and disease, they found no evidence of a predictive association between disability and depression or vice versa.
Taken together, the bulk of available evidence suggests a reciprocal association between physical limitations and depressive symptoms. However, researchers cannot answer with confidence the question of whether these observed linkages imply either mutual or directional causation. Not well considered in prior work is the possibility that the association between physical limitations and depressive symptoms might arise from their shared association with one or more influential third variables.
For example, level of pain is associated with both physical limitations (Bryant, Scarbro, & Baxter, 2001; Grigsby et al., 1999; Lichtenstein, Dhanda, Cornell, Escalante, & Hazuda, 1998) and depressive symptoms (Bair, Robinson, Katon, & Kroenke, 2003; Benjamin, Morris, McBeth, Macfarlane, & Silman, 2000; Corruble & Guelfi, 2000; Ruoff, 1996). Certainly, bodily pain limits the extent to which an individual can engage in physical activity, and the evidence that high levels of chronic pain are emotionally distressing confirms general expectation. The established link between pain and depression noted above may also arise partly from the fact that bodily pain and depression share physiological attributes (Bair et al., 2003).
Social stress is also associated with physical health limitations (Farmer & Ferraro, 1997; Lin & Ensel, 1989; Pavalko, Mossakowski, & Hamilton, 2003; Ross & Mirowsky, 2001) and is a major predictor of depressive symptoms (Bromberger & Matthews, 1996; Chiriboga, Black, Aranda, & Markides, 2002; Kessler, Mickelson, & Williams, 1999; Pearlin, Lieberman, Menaghan, & Mullan, 1981; Taylor & Turner, 2002). There has been substantial progress toward an understanding of the mechanisms by which stress exposure gets translated into increased risk for both physical and emotional health problems. For example, evidence from research on allostatic load (e.g., Geronimus, Hicken, Keene, & Bound, 2006; McEwen & Seeman, 1999; Seeman, Singer, Rowe, Horwitz, & McEwen, 1997) has specified a range of biomarkers that are affected by social stress and that mediate the demonstrated linkage between stress exposure and both morbidity and mortality. In the case of depression, stress exposure influences neuroendocrine responses that are correlates or expressions of depressive symptoms (e.g., Nierop, Bratsikas, Zimmermann, & Ehlert, 2006; Robles, Glaser, & Kiecolt-Glaser, 2005).
As noted elsewhere, most of what is known about the significance of social stress for health is based on studies that have estimated differences in stress exposure solely in terms of recent life events (Turner & Wheaton, 1995). In this context, researchers argued more than a decade ago that the stress hypothesis had not been effectively tested because stress exposure had not been adequately estimated (Turner, Wheaton, & Lloyd, 1995). Recent research has demonstrated the utility of going beyond recent life events to achieve more comprehensive assessments by revealing more powerful predictions of depressive symptomatology (Turner & Avison, 2003; Turner & Lloyd, 1999). Thus, an effective evaluation of possible spuriousness requires consideration of a range of different sources or types of social stress.
Finally, the observed relationship between major depressive disorder and higher levels of depressive symptoms (Breslau, 1985; Cuijpers & Smit, 2004; Horwath, Johnson, Klerman, & Weissman, 1992) is hardly surprising. When this fact is taken with the well-established cross-sectional relationship between depressive disorder and the presence of physical disability (Armenian et al., 1998; Turner et al., 2006), the need to consider the issue of spuriousness with respect to the physical limitation–depressive symptom relationship seems apparent.
Assuming some degree of causality in the observed physical limitation–depressive symptom relationships, a second question that, aside from speculation (Bruce et al., 1994), has largely escaped attention is that of what factors may mediate these directional or bidirectional relationships. The present analyses evaluated the reciprocal association between physical limitations and depressive symptoms over time. We assessed the independent significance of prior level of physical limitations in predicting changes in depressive symptoms, and vice versa, considering the mediating effects of intervening measures of pain and stress exposure.
Methods
Sample
The data employed in this study were from a two-wave (W1 and W2) panel study of Miami-Dade County residents that included a substantial oversampling of individuals with a physical disability. A total of 10,000 randomly selected households were screened with respect to gender, age, ethnicity, disability status, and language preference. Using this sampling frame, the study sample was drawn such that there were even numbers of women and men, even numbers of people screened as having a physical disability and those not, and equivalent numbers of the four major ethnic groups comprising more than 90% of all Miami-Dade County residents (non-Hispanic Whites, Cubans, non-Cuban Hispanics, and African Americans). These proportions departed only slightly from those for the county as a whole. Well-trained and predominantly bilingual interviewers administered computerized questionnaires in either English or Spanish as preferred by each participant. The majority of interviews took place in the homes of participants. However, a small number of interviews were conducted at alternative sites or by telephone when requested by participants.
A total of 1,986 first-wave interviews were completed in 2000–2001 out of 2,420 potential participants released to field study staff. Using participant payments of $50, the study achieved a success rate of 82%. Included were 1,086 adults who screened as having no physical disability and 900 individuals who screened as having a disability. The oversampling of individuals with a physical disability and the fact that the nondisabled participants were group matched on race/ethnicity, gender, and age resulted in a greater proportion of older respondents than in the general population. Ages in the sample ranged from 18 to 93, with a median of 59 (the median age of the general population of Miami-Dade County in 2000 was 35.6; see Census, 2000, Summary File 1, Table P13). Given this discrepancy in ages and the dramatic oversampling of individuals with a physical disability, we can hardly claim that our sample was representative of the Miami-Dade County population. However, the sample was generally representative of physically disabled individuals in the county and of their gender, race/ethnicity, and age counterparts without a disabling condition. Of the 900 who, within the screening process, were reported by a family member as having activity limitations, only 559 confirmed this status within the actual interview. Presumably, this discrepancy arose from differing views about the level of activity limitation that defines disability.
Second-wave interviews of 1,495 W1 participants were completed approximately 3 years later. Excluding 100 W1 participants who had died and 59 who were too ill to be interviewed, the second-wave success rate was 82.5%. Offering, when necessary, participant fees of up to $100 dollars clearly facilitated this achievement. Funding problems dictated the necessity of stopping fieldwork as soon as we were confident in achieving an 80% success rate. As a result, the cases lost to interview included 65 that had been located but interviews not yet scheduled, and 53 who were still in the search process. Only 7.7% refused to participate in a second interview, and we gave up on finding only 5%. A comparison between completed participants and all others regardless of reason for exclusion revealed several statistically significant but rather small differences. Cases lost to W2 interviews, together with those left over when fieldwork was stopped, had previously reported lower levels of social stress, socioeconomic status (SES), and pain, and slightly higher levels of both physical limitations and depressive symptoms. The magnitude of these differences varied from 0.10 SD to slightly more than 0.30 SD. In our view, the nature and magnitude of these differences do not seriously challenge the representativeness of subpopulation employed in these analyses or in any way suggest that selection biases may have accounted for the results presented.
A total of 1,455 study participants provided valid data across all study variables employed in the current analysis. This included 785 women (54%), 343 non-Hispanic Whites (24%), 349 Cuban Americans (24%), 320 non-Cuban Hispanics (22%), and 443 African Americans (30%). The average age of the study respondents was 57 years (SD = 17 years; range = 18–93 years). Forty W2 participants had missing data on one or more variables considered in the analyses (3%). These participants differed from those included only in reporting slightly higher levels of depressive symptoms within the W2 interviews.
Measures
Physical limitations
Problems with physical limitations were indexed at both W1 and W2 by using a measure that combined indicators of physical mobility, instrumental daily activities, and basic activities of daily living. This approach provided a relatively comprehensive picture of physical abilities and limitations, capturing variations at both the severe end and the more able end of the limitations spectrum. Drawing from well-established scales (see Fries, Spitz, Kraines, & Holman, 1980; Nagi, 1976; Rosow & Breslau, 1966), nine items were used to assess physical mobility. Problems with instrumental daily activities were assessed using two items from Lawton and Brody’s (1969) scale, and activities of daily living were assessed using eight items drawn from the work of Katz and colleagues (Katz, Downs, Cash, & Grotz, 1970; Katz, Ford, Moskowitz, Jackson, & Jaffee, 1963) and (Jette and Deniston 1978; Jette, 1980). We should note that of these 19 items, 7 were asked only of persons who had confirmed the presence of a physical disability. These items referred to one’s ability to do such things as dress oneself, take a bath/shower, get out of bed, prepare one’s meals, and climb stairs. We assigned individuals not presented with these items responses of “easy to do” on all seven items. In order to assess the potential impact of this decision, we ran all analyses using only items that were asked of all study respondents; the results were substantively identical to the results presented here. The Appendix presents all items used to index physical limitations. We coded the 19 items such that higher scores indicated greater physical limitations. Because response categories for some items involved a 4-point scale and those for other items involved a 5-point scale, we transformed responses to each item into standard scores, which we summed into our measure of physical limitations. We then restandardized these scores for ease of interpretation so that they had a mean of 0 and a standard deviation of 1. We also standardized all other continuous measures in order to maintain consistency in interpretation. The internal reliability coefficient for physical limitations was .95 within both waves of data. We employed this measure of the presence and severity of physical limitations for all but descriptive analyses, which we report as unstandardized scores.
Depressive symptomatology
Depressive symptoms were assessed at both data points using the Center for Epidemiologic Studies–Depression scale (CES-D), which is a highly reliable and widely used measure of depressive symptomatology (Radloff, 1977). From the original 20-item CES-D index, 6 items involving somatic problems were omitted from all analyses to avoid measurement confounding between physical limitations and depressive symptoms (Ormel et al., 2002). These omitted items included problems with eating, keeping your mind on what you are doing, effort, restlessness, talking, and getting going. In completing the CES-D items, participants were asked about their experiences over the past month rather than the past week using response categories of “not at all,” “occasionally,” “frequently,” and “almost all the time.” We coded items such that higher scores indicated higher levels of depressive symptoms, then summed and standardized scores for analysis (W1 α = .81; W2 α = .84).
Pain
Study participants were asked whether they had experienced any bodily pain over the preceding 4 weeks. Those who answered affirmatively were questioned on the frequency and average intensity of such pain. Response categories for the intensity item ranged from “very mild” (1) to “very severe” (5). Those for frequency ranged from “once or twice” (1) to “everyday or almost everyday” (5). We coded respondents who reported no pain over the past 4 weeks as “none” (0) for intensity of pain and “never” (0) for frequency of pain. We coded both items so that higher values indicated greater intensity and frequency of pain. We derived the pain measure by multiplying scores on the two dimensions and then standardizing the resulting products.
Social stress
The role of stress exposure in changes in physical limitations and depressive symptoms was evaluated using measures of chronic stress, daily discrimination, and recent life events as occurring during the approximately 3-year interval between interviews. The chronic stress measure was an adaptation Wheaton’s (1991, 1994) scale, modified to better capture the kinds of enduring stressors older individuals are likely to experience. Daily discrimination (9 items) and recent life events (32 items, past 12 months) were indexed by previously employed measures (Turner & Avison, 2003; Williams, Yu, Jackson, & Anderson, 1997). We standardized all measures of social stress for analysis.
Lifetime major depression
The lifetime occurrence of major depression was measured using the depression module of the World Mental Health version of the Composite International Diagnostic Interview (Kessler & Ustun, 2004). This instrument has been described in greater detail elsewhere (Turner et al., 2006). In the present analyses we employed diagnostic estimates derived from the W1 interviews.
Sociodemographic variables
We used W1 data to control for age, gender, race/ethnicity, and SES. We measured age as a continuous variable. We based estimates of SES on a composite score that equally weighted the occupational level (Hollingshead, 1957), educational attainment, and household income of each participant. To avoid problems of missing data, particularly on the variable of household income, we standardized scores on each of these dimensions, summed them, and divided them by the number of dimensions on which data were available. Table 1 provides descriptive statistics for all study variables.
Table 1.
Description of Study Variables
| Wave 1 |
Wave 2 |
|||
|---|---|---|---|---|
| Variable | M (SD) | Range | M (SD) | Range |
| Physical limitations | 9.64 (12.34) | 1–83 | 9.85 (12.49) | 1–82 |
| Depressive symptoms | 21.60 (6.61) | 0–53 | 21.50 (6.65) | 4–49 |
| Lifetime major depressiona | 0.09 | |||
| Pain | 4.34 (6.90) | 0–25 | 2.83 (4.93) | 0–20 |
| Chronic stress | 4.40 (4.92) | 0–27 | 5.93 (5.35) | 0–31 |
| Daily discrimination | 13.62 (5.02) | 0–39 | 13.63 (4.92) | 4–39 |
| Recent life events | 1.05 (1.50) | 0–12 | 0.89 (1.33) | 0–9 |
| Demographic controls | ||||
| Femalea | 0.54 | |||
| Non-Hispanic Whitea | 0.24 | |||
| Cubana | 0.24 | |||
| Non-Cuban Hispanica | 0.24 | |||
| African Americana | 0.30 | |||
| Age | 57.03 (16.75) | 18–93 | ||
| Socioeconomic statusb | 0 (1) | −2.72–2.60 | ||
Notes: Shown are unstandardized mean scores (SD) N = 1,455.
Mean scores should be interpreted as proportion of individuals who met criteria.
Standardized score for summed occupational prestige, education, and household income.
Analysis Plan
Our analyses began with a correlation matrix in order to show bivariate associations for key study variables. Using structural equation modeling (SEM), we then tested for reciprocal effects between physical limitations and depressive symptoms over a 3-year period. We then employed this modeling process in order to rule out the possibility of spuriousness stemming from prior pain, stress exposure, and lifetime major depression as assessed at W1. Finally, we used SEM to evaluate the potential mediating effects of pain and social stress assessed at W2 on the physical limitation–depressive symptom relationship.
Results
Table 2 provides the correlations among the study variables, including physical limitations, depressive symptoms, lifetime major depression, pain, and social stress. The table reveals several important findings. First, both physical limitations and depressive symptoms showed significant stability across time (i.e., r = .70, p < .001, for physical limitations from W1 to W2). Second, the associations between physical limitations and depressive symptoms were significant for each wave as well as across waves (i.e., r = .16, p < .001 between physical limitations at W1 and depressive symptoms at W2). Furthermore, the measures of lifetime major depression, pain, and stress were significantly associated with both depressive symptoms and physical limitations. These correlations provided initial support for our hypotheses involving reciprocity, spuriousness, and mediation. Based on these findings, we then estimated the SEM.
Table 2.
Correlation Matrix for Study Variables
| Variable | DSa | DSb | PLa | PLb | LMDa | Paina | Painb | CSa | CSb | DDa | DDb | RLEa | RLEb |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DSa | — | ||||||||||||
| DSb | .35** | — | |||||||||||
| PLa | .21** | .16** | — | ||||||||||
| PLb | .14** | .23** | .70** | — | |||||||||
| LMDa | .24** | .15** | .16** | .08** | — | ||||||||
| Paina | .11** | .09** | .57** | .38** | .17** | — | |||||||
| Painb | .12** | .14** | .40** | .53** | .11** | .41** | — | ||||||
| CSa | .25** | .11** | .04 | −.03 | .29** | .17** | .05* | — | |||||
| CSb | .07** | .03 | −.15** | −.19** | .08** | −.05* | .01 | .29** | — | ||||
| DDa | .13** | .00 | .09** | .00 | .12** | .12** | .03 | .33** | .16** | — | |||
| DDb | .02 | .06* | .02 | .04 | .02 | .02 | .05* | .11** | .29** | .34** | — | ||
| RLEa | .18** | .04 | .04 | .01 | .24** | .13** | .09** | .46** | .14** | .28** | .13** | — | |
| RLEb | .07** | .05* | .00 | .02 | .09** | .05* | .13** | .18** | .37** | .14** | .17** | .17** | — |
Notes: N = 1,455. DS = depressive symptoms (Center for Epidemiologic Studies–Depression scale); PL = physical limitations; LMD = lifetime major depression; Pain = intensity* × frequency of bodily pain; CS = chronic stress; DD = daily discrimination; RLE = recent life events.
Measured at wave 1.
Measured at wave 2.
p ≤ .05;
p ≤ .01.
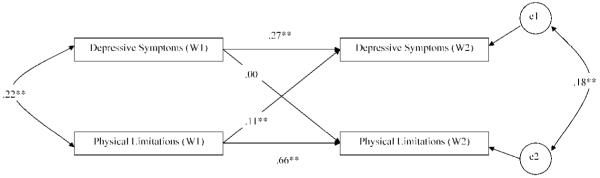
We used AMOS software for the SEM (Arbuckle, 2005). Figure 1 shows the results of our SEM analysis relating to the hypothesized reciprocal effects between physical limitations and depressive symptoms. We included age, gender, race/ethnicity, and SES as control variables but do not show them so that we can more clearly convey the primary findings. Among the control variables in the model, SES and age were negatively associated with depressive symptoms at W2. SES was also negatively associated with physical limitations at W2, and age was positively associated with physical limitations at W2. Being female was positively associated with physical limitations at W2, and both Hispanic groups reported significantly more depressive symptoms at W2 compared to their non-Hispanic White counterparts.
Figure 1.
Reciprocal effects between depressive symptoms and physical limitations. Standardized regression coefficients are shown. N = 1,455. Significant effects for age, gender, race/ethnicity, and socioeconomic status are controlled for in the model but not shown. Model fit: χ2 = 12.26, df = 5; Tucker–Lewis Index = .98; comparative fit index = .99; root mean square error of approximation = .03. W = wave; e1 = error 1; e2 = error 2.
For our model, the chi-square was χ2 (5 N = 1,455) = 12.26, p = .03. The Tucker–Lewis Index (TLI) was .98, the comparative fit index (CFI) was .99, and the root mean square error of approximation was .03. These fit indexes all indicated a good fit of the model to the data (Kline, 2005).
Figure 1 illustrates several findings. First, the stability coefficients for depressive symptoms and physical limitations from W1 to W2 were both significant (b = .27, p < .001, for depressive symptoms; and b = .66, p < .001, for physical limitations). Second and more important, although the level of physical limitations at W1 predicted changes in depressive symptoms (b = .11, p < .001), these results offered no evidence that prior depressive symptoms were of significance in predicting changes in physical limitations. We thus concluded that most of whatever causation may have been involved in the clear relationship between physical limitations and depressive symptomatology over a 3-year period flowed from physical limitations to depressive symptoms rather than in the reverse direction. Although the magnitude of the cross-lagged coefficient for W1 physical limitations was rather modest, the twin facts that this relationship was net of variance shared with depression cross-sectionally and that the prediction involved spans of approximately 3 years suggested substantive as well as statistical significance.
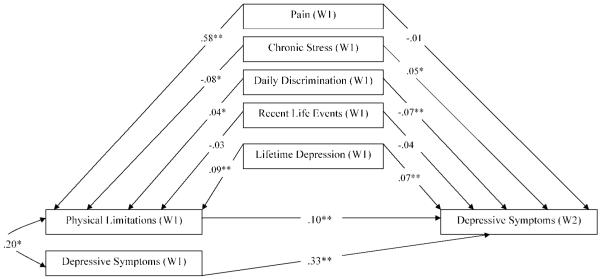
Based on the findings from Figure 1, the remaining analyses focused on W1 physical limitations predicting changes in depressive symptoms. To test the possibility that the physical limitation–depression relationship may have been partially or largely an artifact of associations between these variables and prior levels of pain, stress exposure, and lifetime major depression, we added these variables to the model (see Figure 2) to predict both physical limitations at W1 and depressive symptoms at W2. Results indicated that with pain, stress, and major depression all in the model, the path from physical limitations at W1 to depressive symptoms at W2 remained statistically significant and virtually unchanged (b = .10, p < .001). We concluded that the association between prior physical limitations and changes in depressive symptoms was not an artifact of their shared association with pain, stress exposure, or lifetime major depression.
Figure 2.
Physical limitations predicting changes in depressive symptoms: spurious effects of pain, social stress, and lifetime major depression. Standardized regression coefficients are shown (χ2 = .00, df = 0). N = 1,455. W = wave. *p ≤ .05; **p ≤ .01.
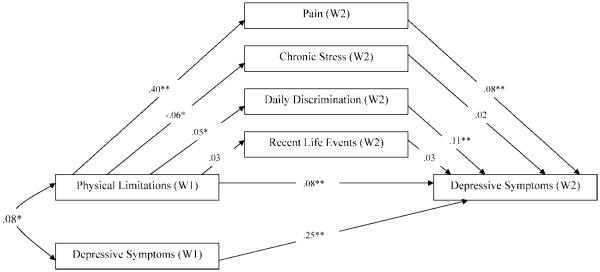
Next, we tested the mediating hypothesis. We proposed that the association between physical limitations and depressive symptoms would be mediated by our indicators of pain and social stress measured at W2. Figure 3 presents these findings. As in Figure 1, we included control variables in the model but do not show them here. The model also indicated a reasonable fit to the data χ2 (19 N = 1,455) = 55.91, p = .00 (TLI = .95; CFI = .99; RMSEA = .04).
Figure 3.
Physical limitations predicting changes in depressive symptoms: mediating effects of pain and social stress. Standardized regression coefficients are shown. N = 1,455. Significant effects for age, gender, race/ethnicity, and socioeconomic status are controlled for in the model but not shown. Model fit: χ2 = 55.91, df = 19; Tucker–Lewis Index = .95; comparative fit index = .99; root mean square error of approximation = .04. Mediation effects using Sobel test: pain, z = 3.03**; chronic stress, z = −0.74; daily discrimination, z = 1.87; recent life events, z = 0.73. W = wave. *p ≤ .05; **p ≤ .01.
Results indicated that physical limitations at W1 predicted pain, chronic stress, and daily discrimination at W2. Pain and daily discrimination also both predicted changes in depressive symptoms. The direct path from physical limitations at W1 to depressive symptoms at W2 was reduced from .11 (see Figure 1) to .09 (p < .01, in Figure 3). With respect to mediating effects, the Sobel test (Sobel, 1982) yielded a highly significant z score of 3.03 for pain. However, neither chronic stress nor recent life events were significant mediators, whereas the mediation effect of daily discrimination was marginally significant statistically (z = 1.87, p < .10). We tested this mediating effect after controlling for depressive symptoms at W1 (b = .25, p < .001). Taken together, the results demonstrated support for the mediating effects of pain and, to a lesser extent, daily discrimination on the association between prior physical limitations and changes in depressive symptoms.
Discussion
This study evaluated the contention that the association between physical limitations and depressive symptoms arises from causal reciprocity, assessed the possibility that this relationship is artifactual, and assessed potential mediating effects of related third variables. Consistent with prior research (Aneshensel et al., 1984; Ormel et al., 2002), we found that prior physical limitations predict changes in depressive symptoms. However, we observed no such symmetry in the capacity of W1 depressive symptoms to predict changes in physical limitations over a 3-year period. That is, although W1 physical limitations predicted changes in depressive symptoms, there was no hint of a reverse association. Accordingly, we argue that much of whatever causation may be involved in the linkage between physical limitations and depressive symptomatology over a 3-year period flows from limitations to depression rather than in the reverse direction. These findings are consistent with the view that physical limitations represent a source of chronic or enduring stress (Turner & McLean, 1989; Turner & Noh, 1988) and the observation that chronic stress is a particularly strong predictor of depressive symptoms (Turner et al., 1995).
The failure to observe either an association between prior depressive symptomatology or prior depressive disorder and changes in physical limitations might be seen as contradicting an array of previous studies (see Armenian et al., 1998; Bruce et al., 1994; Cronin-Stubbs et al., 2000; Dunlop et al., 2005; Jiang et al., 2004; Lenze et al., 2005; Penninx et al., 1998, 1999, 2000). However, most such studies focused on the capacity of prior depressive symptoms (or depressive disorder) to predict the onset of disability rather than changes in the level of physical limitations. Failing to confirm this body of evidence may well arise from the fact that the variance shared by prior physical limitations and depressive symptoms is held constant in analyses addressing changes in limitations over time. In addition, the relatively high stability coefficient observed for physical limitations means that there was more variability in depressive symptoms remaining to be explained. Although this difference in stability of measures may have impacted results to some extent, it does not, in our view, challenge the clear findings presented. The results presented here are consistent with those reported from a population study of elderly biracial participants in which prior depressive symptoms were not associated with declines in physical performance (Everson-Rose et al., 2005). However, readers should bear in mind that the process by which depression may get translated into an increase in physical limitations may take longer than the 3-year follow-up period studied here. As Kelley-Moore and Ferraro (2005) argued, “Health decline is a process that occurs over several years rather than instantaneously” (p. 386).
Although a large body of research has demonstrated a robust correlation between physical limitations and depressive symptoms, few studies have considered the extent to which this apparent linkage might be spurious—that is, driven by factors known to be associated with both indicators of health. We examined the relationship between prior levels of physical limitations and changes in depressive symptoms in the context of measures of pain, stress exposure, and prior lifetime occurrence of major depressive disorder. After controlling for these potential sources of spuriousness, we found that the magnitude of the coefficient representing the association remained strong and statistically significant. This result allows for increased confidence that this frequently observed relationship is real rather than artifactual in nature.
The study also presents evidence of possible mechanisms by which physical limitations are translated into increased mental health risk. We found strong evidence to support the conclusion that the relationship between prior physical limitations and subsequent changes in depressive symptoms is mediated by intervening levels of pain and, to a lesser extent, daily discrimination. These results suggest that physical limitations may partially be translated into increased risk for depressive symptoms through a process of stress generation analogous to that described by Hammen (1991, 2006). That is, in addition to having direct effects, physical limitations appear to indirectly influence depressive symptoms by elevating risk for higher levels of pain and exposure to social stress. Among the stress measures, daily discrimination appears the most salient. This may be a reflection of experiences of stigma associated with being physically limited (Crandall & Moriarty, 1995) or may arise from the fact that approximately three quarters of the sample was drawn from racial/ethnic minority populations.
Several limitations to the current investigation are worthy of note. For one thing, it employed self-report physical limitation measures rather than objective assessments of physical performance. Although it is possible that objective measures of physical limitations might yield different results, prior research provides moderate to strong evidence for the validity of such self-reports evaluated with respect to objectively assessed physical limitations (Cress et al., 1995; Judge, Schechtman, & Cress, 1996; Kempen, Sullivan, van Sonderen, & Ormel, 1999; Myers, Holliday, Harvey, & Hutchinson, 1993). Also reassuring is the fact that these results are generally consistent with prior research employing objective measures of physical performance (see Everson-Rose et al., 2005).
Our consideration of the possibility that the physical limitation–depressive symptom linkage may arise from shared association with influential third variables focused on several factors that prior research has shown to be associated with both physical limitations and depressive symptoms. Clearly, these analyses are far from exhaustive, being limited to self-reports of bodily pain, stress exposure, and lifetime major depression. We also considered only a limited number of potential mediators (i.e., pain, chronic stress, daily discrimination, and recent life events). Our analyses omitted the evaluation of nondisabling medical conditions, cognitive functioning (Bruce, 2001), availability of instrumental support (Kennedy et al., 1990), and several personal resources such as mastery and self-esteem that are relevant to depression (Turner & Lloyd, 1999; Turner, Taylor, & Van Gundy, 2004).
Such limitations notwithstanding, the present study builds on prior research in several important ways. First, it offers a prospective assessment of the potential reciprocal relationships between physical limitations and depressive symptoms based on a community-based sample controlled on gender, age, SES, racial/ethnic variations, and the prior lifetime occurrence of one or more major depressive episodes. Although several prior studies assessing the temporal and reciprocal associations between physical limitations and depressive symptoms have involved community samples (see Geerlings et al., 2001; Meeks et al., 2000; Ormel et al., 2002), these studies focused on participants of a limited age range and a limited range of racial/ethnic diversity. Second, this study contributes to increased confidence that the physical limitation–depression relationship is not spurious, being an association of potential theoretical and practical significance.
In the context of the long-standing argument that physical limitations and pain represent important dimensions of chronic stress (Gurland et al., 1988; Turner & Noh, 1988), it seemed crucial to evaluate the mental health significance of physical limitations in the context of other sources of social stress. Our results leave little doubt that over a 3-year period, physical limitations represent a significant risk factor for depressive symptomatology independent of the effects of other sources of stress exposure, and that this presumably causal linkage accounts for much of the often reported cross-sectional and longitudinal relationship between physical limitations and depressive symptoms.
Acknowledgments
An earlier version of this article was presented at the 102nd Annual Meeting of the American Sociological Association, New York, in August 2007. We are grateful to the reviewers for their conscientious and helpful critiques of our paper. This work was supported by Grants R01DA13292 and R01DA16429 from the National Institute on Drug Abuse to R. Jay Turner.
Appendix
Items for Physical Limitation Scale
| Items asked of all respondents |
| 1. Reach up and get a 5-pound object (such as a bag of sugar) from just above your head |
| 2. Bend down to pick up an object (like a piece of clothing) from the floor |
| 3. Turn faucets on/off |
| 4. Walk ¼ mile |
| 5. Stoop or crouch down |
| 6. Lift 10 pounds |
| 7. Sit for more than 2 hr |
| 8. Stand for long periods, such as 30 min |
| 9. Stand up from sitting |
| 10. Walk more than a mile |
| 11. Moderate activities such as moving a table, pushing a vacuum cleaner, bowling, or playing golf |
| 12. Vigorous activities such as running, lifting heavy objects, or participating in strenuous sports |
| Items asked only of those screened as disabled |
| 13. Can you prepare your own meals? |
| 14. Can you do your housework? |
| 15. Can you dress/undress self? |
| 16. Can you get in/out of bed? |
| 17. Can you take bath/shower? |
| 18. Can you get to the bathroom on time? |
| 19. Can you climb up stairs? |
Footnotes
M. D. Gayman conducted all original data analysis and wrote the paper. R. J. Turner contributed to revising the paper. M. Cui contributed to the final data analysis.
References
- Aneshensel CS, Frerichs RR, Huba GJ. Depression and physical illness: A multiwave, nonrecursive causal model. Journal of Health and Social Behavior. 1984;25:350–371. [PubMed] [Google Scholar]
- Arbuckle JL. AMOS 6.0 user’s guide. SPSS; Chicago, IL: 2005. [Google Scholar]
- Armenian H, Pratt LA, Gallo J, Eaton WW. Psychopathology as a predictor of disability: A population-based follow-up study in Baltimore, Maryland. American Journal of Epidemiology. 1998;148:269–275. doi: 10.1093/oxfordjournals.aje.a009635. [DOI] [PubMed] [Google Scholar]
- Bair MJ, Robinson RL, Katon W, Kroenke K. Depression and pain comorbidity: A literature review. Archives of Internal Medicine. 2003;163:2433–2445. doi: 10.1001/archinte.163.20.2433. [DOI] [PubMed] [Google Scholar]
- Benjamin S, Morris S, McBeth J, Macfarlane GJ, Silman AJ. The association between chronic widespread pain and mental disorder. Arthritis & Rheumatism. 2000;43:561–567. doi: 10.1002/1529-0131(200003)43:3<561::AID-ANR12>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- Breslau N. Depressive symptoms, major depression, and generalized anxiety: A comparison of self-reports on CES-D and results from diagnostic interviews. Psychiatry Research. 1985;15(3):219–229. doi: 10.1016/0165-1781(85)90079-4. [DOI] [PubMed] [Google Scholar]
- Bromberger JT, Matthews KA. A longitudinal study of the effects of pessimism, trait anxiety, and life stress on depressive symptoms in middle-aged women. Psychology and Aging. 1996;11:207–213. doi: 10.1037//0882-7974.11.2.207. [DOI] [PubMed] [Google Scholar]
- Bruce ML. Depression and disability in late life: Directions for future research. American Journal of Geriatric Psychiatry. 2001;9(2):102–112. [PubMed] [Google Scholar]
- Bruce ML, Seeman TE, Merrill SS, Blazer DG. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. American Journal of Public Health. 1994;84:1796–1799. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bryant LL, Scarbro S, Baxter J. Pain, chronic conditions, and worsening physical performance. The Gerontologist. 2001;41(Special Issue I):290–291. [Google Scholar]
- Chiriboga DA, Black SA, Aranda M, Markides K. Stress and depressive symptoms among Mexican American elders. Journal of Gerontology: Psychological Sciences. 2002;57B:P559–P568. doi: 10.1093/geronb/57.6.p559. [DOI] [PubMed] [Google Scholar]
- Corruble E, Guelfi JD. Pain complaints in depressed inpatients. Psychopathology. 2000;33:307–309. doi: 10.1159/000029163. [DOI] [PubMed] [Google Scholar]
- Crandall CS, Moriarty D. Physical illness stigma and social rejection. British Journal of Social Psychology. 1995;34:67–83. doi: 10.1111/j.2044-8309.1995.tb01049.x. [DOI] [PubMed] [Google Scholar]
- Cress ME, Schechtman KB, Mulrow CD, Fiatarone MA, Gerety MB, Buchner DM. Relationship between physical performance and self-perceived physical function. Journal of the American Geriatrics Society. 1995;43:93–101. doi: 10.1111/j.1532-5415.1995.tb06372.x. [DOI] [PubMed] [Google Scholar]
- Cronin-Stubbs D, Mendes de Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA. Six-year effect of depressive symptoms on the course of physical disability in community-living older adults. Archives of Internal Medicine. 2000;160:3074–3080. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- Cuijpers P, Smit F. Subthreshold depression as a risk indicator for major depressive disorder: A systematic review of prospective studies. Acta Psychiatrica Scandinavica. 2004;109:325–331. doi: 10.1111/j.1600-0447.2004.00301.x. [DOI] [PubMed] [Google Scholar]
- Dunlop DD, Manheim LM, Song J, Lyons JS, Chang RW. Incidence of disability among preretirement adults: The impact of depression. American Journal of Public Health. 2005;95:2003–2008. doi: 10.2105/AJPH.2004.050948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Everson-Rose S, Skarupski KA, Bienias JL, Wilson RS, Evans DA, Mendes de Leon CF. Do depressive symptoms predict declines in physical performance in an elderly, biracial population? Psychosomatic Medicine. 2005;67:609–615. doi: 10.1097/01.psy.0000170334.77508.35. [DOI] [PubMed] [Google Scholar]
- Farmer MM, Ferraro KF. Distress and perceived health: Mechanisms of health decline. Journal of Health and Social Behavior. 1997;38:298–311. [PubMed] [Google Scholar]
- Fries JF, Spitz P, Kraines RG, Holman HR. Measurement of patient outcomes in arthritis. Arthritis and Rheumatism. 1980;23(2):137–145. doi: 10.1002/art.1780230202. [DOI] [PubMed] [Google Scholar]
- Geerlings SW, Beekman ATF, Deeg DJH, Twisk JWR, Van Tilburg W. The longitudinal effect of depression on functional limitations and disability in older adults: An eight-wave prospective community-based study. Psychological Medicine. 2001;31:1361–1371. doi: 10.1017/s0033291701004639. [DOI] [PubMed] [Google Scholar]
- Geerlings SW, Beekman ATF, Deeg DJH, Van Tilburg W. Physical health and the onset and persistence of depression in older adults: An eight-wave prospective community-based study. Psychological Medicine. 2000;30:369–380. doi: 10.1017/s0033291799001890. [DOI] [PubMed] [Google Scholar]
- Geronimus AT, Hicken M, Keene D, Bound J. “Weathering” and age patterns of allostatic load scores among blacks and whites in the United States. American Journal of Public Health. 2006;96:826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grigsby J, Morgenstern NE, Kaye K, Shetterly SM, Baxter J, Hamman RF. Effects of pain on physical functioning and ADL/IADL capacity: Results from the San Luis Valley Health and Aging Study. Journal of the American Geriatrics Society. 1999;47:S13. Abstract. [Google Scholar]
- Gurland BJ, Wilder DE, Berkman C. Depression and disability in the elderly: Reciprocal relations and changes with age. International Journal of Geriatric Psychiatry. 1988;3:163–179. [Google Scholar]
- Hammen C. The generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hammen C. Stress generation in depression: Reflections on origins, research, and future directions. Journal of Clinical Psychology. 2006;62:1065–1082. doi: 10.1002/jclp.20293. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB. Two factor index of social position. Author; New Haven, CT: 1957. [Google Scholar]
- Horwath E, Johnson J, Klerman GL, Weissman MM. Depressive symptoms as relative and attributable risk-factors for 1st-onset depression. Archives of General Psychiatry. 1992;49:817–823. doi: 10.1001/archpsyc.1992.01820100061011. [DOI] [PubMed] [Google Scholar]
- Jette AM. Functional status index: Reliability of a chronic disease evaluation instrument. Archives of Physical Medicine and Rehabilitation. 1980;61:395–401. [PubMed] [Google Scholar]
- Jette AM, Deniston OL. Inter-observer reliability of a functional status assessment instrument. Journal of Chronic Diseases. 1978;31:573–580. doi: 10.1016/0021-9681(78)90017-6. [DOI] [PubMed] [Google Scholar]
- Jiang J, Tang Z, Futatsuka M, Zhang K. Exploring the influence of depressive symptoms on physical disability: A cohort study of elderly in Beijing, China. Quality of Life Research. 2004;13:1337–1346. doi: 10.1023/B:QURE.0000037500.26166.0c. [DOI] [PubMed] [Google Scholar]
- Judge JO, Schechtman K, Cress E. The relationship between physical performance measures and independence in instrumental activities of daily living. Journal of the American Geriatrics Society. 1996;44:1332–1441. doi: 10.1111/j.1532-5415.1996.tb01404.x. [DOI] [PubMed] [Google Scholar]
- Katon W, Ciechanowski P. Impact of major depression on chronic medical illness. Journal of Psychosomatic Research. 2002;53:859–863. doi: 10.1016/s0022-3999(02)00313-6. [DOI] [PubMed] [Google Scholar]
- Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. The Gerontologist. 1970;10:20–30. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffee MW. Studies of illness in the aged: The index of ADL. A standardized measure of biological and psychosocial function. Journal of the American Medical Association. 1963;185:914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Kelley-Moore JA, Ferraro KF. A 3-D model of health decline: Disease, disability, and depression among black and white older adults. Journal of Health and Social Behavior. 2005;46:376–391. doi: 10.1177/002214650504600405. [DOI] [PubMed] [Google Scholar]
- Kempen GIJM, Sullivan M, van Sonderen E, Ormel J. Performance-based and self-reported physical functioning in low-functioning older persons: Congruence of change and the impact of depressive symptoms. Journal of Gerontology: Psychological Sciences. 1999;54B:P380–P386. doi: 10.1093/geronb/54b.6.p380. [DOI] [PubMed] [Google Scholar]
- Kennedy GJ, Kelman H, Thomas C. The emergence of depressive symptoms in late life: The importance of declining health and increasing disability. Journal of Community Health. 1990;15(2):93–104. doi: 10.1007/BF01321314. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Mickelson KD, Williams DR. The prevalence, distribution, and mental health correlates of perceived discrimination in the United States. Journal of Health and Social Behavior. 1999;40:208–230. [PubMed] [Google Scholar]
- Kessler RC, Ustun TB. The World Mental Health (WMH) survey initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI) International Journal of Methods in Psychiatric Research. 2004;13:93–121. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2nd ed. Guilford Press; New York: 2005. [Google Scholar]
- Lawton PM, Brody EM. Assessment of older people: Self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9:179–186. [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, et al. The association of late-life depression and anxiety with physical disability—A review of the literature and prospectus for future research. American Journal of Geriatric Psychiatric. 2001;9(2):113–135. [PubMed] [Google Scholar]
- Lenze EJ, Schulz R, Martire LM, Zdaniuk B, Glass T, Kop WJ, et al. The course of functional decline in older people with persistently elevated depressive symptoms: Longitudinal findings from the Cardiovascular Health Study. Journal of the American Geriatrics Society. 2005;53:569–575. doi: 10.1111/j.1532-5415.2005.53202.x. [DOI] [PubMed] [Google Scholar]
- Lichtenstein MJ, Dhanda R, Cornell JE, Escalante A, Hazuda HP. Disaggregating pain and its effect on physical functional limitations. Journal of Gerontology: Medical Sciences. 1998;53A:M361–M371. doi: 10.1093/gerona/53a.5.m361. [DOI] [PubMed] [Google Scholar]
- Lin N, Ensel WM. Life stress and health: Stressors and resources. American Sociological Review. 1989;54:382–399. [Google Scholar]
- McEwen BS, Seeman T. Protective and damaging effects of mediators of stress: Elaborating and testing the concepts of allostasis and allostatic load. Annals of the New York Academy of Sciences. 1999;896:30–47. doi: 10.1111/j.1749-6632.1999.tb08103.x. [DOI] [PubMed] [Google Scholar]
- Meeks S, Murrell SA, Mehl RC. Longitudinal relationships between depressive symptoms and health in normal older and middle-aged adults. Psychology and Aging. 2000;15:100–109. doi: 10.1037//0882-7974.15.1.100. [DOI] [PubMed] [Google Scholar]
- Myers AM, Holliday PJ, Harvey KA, Hutchinson KS. Functional performance measures: Are they superior to self-assessments? Journal of Gerontology: Medical Sciences. 1993;48:M196–M206. doi: 10.1093/geronj/48.5.m196. [DOI] [PubMed] [Google Scholar]
- Nagi SZ. An epidemiology of disability among adults in the United States. Milbank Memorial Fund Quarterly: Health and Society. 1976;54:439–467. [PubMed] [Google Scholar]
- Nierop A, Bratsikas A, Zimmermann R, Ehlert U. Are stress-induced cortisol changes during pregnancy associated with postpartum depressive symptoms? Psychosomatic Medicine. 2006;68:931–937. doi: 10.1097/01.psy.0000244385.93141.3b. [DOI] [PubMed] [Google Scholar]
- Ormel J, Rijsdijk FV, Sullivan M, van Sonderen E, Kempen GIJM. Temporal and reciprocal relationship between IADL/ADL disability and depressive symptoms in late life. Journal of Gerontology: Psychological Sciences. 2002;57B:P338–P347. doi: 10.1093/geronb/57.4.p338. [DOI] [PubMed] [Google Scholar]
- Pavalko EK, Mossakowski KN, Hamilton VJ. Does perceived discrimination affect health? Longitudinal relationships between work discrimination and women’s physical and emotional health. Journal of Health and Social Behavior. 2003;44:18–33. [PubMed] [Google Scholar]
- Pearlin LI, Lieberman M, Menaghan E, Mullan J. The stress process. Journal of Health and Social Behavior. 1981;22:337–356. [PubMed] [Google Scholar]
- Penninx BWJH, Deeg DJH, van Eijk JTM, Beekman ATF, Guralnik JM. Changes in depression and physical decline in older adults: A longitudinal perspective. Journal of Affective Disorders. 2000;61:1–12. doi: 10.1016/s0165-0327(00)00152-x. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Guralnik JM, Ferrucci L, Simonsick EM, Deeg DJH, Wallace RB. Depressive symptoms and physical decline in community-dwelling older persons. Journal of the American Medical Association. 1998;279:1720–1726. doi: 10.1001/jama.279.21.1720. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Leveille S, Ferrucci L, van Eijk JTM, Guralnik JM. Exploring the effect of depression on physical disability: Longitudinal evidence from the Established Populations for Epidemiologic Studies of the Elderly. American Journal of Public Health. 1999;89:1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychosocial Measurement. 1977;1:385–401. [Google Scholar]
- Roberts RE, Kaplan GA, Shema SJ, Strawbridge WJ. Does growing old increase the risk for depression? American Journal of Psychiatry. 1997;154:1384–1390. doi: 10.1176/ajp.154.10.1384. [DOI] [PubMed] [Google Scholar]
- Robles TF, Glaser R, Kiecolt-Glaser JK. Out of balance: A new look at chronic stress, depression, and immunity. Current Directions in Psychological Science. 2005;14(2):111–115. [Google Scholar]
- Rosow I, Breslau N. A Guttman Health Scale for the aged. Journal of Gerontology. 1966;21:556–559. doi: 10.1093/geronj/21.4.556. [DOI] [PubMed] [Google Scholar]
- Ross CE, Mirowsky J. Neighborhood disadvantage, disorder, and health. Journal of Health and Social Behavior. 2001;42:258–276. [PubMed] [Google Scholar]
- Ruoff GE. Depression in the patient with chronic pain. Journal of Family Practice. 1996;43(6):S25–S33. [PubMed] [Google Scholar]
- Schieman S, Plickert G. Functional limitations and changes in levels of depression among older adults: A multiple-hierarchy stratification perspective. Journal of Gerontology: Social Sciences. 2007;62B:S36–S42. doi: 10.1093/geronb/62.1.s36. [DOI] [PubMed] [Google Scholar]
- Seeman TE, Singer BH, Rowe JW, Horwitz RI, McEwen BS. Price of adaptation—allostatic load and its health consequences. Archives of Internal Medicine. 1997;157:2259–2268. [PubMed] [Google Scholar]
- Sobel ME. Asymptotic intervals for indirect effects in structural equations models. In: Leinhart S, editor. Sociological methodology. Jossey-Bass; San Francisco: 1982. pp. 290–312. [Google Scholar]
- Taylor J, Turner RJ. Perceived discrimination, social stress, and depression in the transition to adulthood: Racial contrasts. Social Psychology Quarterly. 2002;65:213–225. [Google Scholar]
- Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk factors for falls, incontinence, and functional dependence: Unifying the approach to geriatric syndromes. Journal of the American Medical Association. 1995;273:1348–1353. [PubMed] [Google Scholar]
- Turner RJ, Avison WR. Status variations in stress exposure: Implications for the interpretation of research on race, socioeconomic status, and gender. Journal of Health and Social Behavior. 2003;44:488–505. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA. The stress process and the social distribution of depression. Journal of Health and Social Behavior. 1999;40:374–404. [PubMed] [Google Scholar]
- Turner RJ, Lloyd DA, Taylor J. Physical disability and mental health: An epidemiology of psychiatric and substance use disorders. Rehabilitation Psychology. 2006;51(3):214–223. [Google Scholar]
- Turner RJ, McLean PD. Physical disability and psychological distress. Rehabilitation Psychology. 1989;34(4):225–242. [Google Scholar]
- Turner RJ, Noh S. Physical disability and depression: A longitudinal analysis. Journal of Health and Social Behavior. 1988;29:23–37. [PubMed] [Google Scholar]
- Turner RJ, Taylor J, Van Gundy K. Personal resources and depression in the transition to adulthood: Ethnic comparisons. Journal of Health and Social Behavior. 2004;45:34–52. doi: 10.1177/002214650404500103. [DOI] [PubMed] [Google Scholar]
- Turner RJ, Wheaton B. Checklist measures of stressful life events. In: Gordon L, Cohen S, Kessler R, editors. Measuring stress: A guide for health and social scientists. Oxford University Press; Oxford, England: 1995. pp. 29–58. [Google Scholar]
- Turner RJ, Wheaton B, Lloyd DA. The epidemiology of social stress. American Sociological Review. 1995;60:104–125. [Google Scholar]
- U.S. Census Bureau . Miami-Dade County, Summary File 1, Table 13. 2000. [Google Scholar]
- Wheaton B. The specification of chronic stress: Models and measurement; Annual Meeting of the Society for the Study of Social Problems; Cincinnati, OH. 1991; Aug, Paper Presentation. [Google Scholar]
- Wheaton B. Sampling the stress universe. In: Avison WR, Gotlib IH, editors. Stress and mental health. Plenum Press; New York: 1994. pp. 77–115. [Google Scholar]
- Williams DR, Yu Y, Jackson JS, Anderson NB. Racial differences in physical and mental health: Socioeconomic status, stress and discrimination. Journal of Health Psychology. 1997;2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- Yang Y, George LK. Functional disability, disability transitions, and depressive symptoms in late life. Journal of Aging and Health. 2005;17:263–292. doi: 10.1177/0898264305276295. [DOI] [PubMed] [Google Scholar]
- Zeiss AM, Lewinsohn PM, Rohde P, Seeley JR. Relationship of physical disease and functional impairment to depression in older people. Psychology and Aging. 1996;11:572–581. doi: 10.1037//0882-7974.11.4.572. [DOI] [PubMed] [Google Scholar]